Abstract
Background
Overuse of diagnostic testing in the hospital setting contributes to high healthcare costs, yet the drivers of diagnostic overuse in this setting are not well-understood. If financial incentives play an important role in perpetuating hospital-level diagnostic overuse, then hospitals with favorable payer mixes might be more likely to exhibit high levels of diagnostic intensity.
Objectives
To apply a previously developed hospital-level diagnostic intensity index to characterize the relationship between payer mix and diagnostic intensity.
Design
Cross-sectional analysis
Subjects
Acute care hospitals in seven states
Main Measures
We utilized a diagnostic intensity index to characterize the level of diagnostic intensity at a given hospital (with higher index values and tertiles signifying higher levels of diagnostic intensity). We used two measures of payer mix: (1) a hospital’s ratio of discharges with Medicare and Medicaid as the primary payer to those with a commercial insurer as the primary payer, (2) a hospital’s disproportionate share hospital ratio.
Key Results
A 5-fold increase in the Medicare or Medicaid to commercial insurance ratio was associated with an adjusted odds ratio of 0.24 (95% CI 0.16–0.36) of being in a higher tertile of the intensity index. A ten percentage point increase in the disproportionate share hospital ratio was associated with an adjusted odds ratio of 0.56 (95% CI 0.42–0.74) of being in a higher intensity index tertile.
Conclusions
At the hospital level, a favorable payer mix is associated with higher diagnostic intensity. This suggests that financial incentives may be a driver of diagnostic overuse.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-022-07453-0.
KEY WORDS: diagnostic intensity, diagnostic overuse, low-value care, payer mix
INTRODUCTION
Low-value care, defined as care for which the “harms or costs outweigh the benefits,”1 is an important contributor to high healthcare costs.2,3 Significant geographic variation in the intensity of healthcare provision and the volume of low-value care has been noted.4,5 Regional factors positively associated with high healthcare intensity include a larger number of physicians, lower density of primary care providers, higher specialist to primary care ratio, higher Medicare malpractice geographic price index, and larger disparity between health insurer and hospital market power.4,6 While the drivers of regional variation in healthcare intensity have been well-studied, its drivers at the hospital-level have not been well-characterized.
Since many incentives which impact physicians’ use of medical resources are crafted at the hospital or health system level, we hypothesized that hospital-level financial factors may be important drivers of overuse. To test this hypothesis, we sought to determine whether diagnostic intensity, as determined by a previously reported hospital-level diagnostic intensity index (DII), is associated with payer mix. We suspect that high levels of diagnostic intensity at the hospital level are associated with higher levels of diagnostic overuse and low-value care.
METHODS
Hospital-Level Diagnostic Intensity Index
We have previously described the development and validation of a hospital-level DII consisting of five metrics.7 The index relies on pairing non-specific symptom-based primary discharge diagnosis codes with diagnostic tests. The five metrics are (1) primary diagnosis of “nausea and vomiting” and body CT scan or esophagogastroduodenoscopy (EGD), (2) primary diagnosis of abdominal pain and body CT scan or EGD, (3) primary diagnosis of “non-specific chest pain” and body CT scan or stress test, (4) primary diagnosis of syncope and stress test, and (5) primary diagnosis of syncope and CT brain.
According to ICD coding guidelines, these discharge diagnosis codes which are in the category of “Symptoms, Signs, and Ill-Defined Conditions” (ICD9 codes 780-796) can only be the primary discharge diagnosis if no more specific diagnosis was made.8 Since positive diagnostic tests typically result in specific disease-based primary discharge diagnosis codes, this index serves as a proxy for rates of non-diagnostic (or negative) testing (with high rates of non-diagnostic testing suggesting a low diagnostic yield). Additional details on the DII are shown in Appendix Table 1.
Measures of Payer Mix and Tests of Temporal Stability
We utilized two pre-defined measures of payer mix: (a) the ratio of Medicare and Medicaid to commercially insured hospitalizations, and (b) the disproportionate share hospital (DSH) ratio. The DSH ratio is the sum of the percentage of Medicare inpatient days attributable to patients who have both Medicare Part A and Supplemental Security Income (for people with little or no income) and the percentage of total inpatient days for patients eligible for Medicaid but not Medicare Part A.9
The payer mix measures were constructed using all hospitalizations at each hospital in 2011. However, we tested their temporal stability between 2011 and 2015. We calculated the intra-class correlation coefficients (ICCs) with mixed-effects (including year as a fixed effect) at the hospital level to test for temporal stability of our payer mix metrics.
