Abstract
Theory and research suggest chronic direct and indirect exposures to racism impact health, and stress-responsive inflammation may play a role in these paths. This study examines links between forms of racism-related stress, salivary markers of inflammation during acute psychosocial stress, and perinatal mental and physical health in a racially heterogenous sample. Pregnant people (n = 108, 27% non-white) self-reported personal and vicarious exposure to racism (racial microaggressions, online racism, overt racial/ethnic discrimination) and racial collective self-esteem, as well as affective symptoms and general physical health. Five saliva samples collected before and after the Trier Social Stress Test were assayed for pro-inflammatory cytokines and C-reactive protein. Results revealed associations between racism-related stress and greater inflammatory reactivity/delayed recovery to acute stress, between racial collective self-esteem and lower levels of inflammation, and between profiles of inflammatory responses to stress and mental and physical symptoms. We discuss implications for understanding perinatal health disparities.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40615-022-01442-z.
Keywords: Racial disparities, Perinatal health, Racism-related stress, Inflammatory response
Racial and ethnic disparities in perinatal mental and physical health have become increasingly recognized as public health crises. Approximately one in five child-bearers experience some type of mental disorder during the perinatal period, most commonly depression and/or anxiety [1, 2], which in turn are associated with parental and neonatal morbidity and mortality, including preeclampsia, cardiovascular disease, preterm birth, and fetal growth impairment [3, 4]. Minoritized Black, Indigenous, and People of Color (BIPOC) child-bearers are two to three times more likely to experience adverse obstetric and pregnancy outcomes in comparison to their white counterparts [5]. There is also higher prevalence and severity of perinatal depression and psychological distress among child-bearers from minoritized racial/ethnic groups [6–8], with emerging research suggesting the COVID-19 pandemic has further exacerbated these racial/ethnic disparities [9]. This differential persists even when accounting for structural risk factors such as socioeconomic status [10] and despite improvements in healthcare quality and access [5], making it all the more urgent to identify and address root causes driving ongoing disparities.
Historically, the literature on perinatal health disparities has focused on the ways that systems and structures (e.g., racial segregation, access to healthcare, income inequality) negatively impact health and development [11], leaving unanswered questions about more proximal influences of racism-related stress and mechanisms by which such stressors impact child-bearers’ health. The present study aims to shed light on pathways by which various forms of racism-related stress may shape health disparities during this critical time. We use cross-sectional data to provide an initial test of proposed links between pregnant people’s experiences of racism-related stress, inflammatory stress responsiveness, and mental health.
Racism-Related Stress, Collective Identity Trauma, and Perinatal Health
Within a racialized context such as the USA, people of all races are exposed in some way to a ubiquitous climate of racism inherent at various levels, from societal structures to media content to interpersonal interactions; however, the way in which a person is racialized dictates differences in both the degree of personal exposure to racist experiences directed against oneself/one’s group and its impact on wellbeing, an imbalance that in turn help to explain widespread health disparities. People from minoritized racial/ethnic groups experience individual, cultural, institutional, and structural racism and discrimination across the lifespan [12]. These interconnected experiences range from interpersonally mediated micro-level insults (e.g., implicit and explicit insults to identity status and exclusions) to macro-aggressions (e.g., personal and vicarious exposure to overt racism, state sanctioned violence and policies perpetuating racism, hate crimes) and serve as persistent psychosocial stressors impacting wellbeing [13]. Developmentally based trauma frameworks help to explain how the persistent collective identity threats presented by such forms of racism may exert ongoing harm—including but not limited to the perinatal period—by classifying these as a type III continuous identity trauma [14]. According to this perspective, the chronic and pervasive racism perpetuated by individuals and social systems continuously traumatizes those from minoritized racial/ethnic groups, depleting the psychosocial reserves needed to cope and sensitizing them to other sources of stress or trauma [14, 15].
These collective identity traumas may be particularly salient during the perinatal period, which can bring increased exposure to racism and discrimination [16, 17], and racism-related stress has been established as a driver of adverse perinatal mental health outcomes [7]. Current knowledge is limited by reliance on retrospective reporting of overt discrimination, and the prospective impacts of more subtle or vicarious forms of interpersonally mediated racism (e.g., microaggressions and online or vicarious experiences of racism) on perinatal health remain largely unknown. This represents a critical omission given escalating exposure to online racism [18], which in turn has been associated with poorer mental health across racial/ethnic groups [19].
Racism-Related Stress, Risk, and Resiliency
To understand and work to alleviate sources of perinatal health disparities, it is critical to determine not only which factors associate with collective identity threaten and/or protect child-bearers’ health, but also how they may do so via stress-responsive physiological mechanisms. Health relies on co-regulation of interconnected stress-responsive neurophysiological systems—i.e., hypothalamic-pituitary-adrenal (HPA) axis, autonomic nervous system (ANS), and immune system (IS) responses that match the demands of a given stressor and recover promptly once it has passed. Chronic exposure to interpersonal stressors, particularly those involving social threat (e.g., social conflict, evaluation, rejection, isolation, and exclusion) have been found to disrupt these core physiological systems [20]. Growing research supports the weathering hypothesis [21], which posits that repeated experiences of racism-related stress and threats to one’s identity give rise to race-based traumatic symptoms and disrupt the body’s stress-responsive systems over time [22, 23]. Indeed, racism-related stress exposure has been linked to elevated glucocorticoids, C-reactive protein (CRP), pro-inflammatory cytokines, and other endocrine risk indicators, not only among BIPOC samples but also in studies of whites [13, 24].
The weathering hypothesis posits that racial health disparities reflect changes in biological process, but there are significant gaps in knowledge of the physiological consequences of racism-related stress during the perinatal period. Prior research has focused primarily on non-pregnant adults [22, 25] and on autonomic and cardiovascular measures. The impact of racism-related stress on immune activity may be particularly relevant during the perinatal period. Acute and chronic stressors can activate key pro-inflammatory pathways, with elevated inflammation in turn linked to obstetric complications such as premature delivery, and to perinatal mental and physical health risks including mood and anxiety disorders [26, 27]; however, no studies to our knowledge have directly tested links between perinatal racism-related stress, inflammatory stress reactivity, and health.
Emerging research supports the utility of salivary markers of inflammation such as IL-6, IL-1ß, TNFα, and CRP that increase in response to acute stress [28] and may serve as important biomarkers of health in their own right, in addition to traditional blood-based biomarkers [29–31]. Studies have demonstrated associations between elevated salivary IL-6, IL-1ß, and/or TNFα measured in response to acute stress and both lifetime trauma exposure and mental health conditions such as PTSD [32–34]. A handful of studies further provide evidence that measures of racism-related stress—i.e., perceived discrimination, fear of deportation among Mexican-origin families—relate to higher stress-responsive salivary inflammation (indexed by CRP, IL-6, or a composite of IL-1ß, IL-6, IL-8, and TNFα) in racially diverse samples [35–37]. Together, these studies support the use of salivary inflammatory markers to identify mechanisms involved in paths from racism-related stressors to perinatal health disparities.
