Abstract
The most common inherited eye disease is retinitis pigmentosa (RP). X-linked RP (XLRP) is one of the most severe types of RP, with a considerable disease burden. Patients with XLRP experience a decrease in their vision and become blind in their 4th decade of life, causing much morbidity after starting a rather normal life. Treatment of XLRP remains challenging, and current treatments are not effective enough in restoring vision. Gene therapy of XLRP, capable of restoring the functional RPGR gene, showed promising results in preclinical studies and clinical trials; however, to date, no approved product has entered the market. The development of a gene therapy product needs through preliminary assessment of the drug in animal models before administration to humans. In this article, we reviewed the genetic pathology of XLRP, along with the preclinical aspects of the XLRP gene therapy, animal models, associated assessments, and future challenges and directions.
Keywords: Adeno-associated virus, Gene therapy, Retinitis pigmentosa, Retinitis pigmentosa GTPase regulator (RPGR)
Key Summary Points
| X-linked retinitis pigmentosa is one of the most severe types of hereditary eye disease. |
| Gene therapy opens a new horizon in treating hereditary eye diseases like Leber congenital amaurosis and X-linked retinitis pigmentosa. |
| There have been several preclinical and clinical trials but no approved drugs yet. |
| Selection of a proper gene therapy strategy, including vector type, animal model, and assessments, is vital for developing an effective gene therapy product. |
| In this article, the preclinical aspects of X-linked retinitis pigmentosa gene therapy and its current challenges have been reviewed. |
Introduction
Retinitis pigmentosa (RP) is the most common inherited eye disease, affecting 1 in 4000 worldwide (approximately 3 million worldwide) [1]. As is understandable from its name, underlying pathology consists of degeneration of the retinal cells and accumulation of retinal pigments, giving the retina a pigmented appearance. RP includes a heterogeneous group of inherited diseases that, along with other conditions, such as Leber congenital amaurosis (LCA), Usher syndrome, and Bardet-Biedl syndrome, cause retinal degeneration [1]. The disease can have different inheritance patterns, including autosomal dominant, autosomal recessive, X-linked recessive, and syndromic (as a part of syndromes), each of which occurs with different prevalence, pathology, intensity, and prognosis based on their underlying mutation [1–4]. The most common type of RP is the autosomal recessive type, which accounts for about 50–60% of RP prevalence, followed by the autosomal dominant type (30–40%) and X-linked type (5–20%) [2, 3]. Despite the differences, the RP disease group has several common clinical features [2]. In these patients, at first, with the loss of rod photoreceptors, which are often located in the peripheral retina and responsible for low-light sight, the person suffers from night vision problems (night blindness) and loss of peripheral visual field (tunnel vision). Next, the cone cells, which are responsible for color vision and accurate vision, begin to degenerate, causing the loss of central vision; eventually, most patients become legally blind. These changes present as a progressive reduction of the ERG response of rod and cone cells. In addition to previous symptoms are destruction of retinal vessels, accumulation of abnormal dark bone-like pigments in the retina, vitreous degeneration, and paleness of the optic nerve head [1, 5, 6].
Unfortunately, no definitive and effective treatment for RP has been suggested so far. Available therapies for RP, at their best, have just been able to delay retinal degeneration by reducing retinal cell death, improving retinal cell function, replacing cells, or creating an artificial retina [7]. Calcium blockers, fibroblast growth factor (FGF), and ciliary neurotrophic factor (CTNF) are examples of pharmacological agents that try to alter the environment of the photoreceptors to prevent the loss of rod cells [8–12]. Dietary supplements such as vitamins A, E, and docosahexaenoic acid (DHA) were also used to treat RP [13–15]. Transplantation of healthy photoreceptor and RPE (retinal pigment epithelium) cells or embryonic stem cells was used for the regeneration of degenerated neurons; however, there are still immunological challenges [1, 16–18]. However, in recent years, especially after the successful results of gene therapy for LCA disease (NCT00821340, NCT00481546, NCT00749957, NCT02781480, NCT01496040, NCT00643747, NCT04516369, NCT00999609), choroideremia (NCT03496012), and X-linked RP (Table 1) and approval of Luxturna (voretigene neparvovec) by FDA and EMA in 2017 [19–21], hopes are rising for the application of gene therapy in the treatment of RP [22, 23].
Table 1.
Summary of clinical trials for RPGR-related X-linked retinitis pigmentosa (XLRP)
| NCT number | Intervention/observation | Design | Number of participants | Start/finish year | Clinical centre(s) | Sponsor |
|---|---|---|---|---|---|---|
| NCT03116113 | Subretinal delivery of AAV8-hRKcoRPGRORF15 (BIIB112) | A multicentre, open-label dose escalation (phase 1) and dose expansion (phase 2/3) clinical trial (XIRIUS Trial) | Phase 1: 18 participants/phase 2: 63 participants | March 2017/November 2020 | Oxford, Manchester, Southampton, UK, Florida, Oregon, Pennsylvania, USA | Nightstar Therapeutics (now Biogen Inc), UK |
| NCT03252847 | Subretinal delivery of AAV2/5-hRKRPGRORF15 | An open-label, multicentre, phase I/II dose escalation trial | 36 participants | July 2017/November 2021 (no reports yet) | London, UK | MeiraGTx, UK |
| NCT03316560 | Subretinal delivery of rAAV2tYFGRK1- coRPGRORF15 | A non-randomized, open-label, phase 1/2 dose escalation study, with a phase 2 randomized, controlled, masked dose expansion study | Phase 1/2: 30 participants/phase 2: 12 participants | April 2018/August 2026 | Colorado, Massachusetts, New York, North Carolina, Ohio, Oregon, Pennsylvania, Texas, USA | Applied Genetic Technologies Corp. (AGTC), USA |
| NCT04850118 | rAAV2tYF-GRK1-hRPGRco (AGTC-501) | A phase 2/3, randomized, controlled, masked, multicentre study | 63 participants | August 2021/March 2029 | Applied Genetic Technologies Corp. | Applied Genetic Technologies Corp. |
| NCT04671433 | AAV5-RPGR | Phase 3 randomized, controlled study | 66 participants | March 2021/July 2022 | California, Florida, Georgia, Massachusetts, Michigan, Texas, USA | MeiraGTx UK II Ltd, Janssen Research & Development, LLC |
| NCT04517149 | 4D-125 | An open-label, phase 1/2 trial | 43 participants | June 2020/May 2029 | Colorado, Florida, Michigan, North Carolina, Oregon, Texas, Utah, USA | 4D Molecular Therapeutics |
| NCT04794101 | AAV5-RPGR | Follow-up phase 3 randomized, controlled study | 66 participants | March 2021/July 2027 | California, Florida, Georgia, Massachusetts, Michigan, Texas, USA | MeiraGTx UK II Ltd, Janssen Research & Development, LLC |
| NCT04312672 | AAV2-RPGR | Follow-up study of an open-label, multicentre, phase I/II dose escalation trial | 36 participants | February 2019/June 2023 | London, UK | MeiraGTx UK II Ltd |
| NCT03584165 | Subretinal delivery of AAV8-hRKcoRPGRORF15 (BIIB112) | A long-term follow-up phase 3 study | 440 participants | June 2018/March 2027 | Multiple centres in the UK, the Netherlands, Germany, France, Finland, Denmark, Canada, USA | NightstaRx Ltd, a Biogen Company |
| NCT03349242 | Prospective natural history study of XLRP | Observational study | 250 participants | December 2017/December 2023 | Massachusetts, Michigan, USA | MeiraGTx, UK |
| NCT03314207 | Prospective natural history study of XLRP caused by RPGR-ORF15 mutations | Observational study | 45 participants | December 2017/December 2021 | New York, North Carolina, Ohio, Oregon, Texas, USA | Applied Genetic Technologies Corp. (AGTC), USA |
X-linked type of RP (X-linked retinitis pigmentosa: XLRP), which is reported with considerable prevalence and severe manifestations, has been studied for gene therapy treatment; fortunately, promising developments in this area have been reported in recent years [4, 24–26]. In this study, we intended to review the characteristics of the XLRP and the basic principles of its preclinical gene therapy along with the current challenges and future perspectives, emphasizing laboratory and preclinical aspects. Note that this review is based on previously conducted studies and does not contain any new studies with human participants or animals.
X-Linked Retinitis Pigmentosa, a Common and Severe Type of RP
XLRP is one of the most severe types of RP, known for its early onset and rapid progression. So far, several gene loci have been suggested for it including RP2 [MIM 312600], RP3 [MIM 312610], RP6 [MIM 31262], RP23 [MIM 300424], RP24 [MIM 300155], and RP34 [MIM 300605]. However, mutations in the two main genes of RP2 and RP3 or retinitis pigmentosa GTPase regulator (RPGR) have been studied more than others [2]. Mutations in the RP2 gene are responsible for about 15% of XLRP cases, probably by truncating a protein responsible for transporting proteins to the cell surface and maintaining the structure of the Golgi apparatus. However, this gene has been less targeted for gene therapy [27, 28]. Mutations in the RPGR gene account for about 70% of XLRP cases and are the most common mutations in the recessive type of RP. The disease is not transmitted from person to person; however, female carriers show different degrees of disease severity, from no symptoms to severe degeneration (male pattern) [2, 29, 30]. People with mutations in the RPGR gene usually experience night blindness in the first decade of their lives. Their visual acuity and visual field continue to decline, and as rod and cone cells continue to die, most become blind in the 4th decade of life. Optical coherence tomography (OCT) of these patients shows progressive thinning of the outer layers of the retina [31, 32].
Genetic Pathology
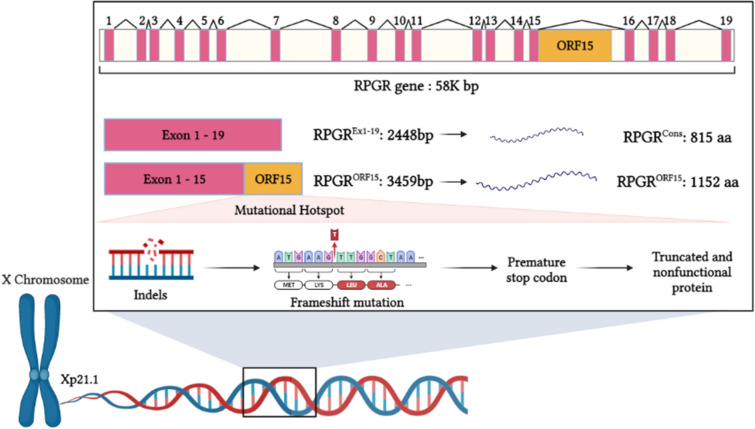
RPGR gene, located in the Xp21.1 region, has a length of 58 kb and is composed of 19 exons. During transcription, ten types of RPGR mRNA are created after intron splicing and five are translated into proteins. Two common types of these mRNAs are RPGREx1−19, containing 19 exons with a length of 2448 bp, which makes a protein with 815 amino acids, and RPGRORF15, including the first 14 exons followed by the 15th exon elongating into the 15th intron with a length of 3459 bp, which encodes a protein with 1152 amino acids. RPGR naturally has two main isoforms in the human body: (1) RPGRconst, which contains all of the 19 exons and is expressed in all tissues across the body, and (2) RPGRORF15, which has 15 exons and the last exon (15th), is continued by the intron next to it and is explicitly expressed in photoreceptor cells [33]. The role of the protein produced by the RPGR gene is not well known. Still, it has been determined that this protein is located in the structure of the connecting cilium of photoreceptors at the junction of the inner part (consisting of the organelles which produce the cell’s necessary proteins and fatty acids) and the outer part (consisting of superimposed disks of the photoreceptor cell membrane which enclosed by the RPE cells and is responsible for the retinoid cycle that leads to vision) of these cells. RPGR protein is involved in the intra-flagellar transportation of proteins. [34, 35]. To date, no disease-causing mutations have been reported in the 16th to 19th exons. However, the final exon of this RPGRORF15, called ORF15, which actually consists of the 15th exon and part of the 15th intron of the RPGR gene, is a mutational hotspot in which > 70% of the RPGR mutations occur. The reason for these mutations is the purine-rich repetitive sequences that can cause abnormal conformations in DNA double helix or triplexes that inhibit the polymerase enzyme and subsequently transcription and translation processes [33, 36]. In addition, repetitive glycine and glutamic acid sequences play an essential role in the isoelectric balance of the resulting protein and hence have a decisive role in the normal function of the rod and cone cells of the retina [37]. Most of the mutations that occur in this region are small deletions of 1–2 or 4–5 bp that cause a frameshift and eventually truncate the protein product. This could cause RPGR protein breakdown and nonfunctioning through changes in the protein isoelectric point or post-translational glutamylation [33, 38, 39]. However, it has been reported that deletions without frameshift (indels), if small, not only are well tolerated but also can increase the genome's stability [40]. A noteworthy point in this regard is the inability of the RPGREx1−19 splice variant to compensate for the RPGR dysfunction caused by the mutant RPGRORF15 splice variant. It seems that the RPGREx1−19 isoform, contrary to RPGRORF15, has trivial expression in the retina [41, 42]. (Fig. 1).
