Abstract
Most sexually active youth in the United States do not believe that they are at risk for contracting HIV and have never been tested. Creating safe environments that promote confidentiality and respect, obtaining an accurate sexual and reproductive health assessment, and providing nonstigmatizing risk counseling are key components of any youth encounters. Pediatricians can play a key role in preventing and controlling HIV infection by promoting risk-reduction counseling and offering routine HIV testing and prophylaxis to adolescent and young adult (youth) patients. In light of persistently high numbers of people living with HIV in the United States and documented missed opportunities for HIV testing, the Centers for Disease Control and Prevention and the US Preventive Services Task Force recommend universal and routine HIV screening among US populations, including youth. Recent advances in HIV diagnostics, treatment, and prevention help support this recommendation. This clinical report reviews epidemiological data and recommends that routine HIV screening be offered to all youth 15 years or older, at least once, in health care settings. After initial screening, youth at increased risk, including those who are sexually active, should be rescreened at least annually, and potentially as frequently as every 3 to 6 months if at high risk (male youth reporting male sexual contact, active injection drug users, transgender youth; youth having sexual partners who are HIV-infected, of both genders, or injection drug users; youth exchanging sex for drugs or money; or youth who have had a diagnosis of or have requested testing for other sexually transmitted infections). Youth at substantial risk for HIV acquisition should be routinely offered HIV preexposure prophylaxis, and HIV postexposure prophylaxis is also indicated after high-risk exposures. This clinical report also addresses consent, confidentiality, and coverage issues that pediatricians face in promoting routine HIV testing and HIV prophylaxis for their patients.
Introduction and Background
The HIV epidemic persists in the United States despite great progress in treatment and continued efforts to identify people living with HIV and AIDS. At year-end 2018, an estimated 1 173 900 people 13 years or older were living with HIV infection in the United States, of whom 47 800 (4%) were adolescents and young adults (hereafter referred to as youth) 13 to 24 years of age.1 These estimates include individuals with both diagnosed and undiagnosed HIV infection. Between 2014 and 2018, new diagnoses of HIV infection decreased among 13- to 24-year-olds; in 2018, youth accounted for 21% (7817 of 37 515) of all new diagnoses of HIV infection in the United States.2 Of the 1.2 million people living with HIV and AIDS in the United States, approximately 14% are people whose infection had not been diagnosed,1 and it is this group that is estimated to account for 38% of HIV transmission; those aware of their HIV infection but not receiving HIV care account for an additional 43% of transmission.3 In 2018, HIV infection was undiagnosed in an estimated 45% of 13- to 24-year-olds living with HIV.1 The percentage of people with undiagnosed HIV infection decreased as age increased, and 13- to 24-year-olds were disproportionately overrepresented compared with all other age groups unaware of their infection.1 Youth with HIV infection are also the least likely of any age group to be linked to HIV care in a timely manner. Youth also have lower rates of viral suppression, making them less likely to stay healthy and increasing their risk of HIV transmission to others.4,5 The American Academy of Pediatrics (AAP) encouraged HIV testing of all sexually active youth in its 2001 and 2011 policy statements.6,7 This clinical report reflects changes in epidemiology, advances in diagnostic testing, and updated recommendations for HIV testing, postexposure prophylaxis (PEP), and new guidance for preexposure prophylaxis (PrEP) in youth at risk for acquiring HIV infection.
The risk of HIV infection varies with many population and individual factors, including, but not limited to, community prevalence rates, sexual networks, sexual behaviors, and concurrent substance use. In US youth, the rate of new HIV diagnoses per 100 000 people increases with age from 0.2 in the 13- to 14-year age group, to 8.1 in the 15- to 19-year age group, and 27.9 in the 20- to 24-year age group (the highest rate is 32.6 in the 24- to 29-year age group).2 In 2018, 88% of 13- to 24-year-olds in whom HIV infection was diagnosed were male, and only 12% were female.2 As with adults, most new youth HIV cases occur through sexual transmission. Among young men, more than 90% of HIV transmissions occur via male-to-male sex, whereas the heterosexual route is the primary means of transmission among female youth.2 In the United States, HIV infection disproportionately affects minority populations, occurring 11 times more often in Black/African American youth and 3.4 times more often in Hispanic/Latinx youth compared with White youth. HIV infection is also more common among youth living in the southern United States.2 The 2019 Youth Risk Behavior Survey found that 27% of high school students reported having engaged in sexual activity (37% by the 12th grade), and 21% had consumed alcohol or used drugs before their last sexual intercourse.8 Among sexually active high school students, 54% reported condom use during their last sexual encounter, a decline from 62% in 2007. More risk behaviors were reported by males who had sexual contact with males (MSM) only or with both male and female individuals. Among sexually active high school students, MSM were more likely than other boys to have had sexual intercourse with 4 or more people in their lifetime (28% compared with 19%, respectively) and significantly more likely to have ever injected any illegal drug (14% compared with 2%, respectively).8 Currently sexually active MSM were less likely to have used a condom during their last sexual intercourse than other males reporting only opposite-sex sexual contact (53% compared with 60%, respectively).8
New information has emerged about HIV infection in transgender populations.9 From 2009 to 2014, HIV infection was diagnosed in 2351 transgender people in the United States; 84% (1974) were transgender women, 15% (361) were transgender men, and less than 1% (16) had another gender identity.10 A 2019 systematic review and meta-analysis of US transgender populations aged 16 to 66 years (which included 14 studies with participants <18 years) found that an estimated 14% of transgender women have HIV infection. By race and ethnicity, an estimated 44% of Black/African American transgender women, 26% of Hispanic/Latinx transgender women, and 7% of White transgender women have HIV infection.11 Among the 3 million HIV testing events reported to the Centers for Disease Control and Prevention (CDC) in 2015, the percentage of transgender people who received a new HIV diagnosis was more than 3 times the national average.9 However, nearly two-thirds of transgender women and men surveyed by the Behavioral Risk Factor Surveillance System in 2014 and 2015 from 28 jurisdictions reported never having been tested for HIV.9
Youth often do not believe that they are at risk for HIV infection and do not get tested. Although 37% of high school students who participated in the Youth Risk Behavior Survey reported being sexually active by the 12th grade, only 13% reported having ever been tested for HIV.8 A survey of young adults aged 18 to 30 years found that more than half (54%) reported they had never been tested for HIV; not believing themselves to be at risk was the most common reported reason (67%), and their doctor having not suggested it was the next most common reported reason (41%) for not having been tested.12 Among those who reported being tested, 69% thought it “seemed like a good idea,” and 46% cited having their health care provider suggest testing was a contributing factor for many.12 Youth also cite concerns about confidentiality, access to testing, and blood draws as barriers to testing and increased availability of oral and rapid testing methods and free testing services as facilitators of their acceptance of HIV testing.13 Unfortunately, HIV testing continues to lag behind other sexually transmitted infection (STI) testing in pediatric primary care of sexually active youth. A minority of pediatricians report on-site HIV testing, and even fewer report access to oral or rapid antibody tests; a majority of pediatricians report lack of time, cultural differences, adolescents’ inaccurate responses to inquiries about sexual behaviors, personal discomfort discussing sexual issues, adolescents’ fear of parent or caregiver notification, lack of adequate payment, lack of interest in adolescent health issues, and insufficient training in how to talk to adolescents about STIs and HIV as the most frequently identified barriers to HIV and STI prevention counseling.14,15 In summary, although multiple barriers exist to testing youth for HIV, evidence shows that routinizing testing recommendations by health care providers and making testing easier by increasing access to HIV testing overall, as well as to newer less invasive test (nonblood draw) methodologies, can help to overcome these barriers. However, any barrier to testing can seem insurmountable if motivations to test (among youth) or recommendations to test (among health care providers) are not present.
In light of the increasing numbers of people with HIV infection and AIDS and missed opportunities for HIV testing, the CDC and the US Preventive Services Task Force (USPSTF) recommend universal (independent of risk factors and/or symptoms) and routine HIV screening rather than targeted (risk factor and/or symptom-based) testing as a national approach in the United States.16,17 Identification of HIV infection as early as possible after acquisition is crucial to rapidly initiating antiretroviral treatment, achieving sustained viral suppression, and preventing or reversing immune depletion in people in whom HIV infection is diagnosed. Early identification and treatment of HIV infection with sustained viral suppression also serve to prevent HIV transmission to partners and within the community (treatment as prevention), because Undetectable viral load effectively means Untransmittable (U=U).18 As of 2017, the US Public Health Service (USPHS) also recommends that HIV PrEP be offered to individuals at substantial risk of HIV infection19; a similar statement was issued by the USPSTF in 2019.20 Four key areas have been prioritized in the US National HIV/AIDS Strategy: (1) widespread testing and linkage to care, enabling people living with HIV to access treatment early; (2) broad support for people living with HIV to remain engaged in comprehensive care, including support for treatment adherence; (3) universal viral suppression among people living with HIV; and (4) full access to comprehensive PrEP services for those for whom it is appropriate and desired, with support for medication adherence for those using PrEP.18 Complex issues of confidentiality, disclosure of HIV status, and consent in adolescent care and variability in how statutes and regulations address these make implementation of these recommendations challenging. Nevertheless, pediatricians can play a key role in preventing and controlling HIV infection by promoting risk reduction and offering HIV testing and prophylaxis to their youth patients.
Risk Assessment and Counseling
Pediatricians are encouraged to address adolescent sexual and reproductive health on a routine basis by obtaining a sexual history, discussing healthy sexuality, performing an appropriate examination, providing patient-centered and age-appropriate anticipatory guidance, and performing appropriate screening and administering vaccinations. The HEADSS (Home, Education and Employment, Activities, Drugs, Sexuality, Suicide/Depression interview acts as a framework for these discussions. The AAP and the Society for Adolescent Health and Medicine affirm adolescents’ right to confidential health care.21 The AAP publications “Sexual and Reproductive Health Care Services in the Pediatric Setting”22 and “Targeted Reforms in Health Care Financing to Improve the Care of Adolescents and Young Adults”23 provide a framework to assist pediatricians in incorporating various aspects of sexual and reproductive health care into their practices and to provide guidance on overcoming barriers to providing this care routinely while maximizing opportunities for confidential health services delivery in their office.
