Abstract
Prolonged intrauterine retention of fetal bones during an abortion procedure can lead to secondary infertility. This review aimed to raise awareness among obstetric/gynaecologists about the possibility of this condition. A total of 17 case reports, seven case series and one retrospective study were included in this review, with 75 patients in total. Overall, 60% had a pregnancy termination in the second trimester, while 20% had a termination during the first trimester. Hysteroscopic resection was used to remove the intrauterine fetal bones in 69% of patients. In total, 59% of patients conceived following the procedure, 1% conceived despite the presence of intrauterine bones, 24% could not conceive at the time of the study and 16% had an unknown outcome. Transvaginal ultrasound was used for diagnosis in 41 (55%) patients, while pelvic ultrasound was used in 21 (28%) patients. In conclusion, secondary infertility is a common occurrence after a dilation and curettage procedure partially due to fetal bone retention. The gold standard for an accurate diagnosis and treatment is hysteroscopy.
Keywords: Incomplete Abortion, Abortion, Therapeutic Abortion, Miscarriage, Infertility
According to the united nations medium-variant projection, the global fertility rate declined from 3.2 live births per woman in 1990 to 2.5 in 2019 and is expected to reach 2.2 live births per woman in 2050 and 1.9 in 2100.1 Each year, more than 227 million women become pregnant worldwide, out of which roughly two-thirds deliver live infants, while the remaining one-third end in miscarriage, stillbirth or induced abortion.2 Globally, one in four pregnancies (25%) end in abortion, of which nearly half (45%) are unsafe abortions.3 Worldwide, 8–12% of couples of reproductive age are affected by infertility.4 It is estimated that one in four couples in developing countries and one in seven couples in developed countries suffer from infertility. The prevalence of infertility in some parts of the world, such as South and Central Asia, the Middle East, North Africa, Sub-Saharan Africa and Central and Eastern Europe, is as high as 30%.5 In the USA, about 1.3 million women are treated annually for infertility, while 2% undergo treatment with assisted reproductive technology.6
Secondary infertility is the most common form of infertility. It is commonly seen in areas with unsafe abortion practices and maternity care, which are often associated with increased chances of infection.7 Post-abortion infection can lead to future fertility problems resulting from damage to the fallopian tubes or direct damage to the endometrial lining leading to adhesions (Asherman’s syndrome). Rarely, surgical mid-trimester abortions can lead to retained fetal bones and cause subfertility.8 As reported by Izhar et al., prolonged intrauterine retention of any fetal bone can lead to secondary infertility.9 Although rare, retained fetal bones are more commonly seen in an anomalous uterus.10 The exact incidence remains unclear; however, the incidence was reported to be 0.15% among 2000 diagnostic hysteroscopies.9,11 Apart from subfertility, retained fetal bones may also present with chronic pelvic pain, dysmenorrhoea, abnormal uterine bleeding and dyspareunia.10 Prolonged retention of fetal bones may lead to chronic inflammation and endometrial damage, making it harder to achieve fertility.10
The present review was focused on outlining the pathophysiology, clinical presentations, diagnostic modalities and treatment options and outcomes in patients with secondary infertility due to fetal bone retention. Sometimes, patients with this condition are asymptomatic and fetal bones can be found as an incidental finding on an ultrasound or hysteroscopy, as part of the infertility workup.10 A high level of suspicion is necessary to diagnose this rare condition; hence, this review aimed to raise awareness among obstetric/gynaecologists about the possibility of this condition.
