Abstract
Objective:
To determine the prevalence of presbyopia, near vision spectacle use, and near vision spectacle coverage among cosmetologists in Mushin Local Government Area of Lagos State with the view of creating awareness, improving productivity and quality of life.
Materials and Methods:
This was a descriptive cross-sectional study, conducted among 251 cosmetologists aged ≥ 30 years. All participants had a standardized protocol including visual acuity assessment (distance and near), anterior and posterior segment examinations, and refraction. Spectacle usage, work, productivity impact, and near vision-related quality of life (NVQoL) information were obtained with the 12-item Near Vision–Related Quality of Life Questionnaire, the Spectacle Usage section of the World Health Organisation (WHO) Spectacle and Work Productivity Questionnaire. Data obtained was analysed using Statistical Package for Social Sciences version 23 (IBM Corp. Armonk, NY).
Results:
Two hundred and fifty-one cosmetologists were studied with a male to female ratio of 1:6.4 and overall mean age of 43.9 ± 6.5 years. The prevalence of presbyopia was 67.3% and the unmet need was 51.3%. Eighty-four percent of presbyopic participants reported severe difficulty with their NVQoL compared to 16% of non-presbyopes. There was a statistically significant association between uncorrected presbyopia and reduced NVQoL (P < 0.001).
Conclusion:
This study demonstrated a relatively high prevalence of presbyopia, high unmet need, and a significant reduction in the near vision-related quality of life. This indicates the need for improved access to refractive services and spectacles among this group of artisans in whom near vision plays an indispensable role
Keywords: Cosmetologists, near vision- spectacle coverage, Nigeria, presbyopia
Introduction
Presbyopia is an irreversible age-related loss of accommodation which results in difficulty with focusing on near targets.[1] It can lead to reduction in near vision, quality of life and economic loss for individuals whose work for livelihood depends on good near vision, regardless of educational background if uncorrected.[1,2] Globally, uncorrected presbyopia is an important cause of visual disability.[3] A meta-analysis done by Fricke et al. in 2015, estimated that there were 1.8 billion people globally with presbyopia.[4] Of these, 826 million people had no spectacles correction or are inadequately corrected and the global unmet need of presbyopia was 45%.[4] There are several ways by which presbyopia could be corrected which include spectacle, contact lens, medical, surgical and laser treatment.[5] Among these interventions, spectacle correction remains the most common, affordable and accessible way of correction.[6,7]
Cosmetologists play an important role in the aesthetic industry and they require good near vision to perform their jobs optimally. They are also at risk of work-related hazards such as accidental needle prick, cuts from the use of sharp instruments and chemical burns,[8,9] which are largely preventable. In a study to determine work-related hazards among hairdressers in Ibadan, Omokhodion et al.[9] reported needles used in fixing hair as the commonest sources of injury (44%). To reduce the risk of such work-related hazards, good near vision is important for these professionals and it will also promote efficiency. Although studies on presbyopia abound among other occupations and population, there is paucity of data on the prevalence of presbyopia among this group of workers.[10,11,12,13] Therefore, this study sought to determine the prevalence of presbyopia, near spectacle use and spectacle coverage as well as the effect of not correcting same.
Materials and Methods
This was a descriptive cross-sectional study that assessed the prevalence of presbyopia, spectacle use and spectacle coverage among cosmetologists aged 30 years and above in Mushin Local Government Area (LGA) of Lagos State from August 15th to December 16th, 2019. The study was approved by the Health Research Ethics Committee of Lagos University Teaching Hospital (ADM/DCST/HREC/APP/2733) and tenets of Helsinki declaration were strictly adhered to. Written informed consent was obtained from all participants.
The study sample size was 255 using the sample size formula for finite population in descriptive studies,[14] using a prevalence of 50%, and allowing for 10% attrition. A two-stage sampling technique was used for the study. The cosmetologists in Mushin LGA were divided into 14 zones with each zone comprising about 40 cosmetologists.
Stage 1: All the 14 zonal associations were included in the study. Eighteen participants from 11 zones and 19 participants from 3 zones were recruited to give a the total sample size required (255)
Stage 2: A systematic random sampling technique was used to determine the participants in each zone using the membership registers as the sampling frame, which was 40 per zone. The sampling interval was determined by dividing the total number of cosmetologists in the zone by the calculated sample size for the zone (that is 40/18 ≈ = 2). Using ballot system, the index subject was selected from the register and every 2nd subject was included in the study until the required sample size was achieved. When a subject was absent, less than 30 years or declined to be a part of the study, the next subject on the register was included in the study.
