Abstract
Background. Taking into account the disproportionate impacts of disease burden from chronic conditions by racial and ethnic group, this scoping review sought to examine the extent to which nutritional interventions incorporated culturally relevant topics into their design and analyses. Methods. A literature search of 5 databases was conducted for any peer-reviewed studies on nutritional and culinary medicine interventions published between 2000 and 2019. Results. Studies were divided into 2 categories, medical education interventions (n = 12) and clinical/community interventions (n = 20). The majority of medical education interventions were not culturally tailored and focused on obesity/weight management within the Northeast and Southeast United States. In contrast, clinical/community interventions were primarily culturally tailored for Latinos/Hispanics and African American/Black populations residing in the Northeast and diagnosed with prediabetes/diabetes mellitus or hypertension/cardiovascular disease. Conclusions. This review identified an existent gap and need for inclusive studies that consider the culturally relevant topics into the design and implementation of nutritional intervention studies. Studies within medical education appeared to be the area where these changes can be most beneficial. There may be some value among clinic and communal-based studies in stratifying heterogeneous subgroups because of the missed cultural nuances missed when grouping larger racial cohorts.
Keywords: cultural competency, culinary medicine, nutritional medicine, nutrition, chronic disease
Culinary medicine is defined as an evidence-based field in medicine that aims to educate patients with the appropriate knowledge on the interplay of food and medicine.
The leading cause of death and disability in the United States can be attributed to chronic diseases. It is estimated that 6 in 10 US adults have one chronic disease (related to cardiovascular disease, cancer, chronic obstructive pulmonary disease, and diabetes) and 4 in 10 US adults have 2 or more chronic diseases. 1 Chronic diseases account for approximately 1.7 million deaths annually, which are two thirds of all US deaths. 2 Furthermore, these conditions account for 75% of health care spending, which equates to approximately $5300 per person annually. This number is even more staggering when looking at Medicare and Medicaid, as the management of chronic diseases accounts for 96% and 83% of health care spending, respectively. 3
Studies have identified disparities in chronic diseases by racial and ethnic groups where Hispanics/Latinos and African Americans disproportionately carry the associated burdens of disease. These disparities are apparent when examining the earlier onset and/or faster development of chronic diseases in comparison to their White counterparts. 4 But these disparities are not only limited to Hispanics/Latinos and African Americans. Similarly, Native Americans suffer from many of the same chronic illnesses as mentioned above, with cardiovascular diseases and diabetes as some of the leading causes of death in this population. 5 Most of these health challenges are attributable to the economic adversity and poor social conditions such as inadequate education and discriminatory health care delivery, in part from the historically low percentage of Native American physicians.6,7 Additionally, Southeast Asians suffer from some of the highest rates of cardiovascular disease out of all ethnic groups. Yet this fact is not readily apparent as Asian Americans have commonly been examined as a monolithic group masking the health needs of individual subgroups.8,9
Incorporating nutritional education into the clinical encounter embraces a more holistic approach to patient care. Although primary care physicians have expressed favorable attitudes toward the incorporation of clinical nutrition in their own practices, 10 physicians in different specialties, such as cardiology, have expressed limited nutritional knowledge. 11 Similarly, studies have demonstrated how nutritional education is insufficiently incorporated into medical curricula despite region or stage of training. 12
There have been steps taken toward addressing this educational gap through the introduction of culinary medicine. Culinary medicine is defined as an evidence-based field in medicine that aims to educate patients with the appropriate knowledge on the interplay of food and medicine. The ultimate goal is to empower patients to make conscientious medical and personal decisions by way of accessing and eating high-quality meals. 13 And as early as 1995, the University of North Carolina at Chapel Hill developed a Nutrition in Medicine project for medical students. This resource was provided free of charge to any interested medical schools with the goal of integrating preventive and therapeutic aspects of nutrition into medical school curricula. 14 In 2013, the first culinary medicine center was started at Tulane University to centralize and provide the most comprehensive culinary medicine curriculum for all health professions including offering Culinary Medicine Continuing Medical Education credits. 15
Food intake patterns and behaviors are considerably varied across racial and ethnic groups. Different ethnic groups practice unique dietary customs or behaviors that may be affected by their environment, socioeconomic status, and cultural factors. This variance in diet has been partly shown to play an important role in the disproportionate representation of chronic diseases. 16 Because of the wide range and variability in dietary consumption, this scoping review aimed to understand the cultural tailoring and applicability of nutritional interventions in the current literature.
