Abstract
PURPOSE OF REVIEW:
Seizure disorders are the most frequent major neurologic complication in pregnancy, affecting 0.3% to 0.8% of all gestations. Women of childbearing age with epilepsy require special care related to pregnancy. This article provides up-to-date information to guide practitioners in the management of epilepsy in pregnancy.
RECENT FINDINGS:
Ongoing multicenter pregnancy registries and studies continue to provide important information on issues related to pregnancy in women with epilepsy. Valproate poses a special risk for malformations and cognitive/behavioral impairments. A few antiseizure medications pose low risks (eg, lamotrigine, levetiracetam), but the risks for many antiseizure medications remain uncertain. Although pregnancy rates differ, a prospective study found no difference in fertility rates between women with epilepsy who were attempting to get pregnant and healthy controls. During pregnancy, folic acid supplementation is important, and a dose greater than 400 mcg/d during early pregnancy (ie, first 12 weeks) is associated with better neurodevelopmental outcome in children of women with epilepsy. Breastfeeding is not harmful and should be encouraged in women with epilepsy even when they are on antiseizure medication treatment.
SUMMARY:
Women with epilepsy should be counseled early and regularly about reproductive health. Practitioners should discuss the risks of various obstetric complications; potential anatomic teratogenicity and neurodevelopmental dysfunction related to fetal antiseizure medication exposure; and a plan of care during pregnancy, delivery, and postpartum. Women with epilepsy should also be reassured that the majority of pregnancies are uneventful.
INTRODUCTION
Epilepsy is one of the most common chronic neurologic conditions, estimated to affect almost 70 million people worldwide.1 The prevalence is similar in females andmales (46.2 per 100,000 compared to 50.7 per 100,000).2 In the United States, 1.2%of the population have an active diagnosis of epilepsy,3 including more than one-half million women of childbearing age.4 In fact, epilepsy is one of the most common neurologic disorders that usually requires continuous treatment throughout pregnancy. This article reviews fertility and contraception in women with epilepsy, the maternal outcomes of women with epilepsy, malformation and cognitive outcomes of children of women with epilepsy, postpartum management (including breastfeeding), and suggested counseling for women of childbearing age.
FERTILITY
Studies on birth rate in patients diagnosed with epilepsy have had conflicting results.5–7 Some have indicated that the birth rate is lower in patients with epilepsy than in the general population. In a population-based study in Finland with a mean follow-up time of 9 years, the birth rate was lower in patients with epilepsy than in the reference cohort among both men (hazard ratio 0.58; 95% confidence interval, 0.54 to 0.62) and women (hazard ratio 0.88; 95% confidence interval, 0.83 to 0.93).5 However, the lower birth rate does not mean lower fertility. The stigma related to epilepsy is known to affect interpersonal relationships, marital status, economic status, and the desire to get pregnant; hence, these psychosocial factors should be considered. A 2018 prospective observational trial that compared women with epilepsy without a preexisting diagnosis of infertility who were attempting to get pregnant and a control group of similar age demonstrated no difference in pregnancy rate (60.7% versus 60.2%, respectively) and time to achieve pregnancy (6 months versus 9 months, respectively) at 1 year.8 This is probably applicable to the common clinical scenario in which women with epilepsy who are thinking about getting pregnant seek information from a neurologist, although nearly all patients in the study were on either lamotrigine or levetiracetam monotherapy and the influence of antiseizure medications on fertility was not further addressed. The class of antiseizure medication and whether or not patients are on antiseizure medication polytherapy has been associated with impaired fertility. A prospective study in India found that polypharmacy of more than three antiseizure medications and the use of phenobarbital were associated with impaired fertility.9 In this study, half of the women with epilepsy receiving phenobarbital were unable to conceive over several years of attempt. US Epilepsy Birth Control Registry data from 2019 have also shown that the live birth to pregnancy ratio was higher with the use of lamotrigine (89.1%) than valproate (63.3%).10 The association of certain antiseizure medications and increased infertility risk has been raised, but it is worth studying in a larger group of women with epilepsy.
CONTRACEPTION AND FAMILY PLANNING
Family planning allows women with epilepsy of childbearing age to attain their desired number of children and timing of intervals between births. More than half of the pregnancies (55% to 65%) in women with epilepsy in the United States were unintended,11,12 which is similar to unplanned pregnancies in the general population (45% to 51%).12 A well-planned pregnancy can reduce the likelihood of seizure recurrence during pregnancy and delivery. Studies from the general population have shown that unplanned pregnancies may be associated with poor fetal and maternal outcomes, such as preterm delivery and low birth weight.13 In addition, spontaneous fetal loss was found to be 2 times more common in unplanned pregnancies (137 out of 391 patients, 35%) than in planned pregnancies (43 out of 262 patients, 16.4%) in women with epilepsy.14 Also, although many women desire pregnancy, some may prefer never to become pregnant or may want to delay for various reasons. Hence, contraception and family planning are important topics when counseling women with epilepsy in clinical practice.
Forms of Contraception
Many forms of contraception are available to women with epilepsy. The most common reversible contraceptive methods include oral contraceptives, the dermal patch, depot medroxyprogesterone acetate injection, vaginal rings that contain hormonal steroids with combined progesterone and estrogen or progesterone alone, copper T intrauterine device (IUD) or levonorgestrel IUD, spermicides, and mechanical barriers such as condoms or a diaphragm. Generally speaking, long-acting reversible contraceptives such as contraceptive implants and IUDs have the lowest contraceptive failure rates of around 1%. The least effective methods are condoms, withdrawal, and fertility awareness–based methods, which have the highest risk of contraceptive failure (ranging from 13% to 20%). The failure rate for all hormonal contraceptive methods combined has been reported to range from 6% to 9% in the general population (TABLE 2-1).15
TABLE 2–1.
Contraceptive Effectivenessa
| Contraceptive method | Risk of contraceptive failureb |
|---|---|
| Tier 1 (most effective methods) | |
| Intrauterine device or implant | 1.4% |
| Tier 2 (moderately effective methods) | |
| Hormonal contraceptives (progesterone-only or combined contraceptives) | |
| Injectable form | 4.0% |
| Oral form | 7.2% |
| Tier 3 (least effective methods) | |
| Male condom | 12.6% |
| Withdrawal | 19.9% |
Data from Sundaram, et al., Perspect Sex Reprod Health.15
Contraceptive failure rates are from the general population assuming typical use, and no drug-drug interactions were considered; the percentage for risk of contraceptive failure was calculated based on the data from the 2006–2010 National Survey of Family Growth in the United States.15
Interaction of Antiseizure Medication and Oral Contraceptives
Oral hormonal contraceptives are almost exclusively absorbed through the intestines, and many of them are metabolized to an inactive compound by the cytochrome P450 P3A4 (CYP3A4) enzyme. Antiseizure medications that are CYP3A4 enzyme inducers accelerate hepatic metabolism of both the estrogenic and progestogenic components of systemic hormonal contraceptives. They decrease the duration and intensity of contraceptives’ efficacy by reducing their circulating levels and cause potential contraceptive failure (TABLE 2-216). This occurs with phenytoin, phenobarbital, and carbamazepine, which are potent CYP3A4 inducers. Several of the newer antiseizure medications, such as oxcarbazepine, topiramate, and felbamate, are less potent CYP3A4 inducers, and some of them may have different effects on the estrogenic and progestogenic components. For example, felbamate predominantly induces metabolism of the progestin component. In a randomized study of healthy women who were taking a low dose of combination oral contraceptive containing 30 mcg ethinyl estradiol and 75 mcg gestodene, treatment with 2400 mg/d felbamate resulted in 42%decrease in the area under the plasma concentration-time curve (AUC) of gestodene (a synthetic progestogen), whereas a clinically relevant effect was not observed for ethinyl estradiol.17 On the other hand, topiramate has a selective role in reducing ethinyl estradiol levels but has no significant effect on the progestin component of oral contraceptives. Topiramate also acts in a dose-dependent manner; when patients were given a low dose of 50 mg/d to 200 mg/d, the ethinyl estradiol AUC reduced 11% to 12%, but when patients were given a higher dose of 400 mg/d, the ethinyl estradiol AUC reduced 22%.18,19 It is unclear how much decrease of either estrogen or progestin level results in contraceptive failure, since both components are important for preventing pregnancy: estrogen suppresses ovulation, and progestin facilitates cervical mucus thickening to prevent sperm passage. The authors usually recommend that women with epilepsy who are concomitantly using an enzyme-inducing antiseizure medication and an oral contraceptive should use a high-dose contraceptive that contains at least 50 mcg of ethinyl estradiol and should use an additional form of contraception such as condoms with spermicide or an intrauterine device.16 Levonorgestrel IUDs are suitable for use as efficacy is maintained, but the progesterone-only pill, progestin/progesterone implants, combined contraceptive patches, and vaginal ring are not recommended because of reduced efficacy.20
TABLE 2–2.
