Abstract
The potential use as vaccine delivery system of Salmonella typhimurium strains harboring defined mutations in the sseC (HH104) and sseD (MvP101) genes, which encode putative effector proteins of the type III secretion system of Salmonella pathogenicity island 2, was evaluated and compared with that of the well-characterized aroA mutant strain SL7207 by using β-galactosidase (β-Gal) as a model antigen. When orally administered to immune-competent or gamma interferon-deficient (IFN-γ−/−) BALB/c mice, both mutants were found to be highly attenuated (50% lethal dose, >109 bacteria). Both strains were also able to efficiently colonize and persist in Peyer’s patches. Immunization with HH104 and MvP101 triggered β-Gal-specific serum and mucosal antibody responses equivalent to or stronger than those observed in SL7207-immunized mice. Although immunoglobulin G2 (IgG2) serum antibodies were dominant in all groups, IgG1 was also significantly increased in mice vaccinated with MvP101 and SL7207. Comparable β-Gal-specific IgA and IgG antibodies were detected in intestinal lavages from mice immunized with the different strains. Antigen-specific CD4+ T-helper cells were generated after vaccination with all vaccine prototypes; however, responses were significantly more efficient when HH104 and MvP101 were used (P < 0.05). Significantly higher levels of IFN-γ were produced by restimulated spleen cells from mice immunized with HH104 than from those vaccinated with the MvP101 or SL7207 derivatives (P ≤ 0.05). Interestingly, the three strains induced major histocompatibility complex class I-restricted CD8+ cytotoxic T cells against β-Gal; however, cytotoxic T-lymphocyte responses were significantly stronger after immunization with HH104 (P < 0.05). These novel S. typhimurium attenuated strains constitute promising delivery systems for vaccine antigens. The qualitative differences observed in the obtained responses with different carriers may be useful for those applications in which a targeted immunomodulation is required.
Vaccination constitutes the most cost-effective tool for the prophylaxis of infectious diseases. Most pathogenic microorganisms either are restricted to the mucosal membranes or need to transit the mucosae during the early steps of the infection (20). Therefore, the elicitation of an efficient immune response at the mucosal level after immunization is highly desired (41). Among the available approaches for triggering an efficient mucosal response, the use of live attenuated Salmonella strains as carriers probably constitutes the most studied strategy (5, 9, 33, 35). Attenuated Salmonella strains can stimulate mucosal as well as systemic immunity against the carrier itself or coexpressed heterologous antigens (1, 3, 8, 10, 37, 44). Safe Salmonella carriers can be generated by introducing defined nonreverting mutations into the chromosome. Although a number of attenuated mutants have been constructed and even characterized in the mouse model with regard to virulence, only a few of them have been evaluated as vaccine carriers. Mutants deficient in the biosynthesis of aromatic amino acids (e.g., aroA, aroC, and aroD mutants) (17, 28) or purines (e.g., purA and purE mutants) (28) or in the production of adenylate cyclase (cya) or the cyclic AMP receptor protein (crp) (4), or with mutations affecting the global regulatory system (phoP/phoQ) (11, 14), have been the most widely characterized.
The development of strategies to stimulate appropriate effector populations according to particular needs would increase the potential of attenuated carriers in vaccinology. The presence of mutations affecting the virulence properties of the carrier, such as the impaired synthesis of essential nutrients, regulatory factors, or metabolic enzymes (4, 11, 14, 17, 28), may influence the course of infection, thereby affecting the quality of the immune response elicited. Therefore, the availability of well-characterized attenuated mutants of Salmonella might facilitate fine tuning of the immune response triggered against heterologous antigens according to clinical requirements.
Salmonella pathogenicity island 2 (SPI2) is required for bacterial systemic spread and survival within phagocytic cells (29, 38). Previous studies aimed at the characterization of the role played by the products encoded by SPI2 led to the identification of two loci, sseC and sseD, which encode putative effector proteins of the SPI2 type III secretion system (16). Salmonella typhimurium strains containing nonpolar mutations in sseC (HH104 [16]) and sseD (MvP101 [this work]) are characterized by impaired virulence, both in vitro and in vivo. This prompted us to analyze the potential of MvP101 and HH104 mutants as carrier strains for the delivery of heterologous antigens, with β-galactosidase (β-Gal) used as a model protein.
MATERIALS AND METHODS
Mice, bacterial strains, and media.
Immunocompetent BALB/c (H-2d) mice (Harlan Winkelmann GmbH, Borchen, Germany) and gamma interferon-deficient (IFN-γ−/−) BALB/c mice (Jackson Laboratory, Bar Harbor, Maine) of 6 to 12 weeks of age were maintained under standard conditions according to institutional guidelines. The bacteria used in this study were S. typhimurium NCTC 12023 (identical to ATCC 14028) and its sseC (sseC::aphT) and sseD (sseD::aphT) derivatives HH104 and MvP101, respectively, and the auxotrophic aroA mutant strain SL7207 {S. typhimurium 2337-65 derivative hisG46 DEL407[aroA::Tn1(Tcs)]} (B. A. D. Stocker). Bacterial strains were routinely grown at 37°C in Luria-Bertani broth or agar (Difco, Detroit, Mich.) supplemented with 100 μg of ampicillin per ml when required. Eukaryotic cells were grown in RPMI 1640 supplemented with 10% fetal calf serum (FCS), 100 U of penicillin per ml, 50 μg of streptomycin per ml, 5 × 10−5 M 2-mercaptoethanol, and 1 mM l-glutamine (GIBCO BRL, Karlsruhe, Germany).
Generation of a nonpolar mutation in the sseD gene.
