BACKGROUND:
Differences in long-term outcomes regarding types of colon resections are inconclusive, precluding patient counseling, effective screening, and personalized treatment.
OBJECTIVE:
This study aimed to compare long-term bowel function and quality of life in patients who underwent right or left hemicolectomy or sigmoid colon resection.
DESIGN:
This was a multicenter cross-sectional study.
SETTINGS:
Seven Dutch hospitals participated in this study.
PATIENTS:
This study included patients who underwent right or left hemicolectomy or sigmoid colon resection without construction of a permanent stoma between 2009 and 2015. Patients who were deceased, mentally impaired, or living abroad were excluded. Eligible patients were sent the validated Defecation and Fecal Continence and Short-Form 36 questionnaires.
MAIN OUTCOME MEASURES:
Constipation, fecal incontinence (both Rome IV criteria), separate bowel symptoms, and generic quality of life were the main outcomes assessed.
RESULTS:
This study included 673 patients who underwent right hemicolectomy, 167 who underwent left hemicolectomy, and 284 who underwent sigmoid colon resection. The median follow-up was 56 months. Sigmoid colon resection increased the likelihood of constipation compared to right and left hemicolectomy (OR, 2.92; 95% CI, 1.80–4.75; p < 0.001 and OR, 1.93; 95% CI, 1.12–3.35; p = 0.019). Liquid incontinence and fecal urgency increased after right hemicolectomy compared to sigmoid colon resection (OR, 2.15; 95% CI, 1.47–3.16; p < 0.001 and OR, 2.01; 95% CI, 1.47–2.74; p < 0.001). Scores on quality-of-life domains were found to be significantly lower after right hemicolectomy.
LIMITATIONS:
Because of the cross-sectional design, longitudinal data are still lacking.
CONCLUSIONS:
Different long-term bowel function problems occur after right or left hemicolectomy or sigmoid colon resection. The latter seems to be associated with more constipation than right or left hemicolectomy. Liquid incontinence and fecal urgency seem to be associated with right hemicolectomy, which may explain the decline in physical and mental generic quality of life of these patients. See Video Abstract at http://links.lww.com/DCR/C13.
DISFUNCIÓN INTESTINAL A LARGO PLAZO Y DISMINUCIÓN DE LA CALIDAD DE VIDA DESPUÉS DE LA CIRUGÍA DE CÁNCER DE COLON: SOLICITUD DE DETECCIÓN Y TRATAMIENTO PERSONALIZADOS
ANTECEDENTES:
Las diferencias en los resultados a largo plazo con respecto a los tipos de resecciones de colon no son concluyentes, lo que impide el asesoramiento preoperatorio del paciente y la detección eficaz y el tratamiento personalizado de la disfunción intestinal postoperatoria durante el seguimiento.
OBJETIVO:
Comparar la función intestinal a largo plazo y la calidad de vida en pacientes sometidos a hemicolectomía derecha o izquierda, o resección de colon sigmoide.
DISEÑO:
Estudio transversal multicéntrico.
AJUSTES:
Participaron siete hospitales holandeses.
PACIENTES:
Se incluyeron pacientes sometidos a hemicolectomía derecha o izquierda, o resección de colon sigmoide sin construcción de estoma permanente entre 2009 y 2015. Se excluyeron pacientes fallecidos, con discapacidad mental o residentes en el extranjero. A los pacientes elegibles se les enviaron los cuestionarios validados de Defecación y Continencia Fecal y Short-Form 36.
PRINCIPALES MEDIDAS DE RESULTADO:
Se evaluaron el estreñimiento, la incontinencia fecal (ambos criterios de Roma IV), los síntomas intestinales separados y la calidad de vida genérica.
RESULTADOS:
Se incluyeron 673 pacientes con hemicolectomía derecha, 167 con hemicolectomía izquierda y 284 con resección de colon sigmoide. La mediana de seguimiento fue de 56 meses (RIC 41-80). La resección del colon sigmoide aumentó la probabilidad de estreñimiento en comparación con la hemicolectomía derecha e izquierda (OR, 2,92, IC 95%, 1,80–4,75, p < 0,001 y OR 1,93, IC 95%, 1,12–3,35, p = 0,019). La incontinencia de líquidos y la urgencia fecal aumentaron después de la hemicolectomía derecha en comparación con la resección del colon sigmoide (OR, 2,15, IC 95%, 1,47–3,16, p < 0,001 y OR 2,01, IC 95%, 1,47–2,74, p < 0,001). Las puntuaciones en los dominios de calidad de vida fueron significativamente más bajas después de la hemicolectomía derecha.
LIMITACIONES:
Debido al diseño transversal, aún faltan datos longitudinales.
CONCLUSIONES:
Se producen diferentes problemas de función intestinal a largo plazo después de la hemicolectomía derecha o izquierda, o la resección del colon sigmoide. Este último parece estar asociado con más estreñimiento que la hemicolectomía derecha o izquierda. La incontinencia de líquidos y la urgencia fecal parecen estar asociadas a la hemicolectomía derecha, lo que puede explicar el deterioro de la calidad de vida física y mental en general de estos pacientes. Consulte Video Resumen en http://links.lww.com/DCR/C13. (Traducción—Dr. Yolanda Colorado)
Keywords: Bowel dysfunction, Colon cancer, Follow-up, Hemicolectomy, Postoperative
Worldwide, more than 1 million patients are diagnosed with colonic cancer every year.1 Developments in surgical techniques and adjuvant chemotherapy regimens resulted in a current 5-year survival rate of 64%.2 This implies that the long-term effects of surgery for colon cancer are becoming important to a growing number of people.
The 3 most performed resections for colon cancer, depending on the location of the tumor, are right hemicolectomy, left hemicolectomy, and sigmoid colon resection. A recent meta-analysis emphasized the magnitude of both constipation-associated and fecal incontinence–associated symptoms after surgery for colon cancer.3 More detailed knowledge of the long-term presence of specific bowel symptoms after the 3 different types of colectomies would not only enhance tailored preoperative patient counseling but would also provide the clinician with practical indications for more direct screening and personalized treatment during regular follow-up.
