Abstract
Purpose of Review
Population aging is occurring worldwide, particularly in developed countries such as the United States (US). However, in the US, the population is aging more rapidly in rural areas than in urban areas. Healthy aging in rural areas presents unique challenges. Understanding and addressing those challenges is essential to ensure healthy aging and promote health equity across the lifespan and all geographies. This review aims to present findings and evaluate recent literature (2019–2022) on rural aging and highlight future directions and opportunities to improve population health in rural communities.
Recent Findings
The review first addresses several methodological considerations in measuring rurality, including the choice of measure used, the composition of each measure, and the limitations and drawbacks of each measure. Next, the review considers important concepts and context when describing what it means to be rural, including social, cultural, economic, and environmental conditions. The review assesses several key epidemiologic studies addressing rural–urban differences in population health among older adults. Health and social services in rural areas are then discussed in the context of healthy aging in rural areas. Racial and ethnic minorities, indigenous peoples, and informal caregivers are considered as special populations in the discussion of rural older adults and healthy aging. Lastly, the review provides evidence to support critical longitudinal, place-based research to promote healthy aging across the rural–urban divide is highlighted.
Summary
Policies, programs, and interventions to reduce rural–urban differences in population health and to promote health equity and healthy aging necessitate a context-specific approach. Considering the cultural context and root causes of rural–urban differences in population health and healthy aging is essential to support the real-world effectiveness of such programs, policies, and interventions.
Keywords: Rural health, Aging, Epidemiology, Social determinants
Introduction
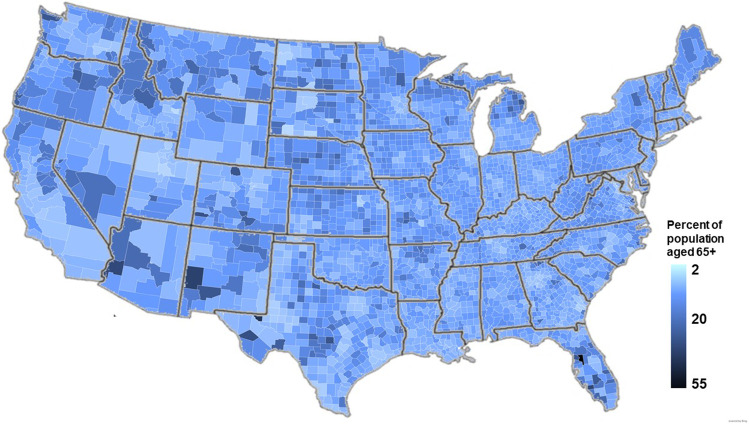
Rural environments present distinct challenges and opportunities for aging populations [1]. As population aging is occurring worldwide, especially in more developed countries such as the United States (US) and many European and East Asian countries [2], understanding current issues facing rural older adults is increasingly important to promote healthy aging. The number of people in the US aged 65 + increased by 54%, from 35 million or 12.4% of the population in 2000 [3] to 54 million or 16.9% of the population in 2022 [4]. Furthermore, although only 15% of the US population lives in “rural” areas, a disproportionate share of older Americans (22%) lives in rural areas (Fig. 1). A 2019 US Census Bureau report found that 17.5% of rural populations were aged 65 + , compared to 13.8% of urban populations [5]. Although the US population is aging in both rural and urban areas, over time, population aging, defined as the number and percent of the population aged 65 + , is occurring more rapidly in rural areas than in urban areas [6].
Fig. 1.
Percent of the population aged 65 + by county (source data: US Census 2020)
Understanding the unique challenges and dynamics of aging in rural communities is critically important to ensure healthy and successful aging and promote health equity across the rural–urban divide. Increasingly, place-based factors, including rurality, are being recognized as directly contributing to healthy aging and playing a vital role in promoting or precluding health equity. A recent study defined “successful aging” in the context of five domains: productivity and engagement, security, equity, cohesion, and well-being [7]. Study findings showed notable variability in successful aging across these domains over time and space, with higher levels of successful aging in more developed, urban regions.
There is, therefore, a critical need to identify and consider rural aging populations as a distinct population subgroup due to the unique cultural, socioeconomic, and health-related attributes inherent in these populations. The National Institute of Minority Health and Health Disparities considers rural populations a health disparity group, in part because these populations have higher rates of mental health concerns, chronic diseases, and worse general health outcomes than non-rural populations [8]. As a result, rural populations, particularly older adults, face elevated rates of morbidity, including obesity [9], diabetes [10, 11], coronary heart disease [12], and cancer [13], COVID-19 [14], as well as excess mortality [10, 13, 15]. Therefore, the review aims to present findings and evaluate recent literature, with a primary focus on research published over the past three years, on a breadth of issues related to aging in rural communities and propose potential future directions to improve population health and promote healthy aging in rural communities. This review focuses primarily on aging in rural communities in the US, drawing on relevant recent literature from other countries to compare and contrast evidence, as well as informing research, policy, and programs aimed at older adults in those rural communities in the US.
Defining Rurality: Methodological Considerations
To highlight the challenges and opportunities facing rural older adults, it is important to first define “rurality” in the context of health research. There is no universally accepted standard of what distinguishes “rural” areas from “urban” areas [16]. For example, the US Census Bureau [17] and the US Health Resources and Services Administration [18] define rural as an area that is not urban. However, most health research considers the concepts of “rural” and “urban” to be complex, multidimensional, and often context-specific [16, 19–22]. The choice of rurality measure influences which areas are classified as most rural or urban [23]. Furthermore, many measures are context-specific for defining “rural” or “urban [2], vary by region [16], and depend primarily on the geographic unit of measurement [24, 25]. In other words, rural communities are not all alike, and existing measures may not fully capture the characteristics that make a place rural. As a result, identified rural–urban associations with population health outcomes vary across region and cultural context [26], and are strongly dependent on the specific measure used [9, 20].
Multiple measures are available to characterize rural–urban status of communities in population health and aging research (Table 1), with the most commonly used measure being population density [27–33]. Often, population density is used as a log-transformed measure or ordinal measure, given the extreme right-skewed nature of the distribution of population density in the US. For example, in 2010, county-level population density ranged from less than 0.1 people per square mile in Yukon-Koyukuk Census Area (county equivalent) to 69,468.4 people per square mile in New York City, with a median county-level population density of just 45.0 people per square mile [4]. The percent of the population considered “urban” is another frequently used measure [34–36]. The US Census Bureau considers “urban” populations to be those located in Census-designated urbanized areas and places of at least 2500 inhabitants outside of urban areas [37]. In addition, distance to the nearest major metropolitan area or city is increasingly used to measure rurality and remoteness in studies of population health, aging, and development [38–40]. Other standard measures of rural–urban status used in health and aging research include several variables produced by the US Department of Agriculture, such as the Rural–Urban Continuum Codes (RUCC) [41, 42], Urban Influence Codes (UIC) [43, 44], and Rural–Urban Commuting Areas (RUCA) [23, 45–47]. However, there is substantial heterogeneity across the measures of rural–urban status [48] with respect to what each measure actually assesses and their associations with other population measures.
Table 1.
Summary of commonly used measures of rural–urban status in the epidemiologic and broader public health literature available on the county level for all US counties
| Measure of rural–urban status | Source | Variable type | Minimum- maximum | General distribution | Definition or description |
|---|---|---|---|---|---|
| Population density | Decennial US Census and American Community Survey | Continuous | < 0.01–69,468.4 per square mile | Highly right-skewed | County population size divided by county land area |
| Percent urban population | Decennial US Census and American Community Survey | Continuous | 0–100% | Right-skewed | US Census definition of percent of county population considered “urban” |
| Rural–Urban Continuum Code (RUCC) |
United States Department of Agriculture (USDA) latest: 2013 |
Ordinal | 1–12 | 12 levels with sub-levels |
Based on proximity of metropolitan statistical area and population size, designed as a continuum |
| Urban Influence Code (UCC) |
United States Department of Agriculture (USDA) latest: 2013 |
Ordinal | 1–9 | 9 levels with sub-levels | Based on the overall estimated economic influence of urban areas on counties and population size |
| Rural–Urban Commuting Area (RUCA) |
United States Department of Agriculture (USDA) latest: 2010 |
Ordinal | 1–10 | 10 levels with sub-levels | Based on a combination of population density, urbanization, and daily commuting time abstracted from the American Community Survey |
| Index of Relative Rurality |
Decennial US Census and American Community Survey (originally developed by researchers at Purdue University) |
Continuous | 0–1 | Nearly symmetric and approximately uniform | Composite scale of several component variables: (1.) population size, population density, percent urban population, and proximity to nearest metropolitan area |
Consider the percentage of the population age 65 + using county-level data from the 2020 US Decennial Census: although the percentage of the population age 65 + had a significant correlation (p < 0.001) with all measures of rural–urban status (population density, distance to nearest metropolitan area, RUCC, UIC, and RUCA), the strength of the Spearman correlation ranged from 0.34 for distance to the nearest metropolitan area to 0.53 for the percentage of the population considered non-urban. Aside from this heterogeneity, an important limitation of these measures is that they focus on only a limited number of characteristics related to rural–urban status (e.g., the influence of urban areas, commuting, etc.).
As a result of the heterogeneity among rural–urban measures used in epidemiologic studies, there is increasing interest in utilizing composite measures of rural–urban status that consider multiple aspects of rural or urban living in health research. One such measure is the Index of Relative Rurality (IRR) [49], which is calculated using population size, population density, distance to nearest metropolitan area, and percent urban population. The IRR has been used in several recent studies on health and aging, including health services utilization [50], geographic inequities in healthcare providers [51], availability of hospice care [52], opioid prescribing patterns [53], obesity [54], and COVID-19-related outcomes [55, 56].
Another consideration when assessing measures of urban–rural status is the geographic level to which rural–urban status is measured and contributes to barriers, challenges, and opportunities in population aging. Several recent studies have used the county as the geographic level on which rural–urban status is ascribed [57–60]. Other studies have examined rural–urban status as a predictor of health and health inequities at a finer geographic level, including zip code [61] and census tract [62]. There is increasing recognition that the influence of rurality on population health and aging is complex and varies based on the geographic unit of observation. Consequently, a recent analysis recommends that, where possible, associations between rural–urban status and health be examined using multilevel models to distinguish these potentially complex pathways [63]. As there is no universally accepted definition of “rural”, in this paper, we will include the results of studies that use an array of definitions of “rural” used in the public and population health, epidemiological, and gerontological literature, and will identify what levels of geography (e.g., state, county, census tract, etc. on which these results were obtained.
Defining Rurality: Concepts and Context
As described above, the concept of rurality is complex, context-specific, and challenging to measure. Common questions asked in population health and aging research are what specific attributes make a place rural and how do these attributes contribute to population health and healthy aging across the lifespan? There is extensive historical research on what attributes are considered when classifying a location as “rural” and “urban” in sociology and other social sciences [64–70]. However, disentangling the multifaceted individual attributes of rural or urban places that contribute to health and well-being is difficult; therefore, less is known to address the question of how community attributes impact health and aging.
