Abstract
Background. Tai Chi is a form of exercise that is accessible to people from different socioeconomic backgrounds, making it a potentially valuable activity for health promotion of older adults. Purpose. The objective of this scoping review was to summarize the current knowledge about the effectiveness of Tai Chi for older adults across a range of general health outcomes from published, peer reviewed, unique meta-analyses. Methods. Meta-analyses were retrieved from Medline, Embase, AMED, CINAHL, SPORTDiscus, PsychINFO, Web of Science, PubMed Health, and the Cochrane Library from database inception to late August 2019. Multistage deduplication and screening processes identified eligible full-length meta-analyses. Two people independently appraised 27 meta-analyses based on the GRADE system and organized results into 3 appendices subsequently collated into heterogeneous, statistically significant, and statistically insignificant tables. Results. “High” and “moderate” quality evidence extracted from these meta-analyses demonstrated that practicing Tai Chi can significantly improve balance, cardiorespiratory fitness, cognition, mobility, proprioception, sleep, and strength; reduce the incidence of falls and nonfatal stroke; and decrease stroke risk factors. Conclusions. Health care providers can now recommend Tai Chi with high level of certainty for health promotion of older adults across a range of general health outcomes for improvement of overall well-being.
Keywords: Tai Chi, health promotion, older adults, effectiveness, scoping review
‘Tai Chi training aims to improve strength, flexibility, balance, and body awareness, as well as increase concentration and reduce feelings of anxiety and stress.’
A growing body of research emphasizes the important role that physical activity plays in general health of older adults. 1 We align our work with the World Health Organization’s definition of general health: “Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.” 2 Physical activity has a direct impact on well-being, which in turn affects quality of life. Health care professionals recommend various forms of physical activity for older adults to manage age-related physical and cognitive changes. Exercise guidelines emphasize the importance of aerobic, strength, and flexibility exercise and balance training to obtain greater health benefits for older adults. 3
Tai Chi is a form of mild-to-moderate aerobic activity that is often recommended for older adults to attenuate the decline of physical and cognitive functions.4,5 It is a traditional Chinese medicine exercise that consists of slow continuous movements coordinated with breathing as well as mindfulness. 6 Tai Chi comprises both physical and mental training, making it a complex intervention helping to find a balance between one’s body and mind. 6 It is considered a safe option of physical activity for older adults as it is a form of exercise that is low in demand. 6 Tai Chi training aims to improve strength, flexibility, balance, and body awareness, as well as increase concentration and reduce feelings of anxiety and stress.6,7 It is an enjoyable and inexpensive form of exercise intervention that is accessible to a wide range of the population from different socioeconomic backgrounds, making it a valuable and promising activity for improvement in overall well-being.
As the practice of Tai Chi becomes more popular, more research is being conducted to study its effects on general health. Solloway and colleagues 8 conducted a “systematic review of systematic reviews” to compile evidence that has been published to date on the effects of Tai Chi on health outcomes. Although they reported promising results of Tai Chi practice on outcomes such as hypertension, balance, cognition, osteoarthritis, mental health, respiratory health of people with chronic obstructive pulmonary disease, pain, and muscle strength, the authors refrained from drawing firm conclusions after indicating limitations of this synthesis. Further work has been subsequently completed by Huston and McFarlane, 9 who published an updated review of the effects of Tai Chi on general health. This more recent study also had limitations that put the credibility of the results under question. Some of the limitations of these papers included the following: (1) both studies are outdated reporting on research published up to February 2014 8 and October 2015, 9 (2) one was restricted to only the MedLine database 9 leading to publication bias, (3) mixed types of evidence including systematic reviews and randomized controlled trials were appraised, 9 (4) the quality of studies was either not evaluated 8 or evaluated in a nontransparent manner, 9 and (5) did not provide detailed data extraction tables.8,9 With an aim to rectify these limitations, we planned to employ a comprehensive search strategy to gather systematic reviews with the most recent research. We then evaluated the quality of each included study in a fully transparent manner using 2 independent reviewers. Last, to support summary tables we provided detailed data extraction tables.
Research studies investigating the effectiveness of Tai Chi on health outcomes usually focus on 1 of 2 groups of individuals: those with and/or those without diagnosed health conditions. Previously, Easwaran and colleagues 10 published a scoping review in which they compiled the body of moderate- and high-quality research evidence from meta-analyses examining the effectiveness of Tai Chi for adults with diagnosed health conditions. The objective of this scoping review is to summarize the current knowledge about the effectiveness of Tai Chi for older adults without diagnosed health conditions across a range of general health outcomes from published, peer-reviewed, unique meta-analyses. The results of this study will be valuable for health care service providers to recommend Tai Chi practices to their older-aged clients for enhancement of overall health and well-being through a potentially effective, safe, and enjoyable activity.
Methods
We used the advanced scoping methods proposed by Levac and colleagues. 11 In addition to identifying the purpose of the work, steps included identifying relevant studies through comprehensive use of multiple databases and a systematic search strategy; selecting relevant articles; charting data (including a quality appraisal); and collating, summarizing, and reporting results. We are aware of the work being conducted by Colquhoun and colleagues 12 in which they plan to elaborate on their recommendations for quality appraisal in scoping reviews; however, in the absence of new guidelines, which were under development at the time we initiated this project, we relied on quality appraisal using the GRADE guidelines. 13
We used the GRADE Handbook 13 to rate the quality of evidence in the studies selected for this scoping review. We intentionally avoided a stance of “clever nihilism” 14 by taking a pragmatic approach to our critical appraisals. Specifically, rather than relying on the risk of bias assessments provided by the authors of the selected manuscripts, we used a more balanced approach by carefully considering the impact of various biases in the context of reported studies. We limited our work to completion of the quality appraisals and did not follow-up with making recommendations based on the evidence (nor did we organize tables in order of importance of the outcomes to people in various categories of health conditions). Based on a client-centered perspective, 15 both of these final steps require participation of older adults to clarify their values and preferences, which was beyond the scope of the study we undertook.
Data Sources and Searches
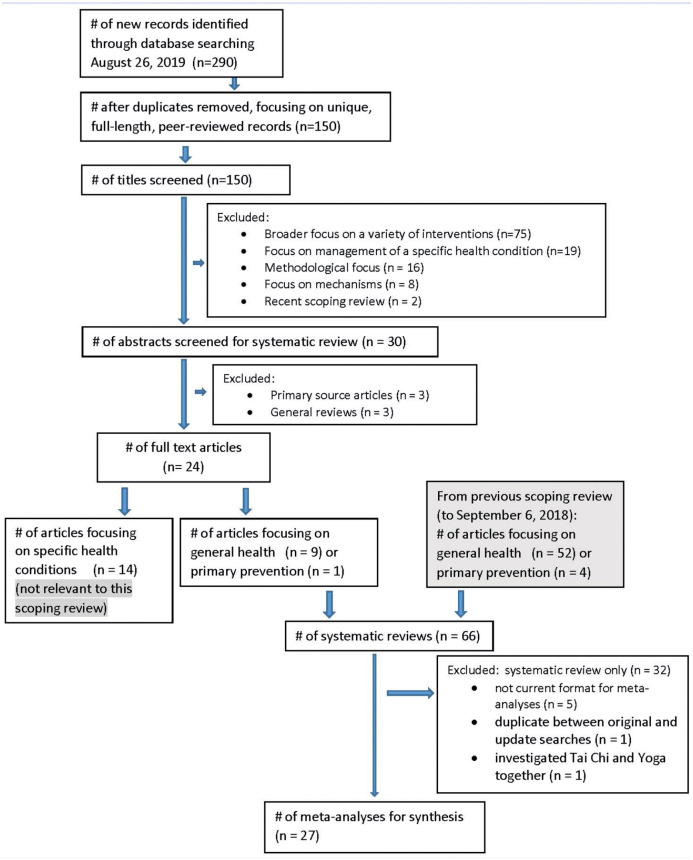
We initially searched the following databases for published, peer-reviewed, English-language systematic reviews from their inception to September 5, 2018, 10 and subsequently updated the search on August 26, 2019: Medline, Embase, AMED, CINAHL, SPORTDiscus, PsychINFO, Web of Science, PubMed Health, and the Cochrane Library. Details of the search strategies are provided in Appendix 1 (available online as supplemental material). Appendix Figure 1 contains details of the original search that resulted in 2626 records being identified (56 of which involved studies of general health). Figure 1 contains details of the updated search resulting in 290 new records being identified. Appendix Figure 1 (and the previous article 10 ) contain details of subsequent screening processes. In this article, we focus on the screening of the new results. Because this study used information in the public domain, it is ethics exempt.