PATHOPHYSIOLOGY AND HYPOTHESIS OF SECONDARY INFERTILITY DUE TO FETAL BONE RETENTION
Prolonged intrauterine retention of any fetal bone can lead to secondary infertility. The earliest report of calcified tissue of fetal origin in utero goes back to 1966.12 These calcified tissues, when deeply embedded in the uterine mucosa, may present with the same contraceptive effect as an intrauterine contraceptive device, thereby causing secondary infertility.13,14 On imaging, these tissues usually present as echogenic foci partially embedded in the endometrial lining, an intrauterine foreign body, thin plates of bone or many fetal bones with a nearly intact morphology.9,12,15,16 Microscopic examinations have revealed necrotic bony trabeculae, bone marrow and chronic inflammation in the intervening spaces within the endometrium during its proliferative phase.16,17
In 1982, Dawood et al. posited that the presence of the fetal bones can act as uterine synechiae or an intrauterine device (IUD) and thus could prevent pregnancy. According to their study, fetal bones near the fundal region also elevated the concentration of endometrial prostaglandin F2 alpha in that region, leading to infertility.18 In addition, Lewis et al. discovered that the pattern of prostanoid increase was similar to that seen in IUD users.19 Another pathogenesis for this condition is endometrial osseous metaplasia, a rare entity.20 However, a previous pregnancy history is reported in >80% of these cases.21 There are two theories regarding the origin of osseous metaplasia: 1) persistence of embryonic bones that keep developing after curettage; and 2) induction of a process of osteogenesis by one’s embryonal cells, provoking the osseous differentiation of hypothetical pluripotent endometrial cells. This process can be differentiated from retained fetal bones by comparing the patient’s short tandem repeats and the bony sample.22
In a study by Wani et al., histopathological examination of retrieved endometrial tissue from 10 patients revealed nonspecific lymphocytic infiltrate with interspersed lamellar bone in six (42.8%) patients and trabecular bone in four (28.5%) patients with scanty endometrial glands and stroma in various hormonal phases. These results confirmed the diagnosis of osseous metaplasia of the endometrial lining.23
Methods
PROTOCOL
This systematic review consists of analysis from published case reports, case series and retrospective studies. It was conducted according to the standards and guidelines established in the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines.
SEARCH STRATEGY
A systematic literature search of four academic databases was conducted in October 2021: PubMed (National Library of Medicine, Maryland, USA), ScienceDirect (Elsevier, Amsterdam, Netherlands), Cochrane (Cochrane Library, London, England) and Google Scholar (Google, California, USA). The search included all relevant articles from inception up to October 2021. Regular terms used were ‘infertility’ and ‘retained fetal bones’. Terms used from the Medical Subject Headings database were ‘infertility, female’ and/or ‘retained’ and/or ‘fetal bones’ and/or ‘abortion’. The search terms were kept broad to encompass all possible relevant studies. Inclusion and exclusion criteria were then applied. The first and second authors screened the title and abstract, then the full paper was read to determine its relevance. At the end of the search, any duplicate articles were eliminated using Microsoft Excel. All selected articles reporting patients with retained fetal bones from a previous pregnancy termination who presented with infertility were included in the analysis.
STUDY SELECTION, EXTRACTION AND ANALYSIS
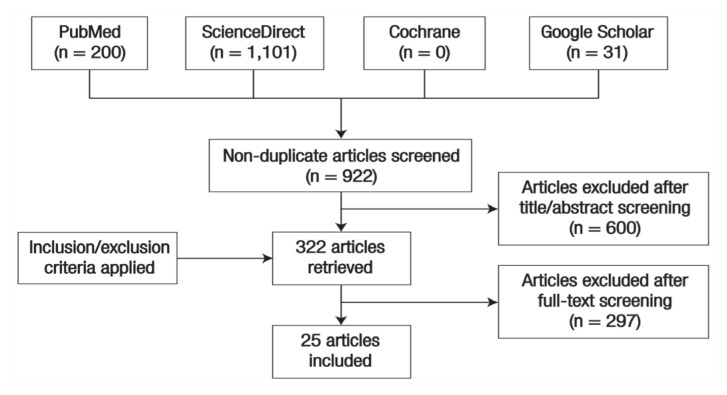
The literature search yielded 1,119 studies. Study selection was completed by three independent, parallel reviewers and performed in two separate stages: (1) title/abstract screening, followed by (2) full-text screening. Data extraction was performed by three investigators, who resolved discrepancies via consensus. A total of 410 duplicates were manually removed and the three investigators independently reviewed all titles and abstracts. Subsequently, 600 studies were deemed irrelevant and excluded after screening their titles and abstracts. The full texts of the articles regarded as potentially eligible for consideration were extracted and screened for further analysis based on the predefined inclusion and exclusion criteria. Finally, 25 studies were selected for inclusion in the review after the full-text screening [Figure 1]. Disagreements between the authors were resolved through consensus and active discussion.
Figure 1.
PRISMA flow diagram depicting search strategy of all relevant articles from inception up to October 2021.