Fig. 1.
Schematic diagram of retinitis pigmentosa GTPase regulator (RPGR) gene structure, splicing variants, and genetic pathogenesis of XLRP
It should be noted that currently, the RP diagnosis is based on clinical features, and then the patient is referred for genetic evaluation of known underlying mutations [20]. Further identification of responsible underlying genes through genetic testing of diagnosed patients and their registration in worldwide databases (Leiden Open Variation Database: www.databases.lovd.nl; RetNet: www.sph.uth.edu; eyeGENE network: www.eyegene.nih.gov) could expand the ground for gene therapy of this disease [43–46].
Animal Models of XLRP Disease
One of the main requirements for studies on the safety and efficacy of RPGR gene therapy, along with a good design and proper selection of viral vectors, is having a suitable animal model for this disease that can successfully simulate the features and behaviours of the disease in humans. Since a wide range of retinal degenerative diseases can occur in humans and other mammals, having representative animal models can help find the pathology and possible treatments of these diseases. Notably, many of the genes that lead to retinal degeneration in animals are common to human pathogenic genes; therefore, these models could be considered accurately, both genetically and phenotypically, the proper model for corresponding human diseases. Animal models for RP and specifically for XLRP exist in two forms: first, the models that naturally have mutations in the RPGR gene; second, the engineered models, in which the RPGR gene is manipulated, creating a transgenic model of XLRP [1]. It is important to note that animal models of disease, in addition to being genotypically and phenotypically comparable, should also be similar in anatomical and physical characteristics. Dogs, mice, rats, cats, chickens, and pigs are among the animals that have either natural or transgenic models for RP. Among them, dogs due to similarity in eye size, pigs due to acceptable size of the eyes and similarities in retinal structure, and cats due to much information available about their retinal neurophysiology and lower level of inflammation secondary to interventions in their eyes have advantages. However, most of the animal models are mice. Mice, with a relatively short lifespan, allow the observation of long-term changes of disease in a relatively shorter time. Compared with mice, rats with almost equal reproduction speed possess better-known photoreceptors and larger eyes, simplifying the evaluation and procedures used [1]. However, there are currently three animal models with natural mutations, including two canine models, i.e., XLPRA1 and XLPRA2 models [47] and a murine model, i.e., rd9 (retinal degeneration 9) mouse model [48], and several models with genetic manipulation for XLRP disease [49].
XLPRA1 canine model of RPGR has a mutation in ORF15 through deletion of five nucleotides (del1028-1032), which makes a premature stop codon and subsequently a truncated protein at the 230th amino acid starting from the C-terminal. The result is the degeneration of retinal photoreceptor cells. The retina of XLPRA1 dogs develops and functions normally at birth. The first histological symptoms (rod cell degeneration) appear at 11 months of age, followed by cone cell degeneration. The first functional symptoms (decrease in amplitude of dark-adapted response of rod and cone cells) appear after 6 months [47]. XLPRA2 canine model, which seems to be a more severe and faster type of XLPRA1, is identified by two-nucleotide deletion (del1084-1085) in the ORF15 exon, which causes frameshift mutation in this gene. The result is 34 extra altered basic amino acids and truncation of the last 161 amino acids in the protein structure. These extra amino acids alter the isoelectric point of the protein and disrupt its function. Degeneration of retinal rod cells of this model follows a biphasic pattern, starting at 4 weeks and reaching a maximum in 6–7 weeks. The rate of cell death decreases afterward and remains constant for at least 9 months. Functional disorders in the form of amplitude reduction and abnormal waveforms in ERG curves start at 5–6 weeks and become more severe with age progression. These two models can be a good representative of XLRP occurring in the 1st decade of human life [47]. Mouse model rd9 in C57Bl6/J mice was caused by mutations in the exon ORF15 through duplication of 32 nucleotides, resulting in a frameshift mutation and causing a premature stop codon and loss of functional protein and gradual loss of photoreceptors. Due to RPGR protein deficiency, rhodopsin and transducin levels in the outer part of the rod cells were decreased, and the opsin in the cone cells was misplaced. In retinal morphological tests, the thickness of the outer nuclear layer decreases, and the pigments are diminished. Retinal functionality of these mice—evaluated by ERG—gradually decreased to 24 months [50, 51].
Other models of the XLRP disease are also developed by genetic manipulation, the most important of which is the RPGR−/− mouse model. This murine model has been created by introducing a vector bearing a transgene truncated at the 4–6th exon into embryonic stem cells. In this murine model, due to early truncation, no functional RPGR protein is generated. Also, these mice do not have any RPGR protein in the connecting cilia area of photoreceptors. However, ERG data show that the retina is morphologically normal until the 30th day of birth, cone cell pigments (opsin) undergo mislocalization from the 20th day of birth, and, instead of being normally on the outside part of the photoreceptors, they move inward and around the nucleus. Although rod cell pigments (rhodopsin) are not affected by mislocalization, their amount decreases. Retinal degeneration—characterized by high expression of GFAP—starts at 2 months of age and becomes more severe at 6 months. At this time, the length of the photoreceptors’ outer part is reduced, and the disc-shaped structure of the photoreceptors’ tail is disrupted. Retinal degenerative changes appear in the forms of the reduced amplitude of b waves in cone cells and a reduction in the slope of the ERG curve of rod cells [49].
Due to similarities in anatomy and sizes of the eyes, diagnostic and therapeutic interventions for the canine models are largely the same as those used for humans. The pattern of photoreceptor loss (first rods, then cones) in canine models is similar to that in humans. However, in addition to the many genetic similarities between mice and humans, the maintenance and reproduction of murine models are more manageable, and surgical interventions are simpler in mice. Hence, choosing the appropriate animal model according to the purpose of the study is crucial.
Gene Therapy Vectors
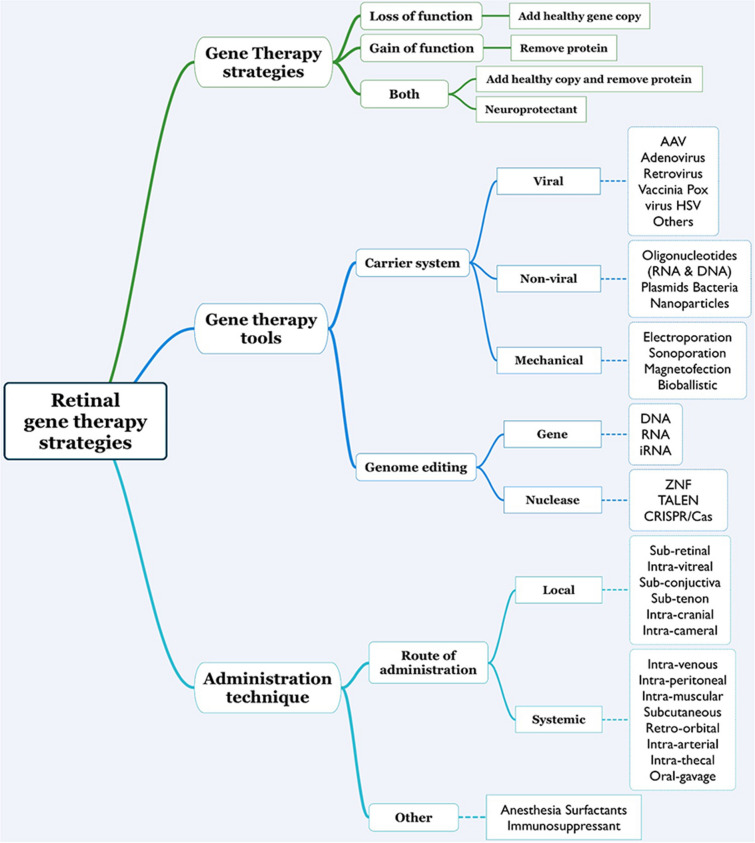
New therapies need to be carefully evaluated and improved before being tested in human clinical trials. In addition to the importance of preclinical models, the selection of an appropriate vector for the transfer of the desired genetic material, the choice of vector transfer method, and the optimization of the transferred gene are of great importance. The principle of viral vector selection is based on the purpose and strategy of gene therapy. Figure 2 shows different elements of retinal gene therapy strategies. In each gene therapy, an appropriate vector type should be selected according to these elements. The most-used gene therapy strategy involves adding a healthy copy of the RPGR gene. Different vectors in inherited eye diseases have been studied extensively in preclinical and clinical studies [52].
Fig. 2.
Retinal gene therapy strategies and their components. Each component is crucial in designing retinal gene therapies
To date, in addition to viral vectors, various other types of vectors, including exosomes/liposomes, antisense oligonucleotides, naked RNA or DNA, and nanoparticles, have also been used. However, in most clinical trial studies, viral vectors have been used [53]. Among different viral vectors, adeno-associated viruses (AAVs) and lentiviruses have been used more than others. Table 2 shows the advantages and disadvantages of the leading viral vectors used for gene therapy of eye diseases. (Table 2) There is greater interest in viral vectors because of their greater potency and ability to be engineered. Other vectors also have usages, such as RNA oligonucleotides in the CRISPR-Cas complex for genetic modification.
Table 2.