Figure 1.
Flow chart of updated database search and manuscript selection.
Study Selection
Deduplication and Focus on Unique, Full-Length Peer-Reviewed Records
Zotero (a freely available referencing system database) was used to initiate the deduplication process; however, manual deletion of additional duplicates was also required. In our context of wishing to review current best evidence in the form of full-length publications, conference abstracts and letters to the editor were deleted. Finally, with a focus on products going through the full peer-review process, theses and books were excluded. This resulted in 150 unique publications of the updated search (Figure 1).
Screening
Given the objective of specifically focusing on evidence related to Tai Chi participation, all articles with titles indicating a more general focus on other interventions (n = 75) were deleted, unless Tai Chi was in the title. Other interventions included aerobic exercise, Chinese exercise (traditional), combat sports, complementary and alternative approaches, exercise (nonspecific), general intervention strategies, integrative medicine and oncology, lifestyle modification, martial arts, massage therapy, meditation, mind-body interventions, mindful practices, movement and body-awareness therapies, nonpharmocologic interventions, physical activity, physical therapy, psychological or psychosocial interventions, rehabilitation, resistance exercise, Scroth exercises, sitting versus standing exercises, therapeutic exercise, or yoga. Similarly, articles focusing on management of a specific health condition, without Tai Chi in the title, were also deleted (n = 19). Health conditions contained in the titles of these articles that were deleted included anxiety, atherosclerosis, breast cancer, cardiovascular disease, cognitive ageing, depression, diabetes, fall prevention, fibromyalgia, heart failure, human immunodeficiency virus, neuropathic pain, osteoarthritis, Parkinson’s disease, somatic disorders, and subacute stroke. The next step in initial screening involved deleting records that were methodologic in focus (n = 16); these comprised primarily of study protocols but also included safety and perspectives on variation in protocols to study Tai Chi. In addition, 8 articles describing mechanisms of Tai Chi (such as the role of meditation and psychobiological factors in late life and how they are effected by Tai Chi and the association of Tai Chi with stress, immunity, asthma and inflammation) were deleted, as were 2 scoping reviews focusing on specific health conditions that were published since the previous search in early September 2018. This resulted in 30 records remaining from the updated search (Figure 1).
A second stage in the screening of records involved a review of abstracts to select only secondary sources. At this stage, 3 records of articles that were primary sources and 3 records that were general reviews or overviews, rather than systematic reviews, were removed. This resulted in 24 records that appeared to be systematic reviews.
Up to this point, screening was done only by the corresponding author. As was done in the previous project, 10 as a means of managing the scope of this project, articles were separated into systematic reviews studying general health outcomes (n = 9) and primary prevention (n = 1) versus specific health conditions (n = 14, which were not relevant in this scoping review) by the entire authorship team. Hereafter, all screening was done independently by 2 people. A total of the previously identified 56 articles and the current 10 newly identified articles yielded 66 article that were first screened to confirm that they were systematic reviews and all were deemed to be so (Figure 1).
As we experienced in the first phase of this 2-part scoping review, we were acutely aware of the overwhelming task of collating qualitative results; therefore, again we decided to focus on meta-analyses. We excluded articles that were systematic reviews only (n = 32) and 5 more dated articles that were meta-analyses, but not formatted in the current style necessary to collate results based on the GRADE guidelines. Also, 1 article that was identified in the original search as being “accepted for publication” was published by the time we did the second search. Finally, 1 article was excluded because it presented combined results for Tai Chi and Yoga, resulting in 27 unique articles for synthesis in this scoping review (Figure 116-42). As a final step in managing the still overwhelming amount of results, we decided to focus on results produced in the meta-analyses that did not demonstrate inconsistency (ie, heterogeneity), thus increasing the “certainty” of current collated knowledge.
Data Extraction and Quality Assessment
Two people independently reviewed and appraised each of the 27 articles. Pairs were each of the 4 first authors with the corresponding author, who reviewed and appraised all selected articles and provided consistency in approach across all appraisals. Any discrepancies in charting or appraisals were settled by consensus. When articles contained results for both total scores and subgroups, only subgroups were charted and only if ≥2 studies were included. As an initial step in collating the results, 3 detailed tables were produced, each of which is reported as an appendix.
For the table of heterogeneous results (ie, P values of the various tests of heterogeneity less than 0.05 and high I2 values 13 or in the absence of these data, visual interpretation of individual studies’ nonoverlapping confidence intervals) only the outcome, source, number of participants in experimental and control groups, P value, value of I2, and results were charted. Based on the well-known heterogeneity of Tai Chi styles and forms, as well as variations in intensity, frequency, and duration of practice, 43 details of the Tai Chi intervention were not recorded. Results that were statistically significant (despite inconsistency across studies) were shaded to highlight preliminary evidence of effectiveness.
For the tables of statistically significant and insignificant results (excluding results previously screened for heterogeneity), results were collated in 2 sections. First, the meta-analyses were described by identifying the source, number of studies, study design(s), number of participants, and details of the intervention in the experimental and control groups, and details of the reporting of adverse events related to Tai Chi. 44 The meta-analyses were then appraised for risk of bias, indirectness, imprecision, and publication bias (all of which could contribute to downgrading of evidence), and other considerations to upgrade, followed by an overall quality appraisal, and recording of the estimate of effect. 13 These 2 tables could not be completed for some meta-analyses that either did not report risk of bias 35 or presented a nontransparent linking of some or all data to original studies. 39 Although not in the original article, one group provided us with detailed tables so that this could be completed. 30
Most frequently, evidence for risk of bias was presented in individual studies using guidelines from the Cochrane Collaboration tool 45 (low risk of bias, high risk of bias, or unclear), which include items relating to random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), or selective reporting (reporting bias). With knowledge that attributes of the instructor and expectation of the participants are key ingredients to the practice of Tai Chi, 46 and as others have done,24,25,38,41,42 it is neither possible nor desirable to blind either instructors or participants; therefore, we did not downgrade for these risks of “bias.” Similarly, for self-reported outcomes, we did not consider lack of blinding of the assessor as a source of bias. Otherwise, we used reported information, and GRADE 13 guidelines to judge the risk as “not serious,” “serious,” or “very serious.” In the absence of guidelines from the Cochrane Collaboration, we also used data reported using the PEDro 47 and Jadad 48 rating systems. The PEDro scale is out of 11 points. Disregarding 2 items for blinding of participants and instructors, we rated risk of bias as “not serious” with average ratings ≥8, “serious” with average ratings of 6 to 7, and “very serious” with average ratings of ≤5. The Jadad scale is out of 5. We considered average ratings of ≥4 as “not serious,” 3 as “serious,” and ≤2 as “very serious.” If details of the individual items were available, we used those rather than the summary score.