Methods
Scoping reviews provide a useful approach in evaluating the extent and depth of academic involvement of the subject under study, 17 particularly among areas of emerging research. 18 Employing this approach allows for researchers to identify the general direction of a scholarly area of interest 17 and, most important, the existing gaps in the literature that would guide future inquiry. 18 Understanding the utility and strength of this approach, we conducted a scoping review to identify the extent to which the current literature on culinary and nutritional medicine interventions have incorporated culturally relevant concepts into their design, implementation, and evaluation. The methodological frameworks outlined by Arksey and O’Malley 17 as well as Levac et al 19 were used to guide our undertaking of this scoping review.
Identifying Research Question
The primary aim of this broad scoping review was to examine the incorporation of cultural relevant concepts in the current literature on culinary and nutritional medicine interventions.
The research team decided to dually focus on assessing interventions within medical education, where undergraduate medical trainees were the target population, as well as interventions within clinical or communal settings with patients as the target population. Our guiding research questions included the following: (1) What proportion of studies have specifically discussed the use or tailoring of culturally relevant concepts in their design, implementation, and evaluation? (2) Which chronic health conditions have been targeted by these same types of interventions? (3) What ethnic and/or racial groups have these interventions been implemented among or designed around? (4) Geographically, where have these interventions been implemented? We utilized this broad approach in designing our scoping review since no other study, to the best of our knowledge, has previously examined culinary and nutritional medicine interventions or their cultural relevancy.
Identifying Relevant Studies
Our study team consulted with 2 medical librarians associated with our institution prior to designing a literature search schema. After consultation and further discussion, the following databases were used to perform our literature search: PubMed, Scopus, Web of Science, CINAHL (Cumulative Index to Nursing and Allied Health Literature), and the Cochrane Database of Systematic Reviews. The Boolean search terms combinations used included the following: “culinary medicine”; “cultural competency” and “nutrition” and “medical education”; “culture” and “nutrition” and “medical education”; “patient nutrition education” and “culture”; “dietary” and “education” and “medical student.”
Study Selection
We limited our review to studies (1) based in the United States, (2) written in English, (3) provided an evaluation of primary or secondary data from an intervention, and (4) were published between January 1, 2000, and November 30, 2019. The research team additionally decided to limit our literature search to studies that have specifically focused on adult populations (>18 years of age) with chronic health conditions associated with behavioral influences. This included but was not limited to type 2 diabetes mellitus (DM), hypertension, heart disease, hyperlipidemia, and obesity. Studies were excluded if they were conducted among (1) pediatric populations (<18 years of age); (2) patients with genetic, autoimmune, or structural gastroenteropathic conditions like inflammatory bowel disease, celiac disease, lactose intolerance, or malabsorptive conditions; (3) patients with temporally bound conditions like pregnancy or being postoperative from surgical procedures; or (4) were nonhuman subjects research conducted in laboratory settings.
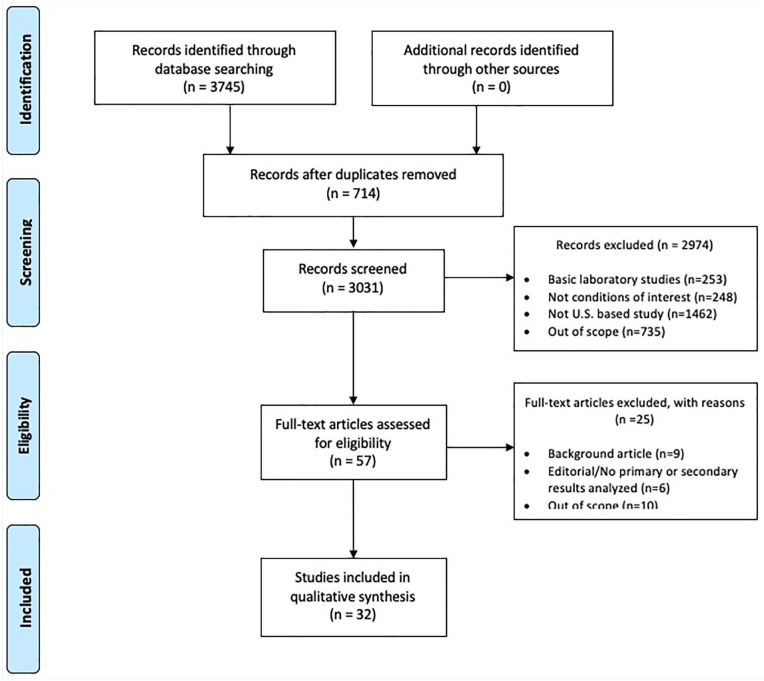
The combinations of Boolean search terms were used to generate an initial collection of articles (n = 3745) that were imported into an EndNote library. After removal of the duplicates (n = 714), the study team (SV, VO, and WJC) independently screened the abstracts from the remaining articles (n = 3031) and coded them for the aforementioned criteria (Figure 1). During this phase of the review, each article was screened by 2 members of the research team with a third used to reconcile differences between the initial coding. The remaining articles (n = 57) were subjected to a full-text review by 2 members of the research team, whereby 25 articles were further excluded (Figure 1). The final set of articles (n = 32) were used in the qualitative synthesis of the scoping review.
