Abstract
Background:
Individuals with substance use disorders (SUDs) have highly heterogeneous presentations and identifying more homogeneous subgroups may foster more personalized treatment. This study used SUD and other psychiatric indicators to characterize latent subgroups of patients in a large inpatient addiction treatment program. The resulting subgroups were then analyzed with respect to differences on clinically informative motivational mechanisms.
Methods:
Patients (n = 803) were assessed for severity of SUD (ie, alcohol use disorder, drug use disorder), post-traumatic stress disorder, anxiety disorders, and major depressive disorder. Confirmatory latent profile analysis (CLPA) was used to identify latent subgroups, hypothesizing 4 subgroups. Subgroups were then characterized with respect to multiple indicators of impulsivity (ie, delay discounting and impulsive personality traits via the UPPS-P) and craving.
Results:
The CLPA confirmed the hypothesized 4-profile solution according to all indicators (eg, entropy = 0.90, all posterior probabilities ⩾.92). Profile 1 (n = 229 [32.2%], 24.9% female, median age in range of 45-49) reflected individuals with high alcohol severity and low psychiatric severity (HAlc/LPsy). Profile 2 (n = 193 [27.1%], 29.3% female, median age in range of 35-39) reflected individuals with high drug and psychiatric severity (HDrug/HPsy). Profile 3 (n = 160 [22.5%], 37.6% female, median age in range of 45-49) reflected individuals with high alcohol severity and psychiatric severity (HAlc/HPsy). Profile 4 (n = 130 [18.3%], 19.4% female, median age in range of 35-39) reflected individuals with high drug severity and low psychiatric severity (HDrug/LPsy). Both high comorbid psychiatric severity subgroups exhibited significantly higher craving and facets of impulsivity.
Conclusions:
The results provide further evidence of 4 latent subgroups among inpatients receiving addiction treatment, varying by alcohol versus other drugs and low versus high psychiatric comorbidity. Furthermore, they reveal the highest craving and impulsivity in the high psychiatric comorbidity groups, suggesting targets for more intensive clinical intervention in these patients.
Keywords: Substance use disorders, impulsivity, craving, treatment, mental health
Introduction
Substance use disorders (SUDs) are a major public health concern that affect society in multiple ways including loss of productivity, increased healthcare costs, increased crime rate, and diminished quality of life for those affected.1,2 Effective treatments for SUDs are necessary, but dropout and the risk of relapse during periods of abstinence is a major challenge.3,4 Studies have reported an average 30% dropout rate and that up to 60% to 90% of individuals relapse within the first year following treatment.5-7 Therefore, approaches to increase treatment effectiveness and remission rates have become important.
Recently, there is growing interest in “precision medicine” or “personalized medicine,” which moves away from a “one-size-fits-all” approach and instead involves tailoring treatment based on an individual’s characteristics.8 Individualized treatment has shown to be a key predictor of treatment success in the field of oncology.9,10 However, this approach is infrequently implemented within large, inpatient SUD treatment and group-based psychiatry programs. In part, the effectiveness of such treatment strategies rests on the ability of clinicians to understand individual characteristics and risk factors, identify patient needs, and administer the most effective treatment program to maximize treatment outcomes.
One strategy for a personalized approach involves using methods that detect heterogeneity and identifying latent subgroups of patients within a clinical population. Syan et al11 used a person-centered approach to classify patients into statistically distinct latent subgroups based on a pattern of responses to substance use severity and mental health indicators (eg, depression, anxiety, and post-traumatic stress disorder). It was found that there were 4 distinct underlying latent profiles. The highest risk profile was characterized by high drug severity, high psychiatric co-morbidity, but low alcohol severity. These individuals were more likely to exhibit high rates of premature termination.11 The lowest risk profile was characterized by high alcohol severity, low drug severity, and low psychiatric severity. These individuals showed significantly lower rates of pre-mature dropout.11 The findings are consistent with earlier studies demonstrating that co-morbid psychiatric and SUD are associated with poor treatment outcomes,12,13 including a more chronic and treatment-resistant trajectory.12 The findings further highlight the underlying heterogeneity in the substance treatment population14,15 and a further need to understand individual differences. Thus, while individuals with SUDs may share certain characteristics (eg, meeting 2 or more diagnostic criteria based on the DSM-V), there appear to be subsets of individuals with more nuanced psychiatric symptom profiles. Moreover, these subgroups may meaningfully differ on treatment-related mechanisms, in turn implying that different treatment options or care paths may be valuable for different groups of patients.