There are three broad, but interconnected categories of attributes that often describe rural places: cultural, social, and environmental factors. Recent studies emphasize that rural culture plays a significant role in shaping rural landscapes, and vise versa. Consequently, culture can and does shape healthy aging in rural environments. Although it would be misleading to classify or view all rural cultures as being one under the umbrella term of a unified rural culture, it is important to recognize the cultural contributions (e.g., norms, values, traditions, perspectives, etc.) that shape rural cultures. The historical events (e.g., migration patterns, economic opportunities, collective hardships, etc.) help shape the culture of places as the people who live in the areas we understand them. As John Steinbeck wrote in Of Mice and Men, “How can we live without our lives? How will we know it’s us without our past?” The history of a place certainly defines the culture there, and can have profound, albeit indirect, influences on population health.
One of the longstanding cultural attributes of rural places within the US is the concept of “rugged individualism,” which values self-reliance over collectivism [71]. One consequence of rugged individualism on healthy aging is the resistance by many living in rural areas to government and communal interventions, which may undermine individual and policy responses to improve health and promote healthy aging at the population level [72, 73]. This was observed during the COVID-19 pandemic in terms of preventive behaviors, vaccinations, and COVID-19 outcomes and could be a contributing factor leading to worse health outcomes for rural populations in the US, particularly among older adults [73, 74]. Other cultural attributes in rural areas that influence healthy aging include an emphasis on kinship relationships and family preservation in the US and internationally [75, 76]. Cultural attributes, such as lower education levels and perceived toughness, are more common in rural areas and can lead to lower health literacy and increased stigma against mental health [77]. Stigma against mental health in rural areas has profound consequences for everyone across the lifespan, including older adults, such as resistance to recognizing essential mental health issues and cognitive decline [78], as well as refusal to access vital services to address these conditions [79, 80].
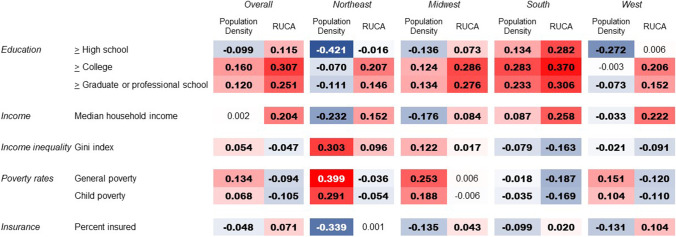
There is wide heterogeneity across the US and globally with respect to the social determinants of rural areas compared to more urban areas [81]. A correlational analysis of US Census tracts in 2020 using two measures of rural–urban status—population density and RUCA—and multiple measures of socioeconomic status showed a significant, positive correlation between rural–urban status measures and education (Fig. 2). However, the associations become less consistent for other social determinants—namely median household income—which was positively associated with RUCA codes, indicating urban areas were wealthier than rural areas, but not significantly associated with population density. Similar results were observed for poverty rates and percent insured: more rural areas fared better than urban areas when measured by RUCA, while urban areas fared better when using population density. Notably, there was substantial variability in the magnitude and direction of the associations both by the rural–urban status measure used (population density versus RUCA) and by US region.
Fig. 2.
Heat map of county-level Spearman correlations between two measures of rural–urban status (population density and Rural–Urban Commuting Area [RUCA]) and measures of social determinants, overall and by US Census region. Red and pink boxes indicate positive associations, and blue areas indicate negative associations. Boldface indicates statistically significant correlation. RUCAs are available from the US Department of Agriculture and are a composite measure of population density, urbanization, and daily commuting time abstracted from the American Community Survey
We can draw three important conclusions from these data. First, “rural” does not necessarily equate to having lower socioeconomic status. While there are indicators (e.g., education) indicating that rural areas generally have lower socioeconomic status than urban areas, even after accounting for the overall lower cost of living, there are other indicators (e.g., income and poverty) that are not correlated with rural–urban status or that indicate better socioeconomic conditions in rural areas than in urban ones. Second, there is clear geographic variability with respect to these correlations between social determinants and rural–urban status. Therefore, a one-size-fits-all approach or generalizing about all rural communities may limit the effectiveness of policies and programs designed to reduce rural–urban health inequities and promote healthy aging. Third, these findings emphasize the earlier discussion about the variability of the measurements used to assess rural–urban status. The lack of consistency between population density and RUCA in their associations with social determinants underscores the notion that many rural–urban differences in health and other factors depend heavily on the choice of rural–urban measurement.
The third broad category of attributes used to classify “rural” versus “urban” are environmental factors, which fall into two interrelated categories: the physical environment and the built environment. The physical environment consists of both the natural and the altered environment—the chemicals, radiation, and biological products that humans introduce into the environment [82], often through waste management, development, and agriculture. The US Environmental Protection Agency defines the “built environment” as all human-made or modified structures that facilitate everyday living, working, and recreation [83]. This would include roadways, buildings, sidewalks, infrastructure for water, sewage, and heating, and recreational spaces.
In rural communities, the physical environment is often, but not always, dominated by green space, agriculture, recreation, and natural green space, which has important implications for healthy aging [84]. It is important to emphasize that the relationships between physical environment and health among older adults are not always clear or linear, and at times, contradictory. For example, green space, including recreational spaces and natural features, may promote healthy aging by increasing perceived security and community social cohesion among older adults, which may lower stress and improve overall population health [85]. One study of an urban area determined that associations between self-reported health and green space were strongest when considering green space across a wide area (blocks, neighborhoods, and communities) surrounding one’s place of residence [86]. Two recent studies of older adults in China found a strong association between green space and self-reported general health, although the association was stronger in urban than rural areas [87, 88]. Declines in physical and mental health among older adults as a result of the COVID-19 pandemic-related safety measures were attenuated in populations with access to green space [89]. A US study of middle-aged adults found that residential areas with more green space were significantly associated with higher overall cognitive function, including faster thinking and better attention [90]. Despite these recent studies on the association between the natural environment and healthy aging, there is a relative paucity of longitudinal, life-course research examining the associations between green space and healthy aging in rural and urban contexts.
A limited number of studies have examined the altered environment's role in healthy aging in rural communities. Rural communities are more likely to depend upon agriculture to sustain the local economy, which has a significant impact on health and aging. Since 2019, numerous studies examining the impacts of agricultural and industrial waste on human health and aging among rural populations have been published, primarily in settings outside of the US, particularly in China [91–93], South Asia [94–96], and sub-Saharan Africa [97–100]. Agricultural waste, more common in rural than urban areas [101], contains multiple types of pollutants, including antibiotics [91, 93, 102], heavy metals [94, 103], ammonia [104], pesticides [96, 99], and many others. Furthermore, residents exposed to pollutants may not be aware of their risk [105]. Further complicating the health risks for older adults of perhaps unknown pollutants from agricultural waste is the location of landfills and other disposal sites in rural areas. It is increasingly evident that the location of these sources of pollution are likely to be situated in areas of lower socioeconomic status [106], and their locations disproportionately impact population health for disadvantaged populations [107]. There is comparatively less research on the temporal or longitudinal linkages between those chemical, radiological, and biological pollutants and their impacts on rural health and aging in the US than internationally. Given that in the US have a greater proportion of older adults are in rural areas than urban areas, and the plethora of mechanisms through which dangerous pollutants can impact health and increase the risk of disease, there is a crucial need to encourage research in this area.
As with research into the natural environment, recent research on the built environment and aging in rural areas of the US is sparse compared to international research [88, 108–116] and the built environment in urban areas of the US [117–119]. The degree to which the built environment affords the ability for people to walk and, more generally, move within a community without the use of other transportation methods [120], is an important, composite attribute of the built environment that impacts older adults’ ability to live and age successfully in both urban and rural communities [121•]. Recent research indicates that higher levels of walkability are associated with increased physical activity [121•, 122], and also allows for better social support [123–125], and reduced loneliness among older adults [123, 126]. Despite the more natural physical environment, rural areas have significantly lower walkability than urban areas [127•]. Walkability has been shown to be an independent risk factor for obesity and related cardiovascular disease (CVD) [128], which has substantial implications for the health of rural older adults.
Other aspects of the built environment directly or indirectly influence population health and healthy aging, including aging rural infrastructure [129, 130], availability of and access to basic health services [131•] and community supports [132], and perceived safety due to the physical infrastructure and surroundings [133]. Research on the built environment and healthy aging is limited, and is largely focused on urban areas in the US and in developed nations outside the US. That said, the existing research suggests a critical need to modify and improve aspects of the built environment, such as walkability and infrastructure (e.g., accessible sidewalks) to improve the ability of older adults to age successfully in rural areas and reduce rural–urban inequalities in health. Although there are practical and significant challenges with translating and adopting initiatives often developed for urban and suburban areas to those rural and under-resourced communities, doing so can positively impact rural aging to an even greater degree than urban areas [121•]. Future studies should examine multilevel factors—individual, neighborhood, and regional—and assess not only clinical measures of population health, but also sociocultural acceptance of modifications to the built environment by those populations most impacted [121•]. To increase the internal validity and strength of evidence, future research should use robust, longitudinal study designs and incorporate researchers, policymakers, and design experts [134].
Epidemiology of Aging and Health Conditions in Rural Areas
Diseases and conditions more prevalent in older populations include frailty, cognitive decline, disabilities, mobility, and falls, in addition to other broad categories of diseases, such as cancers, CVD, and some infectious diseases [135]. Alzheimer’s disease and related dementias (ADHD) are major areas of focus in the epidemiology of aging. A 2020 study using national data of Medicare beneficiaries found that rural residents with ADHD had significantly lower survival rates and spent significantly more time in nursing homes than urban residents with ADHD [136•]. Furthermore, rural residents were less likely than their urban counterparts to receive neuropsychological testing to detect early-onset ADHD, impacting their ability to seek treatment and care [137]. Recent studies also show that the incidence of falls [138] and mortality from falls [139] among older adults are more common in rural than urban areas. As described above, the built environment has important implications for reducing rural–urban inequalities in mobility among older adults [121•], but comprehensive recent research in this domain is lacking (Table 2).
Table 2.