We characterized the distribution of each payer mix using density plots and with mean, median, and standard deviation (SD). Based on the distribution, we winsorized the Medicare and Medicaid to commercially insured ratio at the top and bottom one percentile.
Testing the Relationship Between Payer Mix and Diagnostic Overuse
We constructed a multivariable mixed-effects ordinal logistic regression using a hospital’s DII tertile as the outcome variable and payer mix as the predictor variable of interest. We adjusted for teaching status (categorical variable: major teaching, minor teaching, and non-teaching), mean Elixhauser comorbidity index10 (continuous variable), total hospital beds (continuous variable), and ownership category (categorical variable: (1) government federal and non-federal hospitals, (2) church-operated and non-profit Catholic-controlled hospitals, (3) non-government not-for-profit hospitals, and (4) investor-owned, for-profit hospitals) as well as state random effects. Analyses were done using STATA 15.1 (College Station, TX). We reported the adjusted odds ratio of being in a higher tertile of the DII associated with meaningful increases in the payer mix measures: a 5-fold increase in the Medicare and Medicaid to commercial insurance ratio or a ten percentage point increase in the DSH percentage. We also conducted sensitivity analyses in which we (1) combined non-government, non-profit and investor owned, for profit into one category of the hospital ownership covariate and (2) added state as a covariate and dropped hospital ownership as a covariate.
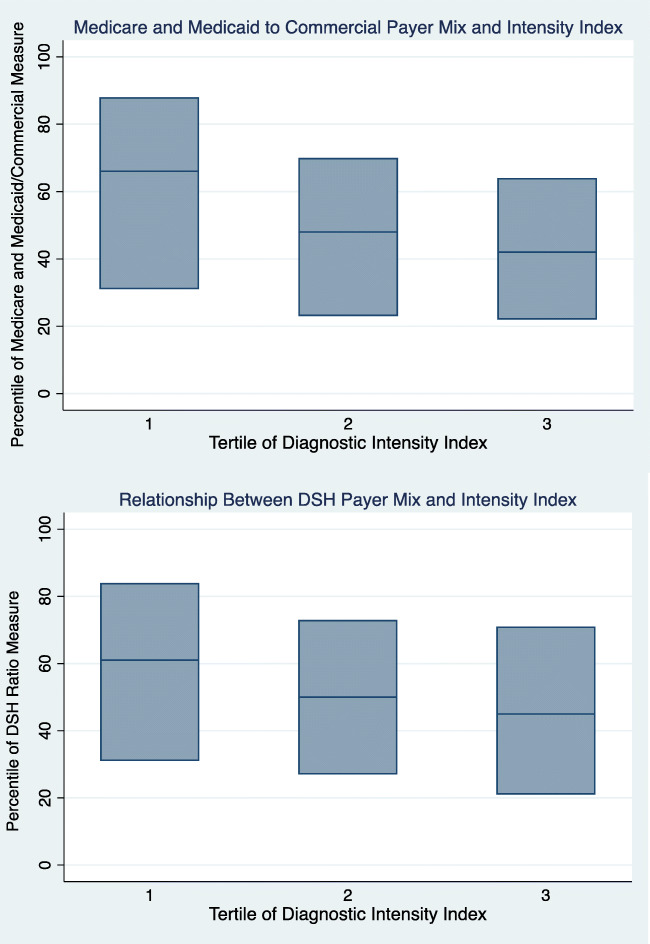
Additionally, we performed a mixed-effects ordinal tertile regression using the same covariates, calculating the adjusted odds ratio of being in a higher tertile of the DII given being in higher tertile of each payer mix measure. We also calculated the predicted probabilities of being in a certain DII tertile given being in a certain tertile of the payer mix measure. Finally, we plotted the range of payer mixes for hospitals in the lowest, middle, and highest tertile of the DII using box plots with the median and interquartile range.