Figure 1.
Literature search results and screening procedures.
From: Moher D, Liberati A, Tetzlaff J, Altman DG; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analysis. PLoS Med. 2009;6(7):e1000097.
Data Extraction
A data collection form was created in Microsoft Excel (Microsoft Corp) in order to capture some of the a priori data initially discussed as being important to the review, as well as emergent themes team members identified during their review of the final set of articles. The general information extracted from each article included the author, publication year, study type, specific study population, geographic location of study, chronic health conditions targeted, study outcomes, and main findings. Each article was read by one member of the research team and reviewed by another member during team meetings where discussions focused on thoroughly assessing the trends and broader themes of the literature.
Analysis and Synthesizing Findings
The dataset created from the review of the final set of articles was subjected to quantitative and qualitative analyses. SPSS 24 (Statistical Package for the Social Sciences) was used to understand the distribution of studies conducted in medical education among undergraduate medical trainees versus those conducted in clinical or communal settings among patients. A case study approach and descriptive analysis was utilized to evaluate the final list of studies as a series of cases in exploring the extent to which cultural competency was incorporated into interventions among patients and medical students. The qualitative analysis is included in the discussion section where we unpack the findings of our review and conclude with points of departure on future scholarly engagements within this growing body of literature.
Consultation
Toward the end of our analyses we engaged in the consultation exercise in order to inform and validate the findings from the scoping review. 17 We consulted with 12 researchers not affiliated with our study team that had expertise in medicine, medical education, nutrition, public health, and the social sciences, particularly in cultural and medical anthropology. Feedback provided by the informants was incorporated into our final analysis as seen appropriate by the study team.
Results
The final set of 32 articles were categorized into medical education interventions or clinical/communal interventions. Studies within medical education focused on assessing the implementation of a nutritional intervention within medical school curricula. Clinical or communal studies concentrated on new practices implemented among patients and aimed at assessing the improvement of health outcomes for a variety of different conditions. Of the total 32 articles, 12 articles pertained to medical education interventions and 20 focused on clinical/community interventions. The data aggregated from each article included the following: cultural tailoring, medical conditions addressed, ethnicity of target group, and geographical location of the study. The medical conditions discussed across all studies were classified as prediabetic/DM, obesity/weight management, hypertension/cardiovascular disease, combination of chronic conditions, or unspecified. The geographical locations were categorized as Midwest, West, Southwest, Southeast, Northeast, or multiregional. The ethnic groups discussed among clinical and communal intervention studies included Hispanic/Latino, African American/Black, Native American, and Asian.
Medical Education Interventions
Among the medical education intervention studies (n = 12), only one (8.3%) of the studies was culturally tailored while the majority (n = 11; 91.7%) of the studies were not (Table 1). This study explored teaching students about healthy diet adaptations from multiple cultures, while the remaining studies focused on general diet recommendations. The medical conditions targeted by these studies primarily focused on obesity and weight management (n = 5; 41.7%), followed by unspecified conditions (n = 4; 33.3%), and combinations of varying chronic conditions (n = 2; 16.7%). The setting of these interventions was largely within the Northeast (n = 6; 50%) and Southeast (n = 2; 16.7%) regions of the United States. The remaining 33% of the studies analyzed were categorized as being within the Midwest, West, Southwest, or multiregional.
Table 1.
Summary of Findings From Studies in Medical Education.
| Study | Region | Participants, n | Chronic conditions addressed | Cultural tailoring |
|---|---|---|---|---|
| Birkhead et al (2014) 20 | Southeast | 125 | Obesity/Weight management | No |
| Conroy et al (2004) 21 | Northeast | 137 | General nutrition | No |
| Dreibelbis and George (2017) 22 | Northeast | No indication | General nutrition | No |
| Fang et al (2019) 23 | Northeast | 117 | Obesity/weight management | No |
| Geller et al (2018) 24 | Multiregional | 738 | Obesity/weight management | No |
| Jacob et al (2016) 25 | Northeast | 90 | Obesity/weight management | No |
| Jaroudi et al (2018) 26 | Southwest | 20 | Chronic kidney disease Hypertension Diabetes mellitus Hyperlipidemia |
Yes |
| Krok-Schoen et al (2017) 27 | Midwest | 29 | Prediabetes/diabetes mellitus | No |
| Monlezun et al (2015) 28 | Southeast | 627 | Obesity/weight management | No |
| Pang et al (2019) 29 | West | 40 | Hypertension Diabetes mellitus |
No |
| Schlair et al (2012) 30 | Northeast | 20 | General nutrition | No |
| Wilechansky et al (2016) 31 | Northeast | 64 | Obesity/weight management | No |
Clinical/Communal interventions
A majority (n = 15; 75%) of the 20 articles that discussed clinical or communal interventions were culturally tailored to their targeted patient population (Table 2). Analysis of the distribution of targeted chronic conditions suggested that individuals diagnosed with prediabetes or DM were a primary focus of these interventions (n = 13; 65%). Hypertension and cardiovascular disease were the second most commonly targeted chronic condition of these studies (n = 3; 15%). The patient populations studied were largely Hispanics/Latinos (n = 10; 50%), followed by African Americans/Black (n = 5; 25%), Asians (n = 4; 20%), and Native Americans (n = 1; 5%). A majority of the interventions were applied to patient populations residing in the Northeast (n = 6; 30%), with populations located in the West (n = 5; 25%), Southeast (n = 5; 25%), Midwest (n = 2; 10%), and Southwest (n = 1; 5%) being less frequently studied.