Because youth are a population at increased risk of HIV infection, they should be routinely assessed for high-risk behaviors and screened for HIV. Resources that facilitate sexual and reproductive health assessment in a busy practice include the Bright Futures Adolescence Tools.24 Although the new CDC recommendations deemphasize risk assessment and counseling as precursors for opt-out testing in the general population, these activities are critical components of routine adolescent health visits. Adolescents may be more willing to disclose high-risk behaviors and discuss sensitive topics if pediatricians establish confidential, private discussions, use screening questionnaires, and increase time spent on these discussions.25,26 Ideally, a confidentiality policy allowing for trusting relationships with adolescent patients should be reviewed with adolescents and their parents or caregivers in early adolescence (ie, before 12 years of age) and can be modeled on a sample provided by Bright Futures.27
Discussing same-sex and opposite-sex attractions, sexual and gender identity, sexual behaviors, and exposure to sexual and gender-based violence or abuse are key components of obtaining sexual histories and providing sexual and reproductive health guidance to adolescents.22,28 Creating a supportive atmosphere and providing factual, nonjudgmental counseling are essential for engaging with youth. By contextualizing HIV risk discussions within comprehensive sexuality education about behaviors other than abstinence or heterosexual norms, youth may have greater comprehension of the problem and their own risk and be willing to seek care from pediatricians.22,27
The USPSTF and the AAP recognize that all youth are at current or future risk of STIs and HIV infection. Both organizations recommend that all youth receive behavioral counseling to prevent STIs, including the recommendation that they delay sexual activity.22,29 Opportunities to discuss HIV and STIs with youth during routine annual well health assessments are often missed, and youth of underresourced ethnic groups are less likely to receive regular preventive health care.30 The administration of vaccines in adolescent and youth populations provides an additional opportunity for health promotion and preventive counseling including STI and HIV prevention among other topics such as healthy diet and exercise.31 School physicals and annual athletic preparticipation physical examinations provide other opportunities to discuss HIV and STIs, conduct risk assessment, and provide health guidance and offer testing; these examinations are often the only contact youth have with any health care provider and should occur in the context of the medical home during the health supervision appointment by the athlete’s primary care provider.25,32
Testing for HIV
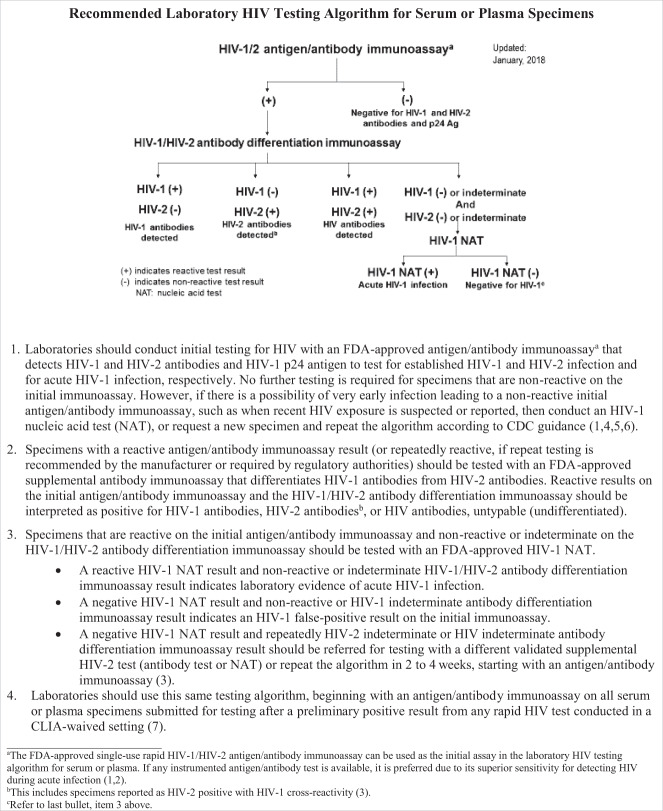
Since the previous versions of AAP policy statements were published, improved immunoassays that combine detection of HIV-specific immunoglobulin M and immunoglobulin G antibodies (AB) with detection of p24 antigen (AG), also called fourth generation combination or “combo” assays, and differentiation assays that distinguish HIV-1 from HIV-2* AB, received US Food and Drug Administration (FDA) approval for use in the diagnosis of HIV infection.33,34 The current national standard HIV diagnostic testing algorithm is summarized in Fig 1.35 Laboratories should conduct initial testing for HIV on serum or plasma with an FDA-approved fourth generation AG/AB combination immunoassay† to screen for established infection with HIV-1 or HIV-2 and for acute HIV-1 infection.33,35 Initial testing with AG/AB combination immunoassays has now replaced third-generation AB immunoassays because AG/AB combination immunoassays detect more acute HIV-1 infections and identify comparable numbers of established HIV-1 and HIV-2 infections with comparable specificity. No further testing is required for specimens that are nonreactive on the initial immunoassay. However, if there is a possibility of early infection leading to a nonreactive initial AG/AB immunoassay, such as when recent HIV exposure (within 2–4 weeks) is suspected or reported or for patients with clinical features of acute HIV infection, then an HIV-1 nucleic acid test (NAT) should be performed on the same sample, or additional blood can be obtained as soon as possible (preferably within 2 weeks), and the algorithm for testing should be repeated according to CDC guidance. Specimens with a reactive AG/AB combination immunoassay result are routinely tested with an FDA-approved antibody immunoassay that differentiates HIV-1 from HIV-2 AB. Reactive results on the initial AG/AB combination immunoassay and the HIV-1/HIV-2 AB differentiation immunoassay should be interpreted as positive for HIV-1 AB, HIV-2 AB, or HIV untypable (undifferentiated) AB. Specimens that are reactive on the initial AG/AB combination immunoassay and nonreactive or indeterminate on the HIV-1/HIV-2 AB differentiation immunoassay are routinely tested with an FDA-approved HIV-1 NAT and interpreted as follows:
A reactive HIV-1 NAT result and nonreactive or indeterminate HIV-1/HIV-2 AB differentiation immunoassay result indicates laboratory evidence of acute HIV-1 infection.
A negative HIV-1 NAT result and nonreactive or HIV-1 indeterminate AB differentiation immunoassay result indicates an HIV-1 false-positive result on the initial immunoassay.
A negative HIV-1 NAT result and repeatedly HIV-2 indeterminate or HIV indeterminate AB differentiation immunoassay result should be referred for testing with a different validated supplemental HIV-2 test (AB test or NAT) or repeat the algorithm in 2 to 4 weeks, starting with an AG/AB immunoassay.33,35
FIGURE 1.
Recommended laboratory HIV testing algorithm for serum or plasma specimens.35aThe FDA-approved single-use rapid HIV-1/HIV-2 antigen/antibody immunoassay can be used as the initial assay in the laboratory HIV testing algorithm for serum or plasma. If any instrumented antigen/antibody test is available, it is preferred because of its superior sensitivity for detecting HIV during acute infection.33,54bThis includes specimens reported as HIV-2 positive with HIV-1 cross-reactivity.55cA negative HIV-1 NAT result and repeatedly HIV-2 indeterminate or HIV indeterminate antibody differentiation immunoassay result should be referred for testing with a different validated supplemental HIV-2 test (antibody test or NAT) or repeat the algorithm in 2 to 4 weeks, starting with an antigen/antibody immunoassay.55 Source: Centers for Disease Control and Prevention and Association of Public Health Laboratories. 2018 Quick reference guide: recommended laboratory HIV testing algorithm for serum or plasma specimens. Available at: https://stacks.cdc.gov/view/cdc/50872.
An estimated 50% of patients acutely infected with HIV present with symptoms to health care providers; however, few providers make the diagnosis at this time.36–38 Symptoms of acute retroviral syndrome are outlined in Table 1. Although some patients with acute HIV-1 infection experience symptoms, a recent prospective study shows that most patients have nonspecific and relatively mild signs and symptoms.39 Pediatricians may not recognize acute HIV-1 infection, because its manifestations are often similar to those of many other viral infections, such as infectious mononucleosis and influenza. Acute infection can also be asymptomatic. Table 1 provides pediatricians with guidance to recognize and diagnose acute HIV-1 infection. Acute HIV-1 infection is part of the differential diagnosis in patients who have a suggestive clinical syndrome (signs or symptoms include but are not limited to one or more of the following: fever, lymphadenopathy, skin rash, myalgia, arthralgia, headache, diarrhea, or oral ulcers), especially those who report recent high-risk behavior (see Table 1).16
TABLE 1.
Identifying and Diagnosing Acute and Recent HIV-1 Infection
| Suspicion of acute HIV-1 infection |
| Acute HIV-1 infection should be considered in individuals with signs or symptoms described below and recent (within 2 to 6 wk) high risk of exposure to HIV-1.a |
| Signs, symptoms, or laboratory findings of acute HIV-1 infection may include but are not limited to one or more of the following: fever, lymphadenopathy, skin rash, myalgia, arthralgia, headache, diarrhea, oral ulcers, leucopenia, thrombocytopenia, transaminase elevation. |
| High-risk exposures include sexual contact with a person who has HIV-1 infection or a person at risk for HIV-1 infection, sharing of injection drug use paraphernalia, or any exposure in which an individual’s mucous membranes or breaks in the skin come in contact with bodily fluid potentially infected with HIV. |
| Differential diagnosis: The differential diagnosis of HIV-1 infection may include but is not limited to viral illnesses such as EBV and non-EBV (eg, cytomegalovirus) infectious mononucleosis syndromes, influenza, viral hepatitis, streptococcal infection, or syphilis. |
| Evaluation and diagnosis of acute HIV-1 infection |
| Acute HIV-1 infection is defined as detectable HIV-1 RNA or p24 antigen (the antigen used in currently available HIV Ag/Ab combination assays) in the setting of a negative or indeterminate HIV-1 antibody test result. |
| A reactive HIV antibody test result or Ag/Ab combination test result must be followed by supplemental confirmatory testing. |
| A negative or indeterminate HIV-1 antibody test result in a person with a reactive Ag/Ab test result or in whom acute HIV-1 infection is suspected requires plasma HIV-1 RNA testing to diagnose acute HIV-1 infection. |
| A positive result on a quantitative or qualitative plasma HIV-1 RNA test in the setting of a negative or indeterminate antibody test result indicates that acute HIV-1 infection is highly likely, in which case, the diagnosis of HIV-1 infection should be later confirmed by subsequent documentation of HIV antibody seroconversion. |
Information from Panel on Antiretroviral Guidelines for Adults and Adolescents.56 Ab, antibody; Ag, antigen; EBV, Epstein-Barr virus.