In particular, patient features that are implicated in treatment outcomes include cravings and impulsivity. Drug cravings (ie, clinically significant levels of subjective desire or urge to use a drug) have shown to be predictive of treatment outcome,16 albeit with some mixed findings.17 Similarly, high levels of impulsivity have shown to be a reliable predictor of drug-seeking and relapse.18,19 Importantly, recent descriptions of impulsivity go beyond its conceptualization as a univariate construct and focus on its multidimensional nature.20 According to one recent conceptualization, impulsivity can be subdivided into impulsive personality traits (ie, self-reported attributions about self-regulatory capacity on personality measures), impulsive action (ie, ability to restrain a prepotent motor response on an inhibitory control performance test, eg, Go/NoGo), and impulsive choice (ie, overvaluation of smaller immediate rewards over larger delayed rewards; steep delay discounting [DD]).20,21 Notably, impulsive personality traits and precipitous DD have been found to have robust prognostic value.22,23 However, in both the case of craving and impulsivity, no previous studies have examined differential expressions within latent subgroups of patients in addiction treatment. By identifying how combinations of presenting substance use and psychiatric symptoms interact to influence these motivational mechanisms, individuals can be matched to relevant therapeutic interventions (ie, a subgroup ie, elevated for craving would putatively benefit from urge management coping skills).
The goal of the current study was to bring together these 2 lines of inquiry, both characterizing the clinical heterogeneity in terms of latent subgroups and examining subgroup differences in terms of craving and impulsivity. Specifically, in a large sample of individuals who were newly admitted to an inpatient addiction treatment program, the first objective was to test the hypothesis that a previously detected 4-profile latent profile solution (ie, High Drug/High Psychiatric Severity, High Drug/Low Psychiatric Severity, High Alcohol/High Psychiatric Severity, and Low Drug/Low Psychiatric Severity11) would be identified using confirmatory latent profile analysis (CLPA). The second objective was to extend the previous findings by examining the observed sub-groups in terms of cravings and impulsivity. It was hypothesized that those with co-morbid substance and psychiatric severity would exhibit higher severity on those motivational mechanisms, especially relating to emotional regulation (eg, negative urgency) because of a negatively reinforcing motivational profile (ie, using substances to cope with mental health symptoms). Overall, the goal of the study was to better characterize individual patient treatment needs, setting the stage of care paths that address common clusters of patients, with the ultimate goal of greater patient engagement, decreases in treatment dropout, and improvements in recovery outcomes.
Methods
Participants
Participants were a sample of individuals (n = 803) admitted to an inpatient addiction treatment program between April 2017 and April 2018. The treatment program is embedded within a larger mental health and addictions treatment center in Guelph, Ontario, Canada. Treatment was provided by a multidisciplinary team comprising of physicians, nurses, and other healthcare workers. Programming was paid for by a combination of semiprivate/private insurance, direct payment, and/or public health insurance (ie, Ontario Health Insurance Program). At the time, the program offered group-based treatment that was 35 to 42 days in length to adults aged 19+ with alcohol and/or substance use disorders (SUDs) and a 56-day integrated program for patients with SUDs and PTSD.