Finally, the social identity approach to health suggests it is important to consider not only risk but also sources of resilience related to collective identity that could be leveraged in perinatal health promotion efforts [38]. Potentially countering the impacts of ongoing racism-related stress and collective identity traumas is collective self-esteem—i.e., one’s personal esteem held for one’s cultural group, and one’s the belief that others feel positively about their cultural group. Collective racial self-esteem has been found to be a coping resource for dealing with psychological distress arising from the fear of experiencing discrimination, at least in discrete BIPOC groups—Chinese and African American—of young adults [39, 40]. To our knowledge, this finding has yet to be extended to more diverse racially/ethnically heterogenous samples and to the perinatal period specifically.
Current Study
In the current study, we investigated cross-sectional associations between reported exposures to overt and subtle or indirect forms of racism and the dysregulation of stress-responsive physiological systems—particularly inflammatory mediators—and mental/physical health in a community sample of pregnant people in a midwestern micro-urban area of the United States. Although exposure to racism-related stress disproportionately impacts the BIPOC community, examining racism-related stress in diverse samples that include both minoritized and non-minoritized racial/ethnic groups is needed to explore potential population-wide effects and disparities. This approach is consistent with understanding that a focus on social determinants of health, such as racism-related stressors, may be more important than studying self-identified race per se, especially in light of recognition of an absence of biological foundation for the concept of race [41, 42]. Indeed, it has been argued that appreciating the full costs of racism for community health requires a wider lens, and that such awareness can help spur needed change at structural levels [43]. This approach allows us to examine the racialized experiences—both more overt/direct/personal and more covert/indirect/vicarious—that drive effects of racism across a community of white and non-white individuals and, by so doing, shed light on the underlying imbalances in preponderance and impact of such experiences that result in disparate health outcomes.
Guided by the aim of illuminating underlying social determinants of perinatal health disparities, we test the primary hypotheses that (1) self-reported exposure to racism-related stress will be associated with stress-induced salivary inflammation during a psychosocial stress session; and (2) collective self-esteem will exert the opposite effect (both as a main effect and as a moderator mitigating racism-related stress). In a secondary step to contextualize and interpret these primary tests, we examine effects involving specific forms of racism-related stress and individual inflammatory markers (IL-6, IL-1ß, TNF-α, and CRP), as well as whether racism-related stress and stress-induced inflammation in turn relate to poorer perinatal health (mood, anxiety and trauma symptoms, physical health problems). Finally, we explore potential moderation of both risk—racism-related stress—and protective—collective self-esteem—effects by participant identification with a minoritized racial/ethnic group to probe whether differential strength of effects could help to explain disparities between white European-American child-bearers and those from minoritized BIPOC groups.
Method
Table 1 provides further descriptive information about the study sample and measures outlined below.
Table 1.
Sample descriptive characteristics
| Variable | Summary statistic |
|---|---|
| Racial/ethnic identification | Proportion |
| White European-American | 73% |
| Black | 9% |
| Latinx | 8% |
| Asian American | 9% |
| Relationship status | |
| Married | 76% |
| Engaged or dating exclusively | 12% |
| Single or dating non-exclusively | 12% |
| Median or mean, SD (range) | |
| Education | College degree (< high school–doctoral degree) |
| Household income | $50,000–$75,000 (< $25,000 to > $200,000) |
| Age | 30, 5.3 (19–40) |
| Microaggressions | 1.88, .28 (1.43–3.30) |
| Perceived discrimination | 1.34, .48 (1.00–3.88) |
| Perceived online racism | 1.47, .41 (1.00–3.47) |
| Depressive symptoms | 11.67, 8.34 (2–38; 24% of sample > 16) |
| Mood and anxiety symptoms | 2.05, .51 (1.27–3.87) |
| Trauma symptoms | 19.69, 12.14 (0–61) |
| Physical symptoms | 2.73, .76 (1.21–4.71) |
| Collective self-esteem | 4.80, .88 (2.50–6.62) |
Microaggressions = mean score on R28REMS; perceived discrimination = mean score on PEDQ-CV; perceived online racism = mean score on PORS; depressive symptoms = total score on CES-D; mood and anxiety symptoms = mean score on MASQ-D30; trauma symptoms = total score on TSC-40; physical symptoms = mean score on PHQ; collective self-esteem = mean score on CSES
Participants
Participants were child-bearers (n = 108) who had completed the prenatal visit of a larger study (BLINDED) and whose data were available for inclusion in the current analysis. Pregnant people were recruited from local health centers, community agencies, and advertisements (e.g., flyers, listserv emails, social media advertisements) in a small midwestern community. To be eligible, participants were required to be adult English speakers, < 32 weeks pregnant with a singleton, and planning to stay in the region for the first two years postnatal. Consistent with Census data [44], participants’ race self-identification reflected the micro-urban midwestern community from which they were drawn. Potential participants were not excluded based on medication use or reported health conditions that did not interfere with completing study requirements, though these factors were considered as potential control variables in analyses.
Procedure
Prior to participating in the study, child-bearers provided written informed consent. During the prenatal visit at 28–32 weeks of pregnancy, conducted either in the laboratory or (as needed during the COVID-19 pandemic) remotely via Zoom1, participants completed a set of questionnaires using Qualtrics, engaged in a psychosocial stress task, and gave saliva samples. The Trier Social Stress Test [TSST, 45] was employed to simulate an acute interpersonal stressor, as it is the most widely used standardized protocol for studies of psychosocial stress and stress biomarker reactivity. The 12-min task asks participants to first prepare and deliver a speech and then perform a mental arithmetic task while being videotaped and rated on their performance by a confederate. Sessions were conducted in the afternoon to minimize the impact of diurnal fluctuations in stress hormones. Five saliva samples were collected during the session to tap stress responsivity. Participants contributed an initial saliva sample by passively drooling into a collection tube before the TSST and the second sample immediately following the task. The remaining samples were collected at 20, 40, and 60 min following peak stress (beginning of mental arithmetic task).
Measures
Determination of Salivary Analytes
Following Riis and colleagues [47], all maternal saliva samples were assayed in duplicate for inflammatory markers (TNFα, IL-1ß IL-6, CRP). On day of assay, samples were allowed to thaw on the bench top until reaching room temperature and centrifuged at 3500 rpm for 15 min to pellet any remaining mucins. The Human CRP (Vascular Injury Panel 2) V-Plex Meso Scale Discovery (MSD)® multi-spot Assay (Ref# K0080900) was employed to measure salivary CRP. Saliva samples are diluted 5-fold (MSD® Assay Diluent) prior to assay. The Human ProInflammatory V-Plex Meso Scale Discovery (MSD)® multi-spot Assay (Ref# K008074) was employed to measure cytokines. Saliva samples are diluted 2-fold in (MSD® Assay Diluent) prior to assay. Salivary analyte concentrations (pg/mL) were determined with MSD Discovery Workbench Software (v. 4.0) using curve fit models (4-PL with a weighting function option of 1/y2). MSD® determines the detection limit for each analyte by interpolating the mean concentration minus 2.5 (SDs) (Avg Concentration blank + 2.5 (SDblank) over several kit lots. Intra- and inter-assay coefficients of variation were, on average, less than 10% and 15%, respectively [see also 36]. The averages of duplicate assay results were used in all statistical analyses.
Perinatal Racism Exposure
Participants reported on perinatal experiences of racism by completing questionnaires assessing experiences of racial microaggressions, online racism exposure, and overt racial and ethnic discrimination.