INCLUSION/EXCLUSION CRITERIA
The eligibility criteria were determined following the patient, intervention, comparison and outcome approach. The following inclusion criteria were considered: participants of all ages, articles published in and after 1982, human subjects and articles written in English. The exclusion criteria consisted of review articles, animal studies, studies published in a language other than English and the absence or unclear reporting of the infertility complication status in post-abortion patients.
QUALITY APPRAISAL
The first and second authors performed quality appraisals. A total of 17 case reports, seven case series and one retrospective study were included in the review, comprising a total of 75 patients.
Results
CLINICAL MANIFESTATIONS
Overall, 25 published papers with a total of 75 cases of retained fetal bones were included. In all 75 cases, women presented with infertility after the termination of pregnancy in either the first or second trimester. Other presenting symptoms included dysmenorrhoea, menorrhagia, chronic pelvic pain, dyspareunia and vaginal discharge. The comprehensive literature review concluded that most patients had a previous pregnancy termination during the second trimester. A total of 45 (60%) cases had a termination in the second trimester, while 15 (20%) had a pregnancy termination during the first trimester. The exact date of termination was unknown for 15 (20%) patients. The interval between termination and reporting of symptoms varied. The shortest interval recorded was 12 months and the longest was 180 months.24,25 In a study by Petrakis et al., a patient presented with chronic pelvic pain and infertility 12 months after a miscarriage at 19 weeks gestation due to placental abruption.24 A summary of cases with retained fetal bones seen in patients presenting with infertility after either a spontaneous or induced pregnancy termination is provided in Table 1.8–10,13,14,16,18,24–41
Table 1.
Summary of cases of retained fetal bones seen in patients presenting with infertility after either a spontaneous or induced pregnancy termination8–10,13,14,16,18,24–41
| Authors and year of publication | Number of cases presenting with infertility | Age in years | Interval between TOP or miscarriage and diagnosis in months | Gestational age at TOP or miscarriage in weeks | Clinical presentation | Diagnostic imaging method | Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|
| Srofenyoh et al.8 (2006) | 3 | 35 | NK | 16 (n = 2); NK (n = 1) | Chronic pelvic pain (n = 1); | Pelvic ultrasound | D&E | Conceive (n = 2); Had not conceived (n = 1) |
| 30 | Dyspareunia (n = 1); | |||||||
| 42 | Secondary Infertility (n = 1) | |||||||
| Izhar et al.9 (2015) | 1 | 36 | NK | 20 | Secondary infertility | Transvaginal ultrasound and SIS | D&C | Scheduled for repeat SIS and kept on high-dose oestrogen. Has not conceived |
| Gainder et al.10 (2018) | 18 | NK | >24 (n = 5); 24–36 (n = 6); >36 (n = 7) | First Trimester (n = 5); Second Trimester (n = 13) | Secondary infertility; Menorrhagia (n = 5); Amenorrhoea (n = 2); Metrorrhagia (n = 4); Chronic pelvic pain (n = 2) | Pelvic ultrasound (n = 17); Hysteroscopy (n = 1) | Hysteroscopy (n = 15); D&C (n = 3) | Conceived (n = 5); Had not conceived (n = 7); Not followed up for conception (n = 6) |
| Lanzarone and Pardey14 (2009) | 1 | 36 | NK | NK | Secondary infertility | Hysteroscopy | Hysteroscopy | SIS determined a normal cavity |
| Patil et al.13 (2013) | 1 | 28 | NK | 6 | Menorrhagia | Hysteroscopy | Hysteroscopy | NK |
| Dajani and Khalaf16 (1985) | 1 | 26 | 18 | 18 | Secondary infertility | Hysterosal-pingogram | D&C | Conceived |
| Dawood and Jarrett18 (1982) | 1 | 22 | 72 | 10 | Secondary infertility | Hysterosal-pingogram | Hysteroscopy with D&C | Had not conceived. |
