Abstract
Objective: To observe the effect of gasless endoscopic thyroidectomy through an axillary approach (GETAN) on the recurrent laryngeal nerve in patients with thyroid cancer. Methods: One hundred and ten patients with thyroid cancer admitted to the department of general surgery, the First Affiliated Hospital of Xiamen University were retrospectively selected as the research subjects. They were divided into an observation group (OG, 55 patients, treated with GETAN) and a control group (CG, 55 patients, treated with conventional radical resection for papillary thyroid cancer). Clinical indicators, pain degree, negative emotions, recurrent laryngeal nerve injury, vocal and swallowing function, and the incidence of complications were compared between the two groups. Results: In terms of clinical indicators, the operation time, intraoperative blood loss, extubation time, and hospitalization time in the OG were shorter than those of the CG (all P<0.05). The scores of Visual Analogue Scale (VAS) at one, two, and three days after surgery in the OG were lower than those in the CG (all P<0.001). As for the negative emotions, the Self-Rating Anxiety Scale score, and Self-Rating Depression Scale score in the OG were lower than those in the CG (both P<0.001). The incidence of postoperative recurrent laryngeal nerve injury in the OG was lower than that of the CG (P<0.001). Another analysis showed that GETAN was a protective factor against recurrent laryngeal nerve injury in patients with thyroid cancer (P<0.05). The Voice Handicap Index and Swallowing impairment score one week and one month after surgery were lower in the OG than in the CG (all P<0.001). The incidence of postoperative complications such as hypocalcemia, wound infection, and numbness of hands and feet in the OG was lower than that in the CG (all P<0.001). Conclusion: The GETAN approach is able to relieve postoperative pain, anxiety, and depression; reduce the laryngeal recurrent nerve injury; promote the recovery of laryngeal recurrent nerve; and decrease the incidence of vocal and swallowing dysfunction It is worthy of clinical promotion.
Keywords: Gasless endoscopy through axillary approach, radical resection of thyroid cancer, thyroid cancer, recurrent laryngeal nerve
Introduction
Thyroid cancer is one of the common endocrine malignant tumors. Its incidence ranks at the forefront among cancers and shows an increasing trend year by year [1-3]. Statistics show the number of new cases of thyroid cancer in China has exceeded 200,000. This cancer is easy to metastasize and has a high mortality, seriously affecting the life quality of patients [4]. Currently, surgery is the main and final treatment option for thyroid cancer [3,5]. Clinically, differentiated thyroid cancer, as the most common type, is mostly “indolent cancer”, with low malignancy and good surgical prognosis. Conventional open thyroid surgery is the most used surgery for thyroid cancer in clinical practice and has a certain clinical efficacy. This surgery has drawbacks such as postoperative complications and aesthetic concern [6,7]. The active exploration of effective radical thyroid surgery methods with fewer complications have gradually become a hot spot. In recent years, endoscopic radical resection of thyroid cancer has become popular because of its advantages such as cosmetic effect. Surgeries with various endoscopic approaches have emerged [8]. The commonly used endoscopic approaches in clinics are natural lumen approach, areola approach, and axillary approach. CO2 filling is required by the above approaches. It forms a closed environment of endoscopic surgery and creates a better vision of surgical fields [9]. The filling process of CO2 can cause side effects such as gas embolism, mediastinal emphysema, and even increased intracranial pressure [9]. Gasless endoscopic thyroidectomy through an axillary approach (GETAN) is a modified transaxillary approach, characterized by the absence of CO2. As a new endoscopic surgical method for the treatment of thyroid cancer, there are few reports on its clinical efficacy and its impact on postoperative recurrent laryngeal nerve injury [10]. This study investigated the effect of GETAN on the recurrent laryngeal nerve injury in patients with thyroid cancer, to provide evidence for clinical treatment.
Materials and methods
General information
In this retrospective study, 110 patients with thyroid cancer treated in the department of general surgery, the First Affiliated Hospital of Xiamen University from January 2019 to June 2020 were included. They were divided into an observation group (OG, 55 patients, treated with GETAN) and a control group (CG, 55 patients, treated with conventional radical resection for papillary thyroid cancer). This study was approved by the Ethics Committee of the First Affiliated Hospital of Xiamen University.