In accordance with a “patient-centered approach,” the GRADE guidelines 13 recommend downgrading for the use of surrogate measures as a source of indirectness. We followed this guideline in our previous work involving a scoping review of meta-analyses focusing on adults with a variety of health conditions. 10 Given our current focus on general health outcomes and health promotion and primary and secondary prevention, as is consistent with an epidemiological orientation 49 and the broad definition of health proposed by the World Health Organization 2 (which includes body structures and functions 50 ), we did not downgrade for this reason. Otherwise, the primary source of indirectness was differences in the target population of samples in individual studies. In our current context, indirectness was flagged as an issue when samples contained adults with identified, but not borderline, health conditions. Indirectness was judged as “not serious,” “serious,” or “very serious.”
For imprecision, we did not conduct formal sample size calculations but rather considered whether larger sample sizes (and therefore tighter confidence intervals) would increase the certainty of either statistically significant or insignificant results. When dichotomous data were reported (such as number of adverse events), we considered the impact of the relatively low number of events.
For publication bias, we relied on evidence from funnel plots (necessitating a minimum of 5 to 10 studies) and did not make a judgement of concern if authors had unsubstantiated reports from previous authors about “some negative studies” being unpublished. We relied on our extensive database searches to minimize publication bias, given that the English language is a major source of publications worldwide. It was interesting to note that of the 27 articles included in this scoping review, 17 and 3 included searches of Chinese (1, 6, 4, and 6 searched 1, 2, 3, or 4 databases, respectively) and Korean (1 and 2 searched 5 or 6 databases, respectively) resources, further reducing the likelihood of publication bias. Publication bias was judged as either “undetected” or “detected” (with evidence from funnel plots and other analyses).
The primary factor potentially upgrading the quality of evidence included a large magnitude of effect. We increased the quality of evidence by one level when the standardized mean difference was greater than 0.80 (interpreted as a “large” effect 51 ), the mean difference was 1.5 times the minimal clinically important difference (MCID) or minimal detectable change (MDC), the relative risk reduction was greater than 50%, or the relative risk was greater than 2. 13 We increased the quality of evidence by 2 levels when the standardized mean difference was greater than 1.0, the relative risk reduction was greater than 80%, or the relative risk was greater than 5. 13 References supporting the MCID (or in it absence, the MDC) were obtained by searching Medline and are contained in the appendices. Unlike our experience in Part 1 of this pair of studies, we found very few references for the MCID or MDC on a variety of outcomes for adults without diagnosed health conditions. In the absence of these values, we repeated the Medline search for test-retest reliability of the specific measures reporting mean differences and calculated the MDC from there. This yielded very little additional information to assist with interpretation.
Explanations of downgrading or upgrading are provided in the detailed appendices. We followed GRADE guidelines 13 to establish the overall quality rating.
Data Synthesis and Analysis
For the primary objective of this scoping review, we summarized the “preliminary evidence of effectiveness” for statistically significant results from heterogeneous findings. For both statistically significant and insignificant findings, we collated evidence of “high” and “moderate” evaluations of quality of evidence, presuming that higher quality evidence is most useful for clinicians upon which to base recommendations for clients. The GRADE system 13 describes “high” quality evidence as providing a very good indication of the likely effect, associated with knowledge users being very confident in the results; “moderate” quality evidence provides a good indication of the likely effect and is associated with moderate confidence. Additionally, we report on documentation of adverse events.
Results
Detailed data extraction tables are contained in Appendices 2, 3, and 4 for heterogeneous, statistically significant, and statistically insignificant results, respectively. Table 1 contains a summary of results with preliminary evidence of effectiveness (ie, heterogeneous results with statistically significant findings). The greatest certainty of results (ie, findings that are not heterogeneous and statistically significant) for outcomes with either “high” or “moderate” ratings for quality of evidence are summarized in Table 2. Appendix 5 summarizes the statistically insignificant results of findings with either “high” or “moderate” quality ratings. The most recent evidence for “high” and “moderate” quality ratings, ordered by magnitude of effect, is summarized in Table 3.
Table 1.
Preliminary Evidence of Effectiveness of Tai Chi (ie, Heterogeneous Results With Statistically Significant Results; All Favoring Tai Chi Except for *, Described in the Narrative Section of the Results).
| Outcome | Source | Magnitude of statistically significant effects | Interpretation |
|---|---|---|---|
| Balance | Song et al (2015) 30 | ||
| Direct measure | Low fall risk group with 6 mo intervention | SMD = 0.64 (95% CI 0.07, 1.21) | Moderate |
| Direct measure | 6 mo of Tai Chi compared to no intervention | SMD = 0.56 (95% CI 0.05, 1.07) | Moderate |
| Dynamic | Low fall risk group with 3 mo intervention | SMD = 0.52 (95% CI 0.23, 0.82) | Moderate |
| Dynamic | 3 mo of Tai Chi compared to no intervention | SMD = 0.49 (95% CI 0.19, 0.78) | Small to moderate |
| Dynamic | 6 mo of Tai Chi compared to no intervention | SMD = 0.45 (95% CI 0.03, 0.88) | Small to moderate |
| Static and dynamic | 3 mo of Tai Chi compared to no intervention | SMD = 0.45 (95% CI 0.12, 0.79) | Small to moderate |
| Static and dynamic | 6 mo of Tai Chi compared to no intervention | SMD = 0.46 (95% CI 0.03, 0.88) | Small to moderate |
| Static | Low fall risk group with 3 mo intervention | SMD = 0.73 (95% CI 0.27, 1.19) | Moderate to large |
| Static | Low fall risk group with 6 mo intervention | SMD = 0.33 (95% CI 0.16, 0.51 | Small to moderate |
| Static | 3 mo of Tai Chi compared to no intervention | SMD = 0.66 (95% CI 0.32, 0.99) | Moderate to large |
| Static | 6 mo of Tai Chi compared to no intervention | SMD = 0.37 (95% CI 0.19, 0.54) | Small to moderate |
| Body composition | Larkey et al (2018) 22 (some with medical diagnoses) | ||
| Body mass index | SMD = −0.39 (95% CI −0.73, −0.04) | Small to moderate | |
| Bone mineral density | Zou et al (2017) 42 (pre- and postmenopausal; osteoporosis, hyperlipidemia) | ||
| Lumbar spine | SMD = 0.26 (95% CI 0.11, 0.40) | Small | |
| Femoral neck | SMD = 0.57 (95% CI 0.36, 0.78) | Moderate | |
| Femoral trochanter | SMD = 0.47 (95% CI 0.19, 0.75) | Small to moderate | |
| Cardiorespiratory fitness | Zheng et al (2015) 40 (healthy community dwellers 45-75 years) | ||
| Diastolic BP | SMD = −0.54 (95% CI −0.90, −0.18) | Moderate | |
| FVC | Intervention < 1 year | MD =359 (95% CI 20, 699) | Large |
| FVC | Intervention > 1 year | MD = 443 (95% CI 271, 614) | Very large |
| Heart rate | Immediately after exercise* | SMD = 3.10 (95% CI 0.91, 5.29) | Very very large |
| Heart rate | Quiet condition | SMD = −0.72 (95% CI −1.27, −0.18) | Moderate to large |
| Stair Test Index | SMD = 1.34 (95% CI = 0.27, 2.40) | Very large | |
| Systolic BP | SMD = −0.93 (95% CI −1.30, −0.56) | Large | |
| CVD risk factors | Pan et al (2016) 29 (Chinese adults >18 years, mean ages 50s and 60s) | ||
| Triglycerides | MD = −16.81 (95% CI −31.27, −2.35) | No information available to interpret MD | |
| Cognition | Wu et al (2013) 35 (adults >55 years) | ||
| Global cognitive function | SMD = 0.28 (95% CI 0.06, 0.50) | Small | |
| Memory function | SMD = 0.41 (95% CI 0.06, 0.76) | Small to moderate | |
| Falls | Huang et al (2017) 21 (>60 years including 2 studies with people with stroke and 2 with people with Parkinson’s) | ||
| Rate of falls | IRR = 0.69 (95% CI 0.0.60, 0.80) | Moderate | |
| Physical function | Chen et al (2014) 17 (Adults ≥45 years with sub-health conditions) | ||
| SMD = 0.49 (95% CI 0.00, 0.99) | Small to moderate | ||
| Psychological health | |||
| General | Chen et al (2014) 17 (Adults ≥45 years with sub-health conditions) | SMD = 0.57 (95% CI 0.21, 0.92) | Moderate |
| Anxiety | Wang et al (2010) 32 (adolescents with attention deficit hyperactivity disorder, adults [some with health conditions, elderly]) | SMD = 0.66 (95% CI 0.29, 1.03) | Moderate to large |
| Depression | Wang et al (2010) 32 (adults [some with health conditions]) | SMD = 0.56 (95% CI 0.31, 0.80) | Moderate |
| Depression | Zhang et al (2019) 37 (people from samples with mean ages ranging from 20.3 to 80.5 years) | SMD = −0.50 (95% CI −0.76, −0.23) | Moderate |
| Stress | Wang et al (2010) 32 (adults with a variety of health conditions) | SMD = 0.66 (95% CI 0.23, 1.09) | Moderate to large |
| Sleep | Du et al (2015) 18 (adults >60 years) | ||
| Global score | SMD = −0.93 (95% CI −1.52, −0.34) | Large | |
| Sleep latency | SMD = −0.75 (95% CI −1.42, −0.07) | Moderate to large | |
| Strength | Liu et al (2011) 26 (adults >50 years) | ||
| MVC of the knee (N) | MD= 5.3 (95% CI 1.12, 9.50) | No information available to interpret MD | |
| Stroke risk factors | Lauche et al (2017) 23 (most with borderline hypertension, >45 years) | ||
| Diastolic BP | MD = −10.7 (95% CI −14.9, −6.4) | No information available to interpret MD | |
| Systolic BP | MD = −15.6 (95% CI −21.2, −10.0) | No information available to interpret MD |
Abbreviations: BP, blood pressure; CI, confidence interval; CVD, cardiovascular disease; FVC, forced vital capacity; IRR, incidence rate ratio; MD, mean difference; mo, months; MVC, maximum voluntary contraction; N, Newtons; SMD, standardized mean difference.