Sources of Data
The DII was constructed using data from 2011 through October 2015 from seven states in the State Inpatient Databases (SID) from the Healthcare Utilization Project of the Agency for Healthcare Research and Quality. These states were chosen based on data availability (some states lacked complete diagnostic testing data) and cost of data acquisition. Pediatric, rehabilitation, long-term care, psychiatric, and specialty hospitals (like surgical sub-specialty and cardiology hospitals) were excluded. We also obtained data for payer mix from the SID using primary payer for each encounter. The Medicare and Medicaid to commercial insurance ratio was determined based on all discharges from a hospital, not just those with diagnosis codes included in our DII. The comorbidity data used to construct the Elixhauser comorbidity index were also extracted from SID data. Data for other hospital covariates—teaching status, total hospital beds, ownership category, and state—were obtained from the American Hospital Association Annual Survey. Each hospital’s DSH ratio was available from the Centers for Medicare and Medicaid Services website.11
RESULTS
DII Tertiles
The hospital-level DII included 620 acute care hospitals from Kentucky, Maryland, New Jersey, New York, North Carolina, Washington, and West Virginia. Index values range from 0 (lowest diagnostic intensity) to 0.986 (highest diagnostic intensity). Based on their index value, hospitals were divided into tertiles of 206 or 207 hospitals, with tertile 1 representing the lowest and tertile 3 representing the highest diagnostic intensity.
Characteristics of Payer Mix Measures
The ICC for the Medicare and Medicaid to commercial insurance ratio at the hospital level was 0.69 (95% confidence interval (CI) 0.65–0.72). The ICC for the DSH ratio was 0.97 (95% CI 0.96–0.97) at the hospital level.
The mean, median, and SD for the Medicare and Medicaid to commercial insurance ratio were 3.40, 2.72, and 2.58 (Appendix Table 2). The mean, median, and SD for the DSH ratio were 0.098, 0.081, and 0.068. The values for both payer mix measures were right-skewed (more extreme values for poorer payer mix) (Appendix Figure 1).
Relationship Between Payer Mix and DII
A more favorable payer mix was associated with higher levels of diagnostic intensity. A 5-fold increase in the Medicare and Medicaid to commercial ratio (corresponding to a 1.94 SD change across the measure, as would be seen when comparing a hospital approximately one SD below the mean to a hospital approximately one SD above the mean) was associated with an adjusted odds ratio of 0.24 (95% CI 0.16–0.36) (Table 1) of being in a higher tertile of the DII. A ten percentage point increase in the DSH ratio (a 1.47 SD increment) was associated with an adjusted odds ratio of 0.56 (95% CI 0.42–0.74) of being in a higher DII tertile (Table 2). The sensitivity analyses did not change the findings.
Table 1.
Mixed effects ordinal logistic regression of diagnostic intensity tertile on Medicare and Medicaid to commercial payer ratio
| Odds ratio | 95% CI | p value | |
|---|---|---|---|
| Five-fold increase in Medicare and Medicaid to commercial payer ratio | 0.24 | 0.16–0.36 | < 0.0001 |
| Teaching status | |||
| Major teaching hospital (referent) | |||
| Minor teaching hospital | 2.36 | 1.17–4.78 | 0.02 |
| Non-teaching hospital | 2.04 | 0.94–4.41 | 0.07 |
| Mean Elixhauser comorbidity score | 1.13 | 1.00–1.27 | 0.05 |
| Total hospital beds | 1.00 | 1.00–1.00 | 0.25 |
| Ownership category | |||
| Government owned (referent) | |||
| Church operated | 1.13 | 0.60–2.15 | 0.70 |
| Non-government, non-profit | 1.44 | 0.91–2.28 | 0.11 |
| Investor owned, for profit | 1.67 | 0.81–3.44 | 0.17 |
Multivariable mixed ordinal regression with tertile of diagnostic intensity index as the outcome variable and 5-fold increase in Medicare and Medicaid to commercial payer ratio as the predictor variable of interest, controlling for teaching status, Elixhauser comorbidity score, total hospital beds, hospital ownership category, and state random effects
CI confidence interval
Table 2.