Table 2.
Summary of Findings From Clinical and Community-Based Studies.
| Study | Region | Participants, n | Chronic conditions addressed | Cultural tailoring | Target population |
|---|---|---|---|---|---|
| Amaro et al (2017) 32 | West | 218 | General nutrition | Yes | Hispanic/Latino |
| Brown et al (2002) 33 | Southwest | 256 | Diabetes mellitus | Yes | Hispanic/Latino |
| Coffman et al (2013) 34 | Southeast | 26 | Diabetes mellitus | No | Hispanic/Latino |
| Cooper et al (2015) 35 | Northeast | 21 | Obesity/weight management | Yes | African American/Black |
| Galasso et al (2005) 36 | Unspecified | 26 | Diabetes mellitus | Yes | African American/Black |
| Gibbs et al (2018) 37 | Midwest | 429 | General nutrition | Yes | Hispanic/Latino |
| Ho et al (2018) 38 | West | 20 | Cardiovascular disease | Yes | Asian/Pacific Islander |
| Kattelmann et al (2009) 39 | Midwest | 104 | Diabetes mellitus | Yes | Native American |
| Metghalchi et al (2208) 40 | West | 24 | Diabetes mellitus | Yes | Hispanic/Latino |
| Miller et al (2014) 41 | Southeast | 24 | Diabetes mellitus | Yes | African American/Black |
| Monlezun et al (2015) 42 | Southeast | 27 | Diabetes mellitus | No | African American/Black |
| Perez-Escamilla et al (2015) 43 | Northeast | 211 | Diabetes mellitus | Yes | Hispanic/Latino |
| Rankins et al (2005) 44 | Southeast | 82 | Hypertension | No | African American/Black |
| Salto et al (2011) 45 | West | 39 | Diabetes mellitus | Yes | Hispanic/Latino |
| Seol et al (2017) 46 | Southeast | 30 | Diabetes mellitus | Yes | Hispanic/Latino |
| Song et al (2010) 47 | Northeast | 79 | Diabetes mellitus | Yes | Asian/Pacific Islander |
| Ursua et al (2014) 48 | Northeast | 57 | Hypertension | No | Asian/Pacific Islander |
| Weinstein et al (2014) 49 | Northeast | 78 | Obesity/weight management Diabetes mellitus |
No | Hispanic/Latino |
| Wheeler et al (2012) 50 | West | 39 | Diabetes mellitus | Yes | Hispanic/Latino |
| Yeh et al (2016) 51 | Northeast | 60 | Prediabetes | Yes | Asian/Pacific Islander |
Discussion
The findings from this scoping review point to the unaddressed need for culturally tailored nutritional interventions, particularly within medical education. Although half of the studies included in this review were culturally tailored, only one was specific to interventions applied to medical students specifically in the Southwestern United States. Medical education interventions appeared to focus on addressing general nutrition and weight management that would benefit obese individuals, as opposed to exclusively addressing nutritional modifications for prediabetes/DM or hypertension/cardiovascular diseases. Half of the medical education interventions were conducted in the Northeastern United States.
According to the studies reviewed, there appears to be a lack of inclusion of culturally relevant topics in nutritional interventions published within medical education. Incorporating more culturally centered nutritional and dietary education in medical curricula can provide a stronger foundation for future physicians in counseling patients in chronic disease management. One potential benefit of cultural inclusion in nutritional counseling is the higher rates of adherence to dietary changes and improvements in disease management. Interventions within medical education also appeared to emphasize the use of certain diets, such as the DASH or Mediterranean diets, within various cultural groups. However, none of the studies reviewed within medical education to the best of our knowledge have explored cultural adaptations of these specific diet interventions. Study findings from our qualitative analysis additionally indicate that medical education primarily focuses on general diet assessment and methods of healthy nutritional counseling, while less emphasis is placed on cultural contribution to meals. Interventions in medical education often included discussions on the importance of exercise and ways to decrease fat and carbohydrate intake. With the exception of one study that taught healthy preparation of cultural meals originating from Nigeria, China, Central America, and the Southern United States, there was no other discussion on culturally tailored approaches to nutritional education.