Interaction of Hormonal Contraceptives and Antiseizure Medications
| Antiseizure medication | Considerations of concomitant use of hormonal contraceptives |
|---|---|
| Enzyme-inducing | |
| Phenytoin, phenobarbital, primidone, carbamazepine, eslicarbazepine acetate, oxcarbazepine, rufinamide, topiramate (≥200 mg/d), perampanel (≥12 mg/d), cenobamate, felbamate | Consider high-dose contraceptives that contain at least 50 mcg ethinyl estradiol If treated with depot medroxyprogesterone acetate injections, they should be given at more frequent intervals (10-week interval rather than 12-week interval)16 Additional form of contraception method should be considered Progesterone-only pill, progestin implant, combined contraceptive patches, and vaginal ring are not recommended because of reduced efficacy Intrauterine devices are not affected by antiseizure medications |
| Non-enzyme-inducing | |
| Acetazolamide, brivaracetam, cannabidiol, clobazam, clonazepam, ethosuximide, gabapentin, lacosamide, levetiracetam, lamotrigine, pregabalin, sodium valproate, stiripentol, tiagabine, vigabatrin, zonisamide | These antiseizure medications do not alter the effectiveness of hormonal contraceptives Lamotrigine levels are decreased 40–60% by ethinyl estradiol/levonorgestrel, which could potentially cause breakthrough seizures; lamotrigine levels should be monitored, and dose may need to be increased if indicated |
Antiseizure medications that do not induce CYP3A, such as lamotrigine, levetiracetam, and zonisamide (TABLE 2-2), are not expected to affect hormonal contraceptives with significant impact. Of note, although progestogens do not alter lamotrigine serum concentrations, the estrogenic component of oral contraceptives induces glucuronidation pathways, which results in a 40% to 60% decrease in lamotrigine level, potentially causing breakthrough seizures. This effect is transient, and lamotrigine levels increase during the hormone-free week of the cycle when not taking the active contraceptive. Patients may experience toxic symptoms during the hormone-free week since they often need higher doses during the active contraceptive period. However, some women with epilepsy on lamotrigine may achieve effective levels during the active contraceptive period and not become toxic during the placebo pill phase. To address this interaction, dose adjustments of lamotrigine should be considered based on the serum level before and after contraceptives are added, or alternative methods, such as an intrauterine device, should be discussed. Knowledge regarding the interaction of oral contraceptives and some of the newest antiseizure medications, such as cannabidiol and fenfluramine, is limited. Cannabidiol is a known CYP3A inhibitor and theoretically should not reduce the estrogenic and progestogenic level, but no studies have been completed thus far. Clinical trials are currently under way to address this question.
MATERNAL AND OBSTETRIC OUTCOMES IN WOMEN WITH EPILEPSY
Seizure disorders are the most frequent major neurologic complication in pregnancy, affecting 0.3% to 0.8% of all gestations.21,22 Approximately 1.3 million women with epilepsy in the United States are in their active reproductive years, and approximately 25,000 infants are born to women with epilepsy each year.23 In general, more than 90% of pregnancies in women with epilepsy result in a normal delivery without any apparent complications.22 However, women with epilepsy are often considered at high risk in pregnancy because of increased obstetric and fetal risks, and maternal mortality is 10 times higher in women with epilepsy than in the general population.24 Women with epilepsy face particular challenges during their pregnancies, including spontaneous abortion, antepartum hemorrhage, gestational hypertension, preeclampsia, breech position, induction of labor, cesarean delivery, and preterm birth.4,25
Seizure Frequency During Pregnancy
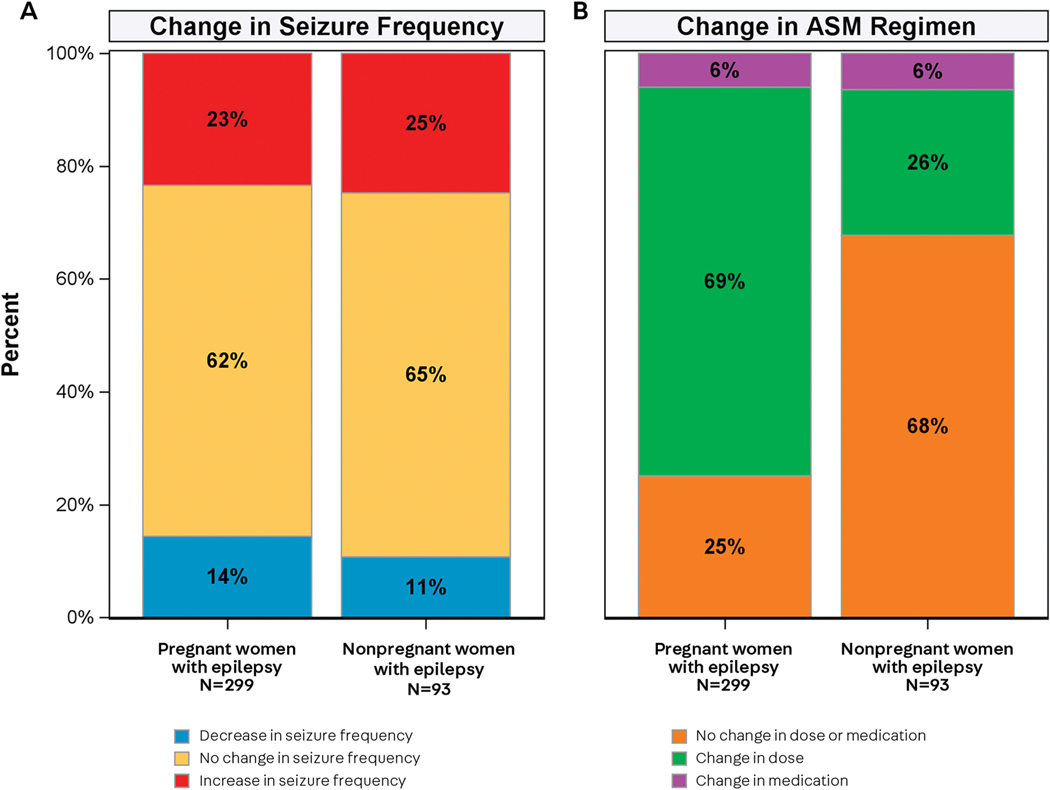
Convulsions are dangerous to women with epilepsy not only because of the risk of seizure-related falls and blunt trauma but also because of potential harm to the fetus from the possibility of hypoxemia and asphyxia. Focal seizures that do not evolve to convulsions are thought unlikely to have a major impact on the fetus, but anecdotal evidence indicates that they may cause transient fetal distress, with fetal heart rate deceleration for up to 2.5 minutes.26 The fundamental reason that women with epilepsy are continuously treated with antiseizure medications throughout pregnancy is to avoid recurrence of seizure activity and its related adverse effects. Seizure burden may increase during labor and delivery, but this occurs in no more than 1% to 2% of pregnancies in women with epilepsy. Most women with epilepsy will not experience a change in the frequency of seizures during pregnancy.27 A recent prospective study in the United States showed that about two-thirds (62%) of women with epilepsy had no change of seizure frequency during pregnancy, which was similar to the number (65%) observed in the control group of nonpregnant women with epilepsy over the same time period. In the study cohort, the percentage of pregnant women with epilepsy who had a higher incidence of seizures during pregnancy than during the postpartum period was also similar to that of women with epilepsy who were not pregnant during the corresponding time period (23% versus 25%).28 The pregnant women with epilepsy in this cohort had more frequent changes in doses of antiseizure medication than nonpregnant women with epilepsy during similar time periods (74% versus 31%), suggesting that close antiseizure medication dose monitoring is important for patients during pregnancy to maximize seizure control because of antiseizure medication clearance changes during pregnancy (FIGURE 2-1).
FIGURE 2–1.
Changes in seizure frequency and antiseizure medication dose. A, Changes in the frequency of seizures that impair awareness in women during pregnancy as compared with postpartum and during equivalent time periods for nonpregnant women. B, Changes in the dose or medication of an antiseizure medication by the time of delivery in pregnant women and by 9 months after enrollment for nonpregnant women.
ASM = antiseizure medication.
Modified with permission from Pennell PB, et al, N Engl J Med.28
Cesarean Delivery
Cesarean delivery was originally intended as an emergency lifesaving procedure for both the mother and the baby, but indications have increased over time. Changing risk profiles (eg, older primiparae) or elective procedures at patients’ request are often cited as reasons for the rise in cesarean deliveries.29 The overall cesarean delivery rate in the United States was 32.7% in 2013,30 and common indications in North America are elective repeat cesarean delivery (30%), dystocia or failure to progress (30%), malpresentation (11%), and fetal heart rate tracings that suggest fetal distress (10%).31 The rate of cesarean delivery varies in different population-based or community-based studies, with a rate of 29.2% globally, 37% in United States, and the highest rate reported as 66% in western China.32–38 This difference may indirectly reflect that gaps exist in the management of pregnancy among different sociodemographic groups.