Mixed effects ordinal logistic regression of diagnostic intensity tertile on disproportionate share hospital ratio
| Odds ratio | 95% CI | p value | |
|---|---|---|---|
| Ten percentage point increase in DSH ratio | 0.56 | 0.42–0.74 | < 0.0001 |
| Teaching status | |||
| Major teaching hospital (referent) | |||
| Minor teaching hospital | 1.15 | 0.56–2.35 | 0.71 |
| Non-teaching hospital | 1.41 | 0.65–3.08 | 0.39 |
| Mean Elixhauser comorbidity score | 1.13 | 0.98–1.30 | 0.11 |
| Total hospital beds | 1.00 | 1.00–1.00 | 0.47 |
| Ownership category | |||
| Government owned (referent) | |||
| Church operated | 1.02 | 0.50–2.07 | 0.96 |
| Non-government, non-profit | 1.61 | 0.96–2.70 | 0.07 |
| Investor owned, for profit | 1.15 | 0.53–2.53 | 0.72 |
Multivariable mixed effects ordinal regression with tertile of diagnostic intensity index as the outcome variable and ten percentage point increase in DSH ratio as the predictor variable of interest, controlling for teaching status, Elixhauser comorbidity score, total hospital beds, hospital ownership category, and state random effects
CI confidence interval, DSH disproportionate share hospital
The adjusted odds ratio of being in a higher tertile of the DII given being in the highest tertile of the Medicare and Medicaid to commercial insurance ratio measure or DSH ratio measure relative to the lowest tertile was associated was 0.29 (95% CI 0.19–0.46) or 0.45 (95% CI 0.28–0.72), respectively (Appendix Table 3). Predicted probabilities demonstrated a similar trend (Appendix Tables 4 and 5). The box plots of interquartile range and median of payer mix measures across DII tertiles showed an association between more favorable payer mix and higher diagnostic intensity (Figure 1).
Figure 1.
Association between payer mix and Diagnostic Intensity Index tertile. Box plots of 25th percentile, median, and 75% percentile for Diagnostic Intensity Index tertiles across range of payer mix measures. Note: Higher tertile implies higher diagnostic intensity
Discussion
We found a significant association between favorable payer mix and higher diagnostic intensity for both payer mix measures at the hospital level. This is consistent with our hypothesis that financial incentives may be a driver of diagnostic overuse at the hospital level as we suspect that diagnostic intensity tracks with diagnostic overuse. There is evidence that financial considerations influence physicians’ non-clinical decisions, including choice of practice locations12 and medical specialization.13 Evidence also suggests that variation in healthcare delivery is due, in part, to financial incentives physicians face. Variation in low-value cancer screening by county income level,14 association between physician ownership of ambulatory surgical centers and volume of surgeries,15 and rates of coronary revascularization after the opening of a physician-owned cardiology specialty hospital relative to a new cardiology program at a general hospital16 all suggest that financial considerations impact clinical decisions. A recent analysis showed that an increase in hospital or health system ownership of physician practices was associated with more lab and imaging tests performed in the hospital relative to non-hospital setting and that overall reimbursement for these tests rose.17 Additionally, an analysis of Medicare Open Payments data found associations between payments from pharmaceutical companies and the rate of prescribing their medications and prescribing more brand name relative to generic drugs.18,19
To date, much of the research relating payer mix to medical intensity has been at regional and patient levels. At the regional level, a systematic review evaluating the relationship between overuse of medications, diagnostic tests, and procedures and different systems of healthcare in the USA did not find that one system (fee-for service versus managed care, the Veterans Affairs health system versus a private setting) was most effective at minimizing overuse (but noted that the evidence was limited).20 One study of seven potentially low-value services found high correlations between overuse in the Medicare fee-for-service population and overuse in the commercially insured population within hospital referral regions.21 Another study found that higher HMO penetration (at the metropolitan statistical area level) was associated with lower hospital revenue which was due to lower prices and to a lesser extent lower utilization.22
At the patient level, the evidence that insurance type affects medical intensity is mixed. A study of Medicare beneficiaries in seven states found that beneficiaries in managed-care plans were less likely to receive guideline-appropriate coronary angiography after myocardial infarction than those in fee-for-service plans.23 A study evaluating the appropriateness of carotid endarterectomy (CEA) for Medicare beneficiaries did not find a significant association between type of Medicare plan (fee-for-service or managed care) and appropriateness of CEA. One study comparing a range of medical services for Medicaid and commercial insurance beneficiaries in Oregon found that Medicaid beneficiaries were more likely to receive ten and less likely to receive five services felt to represent low-value care, suggesting that payer mix may not impact all services uniformly.24 A study of commercially insured patients found that those with consumer-directed health plans (CDHPs) were not less likely to undergo low-value imaging for back pain than those with traditional commercial insurance.25 However, another study evaluating 28 different low-value practices found that commercially insured patients with CDHPs were less likely to receive low-value care.26 None of these studies, however, examined broad utilization at the hospital level—an important limitation given that hospital culture and protocols may be a more potent driver of physician ordering behavior than individual patient insurance status.
