Abstract
Objective
To assess the impact of the addition of 12 maternity leave (ML) weeks (2011), a pay for performance (P4P) exclusive breastfeeding (EBF) promotion strategy (2015), and the COVID-19 pandemic in EBF inequalities in Chile.
Study design
Interrupted time-series analyses (ITSAs).
Methods
Aggregated national EBF data by municipality and month were collected from 2009 to 2020. We assess the impact of the three events in EBF inequalities using two procedures: 1. ITSA stratified by municipal SES quintiles (Q1-Q5); 2. Calculating the EBF slope index of inequality (SII).
Results
The EBF prevalence was higher in lower SES municipalities before and after the three time-events. No impact in EBF inequalities was observed after the extended ML. The P4P strategy increased EBF at six months in all SES quintiles (effect size between 4% and 5%), but in a higher level in poorer municipalities (SII: −0.36% and −1.05%). During COVID-19, wealthier municipalities showed a slightly higher EBF at six months prevalence (SII: 1.44%).
Conclusion
The null impact of the extended ML in EBF inequalities could be explained by a low access to ML among affiliated to the public health system (20%). The P4P strategy includes multiple interventions that seemed effective in increasing EBF across all SES quintiles, but further in lower quintiles. The restrictions in healthcare access in poorer municipalities could explain EBF inequalities during COVID-19.
Keywords: Exclusive breastfeeding, Interrupted time-series, Health policy, COVID-19, Maternity leave, Socio-economic inequalities, Chile
Introduction
The multiple benefits of exclusive breastfeeding (EBF), for children and their mothers, are well established.1, 2, 3, 4
Kawachi describes health inequalities (HI) as ‘measurable unequal distribution, or differences, on a health outcome across individuals or defined population groups’.5
HI could be linked to cultural, ethnic, historical, socio-economic, regional, geographical, and educational factors, among others.6 , 7 These inequalities have also been observed in EBF prevalence, between and within countries.8 , 9
Several countries have introduced successful policies to increase EBF prevalence, such as the Baby-friendly Hospital Initiative; specialised training for health professionals; counselling for mothers and their families; regulation of formula milk sales and marketing; and paid maternity leave (ML).1 , 2 , 10 However, only a few of these interventions have documented a decrease in EBF inequalities.6 , 11 , 12 Some studies have reported that ML could be successful in increasing EBF; however, this policy might present inequalities according to socio-economic status (SES).13 , 14
In the past decade, Chile implemented two policies that directly and indirectly promoted EBF (see Supplemental Table 1): the addition of 12 weeks of ML in October 2011, bringing the total to 24 weeks (five and a half months) and a Pay for Performance (P4P) strategy (usually defined as financial incentives or rewards for healthcare workers), in January 2015.15 , 16 The P4P strategy was designed to improve healthcare goals accomplishment in public healthcare centres (PHCC).17 , 18 In addition, the COVID-19 pandemic revealed deep inequalities in access to healthcare services, increasing household duties in women's and a rise in female unemployment. All these factors could have affected EBF practices.19
A recently Chilean study reported that EBF at six months prevalence was of 49.2% in 2009 and 64.8% by November 2020, successfully achieving the 2025 WHO goal of at least 50% of EBF.20 That same study reported no effect of the extended ML in EBF prevalence, an increase in EBF prevalence at three months by 3.10% and at six by 5.6% after the P4P strategy; and a 4.5% decrease in EBF only at three months after COVID-19.20 However, there were reported differences in EBF by urban and rural areas, and by geographic zones, despite the implementation of national strategies to promote EBF.21 While this study reported differences in the impact of the policies and COVID-19 per region, it did not analyse the impact of these events by SES.
The present article aims to analyse the impact in EBF inequalities by SES – at three and six months – after the extended ML introduced in 2011, the P4P strategy implemented in 2015, and COVID-19 in Chile. We hypothesise that the two policies and COVID-19 reflected in EBF inequalities towards lower-SES municipalities.
Methods
Study design and setting
This is a nationwide study, with data of women and children attending Chile's public healthcare system and affiliated to the National Health Trust (FONASA). The latter comprises around 80% of Chilean women and children,22 covering mainly women and those who are poorer, older, and more ill. The other 20% of the population is attended in the private healthcare system, which is based on private insurers (ISAPREs).23
We used interrupted time-series analyses (ITSAs) to measure changes in EBF inequalities, following the introduction of the two policies and COVID-19. In brief, an ITSA assesses whether there are changes over time in the trends of a determined outcome (EBF prevalence), after a specific event (intervention or a natural experiment), and compares it to an estimated counterfactual trend based on pretreatment observations.24 , 25
Variables and data collection
Exclusive breastfeeding rates
EBF prevalence included monthly records from 324 Chilean municipalities, from January 2009 to November 2020. Data were obtained from the official PHCC feeding registries, recorded at the three- and six-months' health check-ups. The healthcare professionals registered if a child had: EBF or partial breastfeeding; formula or solid food. Registration followed the WHO definition of EBF: ‘Exclusive breastfeeding refers to being uniquely fed by breast milk, from the mother, wet nurse, or pumped milk, without receiving any other kind of food or liquid unless a health professional prescribes a medicament, such as syrup or drops, vitamins or minerals’. This definition includes children who occasionally receive small quantities of water.26 The registries from all PHCC are later collected and summarised per municipality.
Figures of the number of children with up-to-date check-ups were also obtained from the PHCC registries. The following definition was used for up-to-date check-ups: ‘children who attended health check-ups performed at the age of one, three, six, twelve and twenty months’.27
The EBF percentages were calculated using the monthly number of children with EBF (at three or six months) per municipality, divided by the number of children with health check-ups per municipality.
Interventions (predictors)
This study included three time-events, namely two policies and the COVID-19 pandemic:
-
1.
In October 2011, 12 extra weeks of ML were added, bringing the total to 24 weeks. The extended ML also incorporated more flexibility in ML access, aiming to increase ML access in women with informal jobs. Preintervention period was from January 2009 to September 2011, and the intervention period was from October 2011 to December 2014.
-
2.