In some settings, behaviors that increase the risk of HIV-1 infection may not be recognized or perceived as risky by the health care provider or the patient, or both. Thus, even in the absence of reported high-risk behaviors, symptoms and signs consistent with acute retroviral syndrome should motivate practitioners to consider a diagnosis of acute HIV-1 infection.
Patients may not always disclose high-risk behaviors or perceive that such behaviors put them at risk for HIV-1 acquisition. Thus, even in the absence of reported high-risk behaviors, a low threshold is still used for considering and performing testing for a diagnosis of acute HIV-1 infection, especially in high-prevalence areas (areas where ≥1% of people have HIV infection). Current statistics on the prevalence of HIV in different geographical areas in the United States can be found online through AIDSVu (https://aidsvu.org/)40 and the CDC’s AtlasPlus (https://www.cdc.gov/nchhstp/atlas/)41 or via local health departments, where available.
The use of noninvasive rapid oral fluid testing devices that measures HIV AB only and not AG in mucosal transudate is well accepted by youth and is used in many outreach settings.13 In addition, multiple rapid HIV AB tests used in clinical and nonclinical settings on fingerstick or venous serum, plasma, or whole-blood samples provide results in minutes.42–44 Among rapid tests, self-testing HIV AB tests have been approved in the United States since 2012 and are available over the counter, although data on their use in youth remain limited.45–47 In routine care, a negative rapid AB test result does not need confirmation, unless acute HIV infection is suspected. In this case, an HIV AG/AB test or HIV NAT should be performed. The advantage of the rapid AB test is that the results can be given to the patient immediately with the caution that positive results need to be confirmed. The disadvantage of the rapid AB test is that it can be negative during the first weeks up to 6 months after transmission and, therefore, might miss acute HIV infection, as described below. Pediatricians who see youth with initial positive rapid test results should discuss the results with the patient and obtain a confirmatory laboratory-based AG/AB combination immunoassay following the algorithm in Fig 1, with serum or plasma specimens submitted for testing after a reactive (preliminary positive) result from any rapid HIV test.
It is important to disclose a positive HIV test result to youth before involving the parent or caregiver. In fact, disclosure of the HIV status to the parent or caregiver for patients younger than 18 years may require adolescent consent and follows consent and confidentiality regulations outlined in “Consent and Confidentiality.” Preferred methods of communicating about HIV test results to youth need to be discussed before or at the time of testing. Although in-person disclosure is preferred, disclosure can occur by phone or through patient portal when necessary. Patient communication tools and suggested language are available from the CDC (see “Understanding a Positive Result” [www.cdc.gov/hiv/basics/hiv-testing/positive-hiv-results.html]).48 Suggestions for discussion include what follow-up testing may be required, focusing on HIV as a manageable disease, discussing disclosure and stigma, addressing prevention and partner notification, and arranging linkage to care and initiation of antiretroviral treatment. Local health departments, pediatric infectious disease clinics, HIV care and treatment clinics, community partners, and case managers can assist with linking youth with appropriate care and counseling after diagnosis. The federal government maintains a Web site to help people find HIV treatment services across the nation (https://hivinfo.nih.gov/understanding-hiv/fact-sheets/how-find-hiv-treatment-services).49 HIV-infected youth should be cared for by pediatric or adult providers with expertise in HIV medicine.50,51
Negative HIV test results can be communicated in person, by phone or telemedicine, or via electronic health record patient portals. Reviewing negative HIV test results with youth represents an opportunity for pediatricians to provide risk and sexual and reproductive health counseling. With the advent of HIV PrEP as discussed further below, a negative HIV test result in youth at risk for HIV acquisition is also a critical moment for reinforcing the need for repeat testing over time and consideration of the preventive intervention. PrEP has also been described as a “gateway” to primary care, such that individuals receiving PrEP in a community clinic setting may be more likely to receive general primary care.52 In high-risk situations, such as sex with an HIV-infected partner, sexual assault, or other community nonoccupational exposures, HIV PEP should be considered as discussed below, and HIV testing should be repeated per CDC guidance.53
The information in this section was adapted from CDC, USPHS.19
Implementation of HIV Screening
The USPSTF recommends that clinicians routinely screen for HIV infection in adolescents and adults aged 15 to 65 years and screen younger adolescents and older adults at increased risk.17 Opt-out HIV testing, which refers to testing performed unless the patient declines, should be voluntary and done only with the patient’s knowledge and understanding but can be routinely performed without a separate written informed consent or pretest counseling.16 Currently in the United States, the CDC reports that most states meet these recommendations and allow for opt-out HIV testing without written consent.57 Based on explicit language in local statutes and regulations, 39 states at the time of this publication stipulate that HIV testing may be provided to a minor without parental or guardian consent, with caveats58 (eg, lower age limits vary; see details provided under “Consent and Confidentiality”).
Pediatricians should be aware of their local HIV prevalence data, because some US communities have high rates of HIV, which places youth at disproportionate risk. Current statistics on the prevalence of HIV in different geographical areas in the United States can be found online through AIDSVu (https://aidsvu.org/)40 and the CDC’s AtlasPlus (https://www.cdc.gov/nchhstp/atlas/) or via local health departments, where available.41 Pediatricians who care for youth in areas that have low prevalence rates should continue providing targeted testing to youth at risk, including all sexually active adolescents. Community-based targeted approaches to HIV testing may be more effective than universal screening for reaching lesbian, gay, bisexual, and transgender youth of color, identifying previously undiagnosed HIV-infected youth, and linking HIV-negative youth to relevant prevention services.59 Youth at high risk include MSM, active injection drug users, and transgender youth. Risk factors for HIV infection include not using barrier protection during vaginal or anal intercourse; having sexual partners who are HIV-infected, of both genders, or injection drug users; or exchanging sex for drugs or money. Other people at high risk include those who have a diagnosis of or request testing for other STIs. Youth may also request HIV testing in the absence of reported risk factors. Testing should be driven by youth request, not necessarily parent, guardian, or caregiver request. The USPSTF recognizes that categories of risk are not mutually exclusive, the degree of sexual risk is on a continuum, and individuals may not be aware of their sexual partners’ risk factors for HIV infection. Moreover, it is important to bear in mind that youth may be reluctant to disclose having HIV risk factors, even when asked.17 If youth are reluctant to discuss sexual activity and/or risk factors, it is still possible to discuss the risk reduction strategies including PrEP as part of well-being.
In terms of screening frequency, one reasonable approach would be initial screening of all youth, followed by periodic repeat screening (annually) for sexually active youth or more frequent (every 3 months) screening for those youth on PrEP or youth with high-risk behaviors and/or living or receiving medical care in high HIV prevalence settings, such as STI clinics, correctional facilities, homeless shelters, tuberculosis clinics, clinics and community venues serving MSM and transgender populations, and adolescent health settings with a high prevalence of STIs.17 Routine rescreening may not be necessary for individuals who have not been at increased risk since they were found to be HIV-negative.17 Female youth screened during a previous pregnancy should be rescreened during each subsequent pregnancy.17 Because 27% of pregnancies in the United States occur in women younger than 25 years,60 routine HIV screening and rescreening in the third trimester in jurisdictions with high rates of HIV infection in pregnant women can lead to early identification of HIV infection and have a substantial impact on preventing perinatal transmission of HIV.
Although several studies have shown the cost-effectiveness of routine HIV screening, data addressing this issue in youth are insufficient.61–63 One national modeling study assessed the optimal age at which a one-time HIV screen should begin for youth without identified HIV risk factors in the United States and concluded that delaying a one-time routine HIV screen to 25 years of age would optimize clinical outcomes and be cost-effective.64 However, cost-effectiveness analyses were most sensitive to variations in proportion of youth linked to care (which have improved since the model’s assumptions were developed) and costs of HIV screening and care (which may change). The cost-effectiveness analyses also did not account for impact from several generations of transmission averted with earlier diagnosis and could not fully address impact of variation in HIV burden by geography and race.64,65
Nearly half of recently identified infected people had their first HIV test within 1 year of receiving the diagnosis of AIDS. These so-called late testers were generally Black or Latinx youth who partnered with the opposite sex, had limited or incomplete education, and were more likely to be identified through a health care setting than through targeted testing.16 Early testing plays an important role in the health of the individual adolescent and the community. There is evidence that at least 20% of newly diagnosed youth seroconverted within the previous 6 months.66 This early phase of infection is associated with high viremia, during which the risk of infectivity and transmission is greatest.33 People who are aware of their HIV status are more likely to practice safer sex or remain abstinent.67 Patients who learn of their diagnosis and are treated earlier virtually never develop AIDS or have a slower progression to AIDS if they stay adherent to treatment. They are also more likely to preserve or restore immunologic function and are less likely to develop HIV drug resistance68 and transmit HIV to others. Antiretroviral therapy is recommended for all individuals with HIV, including youth, to reduce morbidity and mortality and decrease transmission.