The relationship between a hospital’s payer mix and diagnostic intensity has not been well-studied. However, financial and non-financial incentives that may play into a physician’s decision to order a diagnostic test are often crafted at the hospital level. Hospitals with a large number of commercially insured patients and fewer Medicare and Medicaid patients may be more likely to create incentives and/or have a culture that rewards overtesting because they are likely to benefit from such behavior. Fee-for-service Medicare typically pays non-professional hospital fees based on a prospective payment system (diagnosis-related groups) such that hospitals receive a fixed payment for a hospitalization based on the principal diagnosis and associated comorbidities. In this system, additional tests will not lead to higher payments (excluding professional fees). Commercial insurers pay hospital fees based on agreements determined from negotiations between the payer and hospital, and in cases where hospitals have more market power, this fee structure is more likely to be based on a share of hospital charges (such that more diagnostic testing typically leads to more revenue).27
We suspect that the hospital level, rather than the regional or patient level, is where payer mix is most likely to influence incentive structure. It seems less likely that physicians would base their testing decisions for individual patients on their specific insurance. In fact, research does support the existence of “spillover effects,” by which the dominant payer has hospital-wide effects (even on patients with other types of insurance). Greater Medicare managed care penetration at a given hospital has been shown to decrease hospital spending throughout the healthcare system, even for commercially insured patients.28 Similarly, hospitals with stronger market power and larger commercial payer revenues may be less likely to constrain costs and thus more likely to incur losses on Medicare patients than those with a poorer market position who have more of an implicit need to constrain costs.29 Regional payer mixes, on the other hand, may not accurately reflect the payer mixes of individual hospitals within a region.
Limitations
Our DII is a novel measure of hospital-level diagnostic intensity and not a perfect proxy for diagnostic overuse. Its underlying construct does not imply that “negative” (or uninformative) diagnostic testing is necessarily wasteful. However, hospitals with very high rates of uninformative diagnostic testing (very low levels of diagnostic yield) as identified by our DII are likely overusing testing. Recent research supports that low diagnostic yield based on administrative coding data is a valid proxy for diagnostic overuse.30,31
The SID does not include all observation stays that do not result in inpatient hospitalization, so differential use of observation stays among hospitals could have impacted our results. Additionally, we did not control for managed care penetration. The SID does not have complete information on whether a payer—Medicare, Medicaid, or commercial—is fee-for-service or managed care (this is only available for a subset of states and years). Finally, we attempted to control for hospital variation in patient complexity using the Elixhauser comorbidity index score, but this is not a perfect measure of patient complexity, and it is possible that there was unmeasured variation in patient complexity confounding our results.
Future Research Directions
Future research should evaluate the connection between financial incentives and diagnostic overuse using more granular data (for example, comparing rates of stress testing between hospitals that reward cardiologists for high rates of stress testing and those that do not). Further analyses might also evaluate temporal changes in overuse when there is major and rapid change in financial incentives (such as a change in physician salary or bonus structure at a hospital) or secular shifts (such as initiation of the Total Cost of Care model in Maryland or a major regional increase in accountable care organization penetration). Finally, an analysis of the relationship between managed care penetration and diagnostic intensity at the hospital level would be valuable.
CONCLUSION
Payer mix may be an important driver of diagnostic overuse at the hospital level. This suggests that hospital-level payment incentives may be an important lever to reduce diagnostic intensity and costs and that value-based payment models may be effective if a large enough proportion of a hospital’s patients are enrolled.
Supplementary Information
(DOCX 142 kb)
Funding
Drs. Ellenbogen and Brotman are supported by the Johns Hopkins Hospitalist Scholars Fund (internal funding).
