Abstract
Objectives
To establish the evidence base for the effects on health outcomes and costs of social prescribing link workers (non-health or social care professionals who connect people to community resources) for people in community settings focusing on people experiencing multimorbidity and social deprivation.
Design
Systematic review and narrative synthesis using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach.
Data sources
Cochrane Database, Cochrane Central Register of Controlled Trials, ClinicalTrials.gov, EU Clinical Trials Register, CINAHL, Embase, Global Health, PubMed/MEDLINE, PsycInfo, LILACS, Web of Science and grey literature were searched up to 31 July 2021. A forward citation search was completed on 9 June 2022.
Eligibility criteria
Controlled trials meeting the Cochrane Effectiveness of Practice and Organisation of Care (EPOC) guidance on eligible study designs assessing the effect of social prescribing link workers for adults in community settings on any outcomes. No language restrictions were applied.
Data extraction and synthesis
Two independent reviewers extracted data, evaluated study quality using the Cochrane EPOC risk of bias tool and judged certainty of the evidence. Results were synthesised narratively.
Results
Eight studies (n=6500 participants), with five randomised controlled trials at low risk of bias and three controlled before–after studies at high risk of bias, were included. Four included participants experiencing multimorbidity and social deprivation. Four (n=2186) reported no impact on health-related quality of life (HRQoL). Four (n=1924) reported mental health outcomes with three reporting no impact. Two US studies found improved ratings of high-quality care and reduced hospitalisations for people with multimorbidity experiencing deprivation. No cost-effectiveness analyses were identified. The certainty of the evidence was low or very low.
Conclusions
There is an absence of evidence for social prescribing link workers. Policymakers should note this and support evaluation of current programmes before mainstreaming.
PROSPERO registration number
CRD42019134737.
Keywords: social medicine, primary care, health policy
Strengths and limitations of this study.
This systematic review only included randomised trials and controlled before–after studies that met the Cochrane Effectiveness of Practice and Organisation of Care guidance, to avoid potentially biased results from poorer-quality studies.
Our literature search involved an in-depth search for social prescribing link worker interventions, using a wide range of search terms and with no language, country or date limitations.
The area of social prescribing is a rapidly evolving field, and we conducted a forward citation search of included papers to capture any relevant studies published after our search.
Our broad search resulted in a large number of studies and an initial screen of clearly ineligible studies was conducted by one author only, which may have introduced bias.
The limited number of studies and heterogeneity in study design and intervention meant a meta-analysis was not possible and thus a robust narrative synthesis including an assessment of the certainty of the evidence was conducted.
Introduction
Social prescribing is a way of linking people with complex needs to non-medical supports in the community. There are different models of social prescribing, ranging from online signposting services to individual support from a link worker to access community resource. The link worker model of social prescribing is most frequently used in the UK.1 Link workers are non-health or social care professionals, usually based in primary care or community organisations, who determine the health and well-being needs of people referred to them (usually by healthcare professionals), co-produce a health and well-being plan, and provide support to connect with community resources to meet these needs. No qualifications are specified for link workers, rather there is a focus on relevant experience and skills, such as listening and empathising, to perform the role.2 Many health systems are developing social prescribing initiatives and NHS England is funding link workers in primary care and recommends their use for people who have one or more chronic conditions, need support with their mental health, are isolated or who have complex social problems.3
People experiencing multimorbidity (defined as two or more chronic health conditions) experience fragmented care, poorer health outcomes and more psychological stress, and as multimorbidity becomes the norm among an ageing population, it poses a significant challenge to health systems.4 People with complex multimorbidity account for a higher proportion of hospital admissions and therefore costs, and have higher consultation rates than those without.5 In socially deprived areas, the impact is greater as people experience earlier onset of multimorbidity and are more likely to have mental health comorbidities.6 A 2021 systematic review of interventions targeting people with multimorbidity in primary care identified 16 randomised controlled trials (RCTs) but found limited evidence for interventions that improve outcomes including health-related quality of life (HRQoL) and mental health outcomes.7 The review did not identify any eligible social prescribing link worker interventions but concluded that existing evidence suggests that future research should target a range of areas including patient health behaviours that can be addressed though social prescribing.
Social prescribing link workers may have an impact on health outcomes for people experiencing multimorbidity, particularly in areas of social deprivation, but despite their widespread roll out in the UK, there is limited evidence for their effectiveness.8 If effective, social prescribing link workers should reduce healthcare costs, by addressing the social problems that reportedly drive 20% of primary care attendances and the social determinants of health that lead to poorer outcomes.9 A recent systematic review, however, concluded that there was a lack of evidence for how, for whom and when social prescribing was effective or how much it cost.10 Previous reviews have only looked at UK-based interventions and included a broad range of studies including those with uncontrolled designs.11 12 Social prescribing is, however, gaining momentum internationally, and while interventions are adapted to the local context, there are similarities and potential to learn from experiences in other countries.13 We aimed to systematically review the evidence of effectiveness and costs of social prescribing link worker interventions internationally and to establish the evidence, if any, for their effectiveness in people with multimorbidity and social deprivation.
Methods
We conducted a systematic review of studies reporting effectiveness and/or costs of social prescribing link workers based in primary or community care settings for community-dwelling adults. We included randomised trials and non-randomised trials that met the Cochrane EPOC guidance on eligible study designs.14 We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement for reporting systematic reviews15 (online supplemental appendix 1 16), registered our review on Prospero CRD42019134737 (04/07/2019) and published the protocol.17
bmjopen-2022-062951supp001.pdf (54.7KB, pdf)
Eligibility criteria
Participants/population
We included studies on community-dwelling adults attending primary care. Participants did not need to have any specific index condition. We included all studies whether they focused on participants in areas of social deprivation or not, but we specifically extracted data on social deprivation and multimorbidity where they were reported. We excluded studies on children and those in residential or supported care.
Intervention
Social prescribing link workers may be known by other terms such as community health workers, patient navigators or health facilitators. While all of these work in the area of health, they are generally considered ‘lay workers’ as they have not completed formal professional health or social care qualifications. Similarly, the process of social prescribing may be known by other terms such as ‘community referral’ or ‘navigation’. Inclusion was based on the function of the role, that is, supporting people to improve their health and well-being through connecting them with community resources and health and social care coordination, recognising that there is a wide range of terms used to describe such roles.18
We included interventions that involved:
A referral (including self-referrals) to a link worker (a non-health or social care professional) who was based either in a primary care practice or a community or voluntary organisation.
Participants meeting with a link worker face-to-face at least once, although additional contacts could be via telephone or other remote methods.
Determining an individual range of health and social care supports and community resources that the person would be willing to engage with and being offered support and follow-up to engage with their chosen supports and activities.
We excluded interventions without a link worker that only involved signposting to services, used volunteers as link workers or were delivered by telephone. Interventions where additional support was being provided by healthcare professionals or personal care provided alongside health and social care coordination such as disability support workers were excluded as it was not possible to separate the effects of the different components of care. We excluded multifaceted interventions, which mainly comprised of education and goal-setting around disease control or health behaviour change interventions, even if they had an element of social prescribing as it was not possible to separate the impact of the different components of the intervention.
Comparator(s)
We only included studies with a comparator group that did not involve any social prescribing and met the EPOC guidance on controlled before–after (CBA) studies, that is, contemporaneous data collection, controls drawn from similar sites and at least two intervention and two control sites.14
Setting
Primary care was generally defined as “care provided by clinicians that are available to treat all common conditions in all age groups and have an ongoing relationship with their patients”.19 This definition allowed for a more flexible interpretation in countries that have different models of healthcare. We excluded studies that focused on hospital inpatients or specialist services or were emergency department (ED)-based. The definition of social deprivation is debated. It varies from country to country and is usually based on relative socioeconomic capacity.20 For this review, we did not have a definition of deprivation, rather we described how deprivation was defined in relevant studies.
Outcomes
Main outcome
We included all reported outcomes, but based on our interest in assessing link workers to support patient with multimorbidity, we focused on outcomes in the core outcome set for multimorbidity that recommends primary outcomes of quality of life, mental health and mortality for interventions focused on multimorbidity.21
The primary outcomes for the review were:
Health-related quality of life (HRQoL), as measured by a validated instrument.
