Abstract
Background
Today, the use of data in administrative and clinical processes is quite challenging due to the large volume of data, data collection from various sources, and lack of data structure. As a data management tool, dashboards play an important role in timely visual display of critical information on key performances.
Objectives
This systematic review aimed to identify functional and non-functional requirements, as well as challenges of using dashboards in hospitals.
Methods
In this systematic review, four databases, including the Web of Science, PubMed, EMBASE, and Scopus, were searched to find relevant articles from 2000 until May 30, 2020. The final search was conducted on May 30, 2020. Data collection was performed using a data extraction form and reviewing the content of relevant studies on the potentials and challenges of dashboard implementation.
Results
Fifty-four out of 1254 retrieved articles were selected for this study based on the inclusion and exclusion criteria. The functional requirements for dashboards included reporting, reminders, customization, tracking, alert creation, and assessment of performance indicators. On the other hand, the non-functional requirements included the dashboard speed, security, ease of use, installation on different devices (e.g., PCs and laptops), integration with other systems, web-based design, inclusion of a data warehouse, being up-to-data, and use of data visualization elements based on the user’s needs. Moreover, the identified challenges were categorized into four groups: data sources, dashboard content, dashboard design, implementation, and integration in other systems at the hospital level.
Conclusion
Dashboards, by providing information in an appropriate manner, can lead to the proper use of information by users. In order for a dashboard to be effective in clinical and managerial processes, particular attention must be paid to its capabilities, and the challenges of its implementation need to be addressed.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12911-022-02037-8.
Keywords: Hospital, Dashboard, Capabilities, Challenge
Introduction
Today, healthcare organizations, including hospitals, are struggling with different sources of information chaos, such as information overload/underload, erroneous information, information scatter, and information conflict. Information chaos not only causes dissatisfaction, fatigue, and disappointment among healthcare providers, but also exerts negative effects on patient safety [1]. On the other hand, the use of data in managerial and clinical processes is quite challenging due to the large volume of data, data collection from various sources, and lack of data structures. Consequences, such as increased errors [2], delayed care delivery [3], and reduced patient safety [4] are experienced due to poor data management and presentation.
Since hospitals provide a broad spectrum of diagnostic, curative, and administrative services in a complex and dynamic environment, there is an urgent need for continuous performance monitoring in different hospital departments for proper resource management and high-quality healthcare delivery [5]. Therefore, it is necessary for healthcare providers to obtain the necessary information using a comprehensive and organized method [6]. In fact, dashboards are data management tools that collect data from various information systems available in the organization and present it in a concise, comprehensive, meaningful, and intelligent manner in the form of key performance indicators with alerts on the status of these indicators. In this way, managers can briefly evaluate the performance of their department, identify the problems, and analyze their roots to improve their performance. This process allows managers to briefly evaluate the performance of their departments, identify the existing problems, and analyze their root causes to improve their performance [7, 8].
By providing accurate and timely information, dashboards are not only effective systems to meet the information needs of organizations, but are also helpful in the management of large amounts of data in these organizations [9]. The use of quality dashboards in healthcare settings is expanding. Healthcare dashboards are divided into two main categories of clinical and quality dashboards. Clinical dashboards provide timely and relevant information to help decision-making about patients and improve care [10, 11], whereas quality dashboards provide managers with key performance indicators at the department or organization level to help decision-making [12, 13].
Both functional and non-functional requirements need to be considered when developing a dashboard. The functional requirements deal with functions that a system is intended to perform or deliver [14]. On the other hand, non-functional requirements are a set of specifications that describe the system’s operation capabilities and constraints and attempt to improve its functionality. These are basically the requirements that outline how well it will operate including things like speed, security, reliability, data integrity, etc. [14, 15].
The results of studies show that the use of dashboards have the potential to accelerate data collection, reduce cognitive burden, reduce errors, and improve the awareness situation in healthcare settings [16–18]. The review by Dowding et al. showed that there is some evidence that using dashboards that provide immediate access to information for clinicians can improve adherence to quality guidelines and may help improve patient outcomes [19].
Despite the increasing use of dashboards in hospitals and other health care settings, there are still challenges in content, design, implementation, and integration with other systems. Although there has been research on dashboards in health care, to our knowledge, no systematic review has been conducted on functional and non-functional requirements as well as challenges of hospital dashboards. The current study aimed to review challenges with hospital dashboards and provide recommendations for improvement.
Methods
Data sources and search strategy
The present study was conducted based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [20]. The Web of Science, PubMed, EMBASE, and Scopus databases were searched to identify relevant studies. In the search strategy, combinations of MeSH terms, Emtree terms, and keywords related to dashboards, Capabilities, and hospital were used (Table 1). The search was conducted on May 30, 2020. One researcher (SA) searched the literature and retrieved relevant studies independently. Any uncertainty with the other author (RR) were discussed and resolved. The final stage of the search strategy was the bibliographic check of the selected articles.
Table 1.
Search strategy and keywords
| 1# | dashboard OR whiteboard OR status board OR Electronic tracking board OR visualization OR presentation format OR display format OR performance measurement system |
| 2# | Design OR capability OR feature OR character OR attributes OR function OR usability OR content |
| 3# | Hospital |
| AND | 1# AND 2# AND 3# |
Inclusion and exclusion criteria
The inclusion criteria were as follows: (1) articles written in English; (2) articles that focused on quality/clinical dashboard implementation at hospitals or in hospital wards; and (3) articles that addressed functional and non-functional requirements and challenges of implementing dashboards. The exclusion criteria were non-English articles and studies investigating the implementation of clinical/quality dashboards in non-hospital settings.
Study selection, appraisal, and data extraction
The eligible articles were identified in a two stage process: (1) screening the study title and abstract; and (2) selection of articles by reviewing the full-text manuscripts. Two researchers (RR and SA) independently evaluated the retrieved articles based on the inclusion and exclusion criteria. Each reviewed article was classified as undecided, excluded, or included. The undecided articles were discussed by both reviewers, and then they performed quality assessments independently, and any discrepancies were resolved in group discussions. The Cochrane Effective Practice and Organization of Care (EPOC) guidelines were used to evaluate the quality of retrieved articles. This guideline is developed for the quality assessment of clinical trials, non-clinical trials, before-and-after trials, and case studies [21].
In the data extraction stage, the year of publication, country, and setting were documented for each article (Figs. 2, 3, 4). Next, the goals and requirements of dashboards were categorized as functional requirements, non-functional requirements, and system applications (Table 2). Besides, challenges were categorized into four groups based on similar studies: data source and data generation, dashboard content, dashboard design, and implementation and integration (Table 3).
Fig. 2.
