Abstract
Objectives
To explore ways to enhance the design of risk factor management and weight-loss services for people with overweight/obesity and atrial fibrillation (AF).
Background
AF is the most common cardiac arrhythmia, with serious consequences for health and quality of life. Some evidence indicates weight reduction in people with AF and overweight/obesity may improve symptoms. This population may require additional support with weight management due to factors associated with ageing and health.
Design
Qualitative investigation based on semi-structured interviews.
Methods
12 adult participants (4 female, 8 male) with diagnosed AF and a current or previous body mass index >27 kg/m2 were recruited at a large tertiary cardiac referral centre in southern England between September 2020 and January 2021. Participants completed quality of life and AF symptom questionnaires using Think-Aloud technique and semi-structured interviews relating to their weight management experiences, needs and preferences. Interviews were audio recorded and analysed thematically using the Capability, Opportunity and Motivation-Behaviour model as a theoretical framework.
Results
Three main themes were identified. Being out of rhythm explores the psychological and physical impact of AF on weight management; doing the right thing discusses participants’ weight management experiences and broaching the subject explores participants’ perspectives on weight management conversations with clinicians.
Conclusions
There was dissatisfaction with the weight management advice received from healthcare professionals including cardiologists. Participants wanted open, non-judgemental discussion of cardiac health implications of overweight/obesity supported by referral to weight management services. Improved communication including research findings regarding the benefits of weight loss as a factor in AF management might increase motivation to adhere to weight-loss advice in this population.
Keywords: adult cardiology, cardiac epidemiology, pacing & electrophysiology, organisation of health services, nutrition & dietetics, qualitative research
Strengths and limitations of this study.
Explores views and experiences of patients with atrial fibrillation and overweight, illuminating barriers to weight management.
The Capability, Opportunity and Motivation-Behaviour model facilitated application of findings to strategies to improve clinical practice.
Only included the views of people willing to discuss weight management.
Participants were recruited from an ethnically homogeneous population; further research is needed to reflect the perspectives of the wider population.
Introduction
Mounting evidence demonstrates weight loss improves symptoms and slows disease progression in people with atrial fibrillation (AF) and overweight.1 Yet despite convincing evidence of the health benefits, few cardiac patients with overweight achieve healthy weight management in the long-term.2 Weight loss is a complex and sometimes onerous undertaking, subject to multifactorial biological, behavioural,3 socioeconomic, environmental and personal influences.4 5 Incidence of AF increases with age, meaning patients are likely to be older and experience more concurrent conditions than the populations in general weight management studies. Better understanding of patients’ lived reality of these factors could improve the design of weight management services for this population.
A qualitative synthesis of studies examining weight management among patients with myocardial infarction (MI) undertaking cardiac rehabilitation found the cardiac event served as a ‘wake-up call’, revealing the extent of damage to health.6–8 Although motivated to lose weight, individuals often felt overwhelmed and lacked knowledge and strategies to enact lifestyle changes.6–8 Referral to weight management services was valued and access to supervised exercise facilities allayed safety concerns.6 8 Personalisation of services increased acceptability and compliance.8
The experiences of people with AF are different from those recovering from MI—AF is not acutely life-threatening, cardiac rehabilitation is not routinely provided, treatment success rates vary.9 Growing evidence indicates advice to patients with AF should include proactive weight management10 11 but guidance on tailoring advice and services to meet patients’ needs is limited. No existing qualitative literature explores the experiences of people with overweight and AF. The objective of this study is to identify practical ways to address perceived barriers to weight reduction through better understanding of patients’ experiences and perspectives.
Methods
Language and definitions
Overweight and obesity are defined by WHO as a body mass index (BMI) ≥25 kg/m2 or 30 kg/m2, respectively.12 The inclusion criteria for this study adopted a BMI of 27 kg/m2 or greater, in line with previous quantitative studies of overweight and AF.10 11 The term ‘overweight’ is used in this report to describe a BMI of 27 kg/m2 or over, except when discussing other studies which specifically investigate obesity.
Patient and public involvement
Advice on design, relevance and acceptability was obtained from two volunteers with AF (one also had BMI >27 kg/m2) and previous research experience via a patient and public involvement bulletin. Minor alterations to the patient information sheet were made as advised. No design changes were suggested.
Design
A qualitative interview study design was used to explore patients’ perspectives and experiences13 of living with AF and overweight. Because weight management involves behaviour change, the Capability, Opportunity and Motivation-Behaviour (COM-B) model14—which identifies capability, opportunity and motivation as the three essential elements for behaviour change—was used as the theoretical framework. These elements form the hub of the Behaviour Change Wheel that represents the complexity of the economic, social and political influences that interact with COM elements ultimately determining behavioural choices.15 The model was embedded in study design, as a topic guide for interviews, and as a framework for data analysis to enhance theoretical coherence and consistency.16 Using an interpretive description approach,17 we sought clinically usable explanations for weight management behaviours by exploring complex patient experiences through the conceptual COM-B model.
Context and sampling
Twelve participants were purposively recruited from outpatient services at a large tertiary referral centre in southern England between September 2020 and January 2021. All participants had to have AF, have current or previous BMI of 27 kg/m2 or over and be able to converse in English (see table 1 for selected participant characteristics). Potential participants were approached during hospital appointments by the direct care team and provided with a patient information sheet. Fourteen patients were approached in total; two declined, stating they did not wish to discuss weight management. Recruitment continued until data saturation was reached.
Table 1.