All cosmetologists aged ≥ 30 years who were registered with the Professional Cosmetologists Association of Mushin LGA of Lagos State with best corrected distance visual acuity of 6/12 or better in both eyes and/or at least in one eye were enrolled in the study.
Demographic, medical and social information were obtained and entered into the appropriate section of the questionnaires. The distance visual acuity (VA) in each eye was tested individually using Snellen /Tumbling E chart in ambient outdoor illumination. Distance refraction was performed using an autorefractor (Xin Yuan Model FA 6500 S/N 599® by Chongqing vision star optical co.ltd (vision star) China) for subjects with VA worse than 6/9 after demonstrating improvement when tested with a pinhole. This was followed by subjective refinement using trial lenses and Snellen chart/tumbling E chart. The near vision assessment was performed in ambient light using a near reading chart placed at 40 cm from the eye, measured with a tape measure. Before near vision testing was performed, distance spectacle correction was put in place for participants that demonstrated improvement after refraction. Spherical plus lenses were added in increments of 0.5 dioptres until the subject could read at least N8 or no further improvement occurred. Spectacles were provided at no cost to the presbyopes.
Three months after the initial survey, the impact of the spectacle given on productivity and quality of life was assessed. The 12-item Near Vision–Related Quality of Life (NVQoL) questionnaire,[15] and items drawn from the Spectacle Usage section of the WHO Spectacle and Work Productivity Questionnaire,[16] which were used at the onset of this study, were used to achieve this.
In this study, an individual was considered to have presbyopia if requiring near correction of at least +1.00D in either eye in addition to their best distance correction to achieve vision correction of at least N8 at 40 cm.[13,17] The met need was defined as number of presbyopic participants who already have spectacles and near vision improved to N8 with their spectacles while the unmet need was defined as the number of presbyopic participants who require correction but do not have a pair of spectacles or near spectacles of the appropriate power at the time of the study.[17,18] Therefore, presbyopia correction coverage PCC was calculated using the formular below:
Data entry and cleaning were done using Microsoft Excel (version 2013). Statistical analysis was performed using IBM Statistical Package for Social Sciences (SPSS) version 23 (IBM Corp. Armonk, NY). Descriptive statistics are presented as frequencies and percentages for categorical data. Numeric data are presented using mean and standard deviation when normally distributed. Chi-square test was used to test for associations between categorical variables while Fischer’s exact test was used when frequency in row or column was less than 5.
The near vision-related quality of life was analysed by obtaining an overall score for each subject based on questions concerning daily activities, which was derived by adding the 8 item-specific scores which ranged from 1(no difficulty) to 5 (significant difficulty). The summary score was scaled from 0 to 100 with higher scores representing a higher level of satisfaction. Summary scores of less than 50 were graded severe difficulty, 50 - 69 as moderate difficulty, 70 - 89 as some difficulty while 90 and above as no difficulty. P-values of <0.05 were considered statistically significant at 95% confidence interval.
Results
Of the 255 participants enumerated for this study, 251 participants completed the study and were analysed (response rate of 98.4%). Majority of the participants were in the age range of 40 – 49 years (55.0%) with an overall mean age of 43.9 ± 6.5 years as shown in [Table 1]. There were more female than male participants, with a male to female ratio of 1:6.4.
Table 1.