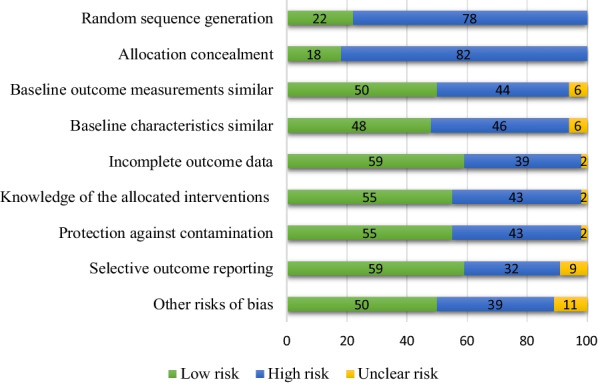
Percent of quality assessment criteria based on EPOC
Fig. 3.
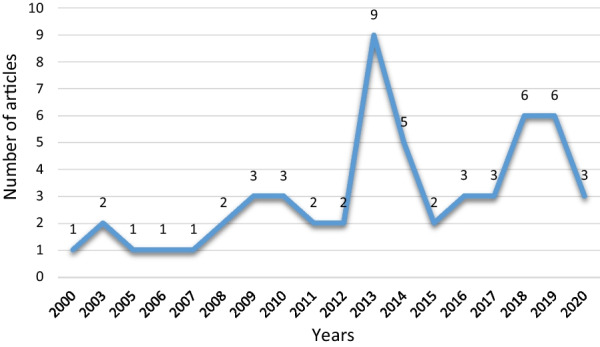
Number of publication by year
Fig. 4.
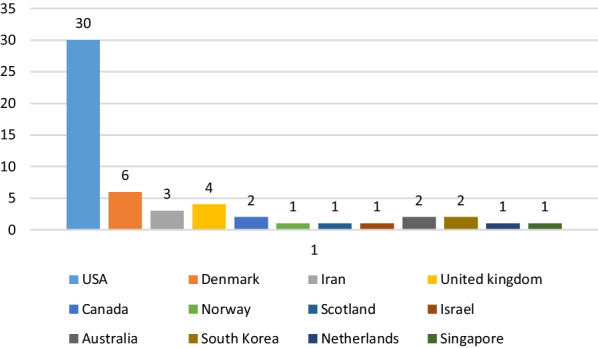
Number of publication by country
Table 2.
Goals and requirements for a hospital dashboard
| Dashboard’s application and requirements | Studies |
|---|---|
| System applications | |
| Quality of care assessment | [24, 26, 28–31, 39, 48–51, 53–55, 57, 59–62, 65, 66, 74] |
| Resource management | [25, 28, 52, 71] |
| Activities monitoring | [22, 24–31, 36, 38, 45–66, 68, 70–72, 74] |
| Analysis and forecasting | [30–32, 48, 65, 68] |
| Functional requirements | |
| Customization | [26–44, 50–52, 57–60, 62–66, 68–74] |
| Alert creation | [23, 26, 28–30, 33, 35–38, 40–45, 47–49, 53, 54, 56–60, 63–66, 68–70, 72, 73] |
| Tracking | [28, 33, 43–49, 53, 54, 56, 57] |
| Performance indicators measurement | [27, 31, 36, 39, 44, 45, 48, 57, 59–62, 69, 71, 72] |
| Reporting | [22–49, 53–55, 57–72, 74] |
| Reminder messages | [26, 29] |
| Non-functional requirements | |
| Use data visualization elements to display data based on user needs | [18, 24, 27–45, 57, 58, 61–64, 66–74] |
| Ability to install on a variety of devices such as PC and Laptop | [25, 49, 58, 69] |
| Speed | [28, 36, 43, 69] |
| Integration with other systems | [26, 28–30, 32, 36, 50, 53, 57, 60, 64, 68, 69, 74] |
| Security | [19, 30, 44, 44, 57, 60, 66] |
| Ease of use | [27, 28, 36, 42, 60, 63, 68, 71] |
| Web based | [22, 24–26, 29, 30, 37, 44, 49–53, 55, 59, 63, 73] |
| Having a data warehouse | [27, 28, 30, 44, 60] |
Table 3.
Challenges with dashboards and solutions
| Main challenges | Solutions |
|---|---|
| Data sources and data generation | |
| Combining multiple computerized systems | Entering the correct data |
| Different data formats | Create data warehouse |
| Data quality | Automatic data collection |
| Fragmented source systems | Use of web service architecture and middleware |
| Redundancy of the data | |
| Manual data entry | |
| Dashboard content | |
| Different needs of users | Stakeholder participation Identify performance indicators appropriate to the goals of the organization |
| The information displayed does not match the needs of users | |
| Non-compliance of key performance indicators with the goals of the organization | |
| Problems with measuring too many performance indicators | |
| Patient privacy | |
| Dashboard design | |
| Users’ differing executive duties | Use of customization feature |
| Cognitive abilities and analytical skills | Use of colour-coding system |
| Problem with type of information displayed through visualization tools | Use of visualization |
| Amount of information presented on dashboard | Accurate understanding of the capabilities of existing systems |
| Provide timely data | |
| Implementation and integrating | |
| Lack of compatibility with workflows | Use of data exchange standards |
| Context sensitivity | Security |
| Lack of integration with other hospital systems | User training |
| Service disruption | Gradual implementation |
| System security | |
| Accessing the dashboard | |
| Increased workload | |
Findings
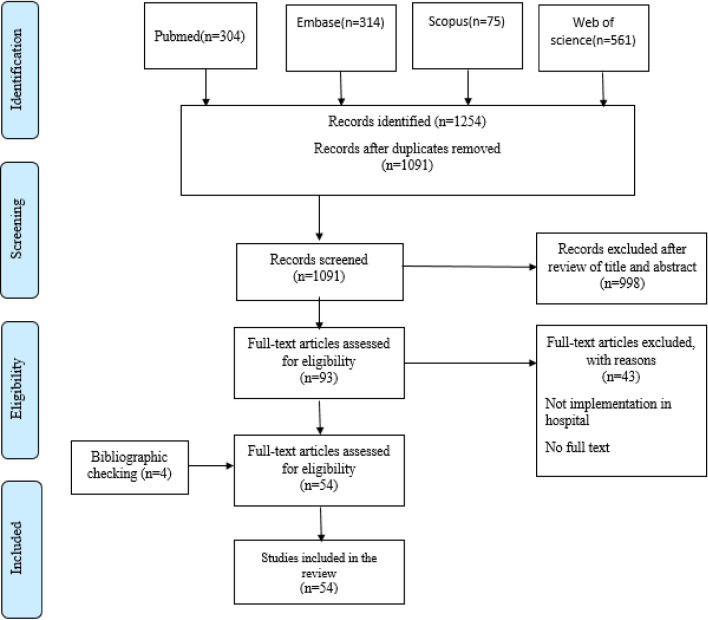
A total of 1254 articles were retrieved in this study, 163 of which were removed due to duplication. Of 1091 articles remaining, 998 were removed after reviewing their titles and abstracts (93 remaining articles). Next, the full-text manuscript of the articles was reviewed, resulting in the elimination of 43 articles. Finally, 50 articles were found eligible for this study. Besides, the reference lists of the selected articles were hand-searched, resulting in the identification of four studies. All extracted articles had an acceptable quality, and no study was removed due to low quality. Finally, a total of 54 articles were considered eligible and examined in this study. The article selection process is shown in Fig. 1.