Table 2.
Statistically Significant Results With “High” and “Moderate” Quality Evidence (All Favoring Tai Chi).
| Outcome | Source | Population and duration of Tai Chi practice | Magnitude of statistically significant effects | Interpretation of magnitude of effects |
|---|---|---|---|---|
| High-quality evidence | ||||
| Balance | ||||
| Berg Balance Scale | Zhao et al (2013) 38 | Adults >60 years, >12 wks of Tai Chi | MD = 2.5 (95% CI 1.5, 3.4) | Small |
| Berg Balance Scale | Huang and Liu (2015) 20 | Adults >60 yrs, 10-24 wks of Tai Chi | MD = 2.2 (95% CI 0.9, 3.4) | Small |
| Mixed measures | Song et al (2015) 30 | Healthy elderly >60 yrs, 20-24 wks of Tai Chi | SMD = 0.83 (95% CI 0.60, 1.06) | Large |
| Balance and mobility | ||||
| Timed Up-and-Go | Zhao et al (2013) 38 | Adults >60 years, >12 wks of Tai Chi | MD = 0.7 (95% CI 0.3, 1.1) | Small |
| Cardiorespiratory fitness | ||||
| Forced vital capacity | Zheng et al (2015) 40 | Healthy community-dwellers 45 75 yrs, average of 10.5 yrs of Tai Chi | MD = 670 (95% CI 345, 995) | Very large |
| Falls | ||||
| Incidence of falls | Zhao et al (2013) 38 | Adults >60 yrs, >12 wks of Tai Chi | RR = 0.82 (95% CI 0.73, 0.92) | Small to moderate |
| Incidence of falls | Lomas-Vega et al (2017) 28 | At-risk older adults (56-98 yrs), <12 mo of Tai Chi | IRR = 0.57 (95% CI 0.46, 0.70) | Moderate to large |
| Sleep | ||||
| Subjective sleep quality | Du et al (2015) 18 | >60 yrs, 8-24 wks of Tai Chi | SMD = −0.83 (95% CI −1.08, −0.57) | Large |
| Strength | ||||
| Isokinetic knee extensor strength | Liu et al (2011) 26 | Women >50 yrs, 4-12 mo of Tai Chi | MD = 19.6 (95% CI 10.3, 28.9) | Large |
| Stroke primary prevention | ||||
| Incidence of non-fatal stroke | Zheng et al (2015) 39 | People with essential hypertension mean age 62 yrs and healthy elders 45-70 yrs, 48 wks to 2 yrs of Tai Chi | RR = 0.11 (95% CI 0.01, 0.85) | Very large |
| Moderate-quality evidence | ||||
| Balance | ||||
| Functional Reach Test | Zhao et al (2013) 38 | People >60 yrs, Tai Chi of >12 wks | MD = 0.8 (95% CI 0.3, 1.2) | Small |
| Single Leg Stance | Huang and Liu (2015) 20 | People >60 yrs, 6 mo of Tai Chi | MD = 5.3 (95% CI 3.4, 7.3) | Small |
| Direct measures | Song et al (2015) 30 | Healthy elderly >70 yrs and participants with vestibular hypofunction mean age 58 yrs, 10-12 wks of Tai Chi | SMD = 0.84 (95% CI 0.28, 1.40) | Large |
| Direct measures | Song et al (2015) 30 | Healthy elderly >70 yrs and participants with vestibular hypofunction mean age 58 yrs, 12-15 wks of Tai Chi | SMD = 0.52 (95% CI 0.19, 0.84) | Moderate |
| Mixed measures | Song et al (2015) 30 | Healthy elderly >60 yrs; low fall risk, 20-24 wks of Tai Chi | SMD = 0.45 (95% CI 0.22, 0.67) | Small to moderate |
| Balance and mobility | ||||
| Timed Up-and-Go Test | Huang and Liu (2015) 20 | Adults >60 yrs, 10-24 wks of Tai Chi | MD = 1.0 (95% CI 0.7, 1.4) | Small |
| Bone mineral density | ||||
| Lumbar spine | Sun et al (2016) 31 | Perimenoppausal and postmenopausal women, 5-12 mo of Tai Chi | MD = 0.03 (95% CI 0.01, 0.05) | Very small |
| Cardiorespiratory fitness | ||||
| Oxygen pulse | Zheng et al (2015) 40 | Healthy community-dwellers aged 45-75 yrs, average of 1-4.7 yrs of Tai Chi | SMD = 1.04 (95% CI 0.69, 1.39) | Very large |
| Peak oxygen uptake | Zheng et al (2015) 40 | Healthy community-dwellers aged 45-75 yrs, average of 1-4.7 yrs of Tai Chi | SMD = 1.33 (95% CI 0.97, 1.70) | Very large |
| Cognition | ||||
| Executive Function | Wayne et al (2014) 34 | Cognitively healthy adults >60 yrs, 24-40 wks of Tai Chi vs active comparison | SMD = 0.51 (95% CI 0.17, 0.85) | Moderate |
| Executive Function | Wayne et al (2014) 34 | Cognitively healthy adults >60 yrs, 10-40 wks of Tai Chi vs control | SMD = 0.39 (P = .004) | Small to moderate |
| Global Cognition | Wayne et al (2014) 34 | Cognitively impaired adults >60 yrs, 3-12 mo of Tai Chi vs active comparison | SMD = 0.30 (95% CI 0.11, 0.49) | Small |
| Global Cognition | Wayne et al (2014) 34 | Cognitively impaired adults >60 yrs, 12-24 wks of Tai Chi vs control | SMD = 0.35 (95% CI 0.11, 0.58) | Small to moderate |
| Falls | ||||
| Falls incidence | Lomas-Vega et al (2017) 28 | At-risk and older adults 56-99 yrs, 12-24 wks of Tai Chi | IRR = 0.87 (95% CI 0.77, 0.99) | Small |
| Number of fallers | Huang et al (2017) 21 | People >60 yrs, including 2 studies with people with stroke and 2 with people with Parkinson’s disease, 4 wks to 2 yrs of Tai Chi | RR = 0.80 (95% CI 0.72, 0.88) | Small |
| Proprioception | ||||
| Knee flexion | Zou et al (2019) 41 | People >55 yrs, mostly healthy except 4/9 studies included people with visual impairments, knee osteoarthritis, and cognitive impairments, 12-24 wks of Tai Chi | SMD = −0.82 (95% CI −1.06, −0.58) | Large |
| Ankle dorsiflexion | Zou et al (2019) 41 | Healthy adults >55 yrs, 16-24 wks of Tai Chi | SMD = −0.75 (95% CI −1.11, −0.39) | Moderate to large |
| Ankle plantarflexion | Zou et al (2019) 41 | Healthy adults >55 yrs, 16-24 wks of Tai Chi | SMD = −0.55 (95% CI −0.90, −0.20) | Moderate |
| Sleep | ||||
| Global score | Du et al (2015) 18 | Adults >60 yrs, 8-12 wks of Tai Chi | SMD = −0.79 (95% CI −1.46, −0.12) | Moderate to large |
| Daytime dysfunction | Adults >60 yrs, 8-24 wks of Tai Chi | SMD = −0.34 (95% CI −0.59, −0.09) | Small to moderate | |
| Habitual sleep efficiency | Adults >60 yrs, 8-24 wks of Tai Chi | SMD = −0.49 (95% CI −0.74, −0.23) | Small to moderate | |
| Sleep disturbance | Adults >60 yrs, 8-24 wks of Tai Chi | SMD = −0.44 (95% CI −0.69, −0.19) | Small to moderate | |
| Sleep duration | Adults >60 yrs, 8-16 wks | SMD = −0.55 (95% CI −0.90, −0.21) | Moderate | |
| Strength | ||||
| Isokinetic knee extensors (N) | Liu et al (2011) 26 | Males, > 55 yrs, 16 wks to average of 11 mo of Tai Chi | MD = 22.7 (95% CI 10.3, 35.1) | Small to moderate |