The 3-kb EcoRI/PstI fragment from plasmid p5-2 (16) harboring the sseD gene was subcloned into pUC18, thereby generating p5-30. Then, the cassette containing the aphT gene from pSB315 (13) was recovered as a HincII fragment and inserted into EcoRV-digested p5-30. The resulting construct, in which an internal EcoRV fragment of sseD was deleted and replaced by the aphT cassette positioned in the same transcriptional orientation as sseD, was named p5-31. The insert of p5-31 was recovered after digestion with SphI and EcoRI and ligated into SphI/EcoRI-digested pGP704 (24) to generate p5-33. Plasmid p5-33 was electroporated into Escherichia coli S17-1 (λpir) and subsequently transferred by conjugation into a spontaneous nalidixic acid-resistant derivative of S. typhimurium NCTC 12023, as previously described (6). Recombinant clones in which the sseD gene was replaced by the disrupted allele containing the aphT cassette were selected by their resistance to kanamycin (50 μg/ml) and nalidixic acid (100 μg/ml). The resulting exconjugants were screened for sensitivity to carbenicillin and further characterized by Southern blot analysis (data not shown). Finally, the mutant sseD allele was transferred into a fresh S. typhimurium NCTC 12023 background by P22 transduction (21).
Plasmid and DNA manipulations.
To achieve constitutive expression of β-Gal, plasmid pAH97 (18) was electroporated into the carrier strains. DNA preparations and genetic manipulations were carried out according to standard protocols (34). Plasmid DNA transformation of bacterial cells was performed by electroporation (27). To determine plasmid stability in vitro, Salmonella mutants containing pAH97 were grown overnight at 37°C with antibiotic selection. Cultures were then diluted on consecutive days in the absence of antibiotic and incubated overnight at 37°C. On each day the percentage of bacteria carrying plasmids was determined by plating dilutions in the presence or absence of antibiotics.
Immunization protocols.
For vaccination, bacteria were grown overnight until they reached mid-log phase. Then, they were harvested by centrifugation (3,000 × g) and resuspended in 5% sodium bicarbonate. Mice were immunized four times at 15-day intervals by gently feeding them the bacterial suspension of approximately 109 CFU/mouse in a volume of approximately 30 μl. Control mice were vaccinated with the plasmidless carrier.
Determination of the LD50.
Doses ranging from 105 to 109 CFU of either S. typhimurium NCTC 12023 (wild type) or the mutants HH104 and MvP101 were orally inoculated into groups of 10 mice, and survival was recorded over a 10-day period. The 50% lethal doses (LD50) of the challenge strains were calculated by the method of Reed and Muench (32).
Determinations of bacterial counts in mouse organs.
Groups of three mice were sacrificed on days 2, 4, 10, and 20 after oral infection with 5 × 109 bacteria per mouse. Spleens and Peyer’s patches were removed and homogenized in sterile phosphate-buffered saline (PBS). The numbers of viable bacteria present in the organs were determined by plating serial dilutions on Luria-Bertani agar plates with or without antibiotics.
Sample collection.
Serum samples were collected at different time points and monitored for the presence of β-Gal-specific antibodies. At day 52 after immunization, intestinal lavages were obtained by flushing the small intestine with 2 ml of PBS supplemented with 50 mM EDTA, 0.1% bovine serum albumin, and 0.1 mg of soybean trypsin inhibitor (Sigma, Deisenhofen, Germany) per ml. Then, lavages were centrifuged (10 min at 600 × g) to remove debris, and supernatant fluids were removed and supplemented with phenylmethylsulfonyl fluoride (10 mM) and NaN3 and stored at −20°C.
Antibody assays.
Antibody titers were determined by an enzyme-linked immunosorbent assay (ELISA). Briefly, 96-well Nunc-Immuno MaxiSorp assay plates (Nunc, Roskilde, Denmark) were coated with 50 μl of β-Gal (5 μg/ml) (Boehringer, Mannheim, Germany) or S. typhimurium lipopolysaccharide (LPS) (20 μg/ml) (Sigma) in coating buffer (0.1 M Na2HPO4, pH 9.0) per well. After overnight incubation at 4°C, plates were blocked with 10% FCS in PBS for 1 h at 37°C. Serial twofold dilutions of serum in FCS-PBS were added (100 μl/well), and plates were incubated for 2 h at 37°C. After four washes with PBS–0.05% Tween 20, the following secondary antibodies were added: biotinylated γ-chain-specific goat anti-mouse immunoglobulin G (IgG), μ-chain-specific goat anti-mouse IgM, and α-chain-specific goat anti-mouse IgA antibodies (Sigma) or, to determine IgG subclass, biotin-conjugated rat anti-mouse IgG1, IgG2a, IgG2b, and IgG3 (Pharmingen, Hamburg, Germany). Plates were further incubated for 2 h at 37°C. After four washes, 100 μl of peroxidase-conjugated streptavidin (Pharmingen) was added to each well and plates were incubated at room temperature for 1 h. After four washes, reactions were developed with ABTS [2,2′-azinobis-(3-ethylbenzthiazoline-6-sulfonic acid)] in 0.1 M citrate-phosphate buffer (pH 4.35) containing 0.01% H2O2. Endpoint titers were expressed as the reciprocal log2 of the last dilution which gave an optical density at 405 nm of 0.1 unit above the values of the negative controls after a 30-min incubation.
To determine the concentration of total Ig present in the intestinal lavages, serial dilutions of the corresponding samples were incubated in microtiter plates that were coated with goat anti-mouse IgG, IgM, and IgA (Sigma) as capture antibodies (100 μl/well); serial dilutions of purified mouse IgG, IgM, and IgA (Sigma) were used to generate standard curves. Detection of antigen-specific Ig was performed as described above.
Cell proliferation assay.
Spleen cell suspensions were enriched for CD4+ T cells by using MiniMACS magnetic Ly-2 and indirect goat anti-mouse IgG microbeads according to the instructions of the manufacturer (Miltenyi Biotec GmbH, Bergisch-Gladbach, Germany). Cell preparations contained >65% CD4+ cells. Cells were adjusted to 2 × 106 cells/ml in complete medium supplemented with 20 U of recombinant interleukin 2 (rIL-2) (Pharmingen) per ml, seeded at 100 μl/well in a flat-bottomed 96-well microtiter plate (Nunc), and incubated for 4 days in the presence of different concentrations of soluble β-Gal. During the final 18 h of culture, 1 μCi of [3H]thymidine (Amersham International, Freiburg, Germany) was added to each well. The cells were harvested on paper filters (Filtermat A; Wallac, Freiburg, Germany) by using a cell harvester (Inotech, Wohlen, Switzerland), and the amount of [3H]thymidine incorporated into the DNA of proliferating cells was determined in a β-scintillation counter (Wallac 1450, MICRO-β TRILUX).