Advantages and disadvantages of the leading viral vectors used for gene therapy of eye diseases
| Viral vector | Description | Advantages | Limitations | Applications |
|---|---|---|---|---|
| Adenoviruses | Non-enveloped, 36 kb genome, non-integrative | Capable of insertion of large fragments of DNA, infection of a large variety of cells, and easy propagation in the body | High immunogenicity (both cellular and humoral) | Transient expression of transgenes, DNA vaccine development due to high immunogenicity |
| Retroviruses (including lentiviruses) | Integrative | Capable of insertion of large fragments of DNA, low immunogenicity, infection of both proliferating and quiescent cells | Insertional mutagenesis | Genetic diseases of T cells including malignancies, HIV/AIDS |
| Adeno-associated virus (AAV) | Non-enveloped, single-stranded DNA, 4.7-kb genome, either integrative or non-integrative | Low immunogenicity, easy propagation in the body, infection of a large variety of cells, long-term gene expression | Limited capacity for transferring genetic materials | Genetic diseases, tumours, neurological, ocular, and cardiovascular diseases |
Given that viral vectors have been the most used and effective vectors in studies so far, we will focus on comparing the most common viral vectors in this article. Lentiviruses belong to the category of retroviruses, but their main difference from other retroviruses is their ability to infect non-dividing cells, in addition to dividing cells, making them a good choice for gene therapy of retinal cells. Lentiviruses, in addition to their high capacity to transmit long genetic fragments (up to about 11 Kbp in the third generation of lentiviruses), through the integration of their genome into the host genome, guarantee the long-term expression of the transgene. In contrast, due to the high degree of integration into the host genome, there is a higher risk for insertional mutagenesis and immune reactions. AAVs, originally discovered as associated viruses with adenoviruses, need certain adenoviruses-related factors to replicate and become pathogens, so these vectors are not inherently pathogenic and induce little immune responses. These two essential features of AAVs have extended their in-vivo applications [54]. AAVs can infect dividing or non-dividing cells and integrate their DNA into the host genome or stand in episomal form (without integration) for expressing transgenes [55]. It is important to note that because the site of possible integration of the virus gene into human chromosomes is known (AAVS1 region in chromosome number 19), these viruses have a low risk for insertional mutagenesis [53].
Depending on the frequency of receptors in each tissue, different virus serotypes have different tropisms to various tissues. Suitable AAV serotypes for the transduction of photoreceptor cells include AAV2, AAV5, and AAV8. RPE cells are transduced well when AAV1, AAV2, AAV4, AAV5, and AAV8 are used. Due to the widespread use of the AAV virus in ocular diseases, virus-specific tropisms for different ocular cell types have also been evaluated (Table 3) [2, 56, 57]. Given that one of the limiting factors in the in vivo use of viral vectors is the non-specific effect on all available cells, using serotypes that are more specific for certain cell types can result in a more targeted and specific therapeutic effect.
Table 3 .
Efficiency of transduction of different retinal cells of different serotypes of AAV vectors in mice
| Capsid/cell type | RPE | Photoreceptor | Ganglion cell layer | Muller cells |
|---|---|---|---|---|
| AAV 1 | + + + | − | − | + |
| AAV 2 | + + | + | + + | + |
| AAV2/2 | + + | + + | + | + + + |
| AAV2/5 | + + + | + + + | − | + |
| AAV 4 | + + | − | − | + |
| AAV 5 | + | + + | − | + |
| AAV 8 | + | + + + | + + | + |
| AAV 9 | − | + + + | + + | + + |
− No transduction, + to + + + , increasing transduction
AAV adeno-associated virus, RPE retinal pigment epithelium
One of the recent advances in the use of AAV vectors is the development of AAV pseudo-types. The virus is produced by putting the genome of one serotype together with the capsid of another serotype of the virus. This way, they have higher transduction ability and different tropism [58, 59]. For example, the transduction ability of the AAV2/5 pseudotype for nervous cells is higher than that of the AAV2 vector (with serotype 2 capsid), and this hybrid virus has a more remarkable ability to spread within the brain. AAV 2, 5, and 8 are the best AAV serotypes for photoreceptors in XLRP patients. Despite the positive results of the AAV2 virus for retinal gene therapy, hybrid viruses originating from this serotype, such as AAV2/5, AAV2/8, and AAV-PHP.eB, have shown better results regarding retinal distribution and transduction of photoreceptors [59–61]. Also, there is a type of hybrid virus called AAV-DJ, whose capsid is formed by the fusion of eight different viral serotypes capsids, making this vector the most potent AAV vector for in vitro transduction and a useful vector for in vivo uses, with broad tropism for a wide range of cell types [62, 63].
In human studies using gene therapy for treating eye diseases, mostly AAV vector has been used, while only in two cases, due to insufficient capacity of AAV for transferring the genes, have lentiviral vectors been used [64, 65]. In other studies, antisense oligonucleotide was used to inhibit gene expression at the transcription level (mRNA) [66, 67]. Paying attention to safe and effective vectors, which have already been used in human studies, can help select the appropriate vector for pre-clinical studies. In preclinical studies most also used AAV vectors for gene transfer. In a study by Buck and Wijnholds, the advantages and disadvantages of using recombinant AAV vectors in gene therapy for eye diseases have been discussed [53]. Briefly, AAV vector (1) can express its transgene in a few days to a few weeks and reach its maximum expression in 4–6 weeks [68]; (2) the virus enters its genome into the cell nucleus in episomal form and can express its genome without integration into the host genome [55]; (3) it can express its gene in a long-term manner. It has been observed that gene expression in dogs has continued for up to 10 years [69]; (4) AAV can have different capsids, resulting in different virus serotypes with different tropisms for tissues. An appropriate AAV serotype could be selected according to the purpose and strategy of gene therapy [70, 71]. (5) AAV can spread efficiently in the tissues and infect a large part of the target tissue. Finally, as mentioned before, (6) AAV administration has been associated with a few dangerous side effects in various studies and is currently one of the safest types of gene therapy [72, 73]. In contrast, (1) the low gene transfer capacity of AAV (about 5 kb) has limited its ability to transmit large gene fragments. (2) Two sequences, called inverted terminal repeats (ITRs), are located on both sides of the transferred gene in the structure of the AAV genome. These sequences may not be stable enough in the structure of the AAV genome and could reduce gene expression. (3) In addition, for significant expression of the transgene, due to the high rate of multiplicity of infection (MOI), a large amount of virus is required, which in turn (4) can stimulate humoral immunity and induce the production of blocking antibodies or activate cellular immunity and inhibit or destruct virus-infected cells, which subsequently can reduce the efficiency of AAV vectors [74].
Preclinical Gene Therapy Trials of XLRP
So far, several preclinical attempts at gene therapy treatment of XLRP have been made. In 2012, the AAV 5 viral vector bearing the gene encoding for RPGR under the guidance of either promoter of interphotoreceptor retinoid-binding protein (IRBP) or human G-protein-coupled receptor kinase 1 (hGRK1) was injected subretinally for treatment of XLRP in two canine models of this disease. It could successfully prevent the degeneration of rod and cone photoreceptors [75]. In another study in 2015, the effect of RPGR gene replacement under the control of the rhodopsin kinase promoter in the knockout mouse model of XLRP disease (RPGR −/−) showed better responses in the electroretinogram (ERG) along with retainment of retinal layers. Moreover, the effect of using different doses of viral vectors on its therapeutic benefit was investigated, and the need for intelligent dose selection to prevent side effects of the virus at high doses was discussed [76]. In another study using a canine model carrying a natural mutation in the RPGR gene (XLPRA2), the effect of different doses of recombinant RPGR gene, which were transferred by AAV serotype 2 or 5 (rAAV2tYF-GRK1-hRPGRco and rAAV5-GRK1-hRPGRco), on the amount of RPGR protein expression, inflammatory reactions, maintenance of the retinal layers thickness, production of antibodies against hRPGR, and spatial correction of opsin in photoreceptors was evaluated. Superior effects of rAAV2tYF-GRK1-hRPGRco and clues for reaching the appropriate dose for human studies were demonstrated [77]. Also, using CRISPR/Cas9 for repairing the RPGR gene with a pattern DNA strand in the process of HDR (homology-directed repair) in the RPGR −/y mouse model has been associated with good therapeutic effects for 6 to 12 months after treatment [78, 79].
The preclinical gene therapies of XLRP are summarized in Table 4. These trials showed that the most commonly used models were the rd9 mice models and XLPRA2 canine model, the latter of which allows injection of larger amounts of vectors with higher precision. The most commonly used vectors were AAV2/5 and AAV2/8; however, CRISPR has recently showed promising results for both model development and reversal of pathology. The current prominent challenges are the stable expression of RPGR and the uniform distribution of subretinally injected vectors across the retina. Given retinal toxicity in high vector doses, dosage-finding preclinical assessments should be carefully done for each agent. Moreover, future preclinical studies should evaluate the effectiveness of vectors with engineered capsids capable of passing through retinal layers after intravitreal injection to reach photoreceptors.
Table 4.