Socio-Demographic Characteristics of Participants
| Variable | Frequency (n = 251) | Percentage |
|---|---|---|
| Age group (Years) | ||
| 30 - 39 | 64 | 25.5 |
| 40 - 49 | 138 | 55.0 |
| ≥ 50 | 49 | 19.5 |
| Total | 251 | 100.0 |
| Mean ± SD | 43.92 ± 6.5 | |
| Gender | ||
| Male | 34 | 13.5 |
| Female | 217 | 86.5 |
| Total | 251 | 100.0 |
| Marital status | ||
| Single | 9 | 3.6 |
| Married | 227 | 90.4 |
| Widow /widower | 10 | 4.0 |
| Divorced | 3 | 1.2 |
| Separated | 2 | 0.8 |
| Total | 251 | 100.0 |
| Level of education | ||
| None | 7 | 2.8 |
| Primary | 34 | 13.5 |
| Secondary | 192 | 76.5 |
| Tertiary | 18 | 7.2 |
| Total | 251 | 100.0 |
One hundred and sixty-nine participants (67.3%) where presbyopic and among these, 129 had no near correction with a magnitude of uncorrected presbyopia of 76.3. The mean age of presbyopes was 46.3 ± 5.0 years. On multivariate logistic regression, only age had a significant relationship with presbyopia. Participants 50 years and above, and within 40 - 49 years were thirty times (OR = 29.97 CI 10.25 - 81.91; P < 0.001) and twenty-eight times (OR = 28.14, CI 12.91- 65.79; P < 0.001) respectively more likely to have presbyopia as displayed in [Table 2].
Table 2.
Association between Presbyopia and Socio-Demographic Characteristics of the Participants
| Bivariate | Multivariate | |||
|---|---|---|---|---|
|
|
|
|||
| Odd ratio (95% CI) | p-value | Odd ratio (95% CI) | p-value | |
| Age group (Years) | ||||
| 30 – 39 (n=64) | 1 | 1 | ||
| 40 – 49 (n=138) | 17.21(14.4-20.3) | <0.001* | 28.14(12.91-65.79) | <0.001* |
| ≥ 50 (n=49) | 16.93(13.2-18.7) | <0.001* | 29.97(10.25-81.91) | <0.001* |
| Gender | ||||
| Male (n=34) | 1 | 1 | ||
| Female (n=217) | 0.92(0.9-1.3) | 0.663 | 0.92(0.9-1.3) | 0.591 |
| Marital status | ||||
| Single (n=9) | 1 | 1 | ||
| Married (n=227) | 3.39(1.7-5.1) | 0.043* | 1.91(0.75-4.81) | 0.173 |
| Widow /widower (n=10) | 7.58(2.5-10.3) | 0.023* | 2.94(0.30-5.01) | 0.311 |
| Divorced (n=3) | 4.15(2.19-6.4) | 0.018* | 2.20(0.21-3.91) | 0.402 |
| Separated (n=2) | 2.03(0.9-3.5) | 0.032* | 2.37(0.41-5.30) | 0.219 |
| Level of education | ||||
| None (n=7) | 1 | 1 | ||
| Primary (n=34) | 0.83(0.7-1.9) | 0.669 | 0.83(0.7-1.9) | 0.721 |
| Secondary (n=192) | 0.88(0.6-1.5) | 0.732 | 0.88(0.6-1.5) | 0.486 |
| Tertiary (n=18) | 1.08(0.8-1.6) | 0.351 | 1.08(0.8-1.6) | 0.222 |
* Statistically significant,
Forty out of 251 participants had spectacle corrected near vision of at least N8, giving a met presbyopic need of 15.9%. Fifty percent (12) of the male participants had spectacle correction as compared to 19% (28) of female with corrected near vision. One hundred and twenty-nine participants could not read N8 at 40 cm due to uncorrected presbyopia, giving an unmet need of 51.4%. Therefore, the presbyopia correction coverage was 23.7%.
The reported source of near correction spectacles included, the eye clinic (23.9%), primary health centre (21.7%), market (21.7%), church (10.9%), roadside shops (6.5%), and optical/optometrist centres (4.3%). The main barrier to the use of near spectacle correction among study participants was cost (43.0%) as shown in [Table 3].
Table 3.
Barriers to the use of Near Vision Spectacles
| Variable | Frequency *(n = 121) | Percentage |
|---|---|---|
| Barriers to the use of spectacles | ||
| Lack of money | 52 | 43.0 |
| Not a priority | 46 | 38.0 |
| Don’t know where to go | 11 | 9.1 |
| Services are too far | 8 | 6.6 |
| Lost/broken/stolen | 6 | 5.0 |
| Stigmatization | 3 | 2.5 |
| Not cosmetically acceptable | 2 | 1.7 |
*Multiple response answer
In evaluating the effect of near vision on work and productivity, 86 (82.7%) of the presbyopic participants reported that it took a longer time to finish their tasks compared to 18 (17.3%) of non-presbyopes. Also, 48 (81.4%) of the presbyopic participants reported a change in their main task due to difficulty with their near vision as compared to 11 (18.6%) of non-presbyopes.