Inclusion criteria
1) Patients who met the diagnostic criteria of thyroid cancer; 2) Patients with single-nodule thyroid cancer that was diagnosed by pathology and imaging examination; 3) Patients with lesion diameter ≤1 cm; 4) Patients with no distant metastasis in preoperative examinations; 5) Patients with surgical indications of GETAN [11].
Exclusion criteria
1) Patients with severe heart, lung, liver, kidney, or brain dysfunctions; 2) Patients with tuberculosis or hematological diseases; 3) Patients with a history of head or neck surgery; 4) Patients with preoperative hoarseness, vocal cord lesions, or swallowing dysfunction; 5) Patients with incomplete follow-up data; 6) Patients with inability to cooperate because of mental illness.
Methods
Surgical methods
The CG was treated with conventional radical resection [12] for papillary thyroid cancer. The patient lay supine on his/her back and was intubated after anesthesia. A 5-6 cm wound was cut along the horizontal neck wrinkle at 2 cm above the sternoclavicular joint. The subcutaneous tissues were cut layer by layer to fully expose the thyroid lobe. After complete resection of the thyroid tumor, a frozen pathological examination was performed right away. For patients with papillary thyroid carcinoma, thyroid lobectomy, isthmus resection, and central lymph node, dissections were performed on the affected side of the thyroid. The drainage tube was placed, and the wound was sutured.
The OG was treated with GETAN [13]. The patient laid supine on his/her back. Patients’ shoulders were slightly raised with their head skewed to the healthy side The affected limb was in 90-degree abduction. The patient was intubated after anesthesia. A 3 cm incision was created at the natural fold between the anterior axillary line and the midaxillary line of the affected side. The tissues were subcutaneously separated until the surface of the pectoralis major muscle. A 5 mm trocar was placed below the incision approximately 2-3 cm from the breast edge. A separation was carried out along the surface of the pectoralis major muscle toward the thyroid. A retractor was used to assist in the process of separation. After separation, an endoscopic lens was placed into the target area. The deep surface of platysma muscle was separated with the aid of an electric knife or ultrasonic knife. One third of the sternocleidomastoid muscle was separated. After separation between the sternal head and the clavicular head, a non-inflatable thyroid retractor was placed into this space, and the sternal head was pulled up. The sternothyroid muscle and omohyoid muscle were exposed. With the help of the endoscope, the thyroid lobe on the affected side was exposed. The thyroid capsule was separated. The peripheral blood vessels were dissociated. The recurrent laryngeal nerve and parathyroid gland were probed and protected. The thyroid lobe and isthmus were resected completely. The pathological tissue was frozen quickly. A pathological examination confirmed papillary thyroid carcinoma. The central lymph node dissection was performed, and the wound was sutured.
Outcome measures
The operation time, intraoperative blood loss, extubation time, and hospitalization time were recorded. The clinical indicators of the two groups were reflected by the above four indexes.
The Visual Analogue Scale (VAS) was used to evaluate the pain degree of the two groups. The VAS score ranged from 0 to 10 points. Higher scores indicated greater pain [14].
The Self-Rating Anxiety Scale (SAS) and Self-Rating Depression Scale (SDS) were used to evaluate the negative emotions of the two groups. SDS was assessed in 4 dimensions using a 4-point scale, including psychotic affective symptoms (2 items), somatic disorders (8 items), psychomotor disorders (2 items), and depressed psychological disorders (8 items). SAS was used to assess the frequency of the anxiety symptoms using a 4-point scale containing 20 items. Both scales have a total score of 100 points. Higher scores indicated more serious negative emotions [15].