Selected participant demographics and characteristics
| Age range (years) | Employment | Education | BMI (kg/m2) | Type of AF | Years since AF diagnosis | Symptomatic | Reported previous weight loss (kg) | Weight loss method |
| 70–79 | Retired teacher | Higher | 30 | Paroxysmal | >10 | Yes | 19 (regained) | Very low calorie (self-directed) |
| 70–79 | Retired from food industry | Secondary | 43 | Paroxysmal | 5 | Yes | Not reported | Very low calorie (self-directed) |
| 60–69 | Cook | Secondary | 25 | Paroxysmal | >10 | Yes | 19 | Dietary, self-directed |
| 60–69 | Hospitality | Further | 28 | Persistent | 9 | Yes | 22 (regained) | Slimming World |
| 50–59 | Tradesperson | Secondary | 28 | Persistent | <1 | Yes | 4 | Diet and exercise, self-directed |
| 60–69 | Leisure industry (retired firefighter) | Further | 41 | Persistent | 2.5 | Yes | 50 (partially regained) | Slimming World |
| 50–59 | Retired firefighter | Secondary | 37 | Persistent | 1.5 | Yes | 19 (regained) | Previously Slimming World. Now on BHF diet (LOSE-AF study) |
| 60–69 | Nurse | Higher | 41 | Paroxysmal | 9 | Yes | Not reported | Various |
| 60–69 | Carer | Further | 36 | Paroxysmal | >10 | Yes | 11 | Diet and exercise, self-directed |
| 60–69 | Tradesperson and business owner | Secondary | 31 | Persistent | >10 | No | 53 (partial regain) | Previously aloe vera diet. Now Cambridge 1:1 (LOSE-AF study) |
| 50–59 | Teacher | Higher | 34 | Persistent | 3 | Yes | 28 (partial regain) | SlimFast |
| 70–80 | Retired electronics engineer | Further | 37 | Persistent | <1 | Yes | 7 | Cambridge 1:1 (LOSE-AF study) |
AF, atrial fibrillation; BHF, British Heart Foundation diet; BMI, body mass index.
Data collection
Interviews were conducted by an experienced female, M-level trained, research nurse (RWB). This information was included in the patient information sheet. One participant was previously known to RWB through participation in an unrelated clinical trial. All others were unknown. Interviews were conducted by telephone due to the COVID-19 pandemic that restricted research and elective clinical activity. The participant known to RWB chose to be interviewed face-to-face in a research facility clinic room after attending a hospital appointment. Two participants were interviewed with their partners in attendance, who occasionally commented in the background. Interviews lasted between 31 and 100 min with a mean of 55 min. Interviews were audio recorded and transcribed verbatim by RWB.
The interview process was carefully planned by RWB, CB and AET to encourage participants to feel comfortable and able to speak openly about their weight management experiences with a focus on service improvement.18 Participants’ experiences were explored using semi-structured interviews.19 To reduce any discomfort discussing weight and to focus on AF,20 participants began by completing two questionnaires frequently used in quantitative studies of AF and hence well validated: Atrial Fibrillation Symptom Severity Scale21; EuroQol-5 Dimension-5L22 using Think-Aloud,23 a technique previously explored in nursing research by CB24 who provided training and oversight to RWB. Participants were encouraged to verbalise their thoughts while completing the questionnaires which enables deeper reflection, self-awareness and insight into the meanings behind their responses about behaviours and decisions.23 The Think-Aloud technique facilitated identification of instances where questionnaire responses reflected adaptations in expectations to accommodate worsening health,24 and has been used previously to explore the support needs of patients with AF.25
A topic guide (online supplemental appendix A) based on the COM-B model helped frame the ongoing interview around physical and psychological capabilities, opportunities and motivation for weight management with reference to the questionnaire responses.18 For example, “In the category ‘Usual Activities’, you answered ‘I have slight problems doing my usual activities’—can you tell me a bit about what your usual activities include? What do you consider the reasons for these problems? [Capability]”. No pilot test was performed but the topic guide was allowed to development as the interviews progressed to follow new lines of enquiry.
bmjopen-2022-065995supp001.pdf (59.4KB, pdf)
Rigour
Several strategies were used to address rigour. Triangulation26 was carried out by providing a summary of the interview to each participant before analysis to confirm it reflected their views, meanings and intentions, and to allow for clarification (no participants asked for changes to be made). Reflexivity was facilitated by writing field notes to record responses, reflections and assumptions following each interview and during transcription. The researchers’ subjectivity was examined using the Peshkin27 28 model of reflection to sharpen awareness of the effect of assumptions, values and biases in shaping the study findings.
The study is reported following the Consolidated criteria for Reporting Qualitative research guidelines29 (online supplemental appendix B) to ensure comprehension and transparency.
bmjopen-2022-065995supp002.pdf (120.8KB, pdf)
Analysis
The transcribed data were imported to a spreadsheet and manually coded line-by-line using the Eclectic Coding process30 to identify processes and phenomena. Process codes, which capture action,30 were widely used to emphasise the active nature of behaviour change within the COM-B model. Descriptive codes were used to summarise topics, and values codes to label participants’ perspectives.30
RWB carried out the initial coding. Coding and subsequent thematic development were reviewed and discussed between RWB, CB and AET to reach consensus.