Half of the participants reported moderate difficulty with their NVQoL (50.2%) while just a few of the participants reported that there was no difficulty (4.4%) with their NVQoL. There was a statistically significant association (p<0.001) between increasing age and difficulty in NVQoL, as almost half of the participants above 50 years reported severe difficulty with their near vision as shown in [Table 4]. Also, 10.1% of female participants reported severe difficulty with near vision related QOL compared to males (8.8%).
Table 4.
Association between Near-vision related Quality of life and Socio-Demographic Characteristics of the Participants
| No difficulty (n = 11) | Some difficulty (n = 89) | Moderate difficulty (n = 126) | Severe difficulty (n = 25) | Fisher exact | p-value | |
|---|---|---|---|---|---|---|
| Age group (Years) | ||||||
| 30 - 39 | 8(12.5) | 42(65.6) | 14(21.9) | 0(0.0) | 19.903 | < 0.001* |
| 40 - 49 | 3(2.2) | 43(31.2) | 87(63.0) | 5(3.6) | ||
| ≥ 50 | 0(0.0) | 4(8.2) | 25(51.0) | 20(40.8) | ||
| Total | 11(4.4) | 89(35.5) | 126(50.1) | 25(10.0) | ||
| Gender | ||||||
| Male | 3(8.8) | 1(2.9) | 27(79.5) | 3(8.8) | 14.501 | < 0.001* |
| Female | 8(3.7) | 88(40.6) | 99(45.6) | 22(10.1) | ||
| Total | 11(4.4) | 89(35.5) | 126(50.1) | 25(10.0) | ||
| Marital status | ||||||
| Single | 1(11.1) | 3(33.3) | 5(55.6) | 0(0.0) | 12.073 | 0.071 |
| Married | 10(4.4) | 81(35.7) | 114(50.2) | 22(9.7) | ||
| Widow | 0(0.0) | 0(0.0) | 7(70.0) | 3(30.0) | ||
| Divorced | 0(0.0) | 3(100.0) | 0(0.0) | 0(0.0) | ||
| Separated | 0(0.0) | 2(100.0) | 0(0.0) | 0(0.0) | ||
| Total | 11(4.4) | 89(35.5) | 126(50.1) | 25(10.0) | ||
| Level of education | ||||||
| None | 0(0.0) | 3(42.9) | 4(57.1) | 0(0.0) | 9.491 | 0.132 |
| Primary | 2(5.9) | 14(41.2) | 14(41.2) | 4(11.7) | ||
| Secondary | 8(4.2) | 71(37.0) | 97(50.5) | 16(8.3) | ||
| Tertiary | 1(5.6) | 1(5.6) | 11(61.0) | 5(27.8) | ||
| Total | 11(4.4) | 89(35.5) | 126(50.1) | 25(10.0) |
* Statistically significant
Eighty-four percent of presbyopic participants reported severe difficulty with their near-vision related QoL compared to 16.0% of non-presbyopes. This association between presbyopia and NVQoL was statistically significant (P < 0.001) as shown in [Table 5].
Table 5.
Association between Presbyopia and Near-vision related Quality of life of the Participants
| Presbyopia | X2 | p-value | ||
|---|---|---|---|---|
|
| ||||
| Present (n = 169) | Absent (n = 82) | |||
| Near-vision related quality of life | ||||
| No difficulty (≥ 90) | 1(9.1) | 10(90.9) | 42.126† | <0.001* |
| Some difficulty (70 - 89) | 45(50.6) | 44(49.4) | ||
| Moderate difficulty (50 - 69) | 102(81.0) | 24(19.0) | ||
| Severe difficulty (< 50) | 21(84.0) | 4(16.0) | ||
| Total | 169(67.3) | 82(32.7) | ||
* statistically significant, †fisher’s exact test, X2 Chi-square
On multivariate logistic regression, there was a correlation with increasing age, being presbyopic and the severity of NVQoL. Participants aged 40 - 49years (OR = 1.96, CI 1.12–2.10; P = 0.043) and above 50years (OR = 2.35, CI 1.90–5.40; P = 0.021) were two times more likely to have difficulty NVQoL as shown in [Table 6]. Presbyopic participants (OR = 3.04, CI 1.34 - 6.50; P = 0.003) were three times more likely to report severe difficulty with NVQoL compared with non-presbyopes as shown in [Table 6].