The findings from this scoping review additionally suggest that studies in clinical and communal settings appeared to more frequently incorporate culturally tailored concepts into the design and implementation of their nutritional interventions. A majority of these studies were conducted in the Northeast, Southeast, and West regions of the country, among Hispanic/Latino populations. These studies primarily focused on prediabetes/DM.
These findings indicate that there was not an even representation of ethnic groups included in the studies. Hispanics/Latinos and African Americans comprised the largest focus as they were included in 75% of the studies. The remaining 25% of the studies focused on Native Americans and Asian Americans. While it may not be surprising that Hispanics/Latinos and African Americans are the most studied since they are the largest ethnic minorities, there remains a disproportionate focus on Hispanics/Latinos when compared with African Americans. Studies focused on Hispanics/Latinos were published twice as much as those focused on African Americans despite this latter having the highest prevalence of chronic diseases out of all the ethnic groups.4,52,53 As indicated in literature, barriers such as mistrust of the health care system and inequitable policies have historically led to low rates of inclusion of African Americans in medical research. 54
Additional qualitative analysis findings also point to the lack of focus on specific at-risk subgroups such as Southeast Asians and Native Americans. Literature generally indicates that Asian Americans are more likely than their white counterpart to have ideal cardiovascular health at a healthy body mass index. 55 Yet it has also been shown that this aggregate data can mask the higher rates of cardiovascular disease associated with Filipinos and Asian Indians.8,9,55 Likewise, this lack of focus has been evident as well with the lack of nutritional interventions specifically directed toward Southeast Asians. As one of the most at-risk subgroups of Asians, Southeast Asians may have significant benefits from focused nutritional interventions. Allowing them to improve their nutritional intake can confer improved cardiovascular health and a lower chronic disease burden. Native Americans as well can benefit from focused nutritional interventions. The unique risk profile of Native Americans including the increasing rates of diabetes 56 indicates that focused interventions may benefit them. Empowering Native Americans to incorporate an element of their culture into their health, via nutritional intake, may alleviate some of the difficulties currently seen from inadequate healthcare delivery and a low representation in healthcare.
Limitations
There are a few notable limitations of this scoping review. First, our review was limited to 5 large search engines/databases. Although we aimed to capture as many relevant published studies as possible, articles in other databases may have not been identified. Additionally, the methodological approach employed in this scoping review did not include works published in gray literature from conferences or scientific meetings. The rationale for not including these works stemmed from some of these works not having undergone the peer-review process, preliminary findings presented, and/or the limited discussions of methods and results that these works may have available. Second, this scoping review focused on studies conducted within the United States which excluded international studies that may have used culturally tailored nutritional interventions either within medical education or clinical and communal settings. We decided to restrict our review to studies within the United States in order to minimize the contrast between countries in terms of structures of medical education as well as demographic differences by geography. Last, our review is temporally limited to approximately 2 decades worth of literature where studies published prior to January 1, 2000, and after November 30, 2019, may have been excluded. To the best of our knowledge, no recent related literature has been published.
Conclusion
Collectively, these findings point to an existent gap and need for inclusive studies within this area of research. The lack of culturally relevant topics in culinary medicine curricula appears to be scant in comparison to clinical nutrition research which does consider dietary differences by cultural groups when addressing holistic chronic disease management. This study also points to the need for further research into how culinary medicine curricula is preparing clinicians to effectively address and impact dietary differences within their heterogeneous patient populations. Review of literature within medical education suggest an area of improvement through the incorporation of culturally relevant topics into the designs and assessments of these interventions. Review of literature within clinical and communal studies highlight the potential value to further stratifying heterogeneous subgroups as there are substantive differences in the prevalence of chronic diseases that are often masked when aggregating them into a larger racial cohorts such as “Hispanics/Latinos” and “Asian Americans.”8,57,58
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: Not applicable, because this article does not contain any studies with human or animal subjects.
Informed Consent: Not applicable, because this article does not contain any studies with human or animal subjects.
Trial Registration: Not applicable, because this article does not contain any clinical trials.