The degree of recurrent laryngeal nerve injury was evaluated. The vocal and swallowing function of the two groups were compared using the Voice Handicap Index (VHI) and Swallowing Impairment Score (SIS) [12]. The VHI and SIS scores ranged from 0 to 4 points. A score ≥1 point (s) indicated dysphagia. VHI assessed the influence of voice abnormality on quality of life in three dimensions: physical, functional, and emotional. The patients were asked about the frequency of certain feelings: 0 point for never, 1 point for occasionally, 2 points for sometimes, 3 points for almost always, and 4 points for always. The subjects were explained about the content based on their educational level and asked to answer the questions based on the actual situation [12]. SIS was evaluated by observing the required time for drinking 30mL of warm water when the patient sat up, and whether they coughed during drinking. The results were scored between 0 and 4 as follows: 0 point if they finished drinking 30 mL water at once, 1 point if they finished the drinking in two times but without coughing, 2 points if they finished the drinking at once but with coughing, 3 points if they finished the drinking in two or more times and with coughing, and 4 points if they were not able to finish drinking and there was frequent coughing.
The incidence of postoperative complications, such as hypocalcemia, wound infection, and numbness of hands and feet in the two groups were observed. Total incidence of complications (%) = cases with complications/total number of cases *100%.
Statistical methods
Statistical software SPSS 26.0 was used for statistical analysis. The measured data were expressed as (x̅ ± sd). The inter-group and intra-group comparisons of measured data were carried out by the paired t-test and independent sample t test. The enumeration data were expressed as n (%). The inter-group and intra-group comparisons of enumeration data were carried out by the χ2 test. The scores of VAS at different time points were tested for homogeneity of variance by repeated measures ANOVA. Pairwise comparison was performed by post hoc Bonferroni. P<0.05 was considered statistically significant.
Results
Comparison of general information
The OG included 24 males and 31 females, with an average age of 41.3±7.3 years, an average course of disease of 3.43±1.47 years, and an average body mass index (BMI) of 24.98±1.39 kg/m2. There were 28 cases with a lesion in the left and 27 cases in the right in the OG, with an average tumor diameter of 0.74±0.16 cm. The CG included 22 males and 33 females, with an average age of 40.9±7.2 years, an average course of disease of 3.14±1.25 years, and an average BMI of 24.98±1.39 kg/m2. There were 32 cases with a lesion in the left and 23 cases in the right in the CG, with an average tumor diameter of 0.72±0.13 cm. There was no obvious difference in age, course of disease, BMI, tumor location, or tumor diameter between the two groups. See Table 1.
Table 1.
Comparison of general information between the two groups (x̅ ± sd)
| Index | Observation group | Control group | t | P | |
|---|---|---|---|---|---|
| Case (n) | 55 | 55 | |||
| Age (year) | 41.6±7.3 | 40.9±7.2 | 7.164 | 0.259 | |
| Male: female | 24:31 | 22:33 | 0.149 | 0.699 | |
| Course of disease (year) | 3.43±1.47 | 3.14±1.25 | 2.351 | 0.194 | |
| BMI (kg/m2) | 24.52±1.33 | 24.98±1.39 | 1.773 | 0.079 | |
| Tumor location | Left | 28 | 32 | 9.783 | 9.783 |
| Right | 27 | 23 | |||
| Tumor diameter (cm) | 0.74±0.16 | 0.72±0.13 | 7.302 | 0.129 | |
Note: BMI: Body Mass Index.
Comparison of clinical indicators
Significant differences were found in clinical indicators (operation time, intraoperative blood loss, extubation time, and hospitalization time) between the two groups (all P<0.05). See Table 2.
Table 2.
Comparison of clinical indicators between the two groups (x̅ ± sd)
| Index | Observation group | Control group | t | P |
|---|---|---|---|---|
| Case (n) | 55 | 55 | ||
| Operation time (min) | 108.95±10.34 | 119.15±10.49 | 11.240 | <0.001 |
| Intraoperative blood loss (mL) | 21.37±6.51 | 28.76±5.98 | 9.573 | 0.010 |
| Extubation time (d) | 3.59±0.74 | 4.43±0.88 | 13.392 | <0.001 |
| Hospitalization time (d) | 5.12±0.68 | 7.52±0.79 | 6.570 | <0.001 |
Comparison of pain degree
There was no significant difference in the preoperative VAS scores between the two groups. The VAS scores one day, two days, and three days after operation in the OG were lower than those in the CG (all P<0.001). See Figure 1.
Figure 1.