In January 2015, a P4P strategy was implemented to promote EBF at six months in PHCC, aiming to encourage health workers to increase EBF promotion. The preintervention period was from January 2009 to December 2014, and the intervention period was from January 2015 to November 2020.
-
3.
March 2020 was the beginning of the COVID-19 pandemic in Chile. The preintervention was considered from January 2015 to March 2020, and the intervention period was from April 2020 to November 2020.
Municipal SES
The municipal SES was measured using the Índice de Desarrollo Socioeconómico (Index of Socioeconomic Development, ISED).28 Gattini developed the ISED in 2013 to enable a better comparison of SES among Chilean municipalities. This index categorises 324 of the 346 Chilean municipalities. Two municipalities were excluded in the SES categorization because they did not include all the basic data, and another 20 were excluded because they had fewer than 2000 inhabitants. The index includes measures of poverty, education, income, life expectancy, and child mortality rates (Table 1 ). While the ISED was originally broken down into 10 deciles, we merged the 10 categories into quintiles to reduce dispersion, with the first quintile being the lowest SES and the fifth quintile the highest. To assess if there were changes in municipal SES during our study period, we compared the municipal rate of people under the poverty line, using data from the National Survey of Socio-Economic Characterisation (Encuesta de Caracterización Socioeconómica Nacional) published in 2011, 2013, 2015, and 2017.29 The Survey was not performed in 2019. No changes in municipal SES were observed during this period (data not shown).
Table 1.
Socio-economic development and health indicators for each municipal socio-economic quintilea in 2013.
| Quintile | Number of municipalities | Population (thousand) | ISEDc average | Economy |
Education |
Housing & hygiene |
Life expectancy |
Human development index | PYLLb |
Swaroop Index |
Infant mortality |
||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Monthly per capita income ($1000) | Poverty % 2006–2011 | Schooling years 2006–2011 | % houses with good or acceptable housing material | % households with running water & pipes | Years (2005–2010) | Ratea1000 habitants 2007–2011 |
% deaths 50+ years/100 deaths 2011 |
a1000 born alive 2009–2011 | |||||
| 1 | 176 | 3347.3 | 0.475 | 134.5 | 21.1 | 8.5 | 75.8 | 74 | 76.1 | 0.450 | 84.4 | 76.2 | 7.6 |
| 2 | 72 | 3306.2 | 0.589 | 164.8 | 16.2 | 9.6 | 81.2 | 91.7 | 76.8 | 0.531 | 77.2 | 73.2 | 8.0 |
| 3 | 36 | 3413.0 | 0.651 | 206.7 | 14.4 | 10.5 | 84.1 | 95.0 | 77.5 | 0.594 | 71.7 | 74.8 | 7.9 |
| 4 | 22 | 3350.5 | 0.675 | 211.7 | 13.2 | 10.8 | 85.6 | 97.2 | 78.2 | 0.625 | 62.1 | 73.9 | 7.6 |
| 5 | 24 | 3501.4 | 0.769 | 399.4 | 7.5 | 11.8 | 89.0 | 98.5 | 78.4 | 0.714 | 69.5 | 77.1 | 7.1 |
Table adapted from Gattini et al.28
Deciles in original table were merged into quintiles.
PYLL: potential years of life lost.
Index of Socio-economic Development.
Covariables
Seasonality
To correct for seasonality, we incorporated a fixed-effect monthly dummy in the models,1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12 with the first month (January) serving as a reference category.
Number of municipalities with EBF data
This variable consisted of the total monthly national number of municipalities that reported data in EBF and was included because the EBF recording could have changed during the study period.
Accessibility to ML
More flexible norms for ML access were introduced together with the extra 12 weeks added to ML; however, no changes in ML access rate were observed during the study period (20% across the period).30 The ML access rate was calculated using monthly aggregated national numbers of ML issued to affiliated to FONASA and divided by the number of new-borns affiliated to FONASA. The Social Welfare Superintendence supplied and authorized the use of the ML data, which is collected by the ML Management and Information System – SIMAT.31
Data analysis
We first described the mean prevalence of EBF at three and six months by ISED quintiles, before and after the three time-events. Later, we ran several ITSA. The ITSA assumed that the SES EBF trends would have not been affected if the three time-events would not have occurred and that no other major interventions were implemented. In our study, the time-series had three segmented point. Each was analysed using independent models to avoid an overlapping effect of the interventions (extended ML from January 2009 to December 2014; P4P from January 2009 to November 2020; and the COVID-19 pandemic from January 2015 to November 2020).
We performed our EBF inequality analyses in two steps. First, we ran ITSA models of the effect of each time-event in EBF prevalence, stratifying by ISED SES quintiles and analysing heterogeneity between quintiles with the Cochran Q test.32 The heterogeneity test compared each quintile to a reference group (wealthiest quintile). Secondly, EBF prevalence was analysed using an absolute health inequality measure, the slope index of inequalities (SII).33 The SII compares a plotted linear regression gradient of EBF prevalence, with the wealthiest quintile compared to the poorest quintile. When the SII is positive, there is a higher accumulation of the outcome (EBF prevalence) among wealthier municipalities. In contrast, when the results are negative, the higher concentration of EBF prevalence is among poorer municipalities. An SII of zero indicates an equal distribution of the outcomes among rich and poor.7 We calculated the SII for each of the 143 months of our study, subsequently included all 143 monthly SII in an ITSA, looking to observe the change in SII EBF prevalence after the time-events.
We used the following regression model (equation (1)) to estimate the trend change in EBF prevalence in step one and repeated them for the three time-events:
| (1) |
EBFsymbolises the outcome at time point T(months) for each equally spaced time point t at individual leveli. Tti represents the time since the beginning of the study (1–143 months). X ti characterises an intervention dummy variable (preintervention period = 0, intervention = 1) and X ti T ti is an interaction term. β 0 is the intercept or EBF baseline of the study period. β 1 is the outcome trend before the intervention, which quantifies the trend in the absence of the intervention. β 2 is the change in the outcome following the intervention. β 3 represents the change in EBF trend in the long term after the intervention, compared to the EBF trend before the intervention. (months 1–12) represents the seasonality adjustment as a seasonal dummy. E ti represents the errors in the model in the study period. These analyses were conducted using the ‘XTITSA’ STATA module.34
| (2) |
Equation (2) used the STATA command ‘ITSA’, which measures each monthly SII as individual data. This article reports results of the short time effect (change of level) after the intervention (β 2) and the long-term effect (β 3). However, only the short time effect coefficients (β 2) are described in the result and discussion sections. The long-term effect results (β 3) showed similar trends to the short time effect (β 2) and can be found in Table 3, Table 4.