In a population-based cohort study in Iceland, the frequency of cesarean delivery in women with epilepsy was almost twice of the general population. Among the most common indications for cesarean deliveries in women with epilepsy were previous cesarean delivery (20%), seizure activity during delivery (11.4%), or carrying the diagnosis of epilepsy (11.4%).21 Notably, about onefourth of the cesarean deliveries were directly attributable to epilepsy. Studies have shown that women with epilepsy are more likely to have either elective cesarean delivery (up to 1.5-fold increase) or emergency cesarean delivery.39 In addition, antiseizure medication exposure has been indicated as an independent risk factor for emergency cesarean delivery.40 It is important to establish multidisciplinary care that includes the patient’s primary care physician, neurologist, and obstetrician and make it clear that the diagnosis of epilepsy itself should not be an indication for cesarean delivery. Seizures during labor are still best treated with the usual rescue therapy using a quick-acting benzodiazepine.41
Gestational Hypertension and Preeclampsia
Gestational hypertension and preeclampsia can occur during pregnancy, and the majority of the cases develop at or near term. Preeclampsia is a pregnancy-specific disease characterized by de novo development of concurrent hypertension and proteinuria, sometimes progressing into a multiorgan cluster of varying clinical features.42 Early studies failed to show significant differences in the incidence of preeclampsia between women with epilepsy and controls.43 However, a pooled analysis including 17 studies showed an increased risk of gestational hypertensive disorders (odds ratio, 1.37; 95% confidence interval, 1.21 to 1.55) in women with epilepsy.25 In a 2017 national cohort study in Sweden, the incidence of preeclampsia was 4% in women with epilepsy compared to 2.8% in the control group,39 which is similar to the rate of preeclampsia in women with epilepsy in the United States (5.9%).38 A registry-based cohort study in Norway collected during 2004 to 2012 similarly observed an increased risk of gestational hypertension in women with epilepsy (odds ratio, 1.5; 95% confidence interval, 1.0 to 2.2), with the most frequent hypertensive complication being mild preeclampsia.44 The risk factors included antiseizure medication use (odds ratio, 1.5; 95% confidence interval, 1.0 to 2.2) and primiparity (odds ratio, 2.4; 95% confidence interval, 1.0 to 5.4).22 Exposure to different antiseizure medications was associated with different outcomes; lamotrigine and levetiracetam did not predispose for mild preeclampsia, whereas valproate was associated with an increased risk of mild preeclampsia.44
FETAL OUTCOMES OF WOMEN WITH EPILEPSY
Although the vast majority of women with epilepsy have uneventful pregnancies and 90% of children born to women with epilepsy are healthy, fetal risks have been associated with maternal epilepsy. These include increased risk of stillbirth, preterm birth, small for gestational age at birth, low Apgar score at 5 minutes, neonatal hypoglycemia, neonatal infection, respiratory distress syndrome, major congenital malformations, and adverse effects on cognitive and behavioral development.39
Spontaneous Abortion
Spontaneous abortion is defined by noninduced fetal death or passage of products of conception before 20 weeks’ gestation. Significant variation exists in reported outcomes in women with epilepsy across geographic regions in countries with different economic status.38 Several registries or retrospective studies have reported spontaneous abortion in women with epilepsy ranging from 0.5% to 39.2%, with an overall rate of 9.1% globally.25,32,38,45–47 The lowest incidence was reported in Norway as 0.5% in women with epilepsy compared to 0.3% in women without epilepsy in a population study that included a total of 372,128 births.22 The reported incidence was moderate in some Asian countries. In a retrospective study based on a Thai population that investigated 44,708 pregnancies, the spontaneous abortion rate was 2.7% in women with epilepsy compared to 0.4% in the control group,32 and a similar rate of 4.2% in women with epilepsy (compared to 2.38% in the control group) was reported in India.48 When interpreting the discrepancy between different studies, it is important to keep in mind the limitations of retrospective studies because of the potential bias secondary to retrospective recall of gestational age at the time of enrollment. Miscarriages occur more frequently early in pregnancy, so many miscarriages may not be recognized. Further, access and availability of prenatal care varies between countries.
Preterm Birth
Preterm birth (ie, delivery at <37 weeks of gestation) has been associated with various adverse adult outcomes, such as increased prevalence of medical disabilities, learning difficulties, and behavioral and psychological problems. The rate of preterm birth, either medically indicated or spontaneous, has been consistently shown to be increased in women with epilepsy across various studies.22,25,32,39,49,50 The overall rate of preterm birth in women with epilepsy is 7.6%, with the highest rate seen in the United States and the lowest in European countries (10.1% compared to 6.1%).38 Exposure to antiseizure medications significantly increases the risk of premature birth in both women with epilepsy (9.3%) and women without epilepsy who were on antiseizure medications for other neuropsychiatric indications (10.5%), when compared to those with neither exposure to antiseizure medication nor diagnosis of epilepsy (6.2%).49,50 In addition, uncontrolled seizure activity, especially the presence of seizures within 6 months of conception, also increases the incidence of premature birth.32
Congenital Malformations
Children of women with epilepsy are at increased risk of congenital malformations when compared with children of women without epilepsy. The incidence of major congenital malformations seems to be associated with early antiseizure medication exposure (first trimester),51,52 polytherapy versus monotherapy of antiseizure medication,53–56 the dose and type of antiseizure medication,54–57 low serum folate concentrations, and low maternal level of education.58 The type of epilepsy or seizures during pregnancy have not been reported to be significantly correlated with the number of minor or major malformations.58,59 In addition, children of women with epilepsy have more minor and major malformations than children of fathers with epilepsy or controls.59 Women with epilepsy who have had a child with a malformation are at increased risk of having other children with malformations when compared with women with epilepsy whose first child did not have a malformation (16.8% compared to 9.8%), indicating the genetic influences on the teratogenic risk.60,61 Hence, the cause is likely multifactorial, with a combination of endogenous and exogenous factors.
When compared to children of healthy women, children of women with epilepsy have been reported to have significantly higher overall rates of congenital malformations, with an approximately threefold increase.62,63 One of the main contributing factors is the teratogenic effects of antiepileptic drugs, although other factors, such as genetically determined individual susceptibility, are also likely to contribute. The most common malformations noted in children of women with epilepsy were cardiovascular defects (in descending order of frequency: atrial or ventricular septal defect, tetralogy of Fallot, patent ductus arteriosus) followed by musculoskeletal defects, which are also the most common defects in offspring of healthy women, although with lower frequency.62,63 The risk of spina bifida was substantially elevated, with 11-fold to 14.7-fold higher risk in the offspring of women with epilepsy, primarily because of use of valproate.63,64 The European Surveillance of Congenital Anomalies (EUROCAT) used a case-control approach employing its antiseizure medication study database derived from 19 population-based congenital anomaly registries including 98,075 cases with malformations among 3.8 million births in Europe. They found an increased risk for spina bifida for two antiseizure medications: valproate (odds ratio, 12.7; 95% confidence interval, 7.7 to 20.7) and carbamazepine (odds ratio, 2.6; 95% confidence interval, 1.2 to 5.3).65,66
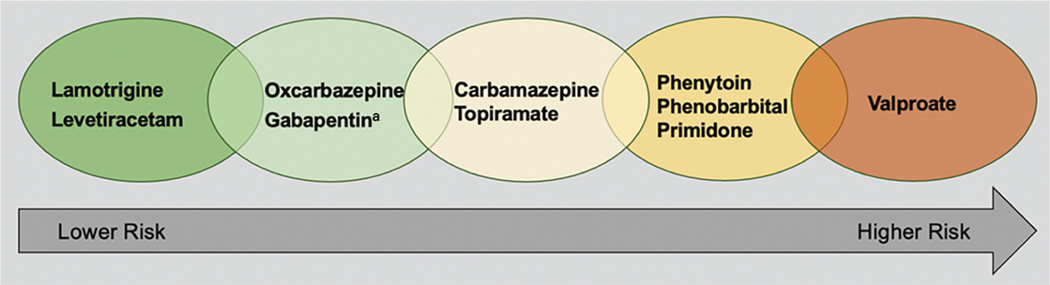
A meta-analysis including 65,533 pregnancies in women with epilepsy exposed to carbamazepine, lamotrigine, phenobarbital, phenytoin, or valproate showed that the overall incidence of congenital malformations in children born to women with epilepsy is approximately threefold that of healthy women (7.08% compared to 2.28%), with the highest incidence for antiseizure medication polytherapy (16.78%).63 Studies have shown that the lowest risk of major congenital malformations was seen in patients with exposure to lamotrigine and levetiracetam, whereas the highest risk was seen with exposure to valproate. A 2016 Cochrane Review conducted a meta-analysis for antiseizure medication monotherapy, and pooled data showed that the malformation prevalence is 1.47% for gabapentin, 1.77% for levetiracetam, 2.39% for oxcarbazepine, 4.28% for topiramate, 4.93% for carbamazepine, 6.26% for phenytoin, 7.10% for phenobarbital, 8.49% for primidone, and 10.93% for valproate (FIGURE 2-2).67 Similarly, it found no difference in malformation prevalence between the children exposed to lamotrigine and the control group, with the majority of evidence coming from pregnancy registries. Of note, the data related to gabapentin are limited, with total cases under 200, so the results should be interpreted with caution. Increased risk was observed for clobazam monotherapy in a very small sample size study.68 Data on zonisamide are also scarce, with 90 cases followed by the North American Antileptic Drug Pregnancy Registry; no major congenital malformations were found, but no definite conclusion could be drawn. Virtually no data are available on other newer antiseizure medications, and further efforts are needed to gain more information.
FIGURE 2–2.
Risk of major congenital malformations associated with antiseizure medication exposure. Pooled data from a meta-analysis of antiseizure monotherapy showed that the malformation prevalence associated with antiseizure medication is 1.47% for gabapentin, 1.77% for levetiracetam, 2.39% for oxcarbazepine, 4.28% for topiramate, 4.93% for carbamazepine, 6.26% for phenytoin, 7.10% for phenobarbital, 8.49% for primidone, and 10.93% for valproate.
aThe sample size for gabapentin-exposed cases is small.
Data from Weston J, et al, Cochrane Database Syst Rev.67
Neuromodulation therapy, including vagus nerve stimulation, direct brain-responsive neurostimulation, and deep brain stimulation, has been used as a nonpharmacologic approach to treat cases of refractory epilepsy. The safety of neuromodulation treatments during pregnancy in women with epilepsy is largely unknown. Among these devices, the most evidence exists for vagus nerve stimulation as it has been used to treat epilepsy for longer than the others. Current literature does not show a clear signal of vagus nerve stimulation–related teratogenicity, although a trend of increased obstetric intervention was reported in vagus nerve stimulation–exposed pregnancies.69,70 A 2021 study showed that no major congenital malformations were identified in direct brain-responsive neurostimulation–exposed pregnancies in 14 women with epilepsy. One child had a minor congenital anomaly of cryptorchidism, but this case was complicated by risk factors of advanced maternal age and bicornuate uterus.71 No studies have been conducted to evaluate the safety of deep brain stimulation in women with epilepsy so far, but it has been shown to have no significant adverse effects on pregnancy outcomes in patients affected by disabling movement disorders and psychiatric diseases.72 All of these data should be interpreted cautiously as sample sizes are small.
Developmental Outcome
Besides having a higher risk of malformations, children born to women with epilepsy are also potentially affected in various domains of their long-term developmental milestones, including language and other cognitive and social/emotional functions.
COGNITIVE IMPAIRMENT.