| Petrakis et al.24 (2019) | 1 | 28 | 12 | 19 | Chronic pelvic pain | Transvaginal ultrasound | Hysteroscopy scheduled but did not comply. | Conceived without removal of fetal bones. |
| Moon et al.25 (1997) | 11 | 26–37 | 12–60 (n = 10); 180 (n = 1) | 16–24 | Secondary infertility | Transvaginal ultrasound | D&C | Conceived (n = 10); Bilateral tubal obstruction. Had not conceived (n = 1) |
| Melius et al.26 (1991) | 1 | 33 | 108 | NK | Secondary infertility | Hysterosal-pingogram | Hysteroscopy | Had not conceived. |
| Chan27 (1996) | 1 | 34 | 108 | 16 | Secondary infertility, Dysmenorrhoea | Transvaginal ultrasound | Hysteroscopy | Returned to a normal menstrual cycle. Not followed up for conception. |
| Arora et al.28 (1998) | 2 | 28 | Case 1: 48 | Case 1: 16 | Secondary infertility | Hysterosal-pingogram | Hysteroscopy | Case 1: Returned to a normal menstrual cycle |
| 27 | Case 2: NK | Case 2: 12 | Case 2: Conceived | |||||
| Tulandi and Sammour29 (2001) | 1 | 33 | 96 | 6 | Secondary infertility | Hysterosal-pingogram | Hysteroscopy | NK |
| Elford and Claman30 (2003) | 1 | 36 | 15 | Late first trimester | Secondary infertility | Pelvic ultrasound | Hysteroscopy with D&C | Conceived |
| Goldberg and Roberts31 (2008) | 1 | 32 | NK | 22 | Secondary infertility | Transvaginal ultrasound | Hysteroscopy | Conceived |
| Kramer and Rhemrev32 (2008) | 1 | 32 | 96 | 12 | Secondary infertility | Hysteroscopy | Hysteroscopy | Conceived |
| Singla et al.33 (2012) | 1 | 23 | 36 | 10 | Secondary infertility | Transvaginal US | Hysteroscopy | Advised a hysterosal-pingogram for tubal patency. Had not conceived. |
| Xiao et al.34 (2014) | 1 | 30 | 108 | 15 | Secondary infertility | Hysteroscopy | Hysteroscopy | Conceived |
| Mishra et al.35 (2018) | 1 | 28 | 60 | 15 | Secondary infertility | Transvaginal ultrasound | Hysteroscopy | Conceived |
| Mahdavi et al.36 (2019) | 1 | 25 | 24 | 15 | Secondary infertility | Hysterosal-pingogram | Hysteroscopy | Conceived |
| Graham et al.37 (2000) | 11 | 23–36 | 24–144 | 10 (n = 2), 12 (n = 1), 14 (n = 3), 16 (n = 2), 20 (n = 1), 24 (n = 1), 26 (n = 1) | Secondary infertility | Transvaginal ultrasound | Hysteroscopy | Conceived (n = 8); Had not conceived (n = 2); NK (n = 1) |
| Pereira et al.38 (2014) | 7 | 24–40 | NK | NK | Secondary infertility | Transvaginal ultrasound (n = 5); Hysteroscopy (n = 2) | Hysteroscopy | Conceived (n = 5); Did not conceive (n = 2) |
| Grigore et al.39 (2014) | 2 | 41 | NK | NK | Secondary infertility | Transvaginal ultrasound | Hysteroscopy | Case 1: Conceived; |
| 34 | Case 2: Resolution of symptoms | |||||||
| Bozdag et al.40 (2015) | 1 | 30 | 10 | NK | Secondary infertility | Transvaginal ultrasound | Hysteroscopy | Conceived |
| Awowole et al.41 (2021) | 4 | NK | NK | NK | Secondary infertility | Transvaginal ultrasound | Hysteroscopy | Conceived |
TOP = termination of pregnancy; NK = not known; D&E = dilation and evacuation; SIS = saline infusion sonography; D&C = dilation and curettage.
DIAGNOSIS
Pelvic ultrasound proved to be an excellent imaging tool for diagnosis in any female with infertility; transvaginal and abdominal ultrasound was used in 41 (55%) and 21 (28%) of the 75 patients, respectively. Areas of interest during the transvaginal ultrasound (TVS) included the patency of fallopian tubes, the size of the uterus and the presence of echogenic areas suggestive of fetal bones in the endometrial cavity. One (1%) patient had a saline infusion sonography (SIS) procedure performed in addition to a TVS, in which highly echogenic areas in the anterior wall of the uterus were visualised.9 Hysterosalpingogram (HSG) was another method used in seven (9%) patients, which looks for filling defects and space-occupying irregularities in the uterine cavity and fallopian tubes. Additionally, hysteroscopy provided both diagnostic and therapeutic benefits in five (7%) patients.