FACScan analysis.
Approximately 5 × 105 cells were incubated in staining buffer (PBS supplemented with 2% FCS and 0.1% sodium azide) with the desired antibody or combination of antibodies for 30 min at 4°C. After washes, cells were analyzed on a FACScan (Becton Dickinson, Erembodegem-Aalst, Belgium). The monoclonal antibodies (MAbs) used were fluorescein isothiocyanate-conjugated anti-CD4 and anti-CD8 (Pharmingen).
Cytokine determinations.
Culture supernatants were collected from proliferating cells on days 2 and 4 and stored at −70°C. Determinations of IL-2, IL-4, IL-5, IL-6, IL-10, and IFN-γ were performed by specific ELISA. In brief, 96-well microtiter plates were coated overnight at 4°C with purified rat anti-mouse IL-2, anti-IL-4, anti-IL-5, anti-IL-6, anti-IL-10, and anti-IFN-γ MAbs (Pharmingen). After three washes, plates were blocked and twofold dilutions of supernatant fluids were added. A standard curve was generated for each cytokine by using murine rIL-2, rIL-4, rIL-5, rIL-6, rIFN-γ, and rIL-10 (Pharmingen). Plates were further incubated at 4°C overnight. After three washes, 100 μl of biotinylated rat anti-mouse IL-2, IL-4, IL-5, IL-6, IL-10, and IFN-γ MAbs (Pharmingen) per well were added and incubated for 45 min at room temperature. After six washes, streptavidin-peroxidase conjugate was added and incubated for 30 min at room temperature. Finally, the plates were developed with ABTS.
Cytotoxicity assay.
Spleen cells were obtained from mice 14 days after the last immunization, and 2 × 106 effector cells were restimulated in vitro for 5 days in complete medium supplemented with 20 U of rIL-2 per ml and a 20 μM concentration of the βGP1 peptide (β-Gal positions 876-884 [TPHPARIGL]), which encompasses the immunodominant H-2Ld-restricted β-Gal epitope (31). After restimulation, the assay was performed by a [3H]thymidine retention method (22). In brief, P815 cells were labelled with [3H]thymidine for 4 h in either complete medium or complete medium supplemented with a 20 μM concentration of βGP1 peptide and used as target cells. After being washed, 2 × 105 labelled targets and serial dilutions of effector cells were incubated in 200 μl of complete medium for 4 h at 37°C. Cells were harvested and specific lysis was determined by the following equation [(retained cpm in the absence of effectors) − (experimentally retained cpm in the presence of effectors)/retained cpm in the absence of effectors] × 100.
Depletion of CD8+ spleen cells.
The CD8+ cell subset was depleted by using MiniMACS magnetic Ly-2 microbeads, according to the manufacturer’s instructions (Miltenyi Biotec GmbH). Depleted cell preparations contained ≤1% CD8+ cells.
Statistical analysis.
Statistical significance between paired samples was determined by Student’s t test.
RESULTS
The MvP101 and HH104 mutants of S. typhimurium are attenuated for immune-competent and IFN-γ−/− mice after administration by the oral route.
It has been previously demonstrated that SPI2 mutants are attenuated for mice when inoculated by the intraperitoneal route (16). To confirm the suitability of the MvP101 and HH104 mutants as live vaccine carriers, their level of attenuation was evaluated by determining the LD50 after oral inoculation of mice. Groups of 10 mice were fed serial dilutions of either MvP101, HH104, or the wild-type parental strain NCTC 12023, and mortality was recorded within a period of 10 days postinfection. The obtained results demonstrated that both mutants are highly attenuated when given orally to BALB/c mice (LD50 above 109 CFU) compared with the parental strain (LD50 = 6.9 × 105 CFU).
To further analyze the virulence of the generated mutants in immunodeficient mice, IFN-γ−/− BALB/c mice received 109 CFU by the oral route and their survival was recorded over a period of 30 days. The tested mutants were highly attenuated in IFN-γ−/− mice, as demonstrated by the 100% survival observed in all groups at 30 days postinfection.
In vitro stability of plasmid pAH97 in recombinant Salmonella strains.
The in vitro stability of the plasmid encoding the model antigen was determined by growing the resulting clones without antibiotic pressure. Bacteria were subcultured for 4 days, and the percentage of cells retaining the plasmid was determined by plating in the presence or absence of antibiotics. The obtained results show that pAH97 was considerably stable in all of the mutants, with approximately 58% (SL7207), 47% (MvP101), and 54% (HH104) of bacteria retaining the plasmid after 4 days of subculture.
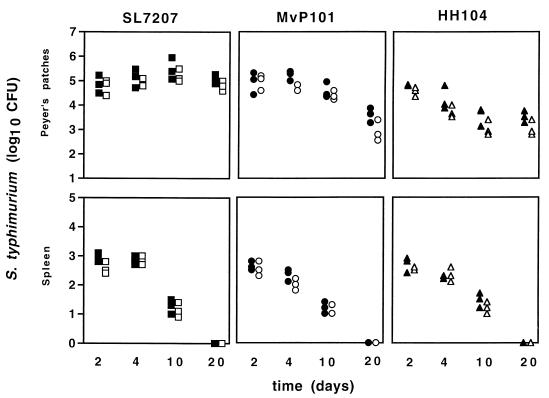
In vivo persistence of Salmonella mutants in mouse organs.
To investigate the ability of the studied mutants to colonize and persist in vivo, groups of mice were orally infected and the numbers of bacteria recovered from Peyer’s patches and spleens were determined at different time intervals. The obtained results showed that all of the strains were able to efficiently colonize and persist in Peyer’s patches (Fig. 1). In contrast, all of the mutants were rapidly cleared from spleens independently of the attenuating mutation. The in vivo stability of the plasmid in the absence of antibiotic selective pressure was similar to that observed in vitro (Fig. 1).