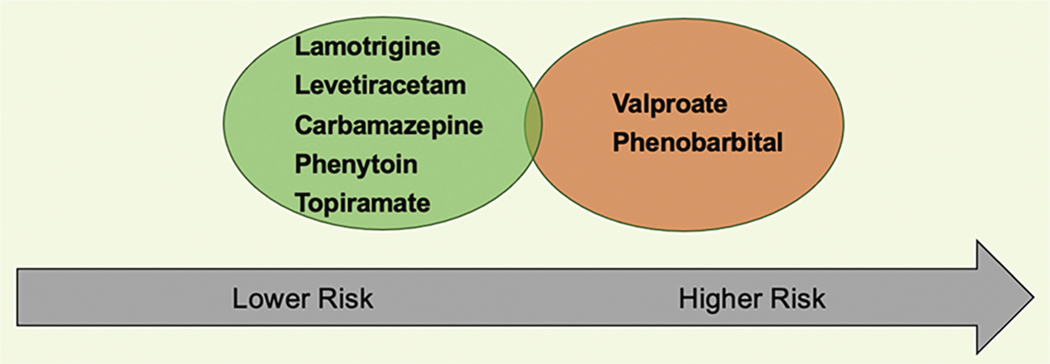
Children born to women with epilepsy have been shown to have lower mean IQ scores, which remains significant after adjustment for multiple confounding factors such as maternal education level, maternal age, maternal marital status, birth order, year of birth, and weight and length at birth.73 Several factors have been identified as related to cognitive outcomes, including frequent tonic-clonic seizures in pregnancy,74 low maternal IQ, maternal education level, and antenatal antiseizure medication exposure.75 Both the NEAD (Neurodevelopmental Effects of Antiepileptic Drugs) cohort and a study from the Liverpool and Manchester Neurodevelopmental Group confirmed the adverse cognitive effects of valproate and accounted for maternal IQ. A significantly lower IQ (mean IQ score of 97) was found in children of women with epilepsy treated with valproate than in children of women with epilepsy taking carbamazepine (mean IQ score of 105), lamotrigine (mean IQ score of 108), or phenytoin (mean IQ score of 108).76,77 Similar effects were also observed for other antiseizure medications, such as phenobarbital (approximately 0.5 standard deviation less than predicted).78 Data from the UK Epilepsy and Pregnancy Register showed that prenatal exposure to levetiracetam or topiramate was not found to be associated with reductions in child cognitive abilities, although sample sizes were small (FIGURE 2-3).79 Unlike major congenital malformations, antiseizure medication exposure during the last trimester may be the most detrimental for cognitive performance.78
FIGURE 2–3.
Neurodevelopmental outcome in children associated with antiseizure medication exposure in women with epilepsy. A significantly lower IQ was found in children of women with epilepsy treated with valproate than in children of women with epilepsy taking carbamazepine, lamotrigine, or phenytoin.76 Similar effects were also observed for other antiseizure medications such as phenobarbital.78 Data from the UK Epilepsy and Pregnancy Register showed that prenatal exposure to levetiracetam and to piramate was not found to be associated with reductions in child cognitive abilities.79
BEHAVIORAL IMPAIRMENT.
In utero exposure to antiseizure medication has been shown to be associated with a significantly increased risk of autism spectrum disorder in the offspring.80,81 Studies have shown that the risk of autism spectrum disorder with valproate exposure was 4.4%, compared to 1.5% in the general population.80 In another study, the correlation of autism spectrum disorder to fetal antiseizure medication exposure was not seen in children exposed to polytherapy without valproate, suggesting that valproate (or valproate dose) rather than polytherapy is the critical determinant of the relationship.82 No significant increase has been found among children exposed to carbamazepine or lamotrigine.83 In addition, children with in utero exposure to valproate are also at a significantly greater risk for a diagnosis of attention-deficit/hyperactivity disorder (ADHD).84 The increased likelihood of autism spectrum disorder and difficulty with adaptive functioning with fetal valproate exposure should be communicated to women with epilepsy when counseling in clinic.
COUNSELING FOR WOMEN WITH EPILEPSY OF CHILDBEARING AGE
All practitioners who care for women with epilepsy should be familiar with the relevant information and provide counseling when an antiseizure medication is first prescribed and yearly on how epilepsy and its treatment may interact with their contraception, conception, and pregnancy. Counseling should be tailored to each individual patient, depending on their age, seizure burden, and antiseizure medication exposure.
Prenatal Care
Family planning and pregnancy should be discussed with all women with epilepsy of childbearing age who are prescribed an antiseizure medication, even if they are not seeking pregnancy. Guidance should be delivered carefully to cover the potential risks but not create needless worry. Patients should be reassured that the majority of pregnancies in women with epilepsy are uneventful. The goal is to provide the information before pregnancy given that the incidence of unplanned pregnancy is more than 50% (CASE 2–1). The discussion should include the possibility of adjusting antiseizure medication management from polytherapy to monotherapy or monotherapy to a lower dose, if possible, and the potential adverse fetal outcomes of the specific antiseizure medication the patient is prescribed. If the patient is being treated with valproate, the potential anatomic and behavioral teratogenic risks should be conveyed, and trials of other antiseizure medications with better teratogenic profiles should be considered if this has not already been done. If the patient is sexually active, the authors recommend folic acid supplementation of 0.4 mg/d to 4 mg/d even if the patient is not seeking pregnancy at the time. The importance of achieving good seizure control before pregnancy should be discussed with the patient, since studies have shown that women with epilepsy who are seizure free in the 9 months before pregnancy have an 84% to 92% chance of remaining seizure free during pregnancy on their current antiseizure medication regimen.4 A therapeutic range of antiseizure medication should be established preconception as a baseline, and patients should be made aware that regular antiseizure medication level monitoring during pregnancy should be considered since the dosage may need to be increased.
FOLIC ACID SUPPLEMENTATION.
During pregnancy, folate requirements are 5- to 10-fold higher compared to nonpregnant women, and adequate periconceptional folate status is essential for structural and functional development of the fetal brain. Periconceptional folate is particularly important to women with epilepsy who are taking antiseizure medications given the fact the several antiseizure medications, especially those that induce cytochrome P450 enzymes, are known to decrease folate levels.85 Folic acid supplementation in early pregnancy is shown to have a preventive effect not only on major congenital malformations in the general population but also on language delay and autistic traits associated with fetal antiseizure medication exposure.86–88 Periconceptional folic acid supplementation at a dose greater than 400 mcg/d is associated with better neurodevelopmental scores across a variety of long-term cognitive variables in children of women with epilepsy at 6 years old.89 The American Academy of Neurology practice guideline recommends 0.4 mg/d to 4 mg/d of preconceptional folic acid supplementation.88 Unfortunately, a current low prevalence of preconception folic acid supplementation (47.6%) in women with epilepsy of childbearing age reflects a need for more education.90
Pregnancy Care
A plan for epilepsy management during pregnancy should be established for women with epilepsy. Patients often have many concerns, including fear about worsening seizures, the possibility of adverse medication effects on their fetus, and potential complications during childbirth. Clinicians should discuss the importance of starting folic acid supplementation if the patient has not already been taking it; the need for frequent monitoring of antiseizure medication concentrations during pregnancy, which could be done in coordination with their obstetrician visits; and the possible need to have their antiseizure medication dose adjusted based on pregnancy drug levels in comparison to their prepregnancy level. Patients should be reassured that most women with epilepsy have an uneventful delivery, with seizures reported in only 2% of women with epilepsy during delivery,91 and that the diagnosis of epilepsy is not an indication per se for cesarean delivery. Patients should also be screened for depression and anxiety and treated or referred, if needed.
ANTISEIZURE MEDICATION MANAGEMENT DURING PREGNANCY.
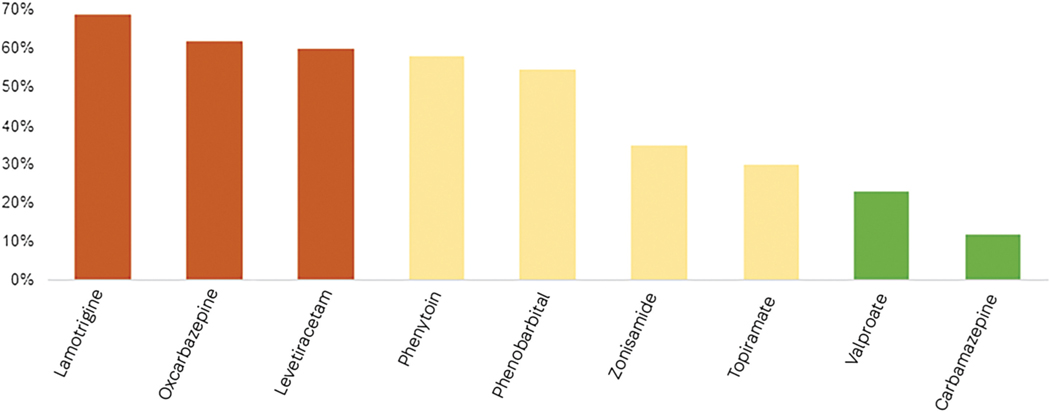
Maternal physiologic changes during pregnancy include increased blood volume and cardiac output, decreased plasma protein concentrations including hypoalbuminemia, delayed gastric emptying, and altered hepatic enzyme activities. Rapid pharmacokinetic changes during pregnancy can result in significant antiseizure medication level changes and put patients at risk of breakthrough seizures. Pronounced declines in serum concentrations can be seen for lamotrigine, which is eliminated by glucuronidation. A decrease in its serum concentration can be seen as early as the third week after conception but is most marked in the mid third trimester.41,92 Its level returns rapidly postpartum and reaches the preconception range within 3 weeks of delivery. Marked interindividual variability has been noted, and pharmacokinetic modeling analysis has demonstrated that most patients (77%) have a 220% increase in lamotrigine clearance, but a subset of patients (23%) have only a 20% increase in lamotrigine clearance.93 Levetiracetam, another antiseizure medication commonly used during pregnancy, also has a significant decline in plasma concentrations (40% to 60%) noted as early as the first trimester. The mechanism is hypothesized to be due to a combination of an increased renal elimination and enhanced enzymatic hydrolysis. Currently, approximately 30 antiseizure medications are approved by the US Food and Drug Administration (FDA), but only a handful of antiseizure medications have been investigated for potential alterations in concentrations in pregnant women with epilepsy. Based on a 2019 International League Against Epilepsy Task Force report on women and pregnancy, the most marked decline in serum concentration is seen with lamotrigine, levetiracetam, and oxcarbazepine (decrease ranging from 40% to 70%). Phenobarbital, phenytoin, topiramate, and zonisamide have a moderate decrease in serum level (ranging from 30% to 60%). In contrast, relatively small changes in serum concentration are seen with carbamazepine and valproate, which usually decrease 10% to 20% (FIGURE 2-4).41 Studies have shown that when antiseizure medication levels decrease by more than 35% when compared to the targeted level, the risk of worsening seizures increases.94 It is important to have a preconception antiseizure medication level established while seizures are effectively controlled, which can then be used as a baseline level to guide antiseizure medication titration during pregnancy (CASE 2–2).
