Abstract
Objective
To examine whether the financial burden of hospitalizations affects the health care utilization of household members of the admitted patient.
Data Sources
We utilized health care claims data from the Massachusetts All‐Payer Claims Database, 2010–2015, to identify emergency hospitalizations of patients on family insurance plans and the health care utilization of the family members on those plans.
Study Design
We used an event‐study analysis to compare health care spending and utilization of family members of a hospitalized individual and family members of an individual who was hospitalized 1 year later. We examine whether such hospitalizations were associated with changes in medical spending, the frequency of ambulatory office visits, other ambulatory care, and preventive care.
Data Collection/Extraction Methods
The analyses include household members of patients with an emergency admission and a length of stay between 5 and 90 days.
Principal Findings
Unexpected hospital admissions reduced household members' health care spending and utilization by more than 6.4% (95% confidence interval [CI]: −8.2%, −4.5%) on average in the year following the hospitalization. Household members had fewer ambulatory visits with primary care physicians (PCPs), fewer referrals to specialists, and reduced utilization of other ambulatory care, including high‐value preventive services. These changes were observed for both children and adults and were exacerbated if members of the household had previously been on Medicaid. The reduction in utilization was less pronounced when the admitted patient and household member shared the same PCP and when their health insurance plan had a family deductible.
Conclusions
Compared with families without a hospitalized family member, family members of hospitalized individuals reduced their medical spending and utilization, including a substantial reduction in the use of preventive care. This study highlights the challenges of providing continuity in care when families face financial hardship.
Keywords: health insurance, health spending, hospitalizations, households, preventive care
What is known on this topic
Severe medical events can negatively impact the financial status of patients and their families.
Prior research has shown that both medical bills and the inability of the admitted patient to work contribute to adverse economic consequences for the household.
It is not known, however, whether and how the financial impact of hospitalizations impacts the health care utilization of others in the household.
What this study adds
Using health care claims data, we found that hospitalizations of family members reduce the utilization of ambulatory care, including preventive care.
We found that the results apply to both children and adults and that the reduction in health care utilization is most pronounced for people with prior Medicaid coverage.
Our findings suggest that continuity of care is jeopardized by hospitalizations in the household, but that institutional features, such as sharing a Primary Care Physician, may attenuate these adverse effects.
1. INTRODUCTION
Health care affordability is an ongoing, major concern for US households, and severe medical events can negatively impact the financial status of patients and their families. 1 , 2 , 3 , 4 In 2019, half of US adults reported that they or a family member postponed or skipped care due to costs, and nearly half of those who struggled to pay medical bills said it had a major impact on their family. 2 Struggles with affordability are not just limited to the uninsured: individuals with employer‐sponsored insurance coverage also report challenges paying medical bills or affording insurance. 4
Hospitalizations are an important contributing factor to US household financial struggles. For example, privately insured individuals who experience a hospitalization have higher average annual out‐of‐pocket spending compared to individuals who do not experience a hospitalization. This additional spending is the result of substantially more spending per encounter and a larger number of encounters which implies clusters of high out‐of‐pocket spending. 5 Unexpected hospitalizations directly affect household financial status via these out‐of‐pocket costs, but also indirectly through the inability of the admitted patient to earn income. 6 , 7 Previous studies have shown that these unexpected medical events lead to poorer credit ratings and – in a small number of cases – bankruptcy. 6 , 8 In addition to the negative financial effects that health issues may have on hospitalized individuals and their families, research in the context of Denmark suggests that exposure to a family member's health shock may lead to other household members improving their health behaviors and using preventive care. 9
However, given the vast differences in the organization of health care and social security between the United States and Denmark it remains unclear how unexpected medical events affect household health care consumption in the United States. First, a reduction in health care use and spending is plausible because the out‐of‐pocket costs and forgone income may impose financial constraints on the household, leading to family members delaying or foregoing medical care. When faced with higher cost sharing, patients often cut back on care across the value spectrum. 10 , 11 Likewise, prior work has suggested that time constraints reduce health care utilization which implies that the time and cognitive burden associated with hospitalizations may also negatively impact family member health care utilization. 12 Second, similar to the Danish case, a family member's unexpected hospitalization may prompt other household members to learn about their own health status and needs, potentially leading to an increase in health care utilization. Finally, a hospitalization event may have a negative impact on financial status but little or no effect on the health care utilization of family members if household spending is reduced only in non‐health care domains. 4
To explore these scenarios, this study assessed the extent to which the unexpected hospitalization of one household member affects the health care consumption patterns of other household members. We focused on unexpected hospitalizations to mitigate concerns about anticipatory behavior. As a summary measure, we first examined the average total medical expenditures of hospitalized individuals' family members. We then explored the impact on the utilization of specific types of care, including office visits for primary care and specialists, use of other types of ambulatory care, and high‐value preventive services. To understand the potential differences across vulnerable patient groups, we examined how medical spending and health care use varied for children and for families that had previously been enrolled in Medicaid. Finally, we assessed whether changes in medical spending and use were attenuated by two institutional features of health care provision: a shared Primary Care Physician with the hospitalized family member and an insurance plan with a family deductible.
2. METHODS
2.1. Data source
We examined the effect of hospitalization on family members' health care utilization using the Massachusetts All‐Payer Claims Database (MA APCD). The MA APCD is collected and maintained by the Center for Health Information and Analysis and contains medical claims for all Massachusetts residents except those enrolled in Medicare fee‐for‐service. We used data from January 1, 2010 to December 31, 2015 for our analyses.
To create our sample of unexpectedly hospitalized individuals and their family members, we selected all inpatient hospital facility claims for emergent or urgent admissions from 2010 to 2015 for non‐pregnancy‐related health issues. Consecutive stay dates for an individual were grouped into a single hospitalization event. We identified the family status of the hospitalized individual based on sharing health insurance plan coverage with other members and limited the sample to hospitalized individuals with other family members on the same plan at the time of hospitalization. To further refine our sample, we identified and removed households with multiple hospitalizations that occurred within 2 weeks of each other, limited our primary sample to hospital stays between 5 and 90 days, and only examined the first such hospitalization event in a household during our analysis period. The 5–90 day requirement ensured that our sample included only severe hospitalizations likely to impact household finances. As a final measure to establish that hospitalizations were unanticipated, we dropped cases where the hospitalized individual experienced either a spending increase in the 6 months prior to a hospitalization or increased spending in the month prior to hospitalization by more than three standard deviations above their mean pre‐hospitalization spending. Appendix A contains further details on study sample construction.