Characteristics and findings of preclinical trials of X-linked retinitis pigmentosa gene therapy
| Authors | Year | Animal model | Agent and gene | Dosage | Findings |
|---|---|---|---|---|---|
| Hong et al. [126] | 2005 | RPGR knockout (KO) mice | Shortened RPGR cDNA | Transfected into mouse embryonic stem cells. Transgenic chimeras were crossed with RPGR-KO mice |
Expression of RPGR-ORF15 in rods and cones Rescue of function and structure of retinal degeneration |
| Beltran et al. [75] | 2012 | XLPRA1 and XLPRA2 canine models | AAV 2/5–vectored human RPGR with human IRBP or GRK1 promoters | 1.05 × 1010 vg in 70 μl at 5th week, 21.25 × 1010 vg in 150 μl at 28th week |
Preserved photoreceptor nuclei and inner/outer segments Improved rod and cone photoreceptor function Reversal of opsin mislocalization |
| Wu et al. [76] | 2015 | Rpgr-KO mice | AAV8-mRpgr (mouse RPGR), AAV8-hRPGR (human RPGR) and AAV9-mRpgr (mouse RPGR) | 1 × 1011 to 1 × 1013 in 1 μl |
Maintained the expression of RPGR-ORF15 throughout the study duration Better electroretinogram response Remarkable preservation of retinal structure and function Retinal toxicity was observed at high vector doses needing dose optimization |
| Beltran et al. [127, 128] | 2015 | XLPRA2 dogs | AAV2/5 vector construct carrying full-length human RPGR1−ORF15 cDNA under control of a hIRBP promoter | 70–150 μl at the concentration of 1.51 × 1011 vg/ml |
Earlier intervention results with better results Preserved therapeutic function of intervention Significant improvement in structural, functional, and behavioural assessments |
| Mookherjee et al. [86] | 2015 | Rp2-KO mice | AAV8-scRK-hRP2 | 1 × 108, 3 × 108 or 1 × 109 vector genomes |
Preservation of cone function, viability Correction of opsin trafficking Retinal toxicity in high dose group |
| Deng et al. [129] | 2015 | C57/B mice | AAV-hIRBP-hRPGR and AAV-hGRK1-hRPGR | 1 μl of AAV at low dose of 1010 vg/ml, middle dose of 1.5 × 1011 vg/ml and high dose of 1013 vg/ml |
Expression of RPGR No retinal toxicity |
| Pawlyk et al. [40] | 2016 | Rpgr−/− mice | AAV2/8-RK-ORF15-L and AAV2/8-RK-ORF15-S | 2 × 109 vg or 5 × 109 vg |
Significant functional and morphological rescue of rods and cones in long RPGR form More stability in shorter form while remaining functional |
| Fischer et al. [25] | 2017 |
Two Mouse models (Rpgr−/y and C57BL/6JRd9/Boc) |
AAV 2/8 encoding for RPGRORF15 with photoreceptor-specific human rhodopsin kinase (RK) promoter | 1.5 × 109 vg in 1.5 μl |
Optimized gene replacement therapy with stable production of the full-length RPGR protein Preserved Glutamulation properties of RPGR following codon optimization Acceptable safety in animals Rescued function of rod and cone receptors |
| Beltran et al. [24] | 2017 | XLPRA2 canine models, macaques (Macaca mulatta and Macaca fascicularis) | AAV2/5 vector carrying hRPGRstb and hRPGRco under control of GRK1 and IRBP promoters | 70–100 μl at the concentration of 1.5 × 1011 and 1.5 × 1012 vg/ml |
Ability of AAV 2/5 to transduct both rod and cone receptors Efficiency of GRK1 and IRBP promoters for rescuing photoreceptors |
| Giacalone et al. [130] | 2019 | Wild-type Sprague-Dawley rats | AAV 2/5-CMV-IA-RPGR | 10 μl of at the concentration of 1 × 1012 vg/ml |
Stable expression of mutant RPGR Functional RPGR transcript and protein production |
| Schlegel et al. [131] | 2019 | B6J.Sv129-Rpgrtm1Sti | AAV2/5.CMV.I-SceI-T2A-GFP and AAV2/8.RK.I-SceI-T2A-GFP | 1 μl each of vector at the concentration of 3 × 1011 vg/ml | Proof of concept of a human-XLRP gene therapy using endonuclease I-SceI |
| Song et al. [77] | 2020 | XLPRA2 canine model | rAAV2tYF-GRK1-hRPGRco or rAAV2tYF-GRK1-hRPGRstb | 150 μl at the concentration of 3.0 × 1012 vg/ml (high dose), 6.0 × 1011 vg/ml (mid dose), or 1.2 × 1011 vg/ml (low dose) |
No significant signs of ocular discomfort or ophthalmic complications Rescue the function and structure of photoreceptors Stronger expression for rAAV2tYF-GRK1-hRPGRco compared to rAAV2tYF-GRK1-hRPGRstb Correction of rod and cone opsin mislocalization |
| Hu et al. [78] | 2020 | Rpgr−/yCas9+/WT mice | AAV 2/8 encoding for sgRNA targeted to the mutant Rpgr locus and donor template | 1 µl at a concentration of 1 × 1012 vector genomes per milliliter |
Significant photoreceptor preservation Therapeutic effect lasts for up to 12 months with no off-target effects |
| Dufour et al. [132] | 2020 | XLPRA2 dog model | AAV2tYF with GRK1 promoter | 0.07 ml at the concentration of low (1.2 × 1011 vg/ml), mid (6 × 1011 vg/ml), or high dose (3 × 1012 vg/ml) |
Well toleration without systemic toxicity Rescue of functional and structural of photoreceptors Posterior segment toxicity at high dose level |
| Gumerson et al. [79] | 2022 | Rd9 mice | Dual AAV vectors: one containing SpCas9 driven by RK promoter and another containing both the RPGR-targeted sgRNA driven by the U6 promoter and tdTomato reporter gene driven by RK promoter | 1 μl of each vector at the concentration of 7.5 × 109–1 × 1010 vg/μl |
Restored reading frame of RPGRORF15 Broad distribution throughout the retina following subretinal injection |
Gene Therapy Clinical Trials of XLRP
The number of clinical trials has increased in recent years. However, few have reported their results. A first-in-human phase 1/2 clinical trial for XLRP demonstrated the safe administration of AAV8 vector expressing codon-optimized human RPGR with sustained visual field improvements [4]. Another phase 1/2 study, using AAV5 hRK-RPGR-ORF15 vectors, showed clinically meaningful improvement in the function and sensitivity of photoreceptors 12 months after injection [80]. As shown in Table 1, gene therapy for XLRP has reached phase 3, and approval of a gene therapy product in the near future is conceivable (Table 1).
Evaluations and Measurements
Evaluating the baseline features and their changes during gene therapy interventions is crucial. It would be useless to perform a gene therapy without precisely knowing the findings of retinal degeneration’s natural course and methods of monitoring the response to treatment. Evaluations should include both functional and morphological (structural) aspects of retinal cells. Functional evaluations include optomotor (optokinetic) assessment, electrophysiology, and visual evoked potentials (VEP). Structural and morphological evaluations include ophthalmoscopy of cornea and lens of mice (with ophthalmoscope or slit lamp), retinography and optical coherence tomography, histology, immunofluorescence, and immunocytochemistry.
Functional Assessments
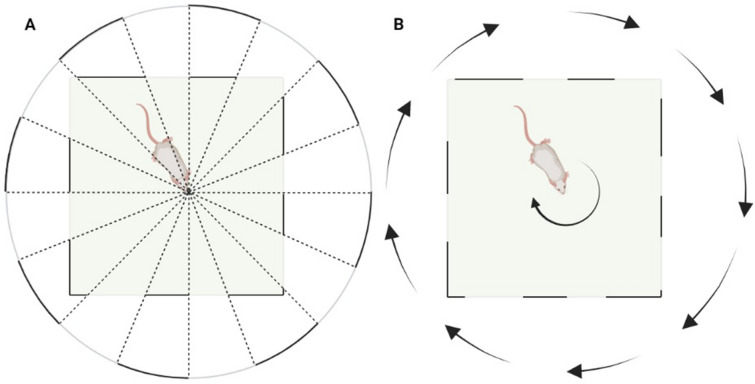
Optomotor Test
The spatial visuality of animals is measured based on the optomotor response. The first optomotor test and measurement device was developed by Prusky et al. in 2004 [81] and later modified for use in rats by Tomita et al. in 2009 [82]. This test is performed in two parts: first for behavioural testing and second for determining visual thresholds. The basis of this test is the rotation of a visual stimulus image—dark and light grids—on the inner surface of a cylinder around the animal (Fig. 3). The animal follows the visual stimulus by rotating its head following the stimulation. The experimenter observes the animal in terms of the simultaneous movement of the animal's head with the visual stimulus. Suppose the movement of the animal's head coincides with the movement of the visual stimulus. In that case, the experimenter understands that the animal can distinguish between dark and light grids and therefore proceeds to the next stage at a higher speed. In the second part of this test, lines are displayed as sinusoidal lines with different frequencies and contrasts for the animal. The animal’s maximum detectable speed is recorded. The measurement of animal models respecting the recognizable image contrast level is the same [83–85].
Fig. 3.
Schema of the optomotor test. A A virtual rotating cylinder consisting of black and white grid lines around the animal is shown in part A. B Animal head movement should be consistent with the rotation of the virtual cylinder
Although the exact mechanism behind the test is not completely clear, it involves both the visual and motor systems [81]. The visual thresholds in mice with RP were considerably reduced, while rescuing the photoreceptors restored the thresholds to a relatively healthy state [86].
Electrophysiological Assessments
Electroretinogram (ERG) is used to study the function of photoreceptors and is one of the most accurate methods to study the function of rod and cone cells. This test, based on the amount of the electrical response of the outer part of the photoreceptors to light stimuli, can examine the function of rod and cone cells separately. This way, retinal degenerative diseases are categorized into rod-cone, cone-rod, and second-order-neuron dysfunction [87]. Usually, the RP is a rod-cone type, and due to retinal degeneration over time, the ERG wave amplitude gradually decreases. The level of the wave amplitude is proportional to the area of the functional retina [20, 88, 89]. The noteworthy point of this test is that because the test examines the entire surface of the retina, the ability of this test to examine visual changes in the macula or minor changes in a limited part of the retina is low. Therefore, while ERG is the best test for diagnosing RP, due to its limited ability to detect small changes, it is not a suitable assessment method for detecting changes during disease progression or treatment response. It can best be used before and after treatment to determine the total effect [90]. The main characteristics of the ERG electrical response waves are the intensity and distance to the peak of the waves. There are two types of waves, “a” and “b”. The “a” wave is associated with the initial response of photoreceptors to light stimuli. In contrast, the “b” wave indicates the function of cells secondary to photoreceptors, such as bipolar cells [91–93]. A decrease in the intensity of the a or b waves of rod or cone cells can represent different pathologies in the retina. Studies have shown that in XLRP animal models, the intensity of a and b waves decreases with age [50]. Also, RPGR gene therapy in these models stops the progression of the disease characterized by the reduction of the ERG wave intensity and an increase in the latency to peak the waves [40].
Visual Evoked Potentials (VEP)
Although there are several ways to check VEP, a similar method to ERG with different places of electrodes is used to examine VEP in animal models [94–96]. Patients with RP have a significant increase in the PR (pattern-reversal)-VEP latency and a decrease in amplitudes [97]. While measurement of VEP was not used widely in preclinical studies of RP, combination recording of ERG and VEP could help localize the affected visual part [98].
Structural and Morphological Assessments
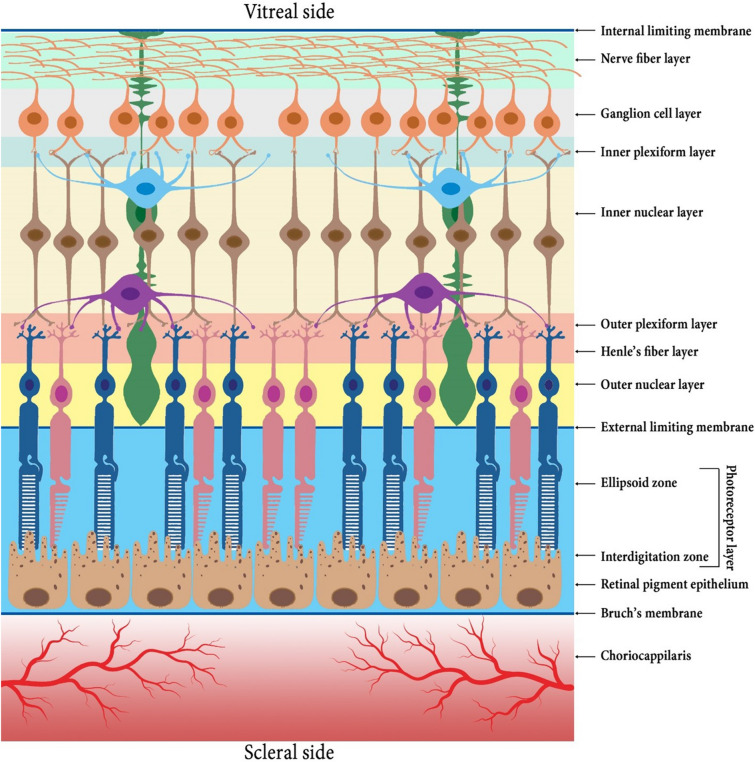
Optical Coherence Tomography (OCT)
The use of OCT as a non-invasive method is an essential tool for ophthalmologists and researchers in the field of eye diseases to study the structure of the retina. Despite the existence of many types of OCT devices for clinical and research applications, the introduction of spectral domain OCT (SD-OCT) devices has increased the accuracy of OCTs (up to about 2 µm), as far as the results of SD-OCT have an acceptable correlation with results obtained from histological assessments [20, 99]. In the study of the retina with great details using SD-OCT devices, 13 different layers can be differentiated (Fig. 4).
Fig. 4.