FIG. 1.
Persistence of Salmonella mutant strains within spleens and Peyer’s Patches of immunized mice. Mice were immunized orally with SL7207 (squares), MvP101 (circles), and HH104 (triangles) mutants of S. typhimurium expressing β-Gal. At 2, 4, 10, and 20 days postinfection, mice were sacrificed and the number of bacteria present in the Peyer’s patches (upper panel) and spleen (lower panel) of each animal was determined by plating serial dilutions in the presence (open symbols) or absence (closed symbols) of ampicillin. Each symbol represents the number of bacteria isolated from organs of individual mice.
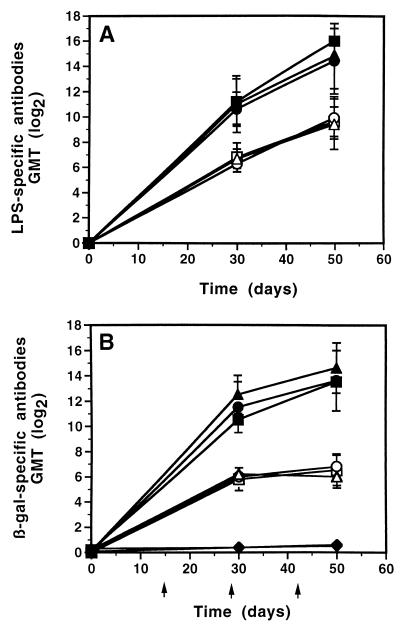
Antibody responses generated in mice orally immunized with attenuated S. typhimurium carriers expressing β-Gal.
Groups of mice (n = 5) were immunized with the recombinant strains MvP101(pAH97) and HH104(pAH97). To estimate the efficacy of the prototypes, an additional group was vaccinated with the well-established carrier strain SL7207(pAH97). Comparable LPS-specific serum antibody titers were detected in sera of immunized mice independently of the carrier employed (Fig. 2A). The ability of the different carriers to induce a systemic humoral response against the heterologous antigen was determined by measuring the titers of β-Gal-specific antibodies in sera of vaccinated mice. As shown in Fig. 2B, significant titers of β-Gal-specific IgG and IgM antibodies were detected at day 30 in all vaccinated animals. In contrast to the IgM titers, which reach a plateau at day 30, the titers of IgG steadily increased until day 52 from immunization, when the experiment was concluded. No significant levels of β-Gal-specific IgA were detected in mice immunized with any of the three recombinant clones (data not shown).
FIG. 2.
Kinetics of LPS-specific (A) and β-Gal-specific (B) serum IgG (solid symbols) and IgM (open symbols) antibody responses in mice (n = 5) after oral immunization with either MvP101(pAH97) (●), HH104(pAH97) (▴), SL7207(pAH97) (■), or carrier alone (⧫). Results are expressed as the reciprocal log2 of the geometric mean endpoint titer (GMT). Standard deviations are indicated by vertical lines. Immunizations are indicated by arrows.
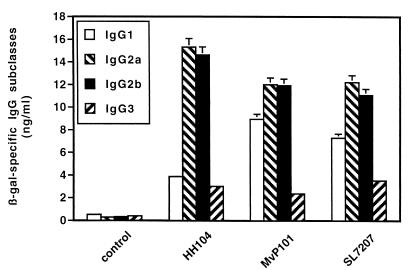
To determine the subclass distribution of the anti-β-Gal IgG, serum samples were analyzed for specific levels of IgG1, IgG2a, IgG2b, and IgG3. The results shown in Fig. 3 demonstrate that the main β-Gal-specific IgG isotype present in sera of animals immunized with HH104(pAH97) was IgG2 (IgG2a/IgG1 ∼ 4), suggesting a predominant Th1 response (42). In contrast, a higher concentration of IgG1 (P ≤ 0.05) was observed in mice immunized with MvP101(pAH97) (IgG2a/IgG1 ∼ 1.3) and SL7202(pAH97) (IgG2a/IgG1 ∼ 1.6), indicating a similar Th1/Th2 mixed response.
FIG. 3.
Subclass profiles of β-Gal-specific IgG antibodies present in sera of mice (n = 5) immunized orally with either MvP101(pAH97), HH104(pAH97), SL7207(pAH97), or carrier alone at day 52 postimmunization. Standard errors of the means are indicated by vertical lines.
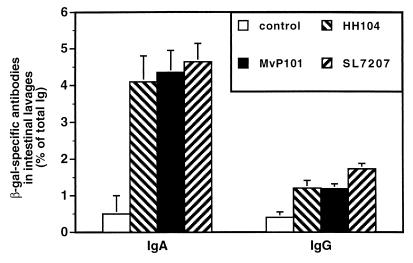
Induction of mucosal immune responses after oral vaccination.
To achieve protection against mucosal pathogens, it is highly desirable to obtain the elicitation of an efficient mucosal response after vaccination with live Salmonella carriers. Therefore, the presence of β-Gal-specific antibodies in intestinal washes from mice immunized with either MvP101, HH104, or SL7207 carrying pAH97 was investigated at day 52 from immunization. As shown in Fig. 4, immunization with all three carriers stimulated the production of significant amounts of β-Gal-specific IgA and, to a lesser extent, favored the transudation of antigen-specific IgG in the intestinal lumen. No statistically significant differences were observed among the mucosal responses to the different recombinant clones.
FIG. 4.
β-Gal-specific antibodies in intestinal lavages of mice immunized orally with either MvP101(pAH97), HH104(pAH97), SL7207(pAH97), or carrier alone at day 52 from immunization. Results are expressed as percentages of the corresponding total Ig subclass present in the intestinal lavage; standard errors of the means are indicated by vertical lines. No significant levels of antigen-specific IgM were detected in any of the groups.
Cellular immune responses triggered after oral immunization with sseC and sseD mutants expressing β-Gal.