Table 3.
EBF at three and six months’ trend, after the implementation of the extended maternity leave, the EBF primary health care goal and after the beginning of the COVID-19 pandemic, by municipal socio-economic status.
| Outcome | %EBF change (95% CI) |
||||
|---|---|---|---|---|---|
| SES 1 | SES 2 | SES 3 | SES 4 | SES 5 | |
| 3 months | |||||
| Extended maternity leave | |||||
| EBF change after ML (β2) | −0.25 (−2.55, 2.05) | 2.78 (0.11, 5.46) | 3.71 (0.00, 7.43) | 1.78 (−2.37, 5.93) | 5.13 (0.40, 9.86) |
| P Heterogeneitya | 0.010a | 0.324 | 0.749 | 0.292 | Reference |
| EBF trend changeb (β3) | 0.10 (0.00, 0.21) | 0.16 (0.04, 0.28) | 0.37 (0.18, 0.56) | 0.22 (−0.01, 0.45) | −0.23 (−0.47, 0.00) |
| Postintervention trendc | 0.03 (−0.04, 0.10) | 0.01 (−0.07, 0.09) | 0.14 (0.16, 0.27) | 0.19 (−0.01, 0.38) | −0.23 (−0.41, −0.06) |
| Primary health care goal | |||||
| EBF change after P4P (β2) | 3.22 (1.32, 5.12) | 1.47 (−0.55, 3.51) | −1.00 (−3.66, 1.66) | 1.18 (−1.79, 4.16) | 3.10 (−0.18, 6.38) |
| P Heterogeneitya | 0.943 | 0.356 | 0.051 | 0.393 | Reference |
| EBF trend changed (β3) | 0.06 (0.01, 0.11) | 0.08 (0.03, 0.14) | 0.08 (0.01, 0.15) | 0.14 (0.06, 0.22) | 0.00 (−0.08, 0.8) |
| Postintervention trende | 0.03 (−0.00, 0.07) | 0.06 (0.02, 0.10) | 0.11 (0.06, 0.17) | 0.13 (0.06, 0.19) | 0.00 (−0.06, 0.06) |
| COVID-19 | |||||
| EBF change after COVID-19 (β2) | −2.21 (−8.37, 3.94) | −4.28 (−10.7, 2.22) | −6.17 (−14.6, 2.31) | −12.15 (−23.2, −1.01) | −5.98 (−14.8, 2.86) |
| P Heterogeneitya | 0.464 | 0.741 | 0.958 | 0.409 | Reference |
| EBF trend changef (β3) | −0.20 (−1.58, 1.17) | 0.27 (−1.13, 1.68) | −0.11 (−1.88, 1.65) | 3.31 (1.00, 5.62) | 0.10 (−1.74, 1.95) |
| Postintervention trendg |
−0.14 (−1.52, 1.23) |
0.34 (−1.06, 1.75) |
0.02 (−1.74, 1.79) |
3.42 (1.11, 5.73) |
0.12 (−1.73, 1.97) |
| 6 months | |||||
| Extended maternity leave, 2011 | |||||
| EBF change after ML (β2) | 1.44 (−1.00,3.90) | −0.75 (−3.71, 2.20) | −0.84 (−4.79, 3.10) | −2.23 (−6.37, 1.90) | −1.87 (−6.54, 2.79) |
| P Heterogeneitya | 0.278 | 0.234 | 0.945 | 0.885 | Reference |
| EBF trend changeb (β3) | 0.03 (−0.07, 0.15) | −0.02 (−0.16, 0.11) | 0.10 (−0.07, 0.29) | 0.00 (−0.19, 0.20) | −0.15 (−0.37, 0.06) |
| Postintervention trendc | 0.08 (0.01, 0.16) | 0.04 (−0.04, 0.13) | 0.08 (−0.03, 0.20) | 0.09 (−0.02, 0.21) | 0.02 (−0.11, 0.16) |
| Primary health care goal | |||||
| EBF change after P4P (β2) | 4.36 (2.49, 6.24) | 4.24 (2.16, 6.32) | 4.79 (2.11, 7.47) | 5.01 (2.12, 7.91) | 4.41 (1.22, 7.60) |
| P Heterogeneitya | 0.977 | 0.923 | 0.846 | 0.781 | Reference |
| EBF trend changed (β3) | 0.05 (0.00, 0.10) | 0.12 (0.06, 0.17) | 0.15 (0.08, 0.22) | 0.18 (0.10, 0.26) | 0.00 (−0.08, 0.08) |
| Postintervention trende | 0.15 (0.11, 0.19) | 0.16 (0.12, 0.21) | 0.18 (0.13, 0.24) | 0.23 (0.16, 0.29) | 0.06 (−0.00, 0.12) |
| COVID-19 | |||||
| EBF change after COVID-19 (β2) | −3.16 (−9.32, 2.98) | −5.00 (−11.5, 1.57) | −1.00 (−9.80, 7.78) | −2.44 (−13.5, 8.62) | 3.74 (−6.47, 13.9) |
| P Heterogeneitya | 0.19 | 0.12 | 0.783 | 0.413 | Reference |
| EBF trend changef (β3) | −0.87 (−2.20, 0.44) | −0.14 (−1.53, 1.23) | −1.63 (−3.48, 0.21) | −1.25 (−3.62, 1.12) | −2.74 (−4.96, −0.53) |
| Postintervention trendg | −0.70 (−2.03, 0.62) | 0.04 (−1.33, 1.43) | −1.42 (−3.27, 0.42) | −1.02 (−3.40, 1.35) | −2.66 (−4.88, −0.44) |
P-Heterogeneity for the EBF change first-month coefficient.