The health care setting has many advantages as a site of HIV testing for youth. Adolescents are more likely to agree to be tested if it is recommended by a physician and in settings where everyone else is screened.12,69 In addition, youth who learn of their diagnosis at a health care facility are more likely to be linked to HIV care in a timely fashion66 and maintain HIV-related health care after initial linkage.70
The use of acute care settings to improve testing rates is attractive to youth, because they are more likely to use urgent care settings for their health care needs.71 In the years before diagnosis, many HIV-infected adults seek care for HIV-related symptoms in acute care settings.72 Implementation of rapid HIV testing in the emergency department setting has improved testing rates and greatly benefits youth who prefer rapid testing. Studies in pediatric emergency departments used multisystem approaches to implement routine screening with rapid HIV testing. A minority of youth (13% to 27%) opted out; younger age and the presence of a guardian were significantly associated with opting out of HIV screening.73,74 Effective implementation of HIV screening in emergency care settings, including pediatric emergency departments, requires commitment by staff, ongoing HIV education and trainings, and an effective means of reminding staff to routinely perform the test (eg, electronic prompts with eligibility criteria). Most importantly, youth-tailored pathways need to provide linkage to preventive and therapeutic care and treatment services after HIV testing in acute care settings such as pediatric emergency departments.
PrEP and PEP
The FDA first approved the use of fixed-dose tenofovir disoproxil fumarate (TDF)/emtricitabine (FTC) for adult HIV PrEP in 2012, as part of a comprehensive prevention strategy that includes other prevention measures, including adherence to daily administration and safer sex practices including barrier protection, to reduce the risk of STIs. On the basis of several studies demonstrating the safety and efficacy of PrEP, in 2014, the USPHS first recommended that PrEP be offered to adults at substantial risk of HIV infection. Updated 2017 USPHS guidelines defined adults (18 years and older) at “substantial risk” of acquiring HIV among sexually active people and persons who inject drugs.19
Referencing the paucity of research inclusive of adolescents younger than 18 years, the 2017 USPHS guidelines recommended that providers should carefully consider potential risks and benefits of providing PrEP to those younger than 18 years who are at high risk for acquiring HIV infection. Since then, 2 Adolescent Medicine Trials Network (ATN) open-label studies have been published and demonstrate the acceptability and safety of PrEP among young MSM ages 15 through 17 years (ATN 113) and 18 through 24 years (ATN 110).75,76 The findings from ATN 113 have informed the expanded approval of TDF/FTC as PrEP for adolescents who weigh at least 77 lb (35 kg).77 In 2019, the USPSTF recommended that clinicians offer PrEP with effective antiretroviral therapy to all people who are at high risk of HIV acquisition.20 In 2019, FDA also approved a second fixed-dose combination tablet tenofovir alafenamide (TAF)/FTC as PrEP for adolescents and adults weighting at least 77 lb (35 kg), excluding those at risk for acquiring HIV through receptive vaginal sex because of the lack of clinical data regarding the efficacy of TAF/FTC in cisgender women.78 Clinical trials to evaluate TAF/FTC safety, efficacy, and adherence in adolescents were not specifically performed; efficacy and safety data to support the FDA approval of TAF/FTC for PrEP were instead extrapolated from the DISCOVER trial in adult MSM and transgender women and from trials of TAF/FTC in adolescents with HIV.79 In 2020, the CDC reviewed clinical considerations specific to PrEP in adolescents and concluded that “PrEP is an effective HIV prevention tool for protecting adolescents at risk for HIV acquisition,” as part of a comprehensive approach to HIV prevention tailored to the adolescent’s specific needs.80
Two once-daily medication regimens have been approved by the FDA for PrEP: TDF coformulated with FTC (comes only as a fixed-dose combination of TDF 300 mg/FTC 200 mg), and TAF coformulated with FTC (comes only as a fixed-dose combination of TAF 25 mg/FTC 200 mg). Both PrEP tablets are prescribed once daily and are generally well tolerated, although TAF/FTC is significantly smaller in size. Both single-tablet PrEP regimens require establishing HIV and hepatitis B status before start and baseline evaluation and monitoring of renal function. Neither medication has been FDA approved for PrEP use on an event-driven basis (around the time of sex, “on-demand”). Furthermore, a longer period of consistent oral dosing of PrEP is required to build up protective levels of antiretroviral medication in vaginal tissue versus rectal tissue, indicating that higher levels of adherence to daily PrEP are necessary to gain protection from vaginal exposures to HIV.81Table 2 summarizes indicators of substantial risk and current guidance for HIV PrEP use, including clinical eligibility, prescribing, and follow-up every 3 months. These indicators require pediatricians to be familiar with the local HIV prevalence and obtain detailed sexual histories from adolescents, including number of sexual partners, information on past STIs, use of barrier protection, whether sex is transactional for drugs or money, and whether they are aware of their sexual partner(s) HIV status. PrEP should also be considered when youth request PrEP yet do not disclose specific risk factors, because youth may be reluctant to disclose having HIV risk factors, even when asked.17
TABLE 2.
Summary of Guidance for HIV PrEP Use
| Sexually Active Youth | Youth Who Inject Drugs | |
|---|---|---|
| Indicators of substantial risk of acquiring HIV | HIV-positive sexual partner | HIV-positive injecting partner |
| High HIV prevalence area | Sharing injection equipment | |
| High HIV prevalence sexual network | ||
| High number of sexual partners | ||
| Recent bacterial STI | ||
| Recurrent PEP use | ||
| Inconsistent or no barrier protection use | ||
| Exchanging sex for drugs or money | ||
| Sexually Active Youth and Youth Who Inject Drugs | ||
| Clinically eligible for PrEP | Negative HIV test result before prescribing PrEP | |
| No signs/symptoms of acute HIV infection | ||
| Documented hepatitis B infection and vaccination statusa | ||
| Normal renal function | ||
| No medications contraindicated for use with TDF/FTC or TAF/FTC | ||
| Prescription | Single daily dose of TDF/FTC, ≤90 day supply | |
| Single daily dose of TAF/FTC, ≤90 day supplyb | ||
| Follow-up (every 3 mo) | Repeat HIV test | |
| Adherence counseling | ||
| Side effect assessment | ||
| Risk reduction counseling and support | ||
| STI symptom assessment and testingc | ||
| Renal function reassessmentd | ||
| Pregnancy intention reassessment and testing for female individualse | ||
| For youth who inject drugs or use other substances, support access to clean needles/syringes and treatment services | ||
Patients determined to be susceptible to HBV infection should be vaccinated. Patients found to be hepatitis B surface antigen positive should be evaluated for possible treatment either by the clinician providing PrEP care or by linkage to an experienced hepatitis B care provider. Hepatitis B virus infection is not a contraindication to PrEP use. Both TDF and FTC are active against hepatitis B. Hepatitis B virus-monoinfected patients taking TDF or FTC, whether as PrEP or to treat hepatitis B infection, who then stop these medications must have their liver function closely monitored for reactivation of hepatitis B virus replication that can result in hepatic damage.
TAF/FTC is not indicated for youth at risk for HIV-1 infection from receptive vaginal sex because the effectiveness in this population has not been evaluated.
Includes oral/rectal STI testing for MSM and other eligible youth.
At 3 mo and every 6 mo thereafter.
Pregnancy and breastfeeding are not contraindications to PrEP prescribing.
Although PrEP is effective for preventing HIV acquisition, efficacy correlates with adherence, and optimizing adherence remains a challenge for youth.80,82 The ATN studies described poor adherence in these groups compared with adult participants in PrEP trials, indicating a need for additional strategies to support adherence, such as the use of mobile technology, peer navigation, and other youth-focused interventions.75,76 Furthermore, knowledge about and uptake of PrEP remain critically low among youth in the United States, representing an additional barrier to scaling up PrEP usage. Youth at high risk for HIV, including youth in high prevalence of HIV and sexual violence settings, lesbian, gay, bisexual, and transgender youth of color, and homeless youth, have the lowest rates of PrEP awareness and uptake.83–86
Understanding health care provider knowledge, attitudes, and willingness to prescribe PrEP will also be crucial in the successful implementation of PrEP for youth.80 Few studies have examined providers’ perspectives on PrEP specifically for youth. In some studies, health care providers have expressed concerns about potential challenges with adherence, high costs, and risk compensation for both adults and adolescents.87,88 In other studies, providers have expressed concerns about the development of viral resistance as a result of incomplete adherence, but selection for HIV drug resistance with PrEP use is likely to be infrequent and most likely to occur in rare circumstances in which PrEP is used inadvertently during undiagnosed HIV infection.89 The benefit of decreased HIV incidence with wider PrEP use is likely to outweigh the risk of harms from possible increases in the prevalence of HIV drug resistance.89 A “purview paradox” has been described in the United States among primary care providers and HIV care providers such that HIV care providers may have few opportunities to prescribe PrEP because they often see few HIV-uninfected patients. Yet primary care providers, who may have more opportunity to provide PrEP to at-risk patients who are HIV-uninfected, describe concerns about PrEP feasibility in their practice given their limited experience with antiretroviral medications.90 Complexities in confidentiality and consent in adolescent care and variability in how statutes and regulations address these issues may make PrEP implementation in minors even more challenging and are addressed in “Consent, Confidentiality, and Coverage.” Primary care providers, who are well-positioned to counsel and offer PrEP to youth, need more education and support to normalize PrEP as part of the sexual and reproductive health education and prevention toolkit for youth. For example, instead of determining PrEP eligibility on the basis of HIV risk factors, PrEP discussions could be incorporated within the context of overall healthy lifestyle promotion.91 Finally, with recent recommendations and practical steps broadening pool of health care providers (including pharmacists) who prescribe PrEP, pediatricians must be prepared to provide counseling, treatment, clinical and laboratory monitoring, and repeat HIV testing to youth who initiate PrEP elsewhere. Providers can also get real-time expert consultation from the national hotline AIDS Education and Training Centers National Clinicians Consultation Center Pre-Exposure Prophylaxis Service (PrEPline): 855-HIV-PrEP (855-448-7737). Numerous online training resources from organizations such as the CDC, AIDS Education and Training Centers, and the National LGBTQIA+ Health Education Center also exist.