Summary of key populations addressed and research domains where additional research is needed
| Key populations addressed | Domains in which additional research is needed |
|---|---|
| Racial and ethnic minorities in rural areas (e.g., African Americans, Hispanic/Latino/a/x populations) | Conduct longitudinal, life-course research examining the associations between green space and healthy aging in rural and urban contexts |
| Informal caregivers to rural older adults | Examine rural informal caregivers to older adults with Alzheimer’s disease and other dementias |
| Indigenous populations from rural regions (e.g., Native Americans, Alaska Natives, Native Hawaiians, First Nations) | Investigate temporal or longitudinal linkages between critical environmental hazards (e.g., chemical, radiological, and biological pollutants) and their impacts on rural health and aging |
| Institutionalized rural older adults (e.g., those living in nursing homes, assisted living facilities, etc.) | Identify and address systematic rural–urban differences in healthcare quality and access |
| Rural older adults with mental health issues | Obtain a more complete picture of population health and quality of life in rural areas by including clinical measures of population health and sociocultural acceptance of modifications that are made to the built environment |
| Assess what specific, multi-level (e.g., individual, neighborhood, community, etc.) attributes of rural living contribute to population health and rural–urban health disparities | |
| Identify and modify aspects of the built environment such as walkability and infrastructure (e.g., accessible sidewalks) to improve the ability of older adults to promote healthy aging in rural areas and reduce rural–urban health disparities | |
| Provide reliable, national or international data to researchers and policymakers on all aspects of health and quality of life in rural and urban areas |
Recent research indicates that rural areas also experience a higher incidence of cancer [140, 141] and lower survival rates for various types of cancer [142–144], which may be due, in part, to reduced access to preventive and screening services in rural areas [145] and increased distance and travel time to seek cancer treatment [42]. Rural–urban differences in the incidence and associated mortality of several infectious diseases among older adults are well documented in the recent literature, including pneumonia [146] and COVID-19 [147–149]. Differences in the risk of CVD and stroke by rural–urban status are pronounced. A 2022 study of Medicare beneficiaries showed that rural older adults had higher rates of hospitalization and mortality from ischemic stroke, myocardial infarctions, and thrombolysis [150]. These results corroborate findings from other recent studies [58, 151–153]. A 2019 study of CVD in Medicare beneficiaries found that rural older adults were more likely to be hospitalized from CVD with more severe disease than their urban counterparts [154•], which was supported by another study that found higher emergency department visits comparing rural to urban populations [155]. Together, these findings lead to another broad observation about rural–urban differences in health. Reducing these pervasive rural–urban inequalities across multiple diseases and chronic conditions requires addressing the root causes of the inequalities throughout the life course. These include, but are not limited to, addressing underlying socioeconomic determinants and environmental factors, and ensuring access to high-quality health services that result in better health outcomes on the population level for all rural and underserved populations [154•, 156].
Mental health issues, often unrelated to aging itself, pose unique challenges for older adults in rural areas. Suicidality, for example, has been a growing issue for older adults across the country over the past several decades and is more prevalent in rural areas [157]. The COVID-19 pandemic exacerbated rural–urban differences in suicidal ideation and attempts [158], particularly among older adults [159]. Effective and widescale screening for precursors of suicidal ideation and attempts are challenging, particularly in rural and remote areas. However, recent research into simple screening measures that can be implemented in primary care, whether in-person or through telemedicine appointments, such as the Ask Suicide Screening Questions toolkit, is both feasible and effective to use in the primary care setting [160, 161]. A pilot study conducted with rural, Appalachian older adults suggests that universal suicide screening tests would have wide acceptability among these populations and that primary care visits would be an effective setting to implement these programs [162]. Over the past several years, US-based research examining the epidemiology of other mental health conditions, such as depression, anxiety, and schizophrenia, among rural older adults or comparing rural and urban older adults is limited. Given the plethora of related rural–urban differences in other population health metrics and predictors, there is a clear need to encourage more detailed and comprehensive research in this area.
Health and Social Services: Access and Quality
As described earlier, access to high-quality health and healthcare services are key components of healthy aging. Recent studies have identified important structural barriers, such as a shortage of healthcare specialists and primary care providers in rural areas that likely contribute to the rural health disadvantage [163, 164]. An example is the relative lack of availability of cancer screening in rural areas compared to more urban areas [145, 165, 166]. Healthcare facilities in rural areas are more likely to be understaffed than comparable facilities in urban areas [51, 167]. When healthcare access is limited, differences in broadband access compared with urban areas likely contributed to the inability of many rural residents to seek health care when in-person care [168]. These differences were exacerbated during the peaks of the COVID-19 pandemic, particularly among older adults, when in-person healthcare was limited and telehealth appointments were often the only choice [169, 170].
Rural areas also experience reduced quality and availability of home and community-based services, including health care [171]. This inhibits older adults living with chronic diseases, cognitive decline, and disabilities from seeking needed services [172], and encourages the use of skilled nursing facilities over aging in place [173]. Although healthcare quality is multifaceted and often difficult to measure, several recent studies have identified rural–urban differences in the quality of healthcare services received after accounting for demographic factors and other social determinants [174]. However, the breadth of recent research on rural–urban differences in quality is limited. Systematic research is needed to quantify these differences to inform policies and interventions designed to improve healthcare equity across geographies.
Special Populations in Rural Areas
The rural population is heterogeneous with respect to socioeconomic, demographic, and cultural factors and should not be considered monolithic in research. There are important population subgroups that merit special attention when conducting research and designing evidence-based policies and interventions. Examples include racial and ethnic minorities, Native or Indigenous people, and informal caregivers for older adults. Although rural areas tend to have a greater proportion of White residents than urban areas, racial and ethnic minorities living in rural areas may experience aspects of rural culture differently than White residents. Prior studies have observed a rural race- and ethnicity-specific health “penalty”, where racial or ethnic disparities in health, health care, or healthcare quality are more severe in rural areas compared to urban areas [175, 176]. A recent study observed such a penalty, and found that differences between Hispanic/Latinx and non-Hispanic/Latinx Medicare beneficiaries were more pronounced in rural areas compared to urban areas. The researchers attributed this difference in part to lower cultural competency and poorer provider-patient communication in rural areas [177]. Another example is social isolation. A 2019 study showed that although White rural older adults reported less social isolation than their urban counterparts, the association was reversed among some racial and ethnic minorities, where rural Black older adults experienced significantly greater social isolation than urban Black older adults [178]. Another recent study found that the well-documented Black-White differences in obesity were significantly worse in rural areas compared to urban areas [54].
Indigenous people in rural areas in the US face unique cultural and technical barriers to healthy aging. These include barriers specific to rural America, barriers within the Indian Health Services system itself, and the limitations of services offered, leading to many health disparities for indigenous populations across the lifespan [179]. Henning-Smith and colleagues found that after adjusting for community-level covariates, the highest rates of premature deaths across the US were in those counties, with a majority of American Indian/Alaska Native residents located in rural areas [180]. Some conditions that created these disparities and barriers to healthy aging could be mitigated to improve health among indigenous populations. These include increasing incentives for indigenous people to enter the healthcare workforce, removing unnecessary barriers to seeking health care, and improving both the quality of and services offered through Indian Health Services, particularly in rural and remote regions and reservations [179, 181].
Informal caregivers—those who provide regular care or assistance to a friend or family member aged 65 + with a chronic health problem, disability, or cognitive decline—are another important population subgroup to consider in the context of aging in rural communities. Over 44 million adults are informal caregivers, representing an essential and often-overlooked component of the broader health care system, allowing older adults to age in place. Informal caregiving is estimated to save the US economy over $500 billion that would be spent on formal care and/or institutionalization of older adults [182]. Approximately one-quarter of all adults aged 45–64 are informal caregivers to older adults [183]. There is a limited amount of research on rural informal caregivers, however. Informal caregivers in rural areas reported geographic barriers such as transportation to provide care and a lack of social services offering caregiver support [184]. Rural informal caregivers provide higher levels of care than their urban counterparts, which has implications for their health and well-being [185]. Younger people are more likely to migrate from rural to urban areas due to a higher perceived likelihood of finding a skilled job with higher incomes and opportunities for advancement [186], which both increases the percent of the population aged 65 + [5] and decreases the pool of informal family caregivers.
In a 2020 study, Pedersen and colleagues raised important methodological issues when studying rural informal caregiving. These include sample size, data access, and how to accurately estimate rurality, as well as the critical need to study this vulnerable population to protect the health and well-being of rural informal caregivers and strengthen their ability to help older adults age successfully in place [187]. There is a clear tradeoff between using primary or secondary data to understand rural caregiving. While primary data collection can be designed to target and recruit rural caregivers and get detailed information about their experiences, limitations include the breadth of coverage and national representativeness of the sample, as well as sample size. Secondary data has the advantages of both a large sample size and national coverage, but recruitment may be biased toward those caregivers who provide less care than other caregivers, and are, therefore, more available to be part of a research study. Researchers using secondary data are limited by the variables already asked during the data collection [187] and may not have the validated and precise data needed to fully address critical research questions. Furthermore, although Alzheimer’s disease and related dementias disproportionately impact racial and ethnic minority groups, these populations and their caregivers have been historically underrepresented in research [188].
To gain a better understanding of the unique needs of rural caregivers, it is necessary to understand who they are, the unique barriers and challenges they face, how best to provide support for their health and well-being, and how to prepare them and informal caregivers for the continued growing population of older adults needing care, particularly in rural areas [189], as new research on rural informal caregivers is somewhat sparse. An example of ongoing data collection efforts specifically targeting geographic aspects of informal caregiving is the National Study of Caregiving (NSOC). NSOC is a national, longitudinal, multi-wave database that provides over 200 variables on all aspects of caregiving, including caregiver health, caregiver burden, activities related to caregiving, and detailed demographics. It is linked to the National Health and Aging Trends Study (NHATS), collectively providing over 500 variables about the caregiver and care recipient on many aspects of health, well-being, and caregiving [190]. Initiatives such as NHATS/NSOC and other databases such as the Health and Retirement Study offer promise to help address the questions of who rural caregivers are and what their needs are, but are still limited by the issues raised by Pedersen and colleagues [187].
Future Directions
This review highlighted recent research on a breadth of issues related to healthy aging in rural communities, emphasizing several practical and research-related challenges associated with studying these vulnerable populations. This body of research aims to reduce rural–urban disparities in population health and promote health equity across the lifespan, regardless of geographic and demographic characteristics, allowing all residents to age in place successfully. Achieving this goal is challenging for a number of reasons. First, not all rural areas are alike. There is substantial heterogeneity among areas categorized as rural with respect to demographics, culture, and population health [81]. Reducing rural–urban health disparities and promoting health equity and healthy aging requires a nuanced, context-specific approach. Policies, programs, and interventions working in one area may not work in all rural areas. Therefore, moving away from one-size-fits-all programs and policies may be more effective at improving health and well-being for rural older adults [191]. Second, there are data-related and methodological challenges in rural areas. Research in rural and remote places poses various challenges for recruitment and retention that often result in biased samples [187, 192]. Third, the complex nature of rural environments is challenging. It is difficult to identify and isolate what specific factors—cultural, socioeconomic, environmental, infrastructural, health systems, etc.—actually drive health disparities among older adults.