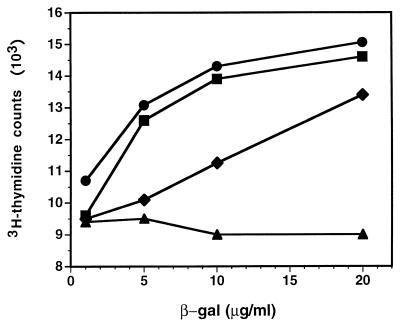
To evaluate the efficacy of the antigen-specific T-cell responses generated in immunized mice, spleen cells were enriched in CD4+ T cells and restimulated in vitro during 4 days with β-Gal. As shown in Fig. 5, although antigen-specific CD4+ spleen cells were generated after vaccination with the three carriers, HH104 and MvP101 were significantly more efficient than SL7207 (P < 0.05) at triggering specific cellular immune responses. In contrast, cells isolated from mice immunized with the carrier alone failed to proliferate in the presence of β-Gal.
FIG. 5.
β-Gal-specific proliferative response of CD4+ enriched spleen cells from mice orally immunized with either MvP101(pAH97) (■), HH104(pAH97) (●), SL7207(pAH97) (⧫), or carrier alone (▴). Cells were restimulated in vitro during 4 days with different concentrations of soluble β-Gal. Values are expressed as mean counts per minute of triplicates; standard errors of the means were in all cases lower than 10%. Background values obtained from wells without stimulating antigen were subtracted.
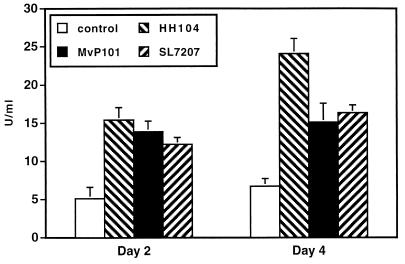
To investigate the Th type of the immune response triggered by immunization, the content of IFN-γ, IL-2, IL-4, IL-5, IL-6, and IL-10 was measured in supernatant fluids of restimulated cells. IFN-γ was the only cytokine significantly increased in all supernatant fluids from the different groups of immunized mice compared to the control group (cells isolated from mice immunized with plasmidless carriers) (Fig. 6). Interestingly, in agreement with IgG isotype patterns, the levels of IFN-γ detected in supernatants from cells of mice immunized with HH104(pAH97) were significantly higher (P < 0.05) than those from animals receiving either MvP101(pAH97) or SL7207(pAH97) (Fig. 6).
FIG. 6.
IFN-γ present in supernatants from cultured CD4+ enriched spleen cells of mice orally immunized with either MvP101(pAH97), HH104(pAH97), SL7207(pAH97), or carrier alone at days 2 and 4 of culture. Spleen cells were isolated from mice at day 52 after immunization, and CD4+ enriched populations were restimulated in vitro for 4 days in the presence of soluble β-Gal (20 μg/ml). IFN-γ production was determined by ELISA. Results are means of three determinations; standard errors of the means are indicated by vertical lines. No significant differences with the control groups were observed when IL-2, IL-4, IL-5, IL-6, and IL-10 were tested (not shown).
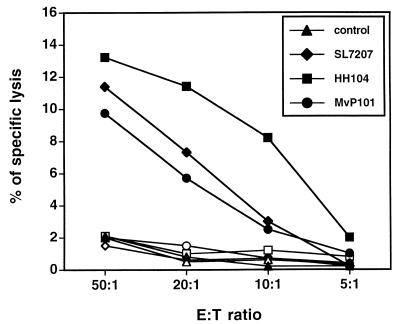
Induction of antigen-specific CTL responses in mice orally immunized with carrier strains expressing β-Gal.
The elicitation of major histocompatibility complex (MHC) class I-restricted responses is particularly important for conferring protection against many intracellular pathogens and tumors. It has been shown that antigen-specific CD8+ cytotoxic T lymphocytes (CTL) can be generated both in vitro and in vivo after immunization with recombinant Salmonella spp. expressing heterologous antigens (2, 10, 23, 30, 43, 44). Therefore, we considered it important to determine whether the tested carriers were also able to trigger a β-Gal-specific CTL response. Spleen cells were collected from mice vaccinated with either MvP101(pAH97), HH104(pAH97), or SL7207(pAH97) at day 52 from immunization and restimulated in vitro with βGP1-pulsed syngenic spleen cells for 5 days. As shown in Fig. 7, spleen cells from mice immunized with the different constructs induced significant lysis of βGP1-loaded target cells compared with unloaded controls (P < 0.05). However, more efficient responses were observed with the carrier strain HH104. Lysis was mediated by CD8+ T cells, since cytotoxic activity was completely abrogated when CD8+ T-effector cells were depleted (data not shown).
FIG. 7.
Recognition of the MHC class I-restricted βGP1 epitope by lymphocytes primed in vivo in mice by oral vaccination with either MvP101(pAH97), HH104(pAH97), SL7207(pAH97), or carrier alone. Spleen cells from immunized mice were restimulated in vitro for 5 days in the presence of 20 μM βGP1. At the end of the culture period, lymphocytes were tested in a [3H]thymidine retention assay with P815 (open symbols) and βGP1-loaded P815 (solid symbols) as targets (T). Results are means of triplicate wells (one of three independent experiments is shown) and are expressed as [(retained cpm in the absence of effectors {E}) − (experimentally retained cpm in the presence of effectors)/retained cpm in the absence of effectors] × 100. Standard errors of the means were lower than 5%.
DISCUSSION
The potential usefulness of attenuated Salmonella spp. as carriers for the delivery of vaccine antigens through the mucosal route has been extensively investigated (5, 9, 33, 35). Salmonella is capable of triggering not only humoral immune responses but also antigen-specific T-helper and cytotoxic responses (1, 3, 8, 10, 37, 44). Therefore, vaccine prototypes based on attenuated Salmonella strains can be employed when effective humoral responses are required (e.g., to achieve clearance of extracellular pathogens) and also in clinical situations in which cytotoxic effector cells are needed (e.g., viral diseases and tumors) (23, 25, 30, 36, 43).
