OBJECTIVES:
Family presence on rounds involves allowing family members to participate in daily healthcare team rounds and is recommended by critical care professional societies. Yet, family presence on rounds is not performed in many institutions. There is a need to synthesize the current evidence base for this practice to inform healthcare providers of the potential benefits and challenges of this approach. The main objective of this study was to explore the impact of family presence on adult ICU rounds on family and healthcare providers.
DATA SOURCES:
Ovid Medline, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Cochrane Library, and PubMed databases were last searched on January 28, 2022. Studies published during the COVID-19 pandemic were included.
STUDY SELECTION:
Studies involving family presence during rounds that included family or healthcare provider perspectives or outcomes were selected. There were no limitations on study design.
DATA EXTRACTION:
Qualitative and quantitative family and provider perspectives, barriers and challenges to family presence, and study outcomes were extracted from studies. The JBI Manual for Evidence Synthesis published guidelines were followed.
DATA SYNTHESIS:
There were 16 studies included. Family reported family presence on rounds as a means of information transfer and an opportunity to ask care-related questions. Family presence on rounds was associated with increased family satisfaction with care, physician comfort, and improved physician-family relationship. Healthcare providers reported a positive perception of family presence on rounds but were concerned about patient confidentiality and perceived efficacy of rounds. Family presence was found to increase rounding time and was felt to negatively impact teaching and opportunities for academic discussions.
CONCLUSIONS:
Family presence on rounds has potential advantages for family and healthcare providers, but important challenges exist. Further studies are needed to understand how to best implement family presence on adult ICU rounds.
Keywords: critical care, family, professional-family relations, teaching rounds
KEY POINTS
Question: A scoping review of the literature was performed to synthesize both healthcare provider and family perspectives regarding family presence on rounds in critical care settings.
Findings: Numerous benefits are present, including improved family satisfaction with care and communication, decreased family anxiety, improved relationships between physicians and family, and increased physician comfort. Concerns were raised, including issues with consistency of care, communication of results, confidentiality, and academic value for healthcare providers in training.
Meaning: These findings represent an updated review of the literature, the last of which has been seen nearly one decade prior. These findings have implications for all healthcare professionals and for family members of critically ill patients.
Family presence on rounds is an approach to multidisciplinary care rounds that allows family members to be present and participate in information sharing and medical decision-making with the healthcare team (1). Critical care professional societies recommend family presence on rounds as a means to engage families in care (1). However, family presence on rounds has not been adopted in a widespread manner as the standard care approach in contemporary adult ICUs (2).
The lack of uptake of this guideline-recommend approach to care may be due to insufficient knowledge of the potential benefits of family presence on rounds for the patient, family member, and healthcare provider. Indeed, most of the literature on family presence on rounds is in the context of pediatric critical care (3, 4). There is therefore a need to synthesize and understand healthcare provider and family perspectives of family presence on adult ICU rounds. In particular, there is a need to explore the impact of family presence on rounds on the learning environment for trainees. Additionally, there may be healthcare provider and family concerns that could limit successful integration of family presence on rounds into routine care. Thus, there is a need to understand the potential barriers to implementing family presence in ICU rounds.
Family presence on ICU rounds may also improve family important outcomes post hospitalization. Hospitalization of a loved one in an ICU is associated with a high prevalence of psychologic symptoms, such as anxiety, depression, and posttraumatic stress, in family members (5). These symptoms often persist post hospitalization and have been termed “post-ICU syndrome-family” (6). Family presence on rounds may play a role in mitigating these symptoms in family members.
Thus, the objectives of this scoping review are 1) to explore family and healthcare provider perspectives on family presence on rounds in adult critical care; 2) to establish the impact of family presence on rounds on family, healthcare provider, and rounding outcomes; and 3) to identify barriers and challenges to implementation of family presence on adult ICU rounds. This synthesis of the current knowledge base can be used to understand the potential advantages and challenges to family presence on ICU rounds and encourage use of this important engagement practice.