Nov. 2011–Dec. 2014 relative to Jan. 2009–Oct. 2011.
Monthly change Nov. 2011–Dec. 2014.
Jan. 2009–Dec. 2014 relative to Jan. 2015–Nov. 2020.
Monthly change Jan. 2015–Nov. 2020.
Jan. 2015–March. 2020 relative to April. 2020–Nov. 2020.
Monthly change April. 2020–Nov. 2020.
Table 4.
Monthly SII of EBF at three and six months, after the implementation of the extended maternity leave, the EBF primary health care goal and after the COVID-19 pandemic. Chile 2009–2020.
| Intervention | SII of EBF prevalence change (95% CI) |
|
|---|---|---|
| 3 months | 6 months | |
| Extended maternity leave, 2011 | ||
| EBF change after ML (β2) | −0.10 (−0.48, 0.27) | −0.21 (−0.56, 0.12) |
| Change in EBF trend from Nov. 2011–Dec. 2014 relative to Jan. 2009–Oct. 2011 (β3) | 0.00 (−0.00, 0.02) | −0.02 (−0.03, −0.00) |
| Postintervention trend (monthly change from Nov. 2011–Dec. 2014) | 0.02 (0.01, 0.03) | 0.00 (−0.01, 0.01) |
| Primary health care goal, 2015 | ||
| EBF change after P4P (β2) | −0.36 (−0.63, −0.09) | −1.05 (−1.37, −0.73) |
| Change in EBF trend from Jan. 2009–Dec. 2014 relative to Jan. 2015–Nov. 2020 (β3) | −0.02 (−0.03, −0.01) | −0.02 (−0.03, −0.01) |
| Postintervention trend (monthly change from Jan. 2015–Nov. 2020) | −0.00 (−0.01, 0.00) | −0.01 (−0.02, −0.00) |
| COVID-19 Pandemic, 2020 | ||
| EBF change after COVID-19 (β2) | −0.45 (−1.17, 0.27) | 1.44 (0.92, 1.97) |
| Change in EBF trend from Jan. 2015–March. 20 relative to April. 2020–Nov. 2020 (β3) | 0.17 (0.03, 0.32) | −0.03 (−0.18, 0.10) |
| Postintervention EBF trend (monthly change from April. 2020–Nov. 2020) | 0.17 (0.02, 0.31) | −0.06 (−0.21, 0.08) |
Autocorrelation and partial autocorrelation were assessed using the Durbin–Watson test and visual plots. As small evidence of autocorrelation was identified, analyses were performed with correction for autocorrelation. We corroborated that our ITS was non-stationary checking for normal distribution of the EBF trend and with summary statistics.
ML access and the number of municipalities with EBF data were included in sensitivity analyses as mediators.
Ethics
This study was approved by the Ethics in Human Research Committee of the Faculty of Medicine, University of Chile, under the Project: 069-2021 and file number: 045. Informed consent was not required because records were aggregated.
Results
Table 2 shows the national prevalence of EBF at three and six months and by ISED SES quintiles, before and after implementing the extended ML, the P4P strategy, and COVID-19. The lower SES quintiles reported a higher mean EBF prevalence at three and six months, before and after each of the three time-events (e.g. EBF at three months was 73.4% in the lowest quintile and 62.3% in the highest quintile before the extended ML, and 72.0% in the lowest quintile and 62.5% in the highest after the extended ML).
Table 2.
Exclusive breastfeeding mean prevalence (95% CI), at three and six months, according to public policy and COVID-19, by municipal socio-economic status, Chile 2009–2020.
| Total country/quintile | Extended maternity leave |
Primary health care goal |
COVID-19 |
|||
|---|---|---|---|---|---|---|
| Beforea | Afterb | Beforea | Afterb | Beforea | Afterb | |
| 3 Months | ||||||
| Total country |
69.5 (69.0, 70.1) |
68.4 (67.9, 69.0) |
69.0 (68.6, 69.4) |
71.6 (71.2, 72.1) |
71.6 (71.2, 72.1) |
71.2 (69.3, 73.1) |
| 1 (lower) | 73.4 (72.5, 74.3)c | 72.0 (71.1, 72.9)c | 72.8 (72.2, 73.3)c | 76.1 (75.3, 77.0)c | 76.2 (75.3, 77.1)c | 75.3 (72.3, 78.2)c |
| 2 | 68.9 (67.9, 69.8)c | 68.1 (67.2, 69.0)c | 68.5 (67.8, 69.1)c | 71.3 (70.5, 72.1)c | 71.3 (70.5, 72.1)c | 71.4 (67.4, 75.4)c |
| 3 | 64.6 (63.4, 65.9)c | 64.9 (63.6, 66.2)c | 64.7 (63.8, 65.6)c | 68.4 (67.4, 69.3)c | 68.4 (67.4, 69.3) | 68.9 (65.4, 72.3) |
| 4 | 59.9 (58.5, 61.4) | 59.7 (58.6, 60.9)c | 59.8 (58.9, 60.8)c | 66.4 (65.4, 67.4) | 66.1 (65.1, 67.1) | 72.2 (58.0, 68.6) |
| 5 (reference) | 62.3 (60.5, 64.1) | 62.5 (60.9, 64.0) | 62.4 (61.2, 63.6) | 66.2 (65.7, 68.0) | 67.2 (66.1, 68.4) | 63.3 (58.0, 68.6) |
| 6 Months | ||||||
| Total country |
49.2 (48.6, 49.8) |
51.5 (50.9, 52.1) |
50.3 (49.9, 50.8) |
62.4 (61.9, 62.9) |
62.2 (61.7, 62.7) |
64.6 (62.5, 66.7) |
| 1 (lower) | 53.4 (50.4, 52.4)c | 55.9 (54.9, 57.0)c | 53.5 (52.8, 54.2)c | 68.3 (64.8,69.1)c | 68.1 (67.2, 69.0)c | 70.8 (67.5, 74.1)c |
| 2 | 49.5 (48.4, 50.6)c | 50.7 (49.6, 51.7)c | 40.4 (39.4, 41.4)c | 55.5 (54.5, 56.5) | 60.9 (60.0, 61.7)c | 63.8 (59.8, 67.8)c |
| 3 | 42.6 (41.3, 44.0) | 43.9 (42.4, 45.3)c | 43.2 (42.3, 44.2)c | 56.8 (55.8, 57.8) | 56.6 (55.6, 57.6) | 59.4 (54.2, 64.5) |
| 4 | 39.8 (38.3, 41.3)c | 40.9 (39.6, 42.2)c | 50.1 (49.3, 50.9)c | 61.1 (60.2, 61.9)c | 55.2 (54.2, 56.2) | 60.3 (55.0, 65.6) |
| 5 (reference) | 43.6 (41.9, 45.4) | 46.7 (45.1,48.2) | 45.3 (44.1, 46.4) | 56.6 (55.3, 57.7) | 56.1 (55.4, 57.8) | 55.8 (49.6, 67.8) |
Before: 1. Extended maternity leave: January 2009/September 2011; 2. Primary Health Care Goal: January 2009/December 2014; 3. COVID-19: January 2015/March 2020.
