Abstract
The Bacillus cereus-group (B. cereus sensu lato) includes common, usually avirulent species, often considered contaminants of patient samples in routine microbiological diagnostics, as well as the highly virulent B. anthracis. Here we describe 16 isolates from 15 patients, identified as B. cereus-group using a MALDI-TOF MS standard database. Whole genome sequencing (WGS) analysis identified five of the isolates as B. anthracis species not carrying the typical virulence plasmids pXO1 and pXO2, four isolates as B. paranthracis, three as B. cereus sensu stricto, two as B. thuringiensis, one as B. mobilis, and one isolate represents a previously undefined species of Bacillus (B. basilensis sp. nov.). More detailed analysis using alternative MALDI-TOF MS databases, biochemical phenotyping, and diagnostic PCRs, gave further conflicting species results. These cases highlight the difficulties in identifying avirulent B. anthracis within the B. cereus-group using standard methods. WGS and alternative MALDI-TOF MS databases offer more accurate species identification, but so far are not routinely applied. We discuss the diagnostic resolution and discrepancies of various identification methods.
Keywords: Bacillus anthracis, Bacillus cereus, clinical microbiology, MALDI-TOF MS, Next generation sequencing, Routine Diagnostics, Taxonomy, Whole genome sequencing
1Introduction
The genus Bacillus is a large heterogeneous group, belonging to the phylum Firmicutes, mainly characterized as aerobic and endospore-forming. Taxonomic misclassifications exist within the genus, leading to proposals to restrict the genus to the two clades of B. subtilis-group and B. cereus-group [1,2]. Bacteria belonging to the B. cereus-group are saprophytic, gram-positive, facultative anaerobic, catalase positive, motile, and spore-forming rods. The B. cereus-group comprises at least eight closely related species: B. cereus sensu stricto (here referred to as B. cereus), B. anthracis, B. thuringiensis, B. mycoides, B. pseudomycoides, B. cytotoxicus, B. weihenstephanensis, and B. toyensis [1,3]. Isolates of the B. cereus-group are commonly found in soil and food, and few, with the exception of B. anthracis, are considered clinically relevant [4]. B. cereus and B. anthracis are the best-studied representatives within the group, responsible for opportunistic food poisoning and the acute and often fatal anthrax disease, respectively [5]. The virulence of B. anthracis is enabled by two virulence plasmids, pXO1 and pXO2, carrying genes encoding for the tripartite toxin and the poly-γ-D-glutamic acid capsule, respectively [5,6].
In clinical routine diagnostics, the fast and reliable identification of B. cereus and B. anthracis is crucial because of the pathogenic and biothreat potential of B. anthracis. The identification is classically based on morphological features. B. anthracis is typically described as non-hemolytic on blood agar with a “Medusa's head” colony morphology. In contrast, B. cereus causes hemolysis and has a grey matt colony morphology [7,8]. Additionally, they can be distinguished by motility, and penicillin and phage γ susceptibility, where B. anthracis shows susceptibility to both [[7], [8], [9], [10], [11]]. Biochemical reaction profiles can differentiate B. anthracis from other members of the B. cereus-group [10,12]. However, phenotypic characteristics may vary within and among species resulting in inconsistent species identification [10]. Species distinction by 16S ribosomal RNA gene sequencing has proven to be difficult [3,5,13]. Standard MALDI-TOF mass spectrometry (MALDI-TOF MS) is faster but reliable differentiation within the B. cereus-group is difficult using commercial databases [14,15]. Alternative diagnostic approaches include specific PCRs targeting toxins, virulence plasmids and chromosomal markers [16]. In order to investigate the ancestral relatedness of isolates and assign species accordingly, genomics provides the gold standard. Many methods have been used to classify genomes within the B. cereus-group: digital DNA:DNA hybridization (dDDH) [3]; the Genome Taxonomy Database (GTDB) [10,17], and average nucleotide identity (ANI), perhaps with a proposed genomospecies cutoff at 92.5% rather than the accepted 95-96% cutoff [18]. Using any of these methods, cases of discrepancy in allocating isolates to species have been described. To add to the confusion, the presence of virulence factors does not always correlate with species identification, as some isolates closely related to B. anthracis do not carry pXO1 and pXO2 [3,19,20]. Conversely, these plasmids have been found within the genome of other Bacillus species [21].
In this study we analyze 16 clinical B. cereus-group isolates from 15 patients, assigned to the B. cereus-group by clinical and morphological features and the MALDI-TOF MS Bruker standard database (sDB). We describe the isolates in depth using phenotypic and genomic methods to highlight the diagnostic complexity.
2Material and methods
2.1Sample collection and culture
The 16 B. cereus-group isolates (Table 1) were collected during July 2019, and between July and September 2021, as well as isolates from interesting clinical cases across this timeframe. Isolates were cultured on Columbia blood agar, supplemented with 5% sheep blood (BD Becton Dickinson, New Jersey, USA) at 37°C under aerobic atmosphere supplemented with 5% CO2 over 24 hours.
Table 1.
Clinical features and evaluation of clinical relevance of B. cereus-group isolates. Names of isolates identified genomically as B. anthracis are shown in bold. The isolate name identified as B. basilensis sp. nov. is shown in italics. ID, identification; PICC, peripherally inserted central venous catheter; NA, not available; MRSA, Methicillin-resistant Staphylococcus aureus; dd, differential diagnosis; GVHD, graft versus host disease; Age groups: 1, <18years; 2, 18-50years; 3, >50years; Amounts: +, low; ++, moderate; +++, numerous; CFU, colony-forming unit. Detailed case reports of selected isolates are given in the supplementary material.