ORCID iDs: Seiichi Villalona  https://orcid.org/0000-0003-2442-576X
https://orcid.org/0000-0003-2442-576X
Wilfrido J. Castillo  https://orcid.org/0000-0001-8527-0015
https://orcid.org/0000-0001-8527-0015
References
- 1.Centers for Disease Control and Prevention. Chronic diseases in America. Published 2019. Accessed April 12, 2020. https://www.cdc.gov/chronicdisease/resources/infographic/chronic-diseases.htm
- 2.Tinker A. How to improve patient outcomes for chronic diseases and comorbidities. Published 2017. Accessed March 16, 2021. https://www.healthcatalyst.com/wp-content/uploads/2014/04/How-to-Improve-Patient-Outcomes.pdf
- 3.Raghupathi W, Raghupathi V. An empirical study of chronic diseases in the United States: a visual analytics approach. Int J Environ Res Public Health. 2018;15:431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Quiñones AR, Botoseneanu A, Markwardt S, et al. Racial/ethnic differences in multimorbidity development and chronic disease accumulation for middle-aged adults. PLoS One. 2019;14:e0218462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Indian Health Service. Indian health disparities. Published 2019. Accessed April 15, 2020. https://www.ihs.gov/sites/newsroom/themes/responsive2017/display_objects/documents/factsheets/Disparities.pdf
- 6.Marcinko T. More native American doctors needed to reduce health disparities in their communities. Published November 13, 2016. Accessed April 15, 2020. https://www.aamc.org/news-insights/more-native-american-doctors-needed-reduce-health-disparities-their-communities
- 7.Robeznieks A. Native Americans work to grow their own physician workforce. Published August 22, 2019. Accessed April 15, 2020. https://www.ama-assn.org/practice-management/physician-diversity/native-americans-work-grow-their-own-physician-workforce
- 8.Gordon NP, Lin TY, Rau J, Lo JC. Aggregation of Asian-American subgroups masks meaningful differences in health and health risks among Asian ethnicities: an electronic health record based cohort study. BMC Public Health. 2019;19:1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.American Heart Association News. South Asians’ high risk of cardiovascular disease has been hidden by a lack of data. Published May 24, 2018. Accessed April 15, 2020. https://www.heart.org/en/news/2018/05/29/south-asians-high-risk-of-cardiovascular-disease-has-been-hidden-by-a-lack-of-data
- 10.Levine BS, Wigren MM, Chapman DS, Kerner JF, Bergman RL, Rivlin RS. A national survey of attitudes and practices of primary-care physicians relating to nutrition: strategies for enhancing the use of clinical nutrition in medical practice. Am J Clin Nutr. 1993;57:115-119. [DOI] [PubMed] [Google Scholar]
- 11.Aggarwal M, Devries S, Freeman AM, et al. The deficit of nutrition education of physicians. Am J Med. 2018;131:339-345. [DOI] [PubMed] [Google Scholar]
- 12.Crowley J, Ball L, Hiddink GJ. Nutrition in medical education: a systematic review. Lancet Planet Health. 2019;3:e379-e389. [DOI] [PubMed] [Google Scholar]
- 13.Puma JL. What is culinary medicine and what does it do? Popul Health Manag. 2016;19:1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lindell KC, Adams KM, Kohlmeier M, Zeisel SH. The evolution of Nutrition in Medicine, a computer-assisted nutrition curriculum. Am J Clin Nutr. 2006;83:956S-962S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Osterweil N. Physicians and chefs cook up healthy med school curriculum. Medscape. Published July 17, 2014. Accessed April 12, 2020. https://www.medscape.com/viewarticle/828443
- 16.Satia JA. Diet-related disparities: understanding the problem and accelerating solutions. J Am Diet Assoc. 2009;109:610-615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19-32. [Google Scholar]
- 18.Peters MDJ, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13:141-146. [DOI] [PubMed] [Google Scholar]
- 19.Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Birkhead AG, Foote S, Monlezun DJ, et al. Medical student-led community cooking classes: a novel preventive medicine model that’s easy to swallow. Am J Prev Med. 2014;46(3):e41-42. doi: 10.1016/j.amepre.2013.11.006 [DOI] [PubMed] [Google Scholar]
- 21.Conroy MB, Delichatsios HK, Hafler JP, Rigotti NA. Impact of a preventive medicine and nutrition curriculum for medical students. Am J Prev Med. 2004;27(1):77-80. doi: 10.1016/j.amepre.2004.03.009 [DOI] [PubMed] [Google Scholar]
- 22.Dreibelbis TD, George DR An Intergenerational Teaching Kitchen: Reimagining a Senior Center as a Shared Site for Medical Students and Elders Enrolled in a Culinary Medicine Course. J Intergener Relatsh. 2017;15(2):174-180. doi: 10.1080/15350770.2017.1294438 [DOI] [Google Scholar]