FIGURE 2–4.
Projected decrease of antiseizure medication concentrations during pregnancy if no dose changes are made.
Data from Tomson T, et al, Epileptic Disord.41
Postpartum Care
Postpartum care is important since women with epilepsy experience many challenges involving physical, social, and psychological well-being. It is a vulnerable time not only because of physical recovery from birth but also because of medication adjustment, sleep deprivation and fatigue, increased stress, and the challenges of breastfeeding.
BREASTFEEDING.
The proportion of women reported to be breastfeeding is lower in women with epilepsy despite studies indicating the safety of breastfeeding in women with epilepsy.11 Breastfeeding provides many benefits to both mothers and children.93 It is associated with decreased risk of type 2 diabetes and breast and ovarian cancer for mothers. Infants who are breastfed also benefit from reduced risk of infections, asthma, obesity, diabetes, childhood leukemia, and sudden infant death syndrome.95 Patients are often concerned that the exposure to antiseizure medication via breast milk could potentially affect their children’s development. Valproate, phenobarbital, phenytoin, and carbamazepine are not thought to penetrate into breast milk at a clinically important level, whereas lamotrigine, levetiracetam, primidone, gabapentin, and topiramate probably penetrate into breast milk in potentially clinically important amounts.88 However, a 2020 study showed the median percentage of infant-to-mother antiseizure medication concentration was 0.3% for oxcarbazepine, 5.3% for levetiracetam, 5.4% for carbamazepine epoxide, 17.2% for topiramate, 21.4% for valproic acid, 28.9% for lamotrigine and 44.2% for zonisamide; all of which were substantially lower than maternal blood concentrations.96 A Norwegian cohort study showed that continuous breastfeeding in children of women using an antiseizure medication was associated with less impaired development at ages 6 and 18 months compared with children who were not breastfed or were breastfed for less than 6 months.97 In the NEAD cohort in the United States, no adverse effects of antiseizure medication exposure via breast milk were observed at age 3 years,98 and breastfed children exhibited higher IQs and enhanced verbal abilities at 6 years of age.99 Although further studies of exposure to other newer antiseizure medications via breast milk are necessary, women with epilepsy should be encouraged to breastfeed their children irrespective of antiseizure medication treatment.
SLEEP DEPRIVATION, DEPRESSION, AND ANXIETY.
Fragmented sleep and fatigue are commonly encountered in the postpartum period, especially if women are breastfeeding every 2 to 4 hours. Sleep deprivation and missed medication during the postpartum period are known to increase the risk of seizures; hence, patients should be encouraged to request family members’ help in feeding infants with either expressed breast milk or formula, allowing them to have some uninterrupted sleep for a longer interval. Furthermore, studies also show that women with epilepsy more often had peripartum depression (26.7%) or anxiety (22.4%) than women without epilepsy (18.9% and 14.8%, respectively), which is linked to high seizure frequency.100 These risks should be discussed with patients, and they should be encouraged to reach out to mental health care providers for proper care with coping techniques and medication treatment if symptoms are identified.
CONCLUSION
Epilepsy brings special issues for women, particularly in pregnancy. In birth control, conception, pregnancy, and postpartum care, women with epilepsy face challenges to carefully balance maintaining seizure freedom with minimizing adverse effects from antiseizure medications and other nonpharmacologic treatments. Management of epilepsy in patients of childbearing age requires careful counseling and planning. Practitioners who care for women with epilepsy should keep up-to-date with the latest guidelines and recommendations to provide the best possible care.
CASE 2–1.
A 21-year-old woman had a history of convulsions since the age of 8. Her seizure symptomatology included generalized tonic-clonic seizures and, less frequently, staring episodes. She had tried lamotrigine in the past, but it caused a skin rash. She was currently taking levetiracetam 1500 mg 2 times a day and had been seizure free in the past 18 months. When she was on a lower dose of 1000 mg 2 times a day, she had more frequent staring episodes and occasional generalized tonic-clonic seizures.
This was her first visit to an adult epilepsy clinic, and during the visit, her previous records were carefully reviewed, including EEG, MRI, and seizure-related history, and confirmed that she had generalized epilepsy of unknown etiology. Contraception and family planning were discussed. The patient indicated that she was sexually active and open-minded about having a child in the future but would defer pregnancy for now. She was not taking folic acid and was using an estrogen-progesterone oral contraceptive. A baseline antiseizure medication level was ordered, and she was prescribed 1 mg/d folic acid.
The neurologist explained that although the antiseizure medication she was currently taking did not have interactions with her oral contraceptive, more than half of pregnancies are unplanned and she might discuss with her OB/GYN about an intrauterine device with better efficacy than her oral contraceptive. She was reassured that levetiracetam has a better teratogenic profile compared to most other antiseizure medications and would be an optimal choice of antiseizure medication if she were to get pregnant. She was also asked to inform her neurologist if she became pregnant so her antiseizure medication level could be monitored monthly to help adjust the dose as needed throughout pregnancy.
COMMENT
This case illustrates key points that should be conveyed to patients when discussing family planning. Patients should be provided with information on the potential teratogenic effects of the antiseizure medication that they are taking and the importance of folic acid supplementation. If the patient is currently on an oral contraceptive, the potential interaction of the oral contraceptive and the antiseizure medication they are being treated with should be discussed. If the patient is on an enzyme-inducing antiseizure medication, an intrauterine device is the best choice to avoid contraceptive failure.
CASE 2–2.
A 26-year-old woman had a history of focal aware seizures that occurred, on average, once per month; rare focal impaired-awareness seizures that occurred once every 1 to 2 years, which were often triggered by alcohol; and convulsions years earlier. She had been followed in the epilepsy clinic for the past year. Her seizure symptomatology included an aura of déjà vu feeling for 10 seconds. She did not feel the aura interrupted her daily activities.
She returned to clinic stating that she was 11 weeks pregnant and had experienced two focal impaired-awareness seizures in the past month, with her typical aura followed by blanking out and right-sided facial twitching. This was an unplanned pregnancy. She was on lamotrigine 200 mg 2 times a day and took folic acid 1 mg/d but admitted taking the folic acid irregularly.
At her first visit to the clinic a year earlier, her lamotrigine level was 9.2 mcg/mL. During this first pregnancy visit, her level of lamotrigine showed a decrease to 5.4 mcg/mL. The neurologist recommended increasing lamotrigine to 250 mg 2 times a day for 1 week followed by an increase to 300 mg2 times a day and continuing her prenatal vitamins with folic acid supplement 1 mg/d regularly.
On a follow-up visit 1 month later, her lamotrigine level was 7.9 mcg/mL. She had not had any further focal impaired-awareness seizures since her last visit but had continued focal aware seizures, so her lamotrigine was increased to 350 mg 2 times a day. Further follow-up 1 month later showed her lamotrigine level was 9.1 mcg/mL. Monthly monitoring of her antiseizure medication continued, with appropriate dose adjustments. She did not experience any further focal impaired-awareness seizures during the pregnancy and had a normal vaginal delivery of a healthy child.
COMMENT
This case illustrates the importance of close monitoring of antiseizure medication levels during pregnancy and establishing a baseline antiseizure medication target level before conception. Antiseizure medication levels can fluctuate substantially during pregnancy because of the pharmacokinetic changes related to pregnancy. Monthly monitoring is recommended, but more frequent monitoring may be needed if dose changes are required. Regular folic acid supplementation is recommended before pregnancy since more than half of pregnancies are unplanned and patients may not recognize the pregnancy until they have already missed a critical time window for positive periconceptional folate effects.
KEY POINTS.
Although pregnancy rates differ, no difference in fertility rate is seen between women with epilepsy who are attempting to get pregnant and healthy controls (60.7% compared to 60.2%).
Certain medications, including valproate and phenobarbital, have been linked to lower fertility, but these findings require further validation in a larger cohort.
Patients treated with CYP3A4 enzyme-inducing antiseizure medications should consider alternative methods of contraception.
Lamotrigine may require substantial titration when it is used in combination with oral hormonal contraceptives.
Knowledge is limited regarding the interaction of oral contraceptives and some of the new antiseizure medications.
Most women with epilepsy will not experience seizure frequency changes during pregnancy.
The diagnosis of epilepsy alone should not be considered as an indication for cesarean delivery.
The risk of gestational hypertension and preeclampsia may be slightly increased in women with epilepsy.
The majority of women with epilepsy have uneventful pregnancies, and 90% of children born to women with epilepsy are healthy.
The risk of major congenital malformations has been associated with first trimester antiseizure medication exposure, the dose and type of antiseizure medication (especially valproate), polytherapy, low folate concentrations, and low maternal level of education.
The teratogenic risks for many antiseizure medications are uncertain. Valproate is the poorest choice of antiseizure medication based on the higher risk profile of both anatomic and behavioral teratogenicity. If used, the dose should be as low as possible.
The impact of neuromodulation therapy on pregnancy outcomes is limited.