Patients completed an electronic questionnaire within the first 7 days of admission designed to assess substance use and psychiatric symptomology to inform patient care. At the time of data collection, patients provided informed consent for the use of their data for secondary research purposes. Patients were excluded from data analysis for the following reasons: (1) had any missing data on the variables used in the latent profile analysis; or (2) identical responses on 3 or more of the measures (ie, low effort or attention as indicated by lack of response variability). Using these criteria, 76 participants were excluded from analysis for missing data and 15 were excluded for careless responding. The final sample (n = 712) was comprised mostly of adults ⩾40+ (~57.7%) with 72.1% males and most having completed some form of college/university (see Table 1 for descriptive statistics). All study procedures were approved by the Regional Centre for Excellence in Ethics, Research Ethics Board at Homewood Healthcare Centre in Guelph, Ontario (Protocol #16-06).
Table 1.
Descriptive statistics and frequencies of participants.
| Measures | Mean (SE) or % |
|---|---|
| Age | |
| Under 25 | 8.3 |
| 25-29 | 8.3 |
| 30-35 | 13.1 |
| 35-39 | 12.6 |
| 40-44 | 15.7 |
| 45-49 | 12.9 |
| 50-54 | 12.1 |
| 55-59 | 9.8 |
| 60+ | 7.2 |
| Biological sex (% female) | 27.9 |
| Education (completed college/university) | 49.0 |
| Employment (employed) | 77.4 |
| AUD symptoms | 7.06 (0.145) |
| DUD symptoms | 4.96 (0.176) |
| PHQ-9 | 12.88 (0.265) |
| GAD-7 | 10.61 (0.232) |
| PCL-5 | 33.16 (0.747) |
Abbreviations: AUD, alcohol use disorder; DUD, drug use disorder; GAD-7, generalized anxiety disorder (7-items); PCL-5, post-traumatic stress disorders checklist for DSM; PHQ-9, patient health questionnaire (9-items).
Assessment measures
Demographics
Demographics information (ie, age, sex, education, employment status, and other descriptive statistics) was obtained from Resident Assessment Instrument-Mental Health, a tool that collects data as part of the Ontario Mental Health Reporting System which is part of regular care.
Substance use disorders
The DSM-5 substance use disorder24 self-report checklist assessed the severity of use over the past year for each endorsed substance including alcohol, cannabis, cocaine, other stimulants, heroin, other opioids, hallucinogens, sedatives, and prescription sleep aids. This measure consists of 11 yes/no symptom questions to determine presence and severity of substance use disorders. Continuous symptom counts were used as indicators in the CLPA, separately for alcohol and using the maximum severity across other psychoactive substances. This coding was for several reasons. Alcohol use was reported by a large majority of patients, making modeling alcohol severity valid across the whole sample, whereas only a minority of patients endorsed the other substances and, in some cases, a very small minority (eg, hallucinogens), creating substantial zero inflation. Furthermore, the distinction between alcohol use disorder and drug use disorder is common in epidemiology for the same reason. Most important, the study was specifically seeking to confirm a 4-profile solution that used a measure of alcohol severity and an aggregated measure of other substance use disorder. Coding separately would thus undermine the confirmatory LPA hypothesis. This self-report measure has been found to function equivalently to semi-structured clinical interviews in previous studies conducted in this treatment program.25
Psychiatric symptoms
The Generalized Anxiety Disorder—7 (GAD-7; anxiety26) is a self-report measure used to assess symptoms of generalized anxiety in the preceding 2 weeks. It is a 7-item measure with response options presented on a four-point Likert-type scale, where responses range from 1 (not at all) to 4 (nearly every day). The clinical threshold of moderate to severe anxiety within this sample was a score of 9 or above. The GAD-7 demonstrated excellent internal consistency (α = .92).
