Abstract
Background:
Global reports indicate rising Achilles tendon rupture (ATR) incidence. In recent decades, the optimal treatment for this injury has been widely studied. Alongside the cumulating comparative evidence regarding the optimal method of treatment, nonoperative treatment has increased in popularity compared with operative treatment.
Purpose:
To determine the current incidence of ATRs and their treatment in Finland and how these have changed from 1997 to 2019.
Study Design:
Descriptive epidemiology study.
Methods:
Two national registers (the National Hospital Discharge Register and the Finnish Register of Primary Health Care Visits) were used to identify all ATR cases and operations to treat them; the incidence was calculated based on the annual adult population size.
Results:
During the study period, ATR incidence increased from 17.3 to 32.3 per 100,000 person-years. The increase in incidence seemed to plateau starting in the second half of the study period. The rise in ATR incidence occurred in both sexes and all age groups but most markedly among the elderly. The incidence of operative treatment decreased from 13.6 to 4.9 per 100,000 person-years. This decline was observed from 2008 onward and in all age groups.
Conclusion:
The incidence of ATRs increased and the use of operative treatment decreased. The decreasing trend of operative treatment is in line with other international reports and resonates with the current literature about the optimal treatment of ATRs.
Keywords: ankle, Achilles tendon, general sports trauma, epidemiology
The incidence of Achilles tendon rupture (ATR) is increasing worldwide. 3,5,8,11,19 In Denmark, the overall incidence of ATR was 31 per 100,000 person-years in 2013, compared with 27 per 100,000 person-years in 1994. 5 ATRs occur predominantly in men; in Sweden, the incidence per 100,000 person-years was 55 for men compared with 14.7 for women in 2012. 8 ATRs have previously been regarded mostly as a sports injury of recreational athletes in the young to middle-aged population, but the current increase in ATR frequency has also been seen in more elderly patients with varying injury mechanisms. 5,6,8,11
Previously, most ATRs were treated operatively, but nonoperative treatment gained popularity during the 2000s as numerous randomized controlled trials (RCTs) comparing ATR treatment types presented comparable outcomes between operative and nonoperative treatment. 5,8,19 Meta-analyses derived from RCTs have not shown a significant difference in functional outcomes between these treatment methods, but when comparing adverse outcomes, nonoperative treatment has been shown to have a higher risk of rerupture, whereas operative treatment has a higher risk of complications, such as infection, thromboembolic events, and sural nerve injury. 2,4,15 –18,20,23 Functional nonoperative treatment with early range of motion and early weightbearing, however, does not seem to have a significantly higher rerupture risk compared with operative treatment. 15,16,20,23
The incidence of ATR surgery increased in Finland between 1987 and 2011, but a trend toward more nonoperative treatment from 2008 onward has been detected. 13 More recent data on ATR incidence and ATR treatment method trends in Finland are lacking. The aim of the current study was to determine the incidence of ATR in Finland between 1997 and 2019 based on data from two national registers: the National Hospital Discharge Register (NHDR) and, for the first time, the Finnish Register of Primary Health Care Visits (PHCR). Another aim was to investigate whether the treatment method of ATRs—operative versus nonoperative—has changed in recent years in Finland, alongside increasing scientific evidence regarding their optimal choice of treatment.
Methods
This is a register study based on data from the NHDR and PHCR, both of which are maintained by the National Institute for Health and Welfare. The NHDR was founded in 1967, and data reporting to the register are obligatory for all public and private hospitals in Finland. The PHCR similarly receives data on all patient encounters within the public primary health care system (primary health care centers) in Finland, and it has been in use since 2011. The registers contain data on age, sex, domicile, external cause of injury, type of injury, primary and secondary diagnoses, type of hospital (public or private), duration of hospital stay, and possible operations performed during the hospital stay. The validity of the NHDR has been found to be good, especially when it comes to orthopaedic trauma. 9,14,22 Ethical approval was received for the study protocol.