Schematic illustration of retinal cell layers
So far, in studies using OCT for examination of the retina in RP patients, cystoid macular edema, epiretinal membrane, thickness and integrity of external limiting membrane (ELM) and ellipsoid zone (EZ) layers, and thickness of the outer nuclear layer (ONL) have been used to diagnose and monitor progression and response to treatment [100–105]. OCT is also used in preclinical studies. Human OCT devices can be used for animals with bigger eyes, like dogs; currently, there are animal OCT devices (such as MICRON III, designed for rodents). These devices use lights with low coherence and analyse their return from the light-scattering surface (such as the retina) to achieve a micrometer resolution. In a study by Nakazawa et al. about the changes in OCT of several mouse models of RP, a series of common features have been suggested, including thinning of the ONL layer and hyperreflective changes in the internal and external retina [106]. In another study on the RPE knockout murine model (a model for LCA disease, recognized as an aggressive form or juvenile form of RP [107, 108]), thinning of the ONL layer and loss of arrangement of internal and external parts of the photoreceptors are described as the changes during LCA [109]. Also, in a study on the effectiveness of RPGR gene therapy, the ONL layer thickness has been considered an indicator of treatment response. Gene therapy could preserve the ONL layer thickness compared with a considerable reduction in the control group [24, 25, 48].
Histology
Histological examination of the animal retina can be a good representative for evaluating the response to treatment and assessing different layers of the retina. Histological examination of the retina can be done using light or electron microscopy, immunofluorescence, or immunocytochemistry methods. Light or electron microscopy of the retina is used to examine the structure of the eye, but immunofluorescence and immunocytochemistry are more commonly used. One of the primary evaluation methods in XLRP disease is assessing RPGR protein mislocalization using immunofluorescence after RPGR staining. In XLRP animal models, RPGR protein is significantly mislocalized in the structure of photoreceptors connecting cilium [38], while adding a normal allele of RPGR gene in these models increases the rate of RPGR protein accumulation with the correct arrangement (narrow band between the inner and outer areas of photoreceptor cells) to the extent that it is not much different from normal cells [40]. Evaluating the order and counting the number of rows of cells in different layers, especially the ONL (outer nuclear layer), is one of the variables for monitoring changes in response to treatment [50, 110].
Ophthalmoscopy of the Lens and Fundus (with Ophthalmoscope or Slit Lamp)
In the ocular examination of animal models of RP, there are spots with pigment accumulation and depigmented spots on the fundus of the eye that give the retina a dotted appearance [111]. Furthermore, during fundus photography, narrow attenuated vessels could be seen [112]. Moreover, posterior subcapsular cataract could be observed during slit-lamp examination [113]. It should be noted that heterozygous females’ examinations showed patches of affected retina as well as patches of intact retina, likely caused by locations where random X-inactivation resulted in expression of the mutant allele [114].
Retinal Angiography
Fluorescein-assisted retinal angiography, although seldom used nowadays, can show attenuation of retinal vessels [2, 111].
Immunoblotting
The immunoblotting assay is used to check for RPGR protein in the retina of mice and plays a vital role in studying XLRP animal models. The method involves harvesting the retina, subsequent separation of proteins using SDS-PAGE, and then RPGR protein (or other proteins according to the purpose of the study) identification using associated antibodies [34, 38].
Challenges in RPGR Gene Therapy
Manufacturing ORF15 in recombination processes: One of the challenges in gene therapy for the RPGR gene is its instability during recombination processes [115]. As mentioned, the ORF15 area is a mutational hotspot and about 80% of the mutations are located in this region. ORF15 is a purine-rich region, making it unstable in the manufacturing process of its entire length. However, studies have shown that this region has different lengths in the healthy general population. Therefore, the full length of this sequence for normal protein function is not necessary [115]. In a study in 2015, the function of RPGR protein made from two ORF15 sequences with different lengths was evaluated. It was reported that although the full-length deletion of ORF 15 interferes with the normal function of this protein, moderately shortening this sequence while maintaining the efficiency and function of the protein increases gene stability in genetic processes. For a similar reason, to date, it has been reported that cloning the entire length of the RPGR sequence in the form of cDNA using RNAs in retinal cells is not possible [40].
The route of vector injection: To perform the gene therapy process, it is necessary to deliver the engineered genetic material to the target cells (photoreceptors). These cells are located on the outside layers of the retina. Currently, because of the excellent features of the eyes for in-vivo gene therapy, genetic materials encompassed in viral vectors are directly injected into the eye and placed in direct contact with retinal cells. However, injecting these viral vectors is not without side effects. Common methods currently used to inject viral vectors into the eye include subretinal and intravitreal injections [116]. These methods have advantages and disadvantages that Peng et al. reviewed in 2017 [116]. In the transscleral subretinal injection method, after inserting the needle into the eye posterior to the eye limbus, through the space behind the ciliary bodies and the zonular filaments, at a tangential angle so that the lens is not damaged, the needle tip is passed through the retina. After reaching the underlying sclera, the injection is made in the subretinal space, while in the intravitreal method, the injection is done into the vitreous cavity after the needle enters the space inside the eye in the area behind the lens and in front of the retina. The subretinal injection, due to the shorter distance the virus has to its target cells, has a comparative advantage. In contrast, this type of injection involves entering viral vectors and genetic material into a space that does not exist physiologically; hence, it could induce retinal detachment and inflammation in the retina. However, in several papers, this retinal detachment has been reported to be temporary and reversible, and inflammation can be controlled with corticosteroid administration [4, 117]. Still, the inflammation can reduce the ability of the viral vector in the transduction of photoreceptors [118, 119]. In addition, subretinal injection leads to more retinal damage and surgical complications. It should be noted that the only approved drug for eye diseases (Luxturna) is to be injected via the subretinal route, and it seems that the skill and experience of the ophthalmologist play a key role in the success and complications of this injection method [116, 120, 121]. In contrast, intravitreal injection, despite being a more straightforward procedure, causing less damage to the retina, inducing a trivial inflammation and higher feasibility, especially in animal models with smaller eyes such as mice, could be less effective because of the longer distance between injected viral vectors and the photoreceptors [116, 122]. In recent years, with the development of various pseudotypes of the AAV, few advancements have been made in this field. These pseudotypes, having a combination of capsids of vector serotypes with stronger tropism for photoreceptor cells and nervous tissue, have shown better performance in passing through multiple layers of the inner retina and reaching the photoreceptor cells [56, 123].
The coverage of the entire retina: One barrier that limits the effectiveness of retinal gene therapy is the limited distribution of viral vectors, especially through subretinal injection. In fact, in the subretinal method, a higher concentration of vectors is introduced to photoreceptor cells and RPE due to the focal entry of the vectors. However, this effect is limited to the injection site, where the bubble of retinal detachment is seen. Recently using scaffolds containing viral vectors has created a new horizon for broader distribution of vectors across the retina [116, 124]. In contrast, during intravitreal injection of vectors, due to the fluidic nature of the vitreous fluid, relatively equal amounts of vectors will be placed in contact with every part of the retinal inner surface, so the inner layers of the retina, including ganglion cell layer and Müller glial cells, are affected similarly [53]. Notably, in the intravitreal injections of recombinant viral vectors and also their newer and more potent variants, such as hybrid vectors in the eyes of rodents, they can affect the entire thickness of the retina, while when used for the eyes of mammals, the inner limiting membrane layer prevents the spread of viral vectors to the inner layers of the retina [53].
Early detection for more effective gene therapy: Recent studies have shown that gene therapy has different efficacy when implemented at various stages of the disease. Despite the impact of other factors, such as the role of the mutated gene and the remaining function of the mutant allele, the significant effect of the timing of gene therapy (at which stage of the disease) creates a narrow opportunity to identify the suitable treatment candidates and implement gene therapy for them [125].
Methods of transgene optimization: One of the barriers to XLRP gene therapy is the nature of the RPGR gene and especially RPGRORF15. As mentioned before, the ORF15 region is a mutational hotspot and, due to the existence of a high number of AG dinucleotides, can be a receiver point in the process of mRNA splicing. In addition, a high percentage of adenine single nucleotides could act as a Lariat branch point and, by creating secondary structures, cause instability in this region during the recombination process [25]. Although RPGRORF15 does not have the last four exons of the complete gene, it has a longer sequence length than RPGREx1−19, which has all exons because the added transcribed ORF15 intron at the end of RPGRORF15 is longer than the last four exons of RPGR gene [4]. Due to the existence of several problems in the synthesis of this region, studies have been done to increase its stability. In different studies, the manufactured RPGRORF15 CDS (coding sequence) has been optimized by the following alterations and reported better results: (1) reducing the frequency of codon coding for trace amino acids from 10 to 1%, (2) removing the restriction site of MfeI enzyme, several splice sites (GGTGAT), four sequence signals for polyadenylation (three AATAAA + ATTAAA), and two poly-T sequences (TTTTTT) and a poly-A sequence (AAAAAAA), (3) optimizing the GC percentage to increase the half-life of mRNA, and (4) reducing tandem repeats [4, 25].
The Future of RPGR Gene Therapy
Although currently no drug other than Luxturna has been approved for gene therapy of eye diseases, it seems that due to a large number of in vitro and preclinical studies on gene therapy for XLRP disease, as well as the existence of several clinical trials in advanced phases, we will have the gene therapy product for XLRP on the pharmaceutical market in the near future. However, addressing the foreseen challenges will be necessary to improve the gene therapy of XLRP.
Acknowledgements
The author thanks Dr. Naser Ahmadbeigi for his kind guidance.
Funding
No funding or sponsorship was received to assist with the preparation or publication of this manuscript.
Author Contributions
Vahid Mansouri contributed to the conceptualization, drafting, and revising of the manuscript.