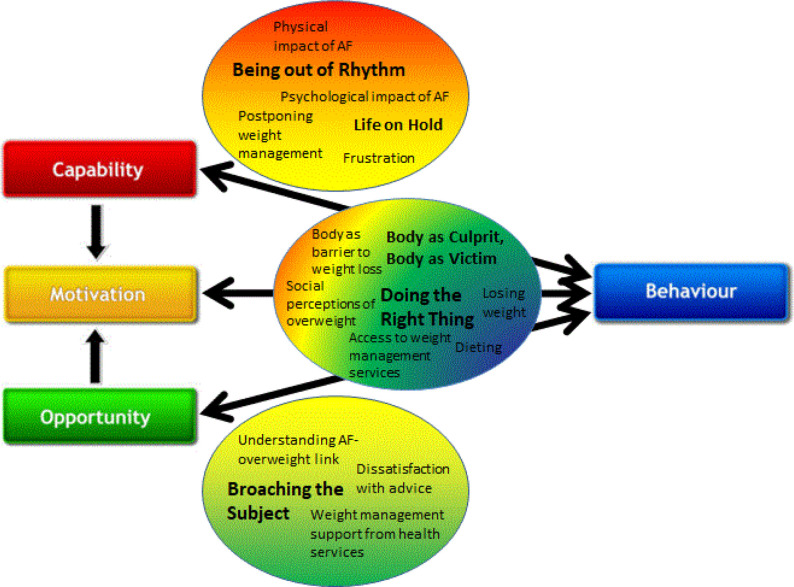
Codes were mapped onto the COM-B framework and organised into subthemes. As working themes were identified, a recoding process was carried out to maintain thematic coherence30 (see table 2 for examples of this process). As coding progressed, themes were identified which transcended the COM-B divisions or reflected the interplay between them (see figure 1). The colour-coded COM-B framework was therefore dismantled, and the individual codes reorganised within the overarching themes. The resulting schema was checked against the original interviews to enrich the authenticity of the description by returning to the participants’ voices and ensure participants’ various perspectives were fairly represented.26
Table 2.
Examples of coding and thematic analysis process
| Quote | Initial codes (initial framework theme) | Recoded to | COM-B category | Theme |
| “It bothers me… not the actual… It bothers me that I can hear it in my ears more than anything”.—Male, aged 70–79 years | Annoying symptoms (what it feels like for me) | Psychological impact of AF | Motivation | Being out of rhythm |
| "At the minute, touch wood… it feels like it wants to start, like at work today it kind of skipped a beat and I thought oh no please don’t start!”—Female, aged 60–69 years | Touching wood (motivation); dreading relapse (capability—psychological) | Psychological impact of AF | Motivation | Being out of rhythm |
| "I know if I lost half a stone I would feel that little bit quicker, a bit lighter, but I wouldn’t want to lose any more than that because it would like take that bit of strength away”.—Male, aged 50–59 years | Being big and strong (motivation—reflective) | Desire to lose weight—confounding factors | Motivation | Doing the right thing |
| "But yeah that’s what I’d like, to go through foods with me, to say well no you can’t really have that—I’m only thinking I’ll have that because it’s got no sugar in it—do you know what I mean? But I don’t think about maybe the fat content. I think about the sugar content, I think oh great I can have that—do you know what I mean? So… It’s someone to sit and educate me, more than anything”.—Female, aged 60–69 years | Nutritional knowledge (capability— psychological); desired help (opportunity—physical); wanting to talk about weight (motivation—automatic); changing diet (behaviour change) | Weight management knowledge; desired help | Capability, Opportunity, Motivation; Behaviour Change |
Doing the right thing |
| "I can’t remember exactly what she said but I think it was around the weight issue. But none of them, none of them have said that the weight was an issue for any of the procedures that were going to be done, so I didn’t make much of it other than to say you know that. But it’s usually that if you lose a bit of weight then. I don’t know I can’t remember what they said but basically lose some weight—it wasn’t an order, it was just advice”.—Male, aged 50–59 years | Risks not explained (motivation—reflective); choosing what to hear (motivation—automatic) | Patient education | Motivation | Broaching the subject |
| "Years ago when I lived in [city] um, they could, sounds silly I know but they could put the gym on prescription for so many months, which is what one doctor done for me and I used to go to the gym, um, oh two, three times a week then”.—Female, aged 60–69 years | Having weight loss prescription (motivation—reflective); doing exercise (capability—physical) | Being referred | Motivation, opportunity | Broaching the subject |
Figure 1.
Map of themes with relation to Capability, Opportunity and Motivation-Behaviour elements.15 AF, atrial fibrillation.
Findings
Participants
The sample included four women and eight men, a gender ratio which corresponds to the general AF population.31 Ages ranged from 50 to 76 years. A range of socioeconomic, educational and professional backgrounds were represented. All participants identified as white British, consistent with the demography of the AF population managed at the study site (table 1).
Time since AF diagnosis ranged from 4 months to 15 years. Five participants had paroxysmal AF (occurring in self-limiting episodes lasting <1 week) and seven had persistent AF (lasting >1 week). Eleven participants reported comorbidities and five reported two or more, which impacted on their activities of daily living and quality of life, the most common being ischaemic heart disease, type 2 diabetes mellitus and joint pain.
BMI ranged from 25 (after sustained weight loss) to 43 kg/m2. All participants reported having lost weight at some point in life, from 4 to 53 kg, but most, at least partially, had regained weight.