Racial microaggression exposure was measured using the Revised Racial and Ethnic Microaggressions Scale [R28REMS, 48], which measures exposure to racial microaggressions and subtle statements and behaviors that unconsciously communicate denigrating messages about racial groups. The scale consists of 30 items with subscales for (a) assumptions of inferiority, (b) second-class citizen and assumptions of criminality, (c) microinvalidations, (d) exoticization/assumptions of similarity, (e) environmental microaggressions, and (f) workplace and school microaggressions. Responses are recorded on a 5-point Likert scale indicating the frequency of experiences that occurred in the past 6 months, where 1 indicates “I did not experience this event” and 5 indicates “I experienced this event 10 or more times.” Internal consistency according to Cronbach’s alpha (.73) was adequate in our sample, with somewhat lower reliability in the white subset (.61) suggesting caution should be exercised in interpretation of what scores mean for this (presumably non-minoritized) group. At the same time, research by scale authors comparing experiences of racial microaggression across white and various BIPOC racial/ethnic groups [49] supports the use of the measure in a racially heterogenous sample such as ours.
Overt racism and discrimination exposure was measured using the Perceived Ethnic Discrimination Questionnaire–Community Version [PEDQ-CV, 50] which measures perceived racial or ethnic discrimination across ethnic groups. The four subscales measure several subdimensions of racism: (a) exclusion, (b) stigmatization, (c) workplace discrimination, and (d) overt threats. The scale consists of 34 items and responses are recorded on a 5-point Likert scale indicating the frequency of experiences that occurred in the past six months, from 1 (never happened) to 5 (happened very often) Internal consistency was strong (alpha = .94; .89 in white subset). This scale was normed with a racially heterogenous sample that included white participants [50], again supporting use of the measure in the current sample.
Online racism exposure was measured using the Perceived Online Racism Scale [PORS, 51] which measures perceived online racist interpersonal interactions and exposure to online racist content. Three subscales assess: (a) personal experience of racial cyber-aggression, (b) vicarious exposure to racial cyber-aggression, and (c) online mediated exposure to racist reality. The scale consists of 22 items and responses are recorded on a 5-point Likert scale indicating the frequency of experiences that occurred in the past six months, from 1 (never) to 5 (all of the time). Internal consistency was good (alpha = .91; .91 in white subset). This scale, while thus far normed only in a BIPOC sample, includes items that tap general racism exposure (not necessarily directed toward oneself/one’s own racial/ethnic group), suggesting it could be applied to a racially heterogenous sample such as the current one.
Perinatal Health
Participants reported on their health with questionnaires assessing affective distress (i.e., depression, anxiety) and trauma symptoms, as well as general physical health.
Affective Symptoms
Participants reported depression symptoms using the Center for Epidemiologic Studies Depression Scale [CES-D, 52], which involves rating the frequency of 20 symptoms of depression in the past week on a 4-point scale (1 = rarely or none of the time to 4 = most or all of the time). Internal consistency reliability (.88) was good for this measure and consistent with prior studies in racially heterogenous samples.
Participants also reported on a broader spectrum of internalizing distress symptoms using a short form of the Mood Anxiety Symptoms Questionnaire [MASQ-D30, 53]. The 30 items tap depression-specific anhedonic depression, anxiety-specific anxious arousal, and general distress symptoms common to both internalizing syndromes. Child-bearers rated how much they had experienced each symptom in the past week on a 5-point scale (1 = not at all to 5 = extremely) Internal consistency was consistent with prior studies in racially heterogenous samples (alpha = .92).
Trauma Symptoms
Trauma symptoms were measured by the Trauma Symptom Checklist–40 [TSC-40, 54]. Participants rated the frequency of 40 symptoms in the past 2 months on a 4-point scale (0 = never to 4 = often). Symptoms tap multiple domains found to be impacted by trauma exposure: anxiety, depression, sexual difficulties, and dissociation. Internal consistency was consistent with prior studies for this measure (alpha = .91).
Physical Health
Participants completed the Physical Health Questionnaire [PHQ, 55] to assess physical wellbeing. This 14-item measure probes the degree to which the respondent has experienced various markers of physical health including sleep quantity/quality, headaches and gastrointestinal distress, and common infectious diseases such as cold and flu. Participants rate their experience of each item in the past month on a 7-point scale from 1 = not at all to 7 = all of the time. Good internal consistency (alpha = .84) was consistent with prior studies.
Collective self-esteem was measured using the Race-Specific Collective Self-Esteem Scale [CSES, 56] which measures participants’ perceptions and feelings related to racial group membership. The four subscales measure personal judgments of one’s social groups, perceptions of how others evaluate one’s social groups, and importance of one’s social groups memberships to self-concept in general (no time range specified). The scale consists of 16 items, and respondents indicate their agreement with each on a 7-point scale. Internal consistency was consistent with prior studies in racially heterogenous samples that included both white and BIPOC participants (alpha = .88; .89 in white subset). This measure was originally validated in majority-white samples similar to that in the current study, further supporting its use here.
Analytic Strategy
Guided by our overall study plan outlined above, and with consideration to how little is currently known about specific associations between each of these stress-induced salivary inflammatory markers and aspects of race-related risk or protection, we tested hypotheses using a two-stage approach in which (1) a composite measure of each construct under investigation was modeled, followed by (2) tests of individual measures to offer both a global and a more fine-grained assessment of these associations. To the extent that results in this cross-sectional sample prove consistent with the larger theoretical model proposed, the current study will provide a basis for a longitudinal study designed to provide confirmatory testing of the broader model. Bivariate associations between salivary analytes and potential control variables—including reported medication use and oral health—did not reveal any consistent associations at p <.10 and so none were included in model testing.
Results
Preliminary Analyses
Supplemental Table S1 presents zero-order correlations among study measures examined, and S2-S3 break down means and correlations by racial/ethnic marginalization status to offer a descriptive picture of group differences in this sample. Correlations among specific measures tapping salivary inflammation, racism-related stress, and collective self-esteem were examined to confirm that composite measures could be constructed for the first stage of model testing.
Baseline Models
All inflammatory markers were correlated with one another (r’s = .36–.64, average r = .50), so an inflammation composite was formed by standardizing each individual marker score and computing the mean; this served as the primary outcome in analyses, with follow-up tests conducted on each individual inflammatory marker to pinpoint specific effects. A quadratic function—i.e., intercept, linear slope, and quadratic slope—was used to model inflammation trajectories across the session. On average, child-bearers displayed an accelerating curve (significantly positive quadratic slope) that decreased during the initial portion of the session followed by an increase in the latter portion. Significant between-person variability was found for intercepts and linear slopes (χ2[105] = 1486.65 and 261.36, both p < .001) but not for quadratic slopes (χ2[105] = 123.85, p = .10); therefore, subsequent models fixed the quadratic term, and effects of between-person predictors on this parameter were not interpreted further. When individual inflammatory marker trajectories were examined, the same overall pattern—i.e., significantly accelerating response curve across the session characterized by decreasing and then increasing inflammation—was noted, with significant between-person variability in all intercepts and linear slopes, as well as in quadratic slopes for IL1-ß and TNF-α.
Explanatory Models—Effects of Racism-Related Stress (Table 2, Top Panel)
Table 2.