Children born to women with epilepsy may have impaired cognitive development; the contributing factors include antenatal antiseizure medication exposure, frequent tonic-clonic seizures in pregnancy, low maternal IQ, and maternal education level.
Women with epilepsy of childbearing potential should be taking folic acid 0.4 mg/d to 4 mg/d.
Monitoring of antiseizure medication levels during pregnancy should be considered.
The most marked decline in serum concentration of antiseizure medications in pregnancy is seen with lamotrigine, levetiracetam, and oxcarbazepine (decrease ranging from 40% to 70%). Carbamazepine and valproate have minimal decreases in serum concentration, usually 10% to 20%.
Breastfeeding while taking antiseizure medication appears to be safe.
ACKNOWLEDGMENT
This work was supported by Dr. Meador’s grant from the National Institutes of Health/National Institute of Neurological Disorders and Stroke/National Institute of Child Health and Human Development (2U01-NS038455).
RELATIONSHIP DISCLOSURE:
Dr Li reports no disclosure. Dr Meador receives research/grant support from Eisai Co, Ltd, and the National Institutes of Health/National Institute of Neurological Disorders and Stroke/National Institute of Child Health and Human Development (2U01-NS038455). Dr Meador’s institution receives financial support from The Epilepsy Study Consortium for his services as a consultant for Eisai Co, Ltd; GW Pharmaceuticals plc; NeuroPace, Inc; Novartis AG; Supernus Pharmaceuticals, Inc; Upsher-Smith Laboratories, LLC; UCB, Inc; and VIVUS LLC.
Footnotes
UNLABELED USE OF PRODUCTS/INVESTIGATIONAL USE DISCLOSURE:
Drs Li and Meador report no disclosures.
Contributor Information
Dr. Yi Li, Clinical Assistant Professor of Neurology and Neurological Sciences, Stanford University, Palo Alto, California.
Kimford J. Meador, Stanford, University School of Medicine, Stanford Neuroscience Health, Center, 213 Quarry Rd, MC 5979, Palo Alto, CA 94304.
REFERENCES
- 1.Ngugi AK, Bottomley C, Kleinschmidt I, et al. Estimation of the burden of active and life-time epilepsy: a meta-analytic approach. Epilepsia 2010;51(5):883–890. doi: 10.1111/j.1528-1167.2009.02481.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Savic I. Sex differences in human epilepsy. Exp Neurol 2014;259:38–43. doi: 10.1016/j.expneurol.2014.04.009 [DOI] [PubMed] [Google Scholar]
- 3.Zack MM, Kobau R. National and state estimates of the numbers of adults and children with active epilepsy—United States, 2015. MMWR Morb Mortal Wkly Rep 2017;66(31):821–825. doi: 10.15585/mmwr.mm6631a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harden CL, Hopp J, Ting TY, et al. Practice parameter update: management issues for women with epilepsy—focus on pregnancy (an evidence-based review): obstetrical complications and change in seizure frequency: report of the Quality Standards Subcommittee and Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology and American Epilepsy Society. Neurology 2009;73(2):126–132. doi: 10.1212/WNL.0b013e3181a6b2f8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Artama M, Isojärvi JI, Raitanen J, Auvinen A. Birth rate among patients with epilepsy: a nationwide population-based cohort study in Finland. Am J Epidemiol 2004;159(11):1057–1063. doi: 10.1093/aje/kwh140 [DOI] [PubMed] [Google Scholar]
- 6.Schupf N, Ottman R. Reproduction among individuals with idiopathic/cryptogenic epilepsy: risk factors for reduced fertility in marriage. Epilepsia 1996;37(9):833–840. doi: 10.1111/j.1528-1157.1996.tb00035.x [DOI] [PubMed] [Google Scholar]
- 7.Olafsson E, Hauser WA, Gudmundsson G. Fertility in patients with epilepsy: apopulation-based study. Neurology 1998;51(1):71–73. doi: 10.1212/wnl.51.1.71 [DOI] [PubMed] [Google Scholar]
- 8.Pennell PB, French JA, Harden CL, et al. Fertility and birth outcomes in women with epilepsy seeking pregnancy. JAMA Neurol 2018;75(8): 962–969. doi: 10.1001/jamaneurol.2018.0646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sukumaran SC, Sarma PS, Thomas SV. Polytherapy increases the risk of infertility in women with epilepsy. Neurology 2010;75(15): 1351–1355. doi: 10.1212/WNL.0b013e3181f73673 [DOI] [PubMed] [Google Scholar]
- 10.MacEachern DB, Mandle HB, Herzog AG. Infertility, impaired fecundity, and live birth/pregnancy ratio in women with epilepsy in the USA: findings of the Epilepsy Birth Control Registry. Epilepsia 2019;60(9):1993–1998. doi: 10.1111/epi.16312 [DOI] [PubMed] [Google Scholar]
- 11.Johnson EL, Burke AE, Wang A, et al. Unintended pregnancy, prenatal care, newborn outcomes, and breastfeeding in women with epilepsy. Neurology 2018;91(11):e1031–e1039. [DOI] [PubMed] [Google Scholar]
- 12.Herzog AG, Mandle HB, Cahill KE, et al. Predictors of unintended pregnancy in women with epilepsy. Neurology 2017;88(8):728–733. doi: 10.1212/WNL.0000000000003637 [DOI] [PubMed] [Google Scholar]
- 13.Mohllajee AP, Curtis KM, Morrow B, Marchbanks PA. Pregnancy intention and its relationship to birth and maternal outcomes. Obstet Gynecol 2007;109(3):678–686. doi: 10.1097/01.AOG.0000255666.78427.c5 [DOI] [PubMed] [Google Scholar]
- 14.Herzog AG, Mandle HB, MacEachern DB. Association of unintended pregnancy with spontaneous fetal loss in women with epilepsy: findings of the epilepsy birth control registry. JAMA Neurol 2019;76(1):50–55. doi: 10.1001/jamaneurol.2018.3089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sundaram A, Vaughan B, Kost K, et al. Contraceptive failure in the United States: estimates from the 2006–2010 National Survey of Family Growth. Perspect Sex Reprod Health 2017;49(1):7–16. doi: 10.1363/psrh.12017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harden CL, Leppik I. Optimizing therapy of seizures in women who use oral contraceptives. Neurology 2006;67(12 suppl 4):S56–S58. doi: 10.1212/wnl.67.12_suppl_4.s56 [DOI] [PubMed] [Google Scholar]
- 17.Saano V, Glue P, Banfield CR, et al. Effects of felbamate on the pharmacokinetics of a lowdose combination oral contraceptive. Clin Pharmacol Ther 1995;58(5):523–531. doi: 10.1016/0009-9236(95)90172-8 [DOI] [PubMed] [Google Scholar]
- 18.Doose DR, Wang SS, Padmanabhan M, et al. Effect of topiramate or carbamazepine on the pharmacokinetics of an oral contraceptive containing norethindrone and ethinyl estradiol in healthy obese and nonobese female subjects. Epilepsia 2003;44(4):540–549. doi: 10.1046/j.1528-1157.2003.55602.x [DOI] [PubMed] [Google Scholar]
- 19.Rosenfeld WE, Doose DR, Walker SA, Nayak RK. Effect of topiramate on the pharmacokinetics of an oral contraceptive containing norethindrone and ethinyl estradiol in patients with epilepsy. Epilepsia 1997;38(3):317–323. doi: 10.1111/j.15281157.1997.tb01123.x [DOI] [PubMed] [Google Scholar]
- 20.Stephen LJ, Harden C, Tomson T, Brodie MJ. Management of epilepsy in women. Lancet Neurol 2019;18(5):481–491. doi: 10.1016/S1474-4422(18)30495-2 [DOI] [PubMed] [Google Scholar]
- 21.Olafsson E, Hallgrimsson JT, Hauser WA, et al. Pregnancies of women with epilepsy: a population-based study in Iceland. Epilepsia 1998;39(8):887–892. doi: 10.1111/j.1528-1157.1998.tb01186.x [DOI] [PubMed] [Google Scholar]
- 22.Borthen I, Eide MG, Veiby G, et al. Complications during pregnancy in women with epilepsy: population-based cohort study. BJOG 2009; 116(13):1736–1742. doi: 10.1111/j.1471-0528.2009.02354.x [DOI] [PubMed] [Google Scholar]
- 23.Kaplan PW, Norwitz ER, Ben-Menachem E, et al. Obstetric risks for women with epilepsy during pregnancy. Epilepsy Behav 2007;11(3):283–291. doi: 10.1016/j.yebeh.2007.08.012 [DOI] [PubMed] [Google Scholar]
- 24.Edey S, Moran N, Nashef L. SUDEP and epilepsyrelated mortality in pregnancy. Epilepsia 2014; 55(7):e72–e74. doi: 10.1111/epi.12621 [DOI] [PubMed] [Google Scholar]
- 25.Viale L, Allotey J, Cheong-See F, et al. Epilepsy in pregnancy and reproductive outcomes: a systematic review and meta-analysis. Lancet 2015;386(10006):1845–1852. doi: 10.1016/S0140-6736(15)00045-8 [DOI] [PubMed] [Google Scholar]
- 26.Sahoo S, Klein P. Maternal complex partial seizure associated with fetal distress. Arch Neurol 2005;62(8):1304–1305. doi: 10.1001/archneur.62.8.1304 [DOI] [PubMed] [Google Scholar]
- 27.Battino D, Tomson T, Bonizzoni E, et al. Seizure control and treatment changes in pregnancy: observations from the EURAP epilepsy pregnancy registry. Epilepsia 2013;54(9): 1621–1627. doi: 10.1111/epi.12302 [DOI] [PubMed] [Google Scholar]
- 28.Pennell PB, French JA, May RC, et al. Changes in seizure frequency and antiepileptic therapy during pregnancy. N Engl J Med 2020;383(26): 2547–2556. doi: 10.1056/NEJMoa2008663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mylonas I, Friese K. Indications for and risks of elective cesarean section. Dtsch Arztebl Int 2015; 112(29–30):489–495. doi: 10.3238/arztebl.2015.0489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Martin JA, Hamilton BE, Osterman MJ, et al. Births: final data for 2013. Natl Vital Stat Rep 2015; 64(1):1–65. [PubMed] [Google Scholar]