Fig. 1.
The flow diagram of the study based on the PRISMA statement
Quality assessment
According to the quality assessment of papers, 22 studies (41%) were considered as “high quality”; 12 studies (22%) were assigned as “fair to good quality”, and 20 studies (37%) were regarded as low quality (Additional file 1: Appendix A).
As Fig. 2 shows, 82% of articles demonstrated a high risk of bias in relation to allocation concealment and 78% demonstrated a high risk of bias with respect to random sequence generation. In addition, 59% of articles showed a low risk of bias pertaining to incomplete outcome data and selective outcome reporting (Fig. 2).
Characteristics of eligible studies
Among the 54 studies, 32 were non-experimental studies (59%), of which 15 were descriptive studies, 14 were cross-sectional studies, and 3 were case studies. Twenty-two studies were experimental studies (41%), of which 21 were non-randomized studies and one was a randomized controlled study. As Fig. 3 shows, the use of dashboards in healthcare is increasing. The majority of eligible studies were performed in the USA, followed by Denmark, England, and Iran (Fig. 4). Most of these studies (n = 43) were conducted in different departments, while 11 studies were performed at hospital levels. Among hospital wards, the majority of studies were performed in the emergency department, followed by the radiology unit and the intensive care unit (Fig. 5).
Fig. 5.
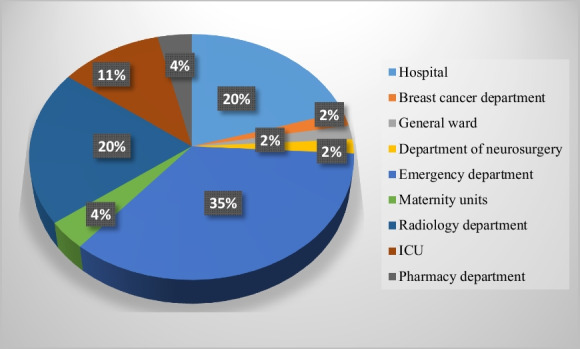
Number of publication by setting
Hospital dashboard requirements
Table 2 lists the functional and non-functional goals and requirements of dashboards.
According to the reviewed papers, the goals of the dashboard include care quality assessment, resource management (staff and equipment), monitoring ongoing activities at the hospital level, and analyzing and forecasting hospital activities. Functional requirements for both quality and clinical dashboards in the literature include the following:
Customization: It enables users to change the type of indicators displayed by the dashboard and optimize their view of the content shown on the screen to best suit their needs and preferences. Customizability in quality dashboards can be used to display and monitor performance indicators that are important to the user and require real-time monitoring. In clinical dashboards, it serves to display clinical information essential to assessing patients’ status.
Alerts creating: This feature creates alerts for indicators that are necessary to the user and demand real-time monitoring. It also gives an alert when the value of the indicators exceeds the defined standard. Alert creation in quality dashboards is used when the value of indicators is higher than the defined standard. In clinical dashboards, this feature alerts physicians or nurses when the results of tests or imaging are ready.
Tracking: This feature tracks the location of patients for real-time monitoring of ongoing activities, identifying crowded wards, and proper allocation of resources. In quality dashboards, this feature is used to determine the location of patients and monitor crowded wards. In clinical dashboards, it serves to locate the physician's instructions and monitor them until the results are ready.
Measuring performance indicators: This involves comparing indicators with standards or with the national average, and comparing indicators over time. In quality dashboards, it is used to measure performance indicators, and in clinical dashboards, to display patients' clinical information.
Reporting: It is the ability to prepare visual reports based on clinical performance indicators in clinical dashboards, and based on managerial performance indicators in quality dashboards. It also involves the ability to create output files in various formats (Excel, Word, PDF),
Reminders: This feature creates reminders about the time of maintenance and inspection of hospital equipment.
Challenges with dashboards and solutions
The identified challenges were categorized into four groups: data sources and data generation [26–30, 40, 47, 54, 56, 69, 71, 72], dashboard content [19, 31, 36, 41, 46–48, 50, 57, 59], dashboard design [19, 26, 33, 34, 36, 40, 41, 54, 69, 70], and implementation and integration [19, 26, 28, 33–37, 40, 44, 50, 56, 67, 69, 70, 72]. The proposed strategies to eliminate these challenges are presented in Table 3.
The proposed solutions to alleviate the challenges of identifying data sources and generating data include inputting the accurate data to the dashboard [44], creating a standard-format data warehouse for data manipulation to facilitate sharing and reduce processing time, updating and creating queries from the dashboard [27, 30, 44, 57], using the architecture of Web services and middleware [26, 29, 44], and utilizing automatic data extraction methods to solve the manual data input problem [47]. The proposed solutions to reduce the challenges of identifying the content of dashboards include stakeholder participation in the development, implementation, and evaluation of the dashboard [19, 31, 36, 44, 54, 63], identification of performance indicators suitable for organizational goals, and not selecting too many indicators for reporting by the dashboard [44]. The proposed solutions to mitigate the challenges associated with dashboard design are matching graphics to the purpose of the content, timely display of data, using a color-coding system, adding customization capabilities [19, 31, 32, 48, 49, 57, 63], proper organization and display of information using visualization tools to help users read and interpret information faster [44], accurate understanding of the capabilities of old systems and how they support clinical activities [34]. The proposed solutions to decrease the challenges of dashboard implementation and integration include integrating and linking the dashboard to other systems, and using data exchange standards [19, 26, 30, 33, 44, 51, 57], user training [36], paying attention to dashboard security when integrated with other systems, determining the access level based on user tasks [19, 44, 57, 60], and gradual implementation of the dashboard [36].
Discussion
This systematic review aimed to identify the functional and non-functional requirements and challenges of using dashboards in hospital settings. Based on the findings, reporting, customization, reminders, assessment of performance indicators, alert creation, and tracking were identified as the functional requirements of quality/clinical dashboards [75, 76]. In a study by Buttigieg et al., monitoring, analysis, alerts, and color coding were described as the main functional requirements of clinical dashboards [7, 16]. Besides, Ghazi Saeedi et al. found alarms, drill down, and timely presentation as the central features of quality dashboards [77]. In Randell et al.'s study [78], the functional requirements of quality dashboards included visualization, interaction, data quality, reporting, and notification.
However, functional capabilities are used in both quality and clinical dashboards depending on the intended environment and purpose. Previous studies found speed, security, ease of use, and integration in other systems as the main non-functional features of dashboards [79]. The findings of the present study also indicated the importance of the mentioned features as non-functional requirements. Moreover, attention to the user-friendliness and user interface (UI) of the software, tailored to the needs of users, increases the successful implementation and continuous use of the system [80]; In the present study, features such as speed, security, and integration with other systems constitute the non-functional requirements of dashboards. To promote the user-friendliness of the system user interface, data visualization tools suited to the nature of data and users’ perception and knowledge should be employed.