Predictions from racism-related stress (top panel) and racial collective self-esteem (lower panel) to child-bearers’ salivary inflammation response to stress
| Predictor of inflammation composite trajectory | Intercept (post-stress level) | Linear slope (post-stress reactivity/recovery) | Quadratic slope (overall response curvature) | |||
|---|---|---|---|---|---|---|
| γ [95% CI] | p | γ [95% CI] | p | γ [95% CI] | p | |
| Racism-related stress composite | .039 [− .14, .22] | .678 | .033 [.001, .065] | .045 | .007 [− .017, .031] | .585 |
| Perceived ethnic/racial discrimination | .065 [− .21, .34] | .647 | .009 [− .023, .041] | .581 | .008 [− .014, .030] | .467 |
| Racial ethnic microaggressions | − .0005 [− .17, .17] | .995 | .046 [.017, .076] | .004 | .015 [− .013, .043] | .284 |
| Perceived online racism | .036 [− .13, .20] | .676 | .012 [− .018, .042] | .426 | − .003 [− .026, .020] | .772 |
| Collective racial self-esteem | − .145 [− .33, .036] | .113 | − .022 [− .058, .014] | .213 | .006 [− .016, .028] | .587 |
| Participant ethnic/racial group (White European-American) | .142 [− .044, .33] | .132 | − .031 [− .067, .005] | .096 | .004 [− .017, .026] | .686 |
| Participant ethnic/racial group × collective racial self-esteem | − .265 [− .44, − .086] | .005 | .016 [− .023, .055] | .412 | .004 [− .021, .029] | .755 |
Gammas represent standardized coefficients; significant effects (p < .05) highlighted in bold
The racism-related stress measures—racial and ethnic microaggressions, online racism exposure, and racial ethnic discrimination exposure—were significantly correlated with one another (r’s = .31–.56, average r = .47), so a mean of standardized scale scores was created to provide a composite index of racism-related stress. The first study hypothesis was addressed by testing the racism-related stress composite as a main effect predictor of inflammation composite trajectories, followed by more specific tests of effects involving individual racism-related stress measures and inflammatory markers. Interactions of racism-related stress with participant minoritization status were also explored to determine whether effects differed depending on whether the child-bearer identified as white European-American (non-minoritized) or another racial/ethnic group (minoritized).
A main effect of the racism-related stress composite on inflammation linear slopes in the positive direction suggested that participants experiencing greater racism-related stress tended to recover less from and/or react more to the stress task (see Fig. 1, top panel). When individual measures were considered, significant paths were detected between the racism-related stress composite and the IL-6 component of inflammation; and between the microaggressions component of racism-related stress in particular and the inflammation composite, as well as CRP, IL1-ß, and IL-6 components. The best-fitting explanatory model with racial and ethnic microaggressions predicting the inflammation composite trajectories offered a significant improvement compared to baseline according to change in the deviance statistic, χ2(3) = 11.74, p = .008, and explained 11% of the variance in linear slopes, representing a medium effect size. Further examination of the subscales within the measure revealed this effect was driven by experiences of microaggressions involving microinvalidations and assumptions of inferiority, criminality, and similarity (but not environmental microaggressions). The interaction of racism-related stress with minoritization status was nonsignificant (standardized coefficients predicting inflammation trajectory terms ranging from − .0085 to .0046, p’s = .75–.95).
Fig. 1.
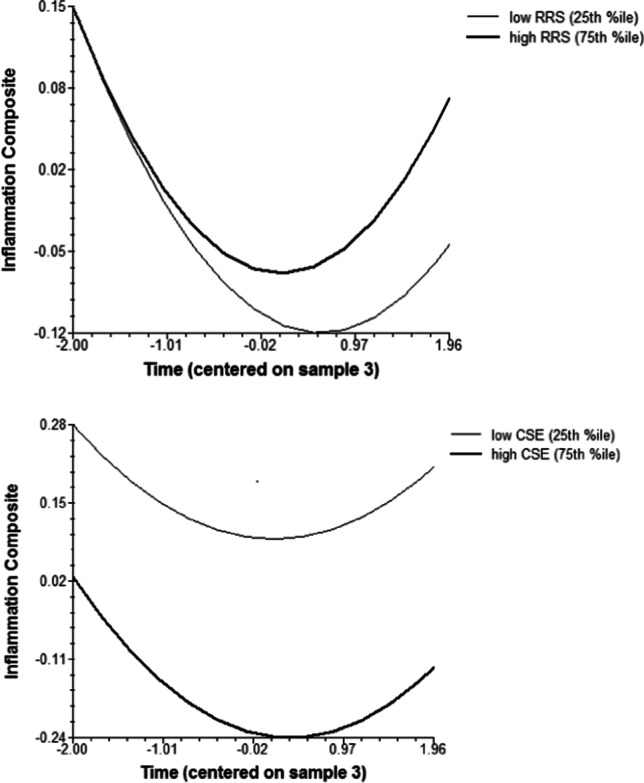
Child-bearers’ expected salivary inflammation trajectories vary by composite racism-related stress (top panel) and racial collective self-esteem (lower panel)
Explanatory Models—Effects of Collective Self-Esteem (Table 2, Lower Panel)
To address the second study hypothesis, models testing main effects of racial collective self-esteem (broader composite measures followed by individual component measures) and then the hypothesized interaction with racism-related stress were examined. Again, the interaction with participant minoritization status was tested in an exploratory manner. Racial collective self-esteem significantly predicted lower inflammation composite intercepts—meaning that participants reporting higher collective self-esteem typically had lower levels of salivary inflammation during the session (see Fig. 1, lower panel)—and this effect was evident for each individual inflammatory marker with the exception of TNFα. Examination of specific subscales showed that the effect was driven by racial collective private self-esteem in particular.
When moderated effects were examined, we found that the hypothesized interaction between racial collective self-esteem and racism-related stress was nonsignificant (standardized coefficients predicting inflammation trajectory terms ranging from − .017 to .0061, p’s = .18–.98), failing to provide support for hypothesis 2. However, an interaction with participant minoritization status was detected such that white European-American child-bearers showed a stronger inflammation-lowering effect of racial collective self-esteem than did their BIPOC counterparts. A region of significance calculation using Preacher, Curran, and Bauer’s [57] online utility confirmed that whereas non-minoritized participants displayed a significant inflammation-lowering effect of collective self-esteem (simple slope = − .31, p = .002), the effect was nonsignificant for those from minoritized racial/ethnic groups (simple slope = .28, p = .12). This moderated effect was significant for the IL-6 and TNFα inflammation components and marginally significant for CRP. The best-fitting explanatory model with participant minoritization status by collective self-esteem predicting the inflammation composite trajectories offered a significant improvement compared to baseline according to change in the deviance statistic, χ2(3) = 15.50, p = .001, and explained 12% of the variance in intercepts, representing a medium effect size.
Secondary Models—Relations with Health
To provide a preliminary interpretive context for understanding how racial collective identity risk/protective measures and accompanying profiles of physiological stress responding might impact child-bearers’ wellbeing, associations with measures of psychological and physical symptoms were examined. The racism-related stress composite correlated with higher symptoms (r’s = .30 to .33, p’s < .003), and racial collective self-esteem with lower symptoms (r’s = − .22 to − .34, p’s < .02), for all measures tested: CES-D depressive symptoms, MASQ affective symptoms, TSC trauma symptoms, and PHQ physical health symptoms. When individual scales were considered, racial and ethnic microaggressions related significantly to CES-D depressive symptoms, MASQ general distress, and TSC dissociation; and both racial/ethnic discrimination and online racism exposure related to all symptom measures.