TREATMENT AND OUTCOME
A hysteroscopic resection alone was performed in 52 patients (69%), while it was performed along with dilation and curettage (D&C) in two (3%) patients. Petrakis et al. presented a case where one (1%) patient had a hysteroscopy scheduled but did not comply with treatment recommendations.25 Other treatment methods used included D&C without hysteroscopy in 17 (23%) patients and dilation and evacuation (D&E) in three (4%) patients. Hysteroscopic resection was used most frequently for the removal of intrauterine fetal bones [Table 1].
Regarding patients experiencing a successful pregnancy post-treatment, the review revealed that 44 (59%) patients conceived following the removal of retained intrauterine fetal bones. One (1%) case was identified in which a patient conceived despite the presence of intrauterine bone fragments.24 In comparison, 18 (24%) patients had not conceived at the time of the study. The remaining 12 (16%) patients either were not followed up for infertility or had other outcomes, or the details of their follow-up are unknown. Other outcomes following treatment that were reported included the patient’s return to a normal menstrual cycle and the resolution of presenting symptoms.
Discussion
Although rare, the intrauterine retention of fetal bones is a potential complication following an abortion, often in the second or third trimester.34 Abortions occurring in the first trimester, when fetal bone ossification has not yet completely occurred, could involve dystrophic calcification of retained products that could also lead to intrauterine bone formation.10 However, it could also occur secondary to osseous metaplasia due to the chronic inflammation of the endometrium.34 Hypercalcaemia, hyperphosphatemia and hypervitaminosis D are rarer causes of this endometrial calcification.10 The incidence of this complication is thought to be underestimated, as symptoms experienced by patients are not readily attributed to the abortion, leading to a considerable delay between the abortion and diagnosis.42
Retained fetal bones exert an intrauterine device (IUD)-like effect, resulting in secondary infertility, and their removal could reverse this effect.34 As seen from the outcomes of included case reports, D&C procedures for the evacuation of the prior non-viable fetus had preceded secondary infertility and the removal of retained fetal bones, most commonly via hysteroscopy, allowed these patients to conceive.6,16,24,25,30–36
The present review found that hysteroscopic removal was performed in 69% of patients, enabling 59% to conceive after the procedure. Other treatment methods used included D&C without hysteroscopy in 23% of patients and D&E in 4% of patients.
In a study by Gainder et al., the data of 6,435 patients who visited a fertility clinic in India were retrospectively reviewed, out of which 18 patients received ‘retained fetal bone’ as the sole diagnosis for their infertility.10 All patients underwent diagnostic hysteroscopy and had the bony fragments removed via hysteroscopy (n = 15) or D&C (n = 3). Despite following up on 12 of the 18 patients for up to 6 years, spontaneous conception was only noted in five patients. It must be noted that these five patients had presented for secondary infertility within 3 years of their previous abortion, while the remaining seven had presented after >3 years. This finding led the authors to conclude that any changes associated with the retention of bony fragments are expected to regress with a return of fertility only if the bony fragments are removed quickly and provided there is no tubal damage or formation of uterine synechiae following the abortion. The long-term presence of bony fragments in the endometrial cavity could have led to endometritis, thus accounting for persistent infertility. The authors also postulated that a few bony fragments could have become so deeply embedded in the endometrium that they could not be successfully removed; thus, these could have continued to act as foreign bodies, preventing intrauterine pregnancy.10
Petrakis et al. similarly reported that achieving childbearing is possible, with spontaneous conception and a high live birth rate, once bony fragments have been removed from the uterine cavity. However, Petrakis et al. also reported the case of a successful live pregnancy, conceived spontaneously and carried to term, in a patient with calcium salt deposits in the placenta and the intrauterine retention of fetal bones from a previous miscarriage at 19 weeks gestation a year prior.24 To date, this is the only reported case where a patient could conceive despite the presence of intrauterine fetal bones.