MATERIALS AND METHODS
Search Strategy
The search strategy was devised in consultation with a medical research librarian. Relevant keywords were used to identify potential studies (Appendix 1, http://links.lww.com/CCX/B80); studies containing the terms “family presence,” “rounds,” and “ICU” either in the title, abstract, or body of the article were extracted. Papers were selected based upon the guidelines specified in the Joanna Briggs Institute Methodology for JBI Scoping Reviews (7) and without any cultural, ethnic, gender, or specific language restrictions. No date restrictions were placed on the search strategy. Studies from the COVID-19 pandemic were included.
“Family” was defined broadly and was considered anyone with a biological, legal, or emotional relationship with the patient whom the patient would like to be involved in care (8, 9). No restrictions were applied in the search methodology on the term “family.”
Information Sources
Sources of information included primary research studies, clinical trials, cross-sectional observational, ethnographic, and interventional studies. Letters to the editor, editorials, and review articles were not included.
Databases
The Ovid Medline, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Cochrane Library and PubMed databases were searched from inception to January 28, 2022.
Search and Selection of Sources of Evidence
The primary search results consisted of records related to “family presence on rounds” and “adult ICU.” Inclusion criteria were studies of family presence on rounds in an ICU with adult patients (age ≥ 18 yr) and including either: 1) family perspectives; 2) healthcare provider perspectives; 3) family, healthcare provider, or rounding outcomes (qualitative or quantitative); or 4) family or healthcare provider barriers and challenges to implementation of family presence on rounds. Studies that included both adult and PICUs were included, although only the findings from the adult ICU were extracted. Exclusion criteria were studies that were not relevant (i.e., did not include family presence on ICU rounds), focused solely on pediatric patients (age ≤ 17 yr) or contained insufficient data for analysis. There were no limitations on study design.
The records were compiled into EndNote X9 (Clarivate, United States). Deduplication was performed in EndnoteX9, and the results were exported into Microsoft Excel (Microsoft Corporation, United States). Nonrelevant references were then excluded. Abstracts were reviewed by two independent reviewers (A.C., M.J.G.) for eligibility, and disagreements were resolved through consensus.
Data Charting Process and Synthesis of Results
Extracted data included first author name, year of publication, country of origin, study type, study setting, time period, healthcare provider or family member involvement, provider perspectives, family perspectives, study outcomes, rounding styles, and barriers or challenges reported to family presence on ICU rounds. Perspectives from both family and providers were reported in the included studies either as survey results or thematic analysis of conducted interviews. Outcomes varied and were often reported as quantitative results. Reported barriers and challenges were mostly the result of interview analyses.