Mental health outcomes, as measured by a validated instrument for screening for mental health conditions.
Additional outcomes
Secondary outcomes included also focused on the core outcome set for multimorbidity.21 While this is a wide range of outcomes it is in keeping with the Medical Research Council (MRC) frameworks’ guide on using multiple outcome measures for complex interventions.22 These included:
Patient-reported outcomes on social-connectedness or isolation, self-rated health, patient experience of care, treatment burden, self-management behaviour and self-efficacy.
Physical activity and function included measures of physical activity (self-reported or objectively measured), physical function, activities of daily living.
Health service utilisation defined as number of general practitionor (GP) visits, ED attendances or hospital admissions as measured via primary care or hospital records or self-reported.
Any physical health data reported was included.
Any cost data or social return on investment data.
Search strategy
We searched 11 bibliographic and trials databases for RCTs and non-RCTs that meet the criteria outlined in the Cochrane Effective Practice and Organisation of Care (EPOC) guidance on study design14 from inception up to July 2021 with no language limits: Cochrane Database, Cochrane Central Register of Controlled Trials, ClinicalTrials.gov, EU Clinical Trials Register, Cumulative Index of Nursing and Allied Health Literature (CINAHL), Embase, Global Health, PubMed/MEDLINE, PsycInfo, LILACS (Latin American and Caribbean Health Sciences Information database) and Web of Science. To identify economic evaluations that may be of relevance we also searched the National Health Service Economic Evaluation Database (NHS EED), Health Technology Assessment Database (both available via the Centre for Reviews and Dissemination (CRD), University of York) and CEA (Cost-Effectiveness Analysis Registry) up to July 2019. The search strategy focused on the use of a range of key words associated with the intervention and was developed with input from a senior information specialist.
We conducted a grey literature search of the following databases: Irish Health Service Executive (HSE) Lenus, RIAN, Open Grey, DART EUROPE, Google and Google Scholar and World Health Organization Library Information System (WHOLIS) up to July 2021. We also conducted a forward and backward citation search of included studies. Relevant websites (The Kings Fund, NHS Social Prescribing, National Institute for Clinical Excellence, Social Prescribing Network, Health Foundation, Nuffield Trust, HSE Social Prescribing, and Oxford Social Prescribing Research Network) were searched manually for evaluations. The first 23 pages of a Google Search for ‘social prescribing’ and the first 21 pages of a Google scholar search were reviewed for additional literature. See supplementary data online supplemental appendix 2 for detailed search strategy.16
bmjopen-2022-062951supp002.pdf (191.3KB, pdf)
Data management
Rayyan was used to sort abstracts for inclusion and exclusion. References were managed with EndNote 8 reference manager. Excel was used to manage extracted data.
Review process
Duplicates were removed using the EndNote function, which identifies potential duplicates, which were then checked and manually reviewed by the lead author (BK). The lead author (BK) then did an initial screen to remove clearly ineligible titles. This step was necessary due to the large number of potentially eligible reports returned by our search strategy. Where it was clear from the title that our eligibility criteria on population, intervention or methods were not met the title was excluded. For example, a title clearly reporting a qualitative study of a healthcare intervention delivered by lay people to children, such as a qualitative study of a community health worker intervention for childhood diarrhoea, would have been excluded. Any report where it was not clear from the title if eligibility criteria were met was reviewed by abstract by BK and AC, who independently reviewed the abstracts of all potentially eligible titles, discarded those that clearly did not meet inclusion criteria and independently reviewed the full texts of the remainder to assess eligibility for final inclusion. Any discrepancies were resolved through discussion with a third reviewer (SMS). Data extraction was completed by the lead author and checked by another author (MOS). Two authors (BK and AC) independently assessed and cross-checked the risk of bias in all included studies using the Cochrane EPOC Guidance for assessing risk of bias.23 The certainty of the evidence for outcomes was independently assessed by two authors (BK and MOS) using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) criteria including risk of bias, consistency of effect, imprecision, indirectness and other potential criteria such as publication bias.24 Any discrepancies were discussed with the senior author (SMS) until consensus was reached. RCTs and CBAs were assessed separately. Overall certainty was based on assessment of evidence from RCTs where more than one was available.
Strategy for data synthesis
Due to the heterogeneity in terms of study design, risk of bias, participants, interventions and outcomes, a narrative synthesis was performed and presented in tabular form to include the following headings: study design, setting, participants, nature of intervention, outcome measures used, effects and costs. We explored the possibility of completing a meta-analysis; however, in the two studies that were similar in terms of study design, intervention characteristics and duration of follow-up, there were insufficient data reported on the primary outcomes. As there were only two studies, authors were not contacted for additional data. We had planned to complete subgroup analyses based on multimorbidity, living in areas of social deprivation and link worker location, but this was not possible due to substantial methodological heterogeneity, including study design and definitions and reporting of multimorbidity and deprivation.
Patient and public involvement
This review is part of one of four PhD projects under a Health Research Board Collaborative Doctoral Award (CDA) in multimorbidity. The original CDA project application and PhD topics had input from a patient and public involvement (PPI) advisory group. A multimorbidity PPI advisory group was set up specifically to support the four PhD projects in the CDA. The lead reviewer (BK) presented the results of this review to the group who provided input on implications for policy, practice and research, included in the discussion. See online supplemental appendix 3 Guidance on Reporting Involvement of Public and Patients (GRIPP) 2 Form in supplementary data for further details on PPI methods.16
bmjopen-2022-062951supp003.pdf (123.8KB, pdf)
Results
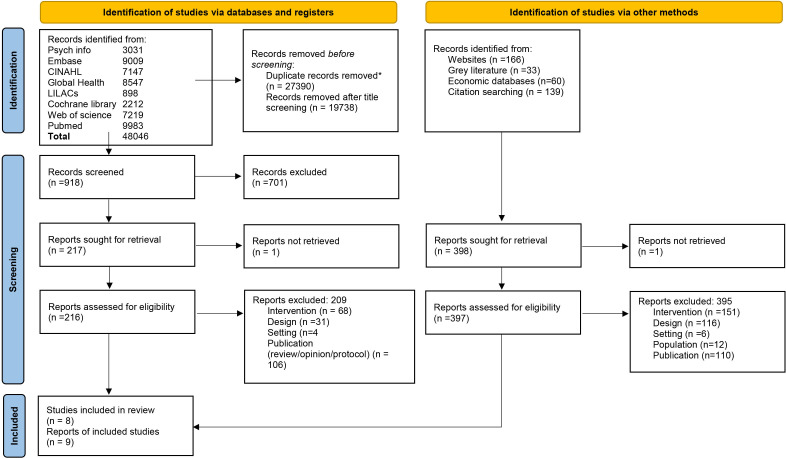
The database search identified 20 656 records after duplicate removal; 19 738 were removed after title screening leaving 918 abstracts for review. A total of 553 full texts were assessed for eligibility including 216 identified from the database search and 397 from other sources. Seven reports of six studies were identified from the database search, one from backward citation searches and one from forward citation searches. Our forward citation search did not identify any corrections or errata related to the included studies (see figure 1: PRISMA flow diagram).
Figure 1.
PRISMA flow diagram. *Duplicates were removed using EndNote Find Duplicate function.