Being out of rhythm
Being out of rhythm describes the physical and psychological disruption AF caused to participants’ lives. Symptoms impeded day-to-day activities, corresponding with the capability component of COM-B. Participants characterised these limitations as a life having lost its rhythm: they could no longer live the life they wanted while experiencing AF and were left waiting to regain their rhythm, both cardiologically and metaphorically. Waiting for treatment, uncertainty of its effectiveness and fear of relapse appeared to sap motivation to engage in healthy lifestyle behaviours. A female participant who experienced infrequent, random-onset AF episodes reflected on how a sense of suspense affected her psychologically:
I just feel edgy when it’s out of sync… I can’t wait for it to drop back into rhythm—Female, aged 70–79 years
The physical impacts of AF included fatigue, breathlessness, chest pain, palpitations and faintness and ranged in severity from mild to debilitating. Nine of the 12 participants had been hospitalised with severe symptoms, and 11 had undergone cardioversion or ablation for symptom management. Although reassured by their cardiologists that AF is not life-threatening, the onset of symptoms could still induce significant anxiety and sometimes panic. This was typified by a healthcare professional participant, who struggled to reconcile her objective clinical understanding of AF with the subjective distress she felt when experiencing arrhythmias:
It is horrible, it is horrible… and it can come on at any time so if I’m at work or at a meeting… you haven’t even got a chance to be away from anyone noticing you’re not very well … you don’t want people to know you’re in AF. Especially people my office who are nurses, they’re not going to take much notice really!—Female, aged 60–69 years
Symptoms impacted family activities, work, housekeeping, hobbies and sleep patterns. The sense of life being suspended was experienced as a Life on hold. Some participants felt unsafe and deliberately limited their activities for fear of precipitating an episode of AF or damaging their heart. Participants who had previously been active identified their symptoms as a cause of weight gain. Inability to exercise impacted energy expenditure, but could also affect motivation by disrupting social lives and removing pleasure. Physical limitations often had psychological ramifications, causing frustration and anxiety about deteriorating health and ageing as expressed by a male participant whose career in the fire service had been truncated by AF:
It’s doing my head in to a point. I hate it. Frustration is a massive thing because I’m in my 50s and like I said I’m an ex-firefighter and all that stuff and I’m used to being healthy and active, I’m not someone for sitting around and watching TV all day.—Male, aged 50–59 years
None of the participants attributed weight gain solely to AF, although some cited reduced physical capacity due to AF symptoms as a contributing factor. Returning to sinus rhythm was for some the only way to regain health and previous lifestyles. This resulted in postponing weight management attempts until such a time when, back in rhythm, they would regain the mental energy to focus on diet and the physical capability to exercise.
Doing the right thing
All participants considered overweight unhealthy and undesirable, and articulated positive health behaviours as doing the right thing. All four elements of the COM-B model are reflected within this theme—participants reported motivation to lose weight and intentional behaviour change but felt their health or bodily constitution hindered their capability, or lacked the opportunity to access appropriate services. Inability to sustain weight loss despite following advice to the best of their ability caused significant frustration. A male participant who had previously lost but then regained weight following a high-protein commercial weight-loss programme reflected on the slower measurable effects of his current low-fat, calorie-controlled approach:
I try and eat healthily—we do eat healthily—we have fruit and veg more, far more than five portions a day, so I believe we eat healthily. I try and exercise, um, so at the moment I’m on this healthy diet that the British Heart Foundation recommend, and my wife’s good at measuring out portion sizes and this sort of thing… So we’ve been doing that for a couple of weeks now and it’s ok but I’ve only lost—for me—hardly anything, like a pound or two—Male, aged 60–69 years
Many participants expressed a sense of unfairness and perceived social judgement towards people with overweight. For some, this created internal conflict as they sought to counter assumptions, while simultaneously berating themselves for a lack of self-discipline. Others viewed their own ill-health as a cause of weight gain, not a consequence of long-term overweight. Four male participants with physically demanding jobs associated being big with being strong.
All participants reported having lost weight at some point in life, citing general health concerns or body image as motivating factors. Organised diet programmes and meal replacement products were identified as helpful in achieving significant weight loss by six participants. Others preferred to self-manage, drawing on calorie reduction and exercise advice from a variety of sources. Repeat cycles of dieting and weight regain were common across the participants. Loss of motivation was frequently cited as precipitating weight regain, often associated with relaxing diet regimes around holidays or weddings. Only one participant maintained her weight loss in the long term, which coincided with significant changes in her lifestyle and personal relationships.
Body as victim, body as culprit illustrates participants’ experiences of managing weight in a body over which they did not feel fully in control. The body was seen as a victim of illness and ageing, with AF conceptualised as an external aggressor to be kept at bay through medication and management of risk factors. Conversely, the body could play the role of culprit in the struggle to achieve a healthy weight, being predisposed to weight gain by ‘genetic’ factors or childhood eating habits. Two participants described food as an addiction, experiencing bodily cravings which they lacked the psychological strength to overcome.
Broaching the subject
Broaching the subject explores participants’ perceptions of consultations where weight management was discussed (or not) and relates to opportunity and motivation within COM-B. Participants indicated they would be open to discussing their weight within the context of a clinical consultation, but perceived healthcare professionals were reluctant to engage in frank discussion. Only one participant knew that overweight is a risk factor for developing AF, and none was aware of evidence for weight-loss improving AF symptoms.10 11 Many reported doctors ‘mentioning’ their weight, which became repetitive and irritating when not accompanied by specific explanations of the health risks, or offers of help. A male participant whose weight had increased since retirement expressed frustration at a perceived lack of practical advice and support from healthcare professionals:
The trouble is, it’s all very well them saying “You should lose weight” but I couldn’t. You know it’s difficult to find proper sensible advice on how to do this. You know there are all these companies that set up but they’re in there to make money.—Male, aged 70–79 years
Many appeared to deny that their health might be damaged by their overweight having never been unequivocally told. When healthcare professionals broached weight management but omitted to refer patients to relevant services, patients sometimes interpreted that their weight was not yet a cause for concern and that behaviour change could be postponed. Some reported requesting help, but that the sort of help they wanted was not available. Preferences varied widely, from very low calorie meal replacements, dietician review, cognitive behavioural therapy to bariatric surgery. The profusion of conflicting weight management advice in the media and suspicions about commercial motivations of providers discouraged some participants from committing.