Although the inflammation composite as a whole did not relate significantly to symptoms, individual inflammatory markers did show associations with symptoms, all in the positive direction: CRP and IL1-ß intercepts related to higher CES-D depressive symptoms; CRP intercepts additionally related to higher MASQ affective symptoms, TSC trauma symptoms, and PHQ physical health symptoms; and IL-6 linear slopes related to higher MASQ anxious arousal. In summary, the above model results show that the stress response characteristics associated with greater racism-related stress and/or lower racial collective self-esteem—i.e., higher salivary inflammation levels and more positive slopes following the stress task—were also associated with adverse perinatal health outcomes.
Discussion
Findings from the current study provide support for an association between a key social determinant of health disparities and both stress-responsive inflammation and perinatal health. Specifically, reported exposure to racism-related stress related to greater inflammatory stress reactivity and prolonged recovery from acute stress, as well as to mental and physical health difficulties during pregnancy. Collectively our observations raise the possibility of negative impacts of exposure to racism toward one’s own and/or other groups—whether experienced directly or indirectly—while shedding light on possible roots of racial/ethnic disparities.
Our findings highlight potential consequences of the more subtle insidious experiences of racism typically receiving less attention. The relation between racism-related stress exposure and inflammatory stress response and recovery was specific to experiences of microaggressions, especially those involving microinvalidations and assumptions of inferiority, criminality, and similarity. Microaggressions—including gendered racial microaggressions in particular—are being recognized as a form of continuous identity trauma giving rise to traumatic stress symptoms [58, 59], though the underlying processes by which these operate to harm child-bearers’ health are less understood given the dearth of previous research investigating stress-responsive mediators in perinatal samples. The current findings are consistent with the idea that chronic and pervasive experiences of subtle continuous identity trauma place a burden on stress-responsive physiological systems—including specific inflammation markers such as IL-6 and CRP implicated in previous studies of overt discrimination in non-perinatal samples [35, 37]—and may deplete psychosocial reserves needed to cope with subsequent stressors. These findings are particularly concerning given the frequency of microaggressions—e.g., 40% of minoritized participants in a large North American sample reporting occurrence of racial discrimination at least once a week [60]—and links to adverse perinatal outcomes [61].
We further found that experiences of discrimination, microaggressions, and online racism related to perinatal health, such that greater exposure to racism-related stress related to elevated affective symptoms and poorer physical health. These findings are consistent with a large body of research in the general population emphasizing racism-related stress as a social determinant of mental and physical health [62, 63] while extending our knowledge regarding processes underlying health risks in the perinatal period, as well as potential intergenerational impacts given downstream effects of child-bearers’ health on infant development and subsequent risk for disorder. In the present sample, stress response characteristics associated with greater racism-related stress exposure (i.e., greater inflammatory stress reactivity and prolonged recovery) were associated with adverse mental and physical health outcomes. Elevated CRP emerged as a consistent correlate of affective and somatic distress, highlighting this marker specifically as a potentially important index of risk. Overall, these results support our hypothesis that racism-related stress may confer risk for perinatal mental and physical disorder via dysregulation of the inflammatory stress response system.
In efforts to identify potential protective factors that may mitigate the risk of racism-related stress for perinatal health, we also examined the buffering potential of racial collective identity. Contrary to prior research suggesting a protective effect of collective self-esteem for racial/ethnic minority groups [39, 40], we did not find that collective identity moderated the effect of racism-related stress in the current sample. Instead, we found the effect of racial collective self-esteem was itself moderated by minoritization status, such that it significantly predicted lower stress-related inflammation for participants who identified as white European-Americans only. This may suggest entrenched racism-related imbalances operate in part through inherent asymmetry in the context in which esteem derived from racial identity develops. Systems of oppression that threaten the collective identity of BIPOC communities do not similarly threaten that of white communities, and it is possible our finding simply captured the effect identity-related pride can exert in the absence of persistent collective identity traumas. In line with the reasoning that white Americans’ personal and vicarious exposure to racism does not convey a collective identity threat carrying a similar psychological and physiological toll, white Americans’ endorsement of experiences of racism have not been found to be associated with the same adverse mental health outcomes as in BIPOC samples [64], a pattern that is also reflected in the present sample. This finding should be interpreted as preliminary and requires replication in larger samples that can better represent the diversity of BIPOC experiences and explore potential moderators such as strength of racial identification.
The current study examined both personal and vicarious exposure to racism-related stressors in a sample comprising the range of racial/ethnic identities that characterize a micro-urban midwestern community in the USA. It is possible that vicarious exposure to racism towards groups other than one’s own may impart harm across minoritized and non-minoritized racial groups [65], and these potential impacts merit investigation in future research. Another question for further exploration regards the ways in which processes detected here may differ across minoritized and non-minoritized child-bearers. There are two bases on which we believe that these measures can be meaningfully interpreted in those who are presumably not the target of racism. First, there is the precedent of previous research with these racism-related stress measures including white and BIPOC participants. Second, the measures contain a mix of items tapping both (a) more general exposure to a racist environment and (b) personal endorsement of perceived race-related discrimination (with the latter types of items likely reflecting something other than actual racism for white participants). While beyond the scope of the current study to probe differences in meaning/interpretation across minoritized and non-minoritized individuals, it may be that such endorsements of race-based discrimination reflect a more generalized sensitivity to social evaluative threat and/or heightened levels of outgroup threat in these child-bearers [66]. Based on theorizing about different costs of racism types identified by Spanierman et al. [65], this pattern may reflect an “insensitive and afraid” profile in which white individuals who have low empathy for and high fear of BIPOC people respond defensively to delivering and/or witnessing racial microaggressions, including with attributions of reverse racism [67]. Our results provide preliminary evidence for the health-related costs of such patterns, in line with the call for further research addressing antecedents and consequences of racism for white individuals. As noted by Clark and Spanierman [67], such research is needed to inform and tailor training models that can help white individuals move toward the behavioral changes that would alleviate ongoing harm to BIPOC communities.
While acknowledging the potential for such distinctions regarding interpretation across minoritized and non-minoritized racialized groups, the current study findings help shed light on sources of known perinatal health disparities by highlighting adverse impacts of racism-related stress we found to be greater in both level of exposure and associations with mental health outcomes among minoritized child-bearers (see supplemental analyses separately describing central tendencies and correlations of racism-related stress measures for white and BIPOC participants). This in turn points to targets for alleviating such disparities through interventions that lessen exposure to racism and associated stressors during this time. Importantly, these results underline that programs aiming to improve perinatal health disparities should address systemic factors driving experiences of racism-related stress and not assume that building individual-level buffers such as collective self-esteem are sufficient to bring about positive change. Indeed, a recent test of a novel racism stress coping intervention [68] showed limited effects on hypothesized inflammation outcomes (TNFα, CRP), highlighting the need for multifaceted change strategies to address entrenched inequities driving health.