After performing these sampling steps, we built our primary analysis sample of household members of the hospitalized individual. For each of these household members – which we refer to as the “at‐risk” household member – we calculated our first outcome variable: an at‐risk household member's total monthly health care spending. Because spending is skewed, we log transform this variable and add 1 to the observations where spending equals 0. Next, we extracted the medical claims for each at‐risk family member by month and evaluated whether they had any ambulatory office visits, consumed other ambulatory care, or received any preventive care. First, ambulatory office visits were identified using Current Procedural Terminology codes 99201‐99205 and 99211‐99215. Second, other ambulatory care was identified by aggregating all medical claims except those covering inpatient episodes, emergency room visits, or ambulatory office visits. Finally, high‐value preventive care was identified using a CMS (Centers for Medicare and Medicaid Services) list of all preventive services (see table F1 in appendix F), including screenings, preventive health visits, and counseling aimed at reducing harmful health behaviors. 13 Note that using preventive services as a primary outcome allowed us to conduct a conservative test of our research question as most of these services involve minimal or no out‐of‐pocket spending.
The reason we focused on non‐urgent, outpatient care services (ambulatory office visits, other ambulatory care, and preventive care) as our primary outcome variables is that, compared to emergency and inpatient care, patients may exercise more discretion over their use without experiencing immediate adverse health consequences. However, we also identified the incidence of emergency care services and inpatient admissions and report the results in Appendix D. We identified emergency room care based on procedure codes, revenue codes, and site of service codes. These codes are listed in Appendix D. In addition to changes in emergency and inpatient care, Appendix D also includes estimates of changes in low‐value care.
We captured two variables to evaluate the responses of vulnerable subpopulations: children and those with previous Medicaid coverage. Children are identified as those 18 years and younger at the time of the hospitalization. Past Medicaid coverage is measured at the household level and equals one if at least one household member had Medicaid coverage in the 24 months prior to the hospitalization event. Finally, we created two variables to test whether the effect of family member hospitalization is attenuated by institutional features of health care provision. First, we measured whether the hospitalized individual and the at‐risk family member share the same PCP. The rationale for measuring this is that a PCP who is aware of the health status of the hospitalized individual may encourage the at‐risk family member(s) to continue to receive the health care they need. Second, we measured whether households larger than two have a family deductible. If they do, the at‐risk household members may face lower out‐of‐pocket costs, which should limit changes in financial status and future health care utilization. We limit our sample to households larger than two because most family deductibles are twice the individual deductible.
2.2. Study design
We used a difference‐in‐differences design that compared changes in outcome measures for families experiencing an unexpected hospitalization with other families who experienced an unexpected hospitalization 1 year later. We start by identifying all families with a hospitalization event in January 2011 and matching them with all families who will experience a hospitalization event in February 2012. We refer to this matched sample as a cohort. We then iterate over the data by month until the final treatment group in November 2014 is matched with the final control group that will experience a hospitalization event in December 2015. We then assign cohort identifiers to each of the cohorts and include them as fixed effects in our regression equation to ensure that our treatment effects are estimated only based on comparisons of those families experiencing a hospitalization event 1 year apart. The effect of the unexpected hospitalization is identified based on the change in differences in outcomes across the treatment and comparison groups over time. This estimation strategy is similar to the stacked regression approach used in earlier work 14 and incorporates recommendations from recent work that suggests that variation in the treatment effect between cohorts introduces bias to the main regression estimates. 15 To ensure that our results are robust to other estimation methods, Appendix B reports the point estimates for three other difference‐in‐differences estimation techniques that were proposed recently. 16 , 17 , 18 The Appendix also includes more details about the stacked regression estimation approach.
2.3. Statistical analysis
Our analysis was conducted at the individual‐month level. We examined outcomes for all individuals in a family, excluding the individual who was unexpectedly hospitalized. We estimated multivariable linear regressions with an interaction between treatment status and each month relative to the hospitalization (range of 12 months pre‐hospitalization and 12 months post‐hospitalization) as the primary explanatory variables. We also included hospitalized family‐by‐cohort fixed effects and month‐by‐cohort fixed effects. This empirical setup safeguards us from weighting issues identified in recent work on differences‐in‐differences with staggered treatments. 15 The month of hospitalization was the designated reference category. We clustered the standard errors at the family level. Appendix B describes the technical aspects of our statistical analysis.
Our study design assumes that absent the unexpected hospitalization, the trends in outcomes for the treatment and comparison families would be parallel. The underlying intuition is that within the window of comparison between treatment and comparison families (1 year), the timing of the hospitalization is as good as random. To assess this assumption, we analyzed spending in the year prior to hospitalization and checked for balance across a range of observable characteristics between the treatment and comparison groups. A table with balance statistics is included in Appendix A.
3. RESULTS
Figure 1 shows the mean total expenditures associated with the hospital admissions of the initially hospitalized household members in our sample. There was no anticipatory spending, suggesting that our strategy to identify unexpected hospitalizations achieved its goal. The figure further demonstrates that the distribution of medical expenditures is skewed given the substantially higher mean compared to the median. Finally, post‐discharge medical expenditures remained substantially above pre‐admission levels.
FIGURE 1.
