Abstract
At present, the mechanism of reciprocal ST-segment depression (RSTD) is unclear. ST-segment changes may be caused by the potential difference between the positive and negative electrodes, although this requires further investigation. The characteristics of RSTD and their relationship with ST-segment elevation in acute ST segment elevation myocardial infarction (STEMI) patients were analyzed. We replaced the negative electrode of the precordial leads of an inferior wall myocardial infarction patient and observed the changes in the ST-segment of the precordial leads. A total of 85 patients were included, of which 75 were patients with RSTD. All 45 patients with inferior myocardial infarction had limb lead RSTD, and 37 had anterior lead ST-segment depression. All ST-segment changes in STEMI can be explained by the proposed mechanism, and the value of ST segment depression in limb leads can be calculated by the value of ST segment elevation. In summary, the mechanism of RSTD in acute myocardial infarction may be that the action potential (AP) of the negative electrode of the lead weakens or disappears and the AP of the positive electrode may not be completely offset, resulting in ST-segment depression. Animal experimental studies are needed for further confirmation. When the negative electrode of the precordial lead is changed in acute inferior wall myocardial infarction patient, the ST-segment of the precordial lead changes accordingly. All the changes are consistent with our analysis.
Keywords: electrocardiogram, mechanism, reciprocal ST-segment depression, STEMI
1. Introduction
Acute ST segment elevation myocardial infarction (STEMI) is often accompanied by ST segment depression in the leads opposite to the leads showing ST segment elevation, known as reciprocal ST segment depression (RSTD), which is seen in either ischemia at distance or mirror reflection of ST segment elevation.[1,2] The RSTD mentioned in this paper refers to mirror reflection of ST segment elevation.
At present, RSTD is described as ST segment elevation in any lead that is associated with RSTD in leads whose positive electrode is directed opposite to the leads with ST segment elevation.[3] However, the posterior leads do not present RSTD in anterior myocardial infarction, and RSTD in anterior leads also occur in inferior myocardial infarction.[4] Therefore, the current view is not accurate, and the mechanisms of RSTD warrant further exploration.
Although RSTD is associated with ST-segment elevation, the mechanism of ST-segment elevation is also unclear.[5] ST-segment elevation is caused by a decrease in the amplitude of the action potential (AAP) in the injured area; however, how this happens is unclear. The few existing theories are considered controversial.[5]
Since the electrocardiogram (ECG) records the potential changes of the positive and negative electrodes,[5] the reason for the ST segment changes should be analyzed from the potential change of the positive and negative electrodes of the leads, respectively.
Transmembrane action potential (AP), formed by transmembrane ions, causes periodic changes in the potential inside myocardial cells, as well as reverse periodic changes in the membrane potential( ).[6] Monophasic AP can record intracellular AP extracellularly, proving that intracellular AP can be recorded by electrodes.[7] The potential change of positive electrode recorded by the lead is the same as the change in membrane potential (
).[6] Monophasic AP can record intracellular AP extracellularly, proving that intracellular AP can be recorded by electrodes.[7] The potential change of positive electrode recorded by the lead is the same as the change in membrane potential ( ), while the potential change of negative electrode is the opposite (
), while the potential change of negative electrode is the opposite ( ), which is similar to the change of intracellular potential. Under normal conditions, all myocardium changes synchronously, there is no current within the myocardium, and this fluctuation of the extracellular potential is not shown on the ECG. When myocardial injury occurs, the AP is weakened, the AP of the normal myocardium cannot be offset by the AP of the injured myocardium, and ST segment changes appear. The ST segment of the lead with the injured area as a positive electrode is elevated, while the ST segment of the lead with the injured area as a negative electrode is depressed. The proposed mechanism seems to explain both ST-segment elevation and RSTD in acute myocardial infarction.
), which is similar to the change of intracellular potential. Under normal conditions, all myocardium changes synchronously, there is no current within the myocardium, and this fluctuation of the extracellular potential is not shown on the ECG. When myocardial injury occurs, the AP is weakened, the AP of the normal myocardium cannot be offset by the AP of the injured myocardium, and ST segment changes appear. The ST segment of the lead with the injured area as a positive electrode is elevated, while the ST segment of the lead with the injured area as a negative electrode is depressed. The proposed mechanism seems to explain both ST-segment elevation and RSTD in acute myocardial infarction.
In this study, the ECG of patients with acute STEMI in our hospital were analyzed to summarize the characteristics of RSTD and explore the mechanism of ST-segment changes in acute STEMI.