In addition to secondary infertility, intrauterine fetal bones could also cause abnormal uterine bleeding, menorrhagia, dysmenorrhea, chronic pelvic pain and abnormal vaginal discharge.34 It was suggested that pelvic pain and dysmenorrhoea could be due to an increase in the levels of prostaglandins from the inflammatory reaction.10 Removal of bony fragments could thus reverse these symptoms.8,10,15,27
Pelvic ultrasounds, pelvic X-rays, hysterosalpingograms and hysteroscopies have been used to detect intrauterine bony fragments.10,37 Shadows observed on ultrasonography are often not definitive for diagnosis but could guide the hysteroscopic removal of these bony fragments.10 A report of calcifications in the endometrium by radiologists is also not definitive for diagnosis. However, it should still raise suspicion about retained fetal bones, especially when coupled with a history of prior abortion.11 An accurate diagnosis is best obtained via hysteroscopy, which will reveal osseous fragments embedded within the endometrium. Although D&C may also be employed to remove these bony fragments, it is a less commonly choice for treatment. Hysteroscopy plays a vital role as a management option, as bony fragments may simultaneously be retrieved during the procedure.10
Conclusion
Secondary infertility is a common occurrence after a D&C procedure. In second-trimester abortions, fetal bone retention could be one of the causes of secondary infertility. The theories discussed in the studies of infertility due to fetal bone retention included elevated endometrial prostaglandin F2, osseous metaplasia and chronic inflammation. To achieve another pregnancy, removal of these retained bones is recommended. The sooner the removal is made, the better are the chances of achieving a future pregnancy. Very rarely has there been reported conception despite the fetal bones retained in the uterine cavity. Besides secondary infertility, patients can also present with dysmenorrhea, menorrhagia, chronic pelvic pain, dyspareunia and vaginal discharge. The gold standard for an accurate diagnosis is hysteroscopy, which provides the added benefit of removing these fragments at the same sitting. Therefore, to improve outcomes and restore fertility in women presenting with secondary infertility after having a prior abortion, physicians must be wary of the possibility of fetal bone retention.
ACKNOWLEDGEMENT
The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS, or the U.S. Government. For more information, please visit HRSA.gov.
Footnotes
AUTHORS’ CONTRIBUTIONS
AA conceptualised and designed the work. AA and JAL collected, analysed and interpreted the data. AA, UM, HL and CP drafted the manuscript. All authors critically revised the manuscript and approved the final version.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
FUNDING
This work is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of an award totaling $473,925 with 15% financed by non-governmental sources.
References
- 1.United Nations Department of Economic and Social Affairs Population Division. World Fertility and Family Planning 2020: Highlights. New York, USA: United Nations; 2020. [Google Scholar]
- 2.Mesce D. Abortion Facts and Figures 2021. Washington, DC, USA: Population Reference Bureau; 2021. [Google Scholar]
- 3.Singh S, Remez L, Sedgh G, Kwok L, Onda T. Abortion Worldwide 2017 Uneven Progress and Unequal Access. New York: Guttmacher Institute; 2018. [Google Scholar]
- 4.Ombelet W, Cooke I, Dyer S, Serour G, Devroey P. Infertility and the provision of infertility medical services in developing countries. Hum Reprod Update. 2008;14:605–21. doi: 10.1093/humupd/dmn042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mascarenhas MN, Flaxman SR, Boerma T, Vanderpoel S, Stevens GA. National, regional, and global trends in infertility prevalence since 1990: A systematic analysis of 277 health surveys. PLoS Med. 2012;9:e1001356. doi: 10.1371/journal.pmed.1001356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Katz P, Showstack J, Smith JF, Nachtigall RD, Millstein SG, Wing H, et al. Costs of infertility treatment: Results from an 18-month prospective cohort study. Fertil Steril. 2011;95:915–21. doi: 10.1016/j.fertnstert.2010.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Inhorn MC, Patrizio P. Infertility around the globe: New thinking on gender, reproductive technologies and global movements in the 21st century. Hum Reprod Update. 2015;21:411–26. doi: 10.1093/humupd/dmv016. [DOI] [PubMed] [Google Scholar]