Critical to the success of these research endeavors is the development and implementation of evidence-based programs for older adults that consider the cultural context in which programs are implemented to create age-friendly communities across all geographies [193]. Evidence-based initiatives can provide needed information for key stakeholders, such as community leaders, policymakers, and funding agencies, to make informed decisions about populations most in need and which populations will benefit most from these initiatives. As discussed earlier, rural areas often have limited healthcare resources compared to urban and suburban areas. Therefore, programs designed to support healthy aging and aging in place in rural areas should complement traditional healthcare services and be readily available in the community [191]. In 2020, the World Health Organization made this a priority by emphasizing its commitment to supporting healthy aging across all communities through supporting age-friendly neighborhoods, increasing collaboration between community stakeholders, government officials, and residents, and making health care, in general, more friendly toward older adults [194]. They also acknowledged that this would require significant shifts in rural culture and a deep monetary commitment to support the implementation of evidence-based initiatives on a mass scale.
There is a clear and urgent need to identify factors contributing to rural–urban and other place-based disparities among older adults. This review provided some recent examples of rural–urban health disparities in mortality, obesity, and other aspects of health. The need to identify, understand, and address rural–urban disparities is particularly urgent because the rural health and mortality penalty has grown steadily and, until the 1970s, has reversed from an urban health and mortality penalty [195]. Pervasive and increasing rural–urban disparities in numerous health outcomes will likely change due to the depopulation and diversification of rural areas [196]. To effect change and promote healthy aging for all, regardless of place, it is crucial to recognize the multidimensional complexity of rural life and develop data, strategies, and initiatives to translate evidence-based research into effective, long-lasting policies.
Footnotes
This article is part of the Topical Collection on Epidemiology of Aging
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Skinner MW, Winterton R. Interrogating the contested spaces of rural aging: implications for research, policy, and practice. Gerontologist. 2018;58(1):15–25. doi: 10.1093/geront/gnx094. [DOI] [PubMed] [Google Scholar]
- 2.Glasgow N, Brown DL. Rural ageing in the United States: trends and contexts. J Rural Stud. 2012;28(4):422–431. doi: 10.1016/j.jrurstud.2012.01.002. [DOI] [Google Scholar]
- 3.Hetzel L, Smith A. Census 2000 Brief: The 65 years and over population: 2000. US Census Bureau. Website: https://www2.census.gov/library/publications/decennial/2000/briefs/c2kbr01-10.pdf. Accessed August 11, 2022.
- 4.US Census Bureau. Data Tools: Explore Census Data. Website: https://www.census.gov/data.html. Accessed August 11, 2022.
- 5.Smith AS, Trevelyan E. The older population in rural America: 2012–2016. Website: https://www.census.gov/content/dam/Census/library/publications/2019/acs/acs-41.pdf. Accessed August 11, 2022.
- 6.Pew Research Center, May 2018, What unites and divides urban, suburban and rural communities. Website: https://www.pewresearch.org/social-trends/wp-content/uploads/sites/3/2018/05/Pew-Research-Center-Community-Type-Full-Report-FINAL.pdf. Accessed August 15, 2022.
- 7.Rehkopf DH, Furstenberg FF, Elser H, Jackson C, Levy N, Rowe JW. Aging Society Research Network. A US state index of successful aging: differences between states and over time. Milbank Q. 2022;100(1):102–33. doi: 10.1111/1468-0009.12542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Academies of Sciences, Engineering, and Medicine. Communities in action: Pathways to health equity. National Academies Press, 2017. 10.17226/24624 [PubMed]
- 9.Cohen SA, Cook SK, Kelley L, Foutz JD, Sando TA. A closer look at rural-urban health disparities: associations between obesity and rurality vary by geospatial and sociodemographic factors. J Rural Health. 2017;33(2):167–179. doi: 10.1111/jrh.12207. [DOI] [PubMed] [Google Scholar]
- 10.Callaghan T, Ferdinand AO, Akinlotan MA, Towne SD, Jr, Bolin J. The changing landscape of diabetes mortality in the United States across region and rurality, 1999–2016. J Rural Health. 2020;36(3):410–415. doi: 10.1111/jrh.12354. [DOI] [PubMed] [Google Scholar]
- 11.O'Connor A, Wellenius G. Rural–urban disparities in the prevalence of diabetes and coronary heart disease. Public Health. 2012;126(10):813–820. doi: 10.1016/j.puhe.2012.05.029. [DOI] [PubMed] [Google Scholar]
- 12.Bossard M, Latifi Y, Fabbri M, Kurmann R, Brinkert M, Wolfrum M, Berte B, Cuculi F, Toggweiler S, Kobza R, Chamberlain AM. Increasing mortality from premature coronary artery disease in women in the rural United States. J Am Heart Assoc. 2020;9(9):e015334. doi: 10.1161/JAHA.119.015334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Garcia MC, Rossen LM, Bastia B, et al. Potentially excess deaths from the five leading causes of death in metropolitan and nonmetropolitan counties—United States, 2010–2017. MMWR. 2019;68(10):1–11. doi: 10.15585/mmwr.ss6810a1. [DOI] [PubMed] [Google Scholar]
- 14.Probst JC, Crouch EL, Eberth JM. COVID-19 risk mitigation behaviors among rural and urban community-dwelling older adults in summer, 2020. J Rural Health. 2021;37(3):473–478. doi: 10.1111/jrh.12600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Coughlin SS, Clary C, Johnson JA, Berman A, Heboyan V, Benevides T, Moore J, George V. Continuing challenges in rural health in the United States. J Environ Health Sci. 2019;5(2):90. [PMC free article] [PubMed] [Google Scholar]
- 16.Isserman AM. In the national interest: defining rural and urban correctly in research and public policy. Int Reg Sci Rev. 2005;28(4):465–499. doi: 10.1177/0160017605279000. [DOI] [Google Scholar]
- 17.Ratcliffe M, Burd C, Holder K, Fields A. Defining rural at the US Census Bureau. ACSGEO-1, US Census Bureau, Washington, DC, 2016., Available at: https://www2.census.gov/geo/pdfs/reference/ua/Defining_Rural.pdf. Accessed August 17, 2022.
- 18.US Health Resources and Services Administration. Defining rural population. Website: https://www.hrsa.gov/rural-health/about-us/what-is-rural. Accessed August 17, 2022.
- 19.Cohen SA, Greaney ML, Sabik NJ. Assessment of dietary patterns, physical activity and obesity from a national survey: rural-urban health disparities in older adults. PLoS One. 2018;13(12):e0208268. doi: 10.1371/journal.pone.0208268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Edwards MB, Matarrita-Cascante D. Rurality in leisure research: a review of four major journals. J Leis Res. 2011;43(4):447–474. doi: 10.1080/00222216.2011.11950245. [DOI] [Google Scholar]
- 21.Schaeffer PV, Kahsai MS, Jackson RW. Beyond the rural–urban dichotomy: essay in honor of Professor AM Isserman. Int Reg Sci Rev. 2013;36(1):81–96. doi: 10.1177/0160017612449981. [DOI] [Google Scholar]
- 22.Nelson KS, Nguyen TD, Brownstein NA, Garcia D, Walker HC, Watson JT, Xin A. Definitions, measures, and uses of rurality: a systematic review of the empirical and quantitative literature. J Rural Stud. 2021;1(82):351–365. doi: 10.1016/j.jrurstud.2021.01.035. [DOI] [Google Scholar]
- 23.Long JC, Delamater PL, Holmes GM. Which definition of rurality should I use?: The relative performance of 8 federal rural definitions in identifying rural-urban disparities. Med Care. 2021;59(10 Suppl 5):S413. doi: 10.1097/MLR.0000000000001612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pong RW, Pitblado JR. Don't take" geography" for granted! Some methodological issues in measuring geographic distribution of physicians. Can J Rural Med. 2001;6(2):103. [Google Scholar]
- 25.Shah TI, Milosavljevic S, Bath B. Measuring geographical accessibility to rural and remote health care services: challenges and considerations. Spat Spatio-Temporal Epidemiol. 2017;1(21):87–96. doi: 10.1016/j.sste.2017.04.002. [DOI] [PubMed] [Google Scholar]
- 26.Lund BC, Ohl ME, Hadlandsmyth K, Mosher HJ. Regional and rural–urban variation in opioid prescribing in the Veterans Health Administration. Mil Med. 2019;184(11–12):894–900. doi: 10.1093/milmed/usz104. [DOI] [PubMed] [Google Scholar]
- 27.Murray CJ, Kulkarni SC, Michaud C, Tomijima N, Bulzacchelli MT, Iandiorio TJ, Ezzati M. Eight Americas: investigating mortality disparities across races, counties, and race-counties in the United States. PLoS Med. 2006;3(9):e260. doi: 10.1371/journal.pmed.0030260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fassio O, Rollero C, De Piccoli N. Health, quality of life and population density: a preliminary study on “contextualized” quality of life. Soc Indic Res. 2013;110(2):479–488. doi: 10.1007/s11205-011-9940-4. [DOI] [Google Scholar]
- 29.Nayar P, Yu F, Apenteng BA. Frontier America's health system challenges and population health outcomes. J Rural Health. 2013;29(3):258–265. doi: 10.1111/j.1748-0361.2012.00451.x. [DOI] [PubMed] [Google Scholar]
- 30.Morris RD, Munasinghe RL. Geographic variability in hospital admission rates for respiratory disease among the elderly in the United States. Chest. 1994;106(4):1172–1181. doi: 10.1378/chest.106.4.1172. [DOI] [PubMed] [Google Scholar]
- 31.Tondo L, Albert MJ, Baldessarini RJ. Suicide rates in relation to health care access in the United States: an ecological study. J Clin Psychiatry. 2006;67(4):517–523. doi: 10.4088/JCP.v67n0402. [DOI] [PubMed] [Google Scholar]
- 32.Zahnd WE, Mueller-Luckey GS, Fogleman AJ, Jenkins WD. Rurality and health in the United States: do our measures and methods capture our intent? J Health Care Poor Underserved. 2019;30(1):70–79. doi: 10.1353/hpu.2019.0008. [DOI] [PubMed] [Google Scholar]
- 33.Wang Q, Wang X, Li R. Does population aging reduce environmental pressures from urbanization in 156 countries? Sci Total Environ. 2022;13:157330. doi: 10.1016/j.scitotenv.2022.157330. [DOI] [PubMed] [Google Scholar]
- 34.Herb J, Stitzenberg K, Holmes M. Comparative Analysis of Rural-Urban Definitions in Predicting Surgeon Workforce Supply. J Surg Res. 2022;1(270):341–347. doi: 10.1016/j.jss.2021.08.046. [DOI] [PubMed] [Google Scholar]
- 35.McCann SJ. State resident volunteering and health are unrelated when neuroticism is controlled: nomothetic evidence using the 50 states of the USA as analytical units. J Soc Psychol. 2020;160(5):702–718. doi: 10.1080/00224545.2020.1738991. [DOI] [PubMed] [Google Scholar]
- 36.Patel A, Gantz O, Zagadailov P, Merchant AM. The role of socioeconomic disparity in colorectal cancer stage at presentation. Updat Surg. 2019;71(3):523–531. doi: 10.1007/s13304-019-00632-5. [DOI] [PubMed] [Google Scholar]
- 37.US Census Bureau. The Urban and Rural Classifications. https://www2.census.gov/geo/pdfs/reference/GARM/Ch12GARM.pdf. Accessed October 17, 2022.