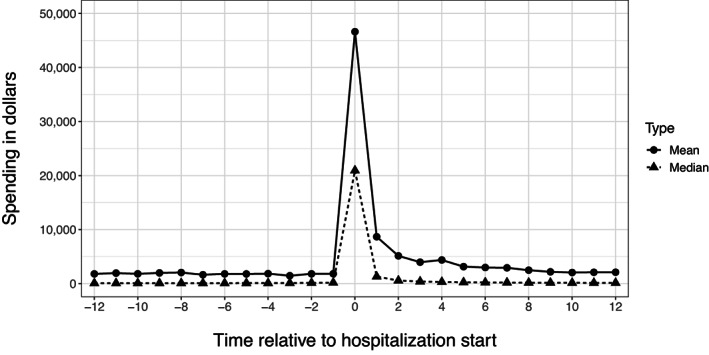
Medical spending of hospitalized family member. This figure shows the mean and median medical spending of the hospitalized family member by month relative to the month of the hospitalization. Source: Author analysis
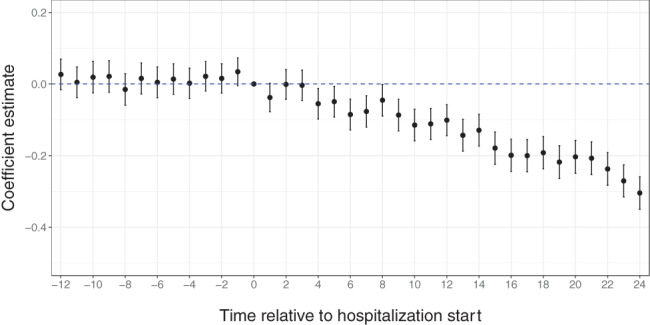
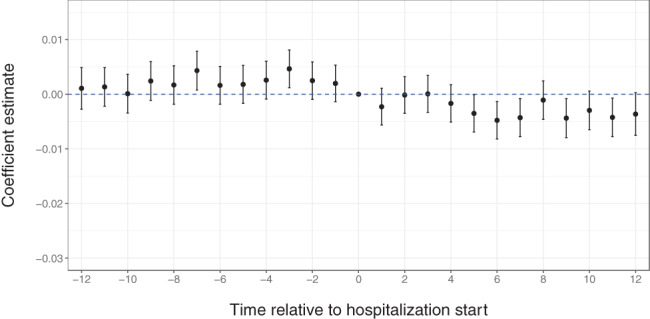
Figure 2 shows the main results of our study. Panel A contains the coefficient estimates and confidence intervals of an event study in which we regressed the logarithm of total medical spending per month for the at‐risk household members on a set of 12 pre‐ and 12 post‐hospitalization month indicators. The coefficient estimates multiplied by 100 can be interpreted as the percent change in medical spending relative to the month prior to hospitalization. The figure shows that in the months prior to the hospitalization, household members had stable and similar spending levels relative to the 1 month prior to hospitalization. Consistent with the results from Figure 1, these results suggest that there was no anticipation of the hospitalization. The graph also shows that in the months following hospitalization, spending levels decreased significantly. For example, in month 4 following the hospitalization, household members of hospitalized patients spent about 5% less (95% confidence interval [CI]:−8.5%, −1.5%) on health care than control households without a hospitalization. This difference grew over time and by month 10 showed a reduction of nearly 15% (95% confidence interval [CI]:−18.1%, −10.6%). In an average month in the year following the hospitalization of a household member, at‐risk family members spent about 6.4% less (95% confidence interval [CI]:−8.2%, −4.6%) on medical care.
FIGURE 2.
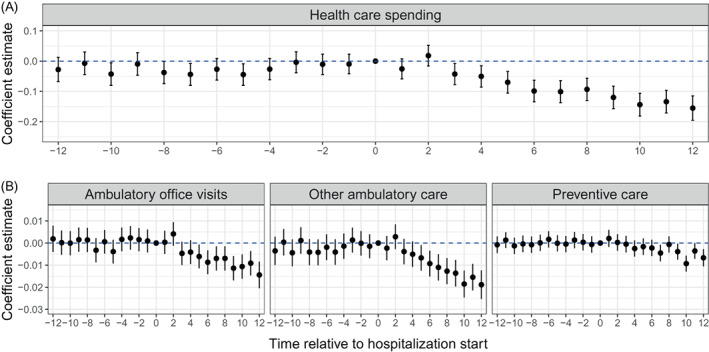
Treatment effects of family member hospitalization on health care spending and utilization. Panel A shows the point estimates from our regression model with log(medical spending) as the outcome. The estimates are relative to the hospitalization month at month 0. Panel B shows the point estimates from our regression model with Pr(Ambulatory office visits = 1), Pr(Other ambulatory care = 1), and Pr(Preventive care = 1) as the outcomes. Source: Author analysis [Color figure can be viewed at wileyonlinelibrary.com]
In subsequent analyses, we sought to examine the type of care that household members of hospitalized patients tend to forgo. Panel B plots the coefficients and confidence intervals from a regression model in which we regressed a monthly indicator of whether the type of care was consumed on the set of 12 pre‐ and 12 post‐hospitalization month indicators. First, we found that the probability of a treated household member seeing their PCP or specialist for an ambulatory office visit decreased by about 3.2% (95% confidence interval [CI]:−4.3%, −2.1%) on average per month. In additional analyses (Appendix D), we showed that the reduction in ambulatory office visits to specialists persisted when conditioning on there being a PCP visit. This suggests that in response to the hospitalization of a household member, PCPs either referred less or patients were less likely to follow up on a referral.
The next outcome we examined was other ambulatory care. This was a broad measure of all outpatient care excluding ambulatory office visits and emergency room visits. Like our results for ambulatory office visits, we found that family members in the treatment group were significantly less likely than control family members to consume ambulatory care in the months following hospitalization. The size of the effect grew over time and peaked in month ten post‐hospitalization.
In considering the implications of these results, it is important to evaluate whether the response of household members was limited to low‐value services or whether high‐value care consumption was affected too. To further examine this, we considered the utilization of high‐value preventive care. Like our other results, we found that treating patients reduced their utilization of these services by about 3.8% (95% confidence interval [CI]:−5.4%, −2.2%) per month on average. We also examined whether family members experienced a shift in the use of low‐value care. The results are included in Appendix D.
Similar models were estimated for emergency room use and inpatient admissions. We found the use of these services was not affected by the hospitalizations of family members which is consistent with patients having less discretion to forgo emergency care and care for severe health conditions (Appendix D contains further details).
We also examined the impact of reductions in the use of medical services on two vulnerable subgroups: children and low‐income families as measured by past Medicaid coverage (Figure 3). In panel A, we subset our main sample to include only children. Here, at‐risk household members included only children, but the hospitalized household member may have been either an adult or child. Like the results for the full sample, we found that the treatment effect of having a hospitalized household member is negative and significant. Specifically, we found that compared to children in households without a hospitalized family member, spending on medical services and consumption of preventive care was lower for children in treatment families, by about 9%–10% in the year following the hospitalization.
FIGURE 3.
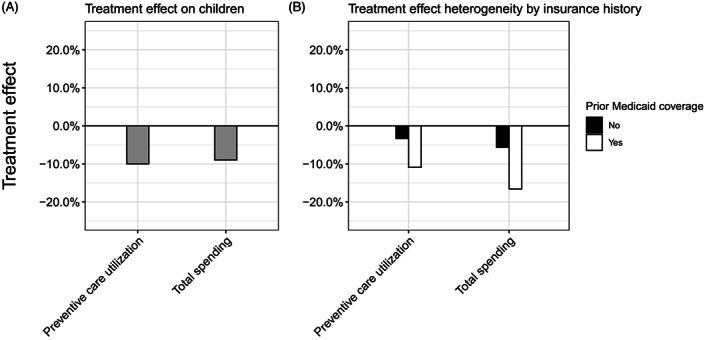
Subgroup analysis—children and prior Medicaid coverage. Panel A shows the treatment effect for children only. Panel B shows the treatment effect of people in families with and without prior coverage by Medicaid. Source: Author analysis
In panel B, we evaluated whether a member of the household was previously covered by Medicaid and used that as an indicator that the household was more likely to be lower income than households without prior Medicaid coverage. We found that the treatment effect was significantly more pronounced for households with prior Medicaid coverage than for families without prior Medicaid coverage. This result was consistent with the idea that low‐income families have smaller buffers to endure the financial consequences of hospitalizations, causing them to forgo more future health care spending than higher‐income households.