The databases were searched for all records with a primary or secondary diagnosis code of S86.0, “injury of Achilles tendon” (International Classification of Diseases, 10th Revision [ICD-10]) between January 1, 1997, and December 31, 2019. The NHDR was also searched for all records with the procedural code NHL10, “suture or reinsertion of Achilles tendon” (Nordic Classification of Surgical Procedures [NCSP]). This was done to identify all nonoperatively and operatively treated patients in both primary health care centers and hospitals in Finland. All duplicate cases between the 2 registers were excluded. All subsequent records with diagnosis code S86.0 were excluded to include only acute ATRs for the incidence calculations. Only records with operative treatment within 30 days of injury were included in the operative treatment incidence calculation to describe firsthand choice of operative treatment, apart from the treatment of ATR sequelae or salvage of failed nonoperative treatment. Only patients 16 years of age and older were included. The incidence was calculated based on the annual adult population size (persons aged ≥16 years) obtained from Statistics Finland. 21 Data on patient age, sex, procedures performed during the hospital stay, injury mechanism, and external cause of injury were also collected. A flowchart of patient inclusion in the study is shown in Figure 1.
Figure 1.
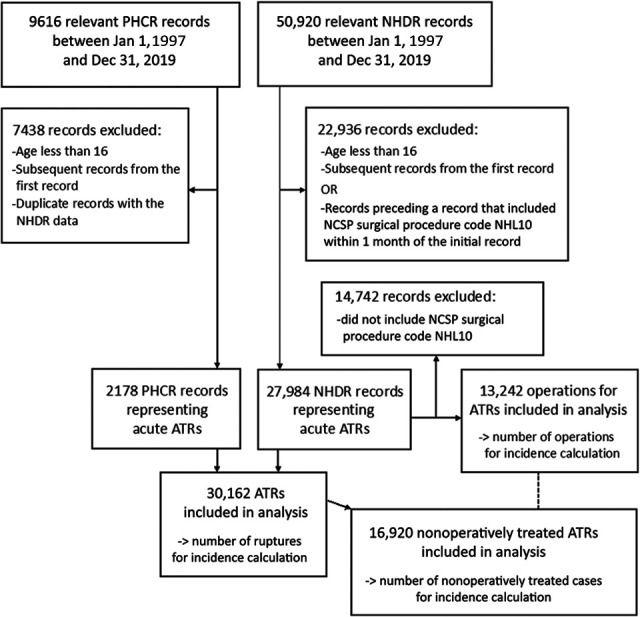
Patient-inclusion flowchart. ATR, Achilles tendon rupture; NCSP, Nordic Classification of Surgical Procedures; NHDR, National Hospital Discharge Register; NHL10, PHCR, Finnish Register of Primary Health Care Visits.
Continuous variables were summarized with means with standard deviations and ranges. The difference in the treatment method of ATRs between sexes was analyzed using the chi-square test. Incidence calculations as well as other statistical reporting were performed using SAS software Version 9.4 of the SAS System for Windows (SAS Institute).
Results
A total of 30,162 acute ATRs were registered in the NHDR and the PHCR during the 23-year study period. Of these cases, 13,242 (44%) were treated operatively and 16,920 (56%) nonoperatively. Overall, 2178 patients were treated nonoperatively in primary health care centers and registered only in the PHCR (Figure 2). The overall incidence of ATRs increased between 1997 and 2019 from 17.3 to 32.3 per 100,000 person-years (Figure 3A). The rise in incidence occurred mainly during the first half of the study period (1997-2011), forming a plateau during the latter half.
Figure 2.
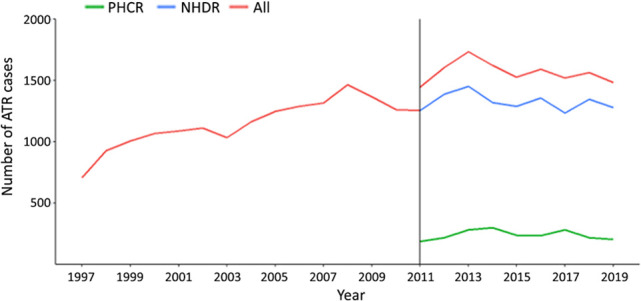
Frequency of Achilles tendon rupture (ATR). NHDR, National Hospital Discharge Register; PHCR, Finnish Register of Primary Health Care Visits.Vertical line indicates the introduction of the PHCR and its data.
