Abstract
Background:
Existing literature suggests that using stigmatizing language may promote negative attitudes and result in more punitive views toward individuals with addiction. It is unclear how the commonly used colloquial terms to describe opioid-exposed mother infant dyads impacts public opinion of pregnant women with opioid use disorder (OUD). We sought to examine the extent to which language such as “opioid addict” and “born addicted” influences the perception of pregnant women with OUD.
Methods:
We conducted a randomized case-based vignette study using a population-weighted sample of parents living in Tennessee, varying in the language used to describe an opioid-exposed mother infant dyad. Participant demographics, views on opioid prescribing, and opinions on criminal justice and child welfare responses following delivery were obtained. Ordinal logistic regression was used to examine the association between vignette type and punitive responses.
Results:
Eleven hundred participants completed the survey. Overall, 30.6% felt the mother should be arrested and 68.6% felt the mother should lose custody of her infant. There was insufficient evidence to suggest a difference in punitive response selection based on the vignette language (p = 0.27). In the adjusted model, the odds of answering a more punitive response among parents who received non-stigmatizing language was 0.8 (95% CI 0.59–1.08) compared to parents who received stigmatizing language in the vignette.
Conclusions:
Many parents hold punitive views toward mothers receiving OUD treatment that was not altered by using less value-laden language. Broader stigma-reduction interventions may be more effective.
Keywords: Stigma, perinatal, parenting, opioid use disorder, child welfare, punitive, language
Introduction
In response to the increasing rate of opioid use disorder (OUD) among pregnant women, states have implemented policies ranging from prioritizing access to treatment to criminalizing substance use in pregnancy.1–5 Between 2014 and 2016, Tennessee became the first state in the United States to enact a law allowing for the prosecution of pregnant women using non-prescribed substances, creating one of the most restrictive statutes toward pregnant women with substance use disorder in the country.6,7 Media coverage of the Tennessee law and other articles about the opioid epidemic in the perinatal period frequently used the terms “pregnant addict” and “addicted baby” to describe opioid-exposed mother-infant dyads.8–11 Existing literature suggests that using stigmatizing language, such as the term “addict,” may promote negative attitudes and result in more punitive views toward individuals with addiction.12–15 It is unclear how the Tennessee law and coverage by the media shaped public opinion of pregnant and parenting women with OUD.
In this context, we sought to understand public perception of pregnant women with OUD and how language referring to addiction may influence public opinion. We conducted a randomized survey experiment among a population-weighted sample of parents with children <18 years old, differing only in the terminology used to describe opioid-exposed mother-infant dyads. We hypothesized that using stigmatizing language would result in greater support for criminal justice and child welfare response than when using more appropriate terminology.
Methods
The Vanderbilt Child Health Poll was conducted by Ipsos using an online platform called KnowledgePanel, a large research panel created by using probability-based address sampling of US households16,17 and additional online panels from Ipsos. Families included in KnowledgePanel or other panels living in Tennessee were invited in September 2019 to participate in larger survey around child health policy (focused on the well-being of children living in Tennessee, health insurance coverage, opioid use, and behavioral health).18 Respondents were required to have at least one child under the age of 18 who lived in the same household. The survey was completed in English and had a median completion time of 10 min. Individuals received an email invitation to complete the poll online at their convenience and non-responders were sent frequent reminders. Ipsos provided participating households with Internet access and computer hardware if needed. Polling took place between October–November of 2019. Participants received a small incentive and entry into a larger raffle with both prizes and cash awards. Sampling continued until there was a large enough sample for the responses to be deemed representative of Tennessee families. Survey weights were created to provide state-wide estimates for parents with children <18 years old and to account for differential non-response bias.