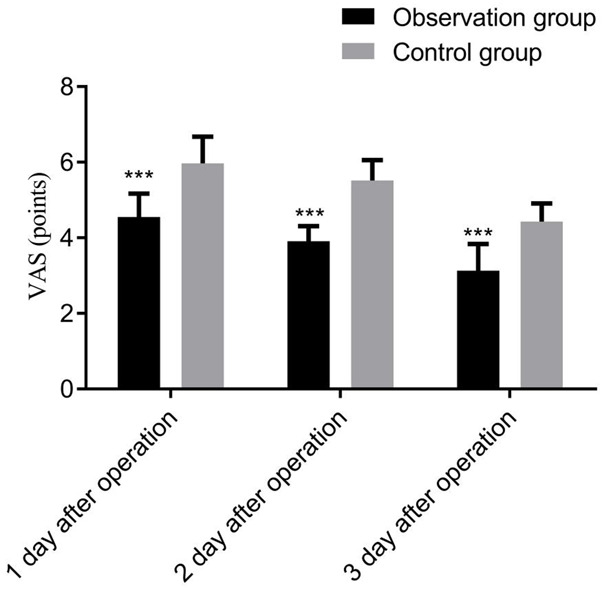
Comparison of pain degree between the two groups. Compared with control group at the same time, ***P<0.001. VAS: Visual Analogue Scale.
Comparison of negative emotions
There was no significant difference in the preoperative SDS and SAS scores between the two groups. The postoperative SDS score and SAS score in the OG were lower than those in the CG (all P<0.001). See Table 3.
Table 3.
Comparison of negative emotions between the two groups (score, x̅ ± sd)
| Index | Observation group | Control group | t | P | |
|---|---|---|---|---|---|
| Case (n) | 55 | 55 | |||
| SDS score | Before treatment | 59.80±4.57 | 60.71±5.62 | 0.829 | 0.481 |
| After treatment | 39.25±5.00 | 45.68±4.47 | 7.280 | <0.001 | |
| SAS score | Before treatment | 61.45±4.23 | 61.79±3.91 | 0.751 | 0.562 |
| After treatment | 44.16±4.02 | 54.28±3.89 | 7.994 | <0.001 | |
Note: SDS: Self-Rating Depression Scale. SAS: Self-Rating Anxiety Scale.
Comparison of recurrent laryngeal nerve injury
After treatment, there were 2 cases of temporary recurrent laryngeal nerve injury (3.64%) and 1 case of permanent recurrent laryngeal nerve injury (1.82%) in the OG. Among them, 2 cases (3.64%) were with unilateral injury and 1 (1.82%) with bilateral injury. In the CG, there were 12 cases of temporary recurrent laryngeal nerve injury (21.82%) and 7 cases of permanent recurrent laryngeal nerve injury (12.73%). Among them, unilateral injury was found in 14 cases (25.45%) and bilateral injury in 5 case (9.09%). The incidence of recurrent laryngeal nerve injury in the OG was lower than that in the CG (P<0.001). See Table 4.
Table 4.
Comparison of recurrent laryngeal nerve injury between the two groups [n (%)]
| Index | Observation group | Control group | χ2 | P | |
|---|---|---|---|---|---|
| Case (n) | 55 | 55 | |||
| Recurrent laryngeal nerve injury | Temporary recurrent laryngeal nerve injury | 2 (3.64) | 12 (21.82) | 7.682 | <0.001 |
| Permanent recurrent laryngeal nerve injury | 1 (1.82) | 7 (12.73) | 2.914 | <0.001 | |
| Unilateral injury | 2 (3.64) | 14 (25.45) | 17.260 | <0.001 | |
| Bilateral injury | 1 (1.82) | 5 (9.09) | 21.993 | <0.001 | |
Analysis of related factors of recurrent laryngeal nerve injury
There were 22 cases of postoperative recurrent laryngeal nerve injury in the 110 patients with thyroid cancer. The univariate analysis showed that the tumor diameter, the extubation time, and the hospitalization time in the patients with recurrent laryngeal nerve injury were longer than those in patients without nerve injury (all P<0.05). The proportion of patients undergoing radical resection for papillary thyroid cancer was higher in the group with recurrent laryngeal nerve injury than that in the group without. See Table 5.
Table 5.
