Dear Editor,
Monkeypox virus (MPXV) is a zoonotic Orthopoxvirus, belonging to the Poxviridae family, first isolated in humans in 1970 in a Congolese child who was initially suspected of having smallpox [1].
Classically, clinical presentation of MPXV infection is similar to that of smallpox but generally less severe with lower complications and case fatality rate [2].
After a prodromal phase with fever, malaise, myalgias, headache and swollen lymph nodes, a characteristic vesiculo-pustular mucocutaneous rash appears on the face and distal extremities, with possible centrifugal progression to the rest of the body. The total number of lesions may vary from a few to thousands [3].
During the emerging MPXV outbreak in multiple non-endemic countries in North America and Europe commenced in May 2022, most cases were reported in men who have sex with men (MSM) with risky sexual behaviour, suggesting that close contact through sexual intercourse could be a route of transmission [4].
In the current outbreak, clinical presentation of MPXV cases has often been atypical, with the rash concentrated in the genital, perianal and oral areas, and a relative mildness or absence of prodromal symptoms [5]. In a preliminary evaluation, these cases could be mistaken for other conditions such as syphilis, lymphogranuloma venereum, molluscum contagiosum, Herpes simplex virus infection and bacterial tonsillitis [6,7].
Herein, we report two cases of human MPXV infection characterized by atypical oropharyngeal involvement, representing a diagnostic challenge. Both patients were living with Human Immunodeficiency virus (HIV), currently under Highly Active Antiretroviral Therapy, with undetectable viral load and good immunological status. Both of them presented to the Sexually Transmitted Diseases Centre of Florence, complaining of the recent appearance of some painful oral ulcerative lesions. Both had a history of syphilis; patient 1 also reported having been treated for gonorrhoea in the past, while patient 2 reported a previous hepatitis C which became negative after treatment. Epidemiological, clinical and laboratory data are summarized in Table 1 .
Table 1.
Epidemiological, clinical and laboratory data of two cases of MPXV with atypical oral presentation.
| Patient | 1 | 2 |
|---|---|---|
| Citizenship | Norwegian | Italian |
| Age | 45 | 69 |
| Sexual Behaviour | MSM | MSM |
| HIV status | Positive | Positive |
| Travel abroad | No | Yes |
| Unprotected oral sex in the previous weeks | Yes | Yes |
| Vaccination for smallpox | No | Yes |
| Previous STD | Syphilis, gonorrhoea | Syphilis, hepatitis C |
| Affected body sites | Oral mucosa, trunk | Oral mucosa, nipple |
| Number of lesions | 2 oral lesions and papular rash on the trunk | 1 oral lesion and 1 nipple lesion |
| Systemic symptoms | Fever, malaise, sore throat and painful cervical lymphadenopathy | Slight sore throat and slightly painful cervical lymphadenopathy |
| MPXV DNA PCR | Positive | Positive |
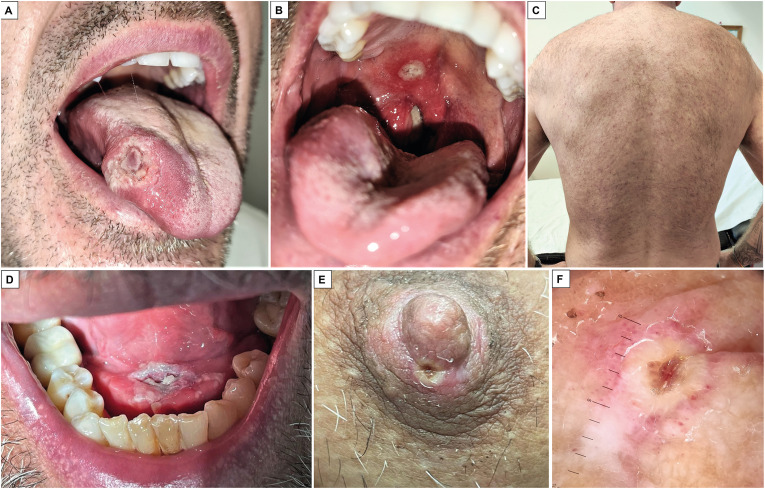
Patient 1 was a 45-year-old Norwegian man with a 9-day history of two painful oral ulcers, soon followed by the development of fever, malaise, sore throat and painful cervical swelling. Physical examination revealed a large, firm, non-tender, ulcerated nodule on the right lateral border of his tongue and a smaller erosive lesion in his hard palate, with surrounding erythema (Fig. 1 A, Fig. 1B). The right tonsil appeared enlarged and partially covered by white-greyish fibrinous exudate, with a slight deviation of the uvula. The patient reported dysphagia, with swallowing and speaking difficulties. A tender, painful right cervical lymphadenopathy was also appreciated on palpation. At the visit, the fever had already resolved and the other systemic symptoms were progressively improving. The patient had no genital or perianal lesions, but a non-pruriginous, papular rash was observed on his trunk (Fig. 1C).