Use of PEP with antiretroviral drugs should be considered for youth who may have been exposed to HIV after an episode of high-risk sexual activity or unsafe needle use or after sexual violence and sexual abuse. Recurrent PEP use is also an indication that PrEP may be indicated. Guidelines for the use of PEP in nonoccupational exposures are available,92 and health care providers can get expert consultation from the AIDS Education and Training Centers National Clinicians Consultation Center Post-Exposure Prophylaxis Hotline (PEPline): 888-HIV-4911 (888-448-4911). (Health care personnel occupational HIV exposures fall under a separate rubric and guidance document and are not typically managed in primary care.93) Survivors of sexual violence should have baseline HIV testing as well as STI screening and treatment and should be offered mental health and other supportive counseling.94,95 Specific sexual violence and sexual abuse reporting requirements for parents, child protective services, or law enforcement vary by state or even local jurisdiction. Pediatricians need to know the specific reporting laws in the states in which they practice.94,96
Consent, Confidentiality, and Coverage
Research has found that youth might forgo sexual and reproductive health services if parental consent is required.97,98 Laws concerning consent and confidentiality for HIV care and treatment vary among states; thus, pediatricians need to familiarize themselves with local laws. The CDC maintains the Web site “State Laws that address High-Impact HIV Prevention Efforts” (https://www.cdc.gov/hiv/policies/law/states/index.html), which can help health care providers seeking clarification of how their state laws and the CDC recommendations apply in clinical practice.57 The Web site comprehensively presents clinicians with regular updates to each state’s HIV testing laws. The CDC (https://www.cdc.gov/hiv/policies/law/states/minors.html), the Guttmacher Institute (https://www.guttmacher.org/state-policy/explore/minors-access-sti-services), and the Center for Adolescent Health and the Law provide resources summarizing minor consent laws for each state.58,99,100 All 50 states and the District of Columbia explicitly allow minors to consent to STI services, although few (11) states require that a minor be of a certain age (generally 12 or 14 years) before being allowed to consent. More than half (32) of states explicitly include HIV testing and treatment, either in the package of STI services to which minors may consent or as part of a law applicable only to HIV testing. Several (18) states allow physicians to inform a minor’s parent or guardian that he or she is seeking or receiving STI services; however, with the exception of 1 state that requires parental notification in the case of a positive HIV test result (Iowa), no state requires that physicians notify parents about services, less than half (23) of jurisdictions permit HIV disclosure to parents or guardians, and few (10) jurisdictions explicitly do not permit disclosure to parents or guardians without consent from the minor. No jurisdiction explicitly prohibits minors’ access to PrEP without parent or guardian consent. Several (16) jurisdictions have statutes and regulations that explicitly allow minors of a particular age to independently access PrEP; the age for access varies by jurisdiction. However, minors might still be legally allowed to access PrEP without parental or guardian consent in some jurisdictions without explicit statutes and regulations. Although state laws are always in evolution and the information presented here is current as of the time of publication, pediatricians need to know and abide by the laws in effect in their jurisdiction. To learn more about laws and legislation in your state, please contact the AAP State Advocacy team at stgov@aap.org.
Physicians have an ethical and legal obligation to maintain confidentiality regarding their patients’ confidential health information, the assurance of which is crucial in optimizing patient testing for HIV and personal disclosure. Only where there is specific legal requirement to report or notify is breaching of confidentiality justified. Disclosure of HIV infection status is regulated by federal policies and state laws. The federal government’s Health Resources and Services Administration Ryan White HIV/AIDS Program requires that health departments receiving money from the Ryan White program show “good faith” efforts to notify the marriage partners of a patient with HIV infection. Some state laws criminalize behaviors that can potentially expose another person to HIV, increase sentence lengths when a person commits certain crimes while infected with HIV, and require disclosure to sexual and/or needle sharing partners by either the patient or their health care provider (“duty to warn”).101,102 Overall, state statutes generally fall into 3 types: (1) some state statutes mandate that the physician provide the contact’s name to the state health agency; the state health agency then notifies the contact; (2) some states give the physician the choice of notifying either the state health agency or the third-party contacts directly; and (3) other states make such disclosures to a state agency optional.103 Because this is an area of state-to-state variation, and because law and policy continually evolve and change, pediatricians should seek advice from public health departments and their own attorneys to understand their legal responsibilities.
Pediatricians who intend to disclose their adolescent patient’s HIV status to parents or guardians should inform the patient of their intent before testing and describe the process of disclosure. Optimally, adolescents would benefit from the support of a parent or guardian when faced with a diagnosis of HIV; however, each case should be approached individually. Disclosure to school or college authorities without an adolescent’s consent is not indicated and can be harmful. Because many electronic health record platforms automatically release laboratory test results to both the patient and parent or legal guardian proxy accounts, pediatricians need to be cognizant of electronic health record settings and the potential of inadvertent disclosure via patient portals.104
Payment and disclosure of STIs and HIV testing, prevention, and treatment to parents via insurance billing are issues that require additional attention. At present, the Affordable Care Act requires coverage of recommended preventive services, including HIV testing and PrEP, without cost-sharing, for the following health plans: nongrandfathered private health insurance plans, Medicare, Medicaid expansion plans, and traditional Medicaid plans (which may cover HIV testing to receive an increase in their federal medical assistance).105 Coverage for PrEP is approved by many insurance plans and is also available through state drug assistance programs and pharmaceutical industry-supported programs. The national Ready, Set, PrEP program (https://www.getyourprep.com/) and local health departments can serve as excellent resources for facilitating access to PrEP among youth and locating the clinics and programs that provide PrEP at no cost to clients. Pediatricians, health advocates, insurers, and states can influence policies around confidentiality and insurance coverage that can address the aforementioned issues. If pediatricians are unable to provide confidential HIV testing for adolescent patients in their office setting, they should identify and refer youth to confidential community-based HIV testing. Increased awareness of community clinical resources will assist providers in referring patients who are not willing to risk potential disclosure of confidential services through electronic health records or billing statements. Title X clinics, funded by the Office of Population Affairs of the US Department of Health and Human Services, provide high-quality, cost-effective family planning and preventive services for women and men with limited resources as well as for youth seeking confidential care (a search tool for clinics is available at: http://www.hhs.gov/opa/title-x-family-planning/initiatives-and-resources/title-x-grantees-list/).106 A CDC Web site (https://gettested.cdc.gov)107 provides assistance in finding local HIV testing sites.
HIV and AIDS are conditions reportable to public health authorities in the United States, and in many jurisdictions, both laboratory reporting data streams and clinical case reports translate information directly to public health departments, which have a role in contact tracing and partner notification. Public health department partner notification services can play a key role in preventing and controlling the HIV epidemic in the United States. Pediatricians should be familiar with state laws, and they should use reasonable means to persuade and support HIV-infected youth to voluntarily inform their partner(s) when applicable. Health care providers seeing patients who are being tested for HIV or STIs should:
Talk about partner notification services, and let patients know that if they are positive for a reportable disease like HIV, they may be asked about partner exposure and may be contacted by someone from the health department.
Inform youth that partner notification services are voluntary and confidential.
Discuss how partner notification services can help their past and/or current sex or drug-injecting partners through early access to testing, treatment, and other services.108
Conclusions and Recommendations
Pediatricians are encouraged to create an environment of confidentiality and tolerance and facilitate open discussion of gender, sexual orientation and behavior, and sexual and reproductive health issues.
Pediatricians should recognize the clinical presentation of the acute retroviral syndrome, which can present clinically as infectious mononucleosis-like and influenza-like syndromes, and consider adding virological testing to AG/AB testing in the diagnostic workup of sexually active youth when symptoms consistent with acute retroviral syndrome are present.
Routine HIV screening is recommended for all youth 15 years or older, at least once, in health care settings.
After initial screening, youth at increased risk, including sexually active youth, should be rescreened at least annually, potentially as frequently as every 3 to 6 months if at high risk (male youth reporting male sexual contact, active injection drug users, transgender youth; having sexual partners who are HIV-infected, of both genders, or injection drug users; exchanging sex for drugs or money; or those who have had a diagnosis of or request testing for other STIs).
Youth who request HIV screening at any time should be tested, even in the absence of reported risk factors.
For youth with a positive HIV test result in any health care or community setting, it is critical to facilitate and confirm prompt linkage to age-appropriate HIV specialty care.
A negative HIV test result provides an opportunity to counsel youth on sexual and reproductive health issues and risk behaviors. All youth at risk for HIV acquisition should be offered HIV PrEP as part of a comprehensive prevention strategy that includes other prevention measures, including adherence to daily administration, and safer sex practices, including barrier protection, to reduce the risk of STIs.
Opt-out HIV testing is preferred if allowed by state laws; rapid AB and AB/AG HIV testing can provide notification of results within a short period of time. Pediatricians should follow the guidelines of their local jurisdictions for routine HIV opt-out testing in youth and are encouraged to advocate for change when such jurisdictions create barriers for implementation of opt-out HIV testing.
In addition to the ambulatory outpatient clinics and inpatient wards, emergency departments and urgent care facilities in areas of high HIV prevalence should implement routine HIV screening for youth, which provides an excellent opportunity to reach youth who may not often seek primary care services.
Use of HIV PEP with antiretroviral drugs should be considered for youth who may have been exposed to HIV after an episode of high-risk sexual activity or unsafe needle use or after sexual violence. Survivors of sexual violence should have baseline HIV testing as well as STI screening and treatment and should be offered mental health and other supportive counseling.
Although parent or guardian involvement in adolescent health care is desired, in the majority of settings in the United States, consent of the adolescent should be sufficient to provide testing and treatment of HIV infection or STIs as part of sexual and reproductive health services. Pediatricians should make use of free and confidential community-based testing programs if there are cost or confidentiality concerns in the office practice setting.
Pediatricians should be familiar with state laws regarding partner notification and should use reasonable means to persuade and support HIV-infected youth to encourage and/or refer partner(s) to be tested when applicable. Pediatricians seeing patients who are being tested for HIV infection or STIs should discuss health department anonymous partner notification services with youth.
Pediatricians are encouraged to advocate for the dissemination of accurate, evidence-based prevention education including HIV PrEP, PEP, and access to confidential HIV and STI counseling, testing, and treatment and partner notification services for youth.
Preventive care screening should include universal coverage and adequate payment for HIV testing, related counseling, PEP, and PrEP. Pediatricians can advocate for confidential billing practices related to HIV and STI testing and prevention in youth.