Table 6.
Logistic regression showing independent predictor of severe difficulty Near-vision related quality of life
| Odd ratio | 95% CI | p-value | |
|---|---|---|---|
| Age group (Years) | |||
| 30 – 39 (n=64) | 1 | ||
| 40 – 49 (n=138) | 1.96 | 1.13 - 2.10 | 0.043* |
| ≥ 50 (n=49) | 2.35 | 1.90 - 5.40 | 0.021* |
| Gender | |||
| Male (n=34) | 1 | ||
| Female (n=217) | 2.96 | 0.73 - 11.99 | 0.128 |
| Presbyopia | |||
| No (n=82) | 1 | ||
| Yes (n=169) | 3.04 | 1.34 - 6.50 | 0.003* |
*Statistically significant
On post-assessment, 80.2%(97) of the participants reported no restriction in work and productivity compared to 36.4%(44) participants pre-assessment. Also,19% (23) of presbyopic participants reported moderate difficulty with their vision during the post-assessment compared with 66.9%(81) pre-assessment as shown in [Figure 1]. There was a correlation (P < 0.001) between correction of presbyopia and NVQoL of life after 3 month of follow up as shown in [Figure 1].
Figure 1.
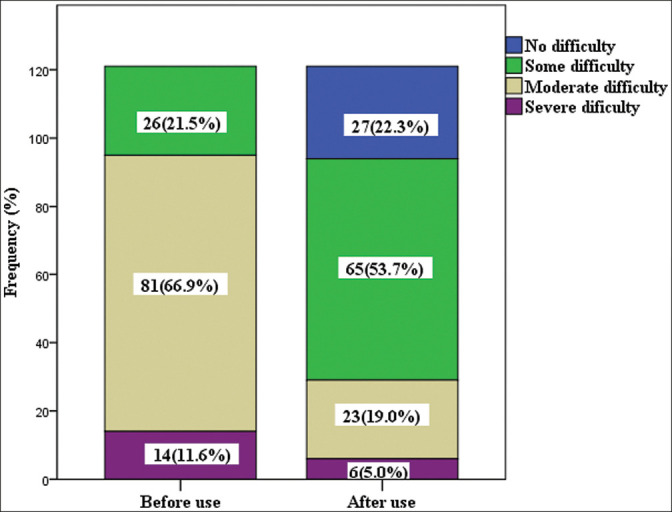
Impact of Corrected Presbyopia on Quality of life among participants. X2 = 79.260, P < 0.001*
Discussion
The prevalence of presbyopia in this current study was 67.3%. This is comparable to the findings of a study conducted in India among cloth weavers where the prevalence of presbyopia was 61.8%.[18] and also a community-based study in Tanzania which reported a prevalence of 61.7%.[12] It was, however, higher than the prevalence reported in a population-based study in northwest, Nigeria (30.4%).[10] and another in Ghana (2%).[8] among hairdressers. The disparity in age and differences in near vision requirements of this study population could have accounted for this difference.
Presbyopia is an age related condition with an onset from 40 years, which corresponds to the productive age of an individual.[1,2] This is in tandem with the findings in this current study as the mean age of presbyopic participants was 46years. On bivariate analysis there was a statistically significant association between increasing age and prevalence of presbyopia with the lowest prevalence among participants aged 30–39 years. This was similar to results from other studies in China,[19] India,[20] Tanzania,[12] and Nigeria,[21] which showed that presbyopia was significantly associated with increasing age. The odds of having presbyopia was 30 times more in older age group. This finding further reiterates the fact that presbyopia is an age-related condition whose prevalence increases with the proportion of aged population.
Presbyopia spectacle correction coverage (PSCC) signifies the percentage of people who can benefit positively from the spectacles.[22] Some studies have reported the factors that may influence PSCC which include age of participants, definition of terms used (functional or objective presbyopia) services provision, services uptake, socioeconomic status and gender (worse among females).[22,23,24] In this current study, PSCC was 23.7%, with met need in just one sixth, and an unmet need in half of the participants studied. Also, half of the male participants as compared to less than 1/4th of the female had spectacle correction. This could be as a result of poor health seeking habbit of women as compared to men.[23] Moreover, women in developing countries are dependent on men for their livelihood.[23] Therefore, the high unmet need in this study maybe explained by the higher percentage of female participants.