After: 1. Extended maternity leave: October 2011/December 2014; 2. Primary Health Care Goal: January 2015/November 2020; 3. COVID-19: April 2020/November 2020.
Comparison between each municipal SES quintile and higher municipal SES quintile (fifth). Significance: P-value = 0.05 or less compared to the reference group (quintile 5).
Table 3 presents the ITSA short-term (β 2) and long-term (β 3) effect estimates for EBF at three and six months, stratified by SES quintiles after the three events. The short-term effect estimates reported an increase in EBF at three months was identified after the implementation of the extended ML in the second, third, and fifth quintiles, with heterogeneity only in the lowest quintile. No changes in EBF at six months were reported after the extended ML. The P4P strategy showed an increase in EBF at three months only in the lowest SES, with no heterogeneity, whereas at six months, the P4P strategy reported an increase in EBF in all quintiles (between 4% and 5% increase), with no heterogeneity. A decrease in EBF at three months was observed during COVID-19 only in the fourth quintile and no effect in EBF at six months, also with no heterogeneity. The results of the sensitivity analyses (adjusted by ML access and municipalities with EBF data) were similar to the main analyses (data not shown).
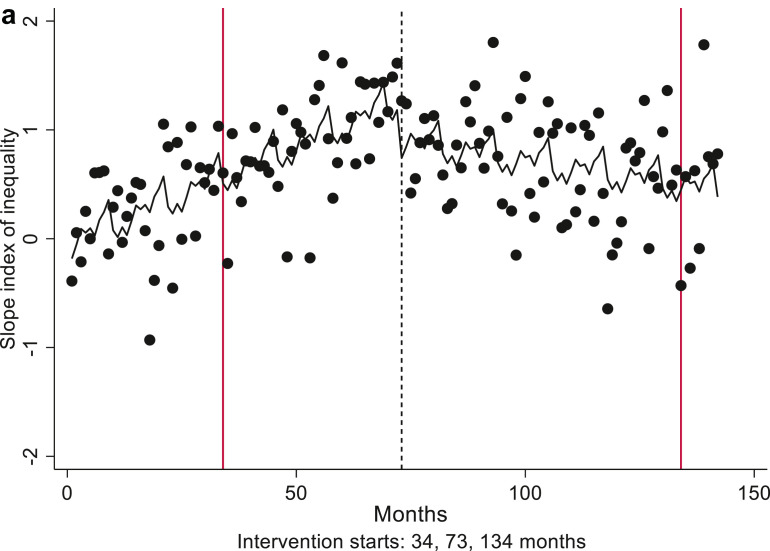
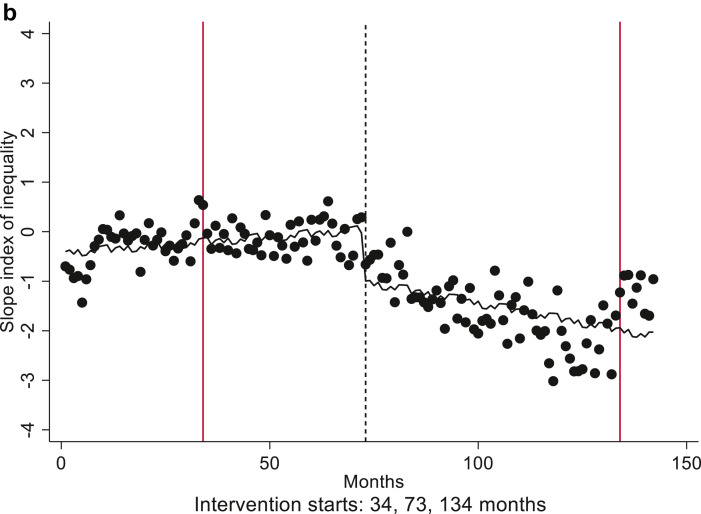
Fig. 1a, Fig. 1b shows the monthly trend of the municipal EBF SII at three and six months. Table 4 presents the ITSA short-term (β 2) and long-term (β 3) estimates of the monthly EBF SII after the extended ML, the P4P strategy and COVID-19. The SII for EBF at three and six months showed no changes after the extended ML. After the P4P strategy, there was a higher EBF concentration at three and six months among women in poorer municipalities (SII: −0.36 [95% CI: −0.63, −0.09] and SII: −1.05 [95% CI: −1.37, −0.73], respectively). No changes in SII for EBF at three months were observed after COVID-19, whereas at six months, EBF was skewed towards wealthier municipalities (SII: 1.44 [95% CI: 0.92, 1.97]).
Fig. 1a.
Exclusive breastfeeding at three months inequality gap trend, from January 2009 to November 2020, measured with slope index of inequality.
Fig. 1b.
Exclusive breastfeeding at six months inequality gap trend, from January 2009 to November 2020, measured with slope index of inequality.
The long-term effect (β 3) in EBF prevalence can be found in Table 3, Table 4. These results reported similar trend to what was observed in the short-term effect (β 2).