| Sample number | Age group | Date of collection | Material | Localization | Culture result (amount) | Infectious disease consultation interpretation | Clinical relevance of B. cereus-group |
|---|---|---|---|---|---|---|---|
| 128633-19 | 2 | 07/19 | Blood | Not known | B. cereus-group | Bacteremia (1/6 bottles positive), dd spondylodiscitis | Relevant |
| 607738-19 | 3 | 07/19 | Swab | Lower leg | B. cereus-group (2 CFU), Enterococcus faecalis (++) | Soft tissue infection after compartment lower leg (E. faecalis) | Not relevant |
| 130277-19 | 2 | 07/19 | Blood | Venous catheter | Staphylococcus hominis, B. cereus-group | Polymicrobial Hickman Catheter infection (3/4 bottles positive) | Relevant |
| 607730-19 | 2 | 07/19 | Biopsy | Upper leg | B. cereus-group (+), Streptococcus constellatus (+), S. aureus (1 CFU), Haemophilus parainfluenzae (+), Prevotella denticola (+) | Colonization of wound | Not relevant |
| 130415-19 | 3 | 07/19 | Blood | Venous peripher | B. cereus-group | Contamination (1/4 bottles positive) | Not relevant |
| 608121-20 | 2 | 08/20 | Swab | Finger | Kocuria spp. (1 CFU), B. cereus-group (+) | Soft tissue and bone infection | Relevant |
| 804229-21 | 1 | 09/21 | Swab | Nose | B. cereus-group (+) | Postnatal adaption disorder, pneumonitis, screening for MRSA | Not relevant |
| 607095-21 | 3 | 07/21 | Biopsy | Lower leg | E. faecalis (+++), B. cereus-group (++) | Soft tissue infection after compartment lower leg (E. faecalis, B. cereus-group) | Relevant |
| 203778-21 | 2 | 08/21 | Swab | Vaginal | B. cereus-group (1 CFU), vaginal flora (+++), gram labile rods (morphotype gardnarella) (+++) | NA | Not relevant |
| 402914-21 | 1 | 08/21 | Swab | Skin abdomen | Skin flora (+), B. cereus-group (1 CFU) | Common B-cell acute lymphoblastic leukemia; stem cell transplantation; facial herpes zoster | Not relevant |
| 129606-21 | 3 | 08/21 | Blood | PICC line | B. cereus-group | Contamination (1/4 bottles positive) | Not relevant |
| 607632-21 | 3 | 08/21 | Biopsy | Lower leg | E. faecalis (+), B. cereus-group (+) | Soft tissue infection after compartment lower leg (E. faecalis, B. cereus-group) | Relevant |
| 403206-21 | 3 | 08/21 | Swab | Cheeks | B. cereus-group (+++), Mixta calida (+++), S. aureus (++), S. hominis (++) | Superficial swab for dermatitis | Not relevant |
| 403291-21 | 2 | 09/21 | Swab | Abdomen | S. aureus (+), B. cereus-group (1 CFU) | Abscess/skin infection with S. aureus | Not relevant |
| 403507-21 | 3 | 09/21 | Swab | Lower arm | B. cereus-group (+) | Colonization of wound | Not relevant |
| 135455-21 | 3 | 09/21 | Blodd | PICC line | B. cereus-group | Polymicrobial catheter infection/dd enteritis with GVHD | Relevant |
2.2Evaluation of clinical relevance
All clinical cases were evaluated regarding the clinical relevance of the B. cereus-group isolates by an infectious diseases specialist.
2.3Species identification
MALDI-TOF MS Microflex LT (Bruker Daltonics, Billerica, Massachusetts, USA) was used, from single bacterial colonies using a simple smear technique with a 1-μl formic acid overlay and cyano-4-hydroxyinnamic acid (CHCA) matrix solution, compared against the main spectra library Bruker Daltonics DB (BDAL, containing 8468 MSP, revision 9) and subsequently against the security relevant DB (SR DB) MBT SR Taxonomy (2017, containing 200 MSP). Additionally, a full protein extraction protocol was performed [22] and spectra collected on Axima™ Confidence (Shimadzu-Biotech Corp., Kyoto, Japan) were compared against the Mabritec® BCG-Classifier contained in the PAPMID™ database [23], which includes ribosomal marker profiles for B. anthracis isolates with and without virulence plasmids. Phenotypic species identification was performed on the VITEK®2 System software version 8.01, (bioMérieux S.A., Marcy-l'Étoile, France) using the VITEK®2 BCL card according to the manufacturer's protocols. This offers to identify Bacillus species using 46 test substrates (Supplemental material Table 1) [12,24]. We identified four key reactions to distinguish B. anthracis from B. cereus: L-lysine arylamidase (LysA), maltotriose (MTE), N-acetyl-D-glucosamine (NAG), and growth in 6.5% NaCl (VITEK® representative, personal communication).
Antibiotic susceptibility testing (AST) for penicillin, clindamycin, levofloxacin and vancomycin was performed using the gradient diffusion method (MIC Test Strip, Liofilchem®, Italy) on Müller-Hinton agar (BD Becton Dickinson, New Jersey, USA) resulting in minimum inhibitory concentrations (MIC) in mg/L. Penicillin was interpreted by Clinical and Laboratory Standards Institute (CLSI) breakpoints, and clindamycin, levofloxacin and vancomycin by European Committee on Antimicrobial Susceptibility Testing (EUCAST) breakpoints [25,26]. Specific PCR assays for B. anthracis targeted the virulence plasmids pXO1 and pXO2 (Supplemental material Table 2), and the chromosomal gyrA gene [27].