The PSCC, met needs and unmet needs in this present study correlates with the study conducted in Abuja[13] that found PSCC of 21% with met need in less than one sixth, and an unmet need in about half of the participants. In the same vein, another study in Ogun State,[24] reported 28.4% for PSCC, with met need in just above one fifth and unmet need in more than half of the participants studied. The similarities in the findings could be partly due to the relatively low socioeconomic status of the participants studied. Conversely, PSCC in this study was lower than the result from the observation in Ilorin.[9] with a PSCC of 46.7% and higher than the findings from Zamfara[7] which reported a low PSCC (0.7%). While the findings from Ilorin may be partially attributed to the existing eye care program in the state, the disparity with the study from Zamfara may be as a result of low level of literacy among the study population in the Zamfara study as compared to our study.
The main barriers to the use of near vision spectacles found in this study were cost in over two-fifth of the presbyopic participants and ‘not being a priority’ in over a third of the presbyopic subjects studied. This corroborates with findings from other studies such as that carried out in Abuja[25] in which more than half of the barriers studied was due to cost and spectacle not being a priority accounted for just about one–fifth. In a study in Enugu,[26] two-fifth of the barriers studied were due to lack of felt need and cost. Financial constraint was a common barrier in all these studies. It can be deduced from these findings that spectacles should be made affordable to increase near vision spectacle coverage which will invariably reduce the burden of uncorrected presbyopia.
Good near vision is of paramount importance even among individuals who use it for tasks other than reading and writing.[10] In our study however, almost half of the presbyopic participants reported a change in main work (such as exclusion of some previously carried out work activities) due to poor near vision. On the other hand only one-fifth of the non-presbyopes reported interference in their main work. This may be due to the fact that most of their work are done at a close range. There was a statistically significant association between uncorrected presbyopia and reduced NVQoL amongst cosmetologists This mirrors the findings reported in China,[15] Tanzania,[6] and Abuja.[25]
There was a threefold increase in the odds of reporting severe difficulty with performing near task among presbyopic participants. This corroborates with the findings by Chiroma et al.[25] where presbyopes reported threefold increase in dependence on other people in carrying out their near task, due to reduction in near vision as compared to non-presbyopes. In addition, Ilesh et al.[11] observed that the degree of presbyopia was associated with increased difficulty with daily tasks and being presbyopic led to an eightfold increase in reporting severe difficulty with daily tasks. Although not significant on multivariate analysis, but in univariate analysis, females participants in our study were more likely than males to report being unsatisfied with their near work, as seen in a Tanzanian[6] study on the impact of presbyopia on quality of life. This finding, along with that seen in other studies further buttresses the possibilities that women are more likely to report challenges with presbyopia.[11,12,20]
There was a significant improvement in NVQoL after intervention with only about a quarter of the participants reporting moderate difficulty with NVQoL compared with more than half before the intervention, with a significant increase in work and productivity. Nadioo et al.[6] and Reddy et al.[27] reported similar findings in improvement on work productivity with near vision spectacle correction. Laviers et al.[28] also reported a significant improvement in quality of life after intervention with majority of the participants willing to recommend use of near vision spectacle to other people who have difficulty with their near vision. This emphasises the need to prioritize eye care services among this cadre of people studied.
The present study is not without its limitations. The subjective assessment of work and productivity activities may have introduced some recall bias. In addition, participants’ response may have been biased by the notion of receiving free eye tests as well as free near-vision spectacles. This was minimized by giving the spectacles at the end of the study. However, the standardised examination procedures, the high response rate (98.2%), and reassessment of the impact of the spectacle provided on quality of life were the strengths of this study.
In conclusion, this current study shows a relatively high prevalence of presbyopia, high unmet need, and low spectacle coverage among cosmetologists in Mushin LGA of Lagos State. Furthermore, this study demonstrated the impact of uncorrected presbyopia on work and productivity as well as reduced NVQoL among cosmetologists. It also highlights the need to provide affordable and accessible, near vision spectacles as well as services not only to the literates, but also to populations where though reading is uncommon, other forms of near-related activities and work are commonly performed.