Both quantitative and qualitative information was extracted from each study. To extract the results, we created a database from included studies with unfiltered raw data only. The data were then categorized into four topic areas: 1) family perspectives; 2) healthcare provider perspectives; 3) family, healthcare provider, and rounding outcomes; and 4) barriers and challenges. We created tables using both the qualitative and quantitative data to compile the perspectives, outcomes, and barriers for both family and healthcare providers. The qualitative data were expressed as thematic data points from each study.
RESULTS
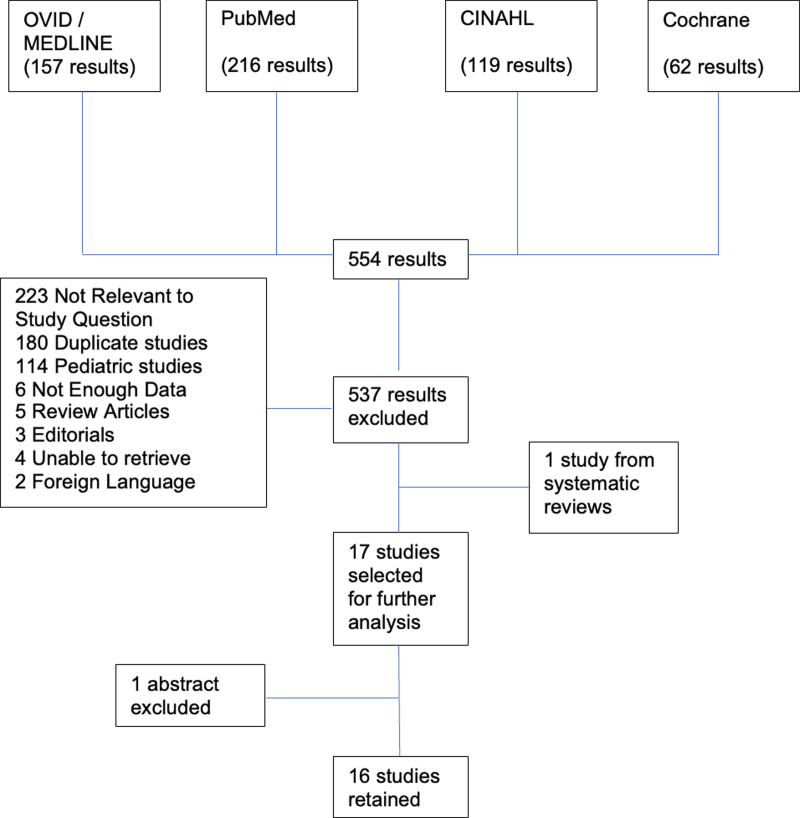
There were 16 studies included in the analysis (Fig. 1). The studies were published from 2003 to 2021. Studies were from the United States (n = 8) (10–17), Canada (n = 5) (18–22), Israel (n = 1) (23), Iran (n = 1) (24), and multiple countries (Canada and United States; n = 1) (25). Studies were qualitative descriptive studies (n = 8) (12–14, 17, 19, 21, 22, 25), cross-sectional surveys (n = 3) (16, 18, 20), and interventional studies (n = 5) (10, 11, 15, 23, 24).
Figure 1.
Scoping review methodology flow diagram. CINAHL = Cumulative Index to Nursing and Allied Health Literature.
Family Perspectives and Outcomes
Supplementary Table 1 (http://links.lww.com/CCX/B80) lists both family and healthcare provider perspectives on family participation in ICU rounds. Family members reported that their participation in rounds was very positive. Families perceived their presence on rounds as a means of transferring information as well as an opportunity to ask questions about their loved ones’ care (12, 17, 19, 21, 25). They were motivated to attend rounds and perceived their presence on rounds as a means to convey respect. Family participation increased their confidence in the care team and decreased their anxiety (12, 17, 21, 24, 25). Interventional studies found that family presence on rounds resulted in increased family satisfaction with care (11, 15, 17, 24).
Healthcare Provider Perspectives and Outcomes
Physicians overall expressed a positive attitude toward family presence at rounds (Supplementary Table 1, http://links.lww.com/CCX/B80). However, interruptions during daily rounds were associated with the perception of a decrease in rounding quality and an increase in possible improvement. These issues were not brought up in timely rounds. Several studies found that healthcare providers believed family presence on rounds would increase rounding time (11, 18, 22, 23).
Physicians felt that family presence on rounds increased physician comfort, improved the physician-family relationship, and was an overall positive experience (Table 1) (14, 16, 18, 21–23). Critical care nurses were also generally positive toward family presence on rounds. However, some nurses reported that family presence on rounds was disruptive and that it should be reserved for properly selected families (22).
Only one study reported the perspectives of medical trainees (13). Residents felt that having family members present during rounds was an opportunity to educate patients and family about the care plan, while also being able to provide updates.
Rounding Structure and Outcomes
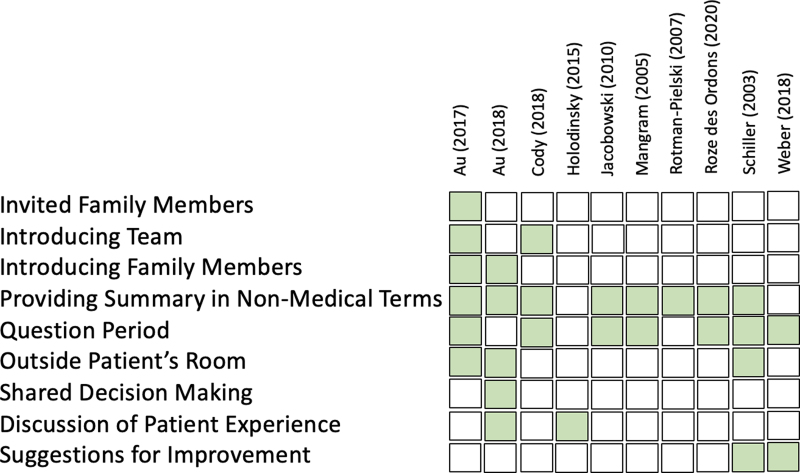
Different aspects of the rounding structure were explored (Fig. 2). Family presence in rounds involved inviting family members, introducing the team and family members, providing a summary in nonmedical terms, and a question period. Other key elements of the family presence in rounds that have been studied include shared decision-making, discussing the patient experience, and suggestions for improvement.