Extreme heterogeneity of the available studies, small cohorts, and the use of many nonvalidated bowel function scores previously precluded comparison of the different types of colon resections.3 Such knowledge could possibly improve our understanding of the functioning of different parts of the colon.
The hypothesis was that sigmoid colon resection will lead to more constipation, given previous reports on difficult emptying and/or straining.4,5 Patients who underwent right hemicolectomy are expected to experience frequent diarrhea or loose stools,6 possibly predisposing them to fecal incontinence. Given the negative influence of constipation and/or fecal incontinence on generic quality of life,7,8 there may also be differences in generic quality of life. Therefore, the aims of this study were to determine and compare long-term bowel function and generic quality of life between patients who had undergone right hemicolectomy, left hemicolectomy, or sigmoid colon resection.
MATERIALS AND METHODS
Study Design
Between October 2017 and December 2019, this cross-sectional study was performed at 7 Dutch hospitals. The mandatory Dutch ColoRectal Audit registry was searched for patients ≥18 years of age, without a previous colectomy, who had undergone either right hemicolectomy, left hemicolectomy, or sigmoid colon resection for colon cancer with curative intention between 2009 and 2015. Excluded were patients who had either died, were mentally impaired, had a permanent stoma, whose address was unknown, or who lived abroad.
Patients who had signed an informed consent form were invited to complete 2 validated questionnaires: the Defecation and Fecal Continence (DeFeC) questionnaire and the Short-Form 36 (see Supplemental Digital Content 1 at http://links.lww.com/DCR/C8).9,10 A link to the digital questionnaires was provided unless the patient preferred to receive a hard copy. The patient data were acquired by 1 investigator who screened all medical records. Adjuvant chemotherapy was administered according to one of the standard regimens: FOLFOX, CAPOX, or capecitabine as a single agent. Radiotherapy in the pelvic region had been administered mainly for previous prostate cancer. The Medical Ethical Review Board of University Medical Center Groningen approved the study (approval code METc 2017/245), and it was performed in accordance with the guidelines on Strengthening the Reporting of Observational Studies in Epidemiology.
Questionnaires
The DeFeC questionnaire contains questions from widely used scoring systems and criteria for various bowel function problems, including the Rome IV criteria for constipation and fecal incontinence, the symptoms of the low anterior resection syndrome (LARS) score, and the Bristol Stool Scale (Supplemental Digital Content 1 at http://links.lww.com/DCR/C8).11–13 The Short-Form 36 is a generic quality-of-life questionnaire containing 36 questions covering 8 domains. The scores range from 0 (bad quality of life) to 100 (good quality of life).10
Definitions
To be diagnosed with constipation according to the Rome IV criteria, patients had to report 2 or more of the following symptoms: straining, lumpy or hard stools, incomplete defecation, anorectal blockage, manual maneuvers to facilitate defecation, and less than 3 spontaneous bowel movements per week.11 Additionally, the regular use of laxatives had to be needed to loosen stool. Fecal incontinence was also defined according to the Rome IV criteria and included any involuntary loss of stool at least 2× per month.12 Furthermore, different subtypes of fecal incontinence were distinguished: soiling (loss of small amounts of feces), urge incontinence (unable to reach the toilet in time), solid incontinence (loss of solid feces without urge), and liquid incontinence (loss of watery feces). The 5 very disabling bowel symptoms of the LARS score (any flatus or liquid incontinence, altered stool frequency, fecal clustering, and fecal urgency) were also analyzed because of their known negative influence on quality of life.13 To define stool consistency, the Bristol Stool Scale was used.
Sigmoid colon resection was defined as the surgical resection of a sigmoid tumor with an anastomosis of >15 cm above the anal verge. Surgical resection of a tumor in the descending colon or distal transverse colon was defined as left hemicolectomy. Follow-up time was defined as the time between completion of the questionnaires and primary surgery or reversal of the temporary stoma. Tumor stage was defined according to the Union for International Cancer Control classification. The Charlson Comorbidity Index was used to score the severity of comorbidities.14 The European Perioperative Clinical Outcome definitions were used to specify postoperative complications other than anastomotic leakage or a reoperation.15
Statistical Analysis
Continuous data were reported as means (SDs) or medians (interquartile ranges) and were compared using either ANOVA or the Kruskal-Wallis test. For categorical data, counts and percentages were given and compared using the χ2 test. To account for multiple testing, subgroup χ2 tests were added. Univariable and multivariable binary logistic regression analyses were performed to identify associations between bowel dysfunction and the 3 types of colon resections. Results were presented as OR with 95% CI. Only relevant univariable variables (p < 0.10) or variables with a theoretical confounding effect based on an extensive literature search were included in the multivariable models. Possible interactions were checked. A p value of <0.05 was considered statistically significant. Missing data were omitted from statistical analyses. All statistical analyses were performed with IBM SPSS Statistics, version 23.0 (Armonk, NY; IBM Corporation).