In the current study, the identified challenges were categorized into four groups: data sources and data generation, dashboard content, dashboard design, and implementation and integration. In a study by Rasmussen et al., four types of challenges, including presentation format, integration, interface design, and development and implementation, were described [81]. Since the presentation format is related to the UI design [82], in the present study, it was classified as dashboard design.
Similarly, Ghazi Saeedi et al. reported four types of implementation challenges, including the development of performance indicators, data sources and data generation, integration of dashboards in source systems, and information presentation problems [77]. In the present study, the development of performance indicators was classified as dashboard content. Regarding the challenges of data sources, due to the dispersion of systems and storing data in different formats in these systems, the creation of a data warehouse for data storage and web service architecture is suggested. In addition, development of a data warehouse is one of the methods to prevent duplications in a dashboard [13, 81, 83].
According to previous studies, data availability is also a major prerequisite for dashboard development [12, 84]. Besides, a service-oriented architecture is necessary for encapsulating data from different systems in a middleware layer for data integration in dashboards, and understanding various data hosting structures, different methods of data proliferation and transfer, and the best query language are necessary for this data structure [85].
Regarding the challenges of dashboard content, in the present study, in relation to the type of information displayed by the dashboard and non-compliance with user needs, user participation and focus on selecting indicators appropriate to the goals of the organization is proposed. Evidence suggests the necessity of engaging users in dashboard development and adaptation processes to reduce resistance to the implementation of these systems [81].
Generally, it is important to select the type and number of indicators in a dashboard [86, 87], and every organization needs to select appropriate indicators depending on its goals [88]. Evidence shows that at least 15–25 indicators are essential in a dashboard [89].
Regarding the challenges of dashboard design, in the present study, to have a compatible system with the users’ cognitive abilities and skills and to provide information in a timely manner s, the capability of customization (to display information tailored to the user’s needs), color-coding systems, and visualization tools has been suggested. Overall, the findings of the current study were consistent with previous studies. According to previous studies, features, such as drill-down, filter, and alerts, are needed in dashboards for customizing the data depending on the user’s needs [12, 17, 90]. Overall, customization is an essential feature for organizing the dashboard content according to the users’ needs and promoting its application by the users [89, 91]. Besides, a color-coding system can be useful for a better understanding and interpretation of displayed information [12].
Besides, the reviewed studies had not used the same techniques to visualize performance indicators. Based on the present study, depending on the type of dashboard, its context, and users, a variety of interactive and visualization techniques are employed in dashboard design. Research suggests that using the same visualization model (in which visualization is performed without considering the user's preferences, abilities, or contexts) would not be effective. On the other hand, the development of adaptive and personalized visualization systems (using which users can change the type of information display according to their individual cognitive style and ability) will help better understand the information displayed by the dashboard [91, 92]. Moreover, in the dashboard, the nature of data and human factors, e.g., experience, skills, preferences, and cognitive styles influence the choice of visualization and interaction techniques [93, 94].
Additionally, regarding the challenges of dashboard implementation and integrating, the present study highlighted the importance of integrating data exchange standards, determining data access levels for dashboards, gradual adaptation of dashboards, and user training as potential solutions to facilitate dashboard adaptation and address its incompatibility with other systems. Since different hospital systems are integrated and linked to dashboards, particular attention should be paid to data security. In addition, data exchange standards are necessary for communication between systems and their integration in hospitals [95]. Theoretically, depending on the importance and quality of information in dashboards, the level of data accessibility can be controlled at different security/privacy levels [96]. It is also recommended to control the level of access based on the user's role and incorporate features, such as read-only or write/edit access [96, 98]. Moreover, the use of “single sign-on” technology is recommended for user login [98]. The present findings also indicated the significant contribution of gradual dashboard implementation and inclusion of features based on the users’ needs for achieving success and meeting the users’ needs [99].
It is also important to pay attention to the context when implementing the dashboard. For instance, a delay in reporting the results of a head CT scan at the emergency department is critical if it takes more than a few minutes; however, a delay in the same CT scan performed on an outpatient basis in other departments may not be important even if it takes several hours. Additionally, a radiologist may have hundreds of reports to sign per day, while an angiographer may have fewer than 10 reports. In the intensive care unit (ICU) and emergency department, the real-time feature is more important than in other departments. Because of these workflow determinants, dashboards must combine context-sensitive parameters to effectively manage workflows. Therefore, dashboards should be optimized, context-sensitive, customizable, and workflow-integrated.
Strengths and limitations
A strength of this study was providing a comprehensive view of the functional and non-functional requirements of dashboards designed in hospitals. It also delineated and categorized the dashboard implementation challenges that may arise in dashboard design and implementation steps and offered solutions to overcome these challenges. The results of this study can lay the ground for better design and implementation of dashboards at the hospital level. It is important to address some limitations of this study. First, all retrieved articles were written in English. Second, data were extracted by one researcher (SA) and evaluated by two researchers (SA and RR), which probably resulted in the unintended removal of some eligible studies. Finally, the inclusion and exclusion criteria of this study focused on the implemented hospital-level dashboards, while those used for data management related to a particular disease were excluded.
Future research
The present study revealed several issues in the evaluation and design of quality/clinical dashboards. Studies should be conducted to examine the effectiveness of using quality/clinical dashboards in patient care processes, to assess the workload of users when using the dashboard, and to measure situation awareness in the presence of the dashboard. Studies should also focus on interactive techniques and data visualization in quality and clinical dashboards according to the environment in which they are used.
Conclusion
As a data management tool, dashboards play a significant role in managing significant amounts of data in healthcare settings, including hospitals. According to the findings, functional requirements for a hospital dashboard were as follows: reporting, customization, reminders, assessment of performance indicators, alert creation, and tracking. Also, non-functional indicators included speed, security, ease of use, installation on different devices (e.g., PCs and laptops), integration in other systems, web-based design, inclusion of a data warehouse, being up-to-data, and use of data visualization elements based on the users' needs; these features contribute to the adaptation and success of dashboards. Considering the challenges of dashboard implementation in hospital settings, particular attention needs to be paid to data sources, dashboard content, UI design, and dashboard implementation and integration in other hospital systems. Finally, by examining the functional and non-functional requirements of hospital dashboards, and by enumerating the various challenges in dashboard design and implementation, these results can be a basis for improving the design and implementation of dashboards at the hospital level.
Supplementary Information
Additional file 1: Appendix A. The result of qualitative evaluation of studies.
Acknowledgements
Not applicable.
Author contributions
Concept and design: SA and RR; Literature search and quality check: SA and RR; Data analysis and interpretation: SA and RR; Manuscript drafting: SA; Editing and critical review: RR; Both authors read and approved the final manuscript.
Funding
Not applicable.
Availability of data and materials
All data used in the publication of this work were obtained from published studies. The abstracts for these studies are available in the web of science, pubmed, embase, and scopus database.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable as the paper does not contain any individual person’s data.