2.4Whole genome sequencing and analysis
DNA was extracted using a Qiagen EZ1 and Qiagen DNA tissue kit, per manufacturer's instructions. WGS used the Illumina DNA prep kit, and NextSeq500 Illumina platform (PE150). Read data was assembled using Unicycler v0.3.0b [28] and annotated using Prokka v1.13 [29]. Long read sequencing was performed on the GridIon (Oxford Nanopore Technologies) following rapid barcoding. Hybrid assembly was performed using Unicycler v0.4.8 [28], and contigs under 1kb removed. Read data and assemblies have been submitted under project PRJEB48754. The 16S rRNA gene was extracted from assemblies and compared against the NCBI 16S rRNA database using Blastn. Assemblies were analysed for MLST (https://pubmlst.org/organisms/bacillus-cereus), rMLST (https://pubmlst.org/species-id), using the TYGS database [30] with additional genomes added for context, GTDB (https://gtdb.ecogenomic.org/), and abricate (https://github.com/tseemann/abricate) using the NCBI [31] and VFDB [32] databases. fastANI v1.32 (https://github.com/ParBLiSS/FastANI) compared putative B. anthracis genomes against a comprehensive selection of assembled genomes from NCBI belonging to B. cereus sensu lato. Mapping against reference plasmids pXO1 NC_007322, pXO2 NC_007323 and pBC218 AAEK01000004 was performed in CLC genomics Workbench v20.0.2. The core genome MLST (cgMLST) analysis was performed in Ridom SeqSphere + v7.7.5 using the scheme described in [33].
Ethical statement
This retrospective observational case-series has been approved by the local ethical committee following the standards of the Swiss Human Research Act (EKNZ 2021-02112). Whenever possible written informed consent was collected, no patient refused participation.
3Results
3.1Clinical case features and routine identification of the isolates
A total of 16 isolates from 15 patients were evaluated. The clinical features of the 15 cases are listed in Table 1. Of the 16 isolates, six isolates were classified as clinically relevant, while 10 were classified as not relevant. Routine analysis using the MALDI-TOF MS sDB assigned 14 isolates to B. cereus and two to B. thuringiensis, with high scores (>2.0) (Table 2).
Table 2.
Bacillus species identification results by using VITEK®2 ID, MALDI-TOF MS, and WGS in all 16 isolates. Names of isolates identified genomically as B. anthracis are shown in bold. The isolate name identified as B. basilensis sp. nov. is shown in italics. ID, identification; DB, database; sDB, standard database; SR, security relevant; dDDH, digital DNA:DNA hybridization.
| Sample number | Date of collection | Specimen | VITEK®2 ID | Probability | MALDI-TOF MS ID standard sDB |
Score | MALDI-TOF MS ID standard sDB + SR DB |
Score | MALDI TOF MS Mabritec® PAPMIDTM BCG-classifier |
Species by genome and dDDH (TYGS) |
|---|---|---|---|---|---|---|---|---|---|---|
| 128633-19 | 15.07.19 | Blood | B. cereus/thuringiensis/mycoides | 99% | B. cereus | 2,44 | B. cereus | 2,44 | B. cereus | B. cereus |
| 607738-19 | 25.07.19 | Swab | B. cereus/thuringiensis/mycoides | 98% | B. cereus | 2,24 | B. anthracis | 2,46 | B. anthracis | B. anthracis |
| 130277-19 | 26.07.19 | Blood | B. cereus/thuringiensis/mycoides | 99% | B. cereus | 2,45 | B. cereus | 2,45 | B. cereus | B. cereus |
| 607730-19 | 26.07.19 | Biopsy | B. cereus/thuringiensis/mycoides | 98% | B. thuringiensis | 2,13 | B. thuringiensis | 2,13 | B. thuringiensis | B. thuringiensis |
| 130415-19 | 27.07.19 | Blood | B. cereus/thuringiensis/mycoides | 98% | B. cereus | 2,32 | B. cereus | 2,51 | B. cereus | B. cereus |
| 608121-20 | 21.08.20 | Swab | B. cereus/thuringiensis/mycoides | 92% | B. cereus | 2,20 | B. anthracis | 2,30 | B. anthracis | B. anthracis |
| 804229-21 | 21.07.21 | Swab | B. cereus/thuringiensis/mycoides | 98% | B. cereus | 2,27 | B. cereus | 2,27 | B. paranthracis | B. paranthracis |
| 607095-21 | 27.07.21 | Biopsy | B. cereus/thuringiensis/mycoides | 95% | B. cereus | 2,19 | B. anthracis | 2,36 | B. anthracis | B. anthracis |
| 203778-21 | 02.08.21 | Swab | B. cereus/thuringiensis/mycoides | 95% | B. cereus | 2,17 | B. anthracis | 2,22 | B. thuringiensis | B. thuringiensis |
| 402914-21 | 05.08.21 | Swab | B. cereus/thuringiensis/mycoides | 90% | B. cereus | 2,34 | B. cereus | 2,34 | B. paranthracis | B. paranthracis |
| 129606-21 | 10.08.21 | Blood | B. cereus/thuringiensis/mycoides | 95% | B. cereus | 2,28 | B. cereus | 2,28 | B. paranthracis | B. paranthracis |
| 607632-21 | 11.08.21 | Biopsy | B. cereus/thuringiensis/mycoides | 99% | B. cereus | 2,22 | B. anthracis | 2,40 | B. anthracis | B. anthracis |
| 403206-21 | 26.08.21 | Swab | B. cereus/thuringiensis/mycoides | 96% | B. cereus | 2,22 | B. anthracis | 2,37 | B. anthracis | B. anthracis |
| 403291-21 | 01.09.21 | Swab | B. cereus/thuringiensis/mycoides | 93% | B. cereus | 2,39 | B. cereus | 2,39 | B. paranthracis | B. paranthracis |
| 403507-21 | 16.09.21 | Swab | B. cereus/thuringiensis/mycoides | 92% | B. cereus | 2,22 | B. cereus | 2,22 | B. genomospecies13 | B. basilensis sp. nov. |
| 135455-21 | 20.09.21 | Blood | B. cereus/thuringiensis/mycoides | 89% | B. thuringiensis | 2,15 | B. thuringiensis | 2,15 | B. mobilis | B. mobilis |
3.1.1Whole genome sequencing and species identification
All 16 isolates underwent genome sequencing for further characterization (Table 3).
Table 3.