Included studies and participants
Nine papers reporting eight studies, including 6500 participants, were identified. Five were RCTs,25–29 three were CBAs30–32 and one paper reported the economic evaluation of an included trial.33 Three studies were from the US27–29 and five from the UK.25 26 30–32
Participants were majority female ranging from 59% to 75% with only one study reporting majority male participants (62%).30 Mean age ranged from 29 to 71 years. One study focused on adults over 75 years, but did not report mean age.25 Three of the seven studies clearly reported including participants experiencing multimorbidity and deprivation. Two of the US trials tested an intervention (the IMPaCT intervention) that targeted people with two or more chronic conditions, living in a high-poverty zip code.27 28 One UK study was based in GP practices located in postcodes with high deprivation and reported a mean of 3.1 self-reported chronic conditions.31 Otherwise, studies recruited participants based on a combination of factors including: social isolation,25 30 32 mental health problems,30 32 age,25 30 frequent ED attendance29 and GP perception of suitability for the intervention.26 31 32
Interventions and comparators
All interventions included referral to a link worker or equivalent, who identified a set of personalised goals and supported participants to achieve these through connecting with community resources. There was considerable variation in the duration and intensity of the link worker interventions. Intervention duration ranged from 1 month to 2 years, with most interventions ranging from 3 to 9 months in duration. Intensity in terms of link worker caseload and number of contacts was only reported in detail in two of the seven studies. The IMPaCT intervention evaluated in the two US trials was 6 months’ duration with weekly contacts as standard. Each link worker worked with 55 clients per year for an average of 38.4 hours suggesting an average of 1 hour per meeting.34 No other studies reported on link worker caseload. Other interventions were less intense in terms of number of contacts. Carnes et al reported that 69% of participants met the link worker once and 17% had two or more contacts.32 Grant et al reported a mean of 1.7 contacts and Mercer et al a mean of 3.1 contacts.26 31 The remaining two studies did not report on numbers of contacts.25 30 Resources referred to were tailored to the individual in all interventions with counselling services, social and craft groups, exercises classes, addiction supports, welfare and employment advice all mentioned as examples of resources. Only one study specifically reported on uptake of community resources, with uptake of resources positively associated with number of link worker contacts and ranging from 36% of participants who had met once to 71% of participants who had met four times.31
All link workers had professional supervision arrangements, which varied across studies. They were managed and employed by either a research team or a host voluntary community organisation. While efforts were made to standardise the IMPaCT intervention,34 with regular supervision and reviews, the other interventions were very flexible, and fidelity was not assessed. In some cases there was considerable variation in how the intervention was implemented across sites, but this was part of a general tailored approach.30 31 The setting also varied. In three studies, link workers were embedded within general practice or equivalent.28 31 32 In two of these studies, one link worker was assigned to a practice.28 31 In the other, three link workers were based across 22 practices.32 The link workers were based in community settings in the remaining five studies.
The comparator was usual care for all studies, with the inclusion of chronic disease goal setting as a co-intervention in two of the RCTs.27 28 The five RCTs randomised participants at the level of the individual. The three CBA studies recruited controls from nearby GP practices with similar demographics but reported significant differences in demographics and baseline outcome scores between groups (see table 1 for a summary).
Table 1.
Summary of characteristics of included studies
| Study ID | Participants | Intervention | Outcomes |
| Randomised trials | |||
| Clarke et al 1992 Community, UK25 |
523 adults over 75 years living alone Age, gender not reported |
Referral: Recruited via mail invitation Link worker: Lay community-based health worker, training and experience not specified. Contacts: Minimum 3 home visits with tailored support Duration: 2 years Comparator: Usual care |
Primary outcome: Survival Secondary outcomes: Activities of daily living Information/orientation score Loneliness Morale Self-rated health Social contacts Primary healthcare utilisation Costs: None reported Data collection: 0, 24 months. Survival assessed at 6-monthly intervals from baseline to 3.5 years |
| Grant et al 2000 Community, UK26 |
152 adults over 16 who GP felt would benefit from intervention Mean age 43.2 years, 75% female. |
Referral: Recruited via GP referral Link worker: Lay ‘referral facilitator’ trained and employed by a community organisation. Based in community Contacts: 1 face-to-face assessment within a week of referral. Average of 1.7 telephone or face-to-face contacts reported Duration: 1 month Comparator: Usual care |
Primary outcomes:
Mental health: depression and anxiety Social support Secondary outcomes: Quality of life Functional health Primary healthcare utilisation including medications and referrals Costs: Intervention Primary healthcare utilisation Referrals to other agencies Data collection: 0, 1, 4 months |
| Heisler et al 2022 Community, USA29 |
3159 adults aged <65 years residing in a low-income zip code with >3 ED visits or one ambulatory care sensitive admission in last year Mean age 29 years, 64% female. |
Referral: Recruited via Medicaid Link worker: Community health workers, familiar with zip code, trained and employed by community organisations Contacts: 55% at least one contact, mean of 1.9 contacts Duration: Tailored, but up to 1 year Comparator: Usual care |
Primary outcomes:
Healthcare utilisations including
Costs: Healthcare utilisation costs Data collection: 12 months pre-and post-randomisation |
| Kangovi et al 2018 Primary care, USA28 |
592 adults attending three primary care clinics, who resided in a high-poverty zip code had a diagnosis for two or more chronic diseases Mean age 52.6 years, 62.5% female. |
Referral: Recruited via primary care clinics (PCPs) Link worker: Community health workers, with high school diploma. 1 month training in motivational interviewing, action planning and on the job. Based in PCPs Contacts: Monthly face-to-face meetings and weekly telephone check-ins. Duration: 6 months Comparator: Chronic disease goal setting with PCP only |
Primary outcome: HRQoL, physical health component (SF-12-V2 PCS) Secondary outcomes: HRQoL, mental health component (SF-12-V2 MCS) Patient activation Chronic disease control (BP, HbA1C, BMI or CPD) Patient-reported quality of primary care All cause hospitalisations Costs: None reported Data collection: 0, 6, 9 months |
| Kangovi et al 2017 Community, USA27 |
302 adults attending GIM clinics, living in deprived area, and were diagnosed with two or more chronic diseases Mean age 56 years, 74% female. |
Referral: Recruited via PCPs Link worker: Community health workers, with high school diploma. 1 month training in motivational interviewing, action planning and on the job. Based in PCPs Contacts: Monthly face-to-face meetings and weekly telephone check ins. Duration: 6 months Comparator: Chronic disease goal setting with PCP only |
Primary outcome:
Change in chronic disease control (HbA1C, BMI, BP, or CPD) Secondary outcomes: Achievement of chronic disease management goals HRQoL (SF-12-V2 PCS and MCS) Patient activation Patient-reported quality of primary care All cause hospitalisations Costs: Return-on-investment analysis reported on cost savings related to reduced hospitalisations33 Data collection: 0, 6 months for PROMs. 6 and 12 months for hospitalisations |
| Controlled before–after studies | |||
| Carnes et al 2017 Primary care, UK32 |
480 adults frequently attending primary care, who presented with social isolation or mild mental health problems. Median age 56 years, 59% female. |
Referral: GP referral Link worker: 3 lay ‘social prescribing coordinators’ (SPC) trained in social work and managed by community organisation. Based across 22 GP practices. Additional support from volunteers available Contacts: Initial 1 hour meeting and up to six sessions with the SPC, unlimited volunteer support Duration: 6 months Comparator: Propensity matched controls drawn from GP practices in nearby areas with no social prescribing service |
Primary outcome: Not specified Secondary outcomes: Self-rated health Mental health: depression and anxiety Well-being Positive and active engagement in life Number of regular activities A&E visits in past 3 months Annual GP consultation rate Number of medications in previous 6 months Costs: None reported Data collection: 0, 8 months |
| Dickens et al 2011 Community, UK30 |
392 adults over 50 years attending primary care at risk of social isolation Mean age 71 years, 62% male. |
Referral: GP referral Link worker: Mentors often with teaching or creative skills, managed by a community organisation. Training not described. Based in community Contacts: Face-to-face meetings, frequency not specified Duration: 3 months Comparator: Matched controls from a sample drawn from 3 GP practices in nearby areas with no mentoring service |
Primary outcome: HRQoL, mental health component (SF-12-V2 MCS) Secondary outcomes: HRQoL, physical health component (SF-12-V2 PCS) HRQoL (EQ-5D-3L) Mental health: depression Social activities Social support Social participation Costs: None reported Data collection: 0, 3 months |
| Mercer et al 2019 Primary care, UK31 |
900 adults attending primary care in most deprived areas of Glasgow deemed suitable for intervention by GP Median age 49 years, 60% female. |
Referral: GP referral Link worker: Community links practitioners with prior experience of community work, managed by a community organisation. 1 month training on role, supporting clients, engaging practices and mapping resources. Based in GP practices Contacts: Face-to-face meetings. Average of 3 meetings reported Duration: 9 months Comparator: Sample drawn from 6 GP practices in Glasgow without a community links practitioner |
Primary outcome: HRQoL (EQ-5D-5L) Secondary outcomes: Well-being Mental health: depression and anxiety Work and social adjustment scale Self-reported lifestyle behaviours (smoking, alcohol, exercise) Costs: None reported Data collection: 0, 9 months |
A&E, Accident and Emergency; A&E, accident and emergency; BMI, body mass index; BP, blood pressure; CPD, chronic pulmonary disease; ED, Emergency Department; ED, emergency department; GIM, author to define; GIM, General Internal Medicine; GP, general practitioner; GP, General Practice; HbA1C, glycated haemoglobin; HRQoL, health-related quality of life; PCP, primary care practice; PROM, patient-reported outcome measure; SPC, social prescribing coordinator.