| Isokinetic knee flexors (N) | Liu et al (2011) 26 | Females, >55 yrs, 16 wks to average of 11 mo of Tai Chi | MD = 15.9 (95% CI 9.0, 22.9) | No information available to interpret MD |
| Isokinetic knee flexors (N) | Liu et al (2011) 26 | Males, >55 yrs, 16 wks to average of 11 mo of Tai Chi | MD = 17.5 (95% CI 7.0, 28.0) | No information available to interpret MD |
| Stroke risk factors | ||||
| Obesity (body mass index) | Lauche et al (2017) 23 | Adults >45 yrs, 10-12 wks of Tai Chi | MD = −1.7 (95% CI −3.1, −0.2) | No information available to interpret MD |
| Fasting blood glucose | Lauche et al (2017) 23 | Adults >45 yrs with type 2 diabetes, 12 wks of Tai Chi | MD = −8.88 (95% CI −16.73, −1.03) | No information available to interpret MD |
| Homeostatic model | Lauche et al (2017) 23 | Adults >45 yrs with type 2 diabetes, 12-24 wks of Tai Chi | MD = −2.9 (95% CI −5.4, −0.4) | No information available to interpret MD |
| Assessment index | ||||
Abbreviations: IRR, incidence rate ratio; MD, mean difference; mo, months; RR, relative risk; wks, weeks; yrs, years.
Table 3.
Bottom-Line Summary of Optimal “High” and “Moderate” Quality Evidence by Magnitude of Effect (ie, Where There Is Evidence of Interpretation).
| Magnitude of effect | Outcome for “high” quality evidence | Outcome for “moderate” quality evidence |
|---|---|---|
| Very large (SMDs ≥1.0 to 1.33) | Improved cardiorespiratory fitness (better forced vital capacity >3.5 × MDC with an average of 10.5 years of practice) | Improved cardiorespiratory fitness (better peak oxygen uptake and oxygen pulse with 1-4.7 years of practice) |
| 89% risk reduction of non-fatal stroke (with 1-2 years of practice) | ||
| Large (SMDs >0.80 to <1.00) | Improved balance using mixed measures (with 20-24 weeks of practice) | Improved balance using direct measures (with 10-12 weeks of practice) |
| Improved subjective sleep quality (with 8-24 weeks of practice) | Improved knee proprioception (with 12-24 weeks of practice) | |
| Improved in knee extensor strength in women (with 4–12 months of practice) | ||
| Moderate to large (SMDs ≥0.65 to <0.80) | 43% risk reduction of falls among adults >55 at risk for falls (with <12 months of practice) | Improved in global sleep score (with 8-12 weeks of practice) |
| Improved ankle dorsiflexion proprioception (with 16-24 weeks of practice) | ||
| Moderate (SMDs ≥0.50 to <0.65) | Improved sleep duration (with 8-16 weeks of practice) | |
| Improved ankle plantarflexion (with 16-24 weeks of practice) | ||
| Improved cognition (executive function, with 24-40 weeks of practice) | ||
| Small to moderate (SMDs ≥0.30 to <0.50) | Improved sleep efficiency and reduced sleep disturbance (with 8-24 weeks of practice) | |
| Improved global cognition (with 12-24 weeks of practice) | ||
| Reduced daytime dysfunction due to sleep disturbance (with 8-24 weeks of practice) | ||
| Improved knee extensor strength in men (with 4-11 months of practice) |
Abbreviations: MDC, minimal detectable change; SMD, standardized mean difference.
All of the statistically significant results favored the Tai Chi intervention, except for one result in the heterogeneous findings (* in Table 1). In a meta-analysis of the outcome of cardiorespiratory fitness, 40 heart rate was significantly higher immediately after Tai Chi compared to the nonintervention control groups. Of the 66 statistically significant results favoring Tai Chi, 39 (59%) received quality ratings of either “high” or “moderate.” Of the 27 statistically significant results with “low” or “very low” quality ratings, 14 were due to a mix of samples (ie, adults with and without health conditions) and 10 were associated with weaker study designs. In contrast, 3 (12%) of the 25 insignificant results received quality ratings of either “high” or “moderate” (with adequate sample sizes), with poor methodologic quality and small sample sizes contributing to lack of power in the remaining studies. Of the 27 meta-analyses, 22 did not mention adverse events at all and 5 reported either “no adverse events” or reported events having occurred, none of which were attributed to Tai Chi.
Discussion
Twenty-seven meta-analyses were synthesized in this scoping review with the aim of summarizing the current knowledge of the effectiveness of Tai Chi on health promotion of older adults. “High” and “moderate” quality evidence indicates that practicing Tai Chi can lead to significant improvements in balance, cardiorespiratory fitness (forced vital capacity and peak oxygen uptake), cognition (global cognition and executive function), mobility, proprioception, sleep and strength, as well as significant reductions in the incidence of falls and nonfatal stroke and reduction in stroke risk factors. Additional preliminary evidence from heterogeneous findings includes potential benefits for adults on the following outcomes: body composition, bone mineral density, cardiorespiratory fitness (diastolic and systolic blood pressure, heart rate, and stair test), cardiovascular disease risk factors, cognition (memory function), physical function, and psychological health (anxiety, depression, and stress). One of the meta-analyses included in this scoping review noted that heart rate was significantly higher immediately after practicing Tai Chi, compared to a nonintervention group, 40 supporting the belief that Tai Chi offers some level of aerobic training. “High” quality evidence suggests Tai Chi has no effects on time to first fall in at-risk and older adults and on cardiorespiratory fitness when practiced for durations as short as 2 to 3 months. Conversely, a very large effect on forced vital capacity was found among people who had been practicing for an average of 10.5 years. Adverse events were inconsistently reported; the few studies that did report adverse events did not attribute them to Tai Chi.
