Description
A girl of middle childhood age had a 1-year history of generalised muscle weakness, low-grade fevers, difficulty in climbing stairs and rising from squatting or lying position and multiple painful swellings mainly over the lower abdomen, buttocks and thighs. On examination, there was evidence of proximal muscle weakness with a positive Gower’s sign. There were no active Gottron’s papules or heliotrope rashes, but a history of truncal rashes early in the course of the disease was reported. The Childhood Myositis Assessment Score was 17/52. Investigations revealed normal blood counts, high erythrocyte sedimentation rate and C reactive protein, normal serum calcium, phosphorus, parathyroid hormone and thyroid function tests, raised creatine phosphokinase and lactic dehydrogenase levels, normal C3–C4 levels, and negative antinuclear antibody and anti-double-stranded DNA. Her myositis profile was positive for NXP2 antibodies. Plain radiographs of the abdomen (figure 1), pelvis and thighs (figure 2) showed multiple linear and stippled calcifications in the subcutaneous tissue, more marked in the lower abdomen and pelvis area. MRI revealed ill-defined high signal in short tau inversion recovery sequences suggestive of muscle oedema in bilateral thigh regions and low-signal foci suggestive of calcifications (figure 3). She was diagnosed with juvenile dermatomyositis (JDM) with calcinosis cutis and started on steroids, methotrexate and monthly disodium pamidronate infusions. She also received 6-month cycles of cyclophosphamide. The patient’s muscle strength improved gradually with medical treatment and physiotherapy. Repeat X-rays of the pelvis and lower limbs after 2 years revealed resolution of calcinosis to a large extent with some remnants in the pelvis and thighs (figure 4) and the presence of metaphyseal zebra lines in both femur and tibia (figure 5). The gap between the lines coincides with the lockdown period during the COVID-19 pandemic when the patient could not attend the hospital for pamidronate infusions.
Figure 1.

X-ray of the lower abdomen and pelvis showing extensive calcinosis.
Figure 2.

X-ray of the pelvis and thighs showing extensive calcinosis.
Figure 3.
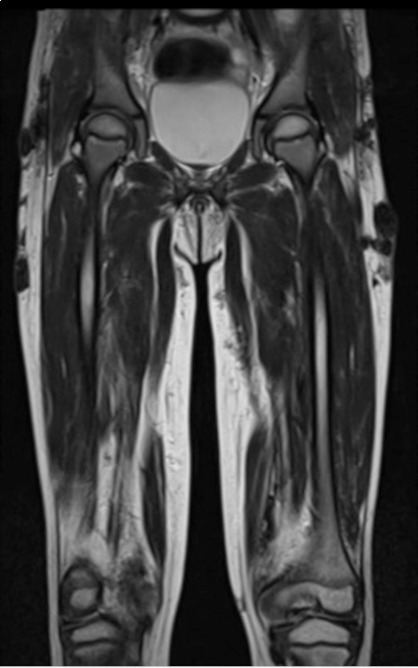
MRI of the thighs showing muscle oedema and calcification.
Figure 4.

X-ray of the pelvis and lower abdomen after treatment shows resolution of calcinosis.
Figure 5.

X-ray of the lower limbs after treatment showing remnant calcinosis and zebra lines (arrows pointing to zebra lines).
JDM is a rare autoimmune disease of childhood with typical skin and muscle involvement. The characteristic features of the disease include symmetrical weakness of proximal muscles, raised muscle enzymes and cutaneous manifestations such as Gottron’s papules, heliotrope rash and shawl sign. About 40% of children with JDM have calcinosis.1 The presence of calcinosis is associated with chronic disease, younger age at disease onset and longer disease duration prior to starting treatment.2 Multiple treatment options have been tried in the treatment of calcinosis but none have been uniformly effective. Apart from systemic immunomodulation including steroids, methotrexate, cyclophosphamide or biologics, alternative therapies including bisphosphonates like disodium pamidronate or intravenous immunoglobulin are the most commonly used medications for treatment of calcinosis.3 Other agents that have been used for treatment of calcinosis are calcium channel blockers intravenously or topical thiosulfate and aluminium hydroxide.
Zebra lines are metaphyseal bands that occur in long bones of young children receiving regular disodium pamidronate therapy. These sclerotic lines represent horizontal trabeculae undergoing turnover, and their occurrence depends on the age of the patients, the dosing interval of bisphosphonate therapy and growth rate of the bone.4 Zebra lines have been described in children with osteogenesis imperfecta on regular bisphosphonate therapy but not in children with JDM receiving this treatment for calcinosis.
Learning points.
Calcinosis cutis may be seen in delayed presentation and treatment of children with juvenile dermatomyositis.
Systemic immunomodulation, along with alternative therapy such as bisphosphonates, is useful in the treatment of calcinosis.
Zebra lines may be seen in long bones of children undergoing pamidronate therapy.
Footnotes
Contributors: MJ diagnosed and managed the patient, conceived and designed the clinical picture. MJ and MM prepared the manuscript. AM interpreted radiology images. All authors revised the final draft and approved it for submission.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Case reports provide a valuable learning resource for the scientific community and can indicate areas of interest for future research. They should not be used in isolation to guide treatment choices or public health policy.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Obtained.
References
- 1.Hoeltzel MF, Oberle EJ, Robinson AB, et al. The presentation, assessment, pathogenesis, and treatment of calcinosis in juvenile dermatomyositis. Curr Rheumatol Rep 2014;16:467. 10.1007/s11926-014-0467-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Twilt M, Feldman BM. An update on the diagnosis and management of juvenile dermatomyositis. Int J Clin Rheumtol 2012;7:325–33. 10.2217/ijr.12.23 [DOI] [Google Scholar]
- 3.Orandi AB, Baszis KW, Dharnidharka VR, et al. Assessment, classification and treatment of calcinosis as a complication of juvenile dermatomyositis: a survey of pediatric rheumatologists by the childhood arthritis and rheumatology research alliance (CARRA). Pediatr Rheumatol 2017;15:71. 10.1186/s12969-017-0199-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al Muderis M, Azzopardi T, Cundy P. Zebra lines of pamidronate therapy in children. J Bone Joint Surg Am 2007;89:1511–6. 10.2106/00004623-200707000-00015 [DOI] [PubMed] [Google Scholar]