Limitations and Future Directions
Even as this study shines a spotlight on promising links between racism-related stress, inflammatory stress reactivity, and perinatal health and provides key initial cross-sectional evidence for proposed paths in the larger hypothesized model, it carries notable limitations that will inform next steps in this work. As acknowledged above, the current sample was relatively modest in size and comprised predominantly white European-American child-bearers. Thus, it may not adequately represent the experiences of child-bearers of color, and further examination in a larger sample containing a higher proportion of child-bearers of minoritized race/ethnicity is merited. At the same time, very small effect sizes suggest that even larger samples may not change the results, and recent calls advocate moving away from a focus on racial/ethnic group categorization toward interrogation of the underlying structural inequities and social determinants impacting health in order to understand and ameliorate disparities [41]. We were also limited to examining concurrent associations at a single timepoint. This makes it difficult to definitively test paths of influence, and conclusions must be tempered accordingly. Further testing of prospective effects on child-bearer health controlling for baseline levels with the completion of the next phase of collection for this longitudinal dataset will offer a stronger basis for concluding that inflammatory stress response helps to explain racism-related stress effects on perinatal health.
The measurement of racism-related stress and health outcomes, although expanding beyond many prior studies by including indirect or vicarious racism exposure and a range of mental and physical health symptoms, was also limited in scope and may not fully capture racism-related stress impacts. Relatedly, we were unable to assess potential intersectional identity threats that may compound harms, and samples representing greater diversity along multiple dimensions will be needed to probe whether there is evidence for compounded or synergistic effects of multiple marginalization (e.g., through sexual/gender minority, disability, and/or class status). Future research that further expands the range of measured identity-related risks, and/or that taps different dimensions of mental and physical health, will help to shed light on when and how racism-related stress exerts the most harmful influences.
The collective identity measure used in this study was likewise limited, and the meaning of this measure for white populations is questionable. For example, it may be that the collective racial self-esteem score tapped into white supremacist beliefs in white European-American participants that help them to justify and thus downgrade the threat of observed racism. It will be important to explore further what this measure may represent for different groups and potentially give white individuals more constructive ways of coping with the awareness of racism and their own involvement in this system by raising awareness and offering tools to work as anti-racist allies [69].
Limitations notwithstanding, the current cross-sectional study provides a useful foundation for a broader explanatory model of how prenatal exposures to racism-related stress drive health disparities going forward into the postpartum via inflammatory stress mediators. In particular, the repeated elicitation of pro-inflammatory reactions by racism-related stressors during pregnancy may help to understand and predict disproportionate risks of obstetric complications and postpartum mental/physical health difficulties affecting BIPOC child-bearers and their infants, opening new areas for prevention and intervention. This possibility underlines the importance of further attention to this understudied system in acute stress situations to understand and intervene on health disparities during this critical life period.
Supplementary Information
Supplementary Information
Below is the link to the electronic supplementary material.
Funding
This work was supported by NICHD grant 1R01HD093627-01A1 awarded to Dr. Laurent.
Declarations
Conflict of Interest
The authors declare no competing interests.
Ethics Approval
This study was performed in line with the principles of the Declaration of Helsinki. All procedures were reviewed and approved by the Institutional Review Board (protocol 18002) at a large midwestern university.
Footnotes
Fourteen of the 108 participants took part in remote sessions. Consistent with recent research in adults [46] showing that internet-delivered TSST elicits equivalent psychophysiological stress responses to the traditional in-person version, we found no differences between remote and laboratory session stress responses as measured by affective state (post-task Positive Negative Affect Schedule scores) and salivary inflammatory biomarkers, group comparison p’s ranging from .17 to .99.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Dennis CL, Falah-Hassani K, Shiri R. Prevalence of antenatal and postnatal anxiety: systematic review and meta-analysis. Br J Psychiatry. 2017;210:315–323. doi: 10.1192/bjp.bp.116.187179. [DOI] [PubMed] [Google Scholar]
- 2.Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: a systematic review of prevalence and incidence. Obstetr Gynecol. 2005;106:1071–1083. doi: 10.1097/01.AOG.0000183597.31630.db. [DOI] [PubMed] [Google Scholar]
- 3.Howard LM, Khalifeh H. Perinatal mental health: a review of progress and challenges. World Psychiatry. 2020;19:313–327. doi: 10.1002/wps.20769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bauer A, Knapp M, Parsonage M. Lifetime costs of perinatal anxiety and depression. J Affect Disord. 2016;192:83–90. doi: 10.1016/j.jad.2015.12.005. [DOI] [PubMed] [Google Scholar]
- 5.Burris HH, Hacker MR. Birth outcome racial disparities: a result of intersecting social and environmental factors. Sem Perinatol. 2017;41:360–366. doi: 10.1053/j.semperi.2017.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ertel KA, Rich-Edwards JW, Koenen KC. Maternal depression in the United States: nationally representative rates and risks. J Women’s Health. 2011;20:1609–1617. doi: 10.1089/jwh.2010.2657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Masters GA, Asipenko E, Bergman AL, Person SD, Brenckle L, Moore Simas TA, Ko JY, Robbins CL, Byatt N. Impact of the COVID-19 pandemic on mental health, access to care, and health disparities in the perinatal period. J Psychiatric Res. 2021;137:126–130. doi: 10.1016/j.jpsychires.2021.02.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rich-Edwards JW, Kleinman K, Abrams A, Harlow BL, McLaughlin TJ, Joffe H, Gillman MW. Sociodemographic predictors of antenatal and postpartum depressive symptoms among women in a medical group practice. J Epidemiol Community Health. 2006;60:221–227. doi: 10.1136/jech.2005.039370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Diaz A, Baweja R, Bonatakis JK, Baweja R. Global health disparities in vulnerable populations of psychiatric patients during the COVID-19 pandemic. World J Psychiatry. 2021;11:94–108. doi: 10.5498/wjp.v11.i4.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rosenthal L, Lobel M. Explaining racial disparities in adverse birth outcomes: unique sources of stress for Black American women. Soc Sci Med. 2011;72:977–983. doi: 10.1016/j.socscimed.2011.01.013. [DOI] [PubMed] [Google Scholar]
- 11.Berry OO, Londoño Tobón A, Njoroge WFM. Social determinants of health: the impact of racism on early childhood mental health. Curr Psychiatry Rep. 2021;23:23. doi: 10.1007/s11920-021-01240-0. [DOI] [PubMed] [Google Scholar]
- 12.Brondolo E, Gallo LC, Myers HF. Race, racism and health: disparities, mechanisms, and interventions. J Behav Med. 2009;32:1–8. doi: 10.1007/s10865-008-9190-3. [DOI] [PubMed] [Google Scholar]
- 13.Lewis TT, Cogburn CD, Williams DR. Self-reported experiences of discrimination and health: scientific advances, ongoing controversies, and emerging issues. Annu Rev Clin Psychol. 2015;11:407–440. doi: 10.1146/annurev-clinpsy-032814-112728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kira IA, Hanaa S, Bujold-Bugeaud M. Gender discrimination (GD): a conceptual trauma-based framework for GD and the development of gender discrimination inventory. Psychol. 2015;6:2041–2070. doi: 10.4236/psych.2015.616201. [DOI] [Google Scholar]