Participants were presented with a case vignette of a mother with OUD who becomes pregnant, receives treatment, and whose infant requires treatment for neonatal opioid withdrawal. Vignettes were randomized to differ only in the description of mother (“opioid addict” v. “woman with opioid use disorder”) and baby (“born addicted” v. “develops drug withdrawal”), as follows:
Ms. Lee is a 23-year-old woman who [is an opioid addict/has an opioid use disorder] who becomes pregnant. During her pregnancy she gets treatment for her [addiction/opioid use disorder], and her infant is [born addicted/develops drug withdrawal]. Her infant stays in the hospital for two weeks for treatment and is now ready to be sent home with plans for medical follow-ups for both Ms. Lee and the baby.
Participants were asked if the mother should be arrested, not be arrested but have her infant placed in foster care or with a family member, or if the infant should be allowed to return to home in the mother’s custody. Demographic data collected on participants included parent age, gender, education, race/ethnicity, marital status, household income, mother head of household (yes/no), employment status, homeowner status, and number of children <18 years old. Additionally, participants were asked about their views on opioids including frequency of prescribing, personal connection to someone suffering from addiction, and worry about addiction among their children as well as children in the state of Tennessee.
We summarized the characteristics of the sample and responses on infant discharge disposition using descriptive statistics, comparing the groups by vignette using Rao–Scott corrected Chi-square tests. We used ordinal logistic regression to examine the extent to which vignette type, characteristics, and views on opioids were associated with post-delivery custody responses from least (parental custody) to moderate (lose parental custody but not arrest) to most (arrest) punitive. All analyses were conducted in R version 3.6.2 (R Core Team, Vienna, Austria) using survey weights to permit population-level inferences. Hierarchical variable clustering using Spearman’s ρ2 was performed to assess for collinearity. As a sensitivity analysis, final model was run without survey to assess whether any main results differ. The Vanderbilt University Medical Center Institutional Review Board reviewed this study and deemed it exempt from full review.
Results
There were 1,100 participants who completed the survey. We observed no statistically significant differences in parent characteristics or prior views and experiences with opioids when stratified by vignette language at the α = 0.05 level (Table 1). There was no evidence to suggest a significant difference in punitive response selection based only on the vignette language (p = 0.27). In the combined sample, 30.6% (95% CI 26.9–34.2%) responded that the mother should be arrested and have her infant placed into foster care or with a family member; 38.0% (95% CI 34.1–42.0%) responded that the mother should not be arrested but have her infant placed into foster care or with a family member; and 31.4% (95% CI 27.5–35.2%) responded that the infant should be allowed to return home with the mother (Table 2). The results from our adjusted model (Figure 1) indicate that the odds of answering a more punitive response among parents who received non-stigmatizing language (“use disorder”) were 0.8 (95% CI 0.59–1.08) times those of parents who saw stigmatizing language (“addicted”) in the vignette. Parents who felt opioids are prescribed too frequently in TN were significantly more likely to answer a more punitive response (aOR 1.5; 95% CI 1.06–2.07).
Table 1.
Participant characteristics and views on opioids and opioid prescribing, by vignette received and overall.