RESULTS
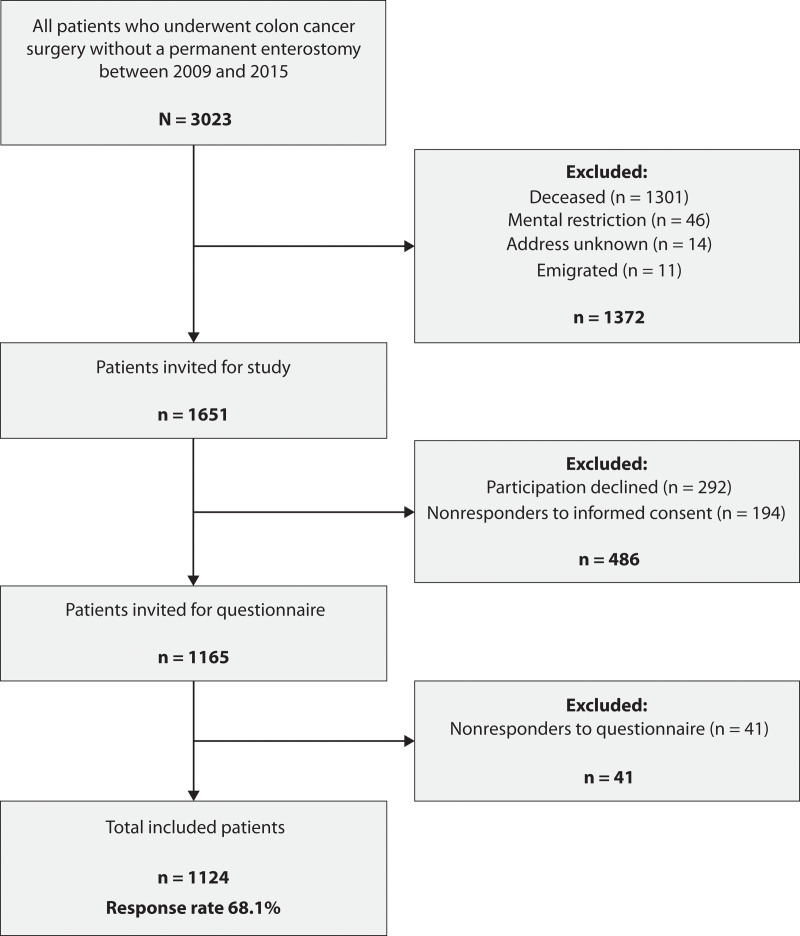
Between 2009 and 2015, a total of 3023 patients underwent right or left hemicolectomy or sigmoid colon resection for colonic cancer without construction of a permanent stoma. After excluding 1372 patients who had either died, had a mental impairment, or had an unknown or foreign address, questionnaires were sent to 1651 patients, 1124 of whom completed the questionnaires (Fig. 1). Ten of the 1114 included patients (0.9%) had 1 or more missing variable for the definition of constipation or fecal incontinence.
FIGURE 1.
Flow chart of patient inclusion and exclusion.
Patient Characteristics
There were 673 patients who had undergone right hemicolectomy, 167 had undergone left hemicolectomy, and 284 patients had undergone sigmoid colon resection. Taken together, the median follow-up time was 56 (interquartile range, 41–80) months. Patient characteristics according to the type of colon resection are shown in Table 1. A drop-out analysis revealed that more nonresponders had undergone sigmoid colon resections than did responders (31.5% versus 25.3%, p = 0.021; see Supplemental Digital Content 2 at http://links.lww.com/DCR/C9). In addition, nonresponders were older than responders and had a higher ASA score (both p < 0.001).
TABLE 1.
Patient characteristics according to the type of colon resection
| Right hemicolectomy, n (%) | Left hemicolectomy, n (%) | Sigmoid colon resection, n (%) | p a | |
|---|---|---|---|---|
| Overall, N (%) | 673 (100.0) | 167 (100.0) | 284 (100.0) | |
| Basic characteristics | ||||
| Men | 314 (46.7) | 99 (59.3) | 181 (63.7) | <0.001 |
| Age at surgery (y) b | 68.5 (9.7) | 65.8 (9.5) | 66.2 (9.5) | <0.001** |
| Follow-up (mo) c | 57.0 (42–79) | 52.0 (38–79) | 58.0 (41–83) | 0.121 |
| BMI at surgery (kg/m2) b | 26.5 (4.2) | 26.6 (4.3) | 27.6 (4.3) | 0.001** |
| ASA score at surgery | ||||
| I | 106 (16.2) | 34 (21.0) | 63 (23.2) | 0.016* |
| II | 403 (61.6) | 96 (59.3) | 172 (63.2) | |
| III | 140 (21.4) | 32 (19.8) | 34 (12.5) | |
| IV | 5 (0.8) | 0 (0.0) | 3 (1.1) | |
| Charlson Comorbidity Index at surgery c | 2.0 (2–2) | 2.0 (2–2) | 2.0 (2–2) | 0.218 |
| Previous lower abdominal surgery | 239 (35.5) | 56 (33.5) | 80 (28.2) | 0.089 |
| Previous upper abdominal surgery | 45 (6.7) | 9 (5.4) | 20 (7.0) | 0.780 |
| Smoking | ||||
| No | 497 (81.5) | 128 (82.6) | 211 (83.7) | 0.596 |
| Yes | 87 (14.3) | 19 (12.3) | 35 (13.9) | |
| Recently quit | 26 (4.3) | 8 (5.2) | 6 (2.4) | |
| Oncologic characteristics | ||||
| Tumor stage (UICC) | ||||
| I | 145 (21.7) | 37 (22.2) | 102 (36.2) | <0.001** |
| II | 315 (47.2) | 65 (38.9) | 88 (31.2) | |
| III | 188 (28.1) | 61 (36.5) | 85 (30.1) | |
| IV | 20 (3.0) | 4 (2.4) | 7 (2.5) | |
| Distant metastasis | ||||
| No | 645 (96.1) | 155 (92.8) | 264 (93.3) | 0.111 |
| Liver | 16 (2.4) | 6 (3.6) | 11 (3.9) | |
| Lung | 5 (0.7) | 1 (0.6) | 5 (1.8) | |
| Multiple locations | 5 (0.7) | 5 (3.0) | 3 (1.1) | |
| Adjuvant treatment | ||||
| Previous radiotherapy in pelvic region | 14 (2.1) | 4 (2.4) | 8 (2.8) | 0.793 |
| Adjuvant therapy | ||||
| No | 470 (72.6) | 97 (60.2) | 196 (71.3) | 0.013* |
| CAPOX | 78 (12.1) | 38 (23.6) | 44 (16.0) | |
| FOLFOX | 63 (9.7) | 16 (9.9) | 22 (8.4) | |
| Capecitabine | 36 (5.6) | 10 (6.2) | 12 (4.4) | |
| Years since last chemotherapy b | 4.0 (3.0–6.0) | 5.0 (4.0–7.0) | 5.0 (3.0–7.0) | 0.498 |
| Surgical characteristics | ||||
| Setting | ||||
| Elective | 605 (91.1) | 138 (84.1) | 248 (89.5) | 0.032* |
| Emergency | 59 (8.9) | 26 (15.9) | 29 (10.5) | |
| Surgical approach | ||||
| Open | 391 (58.7) | 82 (49.1) | 112 (39.6) | <0.001** |
| Laparoscopic | 219 (32.9) | 70 (41.9) | 145 (51.2) | |
| Conversion | 56 (8.4) | 15 (9.0) | 26 (9.2) | |
| Method of anastomosis | ||||
| Handsewn | 398 (61.9) | 107 (71.3) | 113 (41.1) | <0.001** |
| Stapled | 245 (38.1) | 43 (28.7) | 162 (58.9) | |
| Reconstruction | ||||
| Side-to-end | 26 (4.0) | 17 (10.8) | 127 (51.8) | <0.001** |
| Side-to-side | 600 (92.2) | 87 (55.4) | 59 (24.1) | |
| End-to-end | 25 (3.8) | 53 (33.8) | 59 (24.1) | |
| Temporary stoma | 15 (2.2) | 29 (17.4) | 35 (12.3) | <0.001** |
| Postoperative characteristics | ||||
| Anastomotic leakage | 24 (3.6) | 13 (7.8) | 12 (4.2) | 0.057 |
| Reoperation | 43 (6.4) | 16 (9.6) | 23 (8.1) | 0.305 |
| Other types of complications | ||||
| No | 446 (66.3) | 116 (69.5) | 215 (75.7) | 0.024* |
| 1 complication | 152 (22.6) | 40 (24.0) | 50 (17.6) | |
| >1 complication | 75 (11.1) | 11 (6.6) | 19 (6.7) | |
CAPOX, Capecitabine and Oxaliplatin; FOLFOX, Folinic acid, Fluorouracil, and Oxaliplatin; IQR = interquartile range; UICC, Union for International Cancer Control.