Finally, we asked whether there were institutional features that were associated with an attenuation of the impact of hospitalization on the at‐risk household members in our sample (Figure 4). We specifically focused on two attributes that may have offset the adverse consequences of hospitalization: (1) sharing the same PCP and (2) having a plan with a family deductible. A common PCP across the hospitalized individual and at‐risk family members will result in PCP awareness of the hospitalization of a family member and may allow for more effective patient care and advocacy by the PCP. The evidence presented in Figure 4, panel A is consistent with this interpretation. The treatment effect for at‐risk household members who shared a PCP with the hospitalized household member was significantly lower compared to at‐risk household members who did not share the same PCP. We found similar results when we limited the at‐risk household members to children. Note that there is an alternative explanation for this result. If family members share a PCP scheduling their office visits may be more convenient which could prevent the reduction in health care utilization. We tested this channel by evaluating whether family members who did not share a PCP but whose PCPs worked in the same practice displayed similar attenuations of the treatment effect. We find that it does not. These results are included in Appendix E.
FIGURE 4.
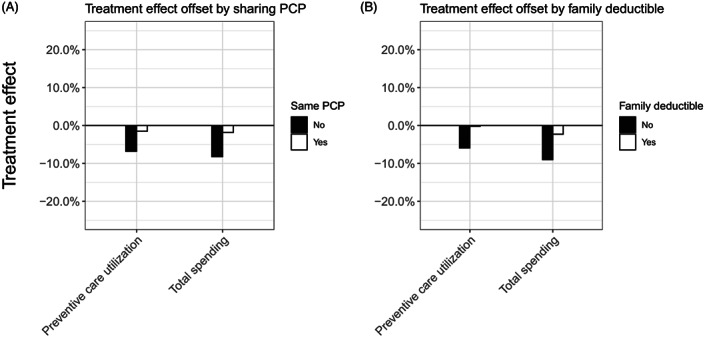
Treatment effect attenuation by shared Primary Care Physician and family deductibles. This figure shows how sharing a Primary Care Physician with the hospitalized family member and having a family deductible attenuates the effect of having a hospitalized family member on medical spending and the use of preventive care. Source: Author analysis
In panel B, we examined whether a family deductible (versus only individual deductibles) reduced the likelihood that household members of hospitalized individuals would forgo future health care. The findings indicated that they did: the treatment effect was significantly less pronounced for households who were on health insurance plans with a family deductible.
4. DISCUSSION
Our study examined the health care utilization of household members of unexpectedly hospitalized individuals. We found that these household members reduced their consumption of non‐urgent care. Specifically, we found that at‐risk household members had fewer ambulatory office visits and reduced their use of other ambulatory care including high‐value preventive care. While this pattern is consistent with patients reducing their health care utilization when facing financial constraints, it is important to note that the reduction may also be driven by the time and cognitive burdens associated with hospitalizations in the household. Our study found that the main effect applies to children too and is exacerbated for low‐income families. Two institutional features—family deductibles and shared PCPs—may attenuate these negative consequences. These results build on prior work conducted in the United States that describes the financial consequences of unexpected hospitalizations and extends it by demonstrating how the consequences of a hospitalization spread within families and negatively impact their health care utilization.
This research highlights how family relationships shape the health care that people consume. Unexpected medical events can impose a financial burden not just on those who are hospitalized but also on their family members. These adverse outcomes have the potential to propagate within families and exacerbate financial and health inequalities. Specifically, while the effects of hospitalizations were substantial on average, they were especially pronounced for low‐income families. The effects described in this study were almost twice as large for low‐income families than for non‐low‐income families. If the lack of current health care use will drive an increased risk of health issues in the future, low‐income families may continue to fight an uphill battle. It is important to note that at the time of hospitalization none of these families were on Medicaid. Medicaid offers no family plans and our sampling strategy relied on identifying hospitalized individuals on family plans at the time of hospitalization. This means that for families with even lower incomes (i.e., those on Medicaid at the time of hospitalization), the consequences might be even more pronounced.
Our study examines two institutional features that may safeguard families from substantial reductions in their health care use. First, our results suggest that a family deductible has the potential to partially shield families from substantial reductions in health care use. Research on family deductibles is relatively scarce and it is unclear how common they are across the United States and how patients value these deductibles when choosing their insurance plan. Based on our findings, however, we believe that future work should examine these questions. Second, we demonstrated that sharing a PCP with your family member may attenuate the effect of hospitalization on a family member's health care use. Additional analyses suggest that the mechanism that is likely to underlie these results is PCP awareness. Specifically, privacy constraints often prevent PCPs from being informed about important family events that may affect their patients. However, when family members share a PCP, the PCP is likely to be better attuned to challenges that a family may face. Not only does this finding highlight the importance of patient‐provider communication within the context of navigating US health care provision, but it also raises the question of whether family members should select similar rather than different health care providers.
Our study had limitations. First, we were only able to analyze health care spending and utilization. When faced with an unexpected hospitalization, household budgets may be reallocated across multiple domains, not just health care. 6 Second, we did not have access to pharmaceutical data. Prescription drug spending is commonly shown to be an area in which patients reduce or delay utilization 19 which implies that our results likely underestimated total health care reallocations. Third, we lacked individual income data. Instead, we followed prior research 20 , 21 and relied on prior Medicaid enrollment as a proxy for low‐income status. Fourth, our definition of a family was based on being enrolled in the same insurance plan at the same time. Thus, our results may not generalize to households where individuals are enrolled in separate insurance plans. Fifth, some of the differences in outcomes we observe might be due to delays in health care utilization, not forgoing it. In Appendix C, we evaluated this concern in more detail. Sixth, our data do not include detailed information about the size of the individual and family deductibles. Seventh, we cannot fully disentangle the financial burden from the time and cognitive burden as the main cause of the reduction in health care utilization. Analyses on how financial status (as measured through prior Medicaid coverage and having a family deductible) moderates the main effect are suggestive of financial burden playing an important role, but they do not rule out time and cognitive factors as an important driver. Because these two causes are likely to require different mitigation strategies, future work should try to document the extent to which these two causes contribute to reduced health care use. Finally, given the limited time frame, we could not evaluate the long‐term consequences of delayed or forgone medical care. While some research has demonstrated the long‐term benefits of preventive care, it was outside of the scope of this study to formally test this. 22
In sum, these findings suggest that the consequences of severe medical events may spread within family households. Policy makers working on making health care more equitable should consider strategies to promote continuity of care and our research suggests that there is an important role for family deductibles and that awareness among providers about health episodes within the family may safeguard against disruption in care provision.