Strengths of our work include the reduced threat of publication bias. We conducted a thorough search on multiple databases (which identified meta-analyses that searched multiple Chinese and Korean databases, in addition to English ones) up to the end of August 2019. Our broader search strategy allowed us to evaluate a collection of relevant meta-analyses which were previously not appraised by Solloway et al 8 and Huston and MacFarlane. 9 In contrast to previous literature,8,9 only meta-analyses were included in this scoping review with the aim of obtaining greater certainty by evaluating the quality of evidence. Each meta-analysis was evaluated using a transparent method by 2 independent raters who produced detailed data extraction tables prior to preparing the summary tables. Additionally, our study focused on summarizing the current knowledge on the effectiveness of Tai Chi on older adults across a range of general health outcomes, whereas previous studies8,9 examined both older adults on general health outcomes and individuals with health conditions.
Limitations of our work arise due to the inconsistent reporting of adverse events in the appraised meta-analyses; this reduces our ability to draw a firm conclusion on the safety of practicing Tai Chi. Nonetheless, most of the events that were reported were minor and not attributed to the practice of Tai Chi. The deduplication and the initial screening processes were performed entirely by the corresponding author; however, we believe this limitation is minimized when considering her more than 30 years of experience as a researcher. 10 In addition, we found it necessary to modify the GRADE guidelines 13 to be more appropriate for studies focusing on rehabilitation than medicine. 10 As previously stated by Wayne and Kaptchuck, 46 the evolving art of Tai Chi is practiced in diverse styles, with each placing variable emphases on the principles of Tai Chi and the content of training. For this reason, we decided to use the heterogeneity criterion as the initial screen, with any statically significant but heterogeneous findings considered only as preliminary evidence. Furthermore, the nature of Tai Chi makes blinding the instructors and participants neither possible nor desirable; 46 therefore, we did not downgrade for lack of blinding. Last, as the focus of our work was on general health outcomes and health promotion, we did not downgrade the use of surrogate measures as a source of indirectness. These modifications to the GRADE guidelines, or use of other guidelines, 12 could lead to disparity in results of a future scoping review on the same topic.
This scoping review summarizes the current knowledge about the effectiveness of Tai Chi for older adults across a range of general health outcomes, with “high” and “moderate” quality evidence providing a level of certainty to health care providers in recommending Tai Chi practice to their older clients. As Tai Chi is a meditative martial art that consists of a series of gentle movements designed to strengthen and relax the body and mind, 9 health care professionals can recommend Tai Chi as a source of physical activity, especially for clients aiming to enhance specific outcomes identified in our work. We believe that evaluating the effectiveness of Tai Chi is important as health care is slowly undergoing a paradigm shift in which a biopsychosocial model of care is gaining popularity. 52 Incorporating a Tai Chi program in a client’s plan not only improves pathology and function but also enhances the individual’s body, mind, and spirit, providing an intervention targeting many aspects of the biopsychosocial model. 10
Given the number of different styles and forms of Tai Chi practiced around the world, opportunities for future research are numerous. In addition to styles and forms, variation can also arise from how Tai Chi is taught and transmitted to the students, thus creating heterogeneity in how Tai Chi is practiced. 46 This heterogeneity limits the conclusions that can be drawn from individual studies. 46 For this reason, future studies should focus on outcomes associated with Tai Chi training as a function of different styles, forms, dosage, and teaching instruction with the aim of discovering the most effective type of Tai Chi engagement. Time is an important factor of physical and psychological interventions; 53 however, the majority of the studies evaluated in this scoping review were only 3 to 6 months in duration. Future research should focus on more longitudinal studies, learning how the benefits of Tai Chi accumulate over time, as the participants become more skilled. Additionally, more studies should be done evaluating the effectiveness of Tai Chi on the health promotion of younger and middle-aged individuals, 53 as the majority of the literature, including our work, focuses on older adults. Last, as stated by Wayne and Kaptchuk, 46 in order to conduct an evidence-based evaluation of Tai Chi, other methods of research such as pragmatic trials, cross-sectional studies of long-term practitioners, community-based prospective cohort studies conducted in ecologically valid settings, and qualitative studies should all be performed in order to better understand the complex and multidimensional aspects of Tai Chi, because intentions, beliefs, teacher-student relationships, and the length of the training likely play a role in the effectiveness of Tai Chi. 46 Furthermore, given the paucity of information on the MCID or MDC of many general health outcomes for older adults, research that assists with interpretation of the magnitude of effects is warranted. Alternatively, authors of meta-analyses could consider reporting all results in standardized mean differences, which can be interpreted using long-recognized guidelines. 51
In conclusion, Tai Chi is an effective, enjoyable, and inexpensive form of exercise intervention that is accessible to a wide range of the population, with 10 or without various health conditions. The results of our study enable health care service providers to recommend Tai Chi as a form of exercise intervention for older adults across a range of general health outcomes with a relatively high level of certainty with the goal of health promotion and improvement of overall well-being.
Supplemental Material
Supplemental material, sj-docx-1-ajl-10.1177_15598276211001291 for Effectiveness of Tai Chi for Health Promotion of Older Adults: A Scoping Review of Meta-Analyses by Fei-Chi Yang, Aishwarya B. Desai, Pelareh Esfahani, Tatiana V. Sokolovskaya and Doreen J. Bartlett in American Journal of Lifestyle Medicine
Supplemental material, sj-docx-2-ajl-10.1177_15598276211001291 for Effectiveness of Tai Chi for Health Promotion of Older Adults: A Scoping Review of Meta-Analyses by Fei-Chi Yang, Aishwarya B. Desai, Pelareh Esfahani, Tatiana V. Sokolovskaya and Doreen J. Bartlett in American Journal of Lifestyle Medicine
Supplemental material, sj-docx-3-ajl-10.1177_15598276211001291 for Effectiveness of Tai Chi for Health Promotion of Older Adults: A Scoping Review of Meta-Analyses by Fei-Chi Yang, Aishwarya B. Desai, Pelareh Esfahani, Tatiana V. Sokolovskaya and Doreen J. Bartlett in American Journal of Lifestyle Medicine
Supplemental material, sj-docx-4-ajl-10.1177_15598276211001291 for Effectiveness of Tai Chi for Health Promotion of Older Adults: A Scoping Review of Meta-Analyses by Fei-Chi Yang, Aishwarya B. Desai, Pelareh Esfahani, Tatiana V. Sokolovskaya and Doreen J. Bartlett in American Journal of Lifestyle Medicine
Supplemental material, sj-docx-5-ajl-10.1177_15598276211001291 for Effectiveness of Tai Chi for Health Promotion of Older Adults: A Scoping Review of Meta-Analyses by Fei-Chi Yang, Aishwarya B. Desai, Pelareh Esfahani, Tatiana V. Sokolovskaya and Doreen J. Bartlett in American Journal of Lifestyle Medicine
Supplemental material, sj-docx-6-ajl-10.1177_15598276211001291 for Effectiveness of Tai Chi for Health Promotion of Older Adults: A Scoping Review of Meta-Analyses by Fei-Chi Yang, Aishwarya B. Desai, Pelareh Esfahani, Tatiana V. Sokolovskaya and Doreen J. Bartlett in American Journal of Lifestyle Medicine
Acknowledgments
We thank John Costella, Research Librarian at Western University, who provided expert advice and guidance in planning our comprehensive search strategy and for orienting us to Zotero, the database management system that we used. Second, we thank Tianna Deluzio, research assistant, who ably conducted the database searches and downloaded the products of the search into Zotero, under the supervision of John Costella. Bartlett is a volunteer Continuing-Instructor-in-Training under the supervision of Fung Loy Kok Institute of Taoism and Professor Emerita at Western University.