- 23.Fang V, Gillespie C, Crowe R, Popeo D, Jay M. Associations between medical students’ beliefs about obesity and clinical counseling proficiency. BMC Obes. 2019; 6:5. doi: 10.1186/s40608-018-0222-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Geller AC, Ockene JK, Kulkarni M, et al. Students’ report of preceptor weight management counseling at eight U.S. medical schools. Am J Prev Med. 2018;55(5):e139-e145. doi: 10.1016/j.amepre.2018.06.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jacob M, Stewart P, Medina-Walpole A, Fong CT. A culinary laboratory for nutrition education. Clin Teach. 2016;13(3):197-201. doi: 10.1111/tct.12403 [DOI] [PubMed] [Google Scholar]
- 26.Jaroudi SS, Sessions WS, Wang VS, et al. Impact of culinary medicine elective on medical students’ culinary knowledge and skills. In: Baylor University Medical Center Proceedings, October vol. 31(4), Taylor & Francis, 2018:439-442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Krok-Schoen JL, Shim R, Nagel R, et al. Outcomes of a health coaching intervention delivered by medical students for older adults with uncontrolled type 2 diabetes. Gerontol Geriatr Educ. 2017;38(3):257-270. doi: 10.1080/02701960.2015.1018514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Monlezun DJ, Leong B, Joo E, Birkhead AG, Sarris L, Harlan TS. Novel longitudinal and propensity score matched analysis of hands-on cooking and nutrition education versus traditional clinical education among 627 medical students. Adv Prev Med. 2015. doi: 10.1155/2015/656780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pang B, Memel Z, Diamant C, Clarke E, Chou S, Gregory H. Culinary medicine and community partnership: hands-on culinary skills training to empower medical students to provide patient-centered nutrition education. Med Educ Online. 2019;24(1). doi: 10.1080/10872981.2019.1630238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schlair S, Hanley K, Gillespie C, et al. How medical students’ behaviors and attitudes affect the impact of a brief curriculum on nutrition counseling. J Nutr Educ Behav. 2012;44(6):653-657. doi: 10.1016/j.jneb.2011.08.006 [DOI] [PubMed] [Google Scholar]
- 31.Wilechansky R, Burgermaster M, Jones D, Seres D. Obesity, diet, and exercise education for the primary care clerkship using an articulate storyline 2 e-learning module. MedEdPORTAL. 2016;12. doi: 10.15766/mep_2374-8265.10497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Amaro H, Cortes DE, Garcia S, Duan L, Black DS. Video-based grocery shopping intervention effect on purchasing behaviors among latina shoppers. Am J Public Health. 2017;107(5):800-806. doi: 10.2105/ajph.2017.303725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brown SA, Garcia AA, Kouzekanani K, Hanis CL. Culturally competent diabetes self-management education for Mexican Americans: the starr county border health initiative. Diabetes Care. 2002;25(2):259-268. doi: 10.2337/diacare.25.2.259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Coffman MJ, Ferguson BL, Steinman L, Talbot LA, Dunbar-Jacob J. A health education pilot for Latina women with diabetes. Clin Nurs Res. 2013;22(1):70-81. doi: 10.1177/1054773812451746 [DOI] [PubMed] [Google Scholar]
- 35.Cooper KC, King MA, Sarpong DF. Tipping the scales on obesity: church-based health promotion for African American women. J Christ Nurs. 2015;32(1):41-45. [PubMed] [Google Scholar]
- 36.Galasso P, Amend A, Melkus GD, Nelson GT. Barriers to medical nutrition therapy in black women with type 2 diabetes mellitus. Diabetes Educ. 2005;31(5):719-725. doi: 10.1177/0145721705280941 [DOI] [PubMed] [Google Scholar]
- 37.Gibbs HD, Camargo J, Owens S, Gajewski B, Cupertino AP. Measuring nutrition literacy in Spanish-speaking latinos: an exploratory validation study. J Immigr Minor Health. 2018;20(6):1508-1515. doi: 10.1007/s10903-017-0678-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ho EY, Acquah J, Chao C, et al. Heart healthy integrative nutritional counseling (H2INC): creating a Chinese medicine + western medicine patient education curriculum for Chinese Americans. Patient Educ Couns. 2018;101(12):2202-2208. doi: 10.1016/j.pec.2018.08.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kattelmann KK, Conti K, Ren C. The medicine wheel nutrition intervention: a diabetes education study with the cheyenne river sioux tribe. J Am Diet Assoc. 