Disclosures
Vahid Mansouri declares that he has no competing interests.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by the author.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
References
- 1.Rivas MA, Vecino E. Animal models and different therapies for treatment of retinitis pigmentosa. Histol Histopathol. 2009;24(10):1295–1322. doi: 10.14670/HH-24.1295. [DOI] [PubMed] [Google Scholar]
- 2.Petrs-Silva H, Linden R. Advances in gene therapy technologies to treat retinitis pigmentosa. Dove Press; 2013. pp. 127–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sahel J, Bonnel S, Mrejen S, Paques M. Retinitis pigmentosa and other dystrophies. Dev Ophthalmol. 2010;47:160–167. doi: 10.1159/000320079. [DOI] [PubMed] [Google Scholar]
- 4.Cehajic-Kapetanovic J, Xue K, de la Martinez-Fernandez CC, et al. Initial results from a first-in-human gene therapy trial on X-linked retinitis pigmentosa caused by mutations in RPGR. Nat Med. 2020;26(3):354–359. doi: 10.1038/s41591-020-0763-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hims MM, Diager SP, Inglehearn CF. Retinitis pigmentosa: genes, proteins and prospects. Dev Ophthalmol. 2003;37:109–125. doi: 10.1159/000072042. [DOI] [PubMed] [Google Scholar]
- 6.Kalloniatis M, Fletcher EL. Retinitis pigmentosa: understanding the clinical presentation, mechanisms and treatment options. Clin Exp Optom. 2004;87(2):65–80. doi: 10.1111/j.1444-0938.2004.tb03152.x. [DOI] [PubMed] [Google Scholar]
- 7.Cross N, van Steen C, Zegaoui Y, Satherley A, Angelillo L. Current and future treatment of retinitis pigmentosa. Clin Ophthalmol. 2022;16:2909–2921. doi: 10.2147/OPTH.S370032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bush RA, Kononen L, Machida S, Sieving PA. The effect of calcium channel blocker diltiazem on photoreceptor degeneration in the rhodopsin Pro213His rat. Invest Ophthalmol Vis Sci. 2000;41(9):2697–2701. [PubMed] [Google Scholar]
- 9.Pawlyk BS, Li T, Scimeca MS, Sandberg MA, Berson EL. Absence of photoreceptor rescue with D-cis-diltiazem in the rd mouse. Invest Ophthalmol Vis Sci. 2002;43(6):1912–1915. [PubMed] [Google Scholar]
- 10.Pearce-Kelling SE, Aleman TS, Nickle A, et al. Calcium channel blocker D-cis-diltiazem does not slow retinal degeneration in the PDE6B mutant rcd1 canine model of retinitis pigmentosa. Mol Vis. 2001;7:42–47. [PubMed] [Google Scholar]
- 11.Bok D, Yasumura D, Matthes MT, et al. Effects of adeno-associated virus-vectored ciliary neurotrophic factor on retinal structure and function in mice with a P216L rds/peripherin mutation. Exp Eye Res. 2002;74(6):719–735. doi: 10.1006/exer.2002.1176. [DOI] [PubMed] [Google Scholar]
- 12.Tao W, Wen R, Goddard MB, et al. Encapsulated cell-based delivery of CNTF reduces photoreceptor degeneration in animal models of retinitis pigmentosa. Invest Ophthalmol Vis Sci. 2002;43(10):3292–3298. [PubMed] [Google Scholar]
- 13.Berson EL, Rosner B, Sandberg MA, et al. A randomized trial of vitamin A and vitamin E supplementation for retinitis pigmentosa. Arch Ophthalmol (Chicago, Ill: 1960). 1993;111(6):761–772. doi: 10.1001/archopht.1993.01090060049022. [DOI] [PubMed] [Google Scholar]
- 14.Berson EL, Weigel-DiFranco C, Rosner B, Gaudio AR, Sandberg MA. Association of vitamin A supplementation with disease course in children with retinitis pigmentosa. JAMA Ophthalmol. 2018;136(5):490–495. doi: 10.1001/jamaophthalmol.2018.0590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Berson EL, Rosner B, Sandberg MA, et al. Clinical trial of docosahexaenoic acid in patients with retinitis pigmentosa receiving vitamin A treatment. Archives of ophthalmology (Chicago, Ill : 1960). 2004;122(9):1297–305. [DOI] [PubMed]
- 16.Reh TA. Photoreceptor transplantation in late stage retinal degeneration. Invest Ophthalmol Vis Sci. 2016;57(5):ORSFg1-7. doi: 10.1167/iovs.15-17659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zarbin MA. Retinal pigment epithelium-retina transplantation for retinal degenerative disease. Am J Ophthalmol. 2008;146(2):151–153. doi: 10.1016/j.ajo.2008.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Singh MS, Park SS, Albini TA, et al. Retinal stem cell transplantation: Balancing safety and potential. Prog Retin Eye Res. 2020;75:100779. doi: 10.1016/j.preteyeres.2019.100779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Darrow JJ. Luxturna: FDA documents reveal the value of a costly gene therapy. Drug Discov Today. 2019;24(4):949–954. doi: 10.1016/j.drudis.2019.01.019. [DOI] [PubMed] [Google Scholar]
- 20.Menghini M, Cehajic-Kapetanovic J, MacLaren RE. Monitoring progression of retinitis pigmentosa: current recommendations and recent advances. Expert Opin Orphan Drugs. 2020;8(2–3):67–78. doi: 10.1080/21678707.2020.1735352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Russell S, Bennett J, Wellman JA, et al. Efficacy and safety of voretigene neparvovec (AAV2-hRPE65v2) in patients with RPE65-mediated inherited retinal dystrophy: a randomised, controlled, open-label, phase 3 trial. Lancet (London, England) 2017;390(10097):849–860. doi: 10.1016/S0140-6736(17)31868-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Battu R, Ratra D, Gopal L. Newer therapeutic options for inherited retinal diseases: Gene and cell replacement therapy. Indian J Ophthalmol. 2022;70(7):2316. doi: 10.4103/ijo.IJO_82_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Amato A, Arrigo A, Aragona E, et al. Gene therapy in inherited retinal diseases: an update on current state of the art. Front Med. 2021;8:750586. doi: 10.3389/fmed.2021.750586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Beltran WA, Cideciyan AV, Boye SE, et al. Optimization of retinal gene therapy for X-linked retinitis pigmentosa due to RPGR mutations. Mol Ther. 2017;25(8):1866–1880. doi: 10.1016/j.ymthe.2017.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fischer MD, McClements ME, de la Martinez-Fernandez CC, et al. Codon-Optimized RPGR improves stability and efficacy of AAV8 gene therapy in two mouse models of X-linked retinitis pigmentosa. Mol Ther. 2017;25(8):1854–1865. doi: 10.1016/j.ymthe.2017.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Georgiou M, Awadh Hashem S, Daich Varela M, Michaelides M. Gene therapy in X-linked retinitis pigmentosa due to defects in RPGR. Int Ophthalmol Clin. 2021;61(4):97–108. doi: 10.1097/IIO.0000000000000384. [DOI] [PubMed] [Google Scholar]
- 27.Mears AJ, Gieser L, Yan D, et al. Protein-truncation mutations in the RP2 gene in a North American cohort of families with X-linked retinitis pigmentosa. Am J Hum Genet. 1999;64(3):897–900. doi: 10.1086/302298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schwahn U, Paland N, Techritz S, Lenzner S, Berger W. Mutations in the X-linked RP2 gene cause intracellular misrouting and loss of the protein. Hum Mol Genet. 2001;10(11):1177–1183. doi: 10.1093/hmg/10.11.1177. [DOI] [PubMed] [Google Scholar]
- 29.Salvetti AP, Nanda A, MacLaren RE. RPGR-related X-linked retinitis pigmentosa carriers with a severe "male pattern". Ophthalmologica Journal international d'ophtalmologie International journal of ophthalmology Zeitschrift fur Augenheilkunde. 2021;244(1):60–67. doi: 10.1159/000503687. [DOI] [PubMed] [Google Scholar]
- 30.Fahim AT, Sullivan LS, Bowne SJ, et al. X-Chromosome inactivation is a biomarker of clinical severity in female carriers of RPGR-associated X-linked retinitis Pigmentosa. Ophthalmol Retina. 2020;4(5):510–520. doi: 10.1016/j.oret.2019.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Aleman TS, Cideciyan AV, Sumaroka A, et al. Inner retinal abnormalities in X-linked retinitis pigmentosa with RPGR mutations. Invest Ophthalmol Vis Sci. 2007;48(10):4759–4765. doi: 10.1167/iovs.07-0453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sandberg MA, Rosner B, Weigel-DiFranco C, Dryja TP, Berson EL. Disease course of patients with X-linked retinitis pigmentosa due to RPGR gene mutations. Invest Ophthalmol Vis Sci. 2007;48(3):1298–1304. doi: 10.1167/iovs.06-0971. [DOI] [PubMed] [Google Scholar]
- 33.Vervoort R, Lennon A, Bird AC, et al. Mutational hot spot within a new RPGR exon in X-linked retinitis pigmentosa. Nat Genet. 2000;25(4):462–466. doi: 10.1038/78182. [DOI] [PubMed] [Google Scholar]
- 34.Khanna H, Hurd TW, Lillo C, et al. RPGR-ORF15, which is mutated in retinitis pigmentosa, associates with SMC1, SMC3, and microtubule transport proteins. J Biol Chem. 2005;280(39):33580–33587. doi: 10.1074/jbc.M505827200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rao KN, Li L, Anand M, Khanna H. Ablation of retinal ciliopathy protein RPGR results in altered photoreceptor ciliary composition. Sci Rep. 2015;5(1):11137. doi: 10.1038/srep11137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hong DH, Li T. Complex expression pattern of RPGR reveals a role for purine-rich exonic splicing enhancers. Invest Ophthalmol Vis Sci. 2002;43(11):3373–3382. [PubMed] [Google Scholar]
- 37.Shu X, Black GC, Rice JM, et al. RPGR mutation analysis and disease: an update. Hum Mutat. 2007;28(4):322–328. doi: 10.1002/humu.20461. [DOI] [PubMed] [Google Scholar]
- 38.Schlegel J, Hoffmann J, Roll D, et al. Toward genome editing in X-linked RP-development of a mouse model with specific treatment relevant features. Transl Res. 2019;203:57–72. doi: 10.1016/j.trsl.2018.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sun X, Park JH, Gumerson J, et al. Loss of RPGR glutamylation underlies the pathogenic mechanism of retinal dystrophy caused by TTLL5 mutations. Proc Natl Acad Sci U S A. 2016;113(21):E2925–E2934. doi: 10.1073/pnas.1523201113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pawlyk BS, Bulgakov OV, Sun X, et al. Photoreceptor rescue by an abbreviated human RPGR gene in a murine model of X-linked retinitis pigmentosa. Gene Ther. 2016;23(2):196–204. doi: 10.1038/gt.2015.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cehajic Kapetanovic J, McClements ME, de la Martinez-Fernandez CC, MacLaren RE. Molecular strategies for RPGR gene therapy. Genes (Basel). 2019;10(9):674. doi: 10.3390/genes10090674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Moreno-Leon L, West EL, O'Hara-Wright M, et al. RPGR isoform imbalance causes ciliary defects due to exon ORF15 mutations in X-linked retinitis pigmentosa (XLRP) Hum Mol Genet. 2021;29(22):3706–3716. doi: 10.1093/hmg/ddaa269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Anasagasti A, Irigoyen C, Barandika O, de Lopez MA, Ruiz-Ederra J. Current mutation discovery approaches in Retinitis Pigmentosa. Vision Res. 2012;75:117–129. doi: 10.1016/j.visres.2012.09.012. [DOI] [PubMed] [Google Scholar]
- 44.Lv X, Zheng Z, Zhi X, et al. Identification of RPGR ORF15 mutation for X-linked retinitis pigmentosa in a large Chinese family and in vitro correction with prime editor. Gene Ther. 2022 doi: 10.1038/s41434-022-00352-3. [DOI] [PubMed] [Google Scholar]
- 45.Mihailovic N, Schimpf-Linzenbold S, Sattler I, Eter N, Heiduschka P. The first reported case of a deletion of the entire RPGR gene in a family with X-linked retinitis pigmentosa. Ophthalmic Genet. 2022;43(5):679–684. doi: 10.1080/13816810.2022.2083181. [DOI] [PubMed] [Google Scholar]
- 46.Goetz KE, Reeves MJ, Gagadam S, et al. Genetic testing for inherited eye conditions in over 6,000 individuals through the eyeGENE network. Am J Med Genet C Semin Med Genet. 2020;184(3):828–837. doi: 10.1002/ajmg.c.31843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhang Q, Acland GM, Wu WX, et al. Different RPGR exon ORF15 mutations in Canids provide insights into photoreceptor cell degeneration. Hum Mol Genet. 2002;11(9):993–1003. doi: 10.1093/hmg/11.9.993. [DOI] [PubMed] [Google Scholar]
- 48.Thompson DA, Khan NW, Othman MI, et al. Rd9 is a naturally occurring mouse model of a common form of retinitis pigmentosa caused by mutations in RPGR-ORF15. PLoS ONE. 2012;7(5):e35865. doi: 10.1371/journal.pone.0035865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hong DH, Pawlyk BS, Shang J, Sandberg MA, Berson EL, Li T. A retinitis pigmentosa GTPase regulator (RPGR)-deficient mouse model for X-linked retinitis pigmentosa (RP3) Proc Natl Acad Sci U S A. 2000;97(7):3649–3654. doi: 10.1073/pnas.97.7.3649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Falasconi A, Biagioni M, Novelli E, Piano I, Gargini C, Strettoi E. Retinal phenotype in the rd9 mutant mouse, a model of X-Linked RP. Front Neurosci. 2019;13(September):991. doi: 10.3389/fnins.2019.00991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Khan NW, Grahek G, Khanna H, Heckenlively JR. Natural History and Characterization of a Mouse Model (rd9) of X-Linked Retinitis Pigmentosa. Investigative Ophthalmology & Visual Science. 2010;51(13):4068-.