Only one participant reported having a meaningful conversation about weight with her cardiologist. As a healthcare professional who described her lifelong overweight as a source of shame and anxiety, she saw this conversation as positive and constructive, despite feeling confronted.
That was a good conversation. Quite a scary one but a good one in that respect because no-one’s actually said AF and weight—that’s the first. And also that’s the first time I’ve ever actually had that proper conversation about it—Female, aged 60–69 years
On discussion with participants of evidence linking weight loss with improvement in AF, all indicated this information would motivate them to persist with weight management.
Discussion
Summary of findings
This is the first qualitative study to explore the weight management experiences of people with AF and overweight. Interviews with 12 participants were analysed using a COM-B framework to illuminate factors affecting sustained weight management. The analysis identified three main themes: being out of rhythm; doing the right thing and broaching the subject. The interplay between the themes and the elements of COM-B (figure 1) highlights areas where improvements in service provision and communication could support patients to initiate and persist with healthy behaviour change.
Participants in this study appeared unaware of the potential benefits of weight loss to manage AF. Furthermore, while all participants recognised overweight as a general health risk, most failed to make the association with their own cardiac health. Those who recognised the general health risk of overweight expressed self-blame and anger as their perceived weakness and lack of self-control to sustain weight loss.
The role of COM-B
COM-B provided a guide for the interviews and analysis, creating a framework for better understanding behaviour change. In this study, participants reported having previously lost weight by changing their behaviour, thus demonstrating their capacity, opportunity and motivation to do so. The complexity of sustaining changes is reflected in their subsequent weight regain.
The focus on participants’ capabilities, opportunities and motivations uncovered various barriers to weight management including reduced physical activity due to AF symptoms, fear of damaging the heart, inadequate communication and support from healthcare professionals, knowledge gaps and lack of access to ‘trusted’ advice and weight management services. Identification of strategies to overcome these barriers could be guided by reference to the outer rings of the Behaviour Change Wheel,15 for example, education and enablement of patients with AF through cardiac rehabilitation provision.32
Participants had all lost weight
Somewhat unexpectedly, participants universally reported successful weight-loss efforts—although rarely sustained in the longer term. This in contrast to the commonly held assumption of healthcare professionals that people with overweight are non-compliant with recommended health behaviours.33 Indeed, research shows most people with overweight have tried or are trying to lose weight.34 Participants were demoralised by healthcare professionals’ failure to acknowledge weight loss, a finding consistent with previous studies of weight management.35
AF symptoms interfered with weight management
The experience of AF symptoms impacted on participants’ willingness to engage in regular exercise that might contribute to weight management. Concerns about damaging the heart are unfounded, indeed studies have shown physical exercise reduces AF burden and improves quality of life.36 Food was seen as a source of comfort during times of anxiety caused by AF symptoms, provoking resistance to weight management through calory-restriction alone. Several participants spoke of postponing weight-loss attempts until an anticipated future time when treatment would restore sinus rhythm. Advances in AF treatment are successfully restoring sinus rhythm in a greater number of patients,37 but to rely solely on medical intervention as the solution would be misplaced. It would seem patients need to become true partners in their care, but that will require greater candour in consultations about lifestyle change as a recommended strategy to improve AF and overall health.38
Participants did not associate AF with overweight
The findings indicate there were significant gaps in knowledge of AF risk factors. Reframing health communication to underscore the weight loss and AF message might serve to better motivate healthy behaviour change.
People who have experienced MI report fear of dying motivated subsequent weight-loss attempts.6–8 The participants who had experienced severe, sudden-onset AF described experiencing fear, vulnerability and disrupted self-image comparable with those who have had an MI. This fear did not translate into motivation to lose weight possibly because, unlike cardiovascular disease, AF is not widely associated with overweight in the public consciousness.39
Lack of awareness of the overweight-AF connection suggests communication of research findings is limited in consultations with patients. By comparison, a recent survey conducted at three hospitals in Belgium found nearly 70% (n=143) of participants were aware of the benefits of weight reduction for AF management.40 It would be valuable to examine if health messaging and advice are different and offer learning to enhance the content of consultations and/or pathways of care.
Getting the tone of weight conversations right is paramount
In common with the wider weight management literature,35 41 participants in this study wanted frank, non-judgemental discussion focused on the health impact of overweight, positive reinforcement of steps they were currently taking, and referral to weight-loss support services. Advice from healthcare professionals was seen as ‘trustworthy’ while commercial services were often viewed with suspicion.