Lead Authors
Katherine Kai-chi Hsu, MD, MPH, FAAP
Natella Yurievna Rakhmanina, MD, PhD, FAAP, Committee on Pediatric AIDS Chairperson 2020-2023
Committee on Pediatric AIDS, 2018–2019
Ellen Gould Chadwick, MD, FAAP, Chairperson
Echezona Edozie Ezeanolue, MD, MPH, FAAP
Katherine Kai-chi Hsu, MD, MPH, FAAP
Ayesha Mirza, MD, FAAP
Rosemary Olivero, MD, FAAP
Natella Yurievna Rakhmanina, MD, PhD, FAAP
Carina A. Rodriguez, MD, FAAP
George Siberry, MD, MPH, FAAP
Previous Committee Members
Elizabeth Montgomery Collins, MD, MPH, FAAP
Liaisons
Bill G. Kapogiannis, MD, FIDSA
Steven Nesheim, MD
Consultant
Athena P. Kourtis, MD, PhD, MPH, FAAP
Staff
Anjie Emanuel, MPH
Heather Stob
Glossary
- AAP
American Academy of Pediatrics
- AB
antibody
- AG
antigen
- ATN
Adolescent Medicine Trials Network
- CDC
Centers for Disease Control and Prevention
- FDA
US Food and Drug Administration
- FTC
emtricitabine
- MSM
males who have sex with males
- NAT
nucleic acid test
- PEP
postexposure prophylaxis
- PrEP
preexposure prophylaxis
- STI
sexually transmitted infection
- TAF
tenofovir alafenamide
- TDF
tenofovir disoproxil fumarate
- USPSTF
US Preventive Services Task Force
- USPHS
US Public Health Service
Footnotes
FUNDING: No external funding.
Drs Hsu and Rakhmanina were equally responsible for conceptualizing, writing, and revising the manuscript and considering input from all reviewers and the board of directors; and all authors approved the final manuscript as submitted.
This document is copyrighted and is property of the American Academy of Pediatrics and its Board of Directors. All authors have filed conflict of interest statements with the American Academy of Pediatrics. Any conflicts have been resolved through a process approved by the Board of Directors. The American Academy of Pediatrics has neither solicited nor accepted any commercial involvement in the development of the content of this publication.
Clinical reports from the American Academy of Pediatrics benefit from expertise and resources of liaisons and internal (AAP) and external reviewers. However, clinical reports from the American Academy of Pediatrics may not reflect the views of the liaisons or the organizations or government agencies that they represent.
The guidance in this report does not indicate an exclusive course of treatment or serve as a standard of medical care. Variations, taking into account individual circumstances, may be appropriate.
All clinical reports from the American Academy of Pediatrics automatically expire 5 years after publication unless reaffirmed, revised, or retired at or before that time.
Despite increasing use of the HIV-1/HIV-2 differentiation assay, HIV-2 diagnosis in the United States is rare and represents a small fraction (<0.1%) of all confirmed HIV cases. However, identifying individuals with HIV-2 infection remains important because of differing epidemiology, clinical course, and management recommendations for individuals with HIV-2 compared with HIV-1. Individuals identified with HIV-2 should be referred to providers with expertise in HIV medicine for further evaluation and management.
The FDA-approved single-use rapid HIV-1/HIV-2 antigen/antibody immunoassay can be used as the initial assay in the laboratory HIV testing algorithm for serum or plasma. If any instrumented antigen/antibody test is available, it is preferred because of its superior sensitivity for detecting HIV during acute infection.
References
- 1. Centers for Disease Control and Prevention . Estimated HIV incidence and prevalence in the United States, 2014-2018. HIV Surveillance Supplemental Report 2020; volume 25, No. 1. 2020. Available at: https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance- supplemental-report-vol-25-1.pdf. Accessed August 3, 2020
- 2. HIV Surveillance Report , 2018 (Updated); vol. 31. 2020. Available at: https://www.cdc.gov/mmwr/volumes/68/wr/mm6811e1.htm. Accessed August 3, 2020
- 3. Li Z, Purcell DW, Sansom SL, Hayes D, Hall HI. Vital Signs: HIV transmission along the continuum of care — United States, 2016. MMWR Morb Mortal Wkly Rep. 2019;68(11):267–272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bradley H, Hall HI, Wolitski RJ, et al. Vital Signs: HIV diagnosis, care, and treatment among persons living with HIV--United States, 2011. MMWR Morb Mortal Wkly Rep. 2014;63(47): 1113–1117 [PMC free article] [PubMed] [Google Scholar]
- 5. Zanoni BC, Mayer KH. The adolescent and young adult HIV cascade of care in the United States: exaggerated health disparities. AIDS Patient Care STDS. 2014;28(3):128–135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. American Academy of Pediatrics. Committee on Pediatric AIDS and Committee on Adolescence; Committee on Pediatric AIDS and Committee on Adolescence . Adolescents and human immunodeficiency virus infection: the role of the pediatrician in prevention and intervention. Pediatrics. 2001; 107(1):188–190 [DOI] [PubMed] [Google Scholar]
- 7. Emmanuel PJ, Martinez J; Committee on Pediatric AIDS . Adolescents and HIV infection: the pediatrician’s role in promoting routine testing. Pediatrics. 2011;128(5):1023–1029 [DOI] [PubMed] [Google Scholar]
- 8. Underwood JM, Brener N, Thornton J, et al. Overview and methods for the Youth Risk Behavior Surveillance — United States, 2019. MMWR Suppl. 2020;69(1):1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Centers for Disease Control and Prevention . HIV among transgender people. Available at: https://www.cdc.gov/hiv/group/gender/transgender/index.html. Accessed August 4, 2020
- 10. Clark H, Babu AS, Wiewel EW, Opoku J, Crepaz N. Diagnosed HIV infection in transgender adults and adolescents: results from the National HIV Surveillance System, 2009-2014. AIDS Behav. 2017;21(9):2774–2783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Becasen JS, Denard CL, Mullins MM, Higa DH, Sipe TA. Estimating the Prevalence of HIV and Sexual Behaviors Among the US Transgender Population: A Systematic Review and Meta-Analysis, 2006-2017. Am J Public Health. 2019;109(1):e1–e8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kaiser Family Foundation . National survey of young adults on HIV/AIDS. Available at: https://www.kff.org/hivaids/report/national-survey-of- young-adults-on-hiv-aids/. Accessed August 4, 2020
- 13. Peralta L, Deeds BG, Hipszer S, Ghalib K. Barriers and facilitators to adolescent HIV testing. AIDS Patient Care STDS. 2007;21(6):400–408 [DOI] [PubMed] [Google Scholar]
- 14. Henry-Reid LM, O’Connor KG, Klein JD, Cooper E, Flynn P, Futterman DC. Current pediatrician practices in identifying high-risk behaviors of adolescents. Pediatrics. 2010;125(4). Available at: www.pediatrics.org/cgi/content/full/125/4/e741 [DOI] [PubMed] [Google Scholar]
- 15. Goyal MK, Witt R, Hayes KL, Zaoutis TE, Gerber JS. Clinician adherence to recommendations for screening of adolescents for sexual activity and sexually transmitted infection/human immunodeficiency virus. J Pediatr. 2014;165(2):343–347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Branson BM, Handsfield HH, Lampe MA, et al. ; Centers for Disease Control and Prevention (CDC) . Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep. 2006;55(RR-14):1–17, quiz CE1–CE4 [PubMed] [Google Scholar]
- 17. US Preventive Services Task Force . Final Recommendation statement: human immunodeficiency virus (HIV) infection: screening. 2019. Available at: https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/human- immunodeficiency-virus-hiv-infection- screening. Accessed September 7, 2019
- 18. Department of Health and Human Services’ Office of HIV/AIDS and Infectious Disease Policy . National HIV/AIDS Strategy for the United States: 2017 Progress Report. Available at: https://files.hiv.gov/s3fs-public/NHAS_Progress_Report_2017.pdf. Accessed April 4, 2019
- 19. Centers for Disease Control and Prevention . US Public Health Service: Preexposure prophylaxis for the prevention of HIV infection in the United States—2017 Update: a clinical practice guideline. 2018. Available at: https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf. Accessed October 5, 2018
- 20. US Preventive Services Task Force . Final recommendation statement: prevention of human immunodeficiency virus (HIV) infection: preexposure prophylaxis. 2019. Available at: https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/ prevention-of-human-immunodeficiency- virus-hiv-infection-pre-exposure- prophylaxis?ds=1&s=HIV. Accessed June 26, 2019
- 21. Society for Adolescent Health and Medicine; American Academy of Pediatrics . Confidentiality protections for adolescents and young adults in the health care billing and insurance claims process. J Adolesc Health. 2016;58(3):374–377 [DOI] [PubMed] [Google Scholar]
- 22. Marcell AV, Burstein GR; COMMITTEE ON ADOLESCENCE . Sexual and reproductive health care services in the pediatric setting. Pediatrics. 2017;140(5): e20172858. [DOI] [PubMed] [Google Scholar]
- 23. Marcell AV, Breuner CC, Hammer L, Hudak ML; Committee on Adolescence; Committee on Child Health Financing . Targeted reforms in health care financing to improve the care of adolescents and young adults. Pediatrics. 2018;142(6):e20172858. [DOI] [PubMed] [Google Scholar]
- 24. American Academy of Pediatrics . Bright Futures: adolescence tools. Available at: https://brightfutures.aap.org/materials-and-tools/tool-and- resource-kit/Pages/adolescence-tools.aspx. Accessed October 5, 2018
- 25. Committee on Adolescence . Achieving quality health services for adolescents. Pediatrics. 2016;138(2):e20161347. [DOI] [PubMed] [Google Scholar]
- 26. Santelli JS, Klein JD, Song X, et al. Discussion of potentially sensitive topics with young people. Pediatrics. 2019;143(2):e20181403. [DOI] [PubMed] [Google Scholar]
- 27. Hagan JF, Shaw JS, Duncan PM, eds.. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents, 4th ed.Elk Grove Village, IL: American Academy of Pediatrics; 2017 [Google Scholar]