P value for comparison of the 3 groups.
Values expressed as medan (SD).
Values expressed as median (IQR).
* Statistical significance of p < 0.05.
** Statistical significance of p < 0.005.
Stool Consistency and Frequency
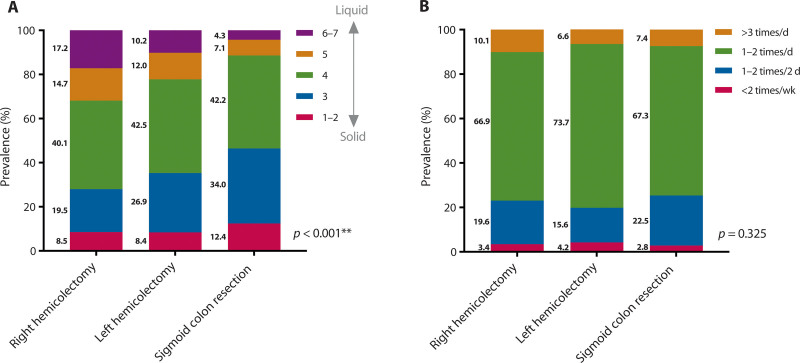
Figure 2 shows the stool consistency after the 3 types of colon resections. On comparing stool consistency, it was found that the stools of patients who had undergone right hemicolectomy were more liquid compared to patients who had undergone left hemicolectomy and sigmoid colon resection (p < 0.001; Fig. 2A). No differences were found for stool frequency (Fig. 2B).
FIGURE 2.
Stool frequency and stool consistency according to the type of colon resection. A, Stool consistency following the Bristol Stool Chart. B, Stool frequency. * Statistical significance of p < 0.05. ** Statistical significance of p < 0.005.
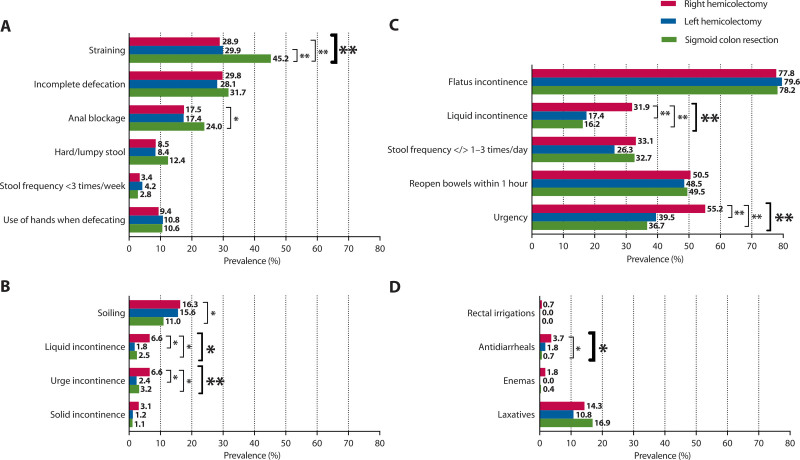
Individual Bowel Symptoms
The prevalence of the different investigated bowel symptoms after the 3 types of colon resections is shown in Figure 3. The prevalence of straining was significantly higher in patients who had undergone sigmoid colon resection compared to patients who had undergone left or right hemicolectomy (45.2% versus 29.9% and 28.9%; p < 0.001; Fig. 3A). Regarding fecal incontinence–associated symptoms, liquid incontinence and urge incontinence were both significantly more prevalent after right hemicolectomy than after left hemicolectomy and sigmoid colon resection (6.6% versus 1.8% and 2.5%, p = 0.004 and 6.6% versus 2.4% and 3.2%, p = 0.021; Fig. 3B). Likewise, liquid incontinence and fecal urgency were the only symptoms of the LARS score that showed a statistically significant difference between patients who had undergone right or left hemicolectomy or sigmoid colon resection (31.9% versus 17.4% and 16.2%, p < 0.001 and 55.2% versus 39.5% and 36.7%, p < 0.001; Fig. 3C).
FIGURE 3.
The prevalence of bowel symptoms and defecation treatment according to the type of colon resection. A, Symptoms of constipation. B, Symptoms of fecal incontinence. C, Symptoms of the low anterior resection syndrome score. D, Use of defecation treatment. * Statistical significance of p < 0.05. ** Statistical significance of p < 0.005.