- 38.Guettabi M, Munasib A. is there a tradeoff between remote living and healthy living? The impact of remoteness on body weight. Rev Reg Stud. 2018;48(2):173–192. [Google Scholar]
- 39.Subramanyam N. A small improvement: small cities lag in expanding household water coverage across urban India. Water Policy. 2020;22(3):468–482. doi: 10.2166/wp.2020.116. [DOI] [Google Scholar]
- 40.Ross A, Clay LA. Capital assets and rural resilience: an analysis of Texas communities impacted by Hurricane Harvey. J Nat Resour Policy Res. 2018;8(1–2):154–186. doi: 10.5325/naturesopolirese.8.1-2.0154. [DOI] [Google Scholar]
- 41.Cossman RE, Cossman JS, Cosby AG, Reavis RM. Reconsidering the rural–urban continuum in rural health research: a test of stable relationships using mortality as a health measure. Popul Res Policy Rev. 2008;27(4):459–476. doi: 10.1007/s11113-008-9069-6. [DOI] [Google Scholar]
- 42.Segel JE, Lengerich EJ. Rural-urban differences in the association between individual, facility, and clinical characteristics and travel time for cancer treatment. BMC Public Health. 2020;20(1):1. doi: 10.1186/s12889-020-8282-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Okunseri CE, Okunseri E, Garcia RI, Visotcky A, Szabo A. Geographic variations in dental sealant utilization by Medicaid enrollees. J Public Health Dent. 2021;81(2):123–130. doi: 10.1111/jphd.12420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Upadhyay N, Rowan PJ, Aparasu RR, Balkrishnan R, Fleming ML, Nair AA, Chen H. Impact of geographic access to primary care providers on pediatric behavioral health screening. Prev Med. 2021;1(153):106856. doi: 10.1016/j.ypmed.2021.106856. [DOI] [PubMed] [Google Scholar]
- 45.Ondusko DS, Liu J, Hatch B, Profit J, Carter EH. Associations between maternal residential rurality and maternal health, access to care, and very low birthweight infant outcomes. J Perinatol. 2022;12:1–8. doi: 10.1038/s41372-022-01456-9. [DOI] [PubMed] [Google Scholar]
- 46.Kurani SS, Lampman MA, Funni SA, Giblon RE, Inselman JW, Shah ND, Allen S, Rushlow D, McCoy RG. Association between area-level socioeconomic deprivation and diabetes care quality in US primary care practices. JAMA Network Open. 2021;4(12):e2138438. doi: 10.1001/jamanetworkopen.2021.38438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gievers L, Khaki S, Dotson A, Chen Z, Macauley RC, Tolle S. Social determinants of health may predict end of life portable orders for life sustaining treatment form completion and treatment selections. Am J Hospice Palliat Med®. 2022;39(6):678–86. doi: 10.1177/10499091211041566. [DOI] [PubMed] [Google Scholar]
- 48.Cohen SA, Kelley L, Bell AE. Spatiotemporal discordance in five common measures of rurality for US counties and applications for health disparities research in older adults. Front Public Health. 2015;25(3):267. doi: 10.3389/fpubh.2015.00267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Waldorf BS. A continuous multidimensional measure of rurality: moving beyond threshold measures. 2006. No. 379–2016–21891). 10.22004/ag.econ.21383
- 50.Inagami S, Gao S, Karimi H, Shendge MM, Probst JC, Stone RA. Adapting the Index of Relative Rurality (IRR) to estimate rurality at the ZIP code level: a rural classification system in health services research. J Rural Health. 2016;32(2):219–227. doi: 10.1111/jrh.12148. [DOI] [PubMed] [Google Scholar]
- 51.Gemelas JC. Post-ACA trends in the US primary care physician shortage with index of relative rurality. J Rural Health. 2021;37(4):700–704. doi: 10.1111/jrh.12506. [DOI] [PubMed] [Google Scholar]
- 52.Svynarenko R, Lindley LC. Defining rurality in hospice research: evaluation of common measures. J Health Care Poor Underserved. 2021;32(4):2167. doi: 10.1353/hpu.2021.0189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sun F. Rurality and opioid prescribing rates in US counties from 2006 to 2018: A spatiotemporal investigation. Soc Sci Med. 2022;1(296):114788. doi: 10.1016/j.socscimed.2022.114788. [DOI] [PubMed] [Google Scholar]
- 54.Cohen SA, Nash CC, Byrne EN, Mitchell LE, Greaney ML. Black/white disparities in obesity widen with increasing rurality: evidence from a national survey. Health Equity. 2022;6(1):178–188. doi: 10.1089/heq.2021.0149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pro G, Gilbert PA, Baldwin JA, Brown CC, Young S, Zaller N. Multilevel modeling of county-level excessive alcohol use, rurality, and COVID-19 case fatality rates in the US. PLoS One. 2021;16(6):e0253466. doi: 10.1371/journal.pone.0253466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pro G, Schumacher K, Hubach R, Zaller N, Giano Z, Camplain R, Camplain C, Haberstroh S, Baldwin JA, Wheeler DL. US trends in mask wearing during the COVID-19 pandemic depend on rurality. Rural Remote Health. 2021;21(3):6596. doi: 10.22605/RRH6596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Daniel C, Aly S, Bae S, Scarinci I, Hardy C, Fouad M, Demark-Wahnefried W. Differences related to cancer screening by minority and rural/urban status in the Deep South: population-based survey results. J Cancer. 2021;12(2):474. doi: 10.7150/jca.49676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kamin Mukaz D, Dawson E, Howard VJ, Cushman M, Higginbotham JC, Judd SE, Kissela BM, Safford MM, Soliman EZ, Howard G. Rural/urban differences in the prevalence of stroke risk factors: a cross-sectional analysis from the REGARDS study. J Rural Health. 2022;38(3):668–673. doi: 10.1111/jrh.12608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Brooks MM, Mueller JT, Thiede BC. County reclassifications and rural–urban mortality disparities in the United States (1970–2018) Am J Public Health. 2020;110(12):1814–1816. doi: 10.2105/AJPH.2020.305895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zahnd WE, Gomez SL, Steck SE, Brown MJ, Ganai S, Zhang J, Arp Adams S, Berger FG, Eberth JM. Rural-urban and racial/ethnic trends and disparities in early-onset and average-onset colorectal cancer. Cancer. 2021;127(2):239–248. doi: 10.1002/cncr.33256. [DOI] [PubMed] [Google Scholar]
- 61.Clark AW, Durkin MJ, Olsen MA, Keller M, Ma Y, O’Neil CA, Butler AM. Rural–urban differences in antibiotic prescribing for uncomplicated urinary tract infection. Infect Control Hosp Epidemiol. 2021;42(12):1437–1444. doi: 10.1017/ice.2021.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Prochaska JD, Jupiter DC, Horel S, Vardeman J, Burdine JN. Rural-urban differences in estimated life expectancy associated with neighborhood-level cumulative social and environmental determinants. Prev Med. 2020;1(139):106214. doi: 10.1016/j.ypmed.2020.106214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zahnd WE, McLafferty SL, Eberth JM. Multilevel analysis in rural cancer control: a conceptual framework and methodological implications. Prev Med. 2019;1(129):105835. doi: 10.1016/j.ypmed.2019.105835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lobao L. A sociology of the periphery versus a peripheral sociology: rural sociology and the dimension of space: 1. Rural Sociol. 1996;61(1):77–102. doi: 10.1111/j.1549-0831.1996.tb00611.x. [DOI] [Google Scholar]
- 65.Jayapalan N. Rural sociology. Atlantic Publishers & Dist; 2002.
- 66.Riney-Kehrberg P, editor. The Routledge history of rural America. New York, NY: Routledge; 2016. [Google Scholar]
- 67.Walker AJ, Ryan RL. Place attachment and landscape preservation in rural New England: a Maine case study. Landsc Urban Plan. 2008;86(2):141–152. doi: 10.1016/j.landurbplan.2008.02.001. [DOI] [Google Scholar]
- 68.Rennison CM, Mondragon HP. Defining Rural. In: Research Methods for Rural Criminologists 2022;1–14. Routledge.
- 69.Williams AM, Cutchin MP. The rural context of health care provision. J Interprof Care. 2002;16(2):107–115. doi: 10.1080/13561820220124120. [DOI] [PubMed] [Google Scholar]
- 70.Thier M, Longhurst JM, Grant PD, Hocking JE. Research deserts: a systematic mapping review of us rural education definitions and geographies. J Res Rural Educ. 2021;37(2).
- 71.Bazzi S, Fiszbein M, Gebresilasse M. Frontier culture: the roots and persistence of “rugged individualism” in the United States. Econometrica. 2020;88(6):2329–2368. doi: 10.3982/ECTA16484. [DOI] [Google Scholar]
- 72.Eppard LM, Rank MR, Bullock HE, Bethlehem PA, Madigan T. Rugged individualism and the misunderstanding of American inequality. Sociol Viewpoints. 2020;34(1):134. [Google Scholar]
- 73.Bazzi S, Fiszbein M, Gebresilasse M. “Rugged individualism” and collective (in) action during the COVID-19 pandemic. J Public Econ. 2021;1(195):104357. doi: 10.1016/j.jpubeco.2020.104357. [DOI] [Google Scholar]
- 74.Watson MF, Bacigalupe G, Daneshpour M, Han WJ, Parra-Cardona R. COVID-19 interconnectedness: Health inequity, the climate crisis, and collective trauma. Fam Process. 2020;59(3):832–846. doi: 10.1111/famp.12572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Osokpo O, Riegel B. Cultural factors influencing self-care by persons with cardiovascular disease: an integrative review. Int J Nurs Stud. 2021;1(116):103383. doi: 10.1016/j.ijnurstu.2019.06.014. [DOI] [PubMed] [Google Scholar]
- 76.Greenfield PM, Brown G, Du H. Shifts in ecology, behavior, values, and relationships during the coronavirus pandemic: survival threat, subsistence activities, conservation of resources, and interdependent families. Curr Res Ecol Soc Psychol. 2021;1(2):100017. doi: 10.1016/j.cresp.2021.100017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Crumb L, Mingo TM, Crowe A. “Get over it and move on”: the impact of mental illness stigma in rural, low-income United States populations. Mental Health Prev. 2019;1(13):143–148. doi: 10.1016/j.mhp.2019.01.010. [DOI] [Google Scholar]
- 78.Knight BG, Winterbotham S. Rural and urban older adults’ perceptions of mental health services accessibility. Aging Ment Health. 2020;24(6):978–984. doi: 10.1080/13607863.2019.1576159. [DOI] [PubMed] [Google Scholar]
- 79.Morales DA, Barksdale CL, Beckel-Mitchener AC. A call to action to address rural mental health disparities. J Clin Transl Sci. 2020;4(5):463–467. doi: 10.1017/cts.2020.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Richman L, Pearson J, Beasley C, Stanifer J. Addressing health inequalities in diverse, rural communities: an unmet need. SSM-Popul Health. 2019;1(7):100398. doi: 10.1016/j.ssmph.2019.100398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kolak M, Bhatt J, Park YH, Padrón NA, Molefe A. Quantification of neighborhood-level social determinants of health in the continental United States. JAMA Netw Open. 2020;3(1):e1919928. doi: 10.1001/jamanetworkopen.2019.19928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.World Health Organization. Connecting global priorities: biodiversity and human health: a state of knowledge review. Website: https://apps.who.int/iris/bitstream/handle/10665/174012/9789241508537_eng.pdf. Accessed August 17, 2022.