Competing interests
The authors declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Beasley JW, Wetterneck TB, Temte J, Lapin JA, Smith P, Rivera-Rodriguez AJ, et al. Information chaos in primary care: implications for physician performance and patient safety. J Am Board Fam Med. 2011;24(6):745–751. doi: 10.3122/jabfm.2011.06.100255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McDonald CJ. Protocol-based computer reminders, the quality of care and the non-perfectability of man. N Engl J Med. 1976;295(24):1351–1355. doi: 10.1056/NEJM197612092952405. [DOI] [PubMed] [Google Scholar]
- 3.McDonald CJ, Callaghan FM, Weissman A, Goodwin RM, Mundkur M, Kuhn T. Use of internist's free time by ambulatory care Electronic Medical Record systems. JAMA Intern Med. 2014;174(11):1860–1863. doi: 10.1001/jamainternmed.2014.4506. [DOI] [PubMed] [Google Scholar]
- 4.Holden RJ. Cognitive performance-altering effects of electronic medical records: an application of the human factors paradigm for patient safety. Cogn Technol Work. 2011;13(1):11–29. doi: 10.1007/s10111-010-0141-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Speziale G. Strategic management of a healthcare organization: engagement, behavioural indicators, and clinical performance. Eur Heart J Suppl. 2015;17(suppl A):A3–A7. doi: 10.1093/eurheartj/suv003. [DOI] [Google Scholar]
- 6.Rabiei R, Mohammadi Moghadam Y, Aslani N, Garavand A, Kazemnejad A, Abhari S. Knowledge management status in a non-governmental public hospital: the current status and improvement solutions. J Health Man Info. 2020;7(1):26–32.
- 7.Buttigieg SC, Pace A, Rathert C. Hospital performance dashboards: a literature review. J Health Organ Manag. 2017;31(3):385–406. doi: 10.1108/JHOM-04-2017-0088. [DOI] [PubMed] [Google Scholar]
- 8.Wilbanks BA, Langford PA. A review of dashboards for data analytics in nursing. Comput Inform Nurs. 2014;32(11):545–549. doi: 10.1097/CIN.0000000000000106. [DOI] [PubMed] [Google Scholar]
- 9.Few S. Information dashboard design: displaying data for at-a-glance monitoring. Berkeley: Analytics Press; 2013. [Google Scholar]
- 10.Batley NJ, Osman HO, Kazzi AA, Musallam KM. Implementation of an emergency department computer system: design features that users value. J Emerg Med. 2011;41(6):693–700. doi: 10.1016/j.jemermed.2010.05.014. [DOI] [PubMed] [Google Scholar]
- 11.Linder JA, Schnipper JL, Tsurikova R, Yu DT, Volk LA, Melnikas AJ, et al. Electronic health record feedback to improve antibiotic prescribing for acute respiratory infections. Am J Manag Care. 2010;16(12 Suppl HIT):e311–e319. [PubMed] [Google Scholar]
- 12.Pauwels K, Ambler T, Clark B, LaPointe P, Reibstein D, Skiera B, et al. Dashboards as a service: why, what, how, and what research is needed? J Serv Res. 2009;12(2):175–189. doi: 10.1177/1094670509344213. [DOI] [Google Scholar]
- 13.Kroch E, Vaughn T, Koepke M, Roman S, Foster D, Sinha S, et al. Hospital boards and quality dashboards. J Patient Saf. 2006;2(1):10–19. [Google Scholar]
- 14.Chung L, Prado Leite JCSD. On non-functional requirements in software engineering. In: Borgida AT, Chaudhri VK, Giorgini P, Yu ES, editors. Conceptual modeling: foundations and applications. Berlin: Springer; 2009. pp. 363–79. [Google Scholar]
- 15.Egan M. Clinical dashboards: impact on workflow, care quality, and patient safety. Crit Care Nurs Q. 2006;29(4):354–361. doi: 10.1097/00002727-200610000-00008. [DOI] [PubMed] [Google Scholar]
- 16.Khairat SS, Dukkipati A, Lauria HA, Bice T, Travers D, Carson SS. The impact of visualization dashboards on quality of care and clinician satisfaction: integrative literature review. JMIR Hum Factors. 2018;5(2):e22. doi: 10.2196/humanfactors.9328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fuller TE, Garabedian PM, Lemonias DP, Joyce E, Schnipper JL, Harry EM, Bates DW, Dalal AK, Benneyan JC. Assessing the cognitive and work load of an inpatient safety dashboard in the context of opioid management. Appl Ergon. 2020;85:103047. doi: 10.1016/j.apergo.2020.103047. [DOI] [PubMed] [Google Scholar]
- 18.Weggelaar-Jansen AM, Broekharst DSE, de Bruijne M. Developing a hospital-wide quality and safety dashboard: a qualitative research study. BMJ Qual Saf. 2018;27(12):1000–1007. doi: 10.1136/bmjqs-2018-007784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dowding D, Randell R, Gardner P, Fitzpatrick G, Dykes P, Favela J, Hamer S, Whitewood-Moores Z, Hardiker N, Borycki E, Currie L. Dashboards for improving patient care: review of the literature. Int J Med Inform. 2015;84(2):87–100. doi: 10.1016/j.ijmedinf.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 20.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cochrane Effective Practice and Organisation of Care (EPOC) Suggested risk of bias criteria for EPOC reviews. EPOC Resources for review authors, 2017. Cited [20 September 2020]. http://epoc.cochrane.org/resources/epoc-resources-review-authors.