- 28. Breuner CC, Mattson G; Committee on Adolescence; Committee on Psychosocial Aspects of Child and Family Health . Sexuality Education for Children and Adolescents. Pediatrics. 2016;138(2): e20161348. [DOI] [PubMed] [Google Scholar]
- 29. US Preventive Services Task Force . Final recommendation statement: sexually transmitted infections: behavioral counseling. 2016. Available at: https://www.uspreventiveservicestaskforce.org/Page/Document/Recommendation StatementFinal/sexually-transmitted- infections-behavioral-counseling. Accessed October 5, 2018
- 30. Burstein GR, Lowry R, Klein JD, Santelli JS. Missed opportunities for sexually transmitted diseases, human immunodeficiency virus, and pregnancy prevention services during adolescent health supervision visits. Pediatrics. 2003;111(5 Pt 1):996–1001 [DOI] [PubMed] [Google Scholar]
- 31. Rupp R, Rosenthal SL, Middleman AB. Vaccination: an opportunity to enhance early adolescent preventative services. J Adolesc Health. 2006;39(4):461–464 [DOI] [PubMed] [Google Scholar]
- 32. Bernhardt DT, Roberts WO, eds.. PPE: Pre-Participation Physical Evaluation, 5th ed.Itasca, IL: American Academy of Pediatrics Publishing Staff; 2019 [Google Scholar]
- 33. Branson BM, Owen SM, Wesolowski LG, et al. Laboratory Testing for the Diagnosis of HIV Infection: Updated Recommendations. 2014. Available at: 10.15620/cdc.23447. Accessed October 8, 2018 [Google Scholar]
- 34. Peruski AH, Wesolowski LG, Delaney KP, et al. Trends in HIV-2 diagnoses and use of the HIV-1/HIV-2 differentiation test – United States, 2010-2017. MMWR Morb Mortal Wkly Rep. 2020;69(3):63–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Centers for Disease Control and Prevention and Association of Public Health Laboratories . 2018 Quick reference guide: recommended laboratory HIV testing algorithm for serum or plasma specimens. 2018. Available at: https://stacks.cdc.gov/view/cdc/50872. Accessed October 8, 2018
- 36. Weintrob AC, Giner J, Menezes P, et al. Infrequent diagnosis of primary human immunodeficiency virus infection: missed opportunities in acute care settings. Arch Intern Med. 2003;163(17):2097–2100 [DOI] [PubMed] [Google Scholar]
- 37. Hightow-Weidman LB, Golin CE, Green K, Shaw EN, MacDonald PD, Leone PA. Identifying people with acute HIV infection: demographic features, risk factors, and use of health care among individuals with AHI in North Carolina. AIDS Behav. 2009;13(6):1075–1083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. McKellar MS, Cope AB, Gay CL, et al. ; Duke-Unc Acute HIV Infection Consortium . Acute HIV-1 infection in the Southeastern United States: a cohort study. AIDS Res Hum Retroviruses. 2013;29(1):121–128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Robb ML, Eller LA, Kibuuka H, et al. ; RV 217 Study Team . Prospective study of acute HIV-1 infection in adults in east Africa and Thailand. N Engl J Med. 2016;374(22):2120–2130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Emory University, Rollins School of Public Health . AIDSVu. Available at: https://aidsvu.org/. Accessed February 28, 2019
- 41. Centers for Disease Control and Prevention . NCHHSTP AtlasPlus. 2017. Available at: https://www.cdc.gov/nchhstp/atlas/index.htm. Accessed October 8, 2018
- 42. Centers for Disease Control and Prevention . Advantages and disadvantages of FDA-approved HIV assays used for screening. 2018. Available at: https://www.cdc.gov/hiv/pdf/testing/hiv-tests-advantages- disadvantages_1.pdf. Accessed October 8, 2018
- 43. Centers for Disease Control and Prevention . Rapid HIV tests suitable for use in clinical settings (CLIA-moderate complexity). 2016. Available at: https://www.cdc.gov/hiv/pdf/testing/rapid- hiv-tests-clinical-moderate-complexity.pdf. Accessed October 8, 2018
- 44. Centers for Disease Control and Prevention . Rapid HIV tests suitable for use in non-clinical settings (CLIA-waived). 2018. Available at: https://www.cdc.gov/hiv/pdf/testing/rapid-hiv-tests-non-clinical.pdf. Accessed October 8, 2018
- 45. US Food and Drug Administration . Facts about in-home HIV testing. 2017. Available at: https://www.fda.gov/ForConsumers/ConsumerUpdates/ucm310545.htm. Accessed April 7, 2019
- 46. Figueroa C, Johnson C, Verster A, Baggaley R. Attitudes and acceptability on HIV self-testing among key populations: a literature review. AIDS Behav. 2015;19(11):1949–1965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Barksdale A, Ellenberger N, Griffith C, Ferrer K, Madati J, Rakhmanina N. Awareness and acceptance of HIV self-testing and PrEP among adolescents, young adults and their caregivers in Washington, DC, USA. 10th International Workshop on HIV Pediatrics Meeting; July 21–22, 2018; Amsterdam, The Netherlands. [Google Scholar]
- 48. Centers for Disease Control and Prevention . Understanding a positive result. Available at: www.cdc.gov/hiv/basics/hiv-testing/positive-hiv-results.html. Accessed September 16, 2020
- 49. Office of AIDS Research, National Institutes of Health . How to find HIV treatment services. 2020. Available at: https://hivinfo.nih.gov/understanding- hiv/fact-sheets/how-find-hiv-treatment- services. Accessed September 21, 2019
- 50. Landon BE, Wilson IB, McInnes K, et al. Physician specialization and the quality of care for human immunodeficiency virus infection. Arch Intern Med. 2005;165(10):1133–1139 [DOI] [PubMed] [Google Scholar]
- 51. Landovitz RJ, Desmond KA, Gildner JL, Leibowitz AA. Quality of care for HIV/AIDS and for primary prevention by HIV specialists and nonspecialists. AIDS Patient Care STDS. 2016;30(9): 395–408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Marcus JL, Levine K, Grasso C, et al. HIV preexposure prophylaxis as a gateway to primary care. Am J Public Health. 2018;108(10):1418–1420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Centers for Disease Control and Prevention . Updated Guidelines for Antiretroviral Postexposure Prophylaxis After Sexual, Injection Drug Use, or Other Nonoccupational Exposure to HIV— United States, 2016. Available at: https://www.cdc.gov/hiv/pdf/programresources/cdc-hiv-npep-guidelines.pdf. Accessed September 7, 2020 [DOI] [PubMed]
- 54. Centers for Disease Control and Prevention . Technical update: use of the determine HIV 1/2 Ag/Ab combo test with serum or plasma in the laboratory algorithm for HIV diagnosis. 2017. Available at: https://stacks.cdc.gov/view/cdc/48472. Accessed February 28, 2019
- 55. Centers for Disease Control and Prevention . Technical update on HIV-1/2 Differentiation assays. 2016. Available at: https://stacks.cdc.gov/view/cdc/40790. Accessed February 28, 2019
- 56. Panel on Antiretroviral Guidelines for Adults and Adolescents . Guidelines for the use of antiretroviral agents in adults and adolescents living with HIV. Available at: https://clinicalinfo.hiv.gov/sites/default/files/guidelines/documents/AdultandAdolescentGL.pdf. Accessed October 8, 2018
- 57. Centers for Disease Control and Prevention . State laws that address high-impact HIV prevention efforts. 2018. Available at: https://www.cdc.gov/hiv/policies/law/states/index.html. Accessed May 29, 2019
- 58. Centers for Disease Control and Prevention . State laws that enable a minor to provide informed consent to receive hiv and std services. Available at https://www.cdc.gov/hiv/policies/law/states/minors.html. Accessed February 28, 2019
- 59. Miller RL, Boyer CB, Chiaramonte D, et al. Evaluating testing strategies for identifying youths with HIV infection and linking youths to biomedical and other prevention services. JAMA Pediatr. 2017;171(6):532–537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, Mathews TJ. Births: final data for 2015. Natl Vital Stat Rep. 2017;66(1):1. [PubMed] [Google Scholar]
- 61. Paltiel AD, Weinstein MC, Kimmel AD, et al. Expanded screening for HIV in the United States--an analysis of cost-effectiveness. N Engl J Med. 2005;352(6):586–595 [DOI] [PubMed] [Google Scholar]
- 62. Walensky RP, Freedberg KA, Weinstein MC, Paltiel AD. Cost-effectiveness of HIV testing and treatment in the United States. Clin Infect Dis. 2007;45 (Suppl 4):S248–S254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Sanders GD, Bayoumi AM, Sundaram V, et al. Cost-effectiveness of screening for HIV in the era of highly active antiretroviral therapy. N Engl J Med. 2005;352(6):570–585 [DOI] [PubMed] [Google Scholar]
- 64. Neilan AM, Dunville R, Ocfemia MCB, et al. The optimal age for screening adolescents and young adults without identified risk factors for HIV. J Adolesc Health. 2018;62(1):22–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Rakhmanina N, Siberry GK. In search of the right time and right place: screening adolescents and youth for human immunodeficiency virus in the United States. J Adolesc Health. 2018;62(1):3–4 [DOI] [PubMed] [Google Scholar]
- 66. Grant AM, Jamieson DJ, Elam-Evans LD, Beck-Sague C, Duerr A, Henderson SL. Reasons for testing and clinical and demographic profile of adolescents with non-perinatally acquired HIV infection. Pediatrics. 2006;117(3). Available at: www.pediatrics.org/cgi/content/full/117/3/e468 [DOI] [PubMed] [Google Scholar]
- 67. Weinhardt LS, Carey MP, Johnson BT, Bickham NL. Effects of HIV counseling and testing on sexual risk behavior: a meta-analytic review of published research, 1985-1997. Am J Public Health. 1999;89(9):1397–1405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Panel on Antiretroviral Therapy and Medical Management of Children Living with HIV . Guidelines for the use of antiretroviral agents in pediatric HIV infection. Available at: https://clinicalinfo.hiv.gov/sites/default/files/guidelines/documents/PedARV_GL.pdf. Accessed October 23, 2018