FUNDING INFORMATION
The authors have no funding to report.
CONFLICT OF INTEREST
The authors report no conflict of interest.
ACKNOWLEDGMENTS
The authors would like to thank the Center for Health Information and Analysis (CHIA) for providing access to the Massachusetts All‐Payer Claims Database (MA APCD) and the editors and anonymous reviewers for their comments and suggestions.
APPENDIX A.
A.1.
A.1. Sample construction
One of the main objectives of our sampling strategy was to identify hospitalizations that could serve as “treatment events,” that is, the family events that we predict to affect the health care spending and utilization of family members. The starting point of our sample selection process was the identification of all inpatient hospital facility claims that were labeled “emergent” or “urgent” admissions between 01/01/2011 and 01/01/2015. The date restrictions allow us to observe at least 1 year of outcome data prior to the hospitalization and at least 1 year of outcome data post‐hospitalization. We only sampled observations with a correct discharge date (i.e., discharge date after admission date) and without diagnosis and procedure codes related to pregnancies. Since our goal is to obtain inpatient episodes (rather than single claims), we identified consecutive stay dates and grouped them into a single hospitalization event.
The next step was to evaluate whether the hospitalized individual was covered by a family health insurance plan at the time of hospitalization. If they were not, we dropped those cases. If they were, we identified the family members on the plan. We refer to these people as at‐risk family members. Given that the goal of our analysis is to examine the effect of hospitalization of one household member on the health care utilization of another household member, we excluded hospitalizations if another household member was hospitalized within 2 weeks of the initial hospitalization. We did this to be able to link the treatment effect to the hospitalization of a family member rather than a common shock. A common shock—such as an accident that involved multiple family members—is likely to have a direct effect on the at‐risk family member, even in the absence of hospitalization of another family member.
We took three more sampling steps to arrive at our final sample. First, because our focus was on hospitalizations between 5 and 90 days, the next step was to drop all cases with shorter and longer hospitalizations. And second, because some individuals in our sample appear multiple times due to multiple hospitalizations, we dropped all hospitalization events that were not the first in our sample.
Based on the resulting sample of treatment events, we examined whether limiting the initial hospitalizations to those labeled emergent or urgent was sufficient to only identify unexpected hospitalizations. We did so by computing and plotting the medical spending of the hospitalized individuals in our sample in the 24 months leading up to the hospitalization. The results are shown in Figure A1, panel A. The graph clearly shows that there is an upward trend in spending that starts about 5 months prior to the hospitalization. To ensure that our sample of hospitalizations only included unanticipated hospitalizations, we identified all individuals in our sample that experienced either a spending increase in the 6 months prior to hospitalization (by identifying those cases in which spending and an indicator for each month relative to the hospitalization month displayed a positive and significant correlation coefficient) or increased spending in the month prior to hospitalization by more than three standard deviations above a patient's mean 12 months pre‐hospitalization spending. We excluded these people from our sample and again plotted the spending patterns relative to the time prior to hospitalization. The results are shown in Figure A1, panel B. The flat spending pattern is consistent with our sample including only unexpected hospitalizations.
FIGURE A1.
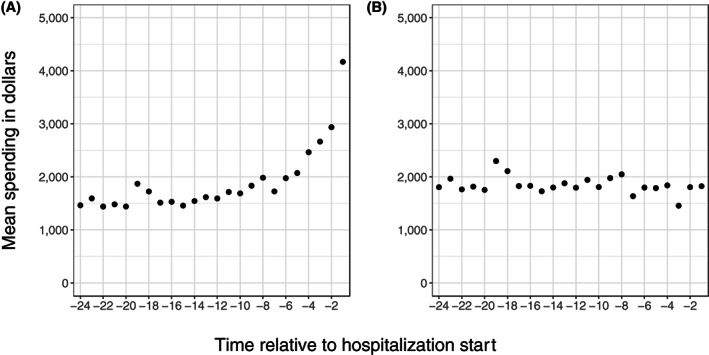
Change in spending patterns of a hospitalized family member
In Figure A2, we have included a flow chart with the sampling steps we have taken as well as the sample size at each of these steps.
FIGURE A2.
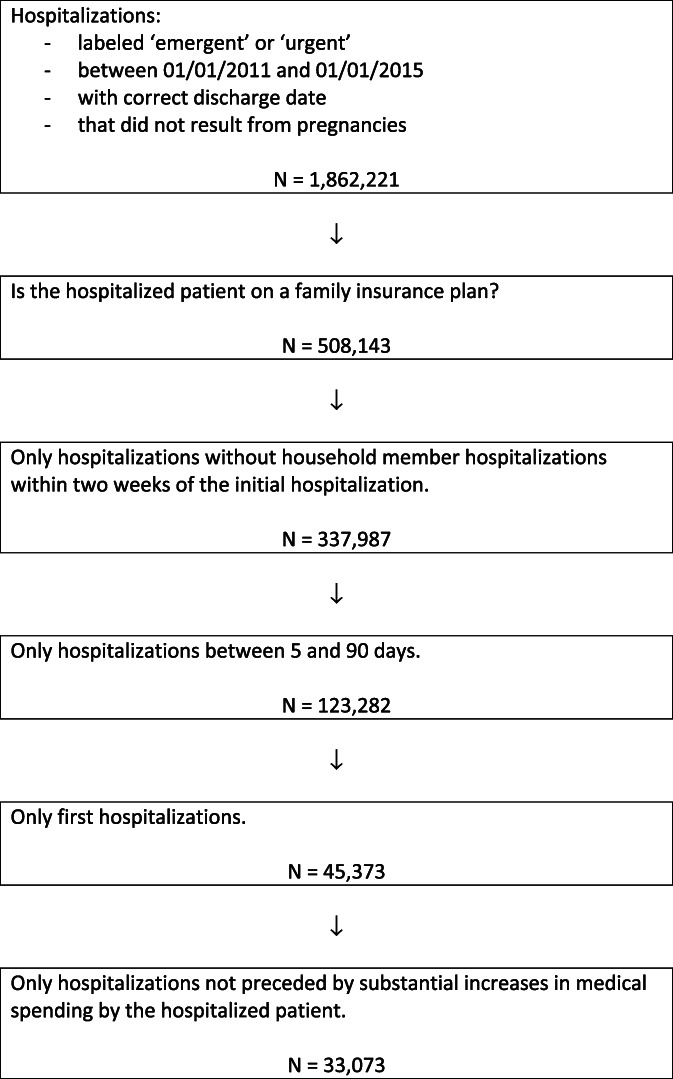
Flow chart of sampling steps
After performing these sampling steps, we matched each “treatment family” to a control family. We do so by identifying all families with a hospitalization event in January 2011 and matching them with all families who will experience a hospitalization event in February 2012. We then iterate over the data by month until the final treatment cohort in November 2014 is matched with the final control cohort that will experience a hospitalization event in December 2015. For this analytic sample, we merged demographic data, outcome data, and data describing the hospitalization event. We then evaluated the similarity between treatment and control cases based on observables. The results are shown in Table A1. In the table, we compare the treatment to control cases. It shows that some families are used as both treatment and control cases while others are used only as treatment or control cases. For example, a family hospitalized in February 2012 will be used as both a treatment and control case. Families with hospitalizations in January 2011 will be used as treatment cases only while families with hospitalizations in December 2014 will be used as control cases only. Note, however, that families are never compared against themselves. The table further shows that treatment and control cases are very similar based on observables which suggest that our sampling strategy may have allowed us to think of our hospitalization events as having quasi‐random timing.