| Type of vignette received | ||||
|---|---|---|---|---|
| Parent demographics | “Addict” and “born addicted” (N = 555) | “Use disorder” and “develops drug withdrawal” (N = 545) | Combined (N = 1100) | p-Value |
| Number of children <18 | ||||
| 1 | 47.7% (41.9, 53.4) | 40.5% (34.8, 46.2) | 43.9% (39.9, 48.0) | p = 0.17 |
| 2 | 33.9% (28.6, 39.2) | 36.5% (31.0, 42.0) | 35.3% (31.4, 39.1) | |
| 3 or more | 18.5% (14.4, 22.5) | 23.0% (18.1, 27.9) | 20.8% (17.6, 24.1) | |
| Age | ||||
| Age | 38.4 (37.3, 39.4) | 38.6 (37.6, 39.6) | 38.5 (37.8, 39.2) | p = 0.29 |
| Gender | ||||
| Female | 60.3% (54.4, 66.2) | 53% (47.2, 58.9) | 56.5% (52.3, 60.7) | p = 0.09 |
| Male | 39.7% (33.8, 45.6) | 47% (41.1, 52.8) | 43.5% (39.3, 47.7) | |
| Highest education | ||||
| HS or less | 37.5% (31.8, 43.1) | 36.3% (30.6, 42.1) | 36.9% (32.8, 40.9) | p = 0.78 |
| Some college | 31.9% (26.9, 36.9) | 30.3% (25.4, 35.3) | 31.1% (27.6, 34.6) | |
| Bachelor or higher | 30.6% (25.3, 36.0) | 33.3% (27.8, 38.8) | 32.0% (28.2, 35.9) | |
| Race/Ethnicity | ||||
| White, Non-Hispanic | 71.4% (65.8, 77.0) | 76.3% (71.1, 81.5) | 73.9% (70.1, 77.8) | p = 0.21 |
| All others | 28.6% (23.0, 34.2) | 23.7% (18.5, 28.9) | 26.1% (22.2, 29.9) | |
| Marital status | ||||
| Married | 68.0% (62.7, 73.3) | 73.8% (69.2, 78.4) | 71.1% (67.5, 74.6) | p = 0.10 |
| Unmarried | 32.0% (26.7, 37.3) | 26.2% (21.6, 30.8) | 28.9% (25.4, 32.5) | |
| Household income | ||||
| Less than $25,000 | 14.2% (11.4, 17.1) | 12.3% (9.7, 14.8) | 13.2% (11.3, 15.1) | p = 0.58 |
| $25,000-$49,999 | 21.5% (17.6, 25.3) | 20.7% (16.9, 24.6) | 21.1% (18.3, 23.8) | |
| $50,000 or more | 64.3% (59.5, 69.1) | 67% (62.3, 71.7) | 65.7% (62.4, 69.1) | |
| Mother head of household | ||||
| Yes | 46.2% (40.6, 51.8) | 40.2% (34.7, 45.6) | 43.1% (39.2, 46.9) | p = 0.13 |
| No | 53.8% (48.2, 59.4) | 59.8% (54.4, 65.3) | 56.9% (53.1, 60.8) | |
| Employment status | ||||
| Working | 75.6% (71.4, 79.7) | 81.0% (77.1, 84.8) | 78.4% (75.6, 81.2) | p = 0.06 |
| Not working | 24.4% (20.3, 28.6) | 19.0% (15.2, 22.9) | 21.6% (18.8, 24.4) | |
| Homeowner status | ||||
| Owned by you or someone in your household | 64.6% (59.4, 69.9) | 72.0% (67.3, 76.8) | 68.5% (65.0, 72.0) | p = 0.06 |
| Rented | 31.1% (26.1, 36.0) | 25.6% (21.0, 30.2) | 28.2% (24.9, 31.6) | |
| Occupied w/out rent payment | 4.3% (1.6, 7.1) | 2.3% (1.2, 3.4) | 3.3% (1.8, 4.7) | |
| Type of home | ||||
| One-family house | 79.8% (75.6, 84.1) | 84% (80.2, 87.8) | 82% (79.1, 84.8) | p = 0.30 |