Shame, vulnerability and stigma are widely reported by people with obesity.42 Perceptions that healthcare professionals judge patients negatively on the basis of their body size can be counterproductive to motivating engagement in weight management35 43 44 and may lead to avoidance of healthcare encounters.45 46 This may be amplified for people with AF in response to feelings of vulnerability due to symptoms; a finding in this study echoing others that explored the experiences of people living with AF.25 47
Healthcare professionals are encouraged to discuss weight opportunistically,48 but many participants in this, and other weight management studies,35 have little recollection of the subject being raised. Some participants interpreted this omission to mean their weight was not a concern, again supported in the literature.35 Patients expect healthcare professionals to discuss their weight when it is clinically relevant, and feel let down when they do not,41 a sentiment echoed by some participants in this study. Opportunistic ‘mentions’ of weight and what they perceived as poor quality information left participants feeling irritated and patronised, especially when not backed up by explanations of the impact of weight loss on their health, congruent with other studies.35 This dissonance between patient preferences and healthcare professionals’ interactions may be due to clinicians’ lack of skills when discussing weight management or fear of engendering a negative reaction.49
Almost all participants in this study, similar to others,35 indicated a willingness to be referred to weight management services. Referral to cardiac rehabilitation has been shown to be motivational to patients with cardiovascular disease and overweight.6 8 Explaining the evidence-based benefits of weight loss to improving AF symptoms, and providing a referral might go some way to addressing the absence of control described in this study. This may offer some agency over both the out of rhythm body and prognosis.
Limitations
This study reflects only the views of people who were willing to discuss weight management as those who were unwilling declined the invitation to participate. The sample was homogeneous—all participants identified as white British. This represented the demographic profile of patients treated for AF at the study centre, and may limit generalisability.
The study was conducted during the COVID-19 pandemic. Some participants noted that their responses to questions were affected by temporaneous restrictions placed on access to opportunities to exercise and socialise. COVID-19 social distancing precautions necessitated the use of telephone interviews for data capture. Historically, telephone interviews were considered inferior, but arguably they give control to the interviewee who is on their own territory.50 Telephone interviews provide visual anonymity, minimising perceived judgement based on physical appearance to which people living with overweight may be sensitised.35
Recommendations
The findings clearly identify the need to improve communication, particularly strengthening the signalling of important research-based evidence to patients where weight management might improve AF symptoms and disease progression. This message could be incorporated in face-to-face discussions in outpatient clinic, patient information leaflets or posters displayed in waiting areas accompanied by details of weight-loss services available through the hospital and in the community.
Locally and more widely, healthcare professionals may benefit from additional training to increase confidence and efficacy in discussing weight with patients. Future research could investigate health education behaviour change among healthcare professionals by applying COM-B to identify gaps in their capability, opportunity and motivation to intervene.
Weight management advice needs to be reinforced with a referral. Options available to clinicians are limited and tend to involve primary care referrals (eg, NHS Digital Weight Management Programme, commercial weight management programmes). Extending access to these schemes to secondary care teams, along with greater involvement of the multidisciplinary team, could provide another opportunity to support patients with weight management.
Conclusions
This study highlights the importance of sensitive and thoughtful weight management discussion with patients with AF and the importance of sharing research findings about weight loss as a means of reducing symptom burden and reversing disease progression. Patients appeared open to difficult conversations about weight within health consultations and expected professionals to address this topic candidly with them. Offering positive feedback on weight management efforts, providing reassurance about the effect of exercise on AF and offering a referral to appropriate services are all ways in which healthcare professionals can promote weight management behaviour change. Skills training to augment healthcare professionals’ confidence when discussing weight management may contribute to person-centred care within this population.
Supplementary Material
Acknowledgments
The authors would like to thank Dr Maria Clark for advice on use of the COM-B model. The authors would also like to thank Crad Allerton and Tony Elliott for providing patient and public involvement advice and Dr Kim Rajappan for providing clinical oversight.
Footnotes
Contributors: RWB: conceptualisation; methodology; investigation; data curation; writing, original draft; project administration; funding acquisition. CB: conceptualisation; methodology; writing, review and editing; supervision; guarantor. AET: conceptualisation; methodology; writing, review and editing; supervision.
Funding: This work was supported by Oxfordshire Health Services Research Committee (grant number 2020-1349).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the 'Methods' section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available in a public, open access repository. Data are available at University of Birmingham UBIRA eData repository with a CC-BY licence DOI: https://doi.org/10.25500/edata.bham.00000851.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Ethical approval was granted by London-Bromley Research Ethics Committee (20/LO/0356). The study was carried out in accordance with the Declaration of Helsinki and the principles of Good Clinical Practice. Written informed consent was obtained from all participants.