Footnotes
Prior Presentations: A preliminary version of this research was presented at the Society of Hospital Medicine National Conference in May 2021.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Oakes AH, Radomski TR. Reducing Low-Value Care and Improving Health Care Value. JAMA. 2021;325(17):1715. doi: 10.1001/jama.2021.3308. [DOI] [PubMed] [Google Scholar]
- 2.Berwick DM, Hackbarth AD. Eliminating Waste in US Health Care. JAMA. 2012;307(14):1513. doi: 10.1001/jama.2012.362. [DOI] [PubMed] [Google Scholar]
- 3.Shrank WH, Rogstad TL, Parekh N. Waste in the US Health Care System: Estimated Costs and Potential for Savings. JAMA. 2019;322(15):1501. doi: 10.1001/jama.2019.13978. [DOI] [PubMed] [Google Scholar]
- 4.Colla CH, Morden NE, Sequist TD, Schpero WL, Rosenthal MB. Choosing Wisely: Prevalence and Correlates of Low-Value Health Care Services in the United States. J Gen Intern Med. 2014;30(2):221–228. doi: 10.1007/s11606-014-3070-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Segal JB, Nassery N, Chang HY, Chang E, Chan K, Bridges JFP. An index for measuring overuse of health care resources with medicare claims. Medical Care. 2015;53(3):230–236. doi: 10.1097/MLR.0000000000000304. [DOI] [PubMed] [Google Scholar]
- 6.Oakes AH, Sen AP, Segal JB. Understanding Geographic Variation in Systemic Overuse Among the Privately Insured. Medical Care. 2020;58(3):257–264. doi: 10.1097/MLR.0000000000001271. [DOI] [PubMed] [Google Scholar]
- 7.Ellenbogen MI, Prichett L, Johnson PT, Brotman DJ. Development of a Simple Index to Measure Overuse of Diagnostic Testing at the Hospital Level Using Administrative Data. J Hosp Med. 2021;16(2):77–83. doi: 10.12788/jhm.3547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.ICD-9-CM Official Guidelines for Coding and Reporting. Centers for Disease Control and Prevention. Accessed March 15, 2019. https://www.cdc.gov/nchs/data/icd/icd9cm_guidelines_2011.pdf
- 9.MLN Fact Sheet - Medicare Disproportionate Share Hospital. Medical Learning Network - Department of Health and Human Services. 2017. Accessed 10 Nov 2018. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/Disproportionate_Share_Hospital.pdf
- 10.Moore BJ, White S, Washington R, Coenen N, Elixhauser A. Identifying Increased Risk of Readmission and In-hospital Mortality Using Hospital Administrative Data: The AHRQ Elixhauser Comorbidity Index. Medical Care. 2017;55(7):698–705. doi: 10.1097/MLR.0000000000000735. [DOI] [PubMed] [Google Scholar]
- 11.Disproportionate Share Hospital (DSH). Centers for Medicare and Medicaid Services. Accessed 22 Oct 2020. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/dsh
- 12.Chang RK, Halfon N. Geographic distribution of pediatricians in the United States: an analysis of the fifty states and Washington, DC. Pediatrics. 1997;100(2 Pt 1):172–179. doi: 10.1542/peds.100.2.172. [DOI] [PubMed] [Google Scholar]
- 13.Nicholson S. Physician Specialty Choice under Uncertainty. Journal of Labor Economics. 2002;20(4):816–847. doi: 10.1086/342039. [DOI] [Google Scholar]
- 14.Welch HG, Fisher ES. Income and Cancer Overdiagnosis — When Too Much Care Is Harmful. New England Journal of Medicine. 2017;376(23):2208–2209. doi: 10.1056/NEJMp1615069. [DOI] [PubMed] [Google Scholar]
- 15.Hollingsworth JM, Ye Z, Strope SA, Krein SL, Hollenbeck AT, Hollenbeck BK. Physician-Ownership Of Ambulatory Surgery Centers Linked To Higher Volume Of Surgeries. Health Affairs. 2010;29(4):683–689. doi: 10.1377/hlthaff.2008.0567. [DOI] [PubMed] [Google Scholar]
- 16.Nallamothu BK. Opening of Specialty Cardiac Hospitals and Use of Coronary Revascularization in Medicare Beneficiaries. JAMA. 2007;297(9):962. doi: 10.1001/jama.297.9.962. [DOI] [PubMed] [Google Scholar]