Discussion
To the best of our knowledge, this is the first study to analyse EBF inequalities in Chile after the implementation of extra 12 weeks of ML in October 2011, the P4P strategy in January 2015 and COVID-19. We observed higher EBF prevalence in lowest SES quintiles at three and six months, in accordance with previously published national35 and international data.6
We identified that the extended ML increased EBF only at three months and only in three SES quintiles. The P4P strategy increased EBF at six months prevalence in all SES strata (ranged from 4% to 5%). No changes in EBF inequality were observed during COVID-19. The EBF prevalence had a higher increase at three and six months in poorer municipalities after the P4P strategy (SII: −0.36 and −1.05, respectively). Conversely, COVID-19 increased EBF at six months by 1.44% only in women living in wealthier municipalities.
Few studies have analysed inequalities in EBF. Bhattacharjee et al.36 reported that EBF increased in 48% of the 94 low- and middle-income countries (LMICs) in the last decades, of these only 40% decreased EBF inequalities. A Latin American multicentre study showed that EBF prevalence was higher in the lowest-income quintiles in several countries, with only one country decreasing EBF inequalities during the study period.6 Another study performed in Brazil, reported that EBF increased in wealthier mothers more rapidly, together with an increase in absolute inequalities in EBF, which is not unusual when the baseline EBF levels among the poor are very low.37
Maternity leave has previously been shown to increase EBF prevalence. Nonetheless, studies have reported that wealthier women might benefit more from ML.14 A study performed in the United States showed a modest increase in EBF at six months after introducing paid ML, but mainly in richer women.38 A British study identified that paid ML was related to a steady increase in breastfeeding initiation in the UK, without reducing EBF inequalities.39 The authors related a greater use of ML in women with higher levels of education, on account of their formal jobs and more access to breastfeeding information.13
We reported null results on the impact of ML in EBF inequalities. A possible explanation for this could be low access to ML among those affiliated to the public health system, where only approximately 20% have access to ML,22 , 31 while a large percentage of women in the lower SES have informal jobs.40 In addition, the extended ML leaves a total of only five and a half months (24 weeks), increasing the need for mothers to introduce formula or solid food before their children turn six months.
Our analyses showed that the P4P strategy increased EBF prevalence at three months only in the lowest quintile and at six months in all quintiles. We observed negative results in the SII for EBF prevalence after the P4P strategy at three and six months, meaning that the EBF prevalence had a greater increase in poorer municipalities. The differences between the stratified analyses and the SII could be explained by a reduction in statistical power in the stratified analyses. Finally, we cannot rule out the possibility of an overlapping effect of the ML plus the P4P.
The COVID-19 pandemic has been an important strain on society, but particularly on women, and at a higher level among poorer women.19 , 41 , 42 A study in the Republic of Ireland found that during COVID-19 confinement, 40% of mothers felt that their EBF was protected in lockdown, while 27% lacked support and faced barriers to breastfeeding, with many even discontinuing the practice. Most of the mothers who stopped EBF earlier than planned were from poorer backgrounds or ethnic minorities.41 A joint Canadian-Australian study revealed that an average Canadian woman with children spent 50 more hours per week than men on childcare during the COVID-19 pandemic. Australian women with children spent nearly 43 h more than men on childcare.43 The higher concentration of EBF in wealthier municipalities identified in our results could be explained by the cut of medical check-ups to the bare minimum in lower-income municipalities, prioritizing COVID-19 traceability, whereas inhabitants of wealthier municipalities might have had access to private health care.
Our study has several limitations. First, this is a quasi-experimental study, without a control group. However, ITSA considers the preintervention period as a counterfactual trend. Second, as only the public health system collects EBF data, our study did not include EBF data from wealthier women (approximately 20%).22 Thus, our results represent only those affiliated to the public sector. Third, it is possible that under- or over-registration might have occurred. However, this bias should not be differentiated by SES. Fourthly, the SII is an absolute measure of health inequalities that considers all the population in an SES gradient, without contemplating that some SESs might not have a gradient behaviour. Finally, we acknowledge that multiple observations before the treatment/shock of interest are required to build a plausible counterfactual when conducting ITSA. Yet, the number of observations post-treatment is mostly important for statistical power considerations, as well as taking into account possible delayed effects. However, in our analysis focusing on the COVID-19 shock, we were able to identify a change in EBF at three months (with statistical precise estimates), but not at six months. Furthermore, the Cochrane EPOC working group guidelines recommend that ‘ITS should have a minimum of three data points before and three after to be considered in a Cochrane review study’.44 We concede that our COVID-19 results should be interpreted with caution regarding the short period post-treatment considered in this study.
Conclusion
Our findings highlight that no EBF inequalities were identified after the implementation of the extended ML, which could be explained by low ML access in public health system-affiliated and the insufficient duration of the ML. Our results also suggest that the P4P is successful in increasing EBF across all socio-economic quintiles, but in a higher level in lower SES municipalities. The COVID-19 pandemic increased EBF at six months in wealthier municipalities, which had lower EBF to begin with.
Our study showed that it is imperative to reinforce EBF support across SES. Increasing the ML current duration, providing more flexible ML access and enhance EBF promotion policies, are more likely to thrive in higher EBF prevalence across SES. Follow-up studies of the EBF trend during the COVID-19 period are required.
Author statements
Acknowledgements
We would like to thank the Social Welfare Superintendence (SUSESO) for providing the information on maternity leave access and to the Ministry of Health for the data on exclusive breastfeeding. Special thanks to Benaiah Moses for English proofreading this manuscript and to Sarah Moses for your inspiration.
Ethical approval
This study was approved by the Ethics in Human Research Committee of the Faculty of Medicine, University of Chile, under the Project: 069-2021 and file number: 045. Informed consent was not required because records were aggregated.
Financial support
The submitted work was financially supported by the Chilean National Fund for Scientific and Technological Development (FONDECYT), under grant numbers 1130277 and 1150878. DN-R holds a Chilean Commission of Science and Technology student fellowship to perform a PhD at the School of Public Health, University of Chile, under grant number 21151097.