References
- 1.Powell-Wiley TM, Poirier P, Burke LE, et al. Obesity and cardiovascular disease: a scientific statement from the American heart association. Circulation 2021;143:e984–1010. 10.1161/CIR.0000000000000973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gomadam PS, Douglas CJ, Sacrinty MT, et al. Degree and direction of change of body weight in cardiac rehabilitation and impact on exercise capacity and cardiac risk factors. Am J Cardiol 2016;117:580–4. 10.1016/j.amjcard.2015.11.045 [DOI] [PubMed] [Google Scholar]
- 3.Ghosh S, Bouchard C. Convergence between biological, behavioural and genetic determinants of obesity. Nat Rev Genet 2017;18:731–48. 10.1038/nrg.2017.72 [DOI] [PubMed] [Google Scholar]
- 4.Garip G, Yardley L. A synthesis of qualitative research on overweight and obese people's views and experiences of weight management. Clin Obes 2011;1:110–26. 10.1111/j.1758-8111.2011.00021.x [DOI] [PubMed] [Google Scholar]
- 5.Greaves C, Poltawski L, Garside R, et al. Understanding the challenge of weight loss maintenance: a systematic review and synthesis of qualitative research on weight loss maintenance. Health Psychol Rev 2017;11:145–63. 10.1080/17437199.2017.1299583 [DOI] [PubMed] [Google Scholar]
- 6.Gallagher R, Kirkness A, Armari E, et al. Weight management issues and strategies for people with high cardiovascular risk undertaking an Australian weight loss program: a focus group study. Nurs Health Sci 2012;14:18–24. 10.1111/j.1442-2018.2011.00651.x [DOI] [PubMed] [Google Scholar]
- 7.Nadarajah S. A phenomenological study on lived experiences of PsychoSocio-Spiritual healing in cardiac rehabilitation patients, 2012. Available: http://hdl.handle.net/10713/2316
- 8.Kramer-Kile M. Diet projects: a study of cardiac rehabilitation participants engaged in changing dietary practices. Semantic Scholar, Corpus ID 149024773, 2013. [Google Scholar]
- 9.Andrade JG, Champagne J, Dubuc M, et al. Cryoballoon or radiofrequency ablation for atrial fibrillation assessed by continuous monitoring: a randomized clinical trial. Circulation 2019;140:1779–88. 10.1161/CIRCULATIONAHA.119.042622 [DOI] [PubMed] [Google Scholar]
- 10.Abed HS, Wittert GA, Leong DP, et al. Effect of weight reduction and cardiometabolic risk factor management on symptom burden and severity in patients with atrial fibrillation: a randomized clinical trial. JAMA 2013;310:2050–60. 10.1001/jama.2013.280521 [DOI] [PubMed] [Google Scholar]
- 11.Pathak RK, Middeldorp ME, Meredith M, et al. Long-term effect of goal-directed weight management in an atrial fibrillation cohort: a long-term follow-up study (legacy). J Am Coll Cardiol 2015;65:2159–69. 10.1016/j.jacc.2015.03.002 [DOI] [PubMed] [Google Scholar]
- 12.World Health Organisation . Obesity. Available: https://www.who.int/health-topics/obesity [Accessed 28 Jun 2021].
- 13.Cresswell J. Research Design Qualitative, Quantitative and Mixed Methods Approaches. 3rd Edition. Thousand Oaks, CA: SAGE, 2009: 3–21. [Google Scholar]
- 14.Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6:42. 10.1186/1748-5908-6-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Michie S, Atkins L, West R. The Behaviour Change Wheel: A Guide to Designing Interventions. London: Silverback Publishing, 2014. [Google Scholar]
- 16.Bradbury-Jones C, Taylor J, Herber O. How theory is used and articulated in qualitative research: development of a new typology. Soc Sci Med 2014;120:135–41. 10.1016/j.socscimed.2014.09.014 [DOI] [PubMed] [Google Scholar]
- 17.Thorne S, Jensen L, Kearney MH, et al. Qualitative metasynthesis: reflections on methodological orientation and ideological agenda. Qual Health Res 2004;14:1342–65. 10.1177/1049732304269888 [DOI] [PubMed] [Google Scholar]
- 18.McIntosh MJ, Morse JM. Situating and constructing diversity in semi-structured interviews. Glob Qual Nurs Res 2015;2:233339361559767. 10.1177/2333393615597674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mitchell G. Use of interviews in nursing research. Nurs Stand 2015;29:44–8. 10.7748/ns.29.43.44.e8905 [DOI] [PubMed] [Google Scholar]
- 20.Whiting LS. Semi-structured interviews: guidance for novice researchers. Nurs Stand 2008;22:35–40. 10.7748/ns2008.02.22.23.35.c6420 [DOI] [PubMed] [Google Scholar]
- 21.Dorian P, Cvitkovic SS, Kerr CR, et al. A novel, simple scale for assessing the symptom severity of atrial fibrillation at the bedside: the CCS-SAF scale. Can J Cardiol 2006;22:383–6. 10.1016/s0828-282x(06)70922-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.EuroQol Research Foundation . EuroQol EQ-5D-5L, 2017. Amsterdam. Available: https://euroqol.org/eq-5d-instruments/eq-5d-3l-about/
- 23.Ericsson K, Simon HA. Protocol Analysis: Verbal reports as data. Cambridge MA US: The MIT Press, 1993. [Google Scholar]
- 24.Bailey C, Kinghorn P, Orlando R. Using 'Think-Aloud' and interview data to explore patient and proxy completion of health and capability measures at the end of life. In: Coast J, ed. Qualitative methods for health economics. London, UK: Rowman & Littlefield, 2017: 231–44. [Google Scholar]
- 25.Zhang L, Gallagher R, Lowres N, et al. Using the 'Think Aloud' technique to explore quality of life issues during standard quality-of-life questionnaires in patients with atrial fibrillation. Heart Lung Circ 2017;26:150–6. 10.1016/j.hlc.2016.05.121 [DOI] [PubMed] [Google Scholar]
- 26.Carter N, Bryant-Lukosius D, DiCenso A, et al. The use of triangulation in qualitative research. Oncol Nurs Forum 2014;41:545–7. 10.1188/14.ONF.545-547 [DOI] [PubMed] [Google Scholar]