- 17.Whaley CM, Zhao X, Richards M, Damberg CL. Higher Medicare Spending On Imaging And Lab Services After Primary Care Physician Group Vertical Integration: Study examines higher Medicare spending on imaging and lab services after primary care physician group vertical integration. Health Affairs. 2021;40(5):702–709. doi: 10.1377/hlthaff.2020.01006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ornstein C, Tigas M, Jones R. Now There’s Proof: Docs Who Get Company Cash Tend to Prescribe More Brand-Name Meds. ProPublica; 2016. Accessed March 24, 2021. https://www.propublica.org/article/doctors-who-take-company-cash-tend-to-prescribe-more-brand-name-drugs
- 19.Fresques F. Doctors Prescribe More of a Drug If They Receive Money from a Pharma Company Tied to It. ProPublica; 2019. Accessed March 24, 2021. https://www.propublica.org/article/doctors-prescribe-more-of-a-drug-if-they-receive-money-from-a-pharma-company-tied-to-it
- 20.Keyhani S, Falk R, Howell EA, Bishop T, Korenstein D. Overuse and systems of care: a systematic review. Medical Care. 2013;51(6):503–508. doi: 10.1097/MLR.0b013e31828dbafe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Colla CH, Morden NE, Sequist TD, Mainor AJ, Li Z, Rosenthal MB. Payer Type and Low-Value Care: Comparing Choosing Wisely Services across Commercial and Medicare Populations. Health Serv Res. 2018;53(2):730–746. doi: 10.1111/1475-6773.12665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shen YC, Wu VY, Melnick G. Trends in hospital cost and revenue, 1994-2005: How are they related to HMO penetration, concentration, and for-profit ownership? Health Serv Res. 2010;45(1):42–61. doi: 10.1111/j.1475-6773.2009.01047.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guadagnoli E, Landrum MB, Peterson EA, Gahart MT, Ryan TJ, McNeil BJ. Appropriateness of coronary angiography after myocardial infarction among Medicare beneficiaries. Managed care versus fee for service. N Engl J Med. 2000;343(20):1460–1466. doi: 10.1056/NEJM200011163432006. [DOI] [PubMed] [Google Scholar]
- 24.Charlesworth CJ, Meath THA, Schwartz AL, McConnell KJ. Comparison of Low-Value Care in Medicaid vs. Commercially Insured Populations. JAMA Intern Med. 2016;176(7):998–1004. doi: 10.1001/jamainternmed.2016.2086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hong AS, Ross-Degnan D, Zhang F, Frank Wharam J. Small decline in low-value back imaging associated with the “choosing wisely” campaign, 2012-14. Health Affairs. 2017;36(4):671–679. doi: 10.1377/hlthaff.2016.1263. [DOI] [PubMed] [Google Scholar]
- 26.Reid RO, Rabideau B, Sood N. Low-Value Health Care Services in a Commercially Insured Population. JAMA Intern Med. 2016;176(10):1567. doi: 10.1001/jamainternmed.2016.5031. [DOI] [PubMed] [Google Scholar]
- 27.Cooper Z, Craig SV, Gaynor M, Van Reenen J. The Price Ain’t Right? Hospital Prices and Health Spending on the Privately Insured*. Q J Econ. 2019;134(1):51–107. doi: 10.1093/qje/qjy020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Baicker K, Chernew ME, Robbins JA. The spillover effects of Medicare managed care: Medicare Advantage and hospital utilization. J Health Econ. 2013;32(6):1289–1300. doi: 10.1016/j.jhealeco.2013.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stensland J, Gaumer ZR, Miller ME. Private-Payer Profits Can Induce Negative Medicare Margins. Health Affairs. 2010;29(5):1045–1051. doi: 10.1377/hlthaff.2009.0599. [DOI] [PubMed] [Google Scholar]
- 30.Venkatesh AK, Agha L, Abaluck J, Rothenberg C, Kabrhel C, Raja AS. Trends and Variation in the Utilization and Diagnostic Yield of Chest Imaging for Medicare Patients With Suspected Pulmonary Embolism in the Emergency Department. Am J Roentgenol. 2018;210(3):572–577. doi: 10.2214/AJR.17.18586. [DOI] [PubMed] [Google Scholar]
- 31.Kline JA, Garrett JS, Sarmiento EJ, Strachan CC, Courtney DM. Over-Testing for Suspected Pulmonary Embolism in American Emergency Departments: The Continuing Epidemic. Circ Cardiovasc Qual Outcomes. 2020;13(1). 10.1161/CIRCOUTCOMES.119.005753 [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 142 kb)