| Apartment building | 11.9% (8.2, 15.6) | 8.8% (5.8, 11.7) | 10.3% (7.9, 12.6) | |
| Other (mobile home, boat, RV, van, etc.) | 8.3% (5.9, 10.7) | 7.2% (4.7, 9.8) | 7.7% (6.0, 9.5) | |
| Opioids are prescribed too frequently in TN | ||||
| Agree | 67.8% (62.4, 73.2) | 72.9% (68.0, 77.7) | 70.4% (66.8, 74.0) | p = 0.2 |
| Disagree | 32.2% (26.8, 37.6) | 27.1% (22.3, 32.0) | 29.5% (25.9, 33.2) | |
| Worry about TN children/teenagers becoming addicted to opioids | ||||
| Agree | 76.3% (71.4, 81.1) | 80.2% (75.7, 84.7) | 78.3% (75.0, 81.6) | p = 0.27 |
| Disagree | 23.7% (18.8, 28.6) | 19.8% (15.3, 24.3) | 21.7% (18.4, 25.0) | |
| Worry about my child becoming addicted to opioids | ||||
| Agree | 33.0% (27.2, 38.6) | 30.3% (25.0, 35.6) | 31.5% (27.7, 35.4) | p = 0.51 |
| Disagree | 67.0% (61.4, 72.6) | 69.7% (64.4, 75.0) | 68.4% (64.5, 72.3) | |
| Do you personally know someone who has [developed an addiction] to opioids? | ||||
| No | 42.8% (37.1, 48.4) | 42.1% (36.3, 47.9) | 42.4% (38.4, 46.5) | p = 0.88 |
| Yes | 57.2% (51.6, 62.9) | 57.9% (52.1, 63.7) | 57.6% (53.5, 61.6) | |
| Was person able to get into treatment for the addiction? | ||||
| No | 35.2% (28.3, 42.1) | 36.8% (30.0, 43.5) | 36% (31.2, 40.9) | p = 0.75 |
| Yes | 64.8% (57.9, 71.7) | 63.2% (56.5, 70.0) | 64% (59.1, 68.8) | |
Table 2.
Participant views on parental criminal justice and child welfare custody decisions by type of vignette received and overall.
| Vignette type | |||
|---|---|---|---|
| Criminal justice and child welfare questions of interest | “Opioid addict” (N = 555) | “Opioid use disorder” (N = 545) | Combined (N = 1100) |
| Ms. Lee should be arrested and have her infant placed into foster care or with a family member (proportion, 95% CI) | 32.1% (26.8, 37.3) | 29.2% (24.1, 34.3) | 30.6% (26.9, 34.2) |
| Ms. Lee should be not be arrested, but have her infant placed into foster care or with a family member | 39.8% (34.1, 45.4) | 36.4% (31.0, 41.9) | 38.0% (34.1, 42.0) |
| Ms. Lee should be not be arrested and be allowed to return home with her infant | 28.2% (23.2, 33.2) | 34.3% (28.6, 40.0) | 31.4% (27.5, 35.2) |
Figure 1.
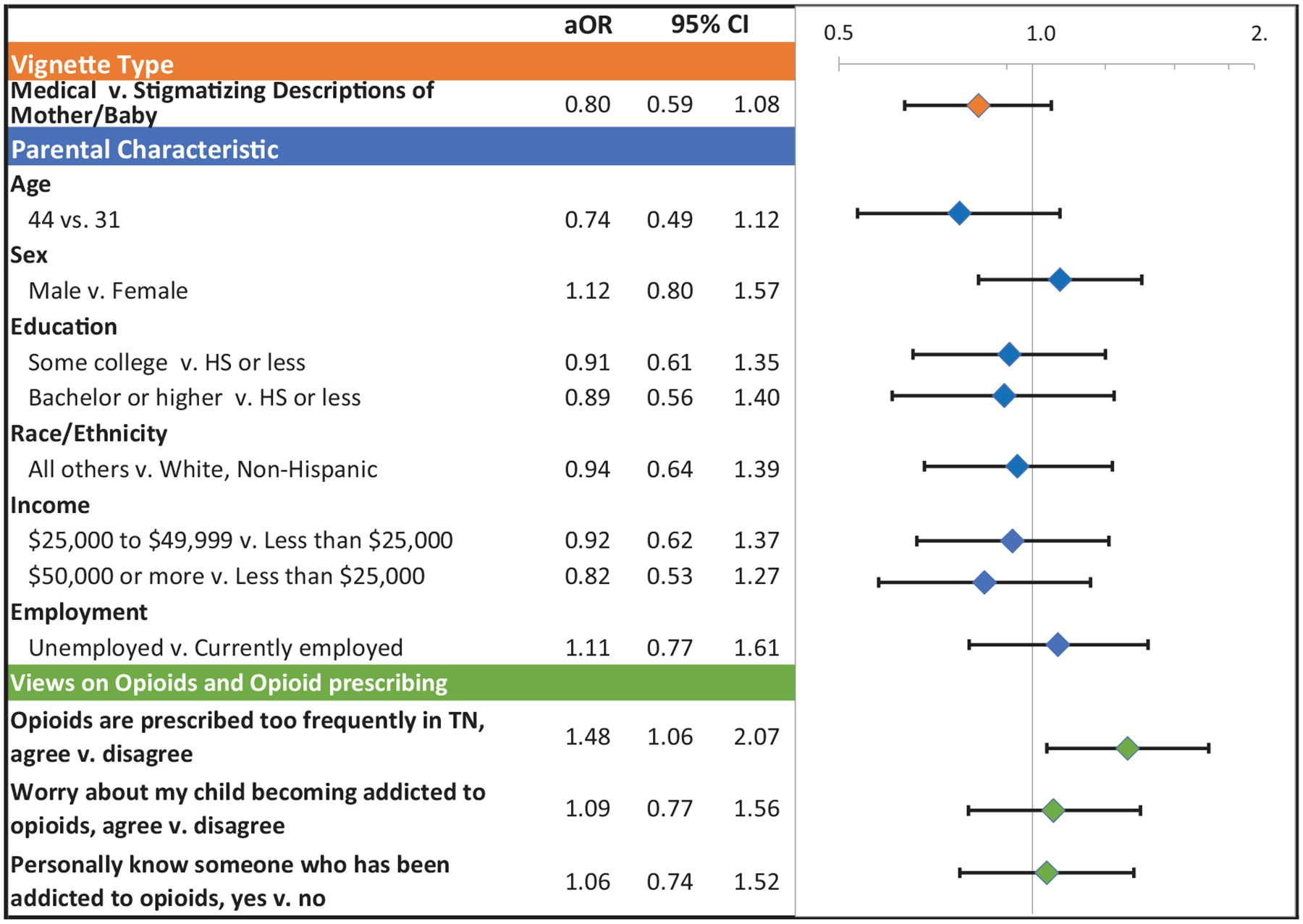
Adjusted ordinal regression assessing factors associated with punitive responses to parental custody at discharge for an opioid-exposed mother-infant dyad.
Review