- 15.Kira IA, Omidy AZ, Fawzi M, Rice KG, Fawzi M, Lewandowski L, Bujold-Bugeaud M. Are the negative mental health effects of gender discrimination (GD) salient across cultures? Does self-esteem mediate these effects: GD as a continuous traumatic stress and the pathways to its negative dynamics? Psychol. 2015;6:93–116. doi: 10.4236/psych.2015.61009. [DOI] [Google Scholar]
- 16.Rosenthal L, Earnshaw VA, Lewis TT, Reid AE, Lewis JB, Stasko EC, Tobin JN, Ickovics JR. Changes in experiences with discrimination across pregnancy and postpartum: age differences and consequences for mental health. Am J Public Health. 2015;105:686–693. doi: 10.2105/AJPH.2014.301906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Scott KA, Davis D. Obstetric racism: naming and identifying a way out of black women’s adverse medical experiences. Am Anthropol. 2021;123:681–684. doi: 10.1111/aman.13559. [DOI] [Google Scholar]
- 18.Dubey AD. The resurgence of cyber racism during the COVID-19 pandemic and its aftereffects: analysis of sentiments and emotions in tweets. JMR Pub Health Surveill. 2020;6:e19833. doi: 10.2196/19833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tao X, Fisher CB. Exposure to social media racial discrimination and mental health among adolescents of color. J Youth Adol. 2020;51:30–44. doi: 10.1007/s10964-021-01514-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Slavich GM, Sacher J. Stress, sex hormones, inflammation, and major depressive disorder: extending social signal transduction theory of depression to account for sex differences in mood disorders. Psychopharmacology. 2019;236:3063–3079. doi: 10.1007/s00213-019-05326-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. Am J Pub Health. 2006;96:826–833. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carter SE, Gibbons FX, Beach SRH. Measuring the biological embedding of racial trauma among Black Americans utilizing the RDoC approach. Dev Psychopathol. 2021;33:1849–1863. doi: 10.1017/S0954579421001073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carter RT, Mazzula S, Victoria R, Vazquez R, Hall S, Smith S, Sant-Barket S, Forsyth J, Bazelais K, Williams B. Initial development of the Race-Based Traumatic Stress Symptom Scale: assessing the emotional impact of racism. Psychol Trauma. 2013;5:1–9. doi: 10.1037/a0025911. [DOI] [Google Scholar]
- 24.Pascoe EA, Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psychol Bull. 2009;135:531–554. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zahodne LB, Kraal AZ, Zaheed A, Farris P, Sol K. Longitudinal effects of race, ethnicity, and psychosocial disadvantage on systemic inflammation. Soc Sci Med - Popul Health. 2019;7:100391. doi: 10.1016/j.ssmph.2019.100391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Knight EL, Jiang Y, Rodriguez-Stanley J, Almeida DM, Engeland CG, Zilioli S. Perceived stress is linked to heightened biomarkers of inflammation via diurnal cortisol in a national sample of adults. Brain Behav Immun. 2021;93:206–213. doi: 10.1016/j.bbi.2021.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stevenson DK, Wong RJ, Aghaeepour N, Maric I, Angst MS, Contrepois K, Darmstadt GL, Drusin ML, Eisenberg ML, Gaudilliere B, Gibbs RS, Gotlib IH, Gould JB, Lee HC, Ling XB, Mayo JA, Moufarrej MN, Quaintance CC, Quake SR, Relman DA, Sirota M, Snyder MP, Sylvester KG, Hao S, Wise PH, Shaw GM, Katz M. Towards personalized medicine in maternal and child health: Integrating biologic and social determinants. Pediatr Res. 2021;89:252–258. doi: 10.1038/s41390-020-0981-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Slavish DC, Graham-Engeland JE, Smyth JM, Engeland CG. Salivary markers of inflammation in response to acute stress. Brain Behav Immun. 2015;44:253–269. doi: 10.1016/j.bbi.2014.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chauhan A, Yadav SS, Dwivedi P, Lal N, Usman K, Khattri S. Correlation of serum and salivary cytokines level with clinical parameters in metabolic syndrome with periodontitis. J Clin Lab Anal. 2016;30:649–655. doi: 10.1002/jcla.21917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gohel V, Jones J, Wehler C. Salivary biomarkers and cardiovascular disease: a systematic review. Clin Chem Lab Med. 2018;56:1432–1442. doi: 10.1515/cclm-2017-1018. [DOI] [PubMed] [Google Scholar]
- 31.Silvestre-Rangil J, Bagán L, Silvestre F-J, Martinez-Herrera M, Bagán J. Periodontal, salivary and IL-6 status in rheumatoid arthritis patients A cross-sectional study. Med Oral Patol Oral Cir Bucal. 2017;22:e595–e600. doi: 10.4317/medoral.21937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Newton TL, Fernandez-Botran R, Miller JJ, Burns VE. Interleukin-6 and soluble interleukin-6 receptr levels in posttraumatic stress disorder: associations with lifetime diagnostic status and psychological context. Biol Psychol. 2014;99:150–159. doi: 10.1016/j.biopsycho.2014.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Szabo YZ, Fernandez-Botran R, Newton TL. Cumulative trauma, emotion reactivity and salivary cytokine levels following acute stress in healthy women. Anxiety Stress Coping. 2019;32:82–94. doi: 10.1080/10615806.2018.1524377. [DOI] [PubMed] [Google Scholar]
- 34.Wang Z, Mandel H, Levingston CA, Young MRI. An exploratory approach demonstrating immune skewing and loss of coordination among cytokines in plasma and saliva of veterans with combat-related PTSD. Hum Immunol. 2016;77:652–657. doi: 10.1016/j.humimm.2016.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lucas T, Wegner R, Pierce JMA, Lumley MA, Laurent HK, Granger DA. Perceived discrimination, racial identity, and multisystem stress response to social evaluative threat among African American men and women. Psychosom Med. 2017;79:293–305. doi: 10.1097/PSY.0000000000000406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Martinez AD, Ruelas L, Granger DA. Household fear of deportation in relation to chronic stress and salivary proinflammatory cytokines in Mexican-origin families post-SB-1070. Soc Sci Med Pop Health. 2018;5:188–200. doi: 10.1016/j.ssmph.2018.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Saban KL, Mathews HL, Bryant FB, Tell D, Joyce C, DeVon HA, Janusek LW. Perceived discrimination is associated with the inflammatory response to acute laboratory stress in women at risk for cardiovascular disease. Brain Behav Immun. 2018;73:625–632. doi: 10.1016/j.bbi.2018.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jetten J, Haslam SA, Cruwys T, Greenaway KH, Haslam C, Steffens NK. Advancing the social identity approach to health and wellbeing: progressing the social cure research agenda. Eur J Soc Psychol. 2017;47:789–802. doi: 10.1002/ejsp.2333. [DOI] [Google Scholar]
- 39.Du H, King RB, Chi P. Self-esteem and subjective well-being revisited: the roles of personal, relational, and collective self-esteem. PLoS One. 2017;12:e0183958. doi: 10.1371/journal.pone.0183958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Constantine MG, Donnely PC, Myers LJ. Collective self-esteem and africultural coping styles in African American adolescents. J Black Stud. 2002;32:698–710. doi: 10.1177/00234702032006004. [DOI] [Google Scholar]
- 41.Shim RS, Compton MT. Addressing the social determinants of mental health: If not now, when? If not us, who? Psychiatr Serv. 2018;69:844–846. doi: 10.1176/appi.ps.201800060. [DOI] [PubMed] [Google Scholar]
- 42.Trujillo AK, Kesse EN, Rollins O, Della Sala S, Cubelli R. A discussion on the notion of race in cognitive neuroscience research. Cortex. 2022;150:153–164. doi: 10.1016/j.cortex.2021.11.007. [DOI] [PubMed] [Google Scholar]
- 43.Lee Y, Muennig P, Kawachi I, Hatzenbuehler ML. Effects of racial prejudice on the health of communities: A multilevel survival analysis. Am J Pub Health. 2015;105:2349–2355. doi: 10.2105/AJPH.2015.302776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.U.S. Census Bureau. Selected housing characteristics, 2010-2019 American Community Survey. 2020; Retrieved from https://www.census.gov/quickfacts/champaigncountyillinois.