- 8.Srofenyoh E, Addison M, Dortey B, Kuffour P. Intrauterine retained fetal bones as a cause of secondary infertility. Ghana Med J. 2006;40:105–9. doi: 10.4314/gmj.v40i3.55262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Izhar R, Husain S, Tahir S, Husain S. Secondary infertility due to retained fetal bones diagnosed via saline sonography. J Coll Physicians Surg Pak. 2016;26:861–2. [PubMed] [Google Scholar]
- 10.Gainder S, Arora P, Dhaliwal LK. Retained intrauterine bony fragments as a cause of secondary infertility in a tertiary level Indian hospital. J Hum Reprod Sci. 2018;11:286–90. doi: 10.4103/jhrs.JHRS_33_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Makris N, Stefanidis K, Loutradis D, Anastasiadou K, Hatjipappas G, Antsaklis A. The incidence of retained fetal bone revealed in 2000 diagnostic hysteroscopies. JSLS. 2006;10:76–7. [PMC free article] [PubMed] [Google Scholar]
- 12.Roth E, Taylor HB. Heterotopic cartilage in the uterus. Obstet Gynecol. 1966;27:838–44. [PubMed] [Google Scholar]
- 13.Patil SB, Narchal S, Paricharak DG, More SS. Endometrial osseous metaplasia: Case report with literature review. Ann Med Health Sci Res. 2013;3:S10–2. doi: 10.4103/2141-9248.121209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lanzarone VF, Pardey JM. Retained intrauterine fetal bone as a rare cause of secondary infertility. Aust N Z J Obstet Gynaecol. 2009;49:700–1. doi: 10.1111/j.1479-828X.2009.01072.x. [DOI] [PubMed] [Google Scholar]
- 15.Cepni I, Kumbak B, Ocal P, Idil M, Aksu F. Infertility due to intra-uterine residual fetal bone fragments: Retained intrauterine fetal bone fragments. J Clin Ultrasound. 2004;32:253–5. doi: 10.1002/jcu.20028. [DOI] [PubMed] [Google Scholar]
- 16.Dajani YF, Khalaf SM. Intrauterine bone contraceptive device: An accident of nature. Fertil Steril. 1985;43:149–50. doi: 10.1016/S0015-0282(16)48335-4. [DOI] [PubMed] [Google Scholar]
- 17.Usha Kiran TS, Bhal PS. The potential consequence of early recognition and treatment of retained fetal bony fragments. J Obstet Gynaecol. 2002;22:443–4. doi: 10.1080/014436102320261177. [DOI] [PubMed] [Google Scholar]
- 18.Dawood MY, Jarrett JC., 2nd Prolonged intrauterine retention of fetal bones after abortion causing infertility. Am J Obstet Gynecol. 1982;143:715–17. doi: 10.1016/0002-9378(82)90120-X. [DOI] [PubMed] [Google Scholar]
- 19.Lewis V, Khan-Dawood F, King M, Beckmann C, Dawood MY. Retention of intrauterine fetal bone increases menstrual prostaglandins. Obstet Gynecol. 1990;75:561–3. [PubMed] [Google Scholar]
- 20.Umashankar T, Patted S, Handigund RS. Endometrial osseous metaplasia: Clinicopathological study of a case and literature review. J Hum Reprod Sci. 2010;3:102–4. doi: 10.4103/0974-1208.69329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Magudapathi C, Anathakrishnan R, Kalargala H. Osseous Meta-plasia of the Endometrium: A rare entity. J Obstet Gynaecol India. 2015;65:342–5. doi: 10.1007/s13224-014-0589-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cayuela E, Perez-Medina T, Vilanova J, Alejo M, Cañadas P. True osseous metaplasia of the endometrium: The bone is not from a fetus. Fertil Steril. 2009;91:1293e1–4. doi: 10.1016/j.fertnstert.2008.12.026. [DOI] [PubMed] [Google Scholar]
- 23.Wani AH, Parry AH, Feroz I, Jehangir M, Rashid M. Imaging of endometrial osseous metaplasia—An uncommon but treatable cause of infertility. Middle East Fertil Soc J. 2020;25:35. doi: 10.1186/s43043-020-00045-0. [DOI] [Google Scholar]