Analysis of related factors of recurrent laryngeal nerve injury
| Group | recurrent laryngeal nerve injury group | Non-recurrent laryngeal nerve injury group | t | P | |
|---|---|---|---|---|---|
| Case (n) | 22 | 88 | |||
| Age (year) | 42.1±7.9 | 39.7±7.1 | 1.386 | 0.168 | |
| Male: female | 9:13 | 37:51 | 0.009 | 0.932 | |
| Course of disease (year) | 3.52±1.52 | 3.11±1.22 | 1.341 | 0.183 | |
| BMI (kg/m2) | 25.02±1.42 | 24.62±1.33 | 1.245 | 0.215 | |
| Tumor Location | Left | 14 | 46 | 0.917 | 0.338 |
| Right | 8 | 42 | |||
| Tumor diameter (cm) | 0.70±0.12 | 2.238 | 0.027 | ||
| Surgical Methods | Radical resection | 19 | 33 | 14.758 | <0.001 |
| GETAN | 3 | 49 | |||
| Operation time (min) | 116.23±10.42 | 113.22±10.54 | 1.201 | 0.232 | |
| Intraoperative blood loss (mL) | 26.83±5.72 | 24.72±6.21 | 1.447 | 0.158 | |
| Extubation time (d) | 4.23±0.83 | 3.82±0.81 | 2.112 | 0.037 | |
| Hospitalization time (d) | 7.22±0.73 | 6.72±0.74 | 2.842 | 0.005 | |
Note: GETAN: Gasless Endoscopic Thyroidectomy Through an Axillary Approach.
Multivariate logistic regression analysis of factors associated with recurrent laryngeal nerve injury
Multivariate Logistic regression analysis showed that GETAN was a protective factor against recurrent laryngeal nerve injury in patients with thyroid cancer (P<0.05). See Table 6.
Table 6.
Multivariate Logistic regression analysis of factors associated with recurrent laryngeal nerve injury
| Factors | β | SE | Wald | OR (95% CI) | P |
|---|---|---|---|---|---|
| Tumor diameter (cm) | 0.892 | 0.723 | 1.053 | 2.212 (0.599-9.931) | 0.323 |
| Surgical methods | -1.923 | 0.745 | 7.636 | 0.721 (0.467-0.821) | 0.033 |
| Extubation time (d) | 0.182 | 0.734 | 0.092 | 0.876 (0.285-2.925) | 0.643 |
| Hospitalization time (d) | 0.945 | 0.719 | 1.028 | 2.032 (0.682-8.923) | 0.291 |
Comparison of vocal and swallowing dysfunction
The incidences of vocal and swallowing dysfunction in the OG were noticeably lower than those in the CG one week and one month after operation (all P<0.001). See Table 7.
Table 7.
Comparison of vocal and swallowing dysfunction between the two groups [n (%)]
| Index | Observation group | Control group | χ2 | P | |
|---|---|---|---|---|---|
| Case (n) | 55 | 55 | |||
| One week after Operation | Vocal dysfunction | 1 (1.82) | 8 (14.55) | 1.190 | <0.001 |
| Swallowing dysfunction | 1 (1.82) | 6 (10.91) | 4.654 | <0.001 | |
| One month after Operation | Vocal dysfunction | 0 (0.00) | 2 (3.64) | 0.982 | <0.001 |
| Swallowing dysfunction | 0 (0.00) | 1 (1.82) | 1.270 | <0.001 | |
Comparison of postoperative complications
The incidences of postoperative complications, like hypocalcemia, wound infection, and numbness of hands and feet in the OG were considerably lower than those in the CG (all P<0.001). See Table 8.
Table 8.
Comparison of postoperative complications between the two groups [n (%)]
| Index | Observation group | Control group | χ2 | P |
|---|---|---|---|---|
| Case (n) | 55 | 55 | ||
| Hypocalcemia | 1 (1.82) | 5 (9.09) | 21.054 | <0.001 |
| Wound infection | 1 (1.82) | 4 (7.27) | 18.212 | <0.001 |
| Numbness in hands and feet | 0 (0.00) | 1 (1.82) | 23.870 | <0.001 |
| Total incidence | 2 (3.64) | 10 (18.18) | 24.901 | <0.001 |
Discussion
Thyroid cancer has a high clinical incidence and poor prognosis. Surgery is currently the main treatment for thyroid cancer. It has been found that recurrent laryngeal nerve injury is a major complication of conventional open thyroid surgery [16]. The injury of the recurrent laryngeal nerve can easily affect patients’ vocal and swallowing function, resulting in a series of complications like hoarseness and dysphagia. This seriously impacts patients’ life quality and prognosis [17]. GETAN has the advantages of small incision and good aesthetic effect. It is highly accepted by patients in clinical practice. Due to the difficulty of the operation, this surgical technique is in the stage of clinical exploration [18,19].