TABLE A1.
Balance table
| Treatment | Control | |
|---|---|---|
| Family observations | 33,073 | 33,073 |
| Both treatment and control | 18,395 | 18,395 |
| Treatment or control only | 14,678 | 12,525 |
| Average day of month stay start | 15.9 | 15.9 |
| Female, hospitalized (%) | 44 | 45 |
| Female, at‐risk (%) | 53 | 53 |
| Length of stay | ||
| 5–7 days | 60 | 60 |
| 8–14 days | 29 | 29 |
| 15–30 days | 9 | 9 |
| 31–90 days | 2 | 2 |
| Average number of family members | 3.1 | 3.1 |
| Family structures (%) | ||
| 2 adults, 1–3 children | 23 | 22 |
| 2 adults only | 20 | 21 |
| 2 elder adults only | 12 | 14 |
| 2 adults, 1–3 young adults | 11 | 11 |
| 1 adult, 1 elder adult | 6 | 6 |
| 1 adult, 1–3 children | 6 | 5 |
| 2 adults, 1 young adult, 1 child | 5 | 5 |
| Other | 17 | 16 |
Note: Child is defined as age <18, Young Adult 19–26, Adult 27–64, and Elder Adult 65+.
APPENDIX B.
B.1.
B.1. Difference‐in‐differences
Recent research has demonstrated that the Two‐Way Fixed Effects strategy which was often used to estimate difference‐in‐differences (DID) models with staggered treatment events may introduce weighting issues that can seriously affect the estimates produced by the model. To overcome these issues, researchers have proposed a variety of solutions each of which rests on different assumptions. The results presented in the main text of this paper were obtained using the method described in Cengiz et al. 14 Specifically, for each month between January, 2011 and December, 2014, we match (only on date) families that experience a hospitalization in month t to families that will experience a hospitalization in month t + 12. We then give each of these groups of treatment and control families a cohort ID and these cohort IDs can be used to limit comparisons to treatment and control family members within a cohort. Specifically, the inclusion of patient by cohort and time by cohort fixed effects in a regression model will effectively address the weighting issues identified in recent work. Thus, our design compares families that are treated earlier to families that are treated later. Because we show that the hospitalizations in our data are likely unexpected, timing of our “treatment” is plausibly exogenous. The regression equation used to obtain the coefficient estimates is as follows:
Where the first summation in captures the time periods leading up to the treatment (“leads”) and the second summation captures the time periods following treatment (“lags”). The first two terms refer to the patient by cohort and time by cohort fixed effects, respectively.
To ensure that our results are not unique to the estimation method used, we replicate our results using three other approaches that were proposed recently. Specifically, we take the four main outcome measures in our paper and estimate the effect of treatment using the methods proposed by Roth and Sant'Anna, 16 Callaway and Sant'Anna, 17 and Sun and Abraham. 18 The results are shown in table B1 and suggest two main takeaways: (1) the estimates presented in the main text can all be replicated using alternative estimation methods and (2) the effect sizes presented in the main text are most in line with the effect sizes using the Roth and Sant'Anna19 method, which is the most conservative method.
TABLE B1.
Evaluating robustness of the DID estimation results
| Method | Log(spending) | Office Visits | Preventive Care | Ambulatory care | ||||
|---|---|---|---|---|---|---|---|---|
| Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE | |
| Roth and Sant'Anna 16 | −0.0715 | 0.0108 | −0.0039 | 0.0014 | −0.0026 | 0.0007 | −0.0082 | 0.0016 |
| Callaway and Sant'Anna 17 | −0.1744 | 0.0144 | −0.0193 | 0.0021 | −0.0069 | 0.0013 | −0.0230 | 0.0023 |
| Sun and Abraham 18 | −0.1680 | 0.0216 | −0.0196 | 0.0029 | −0.0054 | 0.0016 | −0.0203 | 0.0033 |
Note: Each of the estimates presented in this table is significantly different from 0.
APPENDIX C.
C.1.
C.1. Extending the estimation horizon
In the models shown in the main text, outcome differences are evaluated for up to 1‐year post‐hospitalization. One threat that looms large is the possibility that family members delay care rather than forgoing care entirely. To examine whether this is a likely scenario, we have re‐estimated our main medical spending model using a two‐year horizon. The results are shown in Figure C1. The point estimates suggest that the effects of hospitalization of a family member are long‐lived and that delayed care, at least within a two‐year horizon, is unlikely to explain the results.
FIGURE C1.
Forgone versus delayed care [Color figure can be viewed at wileyonlinelibrary.com]
APPENDIX D.
D.1.
D.1. Other outcomes
The main argument tested in this paper is that when family members of hospitalized individuals experience financial hardship because of that hospitalization, they may exercise discretion when making decisions about their health care utilization. But what happens when that health care is emergent or for a severe medical condition? To answer this question, we examined whether emergency room visits and inpatient admissions were affected by hospitalizations of family members. Emergency room visits are identified based on procedure codes (99281, 99282, 99283, 99284, 99285, 99291, 99292), site of service codes (23), and revenue codes (0450, 0451, 0452, 0453, 0454, 0455, 0456, 0457, 0458, 0459, 0981). Inpatient admissions are identified using site of service codes (21 and 51) and facility codes (11). The results are shown in Figure D1. We find that neither emergency room visits nor inpatient admissions follow the same trends as the other outcomes we studied.
FIGURE D1.