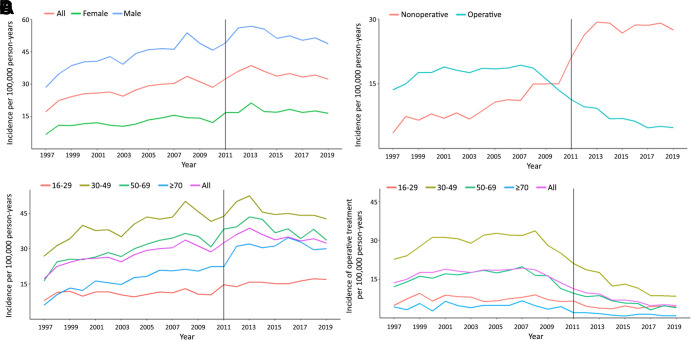
Figure 3.
(A) Overall and sex-adjusted incidence of Achilles tendon rupture (ATR). (B) Incidence of operative and nonoperative treatment for ATR. (C) Age-adjusted incidence of ATR. (D) Age-adjusted incidence of operative treatment for ATR.
The incidence of nonoperative treatment increased considerably (from 3.7 to 27.5 per 100,000 person-years), whereas the incidence of operative treatment decreased (from 13.6 to 4.9 per 100,000 person-years) during the study time (Figure 3B). The decrease in operative treatment occurred from 2008 onward.
The incidence of ATRs rose in both sexes across the study period (Figure 3A). ATRs were most frequent in men (22,735 cases; 75% of all cases) and in the age group of 30 to 49 years. In 1997, the incidences were 28.6 and 6.76 per 100,000 person-years for men and women, respectively. In 2019, the incidence for men was almost threefold compared with that for women, with 48.8 compared to 16.6 per 100,000 person-years, respectively. There was a statistically significant difference in the treatment method of ATRs between sexes during the study period: men were more often treated operatively (47%) than women (36%) (P < .0001).
The mean age of the patients was 44 ± 12.6 years (range, 16-91 years) among operatively treated and 53 ± 16.3 years (range, 16-101 years) among nonoperatively treated patients. The age-adjusted incidence of ATRs increased in every age group during the study period but most significantly in the age group ≥70 years (from 6.1 to 30.1 per 100,000 person-years) (Figure 3C). The incidence of operative treatment decreased in every age group (Figure 3D).
The most commonly reported injury mechanisms were sports injuries (7279 cases), recreational injuries (5082 cases), and domestic accidents (1522 cases).
Discussion
We found that the incidence of ATRs increased in the Finnish population between 1997 and 2019, especially in the older age groups. Despite the increase in ATR incidence, the incidence of operative treatment of ATRs decreased from 13.6 to 4.9 per 100,000 person-years during our study period. A shift toward more nonoperative treatment was observed in all age groups.