Use of Defecation Treatment
Enemas and laxatives were used to treat constipation in less than 16.9% of the patients without significant differences between the types of colon resections (Fig. 3D). Rectal irrigations and antidiarrheals were used in less than 3.7% of the patients for all types of resections. Antidiarrheals were used most often after right hemicolectomy, compared to left hemicolectomy and sigmoid colon resection (3.7% versus 1.8% and 0.7%, p = 0.023).
Constipation and Fecal Incontinence
Overall, the prevalence of constipation was significantly higher in patients who had undergone sigmoid colon resection compared to patients who had undergone right or left hemicolectomy (31.1% versus 17.7% and 21.0% p < 0.001), whereas the prevalence of fecal incontinence was not significantly different (12.7% versus 18.5% and 16.8%; p = 0.088).
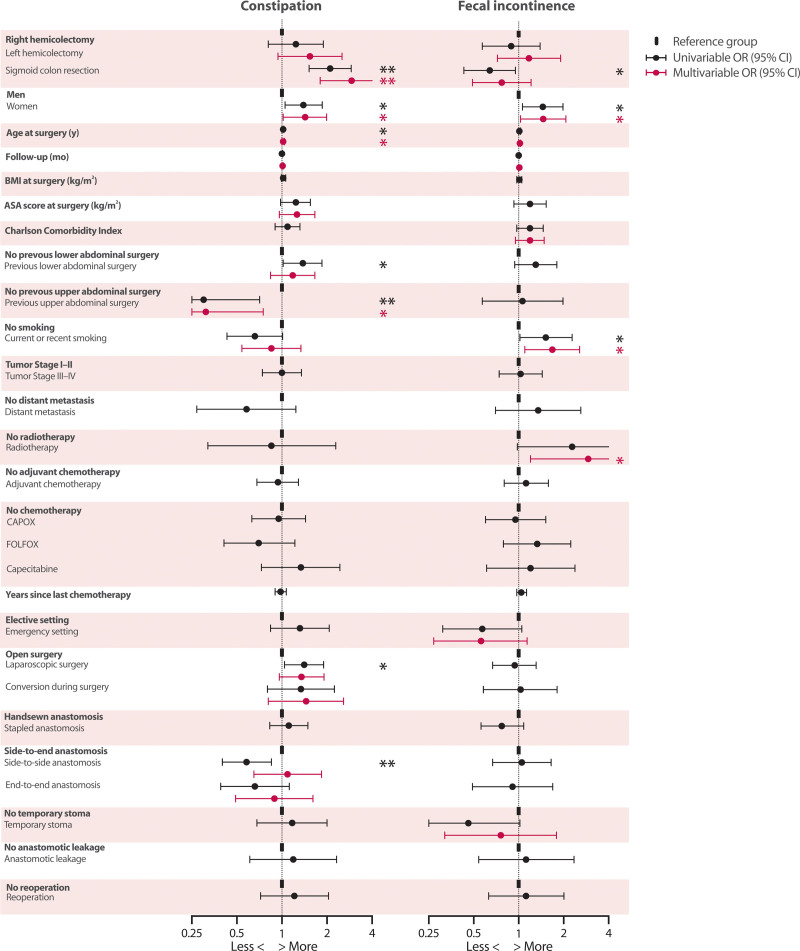
In accordance with these differences in prevalence, a multivariable model of constipation showed an increased likelihood of constipation in patients who had undergone sigmoid colon resection if right hemicolectomy was taken as the reference category (OR, 2.92; 95% CI, 1.80–4.75; p < 0.001). No significant association was found between fecal incontinence and any specific type of colon resection. Additionally, the same univariable and multivariable analyses were performed with left hemicolectomy as the reference category. They also revealed a statistically significant increase in the likelihood of constipation in patients who had undergone sigmoid resection (OR, 1.93; 95% CI, 1.12–3.35; p = 0.019; see Supplemental Digital Content 3 at http://links.lww.com/DCR/C10). A direct comparison between patients who had undergone left hemicolectomy versus sigmoid colon resection did not show significant associations for fecal incontinence.
All univariable and multivariable associations between different characteristics and constipation and fecal incontinence are presented in Figure 4. The exact outcomes of these analyses can be found in Supplemental Digital Content 4 at http://links.lww.com/DCR/C11. Women were more likely to experience both constipation and fecal incontinence (constipation: OR, 1.43; 95% CI, 1.02–1.99; p = 0.038 and fecal incontinence: OR, 1.46; 95% CI, 1.03-2.07; p = 0.036). Likewise, increasing age was also associated with increased odds of constipation (OR, 1.02; 95% CI, 1.00–1.04; p = 0.037). Previous upper abdominal surgery was associated with a decreased likelihood of constipation (OR, 0.31; 95% CI, 0.13–0.75; p = 0.009). Finally, smoking and radiotherapy were found to be significantly associated with fecal incontinence (OR, 1.68; 95% CI, 1.10–2.56; p = 0.017 and OR, 2.92; 95% CI, 1.20–7.08; p = 0.018, respectively).
FIGURE 4.
Univariable and multivariable logistic regression analyses of constipation and fecal incontinence. * Statistical significance of p < 0.05. ** Statistical significance of p < 0.005.
Additionally, using the same multivariable logistic regression model as for overall fecal incontinence, an increased likelihood of liquid incontinence was found in patients who had undergone right hemicolectomy compared to patients who had undergone sigmoid colon resection (OR, 2.15; 95% CI, 1.47–3.16; p < 0.001). A similar multivariable logistic regression model of fecal urgency yielded a comparable result (OR, 2.01; 95% CI, 1.47–2.74; p < 0.001).