Footnotes
Authors’ Note: As this is Part 2 of a pair of studies, portions of the acknowledgements, abstract, methods, references, and appendices from previously published work re reproduced with permission of Taylor & Francis Ltd (Easwaran K, Gopalasingam Y, Green DD, Lach V, Melnyk J, Wan C, Bartlett DJ. Effectiveness of Tai Chi for health promotion for adults with health conditions: A scoping review of meta-analyses. Disability and Rehabilitation. Published online February 18, 2020. https://doi.org/10.1080/09638288.2020.1725916.
Author Contributions: The first (then student) author consistently provided excellent contributions throughout this research, including facilitating resolution of the results of the peer-review process. The next three authors contributed similarly to the work reported here (and therefore are presented in alphabetical order by last name) as part of the degree completion of the MPT Program, under the supervision of Bartlett. Doreen Bartlett contributed to the study conception and design and participated in the literature search. All authors contributed to the critical appraisal of the systematic reviews, and subsequent data extraction and analyses for the appendices and tables. Tatiana Sokolovskaya prepared the first draft of the introduction; Doreen Bartlett wrote the methods section; the results were collated by Pelareh Esfahani and Fei-Chi Yang (who also finalized the references); the discussion was drafted by Aishwarya Desai. All authors commented on previous versions of the manuscript, and read and approved the final manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: Not applicable for a scoping review.
Informed Consent: Not applicable for a scoping review.
Trial Registration: Not applicable for a scoping review.
ORCID iD: Doreen J. Bartlett  https://orcid.org/0000-0001-5469-2696
https://orcid.org/0000-0001-5469-2696
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Boisvert-Vigneault K, Payette H, Audet M, Gaudreau P, Bélanger M, Dionne IJ. Relationships between physical activity across lifetime and health outcomes in older adults: results from the NuAge cohort. Prev Med. 2016;91:37-42. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Frequently asked questions. Accessed February 23, 2021. https://www.who.int/about/who-we-are/frequently-asked-questions
- 3.Canadian Society for Exercise Physiology. Canadian physical activity guidelines for older adults—65 years & older. Accessed February 23, 2021. https://www.csep.ca/CMFiles/Guidelines/CSEP_PAGuidelines_older-adults_en.pdf
- 4.Hsieh CC, Lin PS, Wei YT, Huang YC. Tai Chi based exergaming program for older adults at risk of cognitive impairment. Physiotherapy. 2015;101:e592. [Google Scholar]
- 5.Wu MT, Tang PF, Goh JOS, et al. Task-switching performance improvements after Tai Chi Chuan training are associated with greater prefrontal activation in older adults. Front Aging Neurosci. 2018;10:280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lan C, Chen SY, Lai JS, Wong AMK. Tai Chi Chuan in medicine and health promotion. Evid Based Complement Altern Med. 2013;2013:502131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Song QH, Shen GQ, Xu RM, et al. Effect of Tai Chi exercise on the physical and mental health of the elder patients suffered from anxiety disorder. Int J Physiol Pathophysiol Pharmacol. 2014;6:55-60. [PMC free article] [PubMed] [Google Scholar]
- 8.Solloway MR, Taylor SL, Shekelle PG, et al. An evidence map of the effect of Tai Chi on health outcomes. Syst Rev. 2016;5:126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huston P, McFarlane B. Health benefits of Tai Chi: what is the evidence? Can Fam Physician. 2016;62:881-890. [PMC free article] [PubMed] [Google Scholar]
- 10.Easwaran K, Gopalasingam Y, Green D, et al. Effectiveness of Tai Chi for health promotion for adults with health conditions: a scoping review of meta-analyses. Disabil Rehabil. Published online February 18, 2020. doi: 10.1080/09638288.2020.1725916 [DOI] [PubMed] [Google Scholar]
- 11.Levac D, Colquhoun H, O’Brien K. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Colquhoun HL, Levac D, O’Brien KK, et al. Scoping reviews: time for clarity in definitions, methods, and reporting. J Clin Epidemiol. 2014;67:1291-1294. [DOI] [PubMed] [Google Scholar]
- 13.Schűnemann H, Brozek J, Guyyat G, Oxman A. GRADE Handbook. Accessed February 23, 2021. http://gdt.guidelinedevelopment.org/app/handbook/handbook.html
- 14.Meserve C, Kalet A, Zabar S, Hanley K, Schwartz MD. Clever nihilism: cynicism in evidence-based medicine learners. Med Educ Online. 2005;10:4372. [DOI] [PubMed] [Google Scholar]
- 15.Sumsion T, Law M. A review of evidence on the conceptual elements informing client-centred practice. Can J Occup Ther. 2006;73:153-162. [DOI] [PubMed] [Google Scholar]
- 16.Alenazi AM, Alshehri MM, Hoover JC, Yabroudi MA, Kachanathu SJ, Liu W. The effect of T’ai Chi exercise on lipid profiles: a systematic review and meta-analysis of randomized clinical trials. J Altern Complementary Med. 2018;24:220-230. [DOI] [PubMed] [Google Scholar]
- 17.Chen S, Zhang Y, Chen H, Li C. Effects of Tai Chi exercise on people of middle/senior age with sub-health condition. A systematic review and meta-analysis. Asian J Ex Sports Sci. 2014;11:55-63. [Google Scholar]
- 18.Du S, Dong J, Zhang H, et al. Tai Chi exercise for self-rated sleep quality in older people: a systematic review and meta-analysis. Int J Nurs. 2015;52:368-379. [DOI] [PubMed] [Google Scholar]
- 19.Hu YN, Chung YJ, Yu HK, Chen YC, Tsai CT. Effect of Tai Chi exercise on fall prevention in older adults: systematic review and meta-analysis of randomized controlled trials. Int J Gerontol. 2016;10:131-136. [Google Scholar]
- 20.Huang Y, Liu X. Improvement of balance control ability and flexibility in the elderly Tai Chi Chuan (TCC) practitioners: a systematic review and meta-analysis. Arch Gerontol Geriatr. 2015;60:233-238. [DOI] [PubMed] [Google Scholar]
- 21.Huang ZG, Feng YH, Li YH, Lv CS. Systematic review and meta-analysis: Tai Chi for preventing falls in older adults. BMJ Open. 2017;7:e013661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Larkey LK, James D, Belyea M, Jeong M, Smith LL. Body composition outcomes of Tai Chi and Qigong practice: a systematic review and meta-analysis of randomized controlled trials. Int J Behav Med. 2018;25:487-501. [DOI] [PubMed] [Google Scholar]
- 23.Lauche R, Peng W, Ferguson C, et al. Efficacy of Tai Chi and Qigong for the prevention of stroke and stroke risk factors: a systematic review with meta-analysis. Medicine (Baltimore). 2017;96:e8517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee MS, Lee EN, Ernst E. Is Tai Chi beneficial for improving aerobic capacity? A systematic review. Br J Sports Med. 2009;43:569-573. [DOI] [PubMed] [Google Scholar]
- 25.Lee MS, Lee EN, Kim JI, Ernst E. Tai Chi for lowering resting blood pressure in the elderly: a systematic review. J Eval Clin Pract. 2010;16:818-824. [DOI] [PubMed] [Google Scholar]
- 26.Liu B, Liu ZH, Zhu HE, Mo JC, Cheng DH. Effects of Tai Chi on lower-limb myodynamia in the elderly people: a meta-analysis. J Tradit Chin Med. 2011;31:141-146. [DOI] [PubMed] [Google Scholar]