2009; 109(9):1532-1539. doi: 10.1016/j.jada.2009.06.362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Metghalchi S, Rivera M, Beeson L, et al. Improved clinical outcomes using a culturally sensitive diabetes education program in a Hispanic population. Diabetes Educ. 2008;34(4):698-706. doi: 10.1177/0145721708320913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Miller ST, Oates VJ, Brooks MA, Shintani A, Gebretsadik T, Jenkins DM. Preliminary efficacy of group medical nutrition therapy and motivational interviewing among obese African American women with type 2 diabetes: a pilot study. J Obes. 2014. doi: 10.1155/2014/345941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Monlezun DJ, Leong B, Joo E, Birkhead AG, Sarris L, Harlan TS. Novel longitudinal and propensity score matched analysis of hands-on cooking and nutrition education versus traditional clinical education among 627 medical students. Adv Prev Med. 2015. doi: 10.1155/2015/656780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Perez-Escamilla R, Damio G, Chhabra J, et al. Impact of a community health workers-led structured program on blood glucose control among latinos with type 2 diabetes: the DIALBEST trial. Diabetes Care. 2015;38(2):197-205. doi: 10.2337/dc14-0327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rankins J, Sampson W, Brown B, Jenkins-Salley T. Dietary Approaches to Stop Hypertension (DASH) intervention reduces blood pressure among hypertensive African American patients in a neighborhood health care center. J Nutr Educ Behav. 2005;37(5):259-264. doi: 10.1016/s1499-4046(06)60281-9 [DOI] [PubMed] [Google Scholar]
- 45.Salto LM, Cordero-MacIntyre Z, Beeson L, Schulz E, Firek A, De Leon M. En Balance participants decrease dietary fat and cholesterol intake as part of a culturally sensitive Hispanic diabetes education program. Diabetes Educ. 2011;37(2):239-253. doi: 10.1177/0145721710394874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Seol H, Thompson M, Kreider KE, Vorderstrasse A. Diabetes self-management quality improvement initiative for medically underserved patients. J Nurs Care Qual. 2017;32(3):272-279. doi: 10.1097/ncq.0000000000000243 [DOI] [PubMed] [Google Scholar]
- 47.Song HJ, Han HR, Lee JE, et al. Translating current dietary guidelines into a culturally tailored nutrition education program for Korean American immigrants with type 2 diabetes. Diabetes Educ. 2010;36(5):752-761. doi: 10.1177/0145721710376328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ursua RA, Aguilar DE, Wyatt LC, et al. A community health worker intervention to improve management of hypertension among Filipino Americans in New York and New Jersey: a pilot study. Ethn Dis. 2014;24(1):67-76. [PMC free article] [PubMed] [Google Scholar]
- 49.Weinstein E, Galindo RJ, Fried M, Rucker L, Davis NJ. Impact of a focused nutrition educational intervention coupled with improved access to fresh produce on purchasing behavior and consumption of fruits and vegetables in overweight patients with diabetes mellitus. Diabetes Educ. 2014;40(1):100-106. doi: 10.1177/0145721713508823 [DOI] [PubMed] [Google Scholar]
- 50.Wheeler G, Montgomery SB, Beeson L, et al. En balance: the effects of Spanish diabetes education on physical activity changes and diabetes control. Diabetes Educ. 2012;38(5):723-732. doi: 10.1177/0145721712457249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yeh MC, Heo M, Suchday S, et al. Translation of the diabetes prevention program for diabetes risk reduction in Chinese immigrants in New York City. Diabet Med. 2016;33(4):547-551. doi: 10.1111/dme.12848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Price JH, Khubchandani J, McKinney M, Braun R. Racial/ethnic disparities in chronic diseases of youths and access to health care in the United States. Biomed Res Int. 2013;2013:787616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Centers for Disease Control and Prevention. Adult obesity facts. Published 2020. Accessed April 12, 2020. https://www.cdc.gov/obesity/data/adult.html
- 54.Konkel L. Racial and ethnic disparities in research studies: the challenge of creating more diverse cohorts. Environ Health Perspect. 2015;123:A297-A302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.American Heart Association News. Adjusting BMI eliminates lead Asian Americans hold in heart health. Published June 26, 2019. Accessed April 15, 2020. https://www.heart.org/en/news/2019/06/26/adjusting-bmi-eliminates-lead-asian-americans-hold-in-heart-health
- 56.Burrows NR, Geiss LS, Engelgau MM, Acton KJ. Prevalence of diabetes among Native Americans and Alaska Natives, 1990-1997: an increasing burden. Diabetes Care. 2000;23:1786-1790. [DOI] [PubMed] [Google Scholar]
- 57.Kim D, Li AA, Perumpail RB, et al. Disparate trends in mortality of etiology-specific chronic liver diseases among Hispanic subpopulations. Clin Gastroenterol Hepatol. 2019;17:1607-1615.e1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Martinez-Tyson D, Pathak EB, Soler-Vila H, Flores AM. Looking under the Hispanic umbrella: cancer mortality among Cubans, Mexicans, Puerto Ricans and other Hispanics in Florida. J Immigr Minor Health. 2009;11:249-257. [DOI] [PMC free article] [PubMed] [Google Scholar]