Although many attenuated derivatives of Salmonella spp. have been described (4, 11, 14, 17, 28), only few of them were qualified to be used as vaccine delivery systems (3, 8, 19, 44). The efficacy of a live vaccine carrier relies on a subtle balance between minimal reactogenicity and maximal immunogenicity. The background of the carrier strain used in the formulation, the type of mutation selected to achieve attenuation, and the intrinsic properties of the immunogen seem to be crucial in determining the extent and quality of the immune response elicited (45). Several approaches have been previously used for the construction of live attenuated strains which exhibit satisfactory immunogenicity (4, 7, 11, 17, 28).
Two type III secretion systems have been identified in S. typhimurium, one, located in SPI1, that is required for bacterial invasion of epithelial cells (12) and a second, located in SPI2, that is needed for bacterial growth within the host (15, 29, 38). Based on the level of sequence homology between SPI2-encoded products and proteins from type III secretion systems, it was proposed that sse genes code for effector proteins of SPI2 (16). Here, we have evaluated the potential of S. typhimurium sseC and sseD mutants to deliver vaccine antigens by the oral route. All tested mutants were able to colonize and persist in Peyer’s patches for up to 20 days, but they exhibited impaired capacities to survive in spleens. Our studies also demonstrated that mutations in the sseC and sseD genes result in a significantly impaired bacterial virulence in both immune-competent and immune-deficient (IFN-γ−/−) mice.
The choice of IFN-γ−/− mice as a model for immune deficiency was based in the fact that IFN-γ plays a critical role in S. typhimurium clearance (26). VanCott et al. have recently shown an aroA mutant of S. typhimurium to be virulent in IFN-γ−/− mice (45). In contrast, the aroA strain tested here was attenuated in immunodeficient mice. Different factors, such as the dose, the background of the carrier (2337-65 in this study versus ATCC 14028), or the mouse strain used (BALB/c here versus C57BL/6), may account for the observed discrepancy. Furthermore, minor variations can lead to dramatic effects in this experimental setting. In fact, VanCott et al. reported that 5 × 109 CFU of a phoP mutant was not lethal for IFN-γ−/− mice whereas only a twofold increase in the dose resulted in 50% mortality (45). However, it is important to highlight that the background strain of the sse mutants tested here is the same as in the study of VanCott et al. (45). This suggests that SPI2 mutants exhibit a degree of attenuation in IFN-γ−/− mice that is at least equal to that of phoP mutants.
To thoroughly evaluate the potential of these mutants as vaccine carriers, we have compared the immune responses triggered against the model antigen β-Gal when it was expressed by either the sseC (HH104) and sseD (MvP101) mutants or the aroA mutant strain SL7207. Despite their attenuated virulence, the immunogenicity of the tested carrier strains is maintained intact. The HH104 and MvP101 mutants both stimulated β-Gal-specific systemic and mucosal responses that were as efficient as or stronger than those elicited by the aroA mutant. Oral immunization with the HH104 and SL7207 vaccine carriers resulted in the induction of a β-Gal-specific mixed Th pattern, whereas vaccination with the MvP101 derivative triggered a more Th1 dominant response. More-efficient CTL responses were also observed when this mutant was used for immunization. This might result from the potentiating effect of CTL priming associated with the dominant Th1-type class II-restricted help stimulated by this carrier (39).
Due to safety considerations, vaccine carriers should bear at least two independent attenuating mutations to eliminate the risk associated with the appearance of virulent revertants arising from recombination events. Despite their remarkable attenuation in immune-competent hosts, aro mutants can cause progressive infection in T-cell-deficient animals (40, 45). Therefore, the combination of different mutations might be essential for achieving a perfect balance between immunogenicity and reactogenicity. The characterization of mutants deficient in the production of novel virulence factors will certainly contribute to the development of a new generation of well-defined, highly immunogenic, and safer vaccine carriers. In addition, the availability of well-characterized mutants able to promote specific types of immune responses (e.g., different Th patterns) might also allow modulation of the obtained responses by simply selecting the most appropriate mutant according to the particular application.
ACKNOWLEDGMENTS
We thank B. A. D. Stocker for providing strain SL7207 and K. N. Timmis and J. Heesemann for generous support and encouragement during this study.
This work was in part supported by DFG grant 1964/2-1 and BMBF grant 01KI 9606, “Molekulare und immunologische Aspekte der Prevention klinisch relevanter Pathogene.”