The global reported incidence of ATRs increased in the 2000s. 3,5,8,11,19 The Nordic countries are well represented in this area of study, but although there are published results from Danish and Swedish national registers, there have been no previous studies covering the national incidence of ATRs in Finland. In 2015, Lantto et al 11 published an article on ATR incidence based on a cohort of 515 patients treated in Oulu, Finland, from 1979 to 2011. There was an almost 10-fold increase in the incidence of ATRs (per 100,000 person-years), rising from 2.1 to 21.5 in 2011. Our findings from the first half of our study period were comparable. During the second half of our study period, the increase in ATR incidence seemed to plateau. A coinciding similar trend has been shown in recent Japanese national register data from 2010 to 2017. 26 Huttunen et al 8 studied the incidence of ATRs and their treatment methods in Sweden between 2001 and 2012; here, the ATR incidence (per 100,000 person-years) rose in both sexes in the Swedish population, increasing from 47.0 to 55.2 for men and from 12.0 to 14.7 for women. Ganestam et al 5 published a similar study based on data from the Danish population between 1994 and 2013. The overall ATR incidence rose from 26.95 to 31.17 in Denmark. The overall and sex-adjusted incidences in these two studies are comparable with what we see in the Finnish population in the overlapping time periods. The more pronounced rise in incidence in the elderly age groups compared with younger ones is evident in all three Nordic countries, a fact that may be due to the aging population increasingly taking part in high-demand sports and activities. This is in line with reports from the United Kingdom, the rest of Europe, North America, and Asia. 6,12
The Swedish and Danish hospital discharge registers resemble the NHDR in their data-collection principles: They cover both inpatient and outpatient visits, but, like the NHDR, they do not cover patients treated in primary health care. To the best of our knowledge, this is the first national register study to include ATRs treated in both hospitals and primary health care centers. The introduction of the PHCR in 2011 coincides with a marked increase in ATR incidence and nonoperative treatment incidence for ATRs. It is possible that previous studies based on data only from hospital records have underestimated ATR and nonoperative treatment incidences because data from primary healthcare have not been available. ATRs, as well as several other injuries, do often not require hospitalization or referral to a specialist unit when treated nonoperatively.
The optimal treatment method for ATRs has been widely studied in recent years. Results from numerous RCTs comparing operative and nonoperative treatment have been pooled into several meta-analyses. 2,4,15 –18,20,23 Essentially, nonoperative treatment is associated with a greater risk of rerupture (risk ratio ranging from 0.27 to 0.43 in favor of surgery 16,18 ), whereas operative treatment is associated with surgery-related complications (overall complication risk ratio ranging from 2.76 to 6.06 in favor of nonoperative treatment 16,18 ), especially infections (risk ratio ranging from 3.43 to 6.69 17,18 ), thromboembolic events, and sural nerve damage. However, unlike the risks associated with open surgery, the risk of rerupture has been disputed, and some conflicting interpretations have been presented in the meta-analyses mentioned above. 2,4,15 –18,20,23
Operative treatment was historically considered superior to nonoperative treatment, as reruptures were a frequent concern with nonoperative care. 10 Nonoperative treatment, originally comprising rigid cast immobilization and limited weightbearing, has evolved alongside increasing knowledge of tendon healing principles into a functional rehabilitation strategy with early protected range of motion and early weightbearing. In their 2010 RCT comparing operative and functional nonoperative treatment of ATRs, Willits et al 25 demonstrated no difference in rerupture risk in favor of operative treatment. Wallace et al 24 published similar findings in their RCT a year later. A 2012 meta-analysis by Soroceanu et al 20 pointed out the advantage of early range of motion and that patients with this applied in nonoperative treatment had no greater risk of rerupture compared with operative treatment. Another 2013 meta-analysis by Van der Eng et al 23 concluded that rehabilitation with early weightbearing led to lower rerupture rates, with no difference between operatively and nonoperatively treated patients. Some later meta-analyses interpret the evidence on rerupture rates in favor of operative treatment and have highlighted the advantages of, for example, minimally invasive surgical techniques and the potentially earlier return to work when compared with nonoperative treatment. 2,4,17 Others, on the other hand, have found the rerupture risk difference between treatment groups to be small compared to the overall complication risk difference (1.6% vs 3.3%, respectively), favoring nonoperative treatment, and that across contemporary treatments (prolonged cast immobilization excluded), the risk of rerupture is probably no different between treatment groups. 15,16 The importance of careful individual consideration of the potential risks and advantages between treatment options alongside shared decision making has been highlighted in these two last studies. 15,16 It should be noted that all these abovementioned meta-analyses are derived from RCTs, which are quite heterogeneous in their methodology and rehabilitation protocols for nonoperative and operative treatments. A large portion of the RCTs date back to the first decade of the 21st century or earlier, when functional nonoperative treatment was less mainstream compared to more recent times. Detailed and tested functional nonoperative treatment protocols have later been described and published (for example, the results of the UK-based SMART protocol 7 and UKSTAR multicenter RCT 1 ).