The operation time, intraoperative blood loss, extubation time, and hospitalization time are of great value in evaluating the surgical effects. The results of this study showed that the operation time, intraoperative blood loss, extubation time, and hospitalization time of the patients in the OG were lower than those in the CG. This suggested that the therapeutic effect and safety of GETAN were better than those of conventional open thyroid surgery. This was consistent with the results of Zheng et al. [20].
The VAS score was an important index for clinical determination of pain degree [21]. The results of this study showed the VAS scores of patients in the OG were lower than those in the CG at one, two, and three days after treatment. This indicated that patients who underwent GETAN suffered less pain than patients who underwent conventional open thyroid surgery. This was like the results of Zhang et al. [22].
Anxiety and depression are common negative emotions in patients after thyroid cancer surgery. SDS score and SAS score are important evaluation indicators of negative emotions in patients. The SDS and SAS scores are inversely proportional to the patient’s mental health [23]. In this study, the SDS and SAS scores of patients in the OG were lower than those in the CG. This indicated that patients who underwent GETAN had less postoperative negative emotions than patients who underwent conventional open thyroid surgery.
As for the postoperative recurrent laryngeal nerve injury, its incidence in the OG was lower than that in the CG. Multivariate logistic regression analysis showed that GETAN was a protective factor against recurrent laryngeal nerve injury in patients with thyroid cancer. It indicated that GETAN had a more protective effect on recurrent laryngeal nerve injury than conventional open thyroid surgery. It can reduce the incidence of postoperative recurrent laryngeal nerve injury. This study adopted the operation strategy of “one point, two surfaces, and three lines”. “One point” referred to the breakthrough point which was the starting point of inferior thyroid artery posterior to the cervical sheath. From this point, we tried to find the prevertebral prefascial space layer (surface one), which was used as the operative surface to separate the esophagus and the dorsal thyroid gland to the anterior tracheal space (surface two). The transition from the prevertebral prefascial space to the anterior tracheal space followed the “three lines”, the recurrent laryngeal nerve, the inferior thyroid artery, and the esophagus and thyroid space. After separation, the thyroid and lymph node tissues in the central region were excised. The lymph nodes in the region VII were thoroughly dissected by the traction of thyroid and lymph node tissues. This method thoroughly cleaned the lymph nodes in the central region, and was beneficial to the functional protection of the parathyroid gland and recurrent laryngeal nerve. This was a surgical method worthy of clinical promotion. In clinical practice, the recurrent laryngeal nerve injury can often affect the vocal and swallowing function, resulting in voice disorders and dysphagia. This study found that the incidences of vocal and swallowing dysfunction in the OG one week and one month after the operation were lower than those in the CG. This indicated that patients who underwent GETAN had better vocal and swallowing function and better quality of life than those who underwent conventional open thyroid surgery. This agreed with a previous research conclusion [24].
Hypocalcemia, wound infection, and numbness of hands and feet are common postoperative complications of thyroid cancer, which seriously affect the prognosis of patients. Studies showed that the incidence of transient hypocalcemia after thyroid cancer surgery was 6.9%-49.0%, and the incidence of permanent hypocalcemia was 3.0% [6,7]. Wound infection and numbness of hands and feet reflected the prognosis of patients after the operation. In this study, the total incidence of postoperative complications in the OG was lower than that in the CG. This suggested that GETAN resulted in fewer postoperative complications than conventional open thyroid surgery and led to better prognosis. This was consistent with the previous research results [25].
This study had some limitations, such as limited sample size and the retrospective research design, which can cause certain bias in the results. In the future, we will verify the results of this study through a multi-center study with a larger sample size or a prospective study, aiming to discover more evidence on GETAN for the treatment of thyroid cancer.