Figure 2.
Rounding styles. Summative diagram explaining the rounding style used by healthcare professionals across different studies. Boxes are marked in green when the study reported it in its methodology. The most widely used elements across all studies were providing the family with a summary in nonmedical terms and allowing for a question period (usually at the end of rounds).
Family presence on rounds was associated with the perception of increased rounding time (Table 1) (11, 22). Round length was measured in one study and was found to have increased by 3.5 minutes (rounding time from 5.5 to 9 min) per patient when the family was included in rounds (11). Whereas one study reported reduced teaching during rounds when family was present (22), other studies reported that family presence on rounds did not change the proportion of rounds with bedside teaching, the nature of the teaching, or the quality of the rounds (16, 19).
TABLE 1.
Family Participation in Rounding in the ICU and Outcomes
| Healthcare Provider | Family | Round Structure and Experience |
|---|---|---|
| ↑ Physician comfort (Ingram et al [16]) | ↓ Family anxiety (Jaberi et al [24]) | ↔ Proportion of rounds with bedside teaching (Au et al [19]) |
| ↑ Positive perception of family-centered rounding (Ingram et al [16]; Rotman-Pielski et al [23]) | ↔ Family satisfaction (Weber et al [10]) | ↔ Nature of teaching (Au et al [19]; Ingram et al [16]) |
| ↑ Physician-family relationship (Mangram et al [14]) | ↑ Family satisfaction (Jaberi et al [24]; Cody et al [17], Jacobowski et al [15];Simon et al [11]) | ↔ Quality of rounds (Au et al [19]) |
| ↑ Family communication (Jacobowski et al [15]; Mangram et al [14]; Simon et al [11]) | ↔ Efficiency of rounds (Ingram et al [16]) | |
| ↑ Quality of rounds (Jaberi et al [24]) | ||
| ↑ Rounding time (Santiago et al [22]; Simon et al [11]) | ||
| ↓ Teaching on rounds (Santiago et al [22]) |
↓ = decreased, ↑ = increased, ↔ = unchanged.
Perceived Barriers and Challenges
The barriers and challenges observed by healthcare providers and family members are reported in Supplementary Table 2 (http://links.lww.com/CCX/B80). The main concern raised by healthcare providers regarding the presence of families during rounds was its impact on teaching and academic discussions (13, 21, 22). Residents felt that family presence on rounds resulted in the needs of family being placed above their own and prevented them from receiving formal feedback opportunities (13). The possible breach in patient confidentiality and the fact that family members may have been inadvertently invited to rounds without being the appropriate representative are other concerns that were highlighted by the medical team (19, 21).
Family members reported a lack of consistency between attending staff and treating teams and felt that their experience being present during rounds depended greatly on which attending physician was conducting them (12, 14, 17, 20, 21, 25). There were also inconsistencies in practice observed by family members, such as ICU visiting policies that were arbitrarily followed. Another major concern was the quantity of disruptions occurring during rounds which resulted from frequent paging and phone calls (20).
Families were sometimes not invited to rounds or did not receive a formal introduction (21). Occasionally, comments made by ICU team members were found to be offensive (19). Test results or sensitive information was sometimes disclosed without warning or context (19, 21). In one study, family members reported that their contributions to discussion of patient care were meaningless and did not change the outcome (25).
DISCUSSION
The purpose of this scoping review was to understand the current evidence for family and healthcare provider perspectives, as well as outcomes for family presence on ICU rounds. The review identified that family members reported generally positive experiences and had increased satisfaction and reduced anxiety. Healthcare providers similarly had positive experiences with family presence on rounds but were concerned about the additional time required and patient confidentiality. Family presence on rounds appeared to increase rounding duration.