- 27.Peshkin A. In Search of subjectivity - One’s own. Educational Researcher 1988;17:17–21. 10.3102/0013189X017007017 [DOI] [Google Scholar]
- 28.Bradbury-Jones C. Enhancing rigour in qualitative health research: exploring subjectivity through Peshkin's I's. J Adv Nurs 2007;59:290–8. 10.1111/j.1365-2648.2007.04306.x [DOI] [PubMed] [Google Scholar]
- 29.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349–57. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- 30.Saldaña J. The coding manual for qualitative researchers. 3rd ed. Los Angeles: SAGE, 2015: 188–93. [Google Scholar]
- 31.Magnussen C, Niiranen TJ, Ojeda FM, et al. Sex differences and similarities in atrial fibrillation epidemiology, risk factors, and mortality in community cohorts. Circulation 2017;136:1588–97. 10.1161/CIRCULATIONAHA.117.028981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Williamson TM, Wilton S, Arena R. Abstract P215: a qualitative exploration of barriers and facilitators to a cardiac Rehabilitation-based weight loss program for patients with atrial fibrillation and obesity. Circulation 2022;145. [Epub ahead of print: Published first online 7 April 2022]. [Google Scholar]
- 33.Phelan SM, Burgess DJ, Yeazel MW. Obesity stigma and patient care. Obes Rev 2015;16:319–26. 10.1111/obr.12266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Piernas C, Aveyard P, Jebb SA. Recent trends in weight loss attempts: repeated cross-sectional analyses from the health survey for England. Int J Obes 2016;40:1754–9. 10.1038/ijo.2016.141 [DOI] [PubMed] [Google Scholar]
- 35.Ananthakumar T, Jones NR, Hinton L, et al. Clinical encounters about obesity: systematic review of patients' perspectives. Clin Obes 2020;10:e12347. 10.1111/cob.12347 [DOI] [PubMed] [Google Scholar]
- 36.Elliott AD, Mahajan R, Pathak RK, et al. Exercise training and atrial fibrillation. Circulation 2016;133:457–9. 10.1161/CIRCULATIONAHA.115.020800 [DOI] [PubMed] [Google Scholar]
- 37.Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur J Cardiothorac Surg 2016;50:e1–88. 10.1093/ejcts/ezw313 [DOI] [PubMed] [Google Scholar]
- 38.Dineen-Griffin S, Garcia-Cardenas V, Williams K, et al. Helping patients help themselves: a systematic review of self-management support strategies in primary health care practice. PLoS One 2019;14:e0220116. 10.1371/journal.pone.0220116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.American Heart Association . Who is at risk for atrial fibrillation? Available: https://www.heart.org/en/health-topics/atrial-fibrillation/who-is-at-risk-for-atrial-fibrillation-af-or-afib [Accessed 28 Jan 2021].
- 40.Delesie M, Desteghe L, Bertels M, et al. Motivation of overweight patients with atrial fibrillation to lose weight or to follow a weight loss management program: a cross-sectional study. Acta Cardiol 2021;76:494–503. 10.1080/00015385.2020.1848274 [DOI] [PubMed] [Google Scholar]
- 41.Malterud K, Ulriksen K. Obesity, stigma, and responsibility in health care: a synthesis of qualitative studies. Int J Qual Stud Health Well-being 2011;6. 10.3402/qhw.v6i4.8404. [Epub ahead of print: 22 11 2011]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ogden J, Clementi C. The experience of being obese and the many consequences of stigma. J Obes 2010;2010. 10.1155/2010/429098. [Epub ahead of print: 25 03 2010]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Albury C, Hall A, Syed A, et al. Communication practices for delivering health behaviour change conversations in primary care: a systematic review and thematic synthesis. BMC Fam Pract 2019;20:111. 10.1186/s12875-019-0992-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Williams O, Annandale E. Obesity, stigma and reflexive embodiment: Feeling the 'weight' of expectation. Health 2020;24:421–41. 10.1177/1363459318812007 [DOI] [PubMed] [Google Scholar]
- 45.Albury C, Strain WD, Brocq SL, et al. The importance of language in engagement between health-care professionals and people living with obesity: a joint consensus statement. Lancet Diabetes Endocrinol 2020;8:447–55. 10.1016/S2213-8587(20)30102-9 [DOI] [PubMed] [Google Scholar]
- 46.Ratansi Z. How to discuss weight loss with patients and provide ongoing support, 2020. GP. Available: https://www.gponline.com/discuss-weight-loss-patients-provide-ongoing-support/obesity/obesity/article/1669445
- 47.Stridsman M, Strömberg A, Hendriks J, et al. Patients' experiences of living with atrial fibrillation: a mixed methods study. Cardiol Res Pract 2019;2019:6590358. 10.1155/2019/6590358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.National Institute for Health and Care Excellence . Obesity prevention Clinical guideline [CG43]. London; 2015. https://www.nice.org.uk/guidance/cg43 [PubMed] [Google Scholar]
- 49.Dewhurst A, Peters S, Devereux-Fitzgerald A, et al. Physicians' views and experiences of discussing weight management within routine clinical consultations: a thematic synthesis. Patient Educ Couns 2017;100:897–908. 10.1016/j.pec.2016.12.017 [DOI] [PubMed] [Google Scholar]
- 50.Cachia M, Millward L. The telephone medium and semi‐structured interviews: a complementary fit. Qual Res Organ Manag 2011;6:265–77. 10.1108/17465641111188420 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-065995supp001.pdf (59.4KB, pdf)
bmjopen-2022-065995supp002.pdf (120.8KB, pdf)
Data Availability Statement
Data are available in a public, open access repository. Data are available at University of Birmingham UBIRA eData repository with a CC-BY licence DOI: https://doi.org/10.25500/edata.bham.00000851.