- 22.Seltzer SE, Kelly P, Deibel GM, Ros P. Radiology quality and performance metrics on the Web: a management information and communications tool. Acad Radiol. 2000;7(11):981–985. doi: 10.1016/s1076-6332(00)80182-8. [DOI] [PubMed] [Google Scholar]
- 23.Boger E. Electronic tracking board reduces ED patient length of stay at Indiana Hospital. J Emerg Nurs. 2003;29(1):39–43. 10.1067/men.2003.13. [DOI] [PubMed]
- 24.Nagy PG, Daly M, Warnock M, Ehlers KC, Rehm J. PACSPulse: a web-based DICOM network traffic monitor and analysis tool. Radiographics. 2003;23(3):795–801. doi: 10.1148/rg.233025114. [DOI] [PubMed] [Google Scholar]
- 25.France DJ, Levin S, Hemphill R, Chen K, Rickard D, Makowski R, et al. Emergency physicians' behaviors and workload in the presence of an electronic whiteboard. Int J Med Inform. 2005;74(10):827–837. doi: 10.1016/j.ijmedinf.2005.03.015. [DOI] [PubMed] [Google Scholar]
- 26.Morgan MB, Branstetter BF, 4th, Mates J, Chang PJ. Flying blind: using a digital dashboard to navigate a complex PACS environment. J Digit Imaging. 2006;19(1):69–75. doi: 10.1007/s10278-005-8732-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bahl V, McCreadie SR, Stevenson JG. Developing dashboards to measure and manage inpatient pharmacy costs. Am J Health Syst Pharm. 2007;64(17):1859–1866. doi: 10.2146/ajhp060596. [DOI] [PubMed] [Google Scholar]
- 28.Aronsky D, Jones I, Lanaghan K, Slovis CM. Supporting patient care in the emergency department with a computerized whiteboard system. J Am Med Inform Assoc. 2008;15(2):184–194. doi: 10.1197/jamia.M2489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Morgan MB, Branstetter BF, 4th, Lionetti DM, Richardson JS, Chang PJ. The radiology digital dashboard: effects on report turnaround time. J Digit Imaging. 2008;21(1):50–58. doi: 10.1007/s10278-007-9008-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nagy PG, Warnock MJ, Daly M, Toland C, Meenan CD, Mezrich RS. Informatics in radiology: automated web-based graphical dashboard for radiology operational business intelligence. Radiographics. 2009;29(7):1897–1906. doi: 10.1148/rg.297095701. [DOI] [PubMed] [Google Scholar]
- 31.Wong HJ, Caesar M, Bandali S, Agnew J, Abrams H. Electronic inpatient whiteboards: improving multidisciplinary communication and coordination of care. Int J Med Inform. 2009;78(4):239–247. doi: 10.1016/j.ijmedinf.2008.07.012. [DOI] [PubMed] [Google Scholar]
- 32.Zaydfudim V, Dossett LA, Starmer JM, Arbogast PG, Feurer ID, Ray WA, et al. Implementation of a real-time compliance dashboard to help reduce SICU ventilator-associated pneumonia with the ventilator bundle. Arch Surg. 2009;144(7):656–662. doi: 10.1001/archsurg.2009.117. [DOI] [PubMed] [Google Scholar]
- 33.Abujudeh HH, Kaewlai R, Kodsi SE, Hamill MA. Technical report: Improving quality of communications in emergency radiology with a computerized whiteboard system. Clin Radiol. 2010;65(1):56–62. doi: 10.1016/j.crad.2009.05.015. [DOI] [PubMed] [Google Scholar]
- 34.Bisantz AM, Pennathur PR, Guarrera TK, Fairbanks RJ, Perry SJ, Zwemer F, et al. Emergency Department Status Boards: a case study in information systems transition. J Cogn Eng Decis Mak. 2010;4(1):39–68. doi: 10.1518/155534310X495582. [DOI] [Google Scholar]
- 35.Rasmussen R, Fleron B, Hertzum M, Simonsen J. Balancing tradition and transcendence in the implementation of emergency-department electronic whiteboards. In: MolkaDanielsen J, Nicolaisen HW, Persson JS, editors. Selected papers of the information systems research seminar in Scandinavia. Trondheim: Tapir Academic Publishers; 2010. pp. 73–87. [Google Scholar]
- 36.Hertzum M. Electronic emergency-department whiteboards: a study of clinicians’ expectations and experiences. Int J Med Inform. 2011;80(9):618–630. doi: 10.1016/j.ijmedinf.2011.06.004. [DOI] [PubMed] [Google Scholar]
- 37.Waitman LR, Phillips IE, McCoy AB, Danciu I, Halpenny RM, Nelsen CL, et al. Adopting real-time surveillance dashboards as a component of an enterprisewide medication safety strategy. Jt Comm J Qual Patient Saf. 2011;37(7):326–332. doi: 10.1016/s1553-7250(11)37041-9. [DOI] [PubMed] [Google Scholar]
- 38.Sebastian K, Sari V, Loy LY, Zhang F, Zhang Z, Feng M. Multi-signal Visualization of Physiology (MVP): a novel visualization dashboard for physiological monitoring of Traumatic Brain Injury patients. Annu Int Conf IEEE Eng Med Biol Soc. 2012;2012:2000–2003. doi: 10.1109/EMBC.2012.6346349. [DOI] [PubMed] [Google Scholar]
- 39.Stone-Griffith S, Englebright JD, Cheung D, Korwek KM, Perlin JB. Data-driven process and operational improvement in the emergency department: the ED Dashboard and Reporting Application. J Healthc Manag. 2012;57(3):167–180. [PubMed] [Google Scholar]
- 40.Daley K, Richardson J, James I, Chambers A, Corbett D. Clinical dashboard: use in older adult mental health wards. Psychiatrist. 2013;37(3):85–88. doi: 10.1192/pb.bp.111.035899. [DOI] [Google Scholar]
- 41.Dexheimer JW, Kennebeck S. Modifications and integration of the electronic tracking board in a pediatric emergency department. Pediatr Emerg Care. 2013;29(7):852–857. doi: 10.1097/PEC.0b013e31829ba7ef. [DOI] [PubMed] [Google Scholar]
- 42.Dolan JG, Veazie PJ, Russ AJ. Development and initial evaluation of a treatment decision dashboard. BMC Med Inform Decis Mak. 2013;13:51. doi: 10.1186/1472-6947-13-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hertzum M, Simonsen J. Work-practice changes associated with an electronic emergency department whiteboard. Health Inform J. 2013;19(1):46–60. doi: 10.1177/1460458212454024. [DOI] [PubMed] [Google Scholar]
- 44.Karami M, Safdari R, Rahimi A. Effective radiology dashboards: key research findings. Radiol Manag. 2013;35(2):42–45. [PubMed] [Google Scholar]
- 45.Koch SH, Weir C, Westenskow D, Gondan M, Agutter J, Haar M, et al. Evaluation of the effect of information integration in displays for ICU nurses on situation awareness and task completion time: a prospective randomized controlled study. Int J Med Inform. 2013;82(8):665–675. doi: 10.1016/j.ijmedinf.2012.10.002. [DOI] [PubMed] [Google Scholar]
- 46.Mansoori B, Novak RD, Sivit CJ, Ros PR. Utilization of dashboard technology in academic radiology departments: results of a national survey. J Am Coll Radiol. 2013;10(4):283–288.e3. doi: 10.1016/j.jacr.2012.09.030. [DOI] [PubMed] [Google Scholar]
- 47.Simms RA, Ping H, Yelland A, Beringer AJ, Fox R, Draycott TJ. Development of maternity dashboards across a UK health region; current practice, continuing problems. Eur J Obstet Gynecol Reprod Biol. 2013;170(1):119–124. doi: 10.1016/j.ejogrb.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 48.Sprague AE, Dunn SI, Fell DB, Harrold J, Walker MC, Kelly S, et al. Measuring quality in maternal-newborn care: developing a clinical dashboard. J Obstet Gynaecol Can. 2013;35(1):29–38. doi: 10.1016/s1701-2163(15)31045-8. [DOI] [PubMed] [Google Scholar]