Prior reviews on the impact of family presence on ICU rounds are nearly a decade old and included PICUs in the analysis (26, 27). In addition, there is a relative paucity of evidence for family presence in adult ICUs compared with the PICU setting. Our review included the newer studies that have emerged since these prior publications.
Family involvement in ICU rounds was found to be generally positive. Increased interactions with the multidisciplinary team were found to decrease anxiety, while improving both communication and satisfaction with care. We identified three interventional studies that examined family presence on ICU rounds in adult settings (10, 11, 24). Two studies examined differences in family satisfaction between an intervention group with family present and a control group without family members present during morning rounds (11, 24). Both of these studies reported that family presence led to increased family satisfaction. The interventional study by Weber et al (10) explored the impact of adding two supplementary afternoon dedicated family rounds per week in addition to morning rounds. This study found no change in family satisfaction. Overall, our findings suggest that family presence on morning ICU rounds has a positive outcome on family satisfaction with care. This is consistent with results that have been published in pediatric settings (28–30).
A lack of consistency between different staff physicians and communication issues was a concern to many family members. It appears that some family members are bothered by unpredictability (17, 21) as well as variable rounding styles depending on which physician is conducting them (14, 20, 25). This problem could be addressed with implementation of standardized rounding structure and guidelines for attendings and reinforcement of strict adherence to rounding at the same time every day. This may be challenging to implement given the busy daily routine and frequent interruptions (i.e., calls and pages) in an ICU environment (20). Efforts should be made to reduce these interruptions as much as possible. Redirection of calls and pages to the next person in the chain of command, notably the intensive care fellow or a physician assistant, might help mitigate this issue.
The effect of family presence on healthcare providers was also generally positive. Several studies reported improved relationships between physicians and family members, increased physician comfort, and enhanced positive perceptions of family-centered rounding, as a whole. Previous studies in pediatric settings have also reported similar conclusions, although trainees and nurses were reported to feel less positive toward family involvement (30, 31). One study included in this review also reported that nurses had negative experiences interacting with certain families and suggested that only families that are respectful and reasonable should be selected to participate in rounds (22).
Most concerns from a healthcare provider perspective arose from the educational value and efficiency of having family members present on rounds. There are numerous reports of family presence constraining the academic discussion of patients on rounds (13, 21, 22). Furthermore, in one study conducted by Rabinowitz et al (13), residents believed that the needs of certain families superseded their own, resulting in limited feedback opportunities (21). Of note, only limited evidence exists for the impact of family presence on ICU rounds on medical trainees in adult settings. This same study represents the only one identified by our review that focused on the resident perspective of family presence in rounds (13). Residents represent a valuable part of the healthcare network and are usually in contact with families for extended periods of time. It would thus be of interest for future studies to explore trainees’ perspectives.
The interventional study by Simon et al (11) also demonstrated that rounding time is significantly increased by an average of 4 minutes in groups where family is present on rounds. This could result in significant prolongation of rounds in centers where large numbers of patients are seen in a single day, which could decrease rounding efficiency. These results are contrary to the conclusions communicated in a previous review by Davidson et al (27) which suggested that there was no concrete evidence of rounding prolongation and decreased teaching. Considering the small quantity of high-quality studies, this point deserves further study in future interventional studies. Implementation of a dedicated academic discussion for every patient would be able to subvert this shortcoming but risks prolonging rounds further. It would thus be of value to study different approaches with family presence on rounds that would be able to address all of these issues without compromising the needs of healthcare providers over family members or vice-versa.
Concerns and barriers related to communication, disclosure of information, the training environment, and the impact on rounding are likely similar in many respects between the PICU and adult ICU settings. However, important differences exist between family members in the adult ICU compared with the PICU or neonatal ICU context, including family participant age, relationship, and role. Family members are much older in the adult ICU; the mean age of family member participants was 30 years old in one neonatal ICU study (32) compared with 52 years old in an adult ICU study (33). In the neonatal/PICU, family are almost exclusively parents or surrogates, whereas in the adult ICU, the most prevalent relationships are adult child, spouses/partners, and siblings (32, 33). In addition, the family role also differs considerably between the settings (i.e., breastfeeding/lactation vs support during procedures, delirium reorientation).