- 31.Quinlan JD, Murphy NJ. Cesarean delivery: counseling issues and complication management. Am Fam Physician 2015;91(3): 178–184. [PubMed] [Google Scholar]
- 32.Soontornpun A, Choovanichvong T, Tongsong T. Pregnancy outcomes among women with epilepsy: a retrospective cohort study. Epilepsy Behav 2018;82:52–56. doi: 10.1016/j.yebeh.2018.03.001 [DOI] [PubMed] [Google Scholar]
- 33.He S, Zhu H, Qiu X, et al. Pregnancy outcome in women with epilepsy in Western China: a prospective hospital based study. Epilepsy Behav 2017;74:10–14. doi: 10.1016/j.yebeh.2017.05.034 [DOI] [PubMed] [Google Scholar]
- 34.Artama M, Braumann J, Raitanen J, et al. Women treated for epilepsy during pregnancy: outcomes from a nationwide population-based cohort study. Acta Obstet Gynecol Scand 2017;96(7): 812–820. doi: 10.1111/aogs.13109 [DOI] [PubMed] [Google Scholar]
- 35.Borthen I, Eide MG, Daltveit AK, Gilhus NE. Delivery outcome of women with epilepsy: a population-based cohort study. BJOG 2010; 117(12):1537–1543. doi: 10.1111/j.1471-0528.2010.02694.x [DOI] [PubMed] [Google Scholar]
- 36.Chang TY, Lai CW, Yu HY, et al. Preliminary descriptive statistics of the Taiwanese Registry of Epilepsy and Pregnancy for the first 2 years. Taiwan J Obstet Gynecol 2007;46(1):47–49. doi: 10.1016/s1028-4559(08)60106-0 [DOI] [PubMed] [Google Scholar]
- 37.Katz O, Levy A, Wiznitzer A, Sheiner E. Pregnancy and perinatal outcome in epileptic women: a population-based study. J Matern Fetal Neonatal Med 2006;19(1):21–25. doi: 10.1080/14767050500434096 [DOI] [PubMed] [Google Scholar]
- 38.Allotey J, Aroyo-Manzano D, Lopez P, et al. Global variation in pregnancy complications in women with epilepsy: a meta-analysis. Eur J Obstet Gynecol Reprod Biol 2017;215:12–19. doi: 10.1016/j.ejogrb.2017.05.016 [DOI] [PubMed] [Google Scholar]
- 39.Razaz N, Tomson T, Wikström AK, Cnattingius S. Association between pregnancy and perinatal outcomes among women with epilepsy. JAMA Neurol 2017;74(8):983–991. doi: 10.1001/jamaneurol.2017.1310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Farmen AH, Grundt JH, Nakling JO, et al. Increased rate of acute caesarean sections in women with epilepsy: results from the Oppland Perinatal Database in Norway. Eur J Neurol 2019; 26(4):617–623. doi: 10.1111/ene.13865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tomson T, Battino D, Bromley R, et al. Management of epilepsy in pregnancy: a report from the International League Against Epilepsy Task Force on Women and Pregnancy. Epileptic Disord 2019;21(6):497–517. doi: 10.1684/epd.2019.1105 [DOI] [PubMed] [Google Scholar]
- 42.Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R. Pre-eclampsia. Lancet 2010; 376(9741):631–644. doi: 10.1016/S0140-6736(10)60279-6 [DOI] [PubMed] [Google Scholar]
- 43.Viinikainen K, Heinonen S, Eriksson K, Kalviainen R. Community-based, prospective, controlled study of obstetric and neonatal outcome of 179 pregnancies in women with epilepsy. Epilepsia 2006;47(1):186–192. doi: 10.1111/j.1528-1167.2006.00386.x [DOI] [PubMed] [Google Scholar]
- 44.Danielsson KC, Borthen I, Morken NH, Gilhus NE. Hypertensive pregnancy complications in women with epilepsy and antiepileptic drugs: a population-based cohort study of first pregnancies in Norway. BMJ Open 2018;8(4): e020998. doi: 10.1136/bmjopen-2017-020998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Martin PJ, Millac PA. Pregnancy, epilepsy, management and outcome: a 10-year perspective. Seizure 1993;2(4):277–280. doi: 10.1016/s1059-1311(05)80140-2 [DOI] [PubMed] [Google Scholar]
- 46.Pittschieler S, Brezinka C, Jahn B, et al. Spontaneous abortion and the prophylactic effect of folic acid supplementation in epileptic women undergoing antiepileptic therapy. J Neurol 2008;255(12):1926–1931. doi: 10.1007/s00415-008-0029-1 [DOI] [PubMed] [Google Scholar]
- 47.Bech BH, Kjaersgaard MIS, Pedersen HS, et al. Use of antiepileptic drugs during pregnancy and risk of spontaneous abortion and stillbirth: population based cohort study. BMJ 2014;349: g5159. doi: 10.1136/bmj.g5159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Thomas SV, Sindhu K, Ajaykumar B, et al. Maternal and obstetric outcome of women with epilepsy. Seizure 2009;18(3):163–166. doi: 10.1016/j.seizure.2008.08.010 [DOI] [PubMed] [Google Scholar]
- 49.Hernández-Díaz S, McElrath TF, Pennell PB, et al. Fetal growth and premature delivery in pregnant women on antiepileptic drugs. Ann Neurol 2017; 82(3):457–465. doi: 10.1002/ana.25031 [DOI] [PubMed] [Google Scholar]
- 50.Artama M, Gissler M, Malm H, et al. Effects of maternal epilepsy and antiepileptic drug use during pregnancy on perinatal health in offspring: nationwide, retrospective cohort study in Finland. Drug Saf 2013;36(5):359–369. doi: 10.1007/s40264-013-0052-8 [DOI] [PubMed] [Google Scholar]
- 51.Margulis AV, Mitchell AA, Gilboa SM, et al. Use of topiramate in pregnancy and risk of oral clefts. Am J Obstet Gynecol 2012;207(5):405.e1–405.e7. doi: 10.1016/j.ajog.2012.07.00 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wyszynski DF, Nambisan M, Surve T, et al. Increased rate of major malformations in offspring exposed to valproate during pregnancy. Neurology 2005;64(6):961–965. doi: 10.1212/01.WNL.0000154516.43630.C5 [DOI] [PubMed] [Google Scholar]
- 53.Keni RR, Jose M, Sarma PS, et al. Teratogenicity of antiepileptic dual therapy: dose-dependent, drug-specific, or both? Neurology 2018;90(9): e790–e796. doi: 10.1212/WNL.0000000000005031 [DOI] [PubMed] [Google Scholar]
- 54.Shakir RA, Abdulwahab B. Congenital malformations before and after the onset of maternal epilepsy. Acta Neurol Scand 1991;84(2): 153–156. doi: 10.1111/j.1600-0404.1991.tb04924.x [DOI] [PubMed] [Google Scholar]
- 55.Tomson T, Battino D, Bonizzoni E, et al. Comparative risk of major congenital malformations with eight different antiepileptic drugs: a prospective cohort study of the EURAP registry. Lancet Neurol 2018;17(6):530–538. doi: 10.1016/S1474-4422(18)30107-8 [DOI] [PubMed] [Google Scholar]
- 56.Morrow J, Russell A, Guthrie E, et al. Malformation risks of antiepileptic drugs in pregnancy: a prospective study from the UK Epilepsy and Pregnancy Register. J Neurol Neurosurg Psychiatry 2006;77(2):193–198. doi: 10.1136/jnnp.2005.074203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tomson T, Battino D, Bonizzoni E, et al. Dose-dependent risk of malformations with antiepileptic drugs: an analysis of data from the EURAP epilepsy and pregnancy registry. Lancet Neurol 2011;10(7):609–617. doi: 10.1016/S1474-4422(11)70107-7 [DOI] [PubMed] [Google Scholar]
- 58.Kaaja E, Kaaja R, Hiilesmaa V. Major malformations in offspring of women with epilepsy. Neurology 2003;60(4):575–579. doi: 10.1212/01.wnl.0000044157.28073.dc [DOI] [PubMed] [Google Scholar]
- 59.Koch S, Lösche G, Jager-Romän E, et al. Major and minor birth malformations and antiepileptic drugs. Neurology 1992;42(4 suppl 5):83–88. [PubMed] [Google Scholar]
- 60.Campbell E, Devenney E, Morrow J, et al. Recurrence risk of congenital malformations in infants exposed to antiepileptic drugs in utero. Epilepsia 2013;54(1):165–171. doi: 10.1111/epi.12001 [DOI] [PubMed] [Google Scholar]
- 61.Vajda FJ, O’Brien TJ, Lander CM, et al. Teratogenesis in repeated pregnancies in antiepileptic drug-treated women. Epilepsia 2013;54(1):181–186. doi: 10.1111/j.1528-1167.2012.03625.x [DOI] [PubMed] [Google Scholar]
- 62.Thomas SV, Ajaykumar B, Sindhu K, et al. Cardiac malformations are increased in infants of mothers with epilepsy. Pediatr Cardiol 2008; 29(3):604–608. doi: 10.1007/s00246-007-9161-4 [DOI] [PubMed] [Google Scholar]
- 63.Meador K, Reynolds MW, Crean S, et al. Pregnancy outcomes in women with epilepsy: a systematic review and meta-analysis of published pregnancy registries and cohorts. Epilepsy Res 2008;81(1):1–13. doi: 10.1016/j.eplepsyres.2008.04.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Artama M, Ritvanen A, Gissler M, et al. Congenital structural anomalies in offspring of women with epilepsy—a population-based cohort study in Finland. Int J Epidemiol 2006;35(2):280–287. doi: 10.1093/ije/dyi234 [DOI] [PubMed] [Google Scholar]
- 65.Jentink J, Loane MA, Dolk H, et al. Valproic acid monotherapy in pregnancy and major congenital malformations. N Engl J Med 2010;362(23): 2185–2193. doi: 10.1056/NEJMoa0907328 [DOI] [PubMed] [Google Scholar]