2. Patients and methods
2.1. Study population
The study design is a retrospective analysis of patients admitted to a tertiary hospital (No.1 Hospital of Jingmen City, Hubei Province, China) from January 1, 2018 to March 31, 2021. The study population included patients presenting to the emergency department with symptoms of acute coronary syndrome and ST segment elevation in their ECGs on admission. The study was approved by the No.1 Hospital of Jingmen ethics committee and oral consent was obtained from patients.
3. Method
All patients subsequently underwent emergency coronary angiographies. The ECG and cardiac catheterization images were retrospectively analyzed by cardiologists.
The diagnosis of STEMI was based on the ECG criteria of ST segment deviations provided by the last consensus document.[8] RSTD was defined as ST segment depression >0.05 mV in any leads, 40 ms after the J-point.
Exclusion criteria: Patients with non-coronary artery disease or multi-vessel disease, right or left bundle branch block, hypertrophic or dilated cardiomyopathy, and significant arrhythmias including atrial fibrillation and ventricular tachycardia.
3.1. Study protocol
Patients were divided into 4 groups according to their ECG on admission: The anterior STEMI without RSTD; The anterior STEMI with RSTD; Inferior STEMI with RSTD in the anterior lead; Inferior STEMI without RSTD in the anterior lead.
The number of each group and the characteristics of the ST segment changes were summarized.
4. Results
A total of 85 patients were included, of which 75 were patients with RSTD (10 patients with anterior myocardial infarction had no RSTD), all 45 patients with inferior myocardial infarction had limb leads RSTD, and 37 of them had anterior lead ST segment depression (Right coronary artery occlusion was found in 28 cases and circumflex artery occlusion in 9 cases).
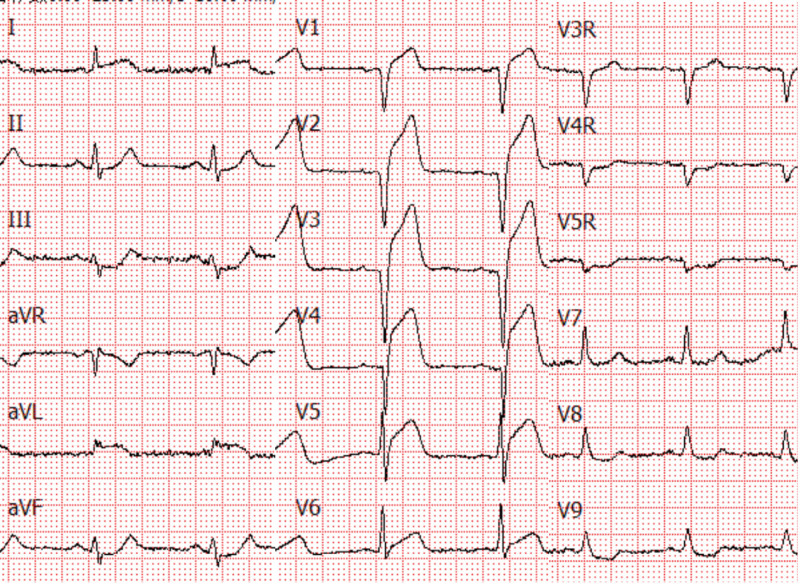
Thirty patients with anterior myocardial infarction were accompanied by mild ST segment changes in the limb leads (ST segment depression ≤0.1 mV appeared in 25 patients and ST segment depression of 0.1–0.2 mV appeared in 5 patients). Twenty-five of the patients combined with inferior ST segment depression. The degree of ST segment depression in lead III was approximately equal to the degree of ST segment elevation in lead aVL. The degree of ST segment depression in lead aVF was about half of that in lead III, and there was no significant depression in lead II (Fig. 1). There were 5 cases of anterior myocardial infarction with ST segment elevation in inferior leads (<0.1 mV) and RSTD in aVR or aVL lead.
Figure 1.
Electrocardiogram of patients with anterolateral wall myocardial infarction.
All ECGs of inferior STEMI had aVL or aVR lead ST segment depression. In 34 cases, the degree of ST segment elevation of lead III was greater than that of lead II (right coronary artery occlusion was found in 27 cases and circumflex artery occlusion in 7 cases). The degree of ST segment depression of lead aVL was significantly greater than that of lead aVR. In 2 cases, the degree of ST segment elevation of lead II was greater than that of lead III (circumflex artery occlusion), and in 9 cases, the degree of ST segment elevation of lead II was similar to that of lead III (right coronary artery occlusion was found in 1 case and circumflex artery occlusion in 8 cases). The ST segment depression of lead aVL and lead aVR was also similar, which was about half of the elevations of the ST segment in lead III and lead II.