Genomic features of described Bacillus species. Names of isolates identified genomically as B. anthracis are shown in bold. The isolate name identified as B. basilensis sp. nov. is shown in italics. Plasmids could only be assigned where ONT sequencing was used, otherwise is given as unknown.
| Isolate | Illumina mean coverage | ONT mean coverage | Assembly size | #Contigs>1kb | #Circular plasmids | %G + C |
|---|---|---|---|---|---|---|
| 128633-19 | 69 | NA | 5380894 | 38 | unknown | 35.1 |
| 607738-19 | 54 | 341 | 5225393 | 1 | 0 | 35.4 |
| 130277-19 | 60 | NA | 5335057 | 48 | unknown | 35.1 |
| 607730-19 | 57 | NA | 5602605 | 42 | unknown | 34.9 |
| 130415-19 | 186 | NA | 6327063 | 228 | unknown | 34.7 |
| 608121-20 | 67 | 250 | 5714974 | 11 | 2 | 35.3 |
| 804229-21 | 101 | NA | 5497486 | 71 | unknown | 35.3 |
| 607095-21 | 102 | 245 | 5234004 | 1 | 0 | 35.4 |
| 203778-21 | 160 | NA | 5761105 | 57 | unknown | 34.9 |
| 402914-21 | 30 | NA | 5501750 | 107 | unknown | 35.1 |
| 129606-21 | 91 | NA | 5533689 | 72 | unknown | 35.1 |
| 607632-21 | 119 | 401 | 5258592 | 2 | 1 | 35.4 |
| 403206-21 | 204 | 63 | 5717356 | 8 | 6 | 35.3 |
| 403291-21 | 62 | NA | 5926503 | 91 | unknown | 34.9 |
| 403507-21 | 84 | 131 | 5785762 | 3 | 2 | 35.2 |
| 135455-21 | 59 | NA | 5649383 | 46 | unknown | 35.3 |
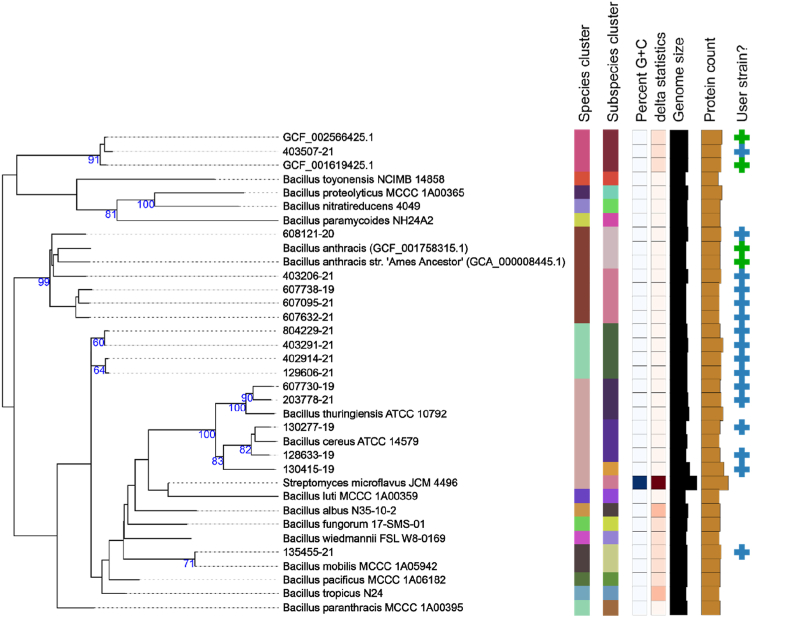
The genome assemblies were used to identify the isolates using several methods (Table 4). GTDB and TYGS give more species-level results, and agree more than the other methods, providing the striking finding that five genomes are defined as belonging to B. anthracis (Fig. 1). This species was not reported at all by 16S rRNA gene identification or rMLST. ANI comparisons for these genomes showed a majority of top hits (96-99.8%) to genomes assigned to B. anthracis (data not shown). However, none of the 16 genomes met the >90% target threshold of the B. anthracis cgMLST scheme. One isolate was not assigned to any existing species, being most closely related to genomes GCF_001619425.1 and GCF_002566425.1. We describe this as B. basilensis sp. nov.
Table 4.
Genomic identification of described Bacillus species. Names of isolates identified genomically as B. anthracis are shown in bold. The isolate name identified as B. basilensis sp. nov. is shown in italics. MLST was performed at https://pubmlst.org/organisms/bacillus-cereus, and rMLST at https://pubmlst.org/species-id. † Where the 16S rRNA gene was found at 14 copies per genome, with 2-6 SNPs between alleles, a representative version was used for the identification. ∗ GTDB warning: Genome has more than 10% of markers with multiple hits.