- 66.Jentink J, Dolk H, Loane MA, et al. Intrauterine exposure to carbamazepine and specific congenital malformations: systematic review and case-control study. BMJ 2010;341:c6581. doi: 10.1136/bmj.c6581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Weston J, Bromley R, Jackson CF, et al. Monotherapy treatment of epilepsy in pregnancy: congenital malformation outcomes in the child. Cochrane Database Syst Rev 2016;11(11): CD010224. doi: 10.1002/14651858.CD010224.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Thomas SV, Jose M, Divakaran S, Sankara Sarma P. Malformation risk of antiepileptic drug exposure during pregnancy in women with epilepsy: results from a pregnancy registry in South India. Epilepsia 2017;58(2):274–281. doi: 10.1111/epi.13632 [DOI] [PubMed] [Google Scholar]
- 69.Sabers A, Battino D, Bonizzoni E, et al. Maternal and fetal outcomes associated with vagus nerve stimulation during pregnancy. Epilepsy Res 2017; 137:159–162. doi: 10.1016/j.eplepsyres.2017.05.013 [DOI] [PubMed] [Google Scholar]
- 70.Suller Marti A, Mirsattari SM, Steven DA, et al. Experience on the use of vagus nerve stimulation during pregnancy. Epilepsy Res 2019;156:106186. doi: 10.1016/j.eplepsyres.2019.106186 [DOI] [PubMed] [Google Scholar]
- 71.Li Y, Eliashiv D, LaHue SC, et al. Pregnancy outcomes of refractory epilepsy patients treated with brain-responsive neurostimulation. Epilepsy Res 2021;169:106532. doi: 10.1016/j.eplepsyres.2020.106532 [DOI] [PubMed] [Google Scholar]
- 72.Scelzo E, Mehrkens JH, Botzel K, et al. Deep brain stimulation during pregnancy and delivery: experience from a series of “DBS babies”. Front Neurol 2015;6:191. doi: 10.3389/fneur.2015.00191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Oyen N, Vollset SE, Eide MG, et al. Maternal epilepsy and offsprings’ adult intelligence: a population-based study from Norway. Epilepsia 2007;48(9):1731–1738. doi: 10.1111/j.1528-1167.2007.01130.x [DOI] [PubMed] [Google Scholar]
- 74.Adab N, Kini U, Vinten J, et al. The longer term outcome of children born to mothers with epilepsy. J Neurol Neurosurg Psychiatry 2004; 75(11):1575–1583. doi: 10.1136/jnnp.2003.029132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Thomas SV, Sukumaran S, Lukose N, et al. Intellectual and language functions in children of mothers with epilepsy. Epilepsia 2007;48(12): 2234–2240. doi: 10.1111/j.1528-1167.2007.01376.x [DOI] [PubMed] [Google Scholar]
- 76.Meador KJ, Baker GA, Browning N, et al. Fetal antiepileptic drug exposure and cognitive outcomes at age 6 years (NEAD study): a prospective observational study. Lancet Neurol 2013;12(3):244–252. doi: 10.1016/S1474-4422(12)70323-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Baker GA, Bromley RL, Briggs M, et al. IQ at 6 years after in utero exposure to antiepileptic drugs: a controlled cohort study. Neurology 2015; 84(4):382–390. doi: 10.1212/WNL.0000000000001182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Reinisch JM, Sanders SA, Mortensen EL, Rubin DB. In utero exposure to phenobarbital and intelligence deficits in adult men. JAMA 1995; 274(19):1518–1525. [PubMed] [Google Scholar]
- 79.Bromley RL, Calderbank R, Cheyne CP, et al. Cognition in school-age children exposed to levetiracetam, topiramate, or sodium valproate. Neurology 2016;87(18):1943–1953. doi: 10.1212/WNL.0000000000003157 [DOI] [PubMed] [Google Scholar]
- 80.Christensen J, Grønborg TK, Sørensen MJ, et al. Prenatal valproate exposure and risk of autism spectrum disorders and childhood autism. JAMA 2013;309(16):1696–1703. doi: 10.1001/jama.2013.2270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bromley RL, Mawer G, Clayton-Smith J, et al. Autism spectrum disorders following in utero exposure to antiepileptic drugs. Neurology 2008; 71(23):1923–1924. doi: 10.1212/01.wnl.0000339399.64213.1a [DOI] [PubMed] [Google Scholar]
- 82.Wood AG, Nadebaum C, Anderson V, et al. Prospective assessment of autism traits in children exposed to antiepileptic drugs during pregnancy. Epilepsia 2015;56(7):1047–1055. doi: 10.1111/epi.13007 [DOI] [PubMed] [Google Scholar]
- 83.Sabers A, Bertelsen FC, Scheel-Krüger J, et al. Long-term valproic acid exposure increases the number of neocortical neurons in the developing rat brain. A possible new animal model of autism. Neurosci Lett 2014;580:12–16. doi: 10.1016/j.neulet.2014.07.036 [DOI] [PubMed] [Google Scholar]
- 84.Cohen MJ, Meador KJ, Browning N, et al. Fetal antiepileptic drug exposure: adaptive and emotional/behavioral functioning at age 6 years. Epilepsy Behav 2013;29(2):308–315. doi: 10.1016/j.yebeh.2013.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Reynolds EH. Antiepileptic drugs, folate and one carbon metabolism revisited. Epilepsy Behav 2020;112:107336. doi: 10.1016/j.yebeh.2020.107336 [DOI] [PubMed] [Google Scholar]
- 86.Husebye ESN, Gilhus NE, Riedel B, et al. Verbal abilities in children of mothers with epilepsy: association to maternal folate status. Neurology 2018;91(9):e811–e821. doi: 10.1212/WNL.0000000000006073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Bjork M, Riedel B, Spigset O, et al. Association of folic acid supplementation during pregnancy with the risk of autistic traits in children exposed to antiepileptic drugs in utero. JAMA Neurol 2018; 75(2):160–168. doi: 10.1001/jamaneurol.2017.3897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Harden CL, Pennell PB, Koppel BS, et al. Practice parameter update: management issues for women with epilepsy—focus on pregnancy (an evidence-based review): vitamin K, folic acid, blood levels, and breastfeeding: report of the Quality Standards Subcommittee and Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology and American Epilepsy Society. Neurology 2009;73(2):142–149. doi: 10.1212/WNL.0b013e3181a6b325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Meador KJ, Pennell PB, May RC, et al. Effects of periconceptional folate on cognition in children of women with epilepsy: NEAD study. Neurology 2020;94(7):e729–e740. doi: 10.1212/WNL.0000000000008757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Herzog AG, MacEachern DB, Mandle HB, et al. Folic acid use by women with epilepsy: findings of the Epilepsy Birth Control Registry. Epilepsy Behav 2017;72:156–160. doi: 10.1016/j.yebeh.2017.05.007 [DOI] [PubMed] [Google Scholar]
- 91.Sveberg L, Svalheim S, Taubøll E. The impact of seizures on pregnancy and delivery. Seizure 2015;28:35–38. doi: 10.1016/j.seizure.2015.02.020 [DOI] [PubMed] [Google Scholar]
- 92.Tomson T, Landmark CJ, Battino D. Antiepileptic drug treatment in pregnancy: changes in drug disposition and their clinical implications. Epilepsia 2013;54(3):405–414. doi: 10.1111/epi.12109 [DOI] [PubMed] [Google Scholar]
- 93.Polepally AR, Pennell PB, Brundage RC, et al. Model-based lamotrigine clearance changes during pregnancy: clinical implication. Ann Clin Transl Neurol 2014;1(2):99–106. doi: 10.1002/acn3.29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Reisinger TL, Newman M, Loring DW, et al. Antiepileptic drug clearance and seizure frequency during pregnancy in women with epilepsy. Epilepsy Behav 2013;29(1):13–18. doi: 10.1016/j.yebeh.2013.06.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ip S, Chung M, Raman G, et al. A summary of the Agency for Healthcare Research and Quality’s evidence report on breastfeeding in developed countries. Breastfeed Med 2009;4(suppl 1): S17–S30. doi: 10.1089/bfm.2009.0050 [DOI] [PubMed] [Google Scholar]
- 96.Birnbaum AK, Meador KJ, Karanam A, et al. Antiepileptic drug exposure in infants of breastfeeding mothers with epilepsy. JAMA Neurol 2020;77(4):441–450. doi: 10.1001/jamaneurol.2019.4443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Veiby G, Engelsen BA, Gilhus NE. Early child development and exposure to antiepileptic drugs prenatally and through breastfeeding: a prospective cohort study on children of women with epilepsy. JAMA Neurol 2013;70(11):1367–1374. doi: 10.1001/jamaneurol.2013.4290 [DOI] [PubMed] [Google Scholar]
- 98.Meador KJ, Baker GA, Browning N, et al. Effects of breastfeeding in children of women taking antiepileptic drugs. Neurology 2010;75(22): 1954–1960. doi: 10.1212/WNL.0b013e3181ffe4a9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Meador KJ, Baker GA, Browning N, et al. Breastfeeding in children of women taking antiepileptic drugs: cognitive outcomes at age 6 years. JAMA Pediatr 2014;168(8):729–736. doi: 10.1001/jamapediatrics.2014.118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Bjork MH, Veiby G, Reiter SC, et al. Depression and anxiety in women with epilepsy during pregnancy and after delivery: a prospective population-based cohort study on frequency, risk factors, medication, and prognosis. Epilepsia 2015;56(1):28–39. doi: 10.1111/epi.12884 [DOI] [PubMed] [Google Scholar]