- 83.United States Environmental Protection Agency. Basic information about the built environment. Website: https://www.epa.gov/smm/basic-information-about-built-environment#builtenviron. Accessed August 19, 2022.
- 84.De Vries S, Verheij RA, Groenewegen PP, Spreeuwenberg P. Natural environments—healthy environments? An exploratory analysis of the relationship between greenspace and health. Environ Plan A. 2003;35(10):1717–1731. doi: 10.1068/a35111. [DOI] [Google Scholar]
- 85.Hong A, Sallis JF, King AC, Conway TL, Saelens B, Cain KL, Fox EH, Frank LD. Linking green space to neighborhood social capital in older adults: the role of perceived safety. Soc Sci Med. 2018;1(207):38–45. doi: 10.1016/j.socscimed.2018.04.051. [DOI] [PubMed] [Google Scholar]
- 86.Reid CE, Kubzansky LD, Li J, Shmool JL, Clougherty JE. It's not easy assessing greenness: a comparison of NDVI datasets and neighborhood types and their associations with self-rated health in New York City. Health Place. 2018;1(54):92–101. doi: 10.1016/j.healthplace.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 87.Huang B, Huang C, Feng Z, Pearce JR, Zhao H, Pan Z, Liu Y. Association between residential greenness and general health among older adults in rural and urban areas in China. Urban For Urban Green. 2021;1(59):126907. doi: 10.1016/j.ufug.2020.126907. [DOI] [Google Scholar]
- 88.Zhang R, Liu S, Li M, He X, Zhou C. The effect of high-density built environments on elderly individuals’ physical health: a cross-sectional study in Guangzhou, China. Int J Environ Res Public Health. 2021;18(19):10250. doi: 10.3390/ijerph181910250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Levinger P, Cerin E, Milner C, Hill KD. Older people and nature: the benefits of outdoors, parks and nature in light of COVID-19 and beyond–where to from here? Int J Environ Health Res. 2022;32(6):1329–1336. doi: 10.1080/09603123.2021.1879739. [DOI] [PubMed] [Google Scholar]
- 90.Jimenez MP, Elliott EG, DeVille NV, Laden F, Hart JE, Weuve J, Grodstein F, James P. Residential green space and cognitive function in a large cohort of middle-aged women. JAMA Network Open. 2022;5(4):e229306. doi: 10.1001/jamanetworkopen.2022.9306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Meng T, Cheng W, Wan T, Wang M, Ren J, Li Y, Huang C. Occurrence of antibiotics in rural drinking water and related human health risk assessment. Environ Technol. 2021;42(5):671–681. doi: 10.1080/09593330.2019.1642390. [DOI] [PubMed] [Google Scholar]
- 92.Xue Y, Guo J, Li C, Xu X, Sun Z, Xu Z, Feng L, Zhang L. Influencing factors of farmers’ cognition on agricultural mulch film pollution in rural China. Sci Total Environ. 2021;15(787):147702. doi: 10.1016/j.scitotenv.2021.147702. [DOI] [Google Scholar]
- 93.Feng L, Cheng Y, Zhang Y, Li Z, Yu Y, Feng L, Zhang S, Xu L. Distribution and human health risk assessment of antibiotic residues in large-scale drinking water sources in Chongqing area of the Yangtze River. Environ Res. 2020;1(185):109386. doi: 10.1016/j.envres.2020.109386. [DOI] [PubMed] [Google Scholar]
- 94.Rudi NN, Muhamad MS, Te Chuan L, Alipal J, Omar S, Hamidon N, Hamid NH, Sunar NM, Ali R, Harun H. Evolution of adsorption process for manganese removal in water via agricultural waste adsorbents. Heliyon. 2020;6(9):e05049. doi: 10.1016/j.heliyon.2020.e05049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Memon QU, Wagan SA, Chunyu D, Shuangxi X, Jingdong L, Damalas CA. Health problems from pesticide exposure and personal protective measures among women cotton workers in southern Pakistan. Sci Total Environ. 2019;1(685):659–666. doi: 10.1016/j.scitotenv.2019.05.173. [DOI] [PubMed] [Google Scholar]
- 96.Kumar V, Kumar P. Pesticides in agriculture and environment: Impacts on human health. Contam Agric Environ: Health Risks Remediat. 2019;25(1):76–95. [Google Scholar]
- 97.Atinkut HB, Yan T, Arega Y, Raza MH. Farmers’ willingness-to-pay for eco-friendly agricultural waste management in Ethiopia: a contingent valuation. J Clean Prod. 2020;10(261):121211. doi: 10.1016/j.jclepro.2020.121211. [DOI] [Google Scholar]
- 98.Orisakwe OE, Frazzoli C, Ilo CE, Oritsemuelebi B. Public health burden of e-waste in Africa. J Health Pollut. 2019;9(22). [DOI] [PMC free article] [PubMed]
- 99.Bertrand PG. Uses and misuses of agricultural pesticides in Africa: neglected public health threats for workers and population. Pestic-Use Misuse Impact Environ. 2019
- 100.Adejumo IO, Adebiyi OA. Agricultural solid wastes: causes, effects, and effective management. Strateg Sustain Solid Waste Manag. 2020;15:8. [Google Scholar]
- 101.United States Environmental Protection Agency. Nonpoint Source: Agriculture. Website: https://www.epa.gov/nps/nonpoint-source-agriculture. Accessed August 18, 2022.
- 102.Chaturvedi P, Shukla P, Giri BS, Chowdhary P, Chandra R, Gupta P, Pandey A. Prevalence and hazardous impact of pharmaceutical and personal care products and antibiotics in environment: a review on emerging contaminants. Environ Res. 2021;1(194):110664. doi: 10.1016/j.envres.2020.110664. [DOI] [PubMed] [Google Scholar]
- 103.Sonone SS, Jadhav S, Sankhla MS, Kumar R. Water contamination by heavy metals and their toxic effect on aquaculture and human health through food Chain. Lett Appl NanoBioScience. 2020;10(2):2148–2166. doi: 10.33263/LIANBS102.21482166. [DOI] [Google Scholar]
- 104.Kuttippurath J, Singh A, Dash SP, Mallick N, Clerbaux C, Van Damme M, Clarisse L, Coheur PF, Raj S, Abbhishek K, Varikoden H. Record high levels of atmospheric ammonia over India: spatial and temporal analyses. Sci Total Environ. 2020;20(740):139986. doi: 10.1016/j.scitotenv.2020.139986. [DOI] [PubMed] [Google Scholar]
- 105.Yang T. Association between perceived environmental pollution and health among urban and rural residents-a Chinese national study. BMC Public Health. 2020;20(1):1. doi: 10.1186/s12889-020-8204-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Cannon C. Examining rural environmental injustice: an analysis of ruralness, class, race, and gender on the presence of landfills across the United States. J Rural Community Dev. 2020;15(1).
- 107.Mattiello A, Chiodini P, Bianco E, Forgione N, Flammia I, Gallo C, Pizzuti R, Panico S. Health effects associated with the disposal of solid waste in landfills and incinerators in populations living in surrounding areas: a systematic review. Int J Public Health. 2013;58(5):725–735. doi: 10.1007/s00038-013-0496-8. [DOI] [PubMed] [Google Scholar]
- 108.Hwang E, Brossoie N, Jeong JW, Song K. The impacts of the neighborhood built environment on social capital for middle-aged and elderly Koreans. Sustainability. 2021;13(2):756. doi: 10.3390/su13020756. [DOI] [Google Scholar]
- 109.Parida D, Khan RR, Lavanya KN. Urban built environment and elderly pedestrian accessibility: insights from South Asia. SN Soc Sci. 2022;2(6):1–21. doi: 10.1007/s43545-022-00391-y. [DOI] [Google Scholar]
- 110.Zheng Z, Liu W, Lu Y, Sun N, Chu Y, Chen H. the influence mechanism of community-built environment on the health of the elderly: from the perspective of low-income groups. [DOI] [PMC free article] [PubMed]
- 111.Tang S, Lee HF, Feng J. Social capital, built environment and mental health: a comparison between the local elderly people and the ‘laopiao’in urban China. Ageing Soc. 2022;42(1):179–203. doi: 10.1017/S0144686X2000077X. [DOI] [Google Scholar]
- 112.Fangfang H, Xiao H, Shuai Z, Qiong W, Jingya Z, Guodong S, Yan Z. Living environment, built environment and cognitive function among older chinese adults: results from a cross-sectional study. J Prev Alzheimer's Dis. 2022;9(1):126–135. doi: 10.14283/jpad.2021.59. [DOI] [PubMed] [Google Scholar]
- 113.Pan H, Liu Y, Chen Y. The health effect of perceived built environment on depression of elderly people in rural China: moderation by income. Health Soc Care Commun. 2021;29(1):185–193. doi: 10.1111/hsc.13081. [DOI] [PubMed] [Google Scholar]
- 114.Zhang Y, He Q, Wu W, Li C. Public transport use among the urban and rural elderly in China. J Transp Land Use. 2018;11(1):701–719. doi: 10.5198/jtlu.2018.978. [DOI] [Google Scholar]
- 115.Wu ZJ, Song Y, Wang HL, Zhang F, Li FH, Wang ZY. Influence of the built environment of Nanjing’s Urban Community on the leisure physical activity of the elderly: an empirical study. BMC Public Health. 2019;19(1):1–1. doi: 10.1186/s12889-019-7643-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Cleland C, Reis RS, Ferreira Hino AA, Hunter R, Fermino RC, Koller de Paiva H, Czestschuk B, Ellis G. Built environment correlates of physical activity and sedentary behaviour in older adults: a comparative review between high and low-middle income countries. Health Place. 2019;57:277–304. [DOI] [PubMed]
- 117.Black K, Jester DJ. Examining older adults’ perspectives on the built environment and correlates of healthy aging in an American age-friendly community. Int J Environ Res Public Health. 2020;17(19):7056. doi: 10.3390/ijerph17197056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Wang Z, Shepley MM. Can aging-in-place be promoted by the built environment near home for physical activity: a case study of non-Hispanic White elderly in Texas. J Housing Built Environ. 2018;33(4):749–766. doi: 10.1007/s10901-017-9584-z. [DOI] [Google Scholar]
- 119.Herbolsheimer F, Mahmood A, Michael YL, Chaudhury H. Everyday walking among older adults and the neighborhood built environment: a comparison between two cities in North America. Front Public Health. 2020;22(8):564533. doi: 10.3389/fpubh.2020.564533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Shields R, Gomes da Silva EJ, Lima e Lima T, Osorio N. Walkability: a review of trends. J Urban: Int Res Placemaking Urban Sustain. 2021;1:1–23.