Generic Quality of Life
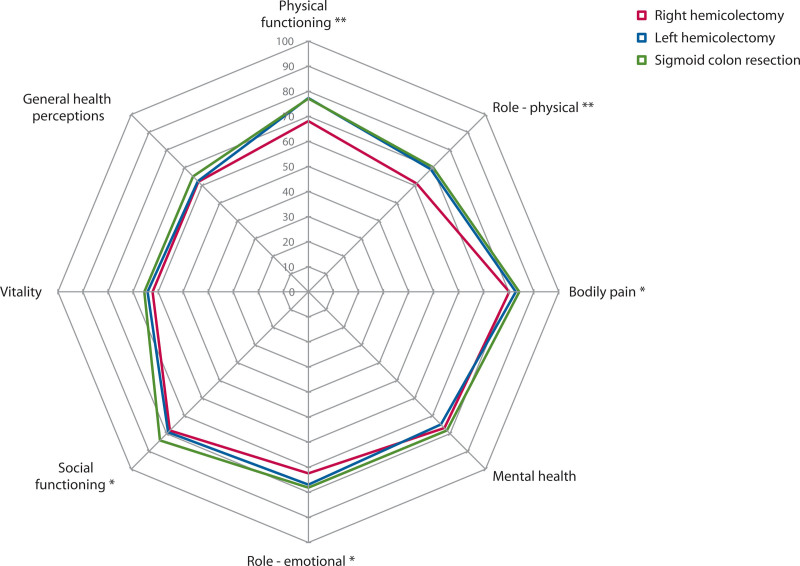
The quality-of-life scores after the 3 different types of colon resections are shown in Figure 5. The scores on different physical domains of quality of life (physical functioning, role-physical, and bodily pain) as well as on different mental domains (social functioning and role-emotional) were significantly lower in patients who had undergone right hemicolectomy (Fig. 5). Subanalysis performed in patients without fecal incontinence still showed worse quality of life on the domains physical functioning and role-physical after right hemicolectomy, whereas no significant difference for the psychosocial domains was observed (see Supplemental Digital Content 5 at http://links.lww.com/DCR/C12).
FIGURE 5.
Generic quality-of life scores according to the type of colon resection.
DISCUSSION
This study shows that patients who underwent sigmoid colon resection are 3× more likely to experience constipation in the long term than patients who underwent right or left hemicolectomy. This finding corroborates with others who found more constipation-associated problems after sigmoid colon resection compared to patients who underwent a hemicolectomy16 or a polypectomy.17 Nevertheless, this study is the first to use a validated constipation score to assess patients who underwent resection for colon cancer. Patients who underwent sigmoid colon resection experienced constipation 1.5× more often than the general Dutch population of comparable age (19.8% versus 31.1%).18
Various pathophysiological factors have been postulated for the association between sigmoid colon resection and constipation. First, after colonic mobilization, the sensory and motor function of the colon might be reduced because of denervation and fibrosis.5,16 Decreased activity of the descending colon and a prolonged transit time were found in patients after surgery for rectal cancer and were attributed to autonomic denervation.19,20 These mechanisms are likely to occur after surgery for colon cancer as well. Second, an animal study showed that after 12 week, levels of nitric oxide synthesis increased in rats with a denervated distal colon compared to rats that had not undergone colon surgery.21 Nitric oxide might downregulate the contractile activity of the colon and lead to constipation, but this warrants further research.
Right hemicolectomy was associated with twice as much liquid incontinence and fecal urgency compared to sigmoid colon resection. Liquid incontinence was probably linked to the more liquid stool consistency that was found in patients after right hemicolectomy, which had also been reported in previous long-term studies.22,23 Comparing stool consistency in patients after right hemicolectomy versus the general population of comparable age illustrates the true increase of liquid to mushy stool after right hemicolectomy (17.2% versus 4.8%, respectively).24 Liquid incontinence and fecal urgency were also the 2 symptoms of the LARS score that showed a significantly higher prevalence after right hemicolectomy.
From a pathophysiological point of view, 2 main issues can be distinguished that predispose patients who underwent right hemicolectomy to more liquid stool. First, the absence of the proximal colon, which is known as the part of the colon that absorbs most of the water from the stool.25 Second, the absence of or damage to the terminal ileum and/or ileocolic valve may lead to bile acid malabsorption, which causes chronic diarrhea.6,26,27 In addition, small-bowel bacterial overgrowth, on account of the absence of the ileocecal valve that acts as a barrier between the flora of the small and large intestine, was proposed as liquifying the stool.6,27 Next to that, some hypothesize that injury to the superior mesenteric nerve plexus could result in neurogenic diarrhea,28 although more recent studies could not prove this association.29,30
Despite the differences in outcomes, personalized treatment after the different types of colon resections seems to be lacking. This may be caused by a lack of awareness among physicians regarding bowel function problems after colon resections. For the rectum resections, postoperative low anterior resection syndrome is receiving more and more attention, but postoperative bowel function problems after colectomies have not been widely investigated. In the current study, only 16.9% of the patients who underwent sigmoid colon resection use laxatives, whereas 31.1% had constipation. Similarly, treatment for fecal incontinence was uncommon. Only 3.7% of the patients who underwent right hemicolectomy were using an antidiarrheal, whereas no less than 6.6% experienced liquid incontinence more than once per month. As bile acid malabsorption is likely to play a role in liquid incontinence after right hemicolectomy, a bile acid sequestrant might relieve these complaints.27 However, less than 10% of the patients in this study who had liquid incontinence after right hemicolectomy reported using a bile acid sequestrant, a situation that leaves room for improvement.
All multivariable models were adjusted for sex, age, and follow-up time, as these factors are well known to influence bowel functioning, also in the context of surgery for colon cancer.5,17,31–33 The current study shows no effect of follow-up time on constipation and fecal incontinence. This is in contrast with the general consensus that the colon structurally adapts over time after surgery.6 These findings imply that prompt treatment of constipation and fecal incontinence is required because the complaints are not likely to resolve spontaneously and might even worsen as more time passes between surgery and follow-up. Concerning smoking, this study shows that smoking seems to be associated with more fecal incontinence after a resection for colon cancer. This might be related to the direct stimulating effect of nicotine on colonic motor activity.34 Finally, the current study provides evidence of a 3-fold increase in fecal incontinence in patients who previously received radiotherapy in the pelvic region for other conditions. This emphasizes the detrimental effect of radiotherapy on fecal incontinence, which has been attributed to structural changes in the irradiated tissue.35
Remarkably, it seems that adjuvant chemotherapy after surgery for colon cancer does not worsen constipation or fecal incontinence in the long term, which has been noted by others as well.17,23,32 However, this is the first study that compares the long-term effects of different chemotherapy regimens and the time since the last chemotherapy treatment, which were both not associated with any of the bowel function problems. Therefore, it seems that the direct cytotoxic effect of chemotherapeutic agents on the mucosa of the GI tract does not have a chronic debilitating impact on patients’ bowel functions, as was suggested previously.36 However, future research is required to establish the exact effects of chemotherapy on long-term bowel function.