To conclude, GETAN had an obvious therapeutic effect in patients with thyroid cancer. This approach can relieve pain, anxiety, and depression; reduce the incidence of recurrent laryngeal nerve injury; and decrease the incidence of vocal and swallowing disorders and complications such as hypocalcemia, wound infection, and numbness of hands and feet, showing a clear curative effect. It is worthy of clinical application.
Disclosure of conflict of interest
None.
References
- 1.Fan J, Lu Y, Zhao G, Li S, Li M, Kong J, Wang T. Mutation characteristics of BRAF V600E, NRAS, TERT genes in papillary thyroid carcinoma and their correlation with clinicopathological characteristics. Mod Oncol. 2021;29:769–773. [Google Scholar]
- 2.Li W, Zhou J, Dong J, Ma Z, Wu M, Miao W, Luo P, Han R. The prevalence of thyroid cancer in Jiangsu province in 2015 and the trend analysis from 2006 to 2015. J Pract Oncol. 2021;35:1. [Google Scholar]
- 3.Xu Z, Ma X. Establishment of a nomogram model for predicting the risk of recurrence in patients with thyroid cancer. J Pract Oncol. 2021;35:35–40. [Google Scholar]
- 4.Sun K, Zheng R, Zhang S, Zeng H, Zou X, Chen R, Gu X, Wei W, Hao J. Report of cancer epidemiology in China, 2015. Chin J Oncol. 2019;41:19–28. doi: 10.3760/cma.j.issn.0253-3766.2019.01.005. [DOI] [PubMed] [Google Scholar]
- 5.Li X, Yidiresi A, Tian Y, Zhang L, Luo J. Clinical analysis of risk factors of early hypocalcemia after total thyroidectomy. Chin J Oper Proced Gen Surg (Electronic Ed) 2021;15:77–79. [Google Scholar]
- 6.Del Rio P, Rossini M, Montana CM, Viani L, Pedrazzi G, Loderer T, Cozzani F. Postoperative hypocalcemia: analysis of factors influencing early hypocalcemia development following thyroid surgery. BMC Surg. 2019;18:25. doi: 10.1186/s12893-019-0483-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eismontas V, Slepavicius A, Janusonis V, Zeromskas P, Beisa V, Strupas K, Dambrauskas Z, Gulbinas A, Martinkenas A. Predictors of postoperative hypocalcemia occurring after a total thyroidectomy: results of prospective multicenter study. BMC Surg. 2018;18:55. doi: 10.1186/s12893-018-0387-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yuan Z, Peng S. Comparison of curative effect between full areola approach laparoscopic surgery and traditional open surgery for the treatment of differentiated thyroid cancer. Chin J Mod Oper Surg. 2020;24:261–266. [Google Scholar]
- 9.Furushima K, Funakoshi T, Kusano H, Miyamoto A, Takahashi T, Horiuchi Y, Itoh Y. Endoscopic-assisted transaxillary approach for first rib resection in thoracic outlet syndrome. Arthrosc Sports Med Rehabil. 2021;3:e155–e162. doi: 10.1016/j.asmr.2020.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wen L, Xiang Y, Shen Z, Wang L. Effect observation and nursing of non-pneumatic transaxillary approach and transthoracic approach in the treatment of thyroid disease. J Pract Med. 2019;37:1727–1731. [Google Scholar]
- 11.Chinese Medical Association Endocrinology Branch, Chinese Medical Association Surgery Branch and Chinese Anti-Cancer Association Head and Neck Tumor Professional Committee Branch. Guidelines for the diagnosis and treatment of thyroid nodules and differentiated thyroid cancer. Chin J Clin Oncol. 2012;39:1249–1271. [Google Scholar]
- 12.Zhang Z, Liu X, Wang Z, Huang J, Zhang N. Effect of total areola endoscopic thyroidectomy on the recurrent laryngeal nerve in patients with thyroid cancer. J Xinxiang Med Univ. 2020;37:743–746. [Google Scholar]