5. Discussion
The current view regarding RSTD is not accurate. Specifically, RSTD neither necessarily occurs on the opposite side of the infarct area nor does it occur only on the opposite side of the infarct area. In present study, we noted that RSTD can occur in any lead with the infarct area as the negative electrode.
The relationship between the magnitude of ST-segment elevation and RSTD is unclear.[3] We found for the first time that the degree of ST-segment depression in limb leads can be calculated from the degree of ST-segment elevation.
The negative electrode of the standard limb leads is a single limb electrode, whereas the negative electrode of the 3 aV limb leads is the average value of the 2 limb electrodes, and this must be calculated.[9]
When the AAP of 1 limb electrode decreased, the degree of ST segment depressions in the standard limb lead with the infarct area as the negative electrode were equal to the degree of ST segment elevation in the lead with the infarct area as the positive electrode, while the degree of ST segment depressions in the aV lead were only half of that in the standard limb lead. Figure 1 is an ECG of a patient with acute anterolateral wall STEMI, the ST segment of lead I elevated by 0.1 mV, indicated the AAP of left arm electrode reduced 0.1 mV (assessed from ECG), the left arm electrode is the negative electrode of lead III, half the negative electrode of the lead aVF, so the ST segment depressed 0.1 mV in lead III and 0.05 mV in the lead aVF.
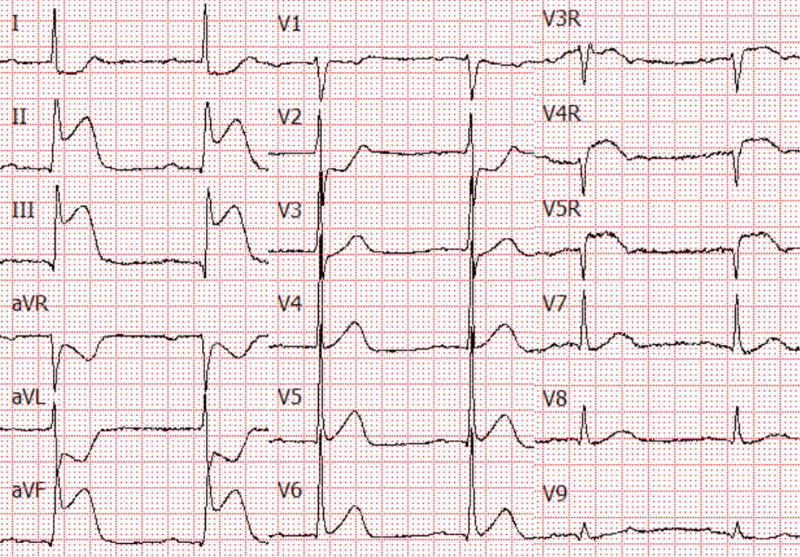
When 2 limb electrodes were affected by myocardial infarction, the electrode recording the normal myocardium should be determined first. Figure 2 shows an ECG of a patient with inferior myocardial infarction and right ventricular myocardial infarction, the normal myocardium was recorded by the left arm electrode. The ST segment of lead III elevated by 0.7 mV indicates that the leg electrode decreased by 0.7 mV. The ST segment of lead II elevated by 0.5 mV indicates that the AAP of the leg electrode was 0.5 mV less than that of the right arm electrode, so the AAP of the right arm electrode was 0.2 mV less than that of the left arm electrode. The negative electrode of aVL is the average value of the right arm and leg electrode, AAP decreased 0.45 mV [(0.7 mV + 0.2 mV)/2], and the ST segment decreased by 0.45 mV. The negative electrode of aVR is the average value of the left arm and leg electrode, AAP decreased 0.35 mV [(0 + 0.7 mV)/2], ST segment decreased by 0.15 mV (0.35–0.2 mV), and lead I decreased by 0.2 mV.
Figure 2.
Electrocardiogram of a patient with acute inferior wall ST segment elevation myocardial infarction and right ventricular myocardial infarction.