| Isolate | MLST | 16S rRNA gene identification: top hit(s) against NCBI rRNA database† | rMLST | GTDB | Species by TYGS, with additional genomes |
|---|---|---|---|---|---|
| 128633-19 | 2593 | 1534bp; 100% match to Bacillus cereus NR_115714.1 | B. cereus (50%)/B. thuringiensis (50%) | B. cereus | B. cereus |
| 607738-19 | 75 | 1550bp; 99.74% match to Bacillus fungorum NR_170494.1 | Bacillus (100%) | B. anthracis∗ | B. anthracis |
| 130277-19 | 177 | 1515bp; 100% match to Bacillus cereus NR_074540.1, Bacillus cereus NR_115714.1 | Bacillus (100%) | B. cereus | B. cereus |
| 607730-19 | 2742 | 1550bp; 99.87% match to Bacillus toyonensis NR_121761.1 | B. cereus (50%)/B. thuringiensis (50%) | B. thuringiensis | B. thuringiensis |
| 130415-19 | 8 | 1520bp; 99.87% match to Bacillus fungorum NR_170494.1 | Bacillus (100%) | B. bombysepticus | B. cereus |
| 608121-20 | 62 | 1550bp; 99.74% match to Bacillus fungorum NR_170494.1 | Bacillus (100%) | B. anthracis∗ | B. anthracis |
| 804229-21 | 26 | 1349bp; 100% match to Bacillus tropicus NR_157736.1, Bacillus nitratireducens NR_157732.1, Bacillus luti NR_157730.1, Bacillus albus NR_157729.1 | Bacillus paranthracis (100%) | B. paranthracis∗ | B. paranthracis |
| 607095-21 | 108 | 1550bp; 99.74% match to Bacillus fungorum NR_170494.1 | B. cereus (100%) | B. anthracis | B. anthracis |
| 203778-21 | new combination: 41,6,12,9,4,114,15 | 1550bp; 99.94% match to Bacillus toyonensis NR_121761.1 | Bacillus (100%) | B. thuringiensis | B. paranthracis |
| 402914-21 | 144 | 1538bp; 99.93% match to Bacillus cereus NR_115714.1 | B. cereus (100%) | B. paranthracis∗ | B. paranthracis |
| 129606-21 | 144 | 1302bp; 99.92% match to Bacillus cereus NR_115714.1 | B. cereus (100%) | B. paranthracis∗ | B. paranthracis |
| 607632-21 | 62 | 1550bp; 99.74% match to Bacillus fungorum NR_170494.1 | Bacillus (100%) | B. anthracis∗ | B. anthracis |
| 403206-21 | 1050 | 1550bp; 99.74% match to Bacillus fungorum NR_170494.1 | Bacillus (100%) | B. anthracis | B. anthracis |
| 403291-21 | 26 | 1509bp; 99.93% match to Bacillus cereus NR_115714.1 | Bacillus (100%) | B. paranthracis∗ | B. paranthracis |
| 403507-21 | partial: not all loci found | 1550bp; 99.81% match to Bacillus fungorum NR_170494.1 | B. cereus (100%) | B. thuringiensis | No matching species (B. basilensis sp. nov.) |
| 135455-21 | 784 | 1550bp; 99.94% match to Bacillus toyonensis NR_121761.1 | B. mobilis (100%) | B. mobilis | B. mobilis |
Fig. 1.
TYGS GBDP tree showing relationships between isolates and references. Figure was generated by TYGS [30], with genomes sequenced in our hospital (blue + in “User genomes” column), and additional genomes added for context (green +): GCA_000008445.1 and GCF_001758315.1 [19] to reflect B. anthracis which is otherwise absent from the TYGS database, GCF_001619425.1 and GCF_002566425.1 to represent members of B. basilensis sp. nov.. Species clusters are defined by dDDH with a 70% cutoff. Isolates 607738-19, 608121-20, 607095-21, 607632-21 and 403206-21 can be seen to belong to the species B. anthracis, using this standard cut-off (Table 4).
None of the isolates were found to contain complete plasmids pXO1, pXO2, or alternative capsule-carrying plasmid pBC218, with all isolates mapping to only 5-53% of these references. None were found to contain anthrax toxins nor capsule genes cya, lef, pagA or capABCDE. All genomes carry the bla1 class A beta-lactamase gene (A7J11_01054 or A7J11_05168) at >90% identity. With the exception of isolate 403507-21 B. basilensis sp. nov., all isolates carry bla2 BcII family beta-lactamase (A7J11_00039, A7J11_05308 or A7J11_05161) at >91% identity, although this gene was disrupted in isolate 608121-20. These genes can lead to penicillin resistance when expression levels are high [34].
These results provide evidence that five isolates are most closely related to B. anthracis, which was not seen from the routine microbiology. Given these discrepant results, and the lack of expert consensus on species identification, further identification methods were performed.
3.2Identification based on phenotype
All 16 isolates showed the classical morphological characteristics of B. cereus: grey, matt colonies exhibiting large double-zone β-hemolysis. A representative example is shown in Supplemental material Fig. 1. Using the VITEK®2 phenotypic test, all isolates were assigned to B. cereus/thuringiensis/mycoides with an identification probability ranging from 89% to 99%, which is the highest level of resolution provided by VITEK®2 BCL card (manufacturer's information) (Table 2). For the four key reactions identified, no isolate showed a similar profile to the reference B. anthracis, and all isolates showed a positive tyrosine arylamidase reaction (Supplemental material Table 3 for key reactions and Supplemental material Table 4 for more detailed reaction profiles). AST showed that all isolates were resistant to penicillin, but susceptible to clindamycin and vancomycin, and susceptible to increased exposure with levofloxacin (Supplemental material Table 5).
3.3Identification based on MALDI-TOF MS and virulence specific real-time PCR
Through re-measuring the MALDI-TOF MS spectra of the isolates and using the SR DB, we assigned six isolates to B. anthracis with high scores (Table 2). Using the Mabritec® PAPMID™ BCG-Classifier database, five isolates were identified as B. anthracis without pXO1 and pXO2, four as B. paranthracis, three as B. cereus, two as B. thuringiensis, one as B. mobilis and one as a previously undescribed “genomospecies 13” described here as B. basilensis sp. nov. (Table 2). B. anthracis specific real-time PCRs were performed on all 16 isolates. All were negative for pXO1, pXO2, and gyrA, this latter likely due to a C-T mutation in the assay probe binding site in the B. anthracis isolates (Supplementary material Fig. 2).
4Discussion
Isolate identification within the B. cereus-group is challenging. Of the various phenotypic and genotypic approaches used in this study to characterize the 16 isolates, we consider genomic analysis by TYGS with appropriate additional comparators to provide the most accurate species assignation. The TYGS results were in agreement with those from Mabritec® PAPMID™ BCG-Classifier database in all cases, and assigned five isolates to B. anthracis, albeit without virulence plasmids, four isolates to B. paranthracis, three to B. cereus, two to B. thuringiensis, one to B. mobilis, and one isolate was identified as a new species, B. basilensis sp. nov. This shows the species diversity that can be hidden behind a generic diagnosis of “B. cereus-group”.
Illustrating the lack of species distinction in morphological and phenotypic tests, all our isolates showed morphology and AST patterns typical for B. cereus. The biochemical reaction profile of all our isolates was consistent with B. cereus/thuringiensis/mycoides, showing that the VITEK®2 BCL card offered no additional diagnostic support. Only 5/16 (31.3%) isolates were correctly identified at the species level using routine microbiological methods. Of note, B. paranthracis and B. mobilis cannot be identified by VITEK®2 BCL card.
