INTRODUCTION
Black individuals living in the United States have higher rates of cardiovascular disease (CVD) than non-Hispanic White (NHW) people. Among Hispanic/Latino individuals, the data are more complex. Despite higher rates and/or poorer control of CVD risk factors and multiple other social and economic disadvantages, age-adjusted CVD mortality rates are one-third lower in Latino than NHW individuals.1,2 Similarly, age-adjusted self-reported rates of CVD are about ten percent lower.1 To date, the reasons for this “Latino Epidemiologic Paradox” remain unclear.3,4 Explanatory hypotheses such as misclassification and immigration-related factors have been refuted. Many also question whether the paradox actually exists. In this study, we analyze data from a diverse national cohort which includes > 40,000 self-reported Hispanic/Latino people to detect for evidence of this Paradox.
METHODS
Created under the National Institutes of Health’s Precision Medicine Initiative, the All of Us Research Program (AoURP) has enrolled over 280,000 core participants of which 80% are from groups historically under-represented in research.5 Data sources include survey data, electronic medical records, as well as laboratory and genetic data collected at over 380 recruitment sites. We accessed data through the AoURP Research Workbench (https://www.researchallofus.org/data-tools/workbench/).6 We included all adults (≥ 18 years) who self-identified as Hispanic, NHWs, and/or Black (non-Hispanic). CVD was determined using electronic health records (EHR) based on AoURP hierarchical grouping using the Observational Medical Outcomes Partnership (OMOP) common data model (https://www.ohdsi.org/data-standardization/the-common-data-model/). The list was further refined by having two investigators (RMV, OC) review each diagnosis code and excluding a small number which were not relevant, e.g., venous disease (list available from corresponding author). We report results stratified by age and gender, using 95% confidence intervals (CI). Age-adjusted CVD rates were calculated in males and females using direct standardization with the AoURP cohort as the standard population. All analyses were done using R environment (©RFoundation, www.r-project.org/).
RESULTS
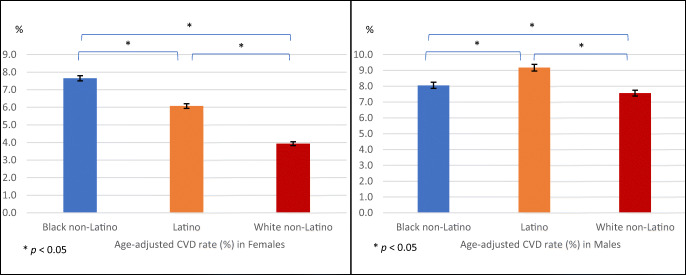
We included 202,013 participants; 57.1% were NHW, 22.2% Black, and 20.7% Latino. The mean age was 51.3 years (± 16.7 years) and 62.3% were females. The crude CVD prevalence was higher in men than women and increased with age. After age adjustment, we found that Latina women had a crude CVD rate of 6.1% (95%CI [6.0, 6.2]). This rate was higher than NHW women (3.9%, 95%CI [3.8, 4.0]) but lower than Black women (7.7%, 95%CI [7.5, 7.8]). The age-adjusted CVD rate was highest among Latino men at 9.2% (95%CI [9.0, 9.4]) versus black at 8.1% (95%CI [7.9,8.2]) and NHW men at 7.6% (95%CI [7.4, 7.8]) (Fig. 1).
Figure 1.
Age-adjusted cardiovascular disease (CVD) prevalence for males and females by ethnic/racial group.
DISCUSSION
Prior data suggesting Latino people have lower rates of CVD than NHWs had been considered paradoxical. In our analysis, they had significantly higher age-adjusted CVD rates than NHW individuals. These findings do not support the Latino Epidemiologic Paradox.
Strengths of our study include the size and diversity of the cohort. With over 40,000 Latino enrollees, AoURP is the largest cohort of Latino people in the United States. By recruiting across a large swath of geographically distinct sites, it includes a wide spectrum of Hispanic subgroups. However, the cohort was not designed using a nationally representative sampling frame. We also age standardized to the AoURP distribution, and prevalence rates may not be fully comparable to those in other studies. In addition, we utilized EHR diagnoses for CVD. Prior work has shown this approach has fair to good validity for heart disease. In addition, our data using EHR diagnoses is comparable to self-reported data from the National Health and Nutrition Survey which finds a CVD prevalence for NHWs at 8.7%1 versus 7.6% in our analysis.
Additional research should continue to examine how CVD varies across Latino subgroups and the roles of other factors such as immigration and acculturation. These variables are currently being collected but not yet publicly available for analysis. Once AoURP makes genetic data available, researchers will also be able to examine the role of both global ancestral alleles and those closer to more local CVD risk loci. In addition, while this paradox has been best described in CVD, it is also evident in other health conditions such as cancer and infant mortality. Regardless of the existence of this paradox, CVD remains a leading cause of death among Latinos. This, along with our findings, further supports ongoing tailored initiatives to control CVD risk factors among Latinos.
Acknowledgements
This study was supported by the All of Us Research Program’s grants. The All of Us Research Program is supported (or funded) by grants through the National Institutes of Health, Office of the Director: Regional Medical Centers: 1 OT2 OD026549; 1 OT2 OD026554; 1 OT2 OD026557; 1 OT2 OD026556; 1 OT2 OD026550; 1 OT2 OD 026552; 1 OT2 OD026553; 1 OT2 OD026548; 1 OT2 OD026551; 1 OT2 OD026555; IAA #: AOD 16037; Federally Qualified Health Centers: HHSN 263201600085U; Data and Research Center: 5 U2C OD023196; Biobank: 1 U24 OD023121; The Participant Center: U24 OD023176; Participant Technology Systems Center: 1 U24 OD023163; Communications and Engagement: 3 OT2 OD023205; 3 OT2 OD023206; and Community Partners: 1 OT2 OD025277; 3 OT2 OD025315; 1 OT2 OD025337; 1 OT2 OD025276. In addition to the funded partners, the All of Us Research Program would not be possible without the contributions made by its participants.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Balfour PC, Jr, Ruiz JM, Talavera GA, Allison MA, Rodriguez CJ. Cardiovascular Disease in Hispanics/Latinos in the United States. J Lat Psychol. 2016;4(2):98–113. doi: 10.1037/lat0000056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Velasco-Mondragon E, Jimenez A, Palladino-Davis AG, et al. Hispanic health in the USA: a scoping review of the literature. Public Health Rev. 2016;4:98–113. doi: 10.1037/lat0000056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ruiz JM, Steffen P, Smith TB. Hispanic mortality paradox: a systematic review and meta-analysis of the longitudinal literature. Am J Public Health. 2013;103(3):e52–60. doi: 10.2105/AJPH.2012.301103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lopez-Jimenez F, Lavie CJ. Hispanics and cardiovascular health and the “Hispanic Paradox”: what is known and what needs to be discovered? Prog Cardiovasc Dis. 2014;57(3):227–229. doi: 10.1016/j.pcad.2014.09.007. [DOI] [PubMed] [Google Scholar]
- 5.Mapes BM, Foster CS, Kusnoor SV, et al. Diversity and inclusion for the All of Us research program: A scoping review. PLoS One. 2020;15(7):e0234962. doi: 10.1371/journal.pone.0234962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ramirez AH, Gebo KA, Harris PA. Progress With the All of Us Research Program: Opening Access for Researchers. JAMA. 2021;325:2441–2442. doi: 10.1001/jama.2021.7702. [DOI] [PubMed] [Google Scholar]