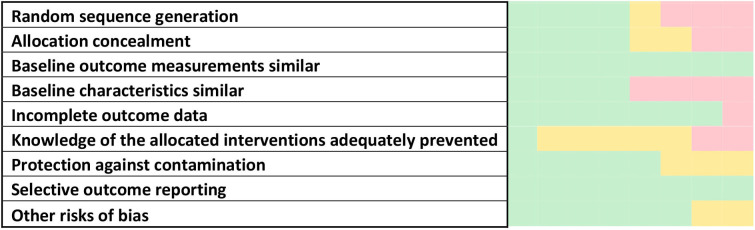
Risk of bias
We used the EPOC guidance to assess risk of bias for both RCTs and CBAs, but have reported them separately for each study design. The RCTs had low risk of bias overall, despite blinding of participants not being possible given the nature of the intervention. Randomisation processes were not clearly reported in one RCT.25 There was high risk of bias in the CBAs. This was due to differences in baseline characteristics and limitations in randomisation and allocation concealment due to study design. A summary of the risk of bias is shown in figure 2. The full risk of bias assessment for all outcomes is available in online supplemental appendix 4 in supplementary data.16
Figure 2.
Risk of bias summary.
bmjopen-2022-062951supp004.pdf (189.6KB, pdf)
Certainty of evidence
For the primary outcomes, the certainty across all study types was low for HRQoL and very low for mental health due to risk of bias, indirectness resulting from differences in interventions and populations across studies, inconsistencies in results and imprecision. The certainty was low for social supports, self-rated health and very low for physical function and activities. For healthcare utilisation, there was very low certainty evidence for hospitalisations based on the US-based RCTs.27–29 There was low certainty evidence for primary care visits, due to indirectness, imprecision and risk of bias (see table 2).
Table 2.
GRADE summary of findings
|
Title: Effect of social prescribing link workers on health outcomes and costs for adults in primary care and community settings
Patients or population: community-dwelling adults Settings: primary and community care Intervention: social prescribing link workers Comparison: usual care | |||
| Outcome | Review finding | Contributing studies (participants) | Overall GRADE assessment |
| Health-related quality of life | Social prescribing link workers may have little or no impact on HRQoL | 2 RCTs (894) US-based 2 CBAs (1292) UK-based |
⊕⊕⊖⊖ Low (Low for RCTs*†‡, Low for CBAs) |
| Mental health | It is unknown if social prescribing link workers improve mental health because the certainty of the evidence is very low | 1 RCT (152) 3 CBAs (1772) All UK-based |
⊕⊖⊖⊖ Very Low§ (Low for RCT*†, Very Low for CBAs¶*) |
| Social contacts and support | Social prescribing link workers may lead to little or no difference in social contacts | 2 RCTs (714) 1 CBA (392) All UK-based |
⊕⊕⊖⊖ Low (Low for RCTs*‡, Low for CBAs) |
| Physical function and activities | It is unknown if social prescribing link workers improve physical function and activity because the certainty of the evidence is very low | 2 RCTs (714) 2 CBAs (1380) All UK-based |
⊕⊖⊖⊖ Very Low (Very Low for RCTs*†‡, Very Low for CBAs¶‡) |
| Self-rated health | Social prescribing link workers may improve self-rated health | 2 RCTs (714) 1 CBA (480) All UK-based |
⊕⊕⊖⊖ Low (Low for RCTs*†, Low for CBA†) |
| Healthcare utilisation: hospitalisation | It is unknown if social prescribing link workers reduce hospitalisations because the certainty of the evidence is very low | 3 RCTs (4053) US-based |
⊕⊖⊖⊖*†, Very Low |
| Healthcare utilisation: primary care visits | Social prescribing link workers may have little or no impact on primary care visits | 3 RCTs (3873) 2 UK- and 1 US-based 1 CBA (480) UK-based |
⊕⊕⊖⊖ Low (Low for RCTs*‡, Very Low for CBAs†) |
RCTs and CBAs were assessed separately for each outcome. If there was limited RCT evidence, then an overall judgement was applied. In this case if there were inconsistencies in results between the two bodies of evidence this was downgraded by one level.
*Downgraded for indirectness.
†Downgraded for inconsistency.
‡Downgraded for imprecision.
§Downgraded for overall inconsistency.
¶Downgraded for risk of bias.
CBA, controlled before–after; HRQoL, health-related quality of life; RCT, randomised controlled trial.
See online supplemental appendix 5 in supplementary data for the full GRADE summary sheet.16
bmjopen-2022-062951supp005.pdf (85.5KB, pdf)
Effectiveness of link worker interventions
Primary outcomes
Four of the eight studies (two RCTs and two CBAs) reported on HRQoL.27 28 30 31 Two studies used the EQ-5D measure with one study reporting no difference,31 while the other study reported a small significant difference between the intervention and control group, in favour of the control group.30 Three studies used the SF-12 measure, with one of the three reporting a significant difference in favour of the intervention for the mental health component score,27 whereas none of the three studies reported any difference in physical component scores.27 28 30 Four studies reported on mental health26 30–32 using HADS-D, HADS-A or GDS-10. Only one of these studies reported evidence of a significant improvement in HADS-A (adjusted Mean Difference −1.9; 95% Confidence Interval −3.0 to −0.7).26 The remaining three studies found no evidence of a difference between groups for any mental health outcomes. See table 3 for a summary of the primary outcome effects.
Table 3.