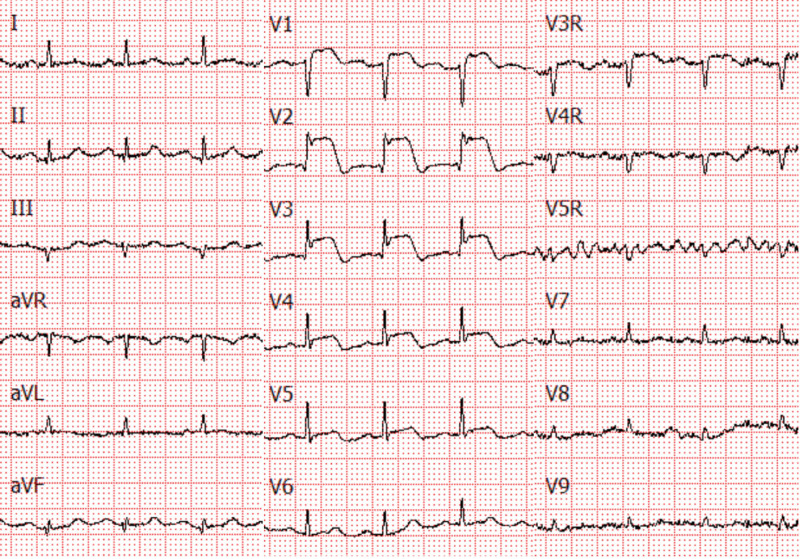
According to the current view, anterior wall myocardial infarction should have RSTD in the posterior wall,[3] but this is not the case (Fig. 3). This is because the negative electrode of all leads is in the limb leads, and part of the anterior wall myocardial infarction may not involve the limb leads. In this study, there were 10 patients with anterior myocardial infarction who showed no RSTD in any leads. There were 24 patients with anterior wall myocardial infarction combined with left lateral wall myocardial infarction and 5 patients with inferior wall myocardial infarction. The range of the inferior wall or left lateral wall myocardial infarction in patients with anterior wall myocardial infarction is generally small, with slight ST segment elevation in limb leads and most patients do not have RSTD in the posterior leads.
Figure 3.
Electrocardiogram of a patient with acute anterior ST segment elevation myocardial infarction.
Currently the depression in leads V1and V2 is considered the reciprocal of and similar in meaning to the ST-segment elevation in the V8 and V9.[3] However, depression in leads V1and V2 is also seen in right ventricular myocardial infarction.[10] The negative electrode of precordial leads is the Wilson’s Central Terminal, which is the average value of 3 limb electrodes. Myocardial infarcts with ST segment elevation in limb leads may cause RSTD in precordial leads. The depression in leads V1 and V2 is the RSTD of ST elevation in the inferior leads, not the posterior ventricular leads. The ST segment depression of V1 was rare in right ventricular myocardial infarction, because right ventricular AP recorded by V1 was decreased too, ST segment was mostly normal or elevated and only a few showed depression.
The reason for the absence of RSTD in the precordial leads in inferior infarction was that the precordial electrode was close to the infarct area and the AAP was also reduced. Another reason was that the AAP of the inferior myocardium was slightly weakened, which had no obvious effect on the potential of the negative electrode of the precordial lead. Among the 13 patients with inferior myocardial infarction without ST segment depression in the anterior leads, ST segment elevation in the inferior leads was 0.1 mV in 5 patients, 0.1 to 0.2 mV in 7 patients, and 0.4 mV in 1 patient (combined with extensive anterior wall ST segment elevation).
The negative electrode of the precordial lead is the average value of the 3 limb electrodes, and the potential of the 3 limb electrodes is inconsistent for the patient of inferior wall myocardial infarction. While placing the 3 limb electrodes in 1 place (limb), the precordial leads with a single limb as the negative electrode can be obtained. ST segment changes in the anterior chest lead can be used to analyze the mechanism of ST segment changes.