In line with the findings of more liquid incontinence and fecal urgency after right hemicolectomy, most physical and mental generic quality-of-life domains were worse in these patients. This observation is corroborated by other long-term studies showing impaired quality of life after right hemicolectomy, especially in patients with loose stools.22,23 Comparable generic quality of life between patients who had undergone right-sided and left-sided colectomies had been found previously, although shorter questionnaires were used that did not distinguish domains.37,38
The large study population, in combination with the validated bowel function scores, strengthens this multicenter study. Although the used scores were not validated for patients who had undergone resection for colon cancer, together, they provide a thorough examination of bowel function that can be compared to other patients and/or to the general population. Furthermore, longitudinal data are lacking. Finally, including long-surviving patients without a permanent stoma, combined with the higher age and worse ASA score of the nonresponders, may have caused selection bias because this would imply that the “most healthy” patients were included in this study. However, this would only reinforce our findings on the large number of bowel function problems after surgery for colon cancer.
CONCLUSION
This study shows clear differences in long-term bowel function problems after right hemicolectomy, left hemicolectomy, or sigmoid colon resection for colon cancer. Sigmoid colon resection seems to be associated with constipation, with alarmingly low treatment ranges. On the contrary, liquid incontinence and fecal urgency seem to be associated with right hemicolectomy, which may explain the decline in physical and mental generic quality of life of these patients. Hopefully, the current results will provide the clinician with a tool to personalize screening and lead to prompt treatment of both constipation and fecal incontinence during the follow-up of surgery for colon cancer.
ACKNOWLEDGMENTS
The authors thank I.A.M. ten Vaarwerk and E. Visser for their help with processing the data of the questionnaires. The authors would also like to thank T. van Wulfften Palthe, PhD, for correcting the English article. Finally, they thank all patients for their participation.
Supplementary Material
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML and PDF versions of this article on the journal’s website (www.dcrjournal.com).
Funding/Support: None reported.
Financial Disclosure: None reported.
REFERENCES
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. [DOI] [PubMed] [Google Scholar]
- 2.Miller KD, Nogueira L, Mariotto AB, et al. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin. 2019;69:363–385. [DOI] [PubMed] [Google Scholar]
- 3.Verkuijl SJ, Jonker JE, Trzpis M, Burgerhof JGM, Broens PMA, Furnée EJB. Functional outcomes of surgery for colon cancer: a systematic review and meta-analysis. Eur J Surg Oncol. 2021;47:960–969. [DOI] [PubMed] [Google Scholar]
- 4.Sato K, Inomata M, Kakisako K, Shiraishi N, Adachi Y, Kitano S. Surgical technique influences bowel function after low anterior resection and sigmoid colectomy. Hepatogastroenterology. 2003;50:1381–1384. [PubMed] [Google Scholar]
- 5.Bertelsen CA, Elfeki H, Neuenschwander AU, Laurberg S, Kristensen B, Emmertsen KJ. The risk of long-term bowel dysfunction after resection for sigmoid adenocarcinoma: a cross-sectional survey comparing complete mesocolic excision with conventional surgery. Colorectal Dis. 2018;20:O256–O266. [DOI] [PubMed] [Google Scholar]
- 6.Hope C, Reilly J, Lund J, Andreyev H. Systematic review: the effect of right hemicolectomy for cancer on postoperative bowel function. Support Care Cancer. 2020;28:4549–4559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Belsey J, Greenfield S, Candy D, Geraint M. Systematic review: impact of constipation on quality of life in adults and children. Aliment Pharmacol Ther. 2010;31:938–949. [DOI] [PubMed] [Google Scholar]
- 8.Parés D, Vial M, Bohle B, et al. Prevalence of faecal incontinence and analysis of its impact on quality of life and mental health. Colorectal Dis. 2011;13:899–905. [DOI] [PubMed] [Google Scholar]
- 9.Meinds RJ, Timmerman MEW, van Meegdenburg MM, Trzpis M, Broens PMA. Reproducibility, feasibility and validity of the Groningen Defecation and Fecal Continence questionnaires. Scand J Gastroenterol. 2018;53:790–796. [DOI] [PubMed] [Google Scholar]
- 10.Ware J, Snoww KK, Kosinski MA, Gandek BG. SF-36 Health Survey: Manual and Interpretation Guide. Boston: MA: The Health Institute, New England Medical Center; 1993. [Google Scholar]
- 11.Mearin F, Lacy BE, Chang L, et al. Bowel disorders. Gastroenterology. 2016;150:1393–1407. [DOI] [PubMed] [Google Scholar]
- 12.Rao SS, Bharucha AE, Chiarioni G, et al. Functional anorectal disorders. Gastroenterology. 2016;150:1430–1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Emmertsen KJ, Laurberg S. Low anterior resection syndrome score: development and validation of a symptom-based scoring system for bowel dysfunction after low anterior resection for rectal cancer. Ann Surg. 2012;255:922–928. [DOI] [PubMed] [Google Scholar]
- 14.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. [DOI] [PubMed] [Google Scholar]
- 15.Jammer I, Wickboldt N, Sander M, et al. ; European Society of Anaesthesiology (ESA) and the European Society of Intensive Care Medicine (ESICM); European Society of Anaesthesiology; European Society of Intensive Care Medicine. Standards for definitions and use of outcome measures for clinical effectiveness research in perioperative medicine: European Perioperative Clinical Outcome (EPCO) definitions: a statement from the ESA-ESICM joint taskforce on perioperative outcome measures. Eur J Anaesthesiol. 2015;32:88–105. [DOI] [PubMed] [Google Scholar]