The original definition of B. anthracis was tightly linked to the presence of the anthrax toxin, making the definition of B. anthracis particularly problematic. Many remain convinced that only tightly related, monomorphic, toxin-carrying strains qualify for the name [18,33]. By dDDH analysis, using the 70% cutoff, the species can be more broadly defined, including non-toxin carrying strains, and those described here [3,19]. B. anthracis is absent from the TYGS database, as no type strain genome sequence exists, which complicates identification, and shows that these tools must be used with caution. B. anthracis exists in the rMLST database, but the isolates presented here are sufficiently divergent not to be recognized as B. anthracis by this method.
Of the isolates, 6/16 were defined as clinically relevant, of which three were identified as B. anthracis. Illumina-based WGS offers high resolution identification, but a turn-around time of several days is too slow to generate an impact in clinical management. Using the MALDI-TOF MS sDB, only 4/16 (25%) isolates were correctly identified. This is expected, since B. anthracis, B. paranthracis and B. mobilis are not in the database, and it is known that commercial standard databases do not reliably differentiate species within the B. cereus-group [15]. Even using the SR DB, only 9/16 (56,3%) isolates were correctly identified, including five correctly identified B. anthracis, but also one falsely identified as B. anthracis. Alternative methods including real-time nanopore sequencing technologies or improved MALDI-TOF MS databases would be valuable additions in these cases. The Mabritec® PAPMID™ database, an online accessible (www.mabriteccentral.com) proprietary database which supports Bruker Biotyper and VITEK® MS bioMérieux data files, is based on in silico predicted ribosomal marker peaks und uses the PAPMID™ algorithm for classification. A sophisticated sample preparation, including the use of sinapinic acid as matrix, was used and all our isolates were correctly identified to species level. The BCG-classifier used is based on deduced reference marker masses from 2204 public B. cereus-group genomes, covering 20 accepted species and 21 genomospecies.
Further improvements to MALDI-TOF MS analyses include identifying specific B. anthracis biomarker candidates [15], using software such as ClinProTools (Bruker) and Matlab (The Mathworks Inc.), combined with different packages for use in R [14,35], using different matrices [35], and direct detection of anthrax toxin component, the lethal factor [36]. Comprehensive databases can increase the probability of confirmed identification up to 93% [37]. However, these methods need to be evaluated for use in routine diagnostics.
The implications of species mis-identification need to be considered. Defining genomic ancestry does not help in assessment of virulence potential, which is of most clinical and biowarfare agent concern. To address this, suggestions have been made for a new taxonomic nomenclature for the B. cereus-group that takes into account phenotypic and genomic characteristics, defining a biovar concept [18] or using BTyper [38]. Anthrax is a notifiable disease: it remains to be clarified whether a non-virulent isolate belonging to B. anthracis requires urgent notification.
Using standard genomic methods of species identification, we have shown that isolates belonging to B. anthracis are frequently found in the clinical routine laboratory, albeit non-toxin-carrying isolates representing more diverse members of the species. We find that routine morphological, phenotypic, and standard MALDI-TOF MS methods are insufficient for accurate species identification within the B. cereus-group, and additional methods should be applied in difficult cases.
4.1Taxonomic description of Bacillus basilensis sp. nov.
A Gram-positive, rod-shaped bacillus (403507-21) was isolated from human superficial skin swab. On the basis of MALDI-TOF MS identification, the isolate was assigned to the Bacillus cereus-group. 16S rRNA gene sequence (accession number: OV062800) analysis shows over 99.8% nucleotide identity to isolates belonging to species Bacillus proteolyticus, Bacillus wiedmannii, B. cereus sensu stricto, Bacillus fungorum, Bacillus tropicus, Bacillus nitratireducens, Bacillus luti and Bacillus albus. Physiological characterization revealed the following traits for the isolate: growth at 37°C under aerobic conditions. The biochemical characteristics of the isolate as determined by VITEK®2 BCL card revealed the following positive reactions: ellman, L-pyrrolidonyl-arylamidase, D-glucose, esculin-hydrolyse, N-acetyl-D-glucosamin, pyruvat, D-ribose, alanin-arylamidase, phenylalanine-arylamidase, tyrosine-arylamidase, glycin-arylamidase, beta-N-acetyl-glucosaminidase. The results of digital DNA–DNA hybridization with a 70% cutoff, performed on the genome assembly, allowed genotypic differentiation of strain 403507-21 from the validly published Bacillus species and show that it falls within the Bacillus cereus-group. Strain 403507-21 therefore represents a new species, for which the name B. basilensis (Etymology: ba.sil.en'sis. L. masc./fem. adj. basilensis, pertaining to Basilea, the Roman name of Basel, Switzerland, where the type strain was isolated) is proposed, with the type strain 403507-21 (DSM 113537, CCUG 75930T).
CRediT authorship contribution statement
Veronika Muigg: Conceptualization, Investigation, Data curation, Formal analysis, Writing – original draft. Aline Cuénod: Investigation, Data curation, Writing – review & editing. Srinithi Purushothaman: Investigation, Data curation, Writing – review & editing. Martin Siegemund: Investigation, Writing – review & editing. Matthias Wittwer: Investigation, Data curation, Writing – review & editing. Valentin Pflüger: Investigation, Data curation, Writing – review & editing. Kristina M. Schmidt: Investigation, Data curation, Writing – review & editing. Maja Weisser: Investigation, Writing – review & editing. Nicole Ritz: Investigation, Writing – review & editing. Andreas Widmer: Investigation, Writing – review & editing. Daniel Goldenberger: Data curation, Writing – review & editing. Vladimira Hinic: Data curation, Writing – review & editing. Tim Roloff: Data curation, Writing – review & editing. Kirstine K. Søgaard: Data curation, Writing – review & editing. Adrian Egli: Conceptualization, Supervision, Writing – review & editing. Helena M.B. Seth-Smith: Conceptualization, Supervision, Data curation, Formal analysis, Visualization, Writing – review & editing.