This study examined the effect of using different terms to describe opioid-exposed mother-infant dyads. Regardless of which vignette a parent received, about one-third of participants felt that the mother who is receiving treatment for her OUD during pregnancy should be arrested, and two-thirds felt that the infant should be placed outside of her care. This finding highlights a high level of stigma toward pregnant women with OUD, including those in treatment. We did not find that the use of stigmatizing terms rather than medically appropriate language to describe the mother and infant significantly affected participants’ responses. Rather, the generally negative views toward mothers with OUD held by parents in Tennessee likely drove the findings we observed.
There has been a rise in punitive policies toward pregnancy and parenting women with substance use disorder in the United States over the past twenty years, despite evidence that they do not result in improved maternal or infant outcomes and have been shown to result in avoidance of prenatal care.19–22 Even though the highly punitive Tennessee law was not renewed in 2016, while in effect it was one of the most punitive statewide policies and may have influenced the views of the parents in our study, yielding a high rate of parents who felt a criminal justice response was justified for a pregnant woman engaged in OUD treatment. Additionally, many parents favored removal of the infant from parental custody, further highlighting the negative views the general public has of mothers with OUD in treatment and their fitness to parent. Pervasive public stigma regarding addiction can result in barriers at the individual level (i.e., fear of stigmatization leading women to avoid care), and the health system and societal level (i.e., underinvestment in social services and addiction treatment; punitive rather than public health-focused policies).12,23
In our final adjusted model, only concern around opioid prescribing in Tennessee, which has historically had one of the highest rates of opioid prescribing nationwide, was associated with more punitive views toward women with OUD, after adjusting for type of vignette received. In the context of a state sanctioning punitive responses to women with OUD as an approach to addressing the harms of increasing opioid use in, it may be that those most fearful of the impact of opioid use in their community have internalized these punitive actions as the appropriate way to address the opioid epidemic. Furthermore, well-intended efforts to reduce excess prescribing may in turn increase stigma toward individuals suffering from OUD.