- 121.Klann A, Vu L, Ewing M, Fenton M, Pojednic R. Translating urban walkability initiatives for older adults in rural and under-resourced communities. Int J Environ Res Public Health. 2019;16(17):3041. doi: 10.3390/ijerph16173041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Amagasa S, Inoue S, Fukushima N, Kikuchi H, Nakaya T, Hanibuchi T, Sallis JF, Owen N. Associations of neighborhood walkability with intensity-and bout-specific physical activity and sedentary behavior of older adults in Japan. Geriatr Gerontol Int. 2019;19(9):861–867. doi: 10.1111/ggi.13730. [DOI] [PubMed] [Google Scholar]
- 123.Lee JH, Tan TH. Neighborhood walkability or third places? Determinants of social support and loneliness among older adults. J Plan Educ Res. 2019;14:0739456X19870295.
- 124.Roy B, Hajduk AM, Tsang S, Geda M, Riley C, Krumholz HM, Chaudhry SI. The association of neighborhood walkability with health outcomes in older adults after acute myocardial infarction: The SILVER-AMI study. Prev Med Rep. 2021;1(23):101391. doi: 10.1016/j.pmedr.2021.101391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Zhu X, Yu CY, Lee C, Lu Z. From walkable communities to active lifestyles: Exploring causal pathways through a case study in Austin, Texas. J Plan Educ Res. 2020;26:0739456X19900528.
- 126.Lam J, Wang S. Built environment and loneliness among older adults in South East Queensland Australia. J Appl Gerontol. 2022;8:07334648221114345. doi: 10.1177/07334648221114345. [DOI] [PubMed] [Google Scholar]
- 127.Watson KB, Whitfield GP, Thomas JV, Berrigan D, Fulton JE, Carlson SA. Associations between the national walkability index and walking among US adults—National Health Interview Survey, 2015. Preventive Med. 2020;137:106122. doi: 10.1016/j.ypmed.2020.106122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Lang IM, Antonakos CL, Judd SE, Colabianchi N. A longitudinal examination of objective neighborhood walkability, body mass index, and waist circumference: the REasons for Geographic And Racial Differences in Stroke study. Int J Behav Nutr Phys Act. 2022;19(1):1–5. doi: 10.1186/s12966-022-01247-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Herrmann VS. Rural ruins in America’s climate change story: Photojournalism, perception, and agency in Shishmaref, Alaska. Ann Am Assoc Geogr. 2019;109(3):857–874. [Google Scholar]
- 130.Verma I, Taegen J. Access to services in rural areas from the point of view of older population—a case study in Finland. Int J Environ Res Public Health. 2019;16(23):4854. doi: 10.3390/ijerph16234854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.van Hoof J, Marston HR, Kazak JK, Buffel T. Ten questions concerning age-friendly cities and communities and the built environment. Build Environ. 2021;15(199):107922. doi: 10.1016/j.buildenv.2021.107922. [DOI] [Google Scholar]
- 132.Zhang X, Warner ME, Wethington E. Can age-friendly planning promote equity in community health across the rural-urban divide in the US? Int J Environ Res Public Health. 2020;17(4):1275. doi: 10.3390/ijerph17041275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Bonaccorsi G, Manzi F, Del Riccio M, Setola N, Naldi E, Milani C, Giorgetti D, Dellisanti C, Lorini C. Impact of the built environment and the neighborhood in promoting the physical activity and the healthy aging in older people: an umbrella review. Int J Environ Res Public Health. 2020;17(17):6127. doi: 10.3390/ijerph17176127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Moore TH, Kesten JM, López-López JA, Ijaz S, McAleenan A, Richards A, Gray S, Savović J, Audrey S. The effects of changes to the built environment on the mental health and well-being of adults: systematic review. Health Place. 2018;1(53):237–257. doi: 10.1016/j.healthplace.2018.07.012. [DOI] [PubMed] [Google Scholar]
- 135.Izquierdo M, Merchant RA, Morley JE, Anker SD, Aprahamian I, Arai H, Aubertin-Leheudre M, Bernabei R, Cadore EL, Cesari M, Chen LK. International exercise recommendations in older adults (ICFSR): expert consensus guidelines. J Nutr Health Aging. 2021;25(7):824–853. doi: 10.1007/s12603-021-1665-8. [DOI] [PubMed] [Google Scholar]
- 136.Rahman M, White EM, Thomas KS, Jutkowitz E. Assessment of rural-rrban differences in health care use and survival among medicare beneficiaries with Alzheimer disease and related Dementia. JAMA Network Open. 2020;3(10):e2022111. doi: 10.1001/jamanetworkopen.2020.22111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Xu WY, Jung J, Retchin SM, Li Y, Roy S. Rural-urban disparities in diagnosis of early-onset dementia. JAMA Network Open. 2022;5(8):e2225805. doi: 10.1001/jamanetworkopen.2022.25805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Moreland B, Kakara R, Henry A. Trends in nonfatal falls and fall-related injuries among adults aged≥ 65 years—United States, 2012–2018. Morb Mortal Wkly Rep. 2020;69(27):875. doi: 10.15585/mmwr.mm6927a5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Burns E, Kakara R. Deaths from falls among persons aged≥ 65 years—United States, 2007–2016. Morb Mortal Wkly Rep. 2018;67(18):509. doi: 10.15585/mmwr.mm6718a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Yu L, Sabatino SA, White MC. Peer reviewed: rural–urban and racial/ethnic disparities in invasive cervical cancer incidence in the United States, 2010–2014. Preventing Chronic Disease. 2019;16. [DOI] [PMC free article] [PubMed]
- 141.Sealy-Jefferson S, Roseland ME, Cote ML, Lehman A, Whitsel EA, Mustafaa FN, Booza J, Simon MS. Rural–urban residence and stage at breast cancer diagnosis among postmenopausal women: the Women's Health Initiative. J Womens Health. 2019;28(2):276–283. doi: 10.1089/jwh.2017.6884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Afshar N, English DR, Milne RL. Rural–urban residence and cancer survival in high-income countries: a systematic review. Cancer. 2019;125(13):2172–2184. doi: 10.1002/cncr.32073. [DOI] [PubMed] [Google Scholar]
- 143.Clarke JA, Despotis AM, Ramirez RJ, Zevallos JP, Mazul AL. Head and neck cancer survival disparities by race and rural–urban context Rural–urban survival disparities by race. Cancer Epidemiol, Biomarkers Prev. 2020;29(10):1955–61. doi: 10.1158/1055-9965.EPI-20-0376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Obeng-Gyasi S, Timsina L, Bhattacharyya O, Fisher CS, Haggstrom DA. Breast cancer presentation, surgical management and mortality across the rural–Urban Continuum in the National Cancer Database. Ann Surg Oncol. 2020;27(6):1805–1815. doi: 10.1245/s10434-020-08376-y. [DOI] [PubMed] [Google Scholar]
- 145.Chandak A, Nayar P, Lin G. Rural-urban disparities in access to breast cancer screening: A spatial clustering analysis. J Rural Health. 2019;35(2):229–235. doi: 10.1111/jrh.12308. [DOI] [PubMed] [Google Scholar]
- 146.Kosar CM, Loomer L, Ferdows NB, Trivedi AN, Panagiotou OA, Rahman M. Assessment of rural-urban differences in postacute care utilization and outcomes among older US adults. JAMA Netw Open. 2020;3(1):e1918738. doi: 10.1001/jamanetworkopen.2019.18738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Peters DJ. Community susceptibility and resiliency to COVID-19 across the rural-urban continuum in the United States. J Rural Health. 2020;36(3):446–456. doi: 10.1111/jrh.12477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Sun Y, Cheng KJ, Monnat SM. Rural-urban and within-rural differences in COVID-19 mortality rates. J Rural Soc Sci. 2022;37(2):3. [Google Scholar]
- 149.Iyanda AE, Boakye KA, Lu Y, Oppong JR. Racial/ethnic heterogeneity and rural-urban disparity of COVID-19 case fatality ratio in the USA: a negative binomial and GIS-based analysis. J Racial Ethn Health Disparities. 2022;9(2):708–721. doi: 10.1007/s40615-021-01006-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Loccoh EC, Joynt Maddox KE, Wang Y, Kazi DS, Yeh RW, Wadhera RK. Rural-urban disparities in outcomes of myocardial infarction, heart failure, and stroke in the United States. J Am Coll Cardiol. 2022;79(3):267–279. doi: 10.1016/j.jacc.2021.10.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Khan MS, Kumar P, Sreenivasan J, Khan SU, Nasir K, Mehra MR, O’Donnell C, Warraich HJ. Rural-urban differences in mortality from ischemic heart disease, heart failure, and stroke in the United States. Circ: Cardiovasc Qual Outcome. 2021;14(4):e007341. [DOI] [PMC free article] [PubMed]
- 152.Aggarwal R, Chiu N, Loccoh EC, Kazi DS, Yeh RW, Wadhera RK. Rural-urban disparities: diabetes, hypertension, heart disease, and stroke mortality among black and white adults, 1999–2018. J Am Coll Cardiol. 2021;77(11):1480–1481. doi: 10.1016/j.jacc.2021.01.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Cross SH, Mehra MR, Bhatt DL, Nasir K, O’Donnell CJ, Califf RM, Warraich HJ. Rural-urban differences in cardiovascular mortality in the US, 1999–2017. JAMA. 2020;323(18):1852–1854. doi: 10.1001/jama.2020.2047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Singh GM, Becquart N, Cruz M, Acevedo A, Mozaffarian D, Naumova EN. Spatiotemporal and demographic trends and disparities in cardiovascular disease among older adults in the United States based on 181 million hospitalization records. J Am Heart Assoc. 2019;8(21):e012727. doi: 10.1161/JAHA.119.012727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Greenwood-Ericksen MB, Kocher K. Trends in emergency department use by rural and urban populations in the United States. JAMA Netw Open. 2019;2(4):e191919. doi: 10.1001/jamanetworkopen.2019.1919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Butkus R, Rapp K, Cooney TG, Engel LS, Health and Public Policy Committee of the American College of Physicians*. Envisioning a better US health care system for all: reducing barriers to care and addressing social determinants of health. Ann Intern Med. 2020;172(2_Supplement):S50–9. [DOI] [PubMed]
- 157.Arbore P. Suicide prevention among rural older adults. Generations. 2019;43(2):62–65. [Google Scholar]
- 158.Monteith LL, Holliday R, Brown TL, Brenner LA, Mohatt NV. Preventing suicide in rural communities during the COVID‐19 pandemic. J Rural Health. 2020. [DOI] [PMC free article] [PubMed]