- 27.Liu F, Wang S. Effect of Tai Chi on bone mineral density in postmenopausal women: a systematic review and meta-analysis of randomized controlled trials. J Chin Med Assoc. 2017;80:790-795. [DOI] [PubMed] [Google Scholar]
- 28.Lomas-Vega R, Obrero-Gaitan E, Molina-Ortega FJ, Del-Pino-Casado R. Tai Chi for risk of falls. A meta-analysis. J Am Geriatr Soc. 2017;65:2037-2043. [DOI] [PubMed] [Google Scholar]
- 29.Pan XH, Mahemuti A, Zhang XH, et al. Effect of Tai Chi exercise on blood lipid profiles: a meta-analysis of randomized controlled trials. J Zhejiang Univ Sci B. 2016;17:640-648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Song R, Ahn S, So H, Lee EH, Chung Y, Park M. Effects of T’ai Chi on balance: a population-based meta-analysis. J Complement Altern Med. 2015;21:141-151. [DOI] [PubMed] [Google Scholar]
- 31.Sun Z, Chen H, Berger MR, Zhang L, Guo H, Huang Y. Effects of Tai Chi exercise on bone health in perimenopausal and postmenopausal women: a systematic review and meta-analysis. Osteoporos Int. 2016;27:2901-2911. [DOI] [PubMed] [Google Scholar]
- 32.Wang C, Bannuru R, Ramel J, Kupelnick B, Scott T, Schmid CH. Tai Chi on psychological well-being: systematic review and meta-analysis. BMC Complement Altern Med. 2010;10:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang Y, Shan W, Li Q, Yang N, Shan W. Tai Chi exercise for the quality of life in a perimenopausal women organization: a systematic review. Worldviews Evid Based Nurs. 2017;14:294-305. [DOI] [PubMed] [Google Scholar]
- 34.Wayne PM, Walsh JN, Taylor-Piliae RE, et al. Effect of Tai Chi on cognitive performance in older adults: systematic review and meta-analysis. J Am Geriatr Soc. 2014;62:25-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wu Y, Wang Y, Burgess EO, Wu J. The effects of Tai Chi exercise on cognitive function in older adults: a meta-analysis. J Sport Health Sci. 2013;2:193-203. [Google Scholar]
- 36.Xiang Y, Lu L, Chen X, Wen Z. Does Tai Chi relieve fatigue? A systematic review and meta-analysis of randomized controlled trials. PLoS One. 2017;12:e0174872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang S, Zou L, Chen LZ, et al. The effect of Tai Chi Chuan on negative emotions in non-clinical populations: a meta-analysis and systematic review. Int J Environ Res Public Health. 2019;16:3033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhao Y, Wang Y, Xu XD, Liu YL. Effectiveness of Tai Chi in fall prevention and balance function in the elderly: a meta-analysis. Chin J Evid Based Med. 2013;13:339-345. [Google Scholar]
- 39.Zheng G, Huang M, Liu F, Li S, Tao J, Chen L. Tai Chi Chuan for the primary prevention of stroke in middle-aged and elderly adults: a systematic review. Evid Based Complement Altern Med. 2015;2015:742152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zheng G, Li S, Huang M, Liu F, Tao J, Chen L. The effect of Tai Chi training on cardiorespiratory fitness in healthy adults: a systematic review and meta-analysis. PLoS One. 2015;10:e0117360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zou L, Han J, Li C, et al. The effects of Tai Chi on lower limb proprioception in adults aged over 55: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2019;100:1102-1113. [DOI] [PubMed] [Google Scholar]
- 42.Zou L, Wang C, Chen K, et al. The effect of Taichi practice on attenuating bone mineral density loss: a systematic review and meta-analysis of randomized controlled trials. Int J Environ Res Public Health. 2017;14:1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wayne PM, Kaptchuk TJ. Challenges inherent to T’ai Chi research: part I—Tai Chi as a complex multicomponent intervention. J Altern Complement Med. 2008;14:95-102. [DOI] [PubMed] [Google Scholar]
- 44.Wayne PM, Berkowitz DL, Litrownik DE, Buring JE, Yeh GY. What do we know about the safety of Tai Chi? A systematic review of adverse event reports in randomized trials. Arch Phys Med Rehabil. 2014;95:2470-2483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Higgins JPT, Altman DG, Gotzche PC; Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane Collaboration’s tool for assessing risk of bias in randomized trials. BMJ. 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wayne PM, Kaptchuk TJ. Challenges inherent to Tai Chi research: part II—defining the intervention and optimal study design. J Altern Complement Med. 2008;14:191-197. [DOI] [PubMed] [Google Scholar]
- 47.Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83:713-721. [PubMed] [Google Scholar]
- 48.Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1-12. [DOI] [PubMed] [Google Scholar]
- 49.Fletcher RH, Fletcher SW, Fletcher GS. Clinical Epidemiology: The Essentials. Wolters Kluwer Health/Lippincott Williams & Wilkins; 2014. [Google Scholar]
- 50.World Health Organization. International classification of functioning, disability and health: ICF. Accessed February 23, 2021. https://apps.who.int/iris/handle/10665/42407
- 51.Cohen J. Statistical Power Analysis for the Behavioral Sciences. Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 52.Sanders T, Foster NE, Bishop A, Ong BN. Biopsychosocial care and the physiotherapy encounter: physiotherapists’ accounts of back pain consultations. BMC Musculoskelet Disord. 2013;14:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kuramoto AM. Therapeutic benefits of Tai Chi exercise: Research review. WMJ. 2006;105:42-46. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-ajl-10.1177_15598276211001291 for Effectiveness of Tai Chi for Health Promotion of Older Adults: A Scoping Review of Meta-Analyses by Fei-Chi Yang, Aishwarya B. Desai, Pelareh Esfahani, Tatiana V. Sokolovskaya and Doreen J. Bartlett in American Journal of Lifestyle Medicine
Supplemental material, sj-docx-2-ajl-10.1177_15598276211001291 for Effectiveness of Tai Chi for Health Promotion of Older Adults: A Scoping Review of Meta-Analyses by Fei-Chi Yang, Aishwarya B. Desai, Pelareh Esfahani, Tatiana V. Sokolovskaya and Doreen J. Bartlett in American Journal of Lifestyle Medicine
Supplemental material, sj-docx-3-ajl-10.1177_15598276211001291 for Effectiveness of Tai Chi for Health Promotion of Older Adults: A Scoping Review of Meta-Analyses by Fei-Chi Yang, Aishwarya B. Desai, Pelareh Esfahani, Tatiana V. Sokolovskaya and Doreen J. Bartlett in American Journal of Lifestyle Medicine
Supplemental material, sj-docx-4-ajl-10.1177_15598276211001291 for Effectiveness of Tai Chi for Health Promotion of Older Adults: A Scoping Review of Meta-Analyses by Fei-Chi Yang, Aishwarya B. Desai, Pelareh Esfahani, Tatiana V. Sokolovskaya and Doreen J. Bartlett in American Journal of Lifestyle Medicine
Supplemental material, sj-docx-5-ajl-10.1177_15598276211001291 for Effectiveness of Tai Chi for Health Promotion of Older Adults: A Scoping Review of Meta-Analyses by Fei-Chi Yang, Aishwarya B. Desai, Pelareh Esfahani, Tatiana V. Sokolovskaya and Doreen J. Bartlett in American Journal of Lifestyle Medicine
Supplemental material, sj-docx-6-ajl-10.1177_15598276211001291 for Effectiveness of Tai Chi for Health Promotion of Older Adults: A Scoping Review of Meta-Analyses by Fei-Chi Yang, Aishwarya B. Desai, Pelareh Esfahani, Tatiana V. Sokolovskaya and Doreen J. Bartlett in American Journal of Lifestyle Medicine