- 49.Crofts J, Moyo J, Ndebele W, Mhlanga S, Draycott T, Sibanda T. Adaptation and implementation of local maternity dashboards in a Zimbabwean hospital to drive clinical improvement. Bull World Health Organ. 2014;92(2):146–152. doi: 10.2471/BLT.13.124347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gjære EA, Lillebo B. Designing privacy-friendly digital whiteboards for mediation of clinical progress. BMC Med Inform Decis Mak. 2014;14:27. doi: 10.1186/1472-6947-14-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.McLaughlin N, Afsar-Manesh N, Ragland V, Buxey F, Martin NA. Tracking and sustaining improvement initiatives: leveraging quality dashboards to lead change in a neurosurgical department. Neurosurgery. 2014;74(3):235–243. doi: 10.1227/NEU.0000000000000265. [DOI] [PubMed] [Google Scholar]
- 52.Russell M, Hogg M, Leach S, Penman M, Friel S. Developing a general ward nursing dashboard. Nurs Stand. 2014;29(15):43–49. doi: 10.7748/ns.29.15.43.e9247. [DOI] [PubMed] [Google Scholar]
- 53.Swartz JL, Cimino JJ, Fred MR, Green RA, Vawdrey DK. Designing a clinical dashboard to fill information gaps in the emergency department. In: AMIA annual symposium proceedings; 2014. p. 1098. [PMC free article] [PubMed]
- 54.Hartzler AL, Chaudhuri S, Fey BC, Flum DR, Lavallee D. Integrating patient-reported outcomes into spine surgical care through visual dashboards: lessons learned from human-centered design. EGEMS. 2015;3(2):1133. doi: 10.13063/2327-9214.1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shaw SJ, Jacobs B, Stockwell DC, Futterman C, Spaeder MC. Effect of a real-time pediatric ICU safety bundle dashboard on quality improvement measures. Jt Commun J Qual Patient Saf. 2015;41(9):414–20. doi: 10.1016/s1553-7250(15)41053-0. [DOI] [PubMed] [Google Scholar]
- 56.Hertzum M, Simonsen J. Effects of electronic emergency-department whiteboards on clinicians’ time distribution and mental workload. Health Inform J. 2016;22(1):3–20. doi: 10.1177/1460458214529678. [DOI] [PubMed] [Google Scholar]
- 57.Karami M, Safdari R. From information management to information visualization: development of radiology dashboards. Appl Clin Inform. 2016;7(2):308–329. doi: 10.4338/ACI-2015-08-RA-0104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mazor I, Heart T, Even A. Simulating the impact of an online digital dashboard in emergency departments on patients length of stay. J Decis Syst. 2016;25(sup1):343–353. doi: 10.1080/12460125.2016.1187422. [DOI] [Google Scholar]
- 59.Franklin A, Gantela S, Shifarraw S, Johnson TR, Robinson DJ, King BR, et al. Dashboard visualizations: supporting real-time throughput decision-making. J Biomed Inform. 2017;211:21–71. doi: 10.1016/j.jbi.2017.05.024. [DOI] [PubMed] [Google Scholar]
- 60.Lee K, Jung SY, Hwang H, Yoo S, Baek HY, Baek RM, et al. A novel concept for integrating and delivering health information using a comprehensive digital dashboard: an analysis of healthcare professionals' intention to adopt a new system and the trend of its real usage. Int J Med Inform. 2017;97:98–108. doi: 10.1016/j.ijmedinf.2016.10.001. [DOI] [PubMed] [Google Scholar]
- 61.Staib A, Sullivan C, Jones M, Griffin B, Bell A, Scott I. The ED-inpatient dashboard: Uniting emergency and inpatient clinicians to improve the efficiency and quality of care for patients requiring emergency admission to hospital. Emerg Med Australas. 2017;29(3):363–366. doi: 10.1111/1742-6723.12661. [DOI] [PubMed] [Google Scholar]
- 62.Martin N, Bergs J, Eerdekens D, Depaire B, Verelst S. Developing an emergency department crowding dashboard: a design science approach. Int Emerg Nurs. 2018;39:68–76. doi: 10.1016/j.ienj.2017.08.001. [DOI] [PubMed] [Google Scholar]
- 63.Martinez DA, Kane EM, Jalalpour M, Scheulen J, Rupani H, Toteja R, et al. An electronic dashboard to monitor patient flow at the johns hopkins hospital: communication of key performance indicators using the donabedian model. J Med Syst. 2018;42(8):133. doi: 10.1007/s10916-018-0988-4. [DOI] [PubMed] [Google Scholar]
- 64.Romero-Brufau S, Kostandy P, Maass KL, Wutthisirisart P, Sir M, Bartholmai B, et al. Development of data integration and visualization tools for the Department of Radiology to display operational and strategic metrics. In: AMIA annual symposium proceedings, San Francisco, CA, vol. 2018;2018. p. 942–51. [PMC free article] [PubMed]
- 65.Shailam R, Botwin A, Stout M, Gee MS. Real-time electronic dashboard technology and its use to improve pediatric radiology workflow. Curr Probl Diagn Radiol. 2018;47(1):3–5. doi: 10.1067/j.cpradiol.2017.03.002. [DOI] [PubMed] [Google Scholar]
- 66.Yoo J, Jung KY, Kim T, Lee T, Hwang SY, Yoon H, et al. Real-time autonomous dashboard for the emergency department: 5-year case study. JMIR mHealth uHealth. 2018;6(11):e10666. doi: 10.2196/10666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hester G, Lang T, Madsen L, Tambyraja R, Zenker P. Timely data for targeted quality improvement interventions: use of a visual analytics dashboard for bronchiolitis. Appl Clin Inform. 2019;10(01):168–174. doi: 10.1055/s-0039-1679868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jebraeily M, ValzadeHasanloei MA, Rahimi B, Saeideh S. Design of a management dashboard for the intensive care unit: determining key performance indicators and their required capabilities. Appl Med Inform. 2019;41(3):111–21. [Google Scholar]
- 69.Randell R, Alvarado N, McVey L, Ruddle RA, Doherty P, Gale C, et al. Requirements for a quality dashboard: lessons from National Clinical Audits. In: AMIA annual symposium proceedings, Washington, DC, USA, vol. 2019; 2020. p. 735–44. [PMC free article] [PubMed]
- 70.Schmidt T, Brabrand M, Lassen AT, Wiil UK. Design and evaluation of a patient monitoring dashboard for emergency departments. Stud Health Technol Inform. 2019;264:788–792. doi: 10.3233/SHTI190331. [DOI] [PubMed] [Google Scholar]