Regardless of whether we consider the available evidence in favor of operative or nonoperative treatment, there are reports of decreasing operative treatment rates for ATRs. In Sweden and Denmark, operative treatment rates have been decreasing since the latter half of the first decade of the 21st century. 5,8 In 2015, Mattila et al 13 reported the incidence of operative treatment of ATRs in Finland between 1987 and 2011. The incidence increased for men and women from 11.1 and 2.5 to 20.5 and 4.2 per 100,000 person-years, respectively; this study pointed out the increasing rate of operative treatment, which rose steadily up to the end of the first decade of the 21st century, peaking from 2007 to 2008, after which an impending decline was noted. We have now verified that this decline in the operative treatment of ATRs has continued. We have also shown that the decline in surgery incidence is a real change in practice, not the result of a possible simultaneous decline in ATR incidence.
Limitations
We acknowledge that the current study has several limitations. First, it is an observational study based on administrative databases. The NHDR and PHCR registers have limitations because of their data-collection principles. The injury mechanisms and external causes of injury were poorly reported, especially in the PHCR, so we were unable to show possible changes in the injury mechanism, or single out sports-related injuries. Second, although the ICD-10 diagnosis code for ATR is quite specific, in the case of reruptures and ATR sequelae, there are no anatomically specific ICD-10 codes or methods of systematic documentation. The NHDR and PHCR also do not report the side of injury (left or right). A person can sustain an acute ATR twice, once in each lower limb. In the interest of clarity and repeatability, we chose to include only the first recorded injury. By doing this, we excluded possible acute ATRs of the other side, which may slightly underestimate the injury incidence. However, because the pool of patients with multiple injury records was quite small and because our aim was mostly to describe the trend in incidence, we consider the risk for significant bias to be small. Additionally, as our aim was to describe firsthand choice of treatment, the operative treatment group included only patients operated on within 30 days of injury. By doing this, roughly 600 patients were categorized as treated nonoperatively, despite a later operation with the NCSP code NHL10. By going through the data manually, we could ascertain that one-tenth of these patients probably suffered an acute injury of the opposite side and were operated on years later after their initial injury, whereas the rest of the patients probably underwent delayed surgery because of failed nonoperative treatment or rerupture. However, the number of these patients was small compared with the study population of 30,162 ATRs and 13,242 operations. Therefore, we do not think that this has caused significant bias in our results. Finally, we wish to emphasize that the aim of this study was not to report or compare results of operative or nonoperative treatment or give treatment recommendations.
Conclusion
The incidence of ATRs increased in Finland from 1997 to 2019. However, the rise seemed to plateau around 2010. The proportion of nonoperative treatment increased continuously throughout the study period. This change in treatment principle is in line with reported international trends and current literature, which has shown that when compared with operative treatment, nonoperative treatment provides comparable functional results with only slightly increased rerupture risk, without the complications associated with surgery.
Footnotes
Final revision submitted June 21, 2022; accepted August 4, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: Support for this study was received from a grant from the Finnish state research fund. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for the study was granted by the Finnish National Institute of Health and Wellness (study permit No. THL/2266/5.05.00/2019).