Financial support and sponsorship
None
Conflict of interest
Authors do not have any financial interests or conflicting relationships related to the manuscript.
Previous presentation
This paper is part of a dissertation submitted to the West African College of Surgeons in part fulfilment of the award of Fellowship of the West African College of Surgeons (Ophthalmology) in October 2020.
Acknowledgement
We acknowledge the cooperation of the Cosmetologists in Mushin LGA of Lagos state and especially the leaders of the association for their participation and cooperation throughout this study.
References
- 1.Care of the patient with presbyopia. In: Mancil GL, Bailey IL, Brookman KE, Campbell BJ, Cho MH, Rosenbloom AA, et al., editors; Heath D, editor. Optometric Clinical Practiceguideline. Third. St. Louis: American Optometric Association; 2010. pp. 1–12. [Google Scholar]
- 2.Malu KN. Presbyopia in Plateau state, Nigeria: A hospital study. J Med Trop. 2013;15:151–5. [Google Scholar]
- 3.Hickenbotham A, Roorda A, Steinmaus C, Glasser A. Meta-analysis of sex differences in presbyopia. Invest Ophthalmol Vis Sci. 2012;53:3215–20. doi: 10.1167/iovs.12-9791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fricke TR, Tahhan N, Resnikoff S, Papas E, Burnett A, Ho SM, et al. Global prevalence of presbyopia and vision impairment from uncorrected presbyopia: Systematic review, meta-analysis, and modelling. Ophthalmology. 2018;125:1492–9. doi: 10.1016/j.ophtha.2018.04.013. [DOI] [PubMed] [Google Scholar]
- 5.Papadopoulos PA, Papadopoulos AP. Current management of presbyopia. Middle East Afr J Ophthalmol. 2014;21:10–7. doi: 10.4103/0974-9233.124080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Naidoo KS, Jaggernath J, Chinanayi FS, Chan VF. Near vision correction and work productivity among textile workers. Afr Vision Eye Health. 2016;75:357–9. [Google Scholar]
- 7.Patel I, West SK. Presbyopia: Prevalence, impact, and interventions. Community Eye Health. 2007;20:40–1. [PMC free article] [PubMed] [Google Scholar]
- 8.Kumah DB, Abdul-Kabir M, Aidoo F, Nuo-Ire Kuutiero IW, Ablordeppey RK, Merepa SS, et al. Prevalence of ocular conditions among hairdressers in the Kumasi metropolis. Ghana BAOJ Ophthalmol. 2017;1:11–12. [Google Scholar]
- 9.Omokhodion FO, Balogun MO, Ola-Olorun FM. Reported occupational hazards and illnesses among hairdressers in ibadan, southwest nigeria. West Afr J Med. 2009;28:20–3. doi: 10.4314/wajm.v28i1.48419. [DOI] [PubMed] [Google Scholar]
- 10.Umar MM, Muhammad N, Alhassan MB. Prevalence of presbyopia and spectacle correction coverage in a rural population of North West Nigeria. Clin Ophthalmol. 2015;9:1195–201. doi: 10.2147/OPTH.S81194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patel I, Munoz B, Burke AG, Kayongoya A, McHiwa W, Schwarzwalder AW, et al. Impact of presbyopia on quality of life in a rural African setting. Ophthalmology. 2006;113:728–34. doi: 10.1016/j.ophtha.2006.01.028. [DOI] [PubMed] [Google Scholar]
- 12.Burke AG, Patel I, Munoz B, Kayongoya A, McHiwa W, Schwarzwalder AW, et al. Population-based study of presbyopia in rural tanzania. Ophthalmology. 2006;113:723–7. doi: 10.1016/j.ophtha.2006.01.030. [DOI] [PubMed] [Google Scholar]
- 13.Muhammad R, Jamda M, Langnap L. Prevalence of presbyopia in rural Abuja, Nigeria. Ann Niger Med. 2015;9:56–58. [Google Scholar]
- 14.Naing L, Winn T, Rusli BN. Practical issues in calculating the sample size for prevalence studies. Archives of Orofacial Sciences. 2006;1:9–14. [Google Scholar]
- 15.Lu Q, Congdon N, He X, Murthy GV, Yang A, He W. Quality of life and near vision impairment due to functional presbyopia among rural chinese adults. Invest Ophthalmol Vis Sci. 2011;52:4118–23. doi: 10.1167/iovs.10-6353. [DOI] [PubMed] [Google Scholar]
- 16.WHO. Spectacle and Work Productivity Questionnaire. [Last accessed on 2020 Jan 12]. Available at http://www.vision2020.org/documents/Committee%20documents/Refractive%20Error/REPComStrategy.doc .