There are important limitations to our study, including the use of a novel vignette and non-validated single question as our primary outcome measure. Some participants with less medical knowledge about neonatal opioid withdrawal syndrome may have misinterpreted the vignette and thought that if the infant required a prolonged hospitalization, then the mother was not in treatment at delivery, prompting the more punitive responses. Further, some participants may have chosen more punitive responses because the vignette did not specify how much ongoing treatment, support and care the dyad would receive after discharge. Additionally, there were likely unmeasured confounders that could have affected participants responses including urban v. rural location of dwelling, or personal or family history with addiction. Finally, the findings may not be generalizable beyond Tennessee, given the unique policy history in the state. These limitations notwithstanding, our finding of strongly punitive views of mothers receiving OUD treatment highlights the need to promote stigma-reduction interventions to ensure pregnant people with OUD feel well.
Conclusion
Many parents hold punitive views toward mothers receiving OUD treatment that were not altered by using less value-laden language. Efforts to address stigma should include person-first language, treatment-focused narratives, but also must extend beyond the choice of specific terms to address broadly-held perspectives about addiction.12,24
Funding
Research reported in this publication was supported by the National Institute on Drug Abuse of the National Institutes of Health under award number [K23DA048169] (Schiff) and [R01DA045729] (Patrick).
Footnotes
Disclosure statement
None of the authors report a conflict of interest. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- [1].Maeda A, Bateman BT, Clancy CR, Creanga AA, Leffert LR. Opioid abuse and dependence during pregnancy: temporal trends and obstetrical outcomes. Anesthesiology. 2014;121(6): 1158–1165. [DOI] [PubMed] [Google Scholar]
- [2].Haight SC, Ko JY, Tong VT, Bohm MK, Callaghan WM. Opioid use disorder documented at delivery hospitalization — United States, 1999–2014. MMWR Morb Mortal Wkly Rep 2018;67(31):845–849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Miranda L, Dixon V, Reyes C. How states handle drug use during pregnancy. Pro Publica. https://projects.propublica.org/graphics/maternity-drug-policies-by-state. Published 2015. Accessed February 1, 2019. [Google Scholar]
- [4].Guttmacher Institute. Substance use during pregnancy. Guttmacher Institute. https://www.guttmacher.org/state-policy/explore/substance-use-during-pregnancy. Published 2017. Accessed November 25, 2017.
- [5].Tennessee Fetal Assault Law (SB 1391). http://www.capitol.tn.gov/Bills/108/Bill/SB1391.pdf. Accessed October 25, 2017.
- [6].Jeltsen M Wave goodbye to harsh Tennessee law targeting pregnant drug users. HuffPost. https://www.huffingtonpost.com/entry/tennessee-pregnant-women-drugs_us_56e862b3e4b065e2e3d79320. Published 2016. Accessed October 25, 2017. [Google Scholar]
- [7].Bach WA. Prosecuting poverty, criminalizing care. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3307889. Published December 2018. Accessed February 1, 2019.