REFERENCES
- 1.Aggarwal A, Kumar S, Jaffe R, Hone D, Gross M, Sadoff J. Oral Salmonella: malaria circumsporozoite recombinants induce specific CD8+ cytotoxic T cells. J Exp Med. 1990;172:1083–1090. doi: 10.1084/jem.172.4.1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brett S J, Rhodes J, Liew F Y, Tite J P. Comparison of antigen presentation of influenza A nucleoprotein expressed in attenuated aroA− Salmonella typhimurium with that of live virus. J Immunol. 1993;150:2869–2884. [PubMed] [Google Scholar]
- 3.Brown A, Hormaeche C E, Demarco de Hormaeche R, Winther M, Dougan G, Maskell D J, Stocker B A D. An attenuated aroA Salmonella typhimurium vaccine elicits humoral and cellular immunity to cloned β-galactosidase in mice. J Infect Dis. 1987;155:86–91. doi: 10.1093/infdis/155.1.86. [DOI] [PubMed] [Google Scholar]
- 4.Curtiss R, III, Kelly S M. Salmonella typhimurium deletion mutants lacking adenylate cyclase and cyclic AMP receptor protein are avirulent and immunogenic. Infect Immun. 1987;55:3035–3043. doi: 10.1128/iai.55.12.3035-3043.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Curtiss R, III, Kelly S M, Tinge S A, Tacket C O, Levine M M, Srinivasan J, Koopman M. Recombinant Salmonella vectors in vaccine development. Dev Biol Stand. 1994;82:23–33. [PubMed] [Google Scholar]
- 6.de Lorenzo V, Timmis K N. Analysis and construction of stable phenotypes in Gram-negative bacteria with Tn5- and Tn10-derived minitransposons. Methods Enzymol. 1994;235:386–405. doi: 10.1016/0076-6879(94)35157-0. [DOI] [PubMed] [Google Scholar]
- 7.Dougan G, Chatfield S N, Pickard D, O’Callaghan D, Maskell D. Construction and characterization of Salmonella vaccine strains harbouring mutations in two different aro genes. J Infect Dis. 1988;158:1329–1335. doi: 10.1093/infdis/158.6.1329. [DOI] [PubMed] [Google Scholar]
- 8.Dunstan S J, Cameron P S, Strugnell R A. Comparison of the abilities of different attenuated Salmonella typhimurium strains to elicit humoral immune responses against a heterologous antigen. Infect Immun. 1998;66:732–740. doi: 10.1128/iai.66.2.732-740.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Everest P, Griffiths P, Dougan G. Live Salmonella vaccines as a route towards oral immunizations. Biologicals. 1995;23:119–124. doi: 10.1006/biol.1995.0022. [DOI] [PubMed] [Google Scholar]
- 10.Flynn J L, Weiss W R, Norris K A, Seifert H S, Kumar S, So M. Generation of a cytotoxic T-lymphocyte response using Salmonella antigen-delivering system. Mol Microbiol. 1990;4:2111–2118. doi: 10.1111/j.1365-2958.1990.tb00572.x. [DOI] [PubMed] [Google Scholar]
- 11.Galán J E, Curtiss R., III Virulence and vaccine potential of phoP mutants of Salmonella typhimurium. Microb Pathog. 1989;6:433–443. doi: 10.1016/0882-4010(89)90085-5. [DOI] [PubMed] [Google Scholar]
- 12.Galán J E, Curtis R., III Cloning and molecular characterization of genes whose products allow Salmonella typhimurium to penetrate tissue culture cells. Proc Natl Acad Sci USA. 1989;86:6383–6387. doi: 10.1073/pnas.86.16.6383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Galán J E, Ginocchio C, Costeas P. Molecular and functional characterization of the Salmonella invasion gene invA: homology of InvA to members of a new protein family. J Bacteriol. 1992;174:4338–4349. doi: 10.1128/jb.174.13.4338-4349.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guo L, Lim K B, Gunn J S, Bainbridge B, Darveau R P, Hackett M, Miller S I. Regulation of lipid A modifications by Salmonella typhimurium virulence genes phoP-phoQ. Science. 1997;276:250–253. doi: 10.1126/science.276.5310.250. [DOI] [PubMed] [Google Scholar]
- 15.Hensel M, Shea J E, Gleeson C, Jones M D, Dalton E, Holden D W. Simultaneous identification of bacterial virulence genes by negative selection. Science. 1995;269:400–403. doi: 10.1126/science.7618105. [DOI] [PubMed] [Google Scholar]
- 16.Hensel M, Shea J E, Waterman S R, Mundy R, Nikolaus T, Banks G, Vazquez-Torres A, Gleeson C, Fang F C, Holden D W. Genes encoding putative effector proteins of the type III secretion system of Salmonella Pathogenicity Island 2 are required for bacterial virulence and proliferation in macrophages. Mol Microbiol. 1998;30:163–174. doi: 10.1046/j.1365-2958.1998.01047.x. [DOI] [PubMed] [Google Scholar]
- 17.Hoiseth S K, Stocker B A D. Aromatic-dependent Salmonella typhimurium are non-virulent and effective as live vaccines. Nature. 1981;291:238–239. doi: 10.1038/291238a0. [DOI] [PubMed] [Google Scholar]
- 18.Holtel A, Timmis K N, Ramos J L. Upstream binding sequences of the XylR activator protein and integration host factor in the xylS gene promoter region of the Pseudomonas TOL plasmid. Nucleic Acids Res. 1992;20:1755–1762. doi: 10.1093/nar/20.7.1755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Karem K L, Chatfield S, Kuklin N, Rouse B T. Differential induction of carrier antigen-specific immunity by Salmonella typhimurium live-vaccine strains after single mucosal or intravenous immunization of BALB/c mice. Infect Immun. 1995;63:4557–4563. doi: 10.1128/iai.63.12.4557-4563.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Levine M M, Kaper J B, Black R E, Clements M L. New knowledge on pathogenesis of bacterial enteric infections as applied to vaccine development. Microbiol Rev. 1983;47:510–550. doi: 10.1128/mr.47.4.510-550.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maloy S R, Steward V L, Taylor R K. Genetic analysis of pathogenic bacteria. Cold Spring Harbor, N.Y: Cold Spring Harbor Laboratory Press; 1996. [Google Scholar]
- 22.Matzinger P. The JAM test. A simple assay for DNA fragmentation and cell death. J Immunol Methods. 1991;145:185–192. doi: 10.1016/0022-1759(91)90325-a. [DOI] [PubMed] [Google Scholar]