Primary outcomes: mean at follow-up and adjusted mean differences
| Health-related quality of life | ||||
| Study ID | Outcome measure | Intervention mean (SD) | Control mean (SD) | Adjusted mean differences (95% CI) |
| Kangovi et al US 2018 RCT28 |
Physical Health Component (SF-12-V2 PCS) | 1.8 (11.2) | 1.6 (9.9) | −0.7 (−2.2 to 0.7)* p=0.3 |
| Mental Health Component (SF-12-V2 MCS) | 2.2 (13.3) | 1.2 (14.1) | 0.8 (−1.1 to 2.6)* p=0.41 |
|
| Kangovi et al US 2017 RCT27 |
Physical Health Component (SF-12-V2 PCS) | 0.9† | 0.5† | p=0.66 |
| Mental Health Component (SF-12-V2 MCS) | 2.3† | 0.2† | p=0.008 | |
| Dickens et al
UK 2011 CBA30 |
Physical Health Component (SF-12-V2 PCS) | 34.8 (11.4) | 42.7 (12.6) | 0.8 (−1.5 to 3.2)‡ p=0.48 |
| Mental Health Component (SF-12-V2 MCS) | 46.7 (11.2) | 49.2 (10.0) | 0.1 (−1.9 to 2.1)‡ p=0.9 |
|
| EQ-5D-3L | 0.6 (0.3) | 0.8 (0.2) | −0.09 (−0.14 to 0.03)‡ p=<0.001 |
|
| Mercer et al UK 2019 CBA31 |
EQ-5D-5L | NR | NR | 0.008 (–0.028 to 0.045)§ p=0.648 |
| Mental health | ||||
| Grant et al UK 2000 RCT26 |
Depression (HADS-D) | 7.1 (4.5) | 9.4 (4.9) | −0.9 (−1.9 to 0.2)¶ p=0.116 |
| Carnes et al UK 2017 CBA32 |
Depression (HADS-D) | 10.1 (5.0) | 5.9 (5.2) | 0.857 (−0.737 to 2.451)** p=NR |
| Dickens et al UK 2015 CBA30 |
Depression (GDS-10) | 4.1 (2.4) | 2.2 (2.1) | 0.2 (-0.2, 0.7)‡ p=0.29 |
| Mercer et al UK 2019 CBA31 |
Depression (HADS-D) | NR | NR | 0.09 (–0.49 to 0.68)§ p=0.753 |
| Grant et al UK 2000 RCT26 |
Anxiety (HADS-A) | 10.6 (4.2) | 12.7 (4.3) | −1.9 (−3.0 to −0.7)* p=0.002 |
| Carnes et al UK 2017 CBA32 |
Anxiety (HADS-A) | 11.2 (5.0) | 7.6 (5.4) | −0.119 (−0.847, 1.609)** p=not reported |
| Mercer et al UK 2019 CBA31 |
Anxiety (HADS-A) | NR | NR | –0.41 (–0.99 to 0.18)§ p=0.172 |
| Clarke et al UK 1992 RCT25 |
HRQoL or mental health were not outcomes for this trial | |||
| Heisler et al US 2022 RCT29 |
HRQoL or mental health were not outcomes for this trial | |||
SF-12v2 = Short Form Health Survey is often used as a health-related quality of life measure, with Physical (PCS) and Mental (MCS) health components reported separately on a scale of 0–100 with 100 representing maximal health. EQ-5D-5L = a standardised measure of self-reported health-related quality of life that assesses five dimensions at five levels of severity, where one is the preferred state of health. EQ-5D-3L = an earlier version of EQ-5D-5L with three levels. GDS = Geriatric Depression Scale, a screening tool for depression in older people with a score of 4 or more indicating possible depression. HADS = Hospital Anxiety and Depression Scale measured on a scale of 0–42 where a higher score indicates worse mental health. HADS-A = Hospital Anxiety and Depression Scale, Anxiety, where a score above 10 indicates possible caseness. HADS-D = Hospital Anxiety and Depression Scale, Depression, where a score above 10 indicates possible caseness.
*Longitudinal estimated difference in difference from 6 to 9 months adjusted for site and chronic disease.
†Unadjusted mean difference. SD and adjusted mean differences not reported.
‡Adjusted for employment status, accommodation type and living circumstances.
§Adjusted for age, sex, SIMD, comorbidity, and significant baseline outcome measures as covariates and includes practice identifier as a random effects term.
¶Adjusted for baseline results.
**Adjusted for age, sex, ethnicity, employment status and living arrangement.
aMD, adjusted Mean Difference; CI, Confidence Interval; NR, not reported; SD, Standard Deviation; SIMD, Scottish Index of Multiple Deprivation.
Secondary outcomes
A wide range of other outcomes was reported, with the studies reporting a mean of six outcomes each, including a range of patient-reported outcome measures (PROMs). Three reported on a measure of social contact or support and found no evidence of a difference between groups.25 26 30 One study reported that intervention participants were more likely to rate getting along with others as ‘worse’ than controls, indicating a possible negative effect.30 In terms of other PROMs, two studies found a positive impact on self-rated health,25 26 one study found a positive effect for general quality of life, assessed by the Delighted Terrible Faces scale26 and two studies reported a positive finding on patient rating of high-quality care.27 28 There were no reported differences for patient activation,27 28 well-being,31 32 loneliness,25 morale,25 work and social adjustment31 or active participation in life.32 Of the four studies that reported a measure of physical activity and function, one study found an improvement in functional health,26 while two others found no evidence of a difference in activities of daily living,25 or physical activity31 and the final study found a reduction in usual activities.32 Three studies reported clinical outcomes, one reported on survival over a 3-year period25 and two looked at chronic disease control for smoking, diabetes, obesity and hypertension.27 28 None reported a statistically significant difference between groups.
Six studies reported on healthcare utilisation, with four reporting on primary care utilisation25 26 29 32 and three on hospitalisations.27–29 One study reported a reduction in primary care attendances in the intervention group, but the control group were significantly different and the authors concluded that their findings more likely represented regression to the mean.32 Of the remaining studies, two found no evidence of an effect on primary healthcare attendances and one US-based study actually found an increase in ambulatory care utilisation.29 One of the two US studies evaluating the IMPaCT intervention found a 24% risk reduction in repeat hospital admissions during the 12-month follow-up period28; the other reported a similar reduction, but it did not reach statistical significance.27 The third study that reported hospital admissions found no significant decrease, but there was a decrease in ED attendances.29 See online supplemental appendix 6 in supplementary data for a full list of outcomes and effects for each study.
bmjopen-2022-062951supp006.pdf (95.8KB, pdf)
Costs and cost-effectiveness
No cost utility or cost-effectiveness analyses were identified in our search. Three RCTs reported on costs26 29 33; one as a cost analysis, one on healthcare utilisation costs only, and the third as a separately published return-on-investment analysis of an included RCT.27 The cost analysis looked at primary care visits, medications, referrals and interventions costs. While the study found a reduction in healthcare costs due to a reduction in referrals, these savings did not offset the costs of the intervention. Therefore, the authors concluded that the intervention was more costly than usual care. The analysis did not consider any measure of health benefits to participants such as quality of life years gained.26 The trial that looked at healthcare utilisation did not report intervention costs. They found that the intervention group had slightly lower ED costs, higher ambulatory care costs and no difference in hospitalisation costs.29 The return-on-investment study examined cost savings related to hospitalisations and outpatient attendances from routine data and included detailed costing of the intervention, which was calculated at $1721.06 per participant. While the number of reduced hospital days was statistically non-significant, they estimated a return of $2.47 for every $1 spent on the intervention.33
Subgroup synthesis: multimorbidity and social deprivation
Four of the eight studies reported a measure of multimorbidity or comorbidity. Two of these were RCTs of the IMPaCT intervention in the US and recruited participants with two or more chronic conditions including hypertension, diabetes, obesity and tobacco dependence.27 28 One was a CBA of the Glasgow Deep End link worker intervention and reported a mean of 3.1 chronic conditions in the intervention group, but this was not an inclusion criterion.31 The final study was a US-based RCT and reported that 27% of participants had a Charlson Comorbidity index of greater than two. All four studies targeted participants in areas of deprivation. Three of these studies measure HRQoL. Two of the studies found no effect and one of the US trials found an effect on the Mental Health Component of the SF-12-V2 only,27 which was not replicated in the second trial of this intervention.28 Only the Deep End link worker CBA reported on mental health and found no evidence of a difference between groups. There were no reported significant effects on other patient-reported outcome measures or chronic disease control. The RCTs of the IMPaCT intervention found a consistent improvement in the proportion of participants reporting high-quality primary care. Both also examined hospitalisations, reporting fewer total days in hospital, although this only reached statistical significance in one of the two studies. The other US-based trial that focused on frequent ED attenders in a deprived zip code found a reduction in ED attendances, but increased costs of ambulatory care and no difference in hospitalisations.29
Discussion
We identified eight studies and one economic evaluation of an included study, but we found no consistent evidence to support the effectiveness of social prescribing link worker interventions for improving HRQoL or mental health. There was no evidence for effectiveness in improving social support, physical function and activities, or primary healthcare utilisation, though there was a suggestion from two studies that interventions led to improved self-rated health and two others reported higher patient ratings for quality care. Three of the studies specifically included participants experiencing multimorbidity and social deprivation with similar findings for HRQoL, though two US RCTs reported a reduction in total days in hospital for people with multimorbidity with low certainty evidence. The certainty of the evidence is low or very low overall due to risk of bias, heterogeneity among studies, inconsistency and imprecision.
Our systematic review has not identified any evidence on the cost-effectiveness of social prescribing link workers. There is some evidence of cost savings based on reduced hospitalisations, but this was a US-based study of an intense structured 6-month intervention and may not translate to other healthcare systems.33 Only one UK-based study reported costs, showing a reduction in referral costs, but no cost–benefit analysis or cost–utility analysis was undertaken.26 The economic evaluation of social prescribing link workers in the literature is weak.