- [8].Liss-Shultz N Tennessee’s war on women is sending new mothers to jail – Mother Jones. Mother Jones. https://www.motherjones.com/politics/2016/03/tennessee-drug-use-pregnancy-fetal-assault-murder-jail-prison-prosecution/. Published March 2016. Accessed February 22, 2019. [Google Scholar]
- [9].Times Editorial Board. The Mothers Society Condemns. The New York Times. https://www.nytimes.com/interactive/2018/12/28/opinion/abortion-law-poverty.html. Published December 28, 2018. Accessed February 22, 2019. [Google Scholar]
- [10].Detoxing for delivery: facing medical challenges, judgment and sometimes jail. Knox News. https://www.knoxnews.com/story/news/local/2016/03/06/detoxing-for-delivery-facing-medical-challenges-judgment-and-sometimes-jail/90876276/. Published 2016. Accessed June 29, 2020. [Google Scholar]
- [11].Mother of drug-addicted infant going to prison. WREG.com. https://wreg.com/news/mother-of-drug-addicted-infant-going-to-prison/. Published 2015. Accessed June 29, 2020.
- [12].McGinty EE, Barry CL. Stigma reduction to combat the addiction crisis – developing an evidence base. N Engl J Med 2020; 382(14):1291–1292. [DOI] [PubMed] [Google Scholar]
- [13].Kelly JF, Dow SJ, Westerhoff C. Does our choice of substance-related terms influence perceptions of treatment need? An empirical investigation with two commonly used terms. J Drug Issues. 2010;40(4):805–818. [Google Scholar]
- [14].Goodyear K, Haass-Koffler CL, Chavanne D. Opioid use and stigma: the role of gender, language and precipitating events. Drug Alcohol Depend. 2018;185:339–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Schiff DM, Stoltman JJK, Nielsen TC, et al. Assessing stigma towards substance use in pregnancy: a randomized study testing the impact of stigmatizing language and type of opioid use on attitudes toward mothers with opioid use disorder. J Addict Med 2021. DOI: 10.1097/ADM.0000000000000832. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Freed GL, Davis MM, Singer DC, et al. Variation in generational perceptions of child health and well-being. Acad Pediatr 2018;18(4):384–389. [DOI] [PubMed] [Google Scholar]
- [17].Patrick SW, Henkhaus LE, Zickafoose JS, et al. Well-being of parents and children during the COVID-19 pandemic: a national survey. Pediatrics. 2020;146(4):e2020016824. [DOI] [PubMed] [Google Scholar]
- [18].Methods – Vanderbilt child health poll. The Center for Child Health Policy. https://www.vumc.org/childhealthpolicy/methods-vanderbilt-child-health-poll. Published 2019. Accessed June 29, 2020.
- [19].Atkins DN, Durrance CP. State policies that treat prenatal substance use as child abuse or neglect fail to achieve their intended goals. Health Aff 2020;39(5):756–763. [DOI] [PubMed] [Google Scholar]
- [20].Faherty LJ, Kranz AM, Russell-Fritch J, Patrick SW, Cantor J, Stein BD. Association of punitive and reporting state policies related to substance use in pregnancy with rates of neonatal abstinence syndrome. JAMA Netw Open. 2019;2(11):e1914078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Poland ML, Dombrowski MP, Ager JW, Sokol RJ. Punishing pregnant drug users: enhancing the flight from care. Drug Alcohol Depend. 1993;31(3):199–203. http://www.ncbi.nlm.nih.gov/pubmed/8462410. [DOI] [PubMed] [Google Scholar]
- [22].Stone R Pregnant women and substance use: fear, stigma, and barriers to care. Heal Justice. 2015;3(1):2. [Google Scholar]
- [23].Kennedy-Hendricks A, Barry CL, Gollust SE, Ensminger ME, Chisolm MS, McGinty EE. Social stigma toward persons with prescription opioid use disorder: associations with public support for punitive and public health-oriented policies. Psychiatr Serv 2017;68(5):462–469. [DOI] [PubMed] [Google Scholar]
- [24].Broyles LM, Binswanger IA, Jenkins JA, et al. Confronting inadvertent stigma and pejorative language in addiction scholarship: a recognition and response. Subst Abus 2014;35(3): 217–221. [DOI] [PMC free article] [PubMed] [Google Scholar]