References
- 1. Costa ML, Achten J, Marian IR, et al. Plaster cast versus functional brace for non-surgical treatment of Achilles tendon rupture (UKSTAR): a multicentre randomised controlled trial and economic evaluation. Lancet. 2020;395(10222):441–448. doi:10.1016/S0140-6736(19)32942-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Deng S, Sun Z, Zhang C, Chen G, Li J. Surgical treatment versus conservative management for acute Achilles tendon rupture: a systematic review and meta-analysis of randomized controlled trials. J Foot Ankle Surg. 2017;56(6):1236–1243. doi:10.1053/J.JFAS.2017.05.036 [DOI] [PubMed] [Google Scholar]
- 3. Erickson BJ, Cvetanovich GL, Nwachukwu BU, et al. Trends in the management of Achilles tendon ruptures in the United States Medicare population, 2005-2011. Orthop J Sports Med. 2014;2(9):2325967114549948. doi:10.1177/2325967114549948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Erickson BJ, Mascarenhas R, Saltzman BM, et al. Is operative treatment of Achilles tendon ruptures superior to nonoperative treatment? A systematic review of overlapping meta-analyses. Orthop J Sports Med. 2015;3(4):23259 67115579188. doi:10.1177/2325967115579188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ganestam A, Kallemose T, Troelsen A, Barfod K. Increasing incidence of acute Achilles tendon rupture and a noticeable decline in surgical treatment from 1994 to 2013. A nationwide registry study of 33,160 patients. Knee Surg Sports Traumatol Arthrosc. 2016;24(12):3730–3737. doi:10.1007/S00167-015-3544-5 [DOI] [PubMed] [Google Scholar]
- 6. Ho G, Tantigate D, Kirschenbaum J, Greisberg JK, Vosseller JT. Increasing age in Achilles rupture patients over time. Injury. 2017;48(7):1701–1709. doi:10.1016/J.INJURY.2017.04.007 [DOI] [PubMed] [Google Scholar]
- 7. Hutchison AM, Topliss C, Beard D, Evans RM, Williams P. The treatment of a rupture of the Achilles tendon using a dedicated management programme. Bone Joint J. 2015;97-B(4):510–515. doi:10.1302/0301-620X.97B4.35314 [DOI] [PubMed] [Google Scholar]
- 8. Huttunen T, Kannus P, Rolf C, Felländer-Tsai L, Mattila V. Acute Achilles tendon ruptures: incidence of injury and surgery in Sweden between 2001 and 2012. Am J Sports Med. 2014;42(10):2419–2423. doi:10.1177/0363546514540599 [DOI] [PubMed] [Google Scholar]
- 9. Huttunen TT, Kannus P, Pihlajamäki H, Mattila VM. Pertrochanteric fracture of the femur in the Finnish National Hospital Discharge Register: validity of procedural coding, external cause for injury and diagnosis. BMC Musculoskelet Disord. 2014;15(1):95–98. doi:10.1186/1471-2474-15-98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jones M, Khan R, Carey Smith R. Surgical interventions for treating acute Achilles tendon rupture: key findings from a recent Cochrane review. J Bone Joint Surg Am. 2012;94(12):e88. doi:10.2106/JBJS.J.01829 [DOI] [PubMed] [Google Scholar]
- 11. Lantto I, Heikkinen J, Flinkkilä T, Ohtonen P, Leppilahti J. Epidemiology of Achilles tendon ruptures: increasing incidence over a 33-year period. Scand J Med Sci Sports. 2015;25(1):e133–e138. doi:10.1111/SMS.12253 [DOI] [PubMed] [Google Scholar]
- 12. Maffulli N, Waterston SW, Squair J, Reaper J, Douglas AS. Changing incidence of Achilles tendon rupture in Scotland: a 15-year study. Clin J Sport Med. 1999;9(3):157–160. doi:10.1097/00042752-199907000-00007 [DOI] [PubMed] [Google Scholar]
- 13. Mattila V, Huttunen T, Haapasalo H, Sillanpää P, Malmivaara A, Pihlajamäki H. Declining incidence of surgery for Achilles tendon rupture follows publication of major RCTs: evidence-influenced change evident using the Finnish registry study. Br J Sports Med. 2015;49(16):1084–1086. doi:10.1136/BJSPORTS-2013-092756 [DOI] [PubMed] [Google Scholar]