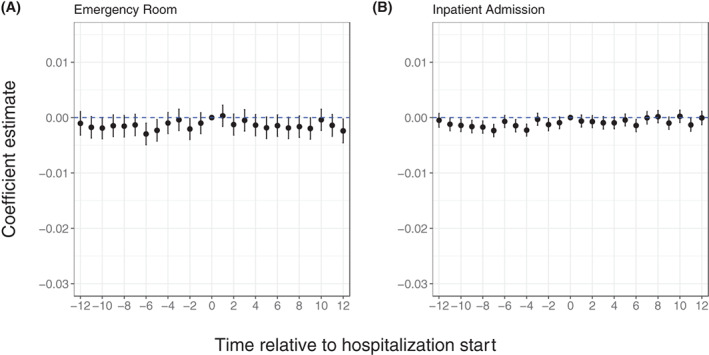
Emergency room use and inpatient admissions [Color figure can be viewed at wileyonlinelibrary.com]
An open question is whether the observed reduction in office visits is partly driven by fewer referrals from PCPs to medical specialists. To test this question, we used the same empirical strategy that underlies the estimates shown in Exhibit 2 and estimate the effect of hospitalization of a family member on the probability of seeing a medical specialist for an office visit while adjusting for whether the patient had visited its PCP. The results are shown in Figure D2. When we conditioned on seeing one's PCP, we find that there is a significant and substantial decrease in the probability of visiting a medical specialist following the hospitalization of a family member.
FIGURE D2.
Specialist office visits [Color figure can be viewed at wileyonlinelibrary.com]
Figure D3 demonstrates that family member hospitalizations do not impact the use of low‐value care (see Table F2 in Appendix F for the list of procedures used to label low‐value care—this list follows the definition of low‐value care used in prior work 11 ) A possible explanation for this null effect is that the sample of families we study comprises two latent subgroups and that one of these subgroups is more likely than the other to seek medical care that is considered low‐value. Consider, for example, one group that responds to financial constraints by cutting back health care utilization and another group that prioritizes health care and reduces spending in non‐health care domains. If this latter group is the group that is most likely to seek low‐value care, it is not surprising that we do not find an effect. Prior work 23 has demonstrated that an important reason why physicians provide low‐value care is patient demand and satisfaction. In sum, we think that one explanation for the result is that the latent subgroup of patients that is unresponsive to the treatment is also the subgroup with the strongest demand for low‐value care.
FIGURE D3.
Low‐value care [Color figure can be viewed at wileyonlinelibrary.com]
APPENDIX E.
E.1.
E.1. Estimated coefficients for exhibits 3 and 4
In Table E1, we present the coefficients of the regression models used to examine the treatment effects on the two subgroups: children and families with Medicaid coverage in the 2 years prior to the hospitalization. These estimates were used to generate Exhibit 3. The first column shows the effect of treatment on the medical spending of the children in our sample while the third column shows the effect on the use of preventive care. Both models show that children are at least as affected by hospitalizations in the family as adults. In model 2 and model 4, we demonstrate that the treatment effect is substantially stronger for families with prior Medicaid coverage than for families without a history of Medicaid coverage.
TABLE E1.
Treatment effect on subgroups
| Log(Spending) | P(Preventive Care = 1) | |||
|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |
| Treat * Post | −0.088*** | −0.056*** | −0.005*** | −0.002*** |
| (0.016) | (0.010) | (0.001) | (0.001) | |
| Treat * Post * Past Medicaid | −0.112** | −0.007** | ||
| (0.041) | (0.003) | |||
| Patient i * cohort Fes | Yes | Yes | Yes | Yes |
| Time * cohort Fes | Yes | Yes | Yes | Yes |
| Num. Obs. | 1,047,644 | 3,459,950 | 1,047,644 | 3,459,950 |
| Sample | Children | Full | Children | Full |
Note: *p < 0.05; **p < 0.01; ***p < 0.001.
In Table E2, we present the coefficients of the regression models used to examine potential offsets of the treatment effect by evaluating the role of shared PCPs and family deductibles. As discussed in the main text of this paper, the coefficients suggest that sharing a PCP of having a family deductible significantly attenuates the negative effect of hospitalizations in the household on the health care utilization of its members.
TABLE E2.
The attenuating effects of shared PCPs and family deductibles
| Log(Spending) | P(Preventive Care = 1) | |||
|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |
| Treat * Post | −0.084*** | −0.086*** | −0.005*** | −0.004*** |
| (0.015) | (0.012) | (0.001) | (0.001) | |
| Treat * Post * Shared PCP | 0.073** | 0.004* | ||
| (0.024) | (0.002) | |||
| Treat * Post * Family deductible | 0.068** | 0.004* | ||
| (0.024) | (0.002) | |||
| Patient i * cohort Fes | Yes | Yes | Yes | Yes |
| Time * cohort Fes | Yes | Yes | Yes | Yes |
| Num. Obs. | 1,815,060 | 2,718,014 | 1,815,060 | 2,718,014 |
| Sample | Full | Fam size >2 | Full | Fam size >2 |
Note: *p < 0.05; **p < 0.01; ***p < 0.001.
In Table E3, we evaluate the mechanism driving the shared PCP results. One interpretation of the shared PCP results presented in Table E2 is that a shared PCP will be aware of the medical adversity faced by the hospitalized patient and may be more proactive in coordinating the care of the patient's family members. An alternative explanation is that a shared PCP means that two family members can receive care in the same practice location. If the hospitalized patient needs to visit the PCP following the hospitalization it may be convenient for the family member to schedule a visit for him or herself as well. To test this second explanation, we construct a variable that equals one if two family members do not share a PCP but their PCPs practice in the same location. If the attenuation of the treatment effect is driven by sharing a practice location but not by sharing a PCP, one would expect that sharing the same location in the absence of sharing a PCP would also attenuate the treatment effect. The results are presented in Table E3. Although the coefficient of interest is positive, we find no significant attenuating effect of having the same practice location only, suggesting that the awareness interpretation is most plausible (Tables F1 and F2).
TABLE E3.
Shared PCP or same practice?
| Log(Spending) | ||
|---|---|---|
| (1) | (2) | |
| Treat * Post | −0.084*** | −0.087*** |
| (0.015) | (0.012) | |
| Treat * Post * Shared PCP | 0.073** | 0.079** |
| (0.024) | (0.021) | |
| Treat * Post * Same Practice | 0.074 | |
| (0.043) | ||
| Patient i * cohort Fes | Yes | Yes |
| Time * cohort Fes | Yes | Yes |
| Num. Obs. | 1,815,060 | 1,815,060 |
APPENDIX F.
TABLE F1.