Acknowledgements
We thank Prof. Mark Pallen, Quadram Institute, England, for help with species naming. We thank Doris Hohler, Magdalena Schneider, Clarisse Straub, Elisabeth Schultheiss, Rosa-Maria Vesco, Christine Kiessling, Daniel Gander, Valerie Courtet and Vincent Hartmann (University Hospital Basel) for excellent technical assistance with strain collection and sequencing. We thank Roxanne Mouchet and Samuel Lüdin (Mabritec®) for excellent technical assistance with MALDI-TOF MS. Assemblies and calculations were performed at sciCORE (http://scicore.unibas.ch) scientific computing facility at the University of Basel.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.nmni.2022.101040.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Bhandari V., Ahmod N.Z., Shah H.N., Gupta R.S. Molecular signatures for Bacillus species: demarcation of the Bacillus subtilis and Bacillus cereus clades in molecular terms and proposal to limit the placement of new species into the genus Bacillus. Int J Syst Evol Microbiol. 2013;63(Pt 7):2712–2726. doi: 10.1099/ijs.0.048488-0. [DOI] [PubMed] [Google Scholar]
- 2.Gupta R.S., Patel S., Saini N., Chen S. Erratum: robust demarcation of seventeen distinct Bacillus species clades, proposed as novel Bacillaceae genera, by phylogenomics and comparative genomic analyses: description of Robertmurraya kyonggiensis sp. nov. and proposal for emended genus Bacillus limiting it only to the members of the subtilis and cereus clades of species. Int J Syst Evol Microbiol. 2020;70(12):6531–6533. doi: 10.1099/ijsem.0.004613. [DOI] [PubMed] [Google Scholar]
- 3.Liu Y., Lai Q., Göker M., Meier-Kolthoff J.P., Wang M., Sun Y., et al. Genomic insights into the taxonomic status of the Bacillus cereus group. Scientific Rep. 2015;5(1) doi: 10.1038/srep14082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carroll K., Pfaller M., Landry M., McAdam A., Patel R., Richter S. 12th ed. ASM Press; 2019. Manual of clinical microbiology; pp. 456–476. [Google Scholar]
- 5.Ehling-Schulz M., Lereclus D., Koehler T.M. The Bacillus cereus group: Bacillus species with pathogenic potential. Microbiol Spectr. 2019;7(3) doi: 10.1128/microbiolspec.gpp3-0032-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Okinaka R., Cloud K., Hampton O., Hoffmaster A., Hill K., Keim P., et al. Sequence, assembly and analysis of pX01 and pX02. J Appl Microbiol. 1999;87(2):261–262. doi: 10.1046/j.1365-2672.1999.00883.x. [DOI] [PubMed] [Google Scholar]
- 7.Bottone E.J. Bacillus cereus, a volatile human pathogen. Clin Microbiol Rev. 2010;23(2):382–398. doi: 10.1128/CMR.00073-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Swartz M.N. Recognition and management of anthrax--an update. N Engl J Med. 2001;345(22):1621–1626. doi: 10.1056/NEJMra012892. [DOI] [PubMed] [Google Scholar]
- 9.Anthrax W.H.O. 4th ed. 2008. Humans and animals. [Google Scholar]
- 10.Carroll L.M., Cheng R.A., Wiedmann M., Kovac J. Keeping up with the Bacillus cereus group: taxonomy through the genomics era and beyond. Crit Rev Food Sci Nutr. 2021:1–26. doi: 10.1080/10408398.2021.1916735. [DOI] [PubMed] [Google Scholar]
- 11.https://www.fda.gov/food/laboratory-methods-food/bam-chapter-14-bacillus-cereus fda.gov. BAM Chapter 14: Bacillus cereus 2021 [Available from:
- 12.Halket G., Dinsdale A.E., Logan N.A. Evaluation of the VITEK2 BCL card for identification of Bacillus species and other aerobic endosporeformers. Lett Appl Microbiol. 2010;50(1):120–126. doi: 10.1111/j.1472-765X.2009.02765.x. [DOI] [PubMed] [Google Scholar]
- 13.Ash C., Farrow J.A., Dorsch M., Stackebrandt E., Collins M.D. Comparative analysis of Bacillus anthracis, Bacillus cereus, and related species on the basis of reverse transcriptase sequencing of 16S rRNA. Int J Syst Bacteriol. 1991;41(3):343–346. doi: 10.1099/00207713-41-3-343. [DOI] [PubMed] [Google Scholar]
- 14.Manzulli V., Rondinone V., Buchicchio A., Serrecchia L., Cipolletta D., Fasanella A., et al. Discrimination of Bacillus cereus group members by MALDI-TOF mass spectrometry. Microorganisms. 2021;9(6) doi: 10.3390/microorganisms9061202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pauker V.I., Thoma B.R., Grass G., Bleichert P., Hanczaruk M., Zöller L., et al. Improved discrimination of Bacillus anthracis from closely related species in the Bacillus cereus sensu lato group based on matrix-assisted laser desorption ionization-time of flight mass spectrometry. J Clin Microbiol. 2018;56(5) doi: 10.1128/JCM.01900-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wielinga P.R., Hamidjaja R.A., Agren J., Knutsson R., Segerman B., Fricker M., et al. A multiplex real-time PCR for identifying and differentiating B. anthracis virulent types. Int J Food Microbiol. 2011;145(Suppl. 1):S137–S144. doi: 10.1016/j.ijfoodmicro.2010.07.039. [DOI] [PubMed] [Google Scholar]
- 17.Parks D.H., Chuvochina M., Chaumeil P.A., Rinke C., Mussig A.J., Hugenholtz P. A complete domain-to-species taxonomy for Bacteria and Archaea. Nat Biotechnol. 2020;38(9):1079–1086. doi: 10.1038/s41587-020-0501-8. [DOI] [PubMed] [Google Scholar]