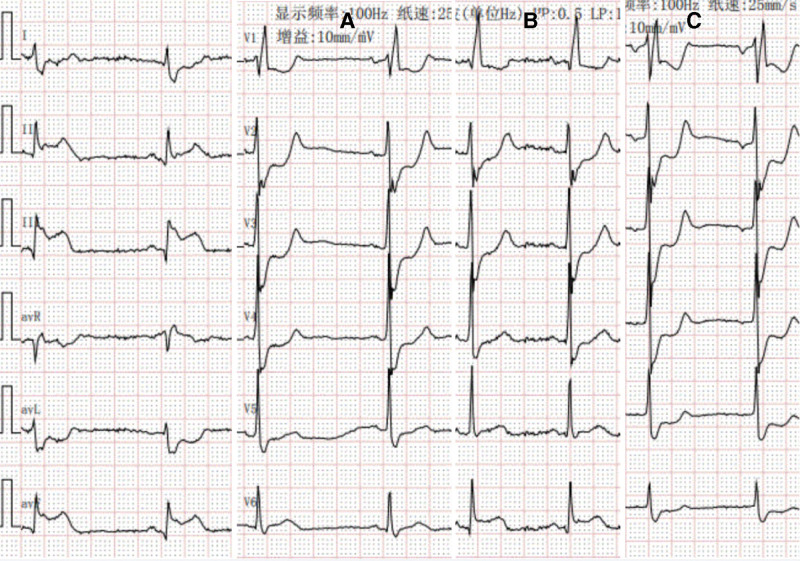
A patient with acute inferior wall myocardial infarction, 99% stenosis in the middle of the right coronary artery, and 60% stenosis in the middle of the anterior descending branch were studied to test our mechanism. It can be speculated from the ECG that the AAP of the leg electrode decreased significantly, the AAP of the right arm electrode decreased slightly, and the AAP of the left arm electrode was normal (Fig. 4).
Figure 4.
An electrocardiogram of a patient with acute inferior wall myocardial infarction. (A) Normal 12-lead electrocardiogram, electrocardiogram of chest leads with left arm (B), and leg (C) as the negative electrode.
The anterior leads with the left arm as the negative electrode are the actual situation. The depressed ST segment indicates that V2 and V3 are the ischemic areas (ischemia via collateral circulation diverting blood to the infarcted region). The elevated ST segment means that V6 is an infarct area (Fig. 4B).
The ST segment depression in the anterior leads was considered RSTD in the Standard 12-lead ECG (Fig. 4A). In addition, the ST segment in V6 is normal because the AAP in the positive and negative electrodes decreased similarly. When the leg is the negative electrode, the AAP in the negative electrode declines more than that of the positive electrode, so the ST segment of V6 is depressed (Fig. 4C).
The ST-segment change in lead V6 indicates that when the AAP of the negative electrode is smaller than that of the positive electrode, the ST-segment decreases. When the AAP of the positive electrode is smaller than that of the negative electrode, the ST-segment elevates. This is consistent with our proposed mechanism.
The link between RSTD and clinical outcomes has been extensively studied since long, and majority of the previous research suggests that RSTD is associated with clinical prognosis.[11–15] ST segment depression occurs in some patients due to multivessel lesions, and the prognosis of these patients is poor. However, even in patients without multivessel disease, RSTD may be associated with poor prognosis. RSTD is related to the degree of ST segment elevation – the more the ST segment elevation in limb leads, the greater the risk of ST segment depression in chest leads. Furthermore, the degree of RSTD between limb leads is directly related to the degree of ST segment elevation in the infarct area.
6. Limitations
It is difficult to obtain patients’ local myocardial AP in AMI patients. Thus, we can only speculate about the mechanism in terms of the characteristics of ST segment change, but the mechanism we have proposed completely conforms to the characteristics of ST segment change, making it the most reasonable and scientific mechanism so far.
In summary, the mechanism of RSTD in acute myocardial infarction may be that the AP of the negative electrode of the lead weakens or disappears and the AP of the positive electrode may not be completely offset, resulting in ST-segment depression. Animal experimental studies are needed for further confirmation.
Author contributions
The study was designed by QG and BY, FB collected the ECG, QG drafted the manuscript, YH contributed to critical revision.
Conceptualization: Yingfu Hu.
Data curation: Fangfang Bie.
Methodology: Fangfang Bie, Yingfu Hu, Bo Yang.
Project administration: Fangfang Bie, Yingfu Hu.
Software: Fangfang Bie.
Supervision: Qijun Gao, Yafeng Chen, Bo Yang.
Visualization: Yafeng Chen.
Writing – original draft: Qijun Gao.
Writing – review & editing: Qijun Gao, Bo Yang.
Abbreviations:
- AAP =
- amplitude of the action potential
- AP =
- action potential
- ECG =
- electrocardiogram
- RSTD =
- reciprocal ST-segment depression
- STEMI =
- ST segment elevation myocardial infarction
The authors have no funding and conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
How to cite this article: Gao Q, Bie F, Hu Y, Chen Y, Yang B. Characteristics and mechanism of reciprocal ST-segment depression in acute ST segment elevation myocardial infarction: Reciprocal ST-segment depression and ST segment elevation myocardial infarction. Medicine 2022;101:44(e31238).
Contributor Information
Qijun Gao, Email: smartgao2008@sina.com.
Yingfu Hu, Email: 1156599741@qq.com.