We did not identify any studies that explored virtual family presence in adult ICU rounds using videoconferencing technology. In the neonatal ICU/PICU setting, videoconferencing was found to be a feasible solution to conduct multidisciplinary rounds, and participants found it effective without interfering with normal workflow (32). There is a great need for studies to be conducted in the adult ICU setting exploring the role of virtual family presence on ICU rounds.
The family member’s relationship to the patient may impact the rounding process and family outcomes. For example, spousal relationship is associated with a higher burden of depressive and anxiety symptoms in family members of ICU patients both during and after their loved one’s ICU stay (34, 35). However, despite our broad search criteria, we did not identify any studies that explored how different family-patient relationships may impact family presence on rounds. There is a need for studies looking at how relationships impact family presence on ICU rounds (36).
Our findings have implications for future research efforts in this field. There are a paucity of high-quality randomized trials investigating the impact of family rounds on patient, family, provider, and healthcare system. Understanding the potential positive and negative impacts of including family in ICU rounds can help determine the net benefit and whether this guideline-recommended practice is warranted. Family participation in ICU rounds may also be beneficial for certain family and/or healthcare settings, but not for others. Thus, there is a need for further studies to define family participant characteristics that may particularly benefit from this approach—as well as those who may not. There are also a lack of studies about whether family rounds in adult subspecialty ICUs (i.e., cardiovascular, neurosurgery, or trauma ICUs) differ compared with the general medical or surgical ICUs. Each of these settings may have different patient characteristics, decision-making implications, and team dynamics. There is also a strong need for additional studies to explore resident perspectives and attitudes toward family participation in ICU rounds.
Systemic and individual barriers may hinder family participation in ICU rounds (37). Health system–related barriers include visitor restrictions, concerns related to infection control, and lack of healthcare provider knowledge about the potential benefits of family presence during ICU rounds. Indeed, an international survey of 345 ICUs from 40 countries found that only 43% of ICUs allowed family presence on rounds (2). Family-related barriers include distance, caretaker role, family member illness, lack of access to reliable transportation, weather conditions, inability to miss work, time, and risks to themselves. Further work is needed to develop implementation strategies to increase uptake of family presence on adult ICU rounds.
The 2017 society guidelines for family-centered care in the neonatal ICU, PICU, and adult ICU recommend that family be offered the option of participating in rounds as a means to improve family engagement and satisfaction, albeit with low quality of supporting evidence. New evidence has emerged since this publication, including data from this review, that may increase the strength of this recommendation (1). New evidence has emerged since this publication, including data from this review, that may increase the strength of a future recommendation.
There are limitations to our study. First, the strength of our conclusion is limited by the availability of studies in the published literature. Second, although our search strategy was broad and designed for maximum sensitivity, it was not exhaustive. Thus, it is possible that there are quantitative and qualitative research studies that were not included in the analysis. Third, there are a lack of studies from non-Western countries, which differ in terms of cultural interactions between providers and families. Therefore, the generalizability of this study’s conclusions may be limited to mostly Western countries. Finally, the COVID-19 pandemic severely restricted families’ ability to be involved in the care of their loved ones. Indeed, many were unable to be present in decision-making due to ICU visiting policy restrictions. Most of the studies included in this review do not comment on this era in healthcare nor consider the impact of the pandemic on current ICU rounding practices worldwide. Studies in the pediatric setting have addressed family presence on rounds with the use of videoconferencing technology, which could be useful during periods of visitation restriction.
CONCLUSIONS
Family presence on rounds represents a rounding style that has numerous benefits for both healthcare providers and family members. However, there are concerns regarding consistency, communication, confidentiality, and academic value that should be addressed in order to improve the interactions of all parties involved. Further research in the form of pilot studies aimed at refining current family rounding practices, as well as implement new practices that address the above-mentioned issues, is required. Once these initial steps have been completed, there will be a need for a large, multicenter interventional trial to definitively evaluate all aspects examined in these mainly cross-sectional observational studies.
Supplementary Material
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccejournal).
Dr. Goldfarb was supported by a Clinical Research Scholars Award from Fonds de Recherche du Québec Santé. The remaining authors have no financial disclosures or conflicts of interest to report.