- 71.van Deen WK, Cho ES, Pustolski K, Wixon D, Lamb S, Valente TW, et al. Involving end-users in the design of an audit and feedback intervention in the emergency department setting–a mixed methods study. BMC Health Serv Res. 2019;19(1):270. doi: 10.1186/s12913-019-4084-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Dixit RA, Hurst S, Adams KT, Boxley C, Lysen-Hendershot K, Bennett SS, et al. Rapid development of visualization dashboards to enhance situation awareness of COVID-19 telehealth initiatives at a multihospital healthcare system. J Am Med Inform Assoc. 2020;27(9):1456–1461. doi: 10.1093/jamia/ocaa161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Janssen A, Donnelly C, Kay J, Thiem P, Saavedra A, Pathmanathan N, et al. Developing an intranet-based lymphedema dashboard for breast cancer multidisciplinary teams: design research study. J Med Internet Res. 2020;22(4):e13188. doi: 10.2196/13188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Williams AA, Jallo J, Yoo EJ. Improving the quality of visualization dashboards in critical care: a mixed-methods study. Am J Med Qual. 2020 doi: 10.1177/1062860620946109. [DOI] [PubMed] [Google Scholar]
- 75.Yigitbasioglu OM, Velcu O. A review of dashboards in performance management: implications for design and research. Int J Account Inf Syst. 2012;13(1):41–59. doi: 10.1016/j.accinf.2011.08.002. [DOI] [Google Scholar]
- 76.Eckerson WW. Performance dashboards: measuring, monitoring, and managing your business. Hoboken: Wiley; 2010. [Google Scholar]
- 77.Ghazisaeidi M, Safdari R, Torabi M, Mirzaee M, Farzi J, Goodini A. Development of performance dashboards in healthcare sector: key practical issues. Acta Inform Med. 2015;23(5):317–321. doi: 10.5455/aim.2015.23.317-321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Randell R, Alvarado N, Elshehaly M, McVey L, West RM, Doherty P, et al. Design and evaluation of an interactive quality dashboard for national clinical audit data: a realist evaluation. Southampton: National Institute for Health and Care Research; 2022. 10.3310/WBKW4927. [PubMed]
- 79.Etxeberria L, Sagardui G, Belategi L. Quality aware software product line engineering. J Braz Comp Soc. 2008;14(1):57–69. doi: 10.1007/BF03192552. [DOI] [Google Scholar]
- 80.Hamborg K-C, Vehse B, Bludau H-B. Questionaire based usability evaluation of hospital information systems. Electron J Inf Syst Eval. 2004;7(1):21–30. [Google Scholar]
- 81.Rasmussen R. Electronic whiteboards in emergency medicine: a systematic review. In: Proceedings of the 2nd ACM SIGHIT international health informatics symposium. Miami: Association for Computing Machinery; 2012. p. 483–92. 10.1145/2110363.2110418.
- 82.Jespersen, S. Dashboard design guidelines for improved evidence based decision making in public health in developing countries. Master thesis, Norway: University of Oslo; 2017.
- 83.Cabitza F, Sarini M, Simone C, Telaro M. When once is not enough: the role of redundancy in a hospital ward setting. In: Proceedings of the 2005 international ACM SIGGROUP conference on Supporting group work. Sanibel Island: ACM Press; 2005. p. 158–67. 10.1145/1099203.1099234.
- 84.Freeman T. Using performance indicators to improve health care quality in the public sector: a review of the literature. Health Serv Manag Res. 2002;15(2):126–137. doi: 10.1258/0951484021912897. [DOI] [PubMed] [Google Scholar]
- 85.Papazoglou MP, Van Den Heuvel W-J. Service oriented architectures: approaches, technologies and research issues. VLDB J. 2007;16(3):389–415. doi: 10.1007/s00778-007-0044-3. [DOI] [Google Scholar]
- 86.Hoekzema G, Abercrombie S, Carr S, Gravel JW, Jr, Hall KL, Kozakowski S, et al. Residency "dashboard": family medicine GME's step towards transparency and accountability? Ann Fam Med. 2010;8(5):470. doi: 10.1370/afm.1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.McLeod B, Zaver F, Avery C, Martin DP, Wang D, Jessen K, et al. Matching capacity to demand: a regional dashboard reduces ambulance avoidance and improves accessibility of receiving hospitals. Acad Emerg Med. 2010;17(12):1383–1389. doi: 10.1111/j.1553-2712.2010.00928.x. [DOI] [PubMed] [Google Scholar]
- 88.Johnson CD, Miranda R, Osborn HH, Miller JM, Prescott SL, Aakre KT, et al. Designing a safer radiology department. AJR Am J Roentgenol. 2012;198(2):398–404. doi: 10.2214/AJR.11.7234. [DOI] [PubMed] [Google Scholar]
- 89.Serb C. Effective dashboards: What to measure and how to show it. Hosp Health Netw. 2011;85(6):8. [PubMed] [Google Scholar]
- 90.Almasi S, Rabiei R, Moghaddasi H, Vahidi-Asl M. Emergency department quality dashboard; a systematic review of performance indicators, functionalities, and challenges. Arch Acad Emerg Med. 2021;9(1):e47. doi: 10.22037/aaem.v9i1.1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Moghaddasi H, Rabiei R, Asadi F, Ostvan N. Evaluation of nursing information systems: application of usability aspects in the development of systems. Healthc Inform Res. 2017;23(2):101–108. doi: 10.4258/hir.2017.23.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Steichen B, Fu B. Towards adaptive information visualization: a study of information visualization aids and the role of user cognitive style. Front Artif Intell. 2019;2:22. doi: 10.3389/frai.2019.00022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Mawad F, Trías M, Giménez A, Maiche A, Ares G. Influence of cognitive style on information processing and selection of yogurt labels: insights from an eye-tracking study. Food Res Int. 2015 doi: 10.1016/j.foodres.2015.04.023. [DOI] [PubMed] [Google Scholar]
- 94.Ziemkiewicz C, Ottley A, Crouser RJ, Chauncey K, Su SL, Chang R. Understanding visualization by understanding individual users. IEEE Comput Graph Appl. 2012;32(6):88–94. doi: 10.1109/MCG.2012.120. [DOI] [PubMed] [Google Scholar]
- 95.McLellan S, Muddimer A, Peres SC. The effect of experience on System Usability Scale ratings. J Usability Stud. 2012;7(2):56–67. [Google Scholar]
- 96.Tøndel IA. Visualization control for event-based public display systems used in a hospital setting. In: Proceedings of the 16th Nordic conference on information security technology for applications. Berlin: Springer; 2011. p. 240–55. 10.1007/978-3-642-29615-4_17.
- 97.Bardram JE, Bossen C. A web of coordinative artifacts: collaborative work at a hospital ward. In: Proceedings of the 2005 international ACM SIGGROUP conference on Supporting group work. New York: Association for Computing Machinery; 2005. 10.1145/1099203.1099235.
- 98.Olsha-Yehiav M, Einbinder JS, Jung E, Linder JA, Greim J, Li Q, et al. Quality Dashboards: technical and architectural considerations of an actionable reporting tool for population management. In: AMIA annual symposium proceedings, vol. 2006; 2006. p. 1052. [PMC free article] [PubMed]
- 99.Gordon J, Richardson E. Continuous improvement in the management of hospital wards: the use of operational dashboards. Int J Manag. 2013;30(4):414. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Appendix A. The result of qualitative evaluation of studies.
Data Availability Statement
All data used in the publication of this work were obtained from published studies. The abstracts for these studies are available in the web of science, pubmed, embase, and scopus database.