Fig. 1.
Large and ulcerated nodule on the right lateral border of the tongue (A), erosive lesion in the hard palate deviating the uvula (B) and non-pruriginous, papular rash on the trunk of patient 1 (C). Ulcerative lesion on the mouth floor (D) and umbilicated pustular lesion on the right nipple of patient 2 (E). Dermoscopy of the right nipple lesion of patient 2 (F).
Patient 2 was a 69-year-old Italian man with a single painful ulcerative lesion that appeared on the floor of his mouth seven days before (Fig. 1D). Furthermore, physical examination revealed a tender, slightly painful, bilateral cervical lymphadenopathy and a single, asymptomatic, umbilicated pustular lesion on the right nipple (Fig. 1E). Dermoscopy of the nipple lesion showed a whitish structureless area, with a brownish central depression and peripheral erythema [7] (Fig. 1F).
Patient 2 denied fever and other systemic symptoms, except for a slight sore throat in spontaneous improvement.
Patient 1 denied travelling abroad in the previous six months but reported having unprotected oral sex with a German man two weeks earlier. Patient 2 reported a recent trip to the Canary Islands in July and risky oral intercourse about ten days before the onset of the oral lesion.
Serology for syphilis resulted repeatedly negative in both patients, except for TPHA attributable to the serological scar of the previous infection. Swabs obtained from the oral lesions and the oro-pharynx tested negative for Herpes simplex virus, Neisseria gonorrhoeae and Chlamydia trachomatis but positive for MPXV on qualitative real-time polymerase-chain-reaction. In patient 2, an additional swab from the nipple lesion resulted positive for MPXV DNA. Interestingly, only patient 2 had been vaccinated for smallpox. Both patients were advised to isolate themselves at home for three weeks. No new lesions appeared during this period. Both patients reported a rapid and self-limited disease course, with no need for any treatment.
The current predilection of MPXV lesions to genital, perianal and oral areas and a positive history of unprotected sexual intercourse suggest lesions may start at the site of inoculation. Similarly, both of our patients reported having unprotected oral sex respectively fourteen and ten days before; in both, the first lesion was observed on the oral cavity. Virus entry through the inoculation site could be followed by the development of systemic symptoms and subsequent dissemination of cutaneous lesions, but there is a great inter-individual clinical variability [5].
Unilesional or paucilesional MPXV cases have already been reported, as well as patients who never develop systemic symptoms [6,7].
The papular rash on the trunk of patient 1 that did not become pustular or ulcerated is a finding that represents an additional change in the clinical presentation of this multifaceted disease.
In the current rapidly growing outbreak of MPXV, these two cases highlight the importance of considering MPXV infection as one of the differential diagnoses in all MSM patients with risky sexual behaviour who exhibited atypical oropharyngeal signs and symptoms. For these cases, it is necessary to ensure accessible, rapid and reliable tests to aid early diagnosis and reduce onward transmission.
Declaration of competing interest
All authors declare no conflicts of interest.
References
- 1.Bunge E.M., Hoet B., Chen L., Lienert F., Weidenthaler H., Baer L.R., et al. The changing epidemiology of human monkeypox-A potential threat? A systematic review. PLoS Neglected Trop Dis. 2022 Feb 11;16(2) doi: 10.1371/journal.and.0010141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bryer J., Freeman E.E., Rosenbach M. Monkeypox emerges on a global scale: a historical review and dermatologic primer. J Am Acad Dermatol. 2022 Jul 8:S0190. doi: 10.1016/j.jaad.2022.07.007. 9622(22)02261-7. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization Disease outbreak news; multi-country monkeypox outbreak in non-endemic countries: update. https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON396 Available at:
- 4.Vallée A., Farfour E., Zucman D. Monkeypox virus: a novel sexually transmitted disease? A case report from France. Trav Med Infect Dis. 2022 Jun 28;49 doi: 10.1016/j.tmaid.2022.102394. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patel A., Bilinska J., Tam J.C.H., Da Silva Fontoura D., Mason C.Y., Daunt A., et al. Clinical features and novel presentations of human monkeypox in a central London centre during the 2022 outbreak: descriptive case series. BMJ. 2022 Jul 28;378 doi: 10.1136/BMJ-2022-072410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Turco M., Mancuso F.R., Pisano L. A Monkeypox virus infection mimicking primary syphilis. Br J Dermatol. 2022 Aug 25 doi: 10.1111/bjd.21847. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 7.Quattri E., Avallone G., Maronese C.A., Cusini M., Carrera C.G., Marzano A.V., Ramoni S. Unilesional monkeypox: a report of two cases from Italy. Trav Med Infect Dis. 2022 Aug 10;49 doi: 10.1016/j.tmaid.2022.102424. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]