REFERENCES
- 1.Davidson JE, Aslakson RA, Long AC, et al. : Guidelines for family-centered care in the neonatal, pediatric, and adult ICU. Crit Care Med 2017; 45:103–128 [DOI] [PubMed] [Google Scholar]
- 2.Kleinpell R, Heyland DK, Lipman J, et al. : Patient and family engagement in the ICU: Report from the task force of the world federation of societies of intensive and critical care medicine. J Crit Care 2018; 48:251–256 [DOI] [PubMed] [Google Scholar]
- 3.Fernandes AK, Wilson S, Nalin AP, et al. : Pediatric family-centered rounds and humanism: A systematic review and qualitative meta-analysis. Hosp Pediatr 2021; 11:636–649 [DOI] [PubMed] [Google Scholar]
- 4.Foster M, Whitehead L, Maybee P: The parents’, hospitalized child’s, and health care providers’ perceptions and experiences of family-centered care within a pediatric critical care setting: A synthesis of quantitative research. J Fam Nurs 2016; 22:6–73 [DOI] [PubMed] [Google Scholar]
- 5.Anderson WG, Arnold RM, Angus DC, et al. : Posttraumatic stress and complicated grief in family members of patients in the intensive care unit. J Gen Intern Med 2008; 23:1871–1876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Davidson JE, Jones C, Bienvenu OJ: Family response to critical illness: Postintensive care syndrome-family. Crit Care Med 2012; 40:618–624 [DOI] [PubMed] [Google Scholar]
- 7.Peters MD, Godfrey CM, Khalil H, et al. : Guidance for conducting systematic scoping reviews. Int J Evidence-Based Healthcare 2015; 13:141–146 [DOI] [PubMed] [Google Scholar]
- 8.Cené CW, Johnson BH, Wells N, et al. : A narrative review of patient and family engagement: The “foundation” of the medical “home.”. Med Care 2016; 54:697–705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brown SM, Rozenblum R, Aboumatar H, et al. : Defining patient and family engagement in the intensive care unit. Am J Respir Crit Care Med 2015; 191:358–360 [DOI] [PubMed] [Google Scholar]
- 10.Weber U, Johnson J, Anderson N, et al. : Dedicated afternoon rounds for ICU patients’ families and family satisfaction with care. Crit Care Med 2018; 46:602–611 [DOI] [PubMed] [Google Scholar]
- 11.Simon K, Sankara IR, Gioe C, et al. : Including family members in rounds to improve communication in intensive care. J Nurs Care Qual 2021; 36:25–31 [DOI] [PubMed] [Google Scholar]
- 12.Schiller WR, Anderson BF: Family as a member of the trauma rounds: A strategy for maximized communication. J Trauma Nurs 2003; 10:93–101 [DOI] [PubMed] [Google Scholar]
- 13.Rabinowitz R, Farnan J, Hulland O, et al. : Rounds today: A qualitative study of internal medicine and pediatrics resident perceptions. J Grad Med Educ 2016; 8:523–531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mangram AJ, McCauley T, Villarreal D, et al. : Families’ perception of the value of timed daily “family rounds” in a trauma ICU. Am Surg 2005; 71:886–891 [PubMed] [Google Scholar]
- 15.Jacobowski NL, Girard TD, Mulder JA, et al. : Communication in critical care: Family rounds in the intensive care unit. Am J Crit Care 2010; 19:421–430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ingram TC, Kamat P, Coopersmith CM, et al. : Intensivist perceptions of family-centered rounds and its impact on physician comfort, staff involvement, teaching, and efficiency. J Crit Care 2014; 29:915–918 [DOI] [PubMed] [Google Scholar]
- 17.Cody SE, Sullivan-Bolyai S, Reid-Ponte P: Making a connection: Family experiences with bedside rounds in the intensive care unit. Crit Care Nurse 2018; 38:1816–1826 [DOI] [PubMed] [Google Scholar]
- 18.Au SS, Roze des Ordons A, Soo A, et al. : Family participation in intensive care unit rounds: Comparing family and provider perspectives. J Crit Care 2017; 38:132–136 [DOI] [PubMed] [Google Scholar]
- 19.Au SS, Roze des Ordons AL, Parsons Leigh J, et al. : A multicenter observational study of family participation in ICU rounds. Crit Care Med 2018; 46:1255–1262 [DOI] [PubMed] [Google Scholar]