- 69. Murphy DA, Mitchell R, Vermund SH, Futterman D, Adolescent Medicine H; Adolescent Medicine HIV/AIDS Research Network . Factors associated with HIV testing among HIV-positive and HIV- negative high-risk adolescents: the REACH Study. Reaching for Excellence in Adolescent Care and Health. Pediatrics. 2002;110(3). Available at: www.pediatrics.org/cgi/content/full/110/3/e36 [DOI] [PubMed] [Google Scholar]
- 70. Philbin MM, Tanner AE, DuVal A, et al. ; Adolescent Trials Network for HIVAIDS Interventions . HIV testing, care referral, and linkage to care intervals affect time to engagement in care for newly diagnosed HIV-infected adolescents in 15 adolescent medicine clinics in the United States. J Acquir Immune Defic Syndr. 2016;72(2):222–229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Miller CA, Tebb KP, Williams JK, Neuhaus JM, Shafer MA. Chlamydial screening in urgent care visits: adolescent-reported acceptability associated with adolescent perception of clinician communication. Arch Pediatr Adolesc Med. 2007;161(8):777–782 [DOI] [PubMed] [Google Scholar]
- 72. Centers for Disease Control and Prevention (CDC) . Missed opportunities for earlier diagnosis of HIV infection--South Carolina, 1997-2005. MMWR Morb Mortal Wkly Rep. 2006;55(47): 1269–1272 [PubMed] [Google Scholar]
- 73. Minniear TD, Gilmore B, Arnold SR, Flynn PM, Knapp KM, Gaur AH. Implementation of and barriers to routine HIV screening for adolescents. Pediatrics. 2009;124(4):1076–1084 [DOI] [PubMed] [Google Scholar]
- 74. Rakhmanina N, Messenger N, Phillips GII, et al. Factors affecting acceptance of routine human immunodeficiency virus screening by adolescents in pediatric emergency departments. J Adolesc Health. 2014;54(2):176–182 [DOI] [PubMed] [Google Scholar]
- 75. Hosek SG, Rudy B, Landovitz R, et al. ; Adolescent Trials Network (ATN) for HIVAIDS Interventions . An HIV preexposure prophylaxis demonstration project and safety study for young MSM. J Acquir Immune Defic Syndr. 2017;74(1):21–29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Hosek SG, Landovitz RJ, Kapogiannis B, et al. Safety and Feasibility of Antiretroviral Preexposure Prophylaxis for Adolescent Men Who Have Sex With Men Aged 15 to 17 Years in the United States. JAMA Pediatr. 2017;171(11): 1063–1071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Food and Drug Administration . Highlights of prescribing information: TRUVADA (emtricitabine and tenofovir disoproxil fumarate) tablets, for oral use. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/021752s055lbl.pdf. Accessed October 5, 2018
- 78. Food and Drug Administration . Highlights of prescribing information: DESCOVY (emtricitabine and tenofovir alafenamide) tablets, for oral use. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/208215s011lbl.pdf. Accessed September 14, 2020
- 79. US Food and Drug Administration . FDA Briefing Document: Meeting of the Antimicrobial Drugs Advisory Committee. Silver Spring, MD: US Food and Drug Administration; 2019. Available at: https://www.fda.gov/media/129607/download. Accessed September 14, 2020 [Google Scholar]
- 80. Tanner MR, Miele P, Carter W, et al. Preexposure prophylaxis for prevention of HIV acquisition among adolescents: Clinical considerations, 2020. MMWR Recomm Rep. 2020;69(3):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Patterson KB, Prince HA, Kraft E, et al. Penetration of tenofovir and emtricitabine in mucosal tissues: implications for prevention of HIV-1 transmission. Sci Transl Med. 2011;3(112):112re4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Allen E, Gordon A, Krakower D, Hsu K. HIV preexposure prophylaxis for adolescents and young adults. Curr Opin Pediatr. 2017;29(4):399–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Siegler AJ, Mouhanna F, Giler RM, et al. The prevalence of pre-exposure prophylaxis use and the pre-exposure prophylaxis-to-need ratio in the fourth quarter of 2017, United States. Ann Epidemiol. 2018; 28(12):841–849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Ajayi AI, Mudefi E, Yusuf MS, Adeniyi OV, Rala N, Goon DT. Low awareness and use of pre-exposure prophylaxis among adolescents and young adults in high HIV and sexual violence prevalence settings. Medicine (Baltimore). 2019;98(43):e17716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Santa Maria D, Flash CA, Narendorf S, et al. Knowledge and attitudes about pre-exposure prophylaxis among young adults experiencing homelessness in seven U.S. cities. J Adolesc Health. 2019;64(5):574–580 [DOI] [PubMed] [Google Scholar]
- 86. Koay WLA, Fortuna G, Griffith C, et al. Awareness of and attitudes toward pre-exposure prophylaxis among predominantly heterosexual black adolescents and young adults and their guardians in an urban area with HIV epidemic in the United States. Pediatr Infect Dis J. 2021;40(4): 351–353 [DOI] [PubMed] [Google Scholar]
- 87. Mullins TLK, Zimet G, Lally M, Kahn JA. Adolescent human immunodeficiency virus care providers’ attitudes toward the use of oral pre-exposure prophylaxis in youth. AIDS Patient Care STDS. 2016;30(7):339–348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Mullins TLK, Zimet G, Lally M, Xu J, Thornton S, Kahn JA. HIV care providers’ intentions to prescribe and actual prescription of pre-exposure prophylaxis to at-risk adolescents and adults. AIDS Patient Care STDS. 2017;31(12):504–516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Gibas KM, van den Berg P, Powell VE, Krakower DS. Drug resistance during HIV pre-exposure prophylaxis. Drugs. 2019;79(6):609–619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Krakower D, Ware N, Mitty JA, Maloney K, Mayer KH. HIV providers’ perceived barriers and facilitators to implementing pre-exposure prophylaxis in care settings: a qualitative study. AIDS Behav. 2014;18(9):1712–1721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Saleska JL, Lee S-J. Normalization of preexposure prophylaxis for adolescents: empowerment, not vulnerability. JAMA Pediatr. 2020; 174(12):1133–1134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Centers for Disease Control and Prevention . Updated guidelines for antiretroviral postexposure prophylaxis after sexual, injection drug use, or other nonoccupational exposure to HIV—United States, 2016. Available at: https://www.cdc.gov/hiv/pdf/programresources/cdc-hiv-npep- guidelines.pdf. Accessed October 5, 2018 [DOI] [PubMed]
- 93. Kuhar DT, Henderson DK, Struble KA, et al. ; US Public Health Service Working Group . Updated US Public Health Service guidelines for the management of occupational exposures to human immunodeficiency virus and recommendations for postexposure prophylaxis. Infect Control Hosp Epidemiol. 2013;34(9): 875–892 [DOI] [PubMed] [Google Scholar]
- 94. Crawford-Jakubiak JE, Alderman EM, Leventhal JM; Committee on Child Abuse and Neglect; Committee on Adolescence . Care of the adolescent after an acute sexual assault. Pediatrics. 2017;139(3):e20164243. [DOI] [PubMed] [Google Scholar]
- 95. Workowski KA, Bachmann LH, Chan PA, et al. Sexually Transmitted Infections Treatment Guidelines, 2021: Sexual Assault and Abuse and STIs. Available at: https://www.cdc.gov/mmwr/volumes/70/rr/rr7004a1.htm#sexualassaultandabuseandstis. Accessed November 28, 2021 [DOI] [PMC free article] [PubMed]
- 96. Child Welfare Information Gateway . State statutes: searchable online database. Available at: https://www.childwelfare.gov/topics/systemwide/laws-policies/state/. Accessed February 21, 2019
- 97. Lehrer JA, Pantell R, Tebb K, Shafer MA. Forgone health care among U.S. adolescents: associations between risk characteristics and confidentiality concern. J Adolesc Health. 2007; 40(3):218–226 [DOI] [PubMed] [Google Scholar]
- 98. Alexander SC, Fortenberry JD, Pollak KI, et al. Sexuality talk during adolescent health maintenance visits. JAMA Pediatr. 2014;168(2): 163–169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Guttmacher Institute . State Laws and Policies: Minors’ access to STI services. Available at: www.guttmacher.org/statecenter/spibs/spib_MASS.pdf. Accessed October 8, 2018
- 100. English A, Bass L, Boyle AD, Eshragh F. State Minor Consent Laws: A Summary, 3rd ed.Chapel Hill, NC: Center for Adolescent Health and the Law; 2010 [Google Scholar]
- 101. Centers for Disease Control and Prevention . HIV and STD criminal laws. Available at: https://www.cdc.gov/hiv/policies/law/states/exposure.html. Accessed January 27, 2020
- 102. Federal HIV Web Council . Your legal rights: limits on confidentiality. Available at: https://www.hiv.gov/hiv-basics/living-well-with-hiv/your-legal- rights/limits-on-confidentiality. Accessed January 27, 2020
- 103. Bradley T. Legal Issues associated with disclosure of patient's HIV-positive status to third parties. TheBodyPro. Available at: www.thebody.com/aahivm/summer02/disclosure.html. Accessed November 3, 2020
- 104. Webber EC, Brick D, Scibilia JP, Dehnel P; Council on Clinical Information Technology; Committee on Medical Liability and Risk Management; Section on Telehealth Care . Electronic communication of the health record and information with pediatric patients and their guardians. Pediatrics. 2019;144(1):e20191359. [DOI] [PubMed] [Google Scholar]
- 105. Centers for Disease Control and Prevention . HIV/AIDS preventive services. Available at: https://www.cdc.gov/nchhstp/preventionthroughhealthcare/preventiveservices/hivaids.htm. Accessed October 8, 2018
- 106. US Department of Health and Human Services, Office of Population Affairs . Title X grantees. Available at: https://www.hhs. gov/opa/title-x-family-planning/title-x-grantees/index.html. Accessed October 8, 2018
- 107. Centers for Disease Control and Prevention . GetTested: National HIV, STD, and hepatitis testing. Available at: https://gettested.cdc.gov. Accessed October 8, 2018
- 108. Centers for Disease Control and Prevention . Partner notification services. Available at: https://www.cdc.gov/actagainstaids/campaigns/pic/talks/partner-notification.html. Accessed October 8, 2018