- 17.Idowu OO, Aribaba OT, Onakoya AO, Rotimi-Samuel A, Musa KO, Akinsola FB. Presbyopia and near spectacle correction coverage among public school teachers in Ifo Township, South-West Nigeria. Niger Postgrad Med J. 2016;23:132–6. doi: 10.4103/1117-1936.190342. [DOI] [PubMed] [Google Scholar]
- 18.Marmamula S, Narsaiah S, Shekhar K, Khanna RC. Presbyopia, spectacles use and spectacle correction coverage for near vision among cloth weaving communities in Prakasam district in South India. Ophthalmic Physiol Opt. 2013;33:597–03. doi: 10.1111/opo.12079. [DOI] [PubMed] [Google Scholar]
- 19.Lu Q, He W, Murthy GV, He X, Congdon N, Zhang L, et al. Presbyopia and near-vision impairment in rural Northern China. Invest Ophthalmol Vis Sci. 2011;52:2300–5. doi: 10.1167/iovs.10-6569. [DOI] [PubMed] [Google Scholar]
- 20.Nirmalan PK, Krishnaiah S, Shamanna BR, Rao GN, Thomas R. A population-based assessment of presbyopia in the state of Andhra Pradesh, South India: The Andhra Pradesh eye disease study. Invest Ophthalmol Vis Sci. 2006;47:2324–8. doi: 10.1167/iovs.05-1192. [DOI] [PubMed] [Google Scholar]
- 21.Obajolowo TS, Owoeye JFA, Adepoju FG. Prevalence and pattern of prebyhopia in a rural Nigerian community. J West African Coll Surg. 2016;6:83–04. [PMC free article] [PubMed] [Google Scholar]
- 22.Marmamula S, Madala SR, Rao GN. Prevalence of uncorrected refractive errors, presbyopia and spectacle coverage in marine fishing communities in South India: Rapid assessment of visual impairment (Ravi) project. Ophthalmic Physiol Opt. 2012;32:149–55. doi: 10.1111/j.1475-1313.2012.00893.x. [DOI] [PubMed] [Google Scholar]
- 23.Muhammad R, Jamda M. Presbyopic correction coverage and barriers to the use of near vision spectacles in rural Abuja, Nigeria. Sub-Saharan African Journal of Medicine. 2016;3:20–4. [Google Scholar]
- 24.Ajibode HA, Fakolujo VO, Onabolu OO, Jagun O, Ogunlesi TA, Abiodun OA. A community-based prevalence of presbyopia and spectacle coverage in Southwest Nigeria. J West Afr Coll Surg. 2016;6:66–82. [PMC free article] [PubMed] [Google Scholar]
- 25.Chiroma MR, Jamda AM. Impact of uncorrected presbyopia on the quality of Life in rural Gwagwalada, Nigeria. J Community Med Prim Health Care. 2017;29:68–73. [Google Scholar]
- 26.Uche JN, Ezegwui IR, Uche E, Onwasigwe EN, Umeh RE, Onwasigwe CN. Prevalence of presbyopia in a rural African community. Rural Remote Health. 2014;14:2731. [PubMed] [Google Scholar]
- 27.Reddy PA, Congdon N, MacKenzie G, Gogate P, Wen Q, Jan C, et al. Effect of providing near glasses on productivity among rural Indian tea workers with presbyopia. Lancet Glob Health. 2018;6:1019–27. doi: 10.1016/S2214-109X(18)30329-2. [DOI] [PubMed] [Google Scholar]
- 28.Laviers HR, Omar F, Jecha H, Kassim G, Gilbert C. Presbyopic spectacle coverage, willingness to pay for near correction, and the impact of correcting uncorrected presbyopia in adults in Zanzibar, East Africa. Invest Ophthalmol Vis Sci. 2010;51:1234–41. doi: 10.1167/iovs.08-3154. [DOI] [PubMed] [Google Scholar]