There remains a lack of studies with a randomised design since the 2017 review10 that called for “less rhetoric and more reality”. There have been many uncontrolled before–after studies identified in subsequent reviews,11 12 35 but the last RCT in a UK setting was over 20 years ago.26 Widening our search beyond the UK setting resulted in the identification of three relevant RCTs and a return-on-investment analysis in a US setting.27 28 33 Ours is the first review to look specifically at populations experiencing multimorbidity or deprivation. We identified some evidence to support reduced hospital admissions for people experiencing multimorbidity and deprivation in the US. Two of these studies also found an improvement in patients’ rating of the quality of their primary care, which has been reported in previous multimorbidity studies.36 The 2021 systematic review of multimorbidity highlighted the potential for interventions to improve patients’ experience of care,7 which some have argued should be an end in itself.37 We reported on the intensity of the intervention, often omitted from previous reviews and indeed in many of the articles in this review. While intensity varied, a more intense intervention with a healthcare coordination component was the only one with a positive impact on healthcare utilisation.33 These findings demonstrate that it is possible to conduct RCTs of social prescribing link worker interventions, but for those with complex needs more intense interventions delivered alongside chronic disease management programmes may be required to improve outcomes.
The main outcomes for the current review were HRQoL and mental health based on the core outcome set in multimorbidity,21 but only two of the seven studies reported on both of these.30 31 With one exception25 the rest reported on at least one. Most studies did cover some of the NHS draft outcome framework for social prescribing recommended outcomes: well-being, social connectedness, ability to manage day-to-day and physical activity.3 However, as per previous reviews10 11 38 there was a lot of variation in outcomes included and how they were measured, making it difficult to synthesise studies and further weakening the evidence. The outcomes chosen, in particular HRQoL, may also have been difficult to improve in the short time frame of most studies. Improving social connections is one of the key mechanisms by which social prescribing is thought to improve outcomes,39 40 but only three studies reported on this. Including this as an outcome in future may help demonstrate interim impact, with the caveat that both relationships and causal mechanisms between social connection and health and well-being are still contested.
Strengths and limitations
This review involved a rigorous search of the international literature including all languages and the grey literature. We used a wide range of terms to describe the link worker role, providing additional evidence on social prescribing link worker interventions. We had robust study design, inclusion criteria and only included studies that met the Cochrane EPOC guidance for inclusion in a systematic review.23 Additional potentially eligible studies did not meet the inclusion criteria for this review due to non-contemporaneous comparisons, too few sites or offering some sort of social prescribing intervention to control groups.41–43 Previous reviews have included uncontrolled studies with the argument that they are used by policymakers as evidence of effectiveness12; however, including these studies with weaker designs can lead to inflated effect sizes and distort the current evidence base. Unlike previous reviews,10–12 35 44 we appraised the overall certainty of the evidence for our selected outcomes, which was low or very low for most outcomes. This review provides the most up-to-date review of evidence internationally for social prescribing link worker interventions.
Due to the complex nature of social prescribing link worker interventions there may have been a degree of subjectivity in determining which ones to include. To minimise this all full texts were independently reviewed, and where there was a question over intervention inclusion it was discussed with a third author. Our protocol made it clear that it was important that social prescribing was the main element of the intervention, but interpretation of this is also dependent on reporting in potentially eligible studies.17 The field is rapidly expanding, and we may have missed studies published since July 2021. Our forward citation search carried out in June 2022 will go some way to mitigate this. We are also aware of protocols that have not published results or were suspended due to COVID-19, including an RCT that we have conducted with analysis ongoing.45
Implications for policy and practice
It could be argued that only four of the studies tested interventions that reflect the format of current social prescribing link worker activities in the UK, which are relatively short and tailored to the individual and locality, with a high degree of flexibility.26 30–32 Even among these, there is variation in terms of the intensity of support and link worker location, with both community and primary care settings. Embedding link workers in a general practice setting can facilitate more intense support and a focus on healthcare coordination, such as in the US IMPaCT intervention.34 One of the UK studies reported that a subgroup of participants who met a link worker three or more times had improvements in HRQoL, mental health and exercise, suggesting intervention duration and intensity is important to consider.31 Current plans for social prescribing link workers in Ireland and the UK suggest at least double the link worker caseload of the IMPaCT intervention,46 47 and a shorter intervention, that may limit link worker capacity to provide the level of support required to provide benefit, particularly for people with multimorbidity living in deprived areas. There is a need to consider flexibility in how new link worker social prescribing interventions are implemented until more evidence is available on how much and what type of support is required and whether such support needs to be better targeted given ever tighter budget constraints and existing health inequalities.
Policymakers need to be aware that there is insufficient evidence to assess the effectiveness of social prescribing link workers and none on the cost-effectiveness so the opportunity cost is unknown. While it is anticipated that social prescribing link workers will reduce healthcare utilisation at the primary care level,9 many evaluations of social prescribing link worker services struggle to get access to healthcare utilisation data.48 Robust evaluations with both patient-reported outcome data and access to healthcare utilisation data to assist economic evaluations need to be embedded into social prescribing programmes. Evidence from this review suggests that such evaluations are possible and that more intense interventions for certain high-need subgroups are worth developing and evaluating in local healthcare contexts.
The PPI group felt a flexible approach was necessary as some people may need longer support, but also raised the issue of fairness for those who have less complex needs who could benefit from shorter interventions. They agreed with the author team’s conclusions that social prescribing link workers should not be rolled out more widely without evaluations built in, and also felt that outcomes and the way they were measured would benefit from patient input.
Implications for future research
For future research and evaluations to address the evidence gap a number of challenges need to be overcome. Social prescribing interventions are meant to be flexible and tailored, not just to the individual, but also the context. This, however, results in a lot of heterogeneity and difficulty in assessing an overall body of evidence. Future studies could address this by reporting on reasons for referral, duration of intervention, number of contacts and link worker caseload. Further research is also needed to better understand the components of social prescribing and indeed this is underway.49 Since the pandemic, link workers have adapted to restrictions and use more remote supports, which has impacted participants’ experiences.50 The impact of this on outcomes is yet to be evaluated.
There are no agreed outcomes or measures for social prescribing. The NHS does not recommend any specific measures in its draft outcomes framework that recommends self-management, physical activity and social connectedness as individual outcomes.3 The Health Service Executive in Ireland also recommends assessing well-being and social connectedness, but not mental health or HRQoL.48 Without the inclusion of a measure that can be used for cost–utility analysis, building the evidence base around cost-effectiveness will be challenging. The EuroQoL HRQoL measure, EQ-5D-5L,51 is one such measure, but it can be difficult to show changes in a relatively short timeframe52 and is quite health-focused whereas social prescribing has potentially wider social benefits. The ICECAP-A (the ICEpop CAPability measure for Adults) is an alternative.53 It measures capability well-being, can be used in economic evaluations and is recommended by the National Institute for Health and Care Excellence (NICE) for use in evaluations of interventions with potential health and social benefits.54 Future studies should consider its inclusion as an outcome. As mentioned previously, social connectedness is another important interim measure to consider. The Medical Research Council Framework for the Evaluation of Complex Intervention to Improve Health Outcomes recommends multiple outcome measures. In the case of social prescribing, a more refined outcomes framework with specified measures developed with input from service users, providers and academics is needed.
The widespread policy of rolling out social prescribing projects regardless of the lack of certainty around cost-effectiveness makes it challenging for researchers to address the evidence gap, especially in identifying suitable controls. While some CBAs in this review attempted to match controls, there were often significant differences in baseline characteristics as controls were drawn from different populations.30 32 Where social prescribing has already been adopted by policymakers, stepped-wedge cluster RCTs and interrupted time series offer an alternative approach to CBAs and can control better for confounding.55 Other jurisdictions considering implementing social prescribing should carefully consider how they evaluate it from inception. RCTs are feasible as shown by the trials in the review. They are of course challenging given the tailored nature of social prescribing link worker interventions, and parallel process evaluations are recommended to evaluate contextual factors and mechanisms of action,56 which in turn can inform further refining of existing programmes. It is clear, however, that further uncontrolled before–after studies will not advance the evidence base.