- 13.Jantharapattana K, Leelasawatsuk P. Transaxillary endoscopic thyroid lobectomy: gas insufflation versus gasless technique. Eur Arch Otorhinolaryngol. 2020;277:2049–2054. doi: 10.1007/s00405-020-05908-w. [DOI] [PubMed] [Google Scholar]
- 14.Dahlstrand U, Sandblom G, Nordin P, Wollert S, Gunnarsson U. Chronic pain after femoral hernia repair: a cross-sectional study. Ann Surg. 2011;254:1017–1021. doi: 10.1097/SLA.0b013e31822ba9b6. [DOI] [PubMed] [Google Scholar]
- 15.Sun W, Xu J, Yang M, Ding X. Effects of comprehensive audio-visual training combined with cognitive behavioral intervention on negative emotion and cognitive function in middle-aged patients with breast cancer during. Chin J Health Psychol. 2021 [Google Scholar]
- 16.Liu S, Li P. Postoperative impact of thyroid surgery through zuckerkandl tubercle positioning of recurrent laryngeal nerve and parathyroid gland on patients with thyroid cancer. Med J Chin PLA. 2020;32:10–13. [Google Scholar]
- 17.Pei M, Chen W, Hu M. Study progress of intraoperative neuro-monitoring of recurrent laryngeal nerve in thyroidectomy. Chin J Otorhinolaryngol Head Neck Surg. 2018;53:474–478. doi: 10.3760/cma.j.issn.1673-0860.2018.06.021. [DOI] [PubMed] [Google Scholar]
- 18.Moran K, Grigorian A, Elfenbein D, Schubl S, Jutric Z, Lekawa M, Nahmias J. Energy vessel sealant devices are associated with decreased risk of neck hematoma after thyroid surgery. Updates Surg. 2020;72:1135–1141. doi: 10.1007/s13304-020-00776-9. [DOI] [PubMed] [Google Scholar]
- 19.Minuto MN, Reina S, Monti E, Ansaldo GL, Varaldo E. Morbidity following thyroid surgery: acceptable rates and how to manage complicated patients. J Endocrinol Invest. 2019;42:1291–1297. doi: 10.1007/s40618-019-01064-z. [DOI] [PubMed] [Google Scholar]
- 20.Zheng C, Mao X, Wang J, Tan Z, Ge M. Preliminary evaluation of effect of endoscopic thyroidectomy using the gasless unilateral axillary approach. Chin J Clin Oncol. 2018;45:27–32. [Google Scholar]
- 21.Shen G, Li C, Zhu H, Zeng J. Safety of dexmedetomidine hydrochloride in combined spinal and epidural anesthesia for knee arthroscopic surgery and the influence of vas and Ramsay scores. Contemp Med. 2020;26:11–14. [Google Scholar]
- 22.Zhang S, Zhang P, Guo S, Lian J, Chen Y, Chen A, Ma Y, Li F. Comparative study of three types of lymphadenectomy along the left recurrent laryngeal nerve by minimally invasive esophagectomy. Thorac Cancer. 2020;11:224–231. doi: 10.1111/1759-7714.13210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li X, Zhong K, Zhang Y. Study on the value of humanistic care on SAS and SDS scores in malignant tumor nursing. Smart Healthc. 2020;6:138–140. [Google Scholar]
- 24.Patel KN, Yip L, Lubitz CC, Grubbs EG, Miller BS, Shen W, Angelos P, Chen H, Doherty GM, Fahey TJ 3rd, Kebebew E, Livolsi VA, Perrier ND, Sipos JA, Sosa JA, Steward D, Tufano RP, McHenry CR, Carty SE. Executive summary of the American association of endocrine surgeons guidelines for the definitive surgical management of thyroid disease in adults. Ann Surg. 2020;271:399–410. doi: 10.1097/SLA.0000000000003735. [DOI] [PubMed] [Google Scholar]
- 25.Chen WS, Zhu LH, Li WJ, Tu PJ, Huang JY, You PL, Pan XJ. Novel technique for lymphadenectomy along left recurrent laryngeal nerve during thoracoscopic esophagectomy. World J Gastroenterol. 2020;26:1340–1351. doi: 10.3748/wjg.v26.i12.1340. [DOI] [PMC free article] [PubMed] [Google Scholar]