- 52.Arabi F, Mansouri V, Ahmadbeigi N. Gene therapy clinical trials, where do we go? An overview. Biomed Pharmacother. 2022;153:113324. doi: 10.1016/j.biopha.2022.113324. [DOI] [PubMed] [Google Scholar]
- 53.Buck TM, Wijnholds J. Recombinant adeno-associated viral vectors (rAAV)-vector elements in ocular gene therapy clinical trials and transgene expression and bioactivity assays. Int J Mol Sci. 2020;21(12):4197. doi: 10.3390/ijms21124197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mendell JR, Al-Zaidy SA, Rodino-Klapac LR, et al. Current clinical applications of in vivo gene therapy with AAVs. Mol Ther. 2021;29(2):464–488. doi: 10.1016/j.ymthe.2020.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bulcha JT, Wang Y, Ma H, Tai PWL, Gao G. Viral vector platforms within the gene therapy landscape. Signal Transduct Target Ther. 2021;6(1):53. doi: 10.1038/s41392-021-00487-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Natkunarajah M, Trittibach P, McIntosh J, et al. Assessment of ocular transduction using single-stranded and self-complementary recombinant adeno-associated virus serotype 2/8. Gene Ther. 2008;15(6):463–467. doi: 10.1038/sj.gt.3303074. [DOI] [PubMed] [Google Scholar]
- 57.Issa PC, De Silva SR, Lipinski DM, et al. Assessment of tropism and effectiveness of new primate-derived hybrid recombinant AAV serotypes in the mouse and primate retina. PLoS ONE. 2013;8(4):e60361. doi: 10.1371/journal.pone.0060361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Burger C, Gorbatyuk OS, Velardo MJ, et al. Recombinant AAV viral vectors pseudotyped with viral capsids from serotypes 1, 2, and 5 display differential efficiency and cell tropism after delivery to different regions of the central nervous system. Mol Ther. 2004;10(2):302–317. doi: 10.1016/j.ymthe.2004.05.024. [DOI] [PubMed] [Google Scholar]
- 59.Ross M, Ofri R. The future of retinal gene therapy: evolving from subretinal to intravitreal vector delivery. Neural Regeneration Res. 2021;16(9):1751. doi: 10.4103/1673-5374.306063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Khabou H, Desrosiers M, Winckler C, et al. Insight into the mechanisms of enhanced retinal transduction by the engineered AAV2 capsid variant -7m8. Biotechnol Bioeng. 2016;113(12):2712–2724. doi: 10.1002/bit.26031. [DOI] [PubMed] [Google Scholar]
- 61.Palfi A, Chadderton N, Millington-Ward S, et al. AAV-PHP.eB transduces both the inner and outer retina with high efficacy in mice. Mol Ther Methods Clin Dev. 2022;25:236–249. doi: 10.1016/j.omtm.2022.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Katada Y, Kobayashi K, Tsubota K, Kurihara T. Evaluation of AAV-DJ vector for retinal gene therapy. PeerJ. 2019;7:e6317. doi: 10.7717/peerj.6317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Grimm D, Lee JS, Wang L, et al. In vitro and in vivo gene therapy vector evolution via multispecies interbreeding and retargeting of adeno-associated viruses. J Virol. 2008;82(12):5887–5911. doi: 10.1128/JVI.00254-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kong J, Kim SR, Binley K, et al. Correction of the disease phenotype in the mouse model of Stargardt disease by lentiviral gene therapy. Gene Ther. 2008;15(19):1311–1320. doi: 10.1038/gt.2008.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zallocchi M, Binley K, Lad Y, et al. EIAV-based retinal gene therapy in the shaker1 mouse model for usher syndrome type 1B: development of UshStat. PLoS ONE. 2014;9(4):e94272. doi: 10.1371/journal.pone.0094272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gupta A, Kafetzis KN, Tagalakis AD, Yu-Wai-Man C. RNA therapeutics in ophthalmology - translation to clinical trials. Exp Eye Res. 2021;205:108482. doi: 10.1016/j.exer.2021.108482. [DOI] [PubMed] [Google Scholar]
- 67.Covello G, Ibrahim GH, Bacchi N, Casarosa S, Denti MA. Exon skipping through chimeric antisense U1 snRNAs to correct retinitis Pigmentosa GTPase-regulator (RPGR) splice defect. Nucleic Acid Ther. 2022;32(4):333–349. doi: 10.1089/nat.2021.0053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Cripe TP, Hutzen B, Currier MA, et al. Leveraging gene therapy to achieve long-term continuous or controllable expression of biotherapeutics. Sci Adv. 2022;8(28):eabm1890. doi: 10.1126/sciadv.abm1890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gardiner KL, Cideciyan AV, Swider M, et al. Long-term structural outcomes of late-stage RPE65 gene therapy. Mol ther. 2020;28(1):266–278. doi: 10.1016/j.ymthe.2019.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Koerber JT, Klimczak R, Jang JH, Dalkara D, Flannery JG, Schaffer DV. Molecular evolution of adeno-associated virus for enhanced glial gene delivery. Mol Ther. 2009;17(12):2088–2095. doi: 10.1038/mt.2009.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Frederick A, Sullivan J, Liu L, et al. Engineered capsids for efficient gene delivery to the retina and cornea. Hum Gene Ther. 2020;31(13–14):756–774. doi: 10.1089/hum.2020.070. [DOI] [PubMed] [Google Scholar]
- 72.Kuzmin DA, Shutova MV, Johnston NR, et al. The clinical landscape for AAV gene therapies. Nat Rev Drug Discov. 2021;20(3):173–175. doi: 10.1038/d41573-021-00017-7. [DOI] [PubMed] [Google Scholar]
- 73.Pleticha J, Heilmann LF, Evans CH, Asokan A, Samulski RJ, Beutler AS. Preclinical toxicity evaluation of AAV for pain: evidence from human AAV studies and from the pharmacology of analgesic drugs. Mol Pain. 2014;10:54. doi: 10.1186/1744-8069-10-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Calcedo R, Wilson JM. Humoral immune response to AAV. Front Immunol. 2013;4:341. doi: 10.3389/fimmu.2013.00341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Beltran WA, Cideciyan AV, Lewin AS, et al. Gene therapy rescues photoreceptor blindness in dogs and paves the way for treating human X-linked retinitis pigmentosa. Proc Natl Acad Sci USA. 2012;109(6):2132–2137. doi: 10.1073/pnas.1118847109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wu Z, Hiriyanna S, Qian H, et al. A long-term efficacy study of gene replacement therapy for RPGR-associated retinal degeneration. Hum Mol Genet. 2015;24(14):3956–3970. doi: 10.1093/hmg/ddv134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Song C, Dufour VL, Cideciyan AV, et al. Dose range finding studies with Two RPGR transgenes in a canine model of X-Linked retinitis pigmentosa treated with subretinal gene therapy. Hum Gene Ther. 2020;31(13–14):743–755. doi: 10.1089/hum.2019.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Hu S, Du J, Chen N, et al. In Vivo CRISPR/Cas9-Mediated genome editing mitigates photoreceptor degeneration in a mouse model of X-linked retinitis pigmentosa. Invest Ophthalmol Vis Sci. 2020;61(4):31. doi: 10.1167/iovs.61.4.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Gumerson JD, Alsufyani A, Yu W, et al. Restoration of RPGR expression in vivo using CRISPR/Cas9 gene editing. Gene Ther. 2022;29(1–2):81–93. doi: 10.1038/s41434-021-00258-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Michaelides M, Xu J, Wang D, et al. AAV5-RPGR (botaretigene sparoparvovec) gene therapy for X-linked retinitis pigmentosa (XLRP) demonstrates localized improvements in static perimetry. Invest Ophthalmol Vis Sci. 2022;63(7):3846. [Google Scholar]
- 81.Prusky GT, Alam NM, Beekman S, Douglas RM. Rapid quantification of adult and developing mouse spatial vision using a virtual optomotor system. Invest Ophthalmol Vis Sci. 2004;45(12):4611–4616. doi: 10.1167/iovs.04-0541. [DOI] [PubMed] [Google Scholar]
- 82.Tomita H, Sugano E, Fukazawa Y, et al. Visual properties of transgenic rats harboring the channelrhodopsin-2 gene regulated by the thy-1.2 promoter. PLoS ONE. 2009;4(11):e7679. doi: 10.1371/journal.pone.0007679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Abdeljalil J, Hamid M, Abdel-Mouttalib O, et al. The optomotor response: a robust first-line visual screening method for mice. Vision Res. 2005;45(11):1439–1446. doi: 10.1016/j.visres.2004.12.015. [DOI] [PubMed] [Google Scholar]
- 84.Kretschmer F, Tariq M, Chatila W, Wu B, Badea TC. Comparison of optomotor and optokinetic reflexes in mice. J Neurophysiol. 2017;118(1):300–316. doi: 10.1152/jn.00055.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Shi C, Yuan X, Chang K, et al. Optimization of Optomotor Response-based Visual Function Assessment in Mice. Sci Rep. 2018;8(1):9708. doi: 10.1038/s41598-018-27329-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mookherjee S, Hiriyanna S, Kaneshiro K, et al. Long-term rescue of cone photoreceptor degeneration in retinitis pigmentosa 2 (RP2)-knockout mice by gene replacement therapy. Hum Mol Genet. 2015;24(22):6446–6458. doi: 10.1093/hmg/ddv354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gundogan FC, Tas A, Sobaci G. Electroretinograms. London: IntechOpen; 2011. Electroretinogram in hereditary retinal disorders; pp. 95–132. [Google Scholar]
- 88.Miyake Y, Shinoda K, et al. Clinical electrophysiology. In: Ryan SJ, Sadda SR, Hinton DR, Schachat AP, Sadda SR, Wilkinson CP, et al., editors. Retina. London: W.B. Saunders; 2013. pp. 202–226. [Google Scholar]
- 89.Robson AG, Frishman LJ, Grigg J, et al. ISCEV Standard for full-field clinical electroretinography (2022 update) Doc Ophthalmol. 2022;144(3):165–177. doi: 10.1007/s10633-022-09872-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zhao C, Yasumura D, Li X, et al. mTOR-mediated dedifferentiation of the retinal pigment epithelium initiates photoreceptor degeneration in mice. J Clin Investig. 2011;121(1):369–383. doi: 10.1172/JCI44303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Benchorin G, Calton MA, Beaulieu MO, Vollrath D. Assessment of murine retinal function by electroretinography. Bio Protoc. 2017;7(7):e2218. doi: 10.21769/BioProtoc.2218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kinoshita J, Peachey NS. Noninvasive electroretinographic procedures for the study of the mouse retina. Curr Protoc Mouse Biol. 2018;8(1):1–16. doi: 10.1002/cpmo.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Pinto LH, Invergo B, Shimomura K, Takahashi JS, Troy JB. Interpretation of the mouse electroretinogram. Doc Ophthalmol. 2007;115(3):127–136. doi: 10.1007/s10633-007-9064-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Marenna S, Castoldi V, d'Isa R, Marco C, Comi G, Leocani L. Semi-invasive and non-invasive recording of visual evoked potentials in mice. Doc Ophthalmol. 2019;138(3):169–179. doi: 10.1007/s10633-019-09680-z. [DOI] [PubMed] [Google Scholar]