Conclusions
Our systematic review suggests that link workers providing social prescribing may have little or no impact on HRQoL, mental health or a range of patient-reported outcomes though they may improve self-rated health. For patients with multimorbidity in areas of deprivation, an intensive link worker intervention probably improves patients’ ratings of high-quality primary care and reduces hospitalisations, but these findings are based on two studies in the US and require evaluation in other health systems. The opportunity costs of investing in social prescribing link workers are unknown and it is essential that high-quality trials determining cost-effectiveness are conducted so that the evidence can catch up with the policy and we avoid wasting valuable time and resources.
Supplementary Material
Acknowledgments
Paul J Murphy MLIS (Information Specialist, Royal College of Surgeons Ireland Library, 26 York Street, Dublin D02 YN77, Ireland) advised on search strategies.
Footnotes
Twitter: @bridgetmkiely
Contributors: BK was the primary reviewer and designed and conducted the search, reviewed identified texts, extracted data, performed the narrative synthesis and wrote the main draft. AC was a second reviewer of identified texts and for the quality assessment. MOS performed citation searches, verified data extraction and was second reviewer for certainty of evidence assessment. FB provided statistical support, wrote the protocol for meta-analysis and advised on feasibility of same. EOS provided health economics expertise and advised on identification and summary of cost analysis studies. DC provided input into the search protocol, in particular descriptions and definitions of the link worker role. SMS conceptualised the original review questions, was involved in designing methods of the review and acted as a third reviewer. SMS is the author acting as guarantor. All authors contributed to critique and revisions of draft manuscripts and have approved the final version.
Funding: This research was funded by the Health Research Board Ireland (Grant Reference HRB CDA 2018 Reference CDA-2018-003). The funders did not have any role in the design of this study.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available in a public, open access repository. All data relevant to the study are included in the article or uploaded as supplementary information. Supplementary data are available on the Open Science Framework: Kiely B. (2022, July 19). Effect of social prescribing link workers on health outcomes and costs for adults in primary care and community settings: a systematic review. https://doi.org/10.17605/OSF.IO/G2Y4C. This project contains the following supplementary data: Appendix 1: PRISMA checklist for ‘A systematic review of the effectiveness of link workers providing social prescribing on health outcomes and costs for adults in primary care and community settings.’ Appendix 2: Full Search Strategy and Results. Appendix 3: GRIPP 2 Form for PPI. Appendix 4: Risk of Bias tables. Appendix 5: GRADE Assessment Sheets. Appendix 6: All outcomes table. Data are available under the terms of the CC-By Attribution-NonCommercial-NoDerivatives 4.0 International.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1. Polley MJ, Fleming J, Anfilogoff T. Making sense of social prescribing. London: University of Westminiter, 2017. [Google Scholar]
- 2. National Health Service (NHS) . NHS careers: social prescribing link worker NHS careers, 2021. Available: https://www.healthcareers.nhs.uk/explore-roles/wider-healthcare-team/roles-wider-healthcare-team/clinical-support-staff/social-prescribing-link-worker/social-prescribing-link-worker
- 3. National Health Service (NHS) . Social prescribing England, 2020. Available: https://www.england.nhs.uk/personalisedcare/social-prescribing/
- 4. Wallace E, Salisbury C, Guthrie B, et al. Managing patients with multimorbidity in primary care. BMJ 2015;350:h176. 10.1136/bmj.h176 [DOI] [PubMed] [Google Scholar]
- 5. Payne RA, Abel GA, Guthrie B, et al. The effect of physical multimorbidity, mental health conditions and socioeconomic deprivation on unplanned admissions to hospital: a retrospective cohort study. CMAJ 2013;185:E221–8. 10.1503/cmaj.121349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Barnett K, Mercer SW, Norbury M, et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 2012;380:37–43. 10.1016/S0140-6736(12)60240-2 [DOI] [PubMed] [Google Scholar]
- 7. Smith SM, Wallace E, Clyne B, et al. Interventions for improving outcomes in patients with multimorbidity in primary care and community setting: a systematic review. Syst Rev 2021;10:271. 10.1186/s13643-021-01817-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Husk K, Elston J, Gradinger F, et al. Social prescribing: where is the evidence? Br J Gen Pract 2019;69:6–7. 10.3399/bjgp19X700325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Drinkwater C, Wildman J, Moffatt S. Social prescribing. BMJ 2019;364:l1285. 10.1136/bmj.l1285 [DOI] [PubMed] [Google Scholar]
- 10. Bickerdike L, Booth A, Wilson PM, et al. Social prescribing: less rhetoric and more reality. A systematic review of the evidence. BMJ Open 2017;7:e013384. 10.1136/bmjopen-2016-013384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Pescheny JV, Randhawa G, Pappas Y. The impact of social prescribing services on service users: a systematic review of the evidence. Eur J Public Health 2020;30:664–73. 10.1093/eurpub/ckz078 [DOI] [PubMed] [Google Scholar]
- 12. Vidovic D, Reinhardt GY, Hammerton C. Can social prescribing foster individual and community well-being? A systematic review of the evidence. Int J Environ Res Public Health 2021;18:5276. 10.3390/ijerph18105276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Morse DF, Sandhu S, Mulligan K, et al. Global developments in social prescribing. BMJ Glob Health 2022;7:e008524. 10.1136/bmjgh-2022-008524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cochrane . Cochrane Effective Practice and Organisation of Care (EPOC), 2017. Available: https://epoc.cochrane.org/sites/epoc.cochrane.org/files/public/uploads/Resources-for-authors2017/what_study_designs_should_be_included_in_an_epoc_review.pdf
- 15. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kiely B, Croke A, O'Shea M. Effect of social prescribing link workers on health outcomes and costs for adults in primary care and community settings: a systematic review. Open Science Framework 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kiely B, Croke A, O'Shea E, et al. Effectiveness of link workers providing social prescribing on health outcomes and costs for adult patients in primary care and community settings. A protocol for a systematic review of the literature. HRB Open Res 2019;2:21. 10.12688/hrbopenres.12936.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tierney S, Wong G, Mahtani KR. Current understanding and implementation of ‘care navigation’ across England: a cross-sectional study of NHS clinical commissioning groups. Br J Gen Pract 2019;69:e675–81. 10.3399/bjgp19X705569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Smith SM, Wallace E, O'Dowd T, et al. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Syst Rev 2016;9. 10.1002/14651858.CD006560.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Butler DC, Petterson S, Phillips RL, et al. Measures of social deprivation that predict health care access and need within a rational area of primary care service delivery. Health Serv Res 2013;48:539–59. 10.1111/j.1475-6773.2012.01449.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Smith SM, Wallace E, Salisbury C, et al. A core outcome set for multimorbidity research (COSmm). Ann Fam Med 2018;16:132–8. 10.1370/afm.2178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Craig P, Dieppe P, Macintyre S, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337:a1655. 10.1136/bmj.a1655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Cochrane . Cochrane Effective Practice and Organisation of Care (EPOC) resources for review authors, 2017. Available: epoc.cochrane.org/resources/epoc-resources-review-authors
- 24. Grading of Recommendations Assessment, Development and Evaluation (GRADE) . Grade working group, 2019. Available: http://www.gradeworkinggroup.org/
- 25. Clarke M, Clarke SJ, Jagger C. Social intervention and the elderly: a randomized controlled trial. Am J Epidemiol 1992;136:1517–23. 10.1093/oxfordjournals.aje.a116473 [DOI] [PubMed] [Google Scholar]