- 16.Ho YH, Low D, Goh HS. Bowel function survey after segmental colorectal resections. Dis Colon Rectum. 1996;39:307–310. [DOI] [PubMed] [Google Scholar]
- 17.Elfeki H, Larsen HM, Emmertsen KJ, et al. Bowel dysfunction after sigmoid resection for cancer and its impact on quality of life. Br J Surg. 2019;106:142–151. [DOI] [PubMed] [Google Scholar]
- 18.Meinds RJ, van Meegdenburg MM, Trzpis M, Broens PM. On the prevalence of constipation and fecal incontinence, and their co-occurrence, in the Netherlands. Int J Colorectal Dis. 2017;32:475–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Catchpole BN. Motor pattern of the left colon before and after surgery for rectal cancer: possible implications in other disorders. Gut. 1988;29:624–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Koda K, Saito N, Seike K, Shimizu K, Kosugi C, Miyazaki M. Denervation of the neorectum as a potential cause of defecatory disorder following low anterior resection for rectal cancer. Dis Colon Rectum. 2005;48:210–217. [DOI] [PubMed] [Google Scholar]
- 21.Shimizu K, Koda K, Kase Y, et al. Induction and recovery of colonic motility/defecatory disorders after extrinsic denervation of the colon and rectum in rats. Surgery. 2006;139:395–406. [DOI] [PubMed] [Google Scholar]
- 22.Ohigashi S, Hoshino Y, Ohde S, Onodera H. Functional outcome, quality of life, and efficacy of probiotics in postoperative patients with colorectal cancer. Surg Today. 2011;41:1200–1206. [DOI] [PubMed] [Google Scholar]
- 23.Larsen HM, Elfeki H, Emmertsen KJ, Laurberg S. Long-term bowel dysfunction after right-sided hemicolectomy for cancer. Acta Oncol. 2020;59:1240–1245. [DOI] [PubMed] [Google Scholar]
- 24.Heaton KW, Radvan J, Cripps H, Mountford RA, Braddon FE, Hughes AO. Defecation frequency and timing, and stool form in the general population: a prospective study. Gut. 1992;33:818–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hall JE, Guyton AC. Guyton and Hall textbook of medical physiology. 12th ed. Philadelphia: Saunders/Elsevier; 2011. [Google Scholar]
- 26.Phillips F, Muls AC, Lalji A, Andreyev HJ. Are bile acid malabsorption and bile acid diarrhoea important causes of loose stool complicating cancer therapy? Colorectal Dis. 2015;17:730–734. [DOI] [PubMed] [Google Scholar]
- 27.Yde J, Larsen HM, Laurberg S, Krogh K, Moeller HB. Chronic diarrhoea following surgery for colon cancer-frequency, causes and treatment options. Int J Colorectal Dis. 2018;33:683–694. [DOI] [PubMed] [Google Scholar]
- 28.Hohenberger W, Weber K, Matzel K, Papadopoulos T, Merkel S. Standardized surgery for colonic cancer: complete mesocolic excision and central ligation—technical notes and outcome. Colorectal Dis. 2009;11:354–64. [DOI] [PubMed] [Google Scholar]
- 29.Bertelsen CA, Larsen HM, Neuenschwander AU, Laurberg S, Kristensen B, Emmertsen KJ. Long-term functional outcome after right-sided complete mesocolic excision compared with conventional colon cancer surgery: a population-based questionnaire study. Dis Colon Rectum. 2018;61:1063–1072. [DOI] [PubMed] [Google Scholar]
- 30.Thorsen Y, Stimec B, Andersen SN, et al. ; RCC study group. Bowel function and quality of life after superior mesenteric nerve plexus transection in right colectomy with D3 extended mesenterectomy. Tech Coloproctol. 2016;20:445–453. [DOI] [PubMed] [Google Scholar]
- 31.van Heinsbergen M, Janssen-Heijnen ML, Leijtens JW, Slooter GD, Konsten JL. Bowel dysfunction after sigmoid resection underestimated: multicentre study on quality of life after surgery for carcinoma of the rectum and sigmoid. Eur J Surg Oncol. 2018;44:1261–1267. [DOI] [PubMed] [Google Scholar]
- 32.Buchli C, Martling A, Sjövall A. Low anterior resection syndrome after right- and left-sided resections for colonic cancer. BJS Open. 2019;3:387–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sarli L, Cinieri FG, Pavlidis C, et al. Anorectal function problems after left hemicolectomy. J Laparoendosc Adv Surg Tech A. 2006;16:565–571. [DOI] [PubMed] [Google Scholar]
- 34.Coulie B, Camilleri M, Bharucha AE, Sandborn WJ, Burton D. Colonic motility in chronic ulcerative proctosigmoiditis and the effects of nicotine on colonic motility in patients and healthy subjects. Aliment Pharmacol Ther. 2001;15:653–663. [DOI] [PubMed] [Google Scholar]
- 35.Peeters KC, van de Velde CJ, Leer JW, et al. Late side effects of short-course preoperative radiotherapy combined with total mesorectal excision for rectal cancer: increased bowel dysfunction in irradiated patients—a Dutch colorectal cancer group study. J Clin Oncol. 2005;23:6199–6206. [DOI] [PubMed] [Google Scholar]
- 36.Andreyev HJ, Davidson SE, Gillespie C, Allum WH, Swarbrick E; British Society of Gastroenterology; Association of Colo-Proctology of Great Britain and Ireland; Association of Upper Gastrointestinal Surgeons; Faculty of Clinical Oncology Section of the Royal College of Radiologists. Practice guidance on the management of acute and chronic gastrointestinal problems arising as a result of treatment for cancer. Gut. 2012;61:179–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Magdeburg J, Glatz N, Post S, Kienle P, Rickert A. Long-term functional outcome of colonic resections: how much does faecal impairment influence quality of life? Colorectal Dis. 2016;18:O405–O413. [DOI] [PubMed] [Google Scholar]
- 38.Brigic A, Sakuma S, Lovegrove RE, et al. A prospective case control study of functional outcomes and related quality of life after colectomy for neoplasia. Int J Colorectal Dis. 2017;32:777–787. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.