- 18.Carroll L.M., Wiedmann M., Kovac J. Proposal of a taxonomic nomenclature for the Bacillus cereus group which reconciles genomic definitions of bacterial species with clinical and industrial phenotypes. mBio. 2020;11(1) doi: 10.1128/mBio.00034-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Banerjee A., Somani V.K., Chakraborty P., Bhatnagar R., Varshney R.K., Echeverría-Vega A., et al. Molecular and genomic characterization of PFAB2: a non-virulent Bacillus anthracis strain isolated from an Indian hot spring. Curr Genomics. 2019;20(7):491–507. doi: 10.2174/1389202920666191203121610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Turnbull P.C., Hutson R.A., Ward M.J., Jones M.N., Quinn C.P., Finnie N.J., et al. Bacillus anthracis but not always anthrax. J Appl Bacteriol. 1992;72(1):21–28. doi: 10.1111/j.1365-2672.1992.tb04876.x. [DOI] [PubMed] [Google Scholar]
- 21.Okinaka R., Pearson T., Keim P. Anthrax, but not Bacillus anthracis? PLoS Pathog. 2006;2(11):e122. doi: 10.1371/journal.ppat.0020122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rothen J., Sapugahawatte D.N., Li C., Lo N., Vogel G., Foucault F., et al. A simple, rapid typing method for Streptococcus agalactiae based on ribosomal subunit proteins by MALDI-TOF MS. Sci Rep. 2020;10(1):8788. doi: 10.1038/s41598-020-65707-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kassim A., Pflüger V., Premji Z., Daubenberger C., Revathi G. Comparison of biomarker based Matrix Assisted Laser Desorption Ionization-Time of Flight Mass Spectrometry (MALDI-TOF MS) and conventional methods in the identification of clinically relevant bacteria and yeast. BMC Microbiol. 2017;17(1):128. doi: 10.1186/s12866-017-1037-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.bioMérieux. VITEK® 2 BCL card. bioMérieux; 2019. version 045519-02, REF 21345. [Google Scholar]
- 25.(CLSI) CLSI . 2015. Methods for antimicrobial dilution and disk susceptibility testing of infrequently isolated or fastidious bacteria. [Google Scholar]
- 26.EUCAST, EUCAST . 2021. EUCAST clinical breakpoints. [Google Scholar]
- 27.Hurtle W., Bode E., Kulesh D.A., Kaplan R.S., Garrison J., Bridge D., et al. Detection of the Bacillus anthracis gyrA gene by using a minor groove binder probe. J Clin Microbiol. 2004;42(1):179–185. doi: 10.1128/JCM.42.1.179-185.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wick R.R., Judd L.M., Gorrie C.L., Holt K.E. Unicycler: resolving bacterial genome assemblies from short and long sequencing reads. PLOS Computational Biol. 2017;13(6) doi: 10.1371/journal.pcbi.1005595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Seemann T. Prokka: rapid prokaryotic genome annotation. Bioinformatics. 2014;30(14):2068–2069. doi: 10.1093/bioinformatics/btu153. [DOI] [PubMed] [Google Scholar]
- 30.Meier-Kolthoff J.P., Göker M. TYGS is an automated high-throughput platform for state-of-the-art genome-based taxonomy. Nat Commun. 2019;10(1):2182. doi: 10.1038/s41467-019-10210-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Feldgarden M., Brover V., Haft D.H., Prasad A.B., Slotta D.J., Tolstoy I., et al. Validating the AMRFinder tool and resistance gene database by using antimicrobial resistance genotype-phenotype correlations in a collection of isolates. Antimicrob Agents Chemother. 2019;63(11) doi: 10.1128/AAC.00483-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen L., Zheng D., Liu B., Yang J., Jin Q. VFDB 2016: hierarchical and refined dataset for big data analysis--10 years on. Nucleic Acids Res. 2016;44(D1):D694–D697. doi: 10.1093/nar/gkv1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Abdel-Glil M.Y., Chiaverini A., Garofolo G., Fasanella A., Parisi A., Harmsen D., et al. A whole-genome-based gene-by-gene typing System for standardized high-resolution strain typing of Bacillus anthracis. J Clin Microbiol. 2021;59(7) doi: 10.1128/JCM.02889-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen Y., Tenover F.C., Koehler T.M. Beta-lactamase gene expression in a penicillin-resistant Bacillus anthracis strain. Antimicrob Agents Chemother. 2004;48(12):4873–4877. doi: 10.1128/AAC.48.12.4873-4877.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Karger A. Current developments to use linear MALDI-TOF spectra for the identification and typing of bacteria and the characterization of other cells/organisms related to infectious diseases. Proteomics Clin Appl. 2016;10(9–10):982–993. doi: 10.1002/prca.201600038. [DOI] [PubMed] [Google Scholar]
- 36.Gallegos-Candela M., Boyer A.E., Woolfitt A.R., Brumlow J., Lins R.C., Quinn C.P., et al. Validated MALDI-TOF-MS method for anthrax lethal factor provides early diagnosis and evaluation of therapeutics. Anal Biochem. 2018;543:97–107. doi: 10.1016/j.ab.2017.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lasch P., Wahab T., Weil S., Pályi B., Tomaso H., Zange S., et al. Identification of highly pathogenic microorganisms by matrix-assisted laser desorption ionization-time of flight mass spectrometry: results of an interlaboratory ring trial. J Clin Microbiol. 2015;53(8):2632–2640. doi: 10.1128/JCM.00813-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Carroll L.M., Kovac J., Miller R.A., Wiedmann M. Rapid, high-throughput identification of anthrax-causing and emetic Bacillus cereus group genome assemblies via BTyper, a computational tool for virulence-based classification of Bacillus cereus group isolates by using nucleotide sequencing data. Appl Environ Microbiol. 2017;83(17) doi: 10.1128/AEM.01096-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.