- 23.Medina E, Guzmán C A, Staendner L H, Colombo M P, Paglia P. Salmonella vaccine carrier strains: effective delivery system to trigger anti-tumor immunity by oral route. Eur J Immunol. 1999;29:1–8. doi: 10.1002/(SICI)1521-4141(199902)29:02<693::AID-IMMU693>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 24.Miller V L, Mekalanos J J. A novel suicide vector and its use in construction of invertion mutations: osmoregulation of outer membrane proteins and virulence determinants in Vibrio cholerae requires toxR. J Bacteriol. 1988;170:2575–2583. doi: 10.1128/jb.170.6.2575-2583.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nardelli-Haefliger D, Roden R B, Benyacoub J, Sahli R, Kraehenbuhl J P, Schiller J T, Lachat P, Potts A, De Grandi P. Human papillomavirus type 16 virus-like particles expressed in attenuated Salmonella typhimurium elicit mucosal and systemic neutralizing antibodies in mice. Infect Immun. 1997;65:3328–3336. doi: 10.1128/iai.65.8.3328-3336.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nauciel C, Espinasse-Maes F. Role of gamma interferon and tumor necrosis factor alpha in resistance to Salmonella typhimurium infection. Infect Immun. 1992;60:450–454. doi: 10.1128/iai.60.2.450-454.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.O’Callaghan D, Charbit A. High efficiency transformation of Salmonella typhimurium and Salmonella typhi by electroporation. Mol Gen Genet. 1990;223:156–158. doi: 10.1007/BF00315809. [DOI] [PubMed] [Google Scholar]
- 28.O’Callaghan D, Maskell D, Liew F Y, Easmon C S F, Dougan G. Characterization of aromatic- and purine-dependent Salmonella typhimurium: attenuation, persistence, and ability to induce protective immunity in BALB/c mice. Infect Immun. 1988;56:419–423. doi: 10.1128/iai.56.2.419-423.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ochman H, Soncini F C, Solomon F, Groisman E A. Identification of a pathogenicity island required for Salmonella survival in host cells. Proc Natl Acad Sci USA. 1996;93:7800–7804. doi: 10.1073/pnas.93.15.7800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Paglia P, Medina E, Arioli I, Guzmán C A, Colombo M P. Gene transfer in dendritic cells, induced by oral DNA vaccination with Salmonella typhimurium, results in protective immunity against murine fibrosarcoma. Blood. 1998;10:46–56. [PubMed] [Google Scholar]
- 31.Rammensee H G, Schild H, Theopold U. Protein-specific cytotoxic T lymphocytes. Recognition of transfectants expressing intracellular, membrane-associated or secreted forms of beta-galactosidase. Immunogenetics. 1989;30:296–302. doi: 10.1007/BF02421334. [DOI] [PubMed] [Google Scholar]
- 32.Reed L J, Muench H. A simple method of estimating fifty per cent end points. Am J Hyg. 1938;27:493–497. [Google Scholar]
- 33.Roberts M, Chatfield S N, Dougan G. Salmonella as carriers of heterologous antigens. In: O’Hagan D T, editor. Novel delivery systems for oral vaccines. Boca Raton, Fla: CRC Press, Inc.; 1994. pp. 27–58. [Google Scholar]
- 34.Sambrook J, Fritsch E F, Maniatis T. Molecular cloning: a laboratory manual. 2nd ed. Cold Spring Harbor, N.Y: Cold Spring Harbor Laboratory Press; 1989. [Google Scholar]
- 35.Schodel F, Curtiss R., III Salmonellae as oral vaccine carriers. Dev Biol Stand. 1995;84:245–253. [PubMed] [Google Scholar]
- 36.Schodel F, Milich D R, Will H. Hepatitis B virus nucleocapsid/pre-S2 fusion proteins expressed in attenuated Salmonella for oral vaccination. J Immunol. 1990;145:4317–4321. [PubMed] [Google Scholar]
- 37.Schorr J, Knapp B, Hundt E, Küpper H A, Amann E. Surface expression of malarial antigens in Salmonella typhimurium: induction of serum antibody response upon oral vaccination of mice. Vaccine. 1991;9:675–681. doi: 10.1016/0264-410x(91)90194-b. [DOI] [PubMed] [Google Scholar]
- 38.Shea J E, Hensel M, Gleeson C, Holden D W. Identification of a virulence locus encoding a second type III secretion system in Salmonella typhimurium. Proc Natl Acad Sci USA. 1996;93:2593–2597. doi: 10.1073/pnas.93.6.2593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shirai M, Pendleton C D, Ahlers J, Takeshita T, Newman M, Berzofsky J A. Helper-cytotoxic T lymphocyte (CTL) determinant linkage required for priming of anti-HIV CD8+ CTL in vivo with peptide vaccine constructs. J Immunol. 1994;152:549–556. [PubMed] [Google Scholar]
- 40.Sinha K, Mastroeni P, Harrison J, Demarco de Hormaeche R, Hormaeche C E. Salmonella typhimurium aroA, htrA, and aroD htrA mutants cause progressive infections in athymic (nu/nu) BALB/c mice. Infect Immun. 1997;65:1566–1569. doi: 10.1128/iai.65.4.1566-1569.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Staats H F, Jackson R J, Marinaro M, Takahashi I, Kiyono H, McGhee J R. Mucosal immunity to infection with implications for vaccine development. Curr Opin Immunol. 1994;6:572–583. doi: 10.1016/0952-7915(94)90144-9. [DOI] [PubMed] [Google Scholar]
- 42.Stevens T L, Bossie A, Sanders V M, Fernandez Botran R, Coffman R L, Mosmann T R, Vitetta E S. Regulation of antibody isotype secretion by subsets of antigen-specific helper T cells. Nature. 1988;334:255–258. doi: 10.1038/334255a0. [DOI] [PubMed] [Google Scholar]
- 43.Tite J P, Gao X M, Hughes Jenkins C M, Lipscombe M, O’Callaghan D, Dougan G, Liew F Y. Anti-viral immunity induced by recombinant nucleoprotein of influenza A virus. III. Delivery of recombinant nucleoprotein to the immune system using attenuated Salmonella typhimurium as a live carrier. Immunology. 1990;70:540–546. [PMC free article] [PubMed] [Google Scholar]
- 44.Turner S J, Carbone F R, Strugnell R A. Salmonella typhimurium ΔaroA ΔaroD mutants expressing a foreign recombinant protein induce specific major histocompatibility complex class I-restricted cytotoxic T lymphocytes in mice. Infect Immun. 1993;61:5374–5380. doi: 10.1128/iai.61.12.5374-5380.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.VanCott J L, Chatfield S N, Roberts M, Hone D M, Hohmann E L, Pascual D W, Yamamoto M, Kiyono H, McGhee J R. Regulation of host immune responses by modification of Salmonella virulence genes. Nat Med. 1998;4:1247–1252. doi: 10.1038/3227. [DOI] [PubMed] [Google Scholar]