- 24.Petrakis E, Chatzipapas I, Papapanagiotou IK, Fotinopoulos P, Siemou P, Ntzeros K, et al. A successful pregnancy despite the presence of an intrauterine fetal bone fragment. Case Rep Obstet and Gynecol. 2019;2019:3064727. doi: 10.1155/2019/3064727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moon HS, Park YH, Kwon HY, Hong SH, Kim SK. Iatrogenic secondary infertility caused by residual intrauterine fetal bone after midtrimester abortion. Am J Obstet Gynecol. 1997;176:369–70. doi: 10.1016/S0002-9378(97)70500-3. [DOI] [PubMed] [Google Scholar]
- 26.Melius FA, Julian TM, Nagel TC. Prolonged retention of intra-uterine bones. Obstet Gynecol. 1991;78:919–21. [PubMed] [Google Scholar]
- 27.Chan NS. Intrauterine retention of fetal bone. Aust N Z J Obstet Gynaecol. 1996;36:368–71. doi: 10.1111/j.1479-828X.1996.tb02733.x. [DOI] [PubMed] [Google Scholar]
- 28.Arora P, Sharma RK, Sodhi B, Chattopadhayay AB. Foetal bones causing secondary infertility. Med J Armed Forces India. 1998;54:282–3. doi: 10.1016/S0377-1237(17)30570-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tulandi T, Sammour A. Retained fetal bones in the uterine cavity. J Am Assoc Gynecol Laparosc. 2001;8:179–80. doi: 10.1016/S1074-3804(05)60574-9. [DOI] [PubMed] [Google Scholar]
- 30.Elford K, Claman P. Novel treatment of a patient with secondary infertility due to retained fetal bone. Fertil Steril. 2003;79:1028–30. doi: 10.1016/S0015-0282(02)04919-1. [DOI] [PubMed] [Google Scholar]
- 31.Goldberg JM, Roberts S. Restoration of fertility after hysteroscopic removal of intrauterine bone fragments. Obstet Gynecol. 2008;112:470–2. doi: 10.1097/AOG.0b013e318173fd4c. [DOI] [PubMed] [Google Scholar]
- 32.Kramer HMC, Rhemrev JPT. Secondary infertility caused by the retention of fetal bones after an abortion: A case report. J Med Case Rep. 2008;2:208. doi: 10.1186/1752-1947-2-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Singla A, Gupta B, Guleria K. First trimester abortion: A rare cause of intrauterine bony spicules. Case Rep Obstet Gynecol. 2012;2012:701021. doi: 10.1155/2012/701021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xiao S, Tian Q, Xue M. Infertility caused by intrauterine fetal bone retention: A case report. J Med Case Rep. 2014;8:177. doi: 10.1186/1752-1947-8-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mishra N, Bharti R, Mittal P, Suri J, Pandey D. Retained intra-uterine foetal bones resulting in secondary infertility: A case report. Cureus. 2018;10:e2575. doi: 10.7759/cureus.2575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mahdavi A, Kazemian S, Koohestani E. Secondary infertility due to intrauterine fetal bone retention: A case report and review of the literature. Int J Reprod Biomed. 2019;17:591–4. doi: 10.18502/ijrm.v17i8.4825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Graham O, Cheng L, Parsons J. The ultrasound diagnosis of retained fetal bones in West African patients complaining of infertility. BJOG. 2000;107:122–4. doi: 10.1111/j.1471-0528.2000.tb11588.x. [DOI] [PubMed] [Google Scholar]
- 38.Pereira MC, Vaz MM, Miranda SP, Araújo SR, Menezes DB, das Chagas Medeiros F. Uterine cavity calcifications: A report of 7 cases and a systematic literature review. J Minim Invasive Gynecol. 2014;21:346–52. doi: 10.1016/j.jmig.2013.11.001. [DOI] [PubMed] [Google Scholar]
- 39.Grigore M, Blidaru I, Iordache F. Intrauterine foreign bodies, other than contraceptive devices and systems, may affect fertility – Report of two very different cases. Eur J Contracept Reprod Health Care. 2014;19:141–3. doi: 10.3109/13625187.2013.856406. [DOI] [PubMed] [Google Scholar]
- 40.Bozdag G, Mumusoglu S, Dogan S, Esinler I, Gunalp S. Osseous metaplasia and subsequent spontaneous pregnancy chance: A case report and review of the literature. Gynecol Obstet Invest. 2015;80:217–22. doi: 10.1159/000439529. [DOI] [PubMed] [Google Scholar]
- 41.Awowole I, Badejoko O, Ayegbusi E, Allen O, Loto O. Infertility due to prolonged retention of fetal bones: A case series. J Gynecol Surg. 2021;38:107–10. doi: 10.1089/gyn.2021.0045. [DOI] [Google Scholar]
- 42.Rådestad A, Flam F. Intrauterine retention of fetal bones after abortion. Acta Obstet Gynecol Scand. 1995;74:662–4. doi: 10.3109/00016349509013487. [DOI] [PubMed] [Google Scholar]