Dear Editor-in-Chief
To investigate the association between disease outbreaks and exposure to particulate matter (PM), different rodent models are directly administered varying doses of PM to verify the progress of the disease (1). The PM treatment methods used for this purpose include intratracheal instillation (ITI), intranasal instillation (INI), whole-body inhalation (WI), and nose-only inhalation (NI) (1,2).
ITI is the most widely used method for evaluating respiratory toxicity and is performed by injecting PM directly into the airway or bronchial tubes using a syringe (1,3). It has the advantage of being able to most effectively confirm the harmfulness of PM compared with other methods; however, it has some disadvantages. Notably, the conditions under which ITI is performed are different to those of exposure to PM in the actual atmospheric environment. This is because a high concentration of PM is artificially injected into the bronchial tubes (1,2).
INI can be regarded as a method that more realistically mimics the conditions of the actual atmospheric environment than ITI. The inner wall of the nose has well-developed blood vessels and is surrounded by a thin layer of mucus; therefore, inhaled PM easily stimulates epithelial cells. Thus, INI is proposed as a suitable method for evaluating the influence of PM on the body (1). However, as the treatment is limited to a small region inside the nose, there is a considerable difference in the amount of PM absorbed, and thus, the difference in the amount of PM administered between groups in animal experiments may be large (1,4).
WI is a treatment method that continuously supplies air containing PM to the chamber where experimental animals are raised such that PM naturally enters the body through the respiratory organs. The conditions of this method most closely resembles those of the actual atmospheric environment (1,2,5). However, dedicated facilities and spaces to continuously supply PM to the chamber may be required, and long-term treatment may be required when this method is compared with ITI and INI (1,2). As described above, various PM treatment methods are used to demonstrate the health hazards posed by exposure to PM, and each approach has its own advantages, limitations, and study design requirements.
Considering that air pollutants, including PM, globally threaten public health, appropriate experimental methods that are more convenient to perform and can investigate the mechanisms of action of translocated particles are required, in addition to the experimental methods described above. Subsequently, this study aimed to demonstrate changes in the severity of systemic inflammation due to different PM administration approaches and verify the usefulness of intravenous (IV) and intraperitoneal (IP) methods by injecting PM10 into experimental animals via these methods.
In this study, 27 4-week-old C57BL/6 mice from Samtako (Osan, Korea) were used in the experiments after a week-long environmental adaptation period.
The study protocol was approved by the animal Ethics Committee of the National Research Foundation of Korea (2020S1A5A8047345).
During the experimental period, water and diet were supplied ad libitum, and 9 mice were randomly assigned to each of the control (CO), IV, and IP groups. For PM treatment, PM10 (ERMCZ120) was purchased from Sigma-Aldrich (St. Louis, USA) and injected twice per week at intervals of 2–3 days for 8 weeks. In the IV group, PM was injected into the tail vein, and in the IP group, 50 μl of PM was injected into the peritoneal cavity. Conversely, the CO group was alternately injected with 50 μl of phosphate-buffered saline into the tail vein and peritoneal cavity once a week. Changes in systemic inflammation levels were verified by measuring the serum levels of interleukin (IL)-6, IL-1β, and tumor necrosis factor (TNF)-α using the blood samples collected from the abdominal inferior vena cava using ELISA kits (R&D Systems, Minneapolis, USA). Statistical analysis was carried out using SPSS 26.0 software (IBM Corporation, Armonk, USA), and differences between groups were verified by one-way analysis of variance.
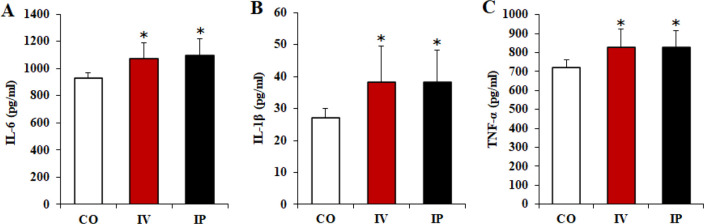
Changes in serum IL-6, IL-1β, and TNF-α levels according to PM treatment using IV and IP methods are shown in Fig. 1. Based on the results of the 8-week treatment, IV and IP groups showed significantly higher serum IL-6, IL-1β, and TNF-α levels than the CO group (P<0.05). However, there was no significant difference among treatment methods (P>0.05). These results suggest that PM administration may trigger a systemic inflammatory response and that both IV and IP methods may be valid treatment methods to verify the harmfulness of PM in rodent models.
Fig. 1:
Changes in serum IL-6 (A), IL-1β (B), and TNF-α (C) levels according to PM treatment. Data are presented as mean ± standard deviation. *versus CO group (P<0.05)
This suggests that future studies will need to verify the severity of inflammation in various target organs, such as the lungs, heart, liver, kidneys, and brain, in addition to the systemic inflammatory response to confirm the health hazards posed by PM exposure.
Acknowledgements
This work was supported by the Ministry of Education of the Republic of Korea and the National Research Foundation of Korea (NRF-2020S1A5A8047345).
References
- 1.Choi JK, Choi IS, Cho KK, et al. (2020). Harmfulness of Particulate Matter in Disease Progression. J Life Sci, 30(2):191–201. [Google Scholar]
- 2.Shang Y, Sun Q. (2018). Particulate air pollution: major research methods and applications in animal models. Environ Dis, 3(3):57–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Helms MN, Torres-Gonzalez E, Goodson P, et al. (2010). Direct tracheal instillation of solutes into mouse lung. J Vis Exp, (42):1941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vidgren MT, Kublik H. (1998). Nasal delivery systems and their effect on deposition and absorption. Adv Drug Deliv Rev, (42)(1–2):157–177. [DOI] [PubMed] [Google Scholar]
- 5.Curbani F, de Oliveira Busato F, do Nascimento MM, et al. (2019). Inhale, exhale: Why particulate matter exposure in animal models are so acute? Environ Pollut, 251:230–237. [DOI] [PubMed] [Google Scholar]