Competing interests
The authors certify that they have no conflict of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.puhe.2022.11.001.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Victora C.G., Bahl R., Barros A.J., França G.V., Horton S., Krasevec J., et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016 Jan;387(10017):475–490. doi: 10.1016/S0140-6736(15)01024-7. [DOI] [PubMed] [Google Scholar]
- 2.Rollins N.C., Bhandari N., Hajeebhoy N., Horton S., Lutter C.K., Martines J.C., et al. Why invest, and what it will take to improve breastfeeding practices? Lancet. 2016 Jan;387(10017):491–504. doi: 10.1016/S0140-6736(15)01044-2. [DOI] [PubMed] [Google Scholar]
- 3.Dror D.K., Allen L.H. Overview of nutrients in human milk. Adv Nutr. 2018 May;9(suppl_1):278S–294S. doi: 10.1093/advances/nmy022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Cancer Research Fund, American Institute for Cancer Research . vol. xxv. WCRF/AICR; Washington, DC: 2018. p. 517. (Food, nutrition, physical activity, and the prevention of cancer: a global perspective). [Google Scholar]
- 5.Kawachi I., Subramanian S.V., Almeida-Filho N. A glossary for health inequalities. J Epidemiol Community Health. 2002 Sep;56(9):647–652. doi: 10.1136/jech.56.9.647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ferreira C.S., Azeredo C.M., Rinaldi A.E.M. Trends in social inequalities in breastfeeding and infant formulas in Latin American countries between the 1990 and 2010 decades. Public Health Nutr. 2021 Jan 27:1–10. doi: 10.1017/S1368980021000392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arcaya M.C., Arcaya A.L., Subramanian S.V. Inequalities in health: definitions, concepts, and theories. Glob Health Action. 2015 Jun 24;8 doi: 10.3402/gha.v8.27106. 27106–27106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barros F.C., Victora C.G., Scherpbier R., Gwatkin D. Socioeconomic inequities in the health and nutrition of children in low/middle income countries. Rev Saude Publica. 2010 Feb;44(1):1–16. doi: 10.1590/s0034-89102010000100001. [DOI] [PubMed] [Google Scholar]
- 9.Dodgson J.E. Considering inequities in breastfeeding. J Hum Lact. 2017 May;33(2):248–249. doi: 10.1177/0890334417699164. [DOI] [PubMed] [Google Scholar]
- 10.Buckland C., Hector D., Kolt G.S., Fahey P., Arora A. Interventions to promote exclusive breastfeeding among young mothers: a systematic review and meta-analysis. Int Breastfeed J. 2020 Dec 1;15(1):102. doi: 10.1186/s13006-020-00340-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saputri N.S., Spagnoletti B.R.M., Morgan A., Wilopo S.A., Singh A., McPake B., et al. Progress towards reducing sociodemographic disparities in breastfeeding outcomes in Indonesia: a trend analysis from 2002 to 2017. BMC Public Health. 2020 Dec;20(1):1112. doi: 10.1186/s12889-020-09194-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.the PATHS Equity Team. Nickel N.C., Martens P.J., Chateau D., Brownell M.D., Sarkar J., et al. Have we left some behind? Trends in socio-economic inequalities in breastfeeding initiation: a population-based epidemiological surveillance study. Can J Public Health. 2014 Sep;105(5):e362–e368. doi: 10.17269/cjph.105.4499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Andres E., Baird S., Bingenheimer J.B., Markus A.R. Maternity leave access and health: a systematic narrative review and conceptual framework development. Matern Child Health J. 2016;20(6):1178–1192. doi: 10.1007/s10995-015-1905-9. [DOI] [PubMed] [Google Scholar]
- 14.Navarro-Rosenblatt D., Garmendia M.L. Maternity Leave and Its Impact on Breastfeeding: A Review of the Literature. Breastfeed Med. 2018 Nov;13(9):589–597. doi: 10.1089/bfm.2018.0132. Epub 2018 Sep 25. PMID: 30256125. [DOI] [PubMed] [Google Scholar]
- 15.Biblioteca del Congreso Nacional . Gobierno de Chile; Chile: 2014. Resolución Exenta 880 [Internet]https://www.leychile.cl/N?i=1067767&f=2014-10-02&p= Available from: [Google Scholar]
- 16.Cornejo-Ovalle M., Brignardello-Petersen R., Pérez G. Pay-for-performance and efficiency in primary oral health care practices in Chile. Rev Clín Periodoncia Implantol Rehabil Oral. 2015 Apr;8(1):60–66. [Google Scholar]
- 17.Langdown C., Peckham S. The use of financial incentives to help improve health outcomes: is the quality and outcomes framework fit for purpose? A systematic review. J Public Health. 2014 Jun;36(2):251–258. doi: 10.1093/pubmed/fdt077. [DOI] [PubMed] [Google Scholar]
- 18.Scott A., Sivey P., Ait Ouakrim D., Willenberg L., Naccarella L., Furler J., et al. In: Cochrane Effective Practice and Organisation of Care Group, editor. 2011 Sep 7. The effect of financial incentives on the quality of health care provided by primary care physicians. (Cochrane Database Syst Rev [Internet]). [cited 2021 Feb 21]; Available from: [DOI] [PubMed] [Google Scholar]
- 19.Busch-Hallen J., Walters D., Rowe S., Chowdhury A., Arabi M. Impact of COVID-19 on maternal and child health. Lancet Glob Health. 2020 Oct;8(10):e1257. doi: 10.1016/S2214-109X(20)30327-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Navarro Rosenblatt D., Garmendia M.L. Archivos Latinoamericanos de Nutrición. 2021. Impact of public health policies and the COVID-19 pandemic on the rend of exclusive breastfeeding in Chile.http://www.alanrevista.org/ediciones/2021/suplemento-1/art-92/ Paraguay. [Internet]. Available from: [Google Scholar]
- 21.Navarro Rosenblatt D., Garmendia M.L. Are there differences between rural/urban areas and geographic zones in exclusive breastfeeding in Chile, after the implementation of two public health policies and the covid-19 pandemic? 2021. https://www.alanrevista.org/ediciones/2021/suplemento-1/art-96/?utm_source=researcher_app&utm_medium=referral&utm_campaign=RESR_MRKT_Researcher_inbound [Internet]. Available from:
- 22.SUSESO . 2016. Protección a la maternidad en Chile: Evolución del Permiso Postnatal Parental a cinco años de su implementación 2011-2016. [Google Scholar]
- 23.Crispi F., Cherla A., Vivaldi E.A., Mossialos E. Rebuilding the broken health contract in Chile. Lancet. 2020 Apr;395(10233):1342. doi: 10.1016/S0140-6736(20)30228-2. [DOI] [PubMed] [Google Scholar]
- 24.Bernal J.L., Cummins S., Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017;46(1):348–355. doi: 10.1093/ije/dyw098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Linden A. Conducting interrupted time-series analysis for single-and multiple-group comparisons. STATA J. 2015;15(2):480–500. [Google Scholar]
- 26.Ministerio de Salud, de Chile., editors. Resúmenes Estadísticos Mensuales DEIS. 2018. http://www.deis.cl/resumenes-estadisticos-mensuales-deis/ [Internet]. Available from: [Google Scholar]
- 27.Ministerio de Salud, de Chile Editor. Ministerio de Salud, Chile; 2013. Manuales series REM, 2013.http://epi.minsal.cl/datos-drs/#/2BT5QWY5W [Internet]. Available from: [Google Scholar]
- 28.Gattini C., Chavez C., Alberts C. 2014. Comunas de Chile, según nivel socio-económico, de salud y desarrollo humano.http://ochisap.cl/ Revisión 2013. [Internet, cited 2020 Oct 31]. Available from: [Google Scholar]
- 29.Ministerio de Desarrollo Social, Ministerio de Desarrollo Social, Ministry of Welfare Nacional Survey of socio-economic Characterization (Encuesta de Caracterización Socioeconómica Nacional, CASEN) 2021. http://observatorio.ministeriodesarrollosocial.gob.cl/encuesta-casen [Internet]. Chile. Available from:
- 30.Gobierno de Chile . Gobierno de Chile; Chile: 2011. Ley 20545 Modifica las Normas de Protección a la Maternidad e Incorpora el Permiso Postnatal Parental.https://www.leychile.cl/Navegar?idNorma=1030936 [Internet] Available from: [Google Scholar]
- 31.SUSESO Sistema de Gestión de Información de Subsidios Maternales – SIMAT Superintendencia de Seguridad social [Internet] 2021. https://www.suseso.cl/608/w3-propertyvalue-59544.html Estadisticas mensuales. Available from:
- 32.Higgins J.P., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003 Sep;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moreno-Betancur M., Latouche A., Menvielle G., Kunst A.E., Rey G. Relative index of inequality and slope index of inequality: a structured regression framework for estimation. Epidemiology. 2015;26(4) doi: 10.1097/EDE.0000000000000311. https://journals.lww.com/epidem/Fulltext/2015/07000/Relative_Index_of_Inequality_and_Slope_Index_of.12.aspx [Internet] Available from: [DOI] [PubMed] [Google Scholar]
- 34.Linden A. XTITSA: Stata module for performing interrupted time-series analysis for panel data. Stat Softw Compon. [Internet] Available from: https://ideas.repec.org/c/boc/bocode/s458903.html.
- 35.Farkas C., Girard L.C. Breastfeeding initiation and duration in Chile: understanding the social and health determinants. J Epidemiol Community Health. 2019 Jul;73(7):637–644. doi: 10.1136/jech-2018-211148. 2019/03/13. [DOI] [PubMed] [Google Scholar]
- 36.Bhattacharjee N.V., Schaeffer L.E., Hay S.I., et al. Mapping inequalities in exclusive breastfeeding in low- and middle-income countries, 2000–2018. Nat Hum Behav. 2021;5:1027–1045. doi: 10.1038/s41562-021-01108-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Santos I.S., Barros F.C., Horta B.L., Menezes A.M.B., Bassani D., Tovo-Rodrigues L., et al. Breastfeeding exclusivity and duration: trends and inequalities in four population-based birth cohorts in Pelotas, Brazil, 1982–2015. Int J Epidemiol. 2019 Apr 1;48(Supplement_1):i72–i79. doi: 10.1093/ije/dyy159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hamad R., Modrek S., White J.S. Paid family leave effects on breastfeeding: a quasi-experimental study of US policies. Am J Public Health. 2019 Jan;109(1):164–166. doi: 10.2105/AJPH.2018.304693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Simpson D.A., Quigley M.A., Kurinczuk J.J., Carson C. Twenty-five-year trends in breastfeeding initiation: the effects of sociodemographic changes in Great Britain, 1985-2010. Washio Y, editor. PLoS One. 2019 Jan 17;14(1) doi: 10.1371/journal.pone.0210838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Instituto Nacional de Estadísticas e Chile . 2015. Mujeres en Chile y mercado del trabajo: Participación laboral femenina y brechas salariales. [Google Scholar]
- 41.Brown A., Shenker N. Experiences of breastfeeding during COVID-19: lessons for future practical and emotional support. Matern Child Nutr. 2020/09/23;17(1) doi: 10.1111/mcn.13088. ed. 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Instituto Nacional de Estadísticas – Chile Bolentín estadístico: empleo trimestral (trimestre movil octubre- diciembre 2020) 2020. https://www.ine.cl/docs/default-source/ocupacion-y-desocupacion/boletines/2020/pa%C3%ADs/bolet%C3%ADn-empleo-nacional-trimestre-m%C3%B3vil-octubre-noviembre-diciembre-2020.pdf [Internet]. Chile. Available from:
- 43.Kotlar B., Gerson E., Petrillo S., Langer A., Tiemeier H. The impact of the COVID-19 pandemic on maternal and perinatal health: a scoping review. Reprod Health. 2021 Dec;18(1):10. doi: 10.1186/s12978-021-01070-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.What study designs can be considered for inclusion in an EPOC review and what should they be called? Cochrane Effective Practice and Organisation of Care (EPOC); 2017. https://epoc.cochrane.org/sites/epoc.cochrane.org/files/public/uploads/Resources-for-authors2017/what_study_designs_should_be_included_in_an_epoc_review.pdf [Internet]. Available from: [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.