- 95.Ridder W, III, Nusinowitz S. The visual evoked potential in the mouse—origins and response characteristics. Vision Res. 2006;46(6–7):902–913. doi: 10.1016/j.visres.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 96.Tomiyama Y, Fujita K, Nishiguchi KM, et al. Measurement of electroretinograms and visually evoked potentials in awake moving mice. PLoS ONE. 2016;11(6):e0156927. doi: 10.1371/journal.pone.0156927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Janáky M, Pálffy A, Horváth G, Tuboly G, Benedek G. Pattern-reversal electroretinograms and visual evoked potentials in retinitis pigmentosa. Doc Ophthalmol. 2008;117(1):27–36. doi: 10.1007/s10633-007-9099-0. [DOI] [PubMed] [Google Scholar]
- 98.Handley SE, Šuštar M, Tekavčič PM. What can visual electrophysiology tell about possible visual-field defects in paediatric patients. Eye. 2021;35(9):2354–2373. doi: 10.1038/s41433-021-01680-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Drexler W, Sattmann H, Hermann B, et al. Enhanced visualization of macular pathology with the use of ultrahigh-resolution optical coherence tomography. Arch Ophthalmol. 2003;121(5):695–706. doi: 10.1001/archopht.121.5.695. [DOI] [PubMed] [Google Scholar]
- 100.Battaglia Parodi M, La Spina C, Triolo G, et al. Correlation of SD-OCT findings and visual function in patients with retinitis pigmentosa. Graefe's Arch Clin Exp Ophthalmol. 2016;254(7):1275–1279. doi: 10.1007/s00417-015-3185-x. [DOI] [PubMed] [Google Scholar]
- 101.Cai CX, Locke KG, Ramachandran R, Birch DG, Hood DC. A comparison of progressive loss of the ellipsoid zone (EZ) band in autosomal dominant and x-linked retinitis pigmentosa. Invest Ophthalmol Vis Sci. 2014;55(11):7417–7422. doi: 10.1167/iovs.14-15013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Fischer MD, Fleischhauer JC, Gillies MC, Sutter FK, Helbig H, Barthelmes D. A new method to monitor visual field defects caused by photoreceptor degeneration by quantitative optical coherence tomography. Invest Ophthalmol Vis Sci. 2008;49(8):3617–3621. doi: 10.1167/iovs.08-2003. [DOI] [PubMed] [Google Scholar]
- 103.Hood DC, Ramachandran R, Holopigian K, Lazow M, Birch DG, Greenstein VC. Method for deriving visual field boundaries from OCT scans of patients with retinitis pigmentosa. Biomed Opt Express. 2011;2(5):1106–1114. doi: 10.1364/BOE.2.001106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Menghini M, Lujan BJ, Zayit-Soudry S, et al. Correlation of outer nuclear layer thickness with cone density values in patients with retinitis pigmentosa and healthy subjects. Invest Ophthalmol Vis Sci. 2014;56(1):372–381. doi: 10.1167/iovs.14-15521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sousa K, Fernandes T, Gentil R, Mendonca L, Falcao M. Outer retinal layers as predictors of visual acuity in retinitis pigmentosa: a cross-sectional study. Graefe's Arch Clin Exp Ophthalmol. 2019;257(2):265–271. doi: 10.1007/s00417-018-4185-4. [DOI] [PubMed] [Google Scholar]
- 106.Nakazawa M, Hara A, Ishiguro SI. Optical coherence tomography of animal models of retinitis pigmentosa: from animal studies to clinical applications. Biomed Res Int. 2019;2019:8276140. doi: 10.1155/2019/8276140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Gu SM, Thompson DA, Srikumari CR, et al. Mutations in RPE65 cause autosomal recessive childhood-onset severe retinal dystrophy. Nat Genet. 1997;17(2):194–197. doi: 10.1038/ng1097-194. [DOI] [PubMed] [Google Scholar]
- 108.Heckenlively JR, Yoser SL, Friedman LH, Oversier JJ. Clinical findings and common symptoms in retinitis pigmentosa. Am J Ophthalmol. 1988;105(5):504–511. doi: 10.1016/0002-9394(88)90242-5. [DOI] [PubMed] [Google Scholar]
- 109.Tanabu R, Sato K, Monai N, et al. The findings of optical coherence tomography of retinal degeneration in relation to the morphological and electroretinographic features in RPE65-/- mice. PLoS ONE. 2019;14(1):e0210439. doi: 10.1371/journal.pone.0210439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Barone I, Novelli E, Piano I, Gargini C, Strettoi E. Environmental enrichment extends photoreceptor survival and visual function in a mouse model of retinitis pigmentosa. PLoS ONE. 2012;7(11):e50726. doi: 10.1371/journal.pone.0050726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Shintani K, Shechtman DL, Gurwood AS. Review and update: current treatment trends for patients with retinitis pigmentosa. Optometry. 2009;80(7):384–401. doi: 10.1016/j.optm.2008.01.026. [DOI] [PubMed] [Google Scholar]
- 112.Brancati N, Frucci M, Gragnaniello D, Riccio D, Di Iorio V, Di Perna L. Automatic segmentation of pigment deposits in retinal fundus images of Retinitis Pigmentosa. Comput Med Imaging Graphics. 2018;66:73–81. doi: 10.1016/j.compmedimag.2018.03.002. [DOI] [PubMed] [Google Scholar]
- 113.Hong Y, Li H, Sun Y, Ji Y. A review of complicated cataract in retinitis pigmentosa: pathogenesis and cataract surgery. J Ophthalmol. 2020;2020:6699103. doi: 10.1155/2020/6699103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Winkler PA, Occelli LM, Petersen-Jones SM. Large Animal Models of Inherited Retinal Degenerations: A Review. Cells. 2020;9(4):882. doi: 10.3390/cells9040882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.De La Martinez-Fernandez CC, Cehajic-Kapetanovic J, MacLaren RE. RPGR gene therapy presents challenges in cloning the coding sequence. Expert Opin Biol Ther. 2020;20(1):63–71. doi: 10.1080/14712598.2020.1680635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Peng Y, Tang L, Zhou Y. Subretinal injection: a review on the novel route of therapeutic delivery for vitreoretinal diseases. Ophthalmic Res. 2017;58(4):217–226. doi: 10.1159/000479157. [DOI] [PubMed] [Google Scholar]
- 117.Qi Y, Dai X, Zhang H, et al. Trans-corneal subretinal injection in mice and its effect on the function and morphology of the retina. PLoS ONE. 2015;10(8):e0136523. doi: 10.1371/journal.pone.0136523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Fisher SK, Lewis GP, Linberg KA, Verardo MR. Cellular remodeling in mammalian retina: results from studies of experimental retinal detachment. Prog Retin Eye Res. 2005;24(3):395–431. doi: 10.1016/j.preteyeres.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 119.Westenskow PD, Kurihara T, Bravo S, et al. Performing subretinal injections in rodents to deliver retinal pigment epithelium cells in suspension. J Vis Exp. 2015;95:52247. doi: 10.3791/52247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Weng CY. Bilateral subretinal voretigene neparvovec-rzyl (luxturna) gene therapy. Ophthalmol Retina. 2019;3(5):450. doi: 10.1016/j.oret.2019.02.007. [DOI] [PubMed] [Google Scholar]
- 121.Xue K, Groppe M, Salvetti AP, MacLaren RE. Technique of retinal gene therapy: delivery of viral vector into the subretinal space. Eye (Lond) 2017;31(9):1308–1316. doi: 10.1038/eye.2017.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Dias MS, Araujo VG, Vasconcelos T, et al. Retina transduction by rAAV2 after intravitreal injection: comparison between mouse and rat. Gene Ther. 2019;26(12):479–490. doi: 10.1038/s41434-019-0100-9. [DOI] [PubMed] [Google Scholar]
- 123.De Silva SR, Charbel Issa P, Singh MS, et al. Single residue AAV capsid mutation improves transduction of photoreceptors in the Abca4(-/-) mouse and bipolar cells in the rd1 mouse and human retina ex vivo. Gene Ther. 2016;23(11):767–774. doi: 10.1038/gt.2016.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Stout JT, Francis PJ. Surgical approaches to gene and stem cell therapy for retinal disease. Hum Gene Ther. 2011;22(5):531–535. doi: 10.1089/hum.2011.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Datta P, Ruffcorn A, Seo S. Limited time window for retinal gene therapy in a preclinical model of ciliopathy. Hum Mol Genet. 2020;29(14):2337–2352. doi: 10.1093/hmg/ddaa124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Hong DH, Pawlyk BS, Adamian M, Sandberg MA, Li T. A single, abbreviated RPGR-ORF15 variant reconstitutes RPGR function in vivo. Invest Ophthalmol Vis Sci. 2005;46(2):435–441. doi: 10.1167/iovs.04-1065. [DOI] [PubMed] [Google Scholar]
- 127.Beltran WA, Cideciyan AV, Iwabe S, et al. Gene therapy for RPGR-XLRP in a canine model results in retained photoreceptors and vision for at least 2.5 years. Invest Ophthalmol Vis Sci. 2015;56(7):2588. [Google Scholar]
- 128.Beltran WA, Cideciyan AV, Iwabe S, et al. Successful arrest of photoreceptor and vision loss expands the therapeutic window of retinal gene therapy to later stages of disease. Proc Natl Acad Sci U S A. 2015;112(43):E5844–E5853. doi: 10.1073/pnas.1509914112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Deng WT, Dyka FM, Dinculescu A, et al. Stability and safety of an AAV vector for treating RPGR-ORF15 X-linked retinitis pigmentosa. Hum Gene Ther. 2015;26(9):593–602. doi: 10.1089/hum.2015.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Giacalone JC, Andorf JL, Zhang Q, et al. Development of a molecularly stable gene therapy vector for the treatment of RPGR-associated X-linked retinitis pigmentosa. Hum Gene Ther. 2019;30(8):967–974. doi: 10.1089/hum.2018.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Schlegel J, Hoffmann J, Röll D, et al. Toward genome editing in X-linked RP-development of a mouse model with specific treatment relevant features. Transl Res. 2019;203:57–72. doi: 10.1016/j.trsl.2018.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Dufour VL, Cideciyan AV, Ye GJ, et al. Toxicity and efficacy evaluation of an adeno-associated virus vector expressing codon-optimized RPGR delivered by subretinal injection in a canine model of X-linked retinitis pigmentosa. Hum Gene Ther. 2020;31(3–4):253–267. doi: 10.1089/hum.2019.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.