- 26. Grant C, Goodenough T, Harvey I, et al. A randomised controlled trial and economic evaluation of a referrals facilitator between primary care and the voluntary sector. BMJ 2000;320:419–23. 10.1136/bmj.320.7232.419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kangovi S, Mitra N, Grande D, et al. Community health worker support for disadvantaged patients with multiple chronic diseases: a randomized clinical trial. Am J Public Health 2017;107:1660–7. 10.2105/AJPH.2017.303985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kangovi S, Mitra N, Norton L, et al. Effect of community health worker support on clinical outcomes of low-income patients across primary care facilities: a randomized clinical trial. JAMA Intern Med 2018;178:1635–43. 10.1001/jamainternmed.2018.4630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Heisler M, Lapidos A, Kieffer E, et al. Impact on health care utilization and costs of a Medicaid community health worker program in Detroit, 2018-2020: a randomized program evaluation. Am J Public Health 2022;112:766–75. 10.2105/AJPH.2021.306700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Dickens AP, Richards SH, Hawton A, et al. An evaluation of the effectiveness of a community mentoring service for socially isolated older people: a controlled trial. BMC Public Health 2011;11:218. 10.1186/1471-2458-11-218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Mercer SW, Fitzpatrick B, Grant L, et al. Effectiveness of community-links practitioners in areas of high socioeconomic deprivation. Ann Fam Med 2019;17:518–25. 10.1370/afm.2429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Carnes D, Sohanpal R, Frostick C, et al. The impact of a social prescribing service on patients in primary care: a mixed methods evaluation. BMC Health Serv Res 2017;17:1–9. 10.1186/s12913-017-2778-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kangovi S, Mitra N, Grande D, et al. Evidence-based community health worker program addresses unmet social needs and generates positive return on investment. Health Aff 2020;39:207–13. 10.1377/hlthaff.2019.00981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kangovi S, Carter T, Charles D, et al. Toward a scalable, patient-centered community health worker model: adapting the IMPaCT intervention for use in the outpatient setting. Popul Health Manag 2016;19:380–8. 10.1089/pop.2015.0157 [DOI] [PubMed] [Google Scholar]
- 35. Reinhardt GY, Vidovic D, Hammerton C. Understanding loneliness: a systematic review of the impact of social prescribing initiatives on loneliness. Perspect Public Health 2021;141:204–13. 10.1177/1757913920967040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Salisbury C, Man M-S, Bower P, et al. Management of multimorbidity using a patient-centred care model: a pragmatic cluster-randomised trial of the 3D approach. Lancet 2018;392:41–50. 10.1016/S0140-6736(18)31308-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Dowrick C. Patient-centred care for multimorbidity: an end in itself? Lancet 2018;392:4–5. 10.1016/S0140-6736(18)31386-2 [DOI] [PubMed] [Google Scholar]
- 38. Thomas G, Lynch M, Spencer LH. A systematic review to examine the evidence in developing social prescribing interventions that apply a co-productive, co-designed approach to improve well-being outcomes in a community setting. Int J Environ Res Public Health 2021;18:3896. 10.3390/ijerph18083896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Tierney S, Wong G, Roberts N, et al. Supporting social prescribing in primary care by linking people to local assets: a realist review. BMC Med 2020;18:49. 10.1186/s12916-020-1510-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kellezi B, Wakefield JRH, Stevenson C, et al. The social cure of social prescribing: a mixed-methods study on the benefits of social connectedness on quality and effectiveness of care provision. BMJ Open 2019;9:e033137. 10.1136/bmjopen-2019-033137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Maughan DL, Patel A, Parveen T, et al. Primary-care-based social prescribing for mental health: an analysis of financial and environmental sustainability. Prim Health Care Res Dev 2016;17:114–21. 10.1017/S1463423615000328 [DOI] [PubMed] [Google Scholar]
- 42. Foster A, Thompson J, Holding E, et al. Impact of social prescribing to address loneliness: a mixed methods evaluation of a national social prescribing programme. Health Soc Care Community 2021;29:1439–49. 10.1111/hsc.13200 [DOI] [PubMed] [Google Scholar]
- 43. Embick ER, Maeng DD, Juskiewicz I, et al. Demonstrated health care cost savings for women: findings from a community health worker intervention designed to address depression and unmet social needs. Arch Womens Ment Health 2021;24:85–92. 10.1007/s00737-020-01045-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Costa A, Sousa CJ, Seabra PRC, et al. Effectiveness of social prescribing programs in the primary health-care context: a systematic literature review. Sustainability 2021;13:2731. 10.3390/su13052731 [DOI] [Google Scholar]
- 45. Kiely B, Clyne B, Boland F, et al. Link workers providing social prescribing and health and social care coordination for people with multimorbidity in socially deprived areas (the LinkMM trial): protocol for a pragmatic randomised controlled trial. BMJ Open 2021;11:e041809. 10.1136/bmjopen-2020-041809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. National Health Service (NHS) . NHS long term plan, 2019. Available: https://www.longtermplan.nhs.uk
- 47. Health and Safety Executive (HSE) . HSE social prescribing framework 2021. Available: https://www.hse.ie/eng/about/who/healthwellbeing/our-priority-programmes/mental-health-and-wellbeing/hse-social-prescribing-framework.pdf
- 48. Health and Safety Executive (HSE) . Building the capacity for the evaluation of social prescribing. Evaluability assessment, 2020. Available: https://www.hse.ie/eng/about/who/healthwellbeing/our-priority-programmes/mental-health-and-wellbeing/building-capacity-for-the-evaluation-of-social-prescribing-evaluability-assessment.pdf
- 49. Tierney S, Mahtani KR. Understanding the implementation of link workers in primary care: a realist evaluation to inform current and future policy, 2021. Available: https://fundingawards.nihr.ac.uk/award/NIHR130247
- 50. Morris SL, Gibson K, Wildman JM, et al. Social prescribing during the COVID-19 pandemic: a qualitative study of service providers' and clients' experiences. BMC Health Serv Res 2022;22:258. 10.1186/s12913-022-07616-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Gusi N, Olivares PR, Rajendram R. The EQ-5D health-related quality of life questionnaire. In: Preedy VR, Watson RR, eds. Handbook of disease burdens and quality of life measures. New York, NY: Springer New York, 2010: 87–99. [Google Scholar]
- 52. Fortin M, Stewart M, Ngangue P, et al. Scaling up patient-centered interdisciplinary care for multimorbidity: a pragmatic mixed-methods randomized controlled trial. Ann Fam Med 2021;19:126–34. 10.1370/afm.2650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Al-Janabi H, Flynn TN, Coast J. Development of a self-report measure of capability wellbeing for adults: the ICECAP-A. Qual Life Res 2012;21:167–76. 10.1007/s11136-011-9927-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. National Institute for Health and Care Excellence (NICE) . Developing NICE guidelines: the manual. London: NICE, 2014. https://www.nice.org.uk/process/pmg20/chapter/incorporating-economic-evaluation [PubMed] [Google Scholar]
- 55. Schünemann HJ, Cuello C, Akl EA, et al. GRADE guidelines: 18. How ROBINS-I and other tools to assess risk of bias in nonrandomized studies should be used to rate the certainty of a body of evidence. J Clin Epidemiol 2019;111:105–14. 10.1016/j.jclinepi.2018.01.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Moore GF, Audrey S, Barker M, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350:h1258. 10.1136/bmj.h1258 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-062951supp001.pdf (54.7KB, pdf)
bmjopen-2022-062951supp002.pdf (191.3KB, pdf)
bmjopen-2022-062951supp003.pdf (123.8KB, pdf)
bmjopen-2022-062951supp004.pdf (189.6KB, pdf)
bmjopen-2022-062951supp005.pdf (85.5KB, pdf)
bmjopen-2022-062951supp006.pdf (95.8KB, pdf)
Data Availability Statement
Data are available in a public, open access repository. All data relevant to the study are included in the article or uploaded as supplementary information. Supplementary data are available on the Open Science Framework: Kiely B. (2022, July 19). Effect of social prescribing link workers on health outcomes and costs for adults in primary care and community settings: a systematic review. https://doi.org/10.17605/OSF.IO/G2Y4C. This project contains the following supplementary data: Appendix 1: PRISMA checklist for ‘A systematic review of the effectiveness of link workers providing social prescribing on health outcomes and costs for adults in primary care and community settings.’ Appendix 2: Full Search Strategy and Results. Appendix 3: GRIPP 2 Form for PPI. Appendix 4: Risk of Bias tables. Appendix 5: GRADE Assessment Sheets. Appendix 6: All outcomes table. Data are available under the terms of the CC-By Attribution-NonCommercial-NoDerivatives 4.0 International.