- 20.Holodinsky JK, Hebert MA, Zygun DA, et al. : A survey of rounding practices in Canadian adult intensive care units. PLoS One 2015; 10:e0145408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roze des Ordons AL, Au S, Blades K, et al. : Family participation in ICU rounds—Working toward improvement. J Eval Clin Pract 2020; 26:1620–1628 [DOI] [PubMed] [Google Scholar]
- 22.Santiago C, Lazar L, Jiang D, et al. : A survey of the attitudes and perceptions of multidisciplinary team members towards family presence at bedside rounds in the intensive care unit. Intensive Crit Care Nurs 2014; 30:13–21 [DOI] [PubMed] [Google Scholar]
- 23.Rotman-Pikielny P, Rabin B, Amoyal S, et al. : Participation of family members in ward rounds: Attitude of medical staff, patients and relatives. Patient Educ Couns 2007; 65:166–170 [DOI] [PubMed] [Google Scholar]
- 24.Jaberi AA, Zamani F, Nadimi AE, et al. : Effect of family presence during teaching rounds on patient’s anxiety and satisfaction in cardiac intensive care unit: A double-blind randomized controlled trial. J Educ Health Promot 2020; 9:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reeves S, McMillan SE, Kachan N, et al. : Interprofessional collaboration and family member involvement in intensive care units: Emerging themes from a multi-sited ethnography. J Interprof Care 2015; 29:230–237 [DOI] [PubMed] [Google Scholar]
- 26.Cypress BS: Family presence on rounds. Dimens Crit Care Nurs 2012; 31:53–64 [DOI] [PubMed] [Google Scholar]
- 27.Davidson JE: Family presence on rounds in neonatal, pediatric, and adult intensive care units. Ann Am Thorac Soc 2013; 10:152–156 [DOI] [PubMed] [Google Scholar]
- 28.Aronson PL, Yau J, Helfaer MA, et al. : Impact of family presence during pediatric intensive care unit rounds on the family and medical team. Pediatrics 2009; 124:1119–1125 [DOI] [PubMed] [Google Scholar]
- 29.Cameron MA, Schleien CL, Morris MC: Parental presence on pediatric intensive care unit rounds. J Pediatr 2009; 155:522–528 [DOI] [PubMed] [Google Scholar]
- 30.Lopez M, Vaks Y, Wilson M, et al. : Impacting satisfaction, learning, and efficiency through structured interdisciplinary rounding in a pediatric intensive care unit: A quality improvement project. Pediatr Qual Saf 2019; 4:e176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Levin AB, Fisher KR, Cato KD, et al. : An evaluation of family-centered rounds in the PICU: Room for improvement suggested by families and providers. Pediatr Crit Care Med: 2015; 16:801–807 [DOI] [PubMed] [Google Scholar]
- 32.Rosenthal JL, Sauers-Ford HS, Williams J, et al. : Virtual family-centered rounds in the neonatal intensive care unit: A randomized controlled pilot trial. Acad Pediatr 2021; 21:1244–1252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Goldfarb M, Debigaré S, Foster N, et al. : Development of a family engagement measure for the intensive care unit. CJC Open 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Alfheim HB, Rosseland LA, Hofsø K, et al. : Multiple symptoms in family caregivers of intensive care unit patients. J Pain Symptom Manage 2018; 55:387–394 [DOI] [PubMed] [Google Scholar]
- 35.Johnson CC, Suchyta MR, Darowski ES, et al. : Psychological sequelae in family caregivers of critically III intensive care unit patients. A systematic review. Ann Am Thorac Soc 2019; 16:894–909 [DOI] [PubMed] [Google Scholar]
- 36.Olding M, McMillan SE, Reeves S, et al. : Patient and family involvement in adult critical and intensive care settings: A scoping review. Health Expect 2016; 19:1183–1202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Davidson JE, Savidan KA, Barker N, et al. : Using evidence to overcome obstacles to family presence. Crit Care Nurs Q 2014; 37:407–421 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.