- 45.Kirschbaum C, Pirke KM, Hellhammer DH. The ‘Trier Social Stress Test’— a tool for investigating psychobiological stress responses in a laboratory setting. Neuropsychobiol. 1993;28:76–81. doi: 10.1159/000119004. [DOI] [PubMed] [Google Scholar]
- 46.Eagle DE, Rash JA, Tice L, Proeschold-Bell RJ. Evaluation of a remote, internet-delivered version of the Trier Social Stress Test. Int J Psychophysiol. 2021;165:137–144. doi: 10.1016/j.ijpsycho.2021.03.009. [DOI] [PubMed] [Google Scholar]
- 47.Riis JL, Ahmadi H, Hamilton KR, Hand T, Granger DA. Best practice recommendations for the measurement and interpretation of salivary proinflammatory cytokines in biobehavioral research. Brain Behav Immun. 2021;91:105–116. doi: 10.1016/j.bbi.2020.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Forrest-Bank S, Jenson JM, Trecartin S. The revised 28-item Racial and Ethnic Microaggressions Scale (R28REMS): Examining the factorial structure for Black, Latino/Hispanic, and Asian young adults. J Soc Serv Res. 2015;41:1–19. doi: 10.1080/01488376.2014.987944. [DOI] [Google Scholar]
- 49.Forrest-Bank S, Jenson J. Differences in experiences of racial and ethnic microaggression among Asian, Latino/Hispanic, Black, and White young adults. J Sociol Soc Welfare. 2015;42:141–161. [Google Scholar]
- 50.Brondolo E, Kelly KP, Coakley V, Gordon T, Thompson S, Levy E, Cassells A, Tobin JN, Sweeney M, Contrada RJ. The Perceived Ethnic Discrimination Questionnaire: Development and preliminary validation of a community version. J Appl Soc Psychol. 2005;35:335–365. doi: 10.1111/j.1559-1816.2005.tb02124.x. [DOI] [Google Scholar]
- 51.Keum BT, Miller MJ. Racism in digital era: development and initial validation of the Perceived Online Racism Scale (PORS v10) J Couns Psychol. 2017;64:310–324. doi: 10.1037/cou0000205. [DOI] [PubMed] [Google Scholar]
- 52.Radloff LS. The CESD-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- 53.Wardenaar KJ, van Veen T, Giltary EJ, de Beurs E, Penninx BWJH, Zitman FG. Development and validation of a 30-item short adaptation of the Mood and Anxiety Symptoms Questionnaire (MASQ) Psychiatr Res. 2010;179:101–106. doi: 10.1016/j.psychres.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 54.Elliot DA, Briere J. Sexual abuse trauma among professional women: validating the Trauma Symptom Checklist-40 (TSC-40) Child Abuse Negl. 1992;16:391–398. doi: 10.1016/0145-2134(92)90048-V. [DOI] [PubMed] [Google Scholar]
- 55.Schat A, Kelloway K, Desmarais S. The Physical Health Questionnaire (PHQ): Construct validation of a self-report scale of somatic symptoms. J Occup Health Psychol. 2005;10:363–381. doi: 10.1037/1076-8998.10.4.363. [DOI] [PubMed] [Google Scholar]
- 56.Luhtanen R, Crocker J. A collective self-esteem scale: self-evaluation of one’s social identity. Personal Psychol Bull. 1992;18:302–318. doi: 10.1177/0146167292183006. [DOI] [Google Scholar]
- 57.Preacher KJ, Curran PJ, Bauer DJ. Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. J Educ Behav Stat. 2006;31:437–448. doi: 10.3102/10769986031004437. [DOI] [Google Scholar]
- 58.Dale SK, Safren SA. Gendered racial microaggressions predict posttraumatic stress disorder symptoms and cognitions among Black women living with HIV. Psychol Trauma. 2019;11:685–694. doi: 10.1037/tra0000467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Moody AT, Lewis JA. Gendered racial microaggressions and traumatic stress symptoms among Black women. Psychol Women Q. 2019;43:201–214. doi: 10.1177/0361684319828288. [DOI] [Google Scholar]
- 60.Cénat JM, Hajizadeh S, Dalexis RD, Ndengeyingoma A, Guerrier M, Kogan C. Prevalence and effects of daily and major experiences of racial discrimination and microaggressions among Black individuals in Canada. J Interpers Violence. 2021; online ahead of print. [DOI] [PubMed]
- 61.Slaughter-Acey JC, Sealy-Jefferson S, Helmkamp L, Caldwell CH, Osypuk TL, Platt RW, Straughe JK, Dailey-Okezie RK, Abeysekara P, Misra DP. Racism in the form of micro aggressions and the risk of preterm birth among black women. Ann Epidemiol. 2016;26:7–13. doi: 10.1016/j.annepidem.2015.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Salihu HM, Salinas-Miranda AA, King LM, Dongarwar D, Yusuf KK, Ibrahimi S, Ikedionwu CA, Berry EL. Racism, psycho-social stress, and health-related quality of life. Int J MCH AIDS. 2020;9:73–76. doi: 10.21106/ijma.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Williams DR. Stress and the mental health of populations of color: advancing our understanding of race-related stressors. J Health Soc Behav. 2018;59:466–485. doi: 10.1177/0022146518814251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Soto JA, Dawson-Andoh NA, BeLue R. The relationship between perceived discrimination and generalized anxiety disorder among African Americans, Afro Caribbeans, and non-Hispanic Whites. J Anxiety Disord. 2011;25:258–265. doi: 10.1016/j.janxdis.2010.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Spanierman LB, Poteat VP, Beer AM, Armstrong PI. Psychosocial costs of racism to Whites: exploring patterns through cluster analysis. J Couns Psychol. 2006;53:434–441. doi: 10.1037/0022-0167.53.4.434. [DOI] [Google Scholar]
- 66.Stephan WG, Boniecki KA, Ybarra O, Bettencourt A, Ervin KS, Jackson LA, McNatt PS, Renfro CL. The role of threats in the racial attitudes of blacks and whites. Pers Soc Psychol Bull. 2002;28:1242–1254. doi: 10.1177/01461672022812009. [DOI] [Google Scholar]
- 67.Clark DA, Spanierman L. “I didn’t know that was racist”: costs of racial microaggressions to white people. In: Torino GC, Rivera DP, Capodilup CM, Nadal KL, Sue DW, editors. Microaggression theory: influence and implications. Hoboken, New Jersey: Wiley & Sons; 2019. pp. 138–155. [Google Scholar]
- 68.Saban KL, Motley D, Shawahin L, Mathews HL, Tell D, De La Pena P, Janusek LW. Preliminary evidence for a race-based stress reduction intervention for Black women at risk for cardiovascular disease. Complement Ther Med. 2021;58:102710. doi: 10.1016/j.ctim.2021.102710. [DOI] [PubMed] [Google Scholar]
- 69.Kivel P. Uprooting racism: how white people can work for racial justice. Philadelphia, PA: New Society Publishers; 1996. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