- 159.Troutman-Jordan M, Kazemi DM. COVID-19's impact on the mental health of older adults: increase in isolation, depression, and suicide risk. An urgent call for action: Public health nursing; 2020. [DOI] [PubMed] [Google Scholar]
- 160.LeCloux MA, Weimer M, Culp SL, Bjorkgren K, Service S, Campo JV. The feasibility and impact of a suicide risk screening program in rural adult primary care: a pilot test of the ask suicide-screening questions toolkit. Psychosomatics. 2020;61(6):698–706. doi: 10.1016/j.psym.2020.05.002. [DOI] [PubMed] [Google Scholar]
- 161.Christensen-LeCloux M, Weimer M, Bjorkgren K, Booker W, Campo JV. Universal suicide risk screening: views of rural adults on acceptability and implementation in primary care. Gen Hosp Psychiatry. 2021;1(71):102–107. doi: 10.1016/j.genhosppsych.2021.03.009. [DOI] [PubMed] [Google Scholar]
- 162.Horowitz LM, Snyder DJ, Boudreaux ED, He JP, Harrington CJ, Cai J, Claassen CA, Salhany JE, Dao T, Chaves JF, Jobes DA. Validation of the ask suicide-screening questions for adult medical inpatients: a brief tool for all ages. Psychosomatics. 2020;61(6):713–722. doi: 10.1016/j.psym.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Chen X, Orom H, Hay JL, Waters EA, Schofield E, Li Y, Kiviniemi MT. Differences in rural and urban health information access and use. J Rural Health. 2019;35(3):405–417. doi: 10.1111/jrh.12335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Johnston KJ, Wen H, Joynt Maddox KE. Lack of access to specialists associated with mortality and preventable hospitalizations of rural Medicare beneficiaries. Health Aff. 2019;38(12):1993–2002. doi: 10.1377/hlthaff.2019.00838. [DOI] [PubMed] [Google Scholar]
- 165.Odahowski CL, Zahnd WE, Eberth JM. Challenges and opportunities for lung cancer screening in rural America. J Am Coll Radiol. 2019;16(4):590–595. doi: 10.1016/j.jacr.2019.01.001. [DOI] [PubMed] [Google Scholar]
- 166.Zgodic A, Zahnd WE, Advani S, Eberth JM. Low-dose CT lung cancer screening uptake: A rural–urban comparison. J Rural Health. 2022;38(1):40–53. doi: 10.1111/jrh.12568. [DOI] [PubMed] [Google Scholar]
- 167.Smith JG, Plover CM, McChesney MC, Lake ET. Isolated, small, and large hospitals have fewer nursing resources than urban hospitals: implications for rural health policy. Public Health Nurs. 2019;36(4):469–477. doi: 10.1111/phn.12612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Khairat S, Haithcoat T, Liu S, Zaman T, Edson B, Gianforcaro R, Shyu CR. Advancing health equity and access using telemedicine: a geospatial assessment. J Am Med Inform Assoc. 2019;26(8–9):796–805. doi: 10.1093/jamia/ocz108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Hirko KA, Kerver JM, Ford S, Szafranski C, Beckett J, Kitchen C, Wendling AL. Telehealth in response to the COVID-19 pandemic: Implications for rural health disparities. J Am Med Inform Assoc. 2020;27(11):1816–1818. doi: 10.1093/jamia/ocaa156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Henning-Smith C. The unique impact of COVID-19 on older adults in rural areas. J Aging Soc Policy. 2020;32(4–5):396–402. doi: 10.1080/08959420.2020.1770036. [DOI] [PubMed] [Google Scholar]
- 171.Fong MC, Russell D, Gao O, Franzosa E. Contextual forces shaping home-based healthcare services between 2010 and 2020: Insights from the social-ecological model and organizational theory. Gerontologist. 2022. [DOI] [PMC free article] [PubMed]
- 172.Siconolfi D, Shih RA, Friedman EM, Kotzias VI, Ahluwalia SC, Phillips JL, Saliba D. Rural-urban disparities in access to home-and community-based services and supports: stakeholder perspectives from 14 states. J Am Med Dir Assoc. 2019;20(4):503–508. doi: 10.1016/j.jamda.2019.01.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Coburn AF, Ziller EC, Paluso N, Thayer D, Talbot JA. Long-term services and supports use among older Medicare beneficiaries in rural and urban areas. Res Aging. 2019;41(3):241–264. doi: 10.1177/0164027518824117. [DOI] [PubMed] [Google Scholar]
- 174.Kang Y, Tzeng HM, Zhang T. Rural disparities in hospital patient satisfaction: multilevel analysis of the Massachusetts AHA, SID, and HCAHPS data. J Patient Experience. 2020;7(4):607–614. doi: 10.1177/2374373519862933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Cossman J, James W, Wolf JK. The differential effects of rural health care access on race-specific mortality. SSM-Popul Health. 2017;1(3):618–623. doi: 10.1016/j.ssmph.2017.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.James W, Cossman JS. Long-term trends in Black and White mortality in the rural United States: evidence of a race-specific rural mortality penalty. J Rural Health. 2017;33(1):21–31. doi: 10.1111/jrh.12181. [DOI] [PubMed] [Google Scholar]
- 177.Martino SC, Elliott MN, Hambarsoomian K, Weech-Maldonado R, Tamayo L, Gaillot S, Haviland AM. Disparities in care experienced by older Hispanic Medicare beneficiaries in urban and rural areas. Med Care. 2022;60(1):37–43. doi: 10.1097/MLR.0000000000001667. [DOI] [PubMed] [Google Scholar]
- 178.Henning-Smith C, Moscovice I, Kozhimannil K. Differences in social isolation and its relationship to health by rurality. J Rural Health. 2019;35(4):540–549. doi: 10.1111/jrh.12344. [DOI] [PubMed] [Google Scholar]
- 179.Cromer KJ, Wofford L, Wyant DK. Barriers to healthcare access facing American Indian and Alaska Natives in rural America. J Community Health Nurs. 2019;36(4):165–187. doi: 10.1080/07370016.2019.1665320. [DOI] [PubMed] [Google Scholar]
- 180.Henning-Smith CE, Hernandez AM, Hardeman RR, Ramirez MR, Kozhimannil KB. Rural counties with majority black or indigenous populations suffer the highest rates of premature death in the US. Health Aff. 2019;38(12):2019–2026. doi: 10.1377/hlthaff.2019.00847. [DOI] [PubMed] [Google Scholar]
- 181.Loh IH, Trude AC, Setiono F, Redmond L, Jock B, Gittelsohn J. Dietary Intake of Upper Midwest and Southwest Native American Adults. Ecol Food Nutr. 2020;59(5):486–505. doi: 10.1080/03670244.2020.1752685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Chari AV, Engberg J, Ray KN, Mehrotra A. The opportunity costs of informal elder-care in the United States: new estimates from the American Time Use Survey. Health Serv Res. 2015;50(3):871. doi: 10.1111/1475-6773.12238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Centers for Disease Control and Prevention. Caregiving for family and friends: a public health issue. Website: https://www.cdc.gov/aging/agingdata/docs/caregiver-brief-508.pdf. Accessed August 19, 2022.
- 184.Gibson A, Holmes SD, Fields NL, Richardson VE. Providing care for persons with dementia in rural communities: informal caregivers’ perceptions of supports and services. J Gerontol Soc Work. 2019;62(6):630–648. doi: 10.1080/01634372.2019.1636332. [DOI] [PubMed] [Google Scholar]
- 185.Cohen SA, Ahmed N, Brown MJ, Meucci MR, Greaney ML. Rural-urban differences in informal caregiving and health-related quality of life. J Rural Health. 2022;38(2):442–456. doi: 10.1111/jrh.12581. [DOI] [PubMed] [Google Scholar]
- 186.Vazzana CM, Rudi-Polloshka J. Appalachia has got talent, but why does it flow away? A study on the determinants of brain drain from rural USA. Econ Dev Q. 2019;33(3):220–233. doi: 10.1177/0891242419844320. [DOI] [Google Scholar]
- 187.Pedersen DE, Minnotte KL, Ruthig JC. Challenges of using secondary data to study rural caregiving within the United States. Sociol Inq. 2020;90(4):955–970. doi: 10.1111/soin.12364. [DOI] [Google Scholar]
- 188.Gilmore-Bykovskyi AL, Jin Y, Gleason C, Flowers-Benton S, Block LM, Dilworth-Anderson P, Barnes LL, Shah MN, Zuelsdorff M. Recruitment and retention of underrepresented populations in Alzheimer's disease research: a systematic review. Alzheimer's Dement: Transl Res Clin Interv. 2019;1(5):751–770. doi: 10.1016/j.trci.2019.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.National Alliance for Caregiving. Caregiving in rural America. Website: https://www.caregiving.org/wp-content/uploads/2020/05/Easter-Seals_NAC_Caregiving_in_Rural.pdf. Accessed August 19, 2022.
- 190.National Health and Aging Trends Study (NHATS) User Guide, July 2022. Website: https://www.nhats.org/sites/default/files/2022-07/NHATS_User_Guide_R11_Beta_Release.pdf. Accessed August 19, 2022.
- 191.Smith ML, Towne SD, Jr, Herrera-Venson A, Cameron K, Horel SA, Ory MG, Gilchrist CL, Schneider EC, DiCocco C, Skowronski S. Delivery of fall prevention interventions for at-risk older adults in rural areas: findings from a national dissemination. Int J Environ Res Public Health. 2018;15(12):2798. doi: 10.3390/ijerph15122798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Watson NL, Mull KE, Heffner JL, McClure JB, Bricker JB. Participant recruitment and retention in remote eHealth intervention trials: methods and lessons learned from a large randomized controlled trial of two web-based smoking interventions. J Med Internet Res. 2018;20(8):e10351. doi: 10.2196/10351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Kim K, Buckley TD, Burnette D, Huang J, Kim S. Age-friendly communities and older adults’ health in the United States. Int J Environ Res Public Health. 2022;19(15):9292. doi: 10.3390/ijerph19159292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Rudnicka E, Napierała P, Podfigurna A, Męczekalski B, Smolarczyk R, Grymowicz M. The World Health Organization (WHO) approach to healthy ageing. Maturitas. 2020;1(139):6–11. doi: 10.1016/j.maturitas.2020.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.James W, Cossman J, Wolf JK. Persistence of death in the United States: the remarkably different mortality patterns between America’s Heartland and Dixieland. Demogr Res. 2018;1(39):897–910. doi: 10.4054/DemRes.2018.39.33. [DOI] [Google Scholar]
- 196.Jensen L, Monnat SM, Green JJ, Hunter LM, Sliwinski MJ. Rural population health and aging: toward a multilevel and multidimensional research agenda for the 2020s. Am J Public Health. 2020;110(9):1328. doi: 10.2105/AJPH.2020.305782. [DOI] [PMC free article] [PubMed] [Google Scholar]