List of preventive care procedures plus modifiers
| Procedure | Modifier |
|---|---|
| Alcohol Misuse Screening & Counseling | |
| Annual Wellness Visit | |
| Bone mass measurements | |
| Cardiovascular disease screening tests | |
| Cervical Cancer Screening with Human Papillomavirus Tests | Women 21–65 |
| Colorectal cancer screening | Men 50–75 |
| Counseling to prevent tobacco use | |
| Depression screening | |
| Diabetes screening | |
| Diabetes self‐management training | |
| Flu shot and administration | |
| Glaucoma screening | Adults over 40 |
| Hepatitis B screening | |
| Hepatitis B shot and administration | |
| Hepatitis C screening | |
| HIV screening | |
| IBT for cardiovascular disease | |
| IBT for obesity | |
| Initial preventive physical exam | |
| Lung cancer screening | Adults 50–80 |
| Mammography screening | Women 40–74 |
| Medical Nutrition Therapy | |
| Pap tests screening | Women 21–65 |
| Pneumococcal Shot & Administration | |
| Prolonged preventive services | |
| Prostate cancer screening | Men 55–69 |
| Sexually Transmitted Infection (STI) Screening & High‐Intensity Behavioral Counseling to Prevent STIs | |
| Ultrasound AAA screening | Men 65–75 |
TABLE F2.
List of low‐value care procedures plus modifiers
| Procedure | Modifier |
|---|---|
| CT scan of sinuses for acute sinusitis | |
| Head imaging for uncomplicated headache | |
| Back imaging for non‐specific low back pain | |
| Colorectal cancer screening | Men under 50 |
Bergquist S, de Vaan M. Hospitalizations reduce health care utilization of household members. Health Serv Res. 2022;57(6):1274‐1287. doi: 10.1111/1475-6773.14050
REFERENCES
- 1. Collins SR, Aboulafia GN, Gunja MZ. As the pandemic eases, what is the state of health care coverage and affordability in the U.S.? 2021. Accessed January 07, 2022. Available at: https://www.commonwealthfund.org/publications/issue-briefs/2021/jul/as-pandemic-eases-what-is-state-coverage-affordability-survey.
- 2. Kearney A, Hamel L, Stokes M, Brodie M. Americans' challenges with health care costs. 2021. Accessed January 7, 2022. Available at: https://www.kff.org/health-costs/issue-brief/americans-challenges-with-health-care-costs/.
- 3. Bethune S. Majority of Americans stressed by health insurance costs. Accessed January 07, 2022. Available at: https://www.apa.org/monitor/2018/04/insurance-costs.
- 4. Hamel L, Muñana C, Brodie M. Kaiser Family Foundation/LA times survey of adults with employer‐sponsored health insurance. 2019. Accessed January 07, 2022. Available at: https://www.kff.org/private-insurance/report/kaiser-family-foundation-la-times-survey-of-adults-with-employer-sponsored-insurance/.
- 5. Chen S, Shafer PR, Dusetzina SB, Horný M. Annual out‐of‐pocket spending clusters within short time intervals: implications for health care affordability. Health Aff. 2021;40:274‐280. [DOI] [PubMed] [Google Scholar]
- 6. Dobkin C, Finkelstein A, Kluender R, Notowidigdo MJ. The economic consequences of hospital admissions. Am Econ Rev. 2018;108:308‐352. [PubMed] [Google Scholar]
- 7. Fadlon I, Nielsen TH. Family labor supply responses to severe health shocks: evidence from Danish administrative records. Am Econ J Appl Econ. 2021;13:1‐30. [Google Scholar]
- 8. Cha AE, Cohen RA. Problems paying medical bills, 2018. NCHS Data Brief. 2020;357:1‐8. [PubMed] [Google Scholar]
- 9. Fadlon I, Nielsen TH. Family health behaviors. Am Econ Rev. 2019;109:3162‐3191. [Google Scholar]
- 10. Newhouse JP. Free for all? Lessons from the RAND Health Insurance Experiment. Harvard University Press; 1993. [Google Scholar]
- 11. Brot‐Goldberg ZC, Chandra A, Handel BR, Kolstad JT. What does a deductible do? The impact of cost‐sharing on health care prices, quantities, and spending dynamics. Q J Econ. 2017;132:1261‐1318. [Google Scholar]
- 12. Lucifora C, Vigani D. Health care utilization at retirement: the role of the opportunity cost of time. Health Econ. 2018;27:2030‐2050. [DOI] [PubMed] [Google Scholar]
- 13. Preventive Services Chart | Medicare learning network®. 2022. Accessed March 01, 2022. Available at: https://www.cms.gov/Medicare/Prevention/PrevntionGenInfo/medicare-preventive-services/MPS-QuickReferenceChart-1.html.
- 14. Cengiz D, Dube A, Lindner A, Zipperer B. The effect of minimum wages on low‐wage jobs. Q J Econ. 2019;134:1405‐1454. [Google Scholar]
- 15. Goodman‐Bacon A. Difference‐in‐differences with variation in treatment timing. J Economet. 2021;225:254‐277. [Google Scholar]
- 16. Roth J, Sant'Anna PHC. Efficient estimation for staggered rollout designs. arXiv preprint arXiv:2102.01291, 2021. Accessed June 13, 2022.
- 17. Callaway B, Sant'Anna PHC. Difference‐in‐differences with multiple time periods. J Economet. 2021;225:200‐230. [Google Scholar]
- 18. Sun L, Abraham S. Estimating dynamic treatment effects in events studies with heterogeneous treatment effects. J Economet. 2021;225:175‐199. [Google Scholar]
- 19. Piette JD, Heisler M, Krein S, Kerr EA. The role of patient‐physician trust in moderating medication nonadherence due to cost pressures. Arch Intern Med. 2005;165:1749‐1755. [DOI] [PubMed] [Google Scholar]
- 20. Schechter MS, Shelton BJ, Margolis PA, Fitzsimmons SC. The association of socioeconomic status with outcomes in cystic fibrosis patients in the United States. Am J Respir Crit Care Med. 2001;163:1331‐1337. [DOI] [PubMed] [Google Scholar]
- 21. Quittner AL, Schechter MS, Rasouliyan L, Haselkorn T, Pasta DJ, Wagener JS. Impact of socioeconomic status, race, and ethnicity on quality of life in patients with cystic fibrosis in the United States. Chest. 2010;137:642‐650. [DOI] [PubMed] [Google Scholar]
- 22. The Diabetes Prevention Program Research Group . The 10‐year cost‐effectiveness of lifestyle intervention or metformin for diabetes prevention: an intent‐to‐treat analysis of the DPP/DPPOS. Diabetes Care. 2012;35:723‐730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Colla CH, Mainor AJ. Choosing Wisely campaign: valuable for providers who knew about it, but awareness remained constant. Health Aff. 2017;36:2005‐2011. [DOI] [PubMed] [Google Scholar]