Yafeng Chen, Email: yafenchen2020@sina.com.
Bo Yang, Email: yangbo201504@sina.com.
References
- [1].Radwan HI, Ahmed AAE, Ammar AS, et al. Relation of collateral circulation with reciprocal changes in patients with acute ST-elevation myocardial infarction. J Electrocardiol. 2020;60:36–43. [DOI] [PubMed] [Google Scholar]
- [2].Vaidya GN, Antoine S, Imam SH, et al. Reciprocal ST-segment changes in myocardial infarction: ischemia at distance versus mirror reflection of ST-elevation. Am J Med Sci. 2018;355:162–7. [DOI] [PubMed] [Google Scholar]
- [3].Rautaharju PM, Surawicz B, Gettes LS, et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part IV: the ST segment, T and U waves, and the QT interval: a scientific statement from the American heart association electrocardiography and arrhythmias committee, council on clinical cardiology; the American college of cardiology foundation; and the heart rhythm society. Endorsed by the international society for computerized electrocardiology. J Am Coll Cardiol. 2009;53:982–91. [DOI] [PubMed] [Google Scholar]
- [4].Birnbaum Y, Wagner GS, Barbash GI, et al. Correlation of angiographic findings and right (V1 to V3) versus left (V4 to V6) precordial ST-segment depression in inferior wall acute myocardial infarction. Am J Cardiol. 1999;83:143–8. [DOI] [PubMed] [Google Scholar]
- [5].Bayés de Luna A, ed. Ischemia and Necrosis in Clinical Electrocardiography. 4th ed. Chichester, UK: Wiley-Blackwell Publishing; 2012. 216–270. [Google Scholar]
- [6].Bayés de Luna A, Goldwasser D, Fiol M, et al. Surface electrocardiography. In: Fuster V, Harrington RA, Narula J, et al. eds. Hurst’s The Heart. McGrawHill; 2017:14e-. [Google Scholar]
- [7].Tse G, Wong ST, Tse V, et al. Monophasic action potential recordings: which is the recording electrode? J Basic Clin Physiol Pharmacol. 2016;27:457–62. [DOI] [PubMed] [Google Scholar]
- [8].Thygesen K, Alpert JS, Jaffe AS, et al. Executive group on behalf of the joint European society of cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) task force for the universal definition of myocardial infarction. Fourth universal definition of myocardial infarction (2018). J Am Coll Cardiol. 2018;72:2231–64.30153967 [Google Scholar]
- [9].Tierala I, Nikus KC, Sclarovsky S, et al. Predicting the culprit artery in acute ST-elevation myocardial infarction and introducing a new algorithm to predict infarct-related artery in inferior ST-elevation myocardial infarction: correlation with coronary anatomy in the HAAMU Trial. J Electrocardiol. 2009;42:120–7. [DOI] [PubMed] [Google Scholar]
- [10].Peterson ED, Hathaway WR, Zabel KM, et al. Prognostic significance of precordial ST segment depression during inferior myocardial infarction in the thrombolytic era: results in 16,521 patients. J Am Coll Cardiol. 1996;28:305–12. [DOI] [PubMed] [Google Scholar]
- [11].Kidambi A, Mather AN, Uddin A, et al. Reciprocal ECG change in reperfused ST-elevation myocardial infarction is associated with myocardial salvage and area at risk assessed by cardiovascular magnetic resonance. Heart. 2013;99:1658–62. [DOI] [PubMed] [Google Scholar]
- [12].Chen TE, Lo PH, Li TC, et al. Prognostic significance of reciprocal ST-segment depression in patients with acute STEMI undergoing immediate invasive intervention. Am J Emerg Med. 2012;30:1865–71. [DOI] [PubMed] [Google Scholar]
- [13].Namdar H, Imani L, Ghaffari S, et al. ST-segment depression in left precordial leads in electrocardiogram of patients with acute inferior myocardial infarction undergoing primary percutaneous coronary intervention. Interv Med Appl Sci. 2018;10:191–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Birnbaum Y, Herz I, Sclarovsky S, et al. Prognostic significance of precordial ST segment depression on admission electrocardiogram in patients with inferior wall myocardial infarction. J Am Coll Cardiol. 1996;28:313–8. [DOI] [PubMed] [Google Scholar]
- [15].Yousif H, Lo E, Taha T, et al. The diagnostic significance of reciprocal ST segment depression in acute myocardial infarction. Q J Med. 1989;72:849–55. [PubMed] [Google Scholar]