- 14. Mattila VM, Sillanpää P, Iivonen T, Parkkari J, Kannus P, Pihlajamäki H. Coverage and accuracy of diagnosis of cruciate ligament injury in the Finnish National Hospital Discharge Register. Injury. 2008;39(12):1373–1376. doi:10.1016/j.injury.2008.05.007 [DOI] [PubMed] [Google Scholar]
- 15. Meulenkamp B, Woolnough T, Cheng W, et al. What is the best evidence to guide management of acute Achilles tendon ruptures? A systematic review and network meta-analysis of randomized controlled trials. Clin Orthop Relat Res. 2021;479(10):2119–2131. doi:10.1097/CORR.0000000000001861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ochen Y, Beks RB, Van Heijl M, et al. Operative treatment versus nonoperative treatment of Achilles tendon ruptures: systematic review and meta-analysis. BMJ. 2019;364:K5120. doi:10.1136/BMJ.K5120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Reda Y, Farouk A, Abdelmonem I, El Shazly OA. Surgical versus non-surgical treatment for acute Achilles’ tendon rupture. A systematic review of literature and meta-analysis. Foot Ankle Surg. 2020;26(3):280–288. doi:10.1016/j.fas.2019.03.010 [DOI] [PubMed] [Google Scholar]
- 18. Seow D, Yasui Y, Calder JDF, Kennedy JG, Pearce CJ. Treatment of acute Achilles tendon ruptures: a systematic review and meta-analysis of complication rates with best- and worst-case analyses for rerupture rates. Am J Sports Med. 2021;49(13):3728–3748. doi:10.1177/0363546521998284 [DOI] [PubMed] [Google Scholar]
- 19. Sheth U, Wasserstein D, Jenkinson R, Moineddin R, Kreder H, Jaglal SB. The epidemiology and trends in management of acute Achilles tendon ruptures in Ontario, Canada: a population-based study of 27 607 patients. Bone Joint J. 2017;99-B(1):78–86. doi:10.1302/0301-620X.99B1.BJJ-2016-0434.R1 [DOI] [PubMed] [Google Scholar]
- 20. Soroceanu A, Sidhwa F, Aarabi S, Kaufman A, Glazebrook M. Surgical versus nonsurgical treatment of acute Achilles tendon rupture: a meta-analysis of randomized trials. J Bone Joint Surg Am. 2012;94(23):2136–2143. doi:10.2106/JBJS.K.00917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Statistics Finland. Population structure. Accessed October 9, 2022. https://stat.fi/index_en.html
- 22. Sund R. Quality of the Finnish Hospital Discharge Register: a systematic review. Scand J Public Health. 2012;40(6):505–515. doi:10.1177/1403494812456637 [DOI] [PubMed] [Google Scholar]
- 23. Van der Eng D, Schepers T, Goslings J, Schep N. Rerupture rate after early weightbearing in operative versus conservative treatment of Achilles tendon ruptures: a meta-analysis. J Foot Ankle Surg. 2013;52(5):622–628. doi:10.1053/J.JFAS.2013.03.027 [DOI] [PubMed] [Google Scholar]
- 24. Wallace RGH, Heyes GJ, Michael ALR. The non-operative functional management of patients with a rupture of the tendo Achillis leads to low rates of re-rupture. J Bone Joint Surg Br. 2011;93B(10):1362–1366. doi:10.1302/0301-620X.93B10.26187 [DOI] [PubMed] [Google Scholar]
- 25. Willits K, Amendola A, Bryant D, et al. Operative versus nonoperative treatment of acute Achilles tendon ruptures: a multicenter randomized trial using accelerated functional rehabilitation. J Bone Joint Surg Am. 2010;92(17):2767–2775. doi:10.2106/JBJS.I.01401 [DOI] [PubMed] [Google Scholar]
- 26. Yamaguchi S, Kimura S, Akagi R, et al. Increase in Achilles tendon rupture surgery in Japan: results from a nationwide health care database. Orthop J Sports Med. 2021;9(10):23259671211034128. doi:10.1177/23259671211034128 [DOI] [PMC free article] [PubMed] [Google Scholar]