The Patient Health Questionnaire—9 (PHQ-9; depression) is a self-report measure used to assess symptoms of depression during the preceding 2 weeks.27 It is a 9-item measure with response options presented on a four-point Likert-type scale, where responses range from 1 (not at all) to 4 (nearly every day). The clinical threshold of moderate to severe depression within this sample was an obtained PHQ-9 score of 16 or above.25 The PHQ-9 demonstrated excellent internal consistency (α = .93).
The Post-Traumatic Stress Disorders Checklist for DSM 5 (PCL-5) is a standardized self-report measure used to assess key symptoms of post-traumatic stress disorder (PTSD).28 It is a 20-item measure with response options presented on a five-point Likert-type scale, where responses range from 0 (not at all) to 4 (extreme). The recommended cut-off to diagnose PTSD ranges from 30 to 60 (reviewed in McDonald and Calhoun28). The clinical threshold of probable PTSD within this sample was an obtained PCL score of 42 or above.25 The PCL-5 demonstrated excellent internal consistency (α = .96).
Impulsivity
The Monetary Choice Questionnaire (MCQ) is a measure of impulsive choice, or delay discounting, whereby individuals make choices between smaller immediate rewards and larger delayed rewards.29 Only the medium magnitude reward items were used (average delayed reward = $55).30 Responses can be used to determine temporal discounting function, commonly referred to as k. The higher the k, the more an individual discounts larger future reward.
The UPPS-P Impulsive Behavior Scale—Brief is a measure of impulsive personality traits informed by the 5 Factor Model of personality.31,32 It is a 20-item self-report questionnaire, where each item is rated on a 4-point Likert-type scale, 1 (Strongly agree)—4 (Strongly disagree). The responses are then categorized into 5 different domains: Negative Urgency (ie, tendency to act rashly when experiencing negative emotions; α = .74), Positive Urgency (ie, tendency to act rashly when experiencing positive emotions; α = .81), Lack of Perseverance (ie, inability to sustain attention and lack of motivation to complete task; α = .70), Lack of Premeditation (ie, tendency to act without thinking; α = .84), and Sensation Seeking (tendency to seek out and enjoy novel or exciting activities; α = .66).
Craving
Aggregated Penn Craving Scale (ADCS33) is an adaptation of the Pennsylvania alcohol cravings scale.34 It is a measure of craving for psychoactive substance use. It is a 5-item scale scored on a Likert Scale from 0 (never/none) to 6 (nearly every day/strong) assessing frequency, duration, and severity of drug cravings over the past week.
Data analysis
The first objective was to confirm a previously detected 4-profile latent profile solution in individuals in inpatient addiction treatment (ie, High Drug/High Psychiatric Severity, High Drug/Low Psychiatric Severity, High Alcohol/High Psychiatric Severity, and High Alcohol/Low Psychiatric Severity11). For this, a confirmatory latent profile analysis (CLPA) was performed, testing 4 profiles imposed on the data. Note that in contrast to latent class analysis, which uses dichotomous indicators, latent profile analysis uses dimensional (continuous) indicators. In this case, the continuous indicators were: (1) severity of alcohol use disorder; (2) severity of other drug use disorder; (3) depression severity (PHQ-9); (4) anxiety severity (GAD-7); and (5) PTSD severity (PCL-5). These broadly map to the indicators used in the previous report of a 4-profile solution. More specifically, in this approach, 2 models examined the 4-profile solutions with varying constraints on drug use, alcohol use, and psychiatric severity. In the first model, parameter constraints were set which: (1) restricted the standardized means of PHQ, GAD, and PCL to be equal to one another within each profile; (2) 2 profiles were constrained to have higher standardized means on PHQ, GAD, and PCL compared to the remaining 2 profiles; (3) constraints were set such that the 2 profiles with higher psychiatric severity would have equal psychiatric severity to one another and the 2 profiles with lower psychiatric severity would similarly have equal psychiatric severity to one another; and (4) 1 high psychiatric severity profile and 1 low psychiatric severity profile were constrained to have higher drug use severity and lower alcohol use severity compared to the remaining 2 profiles; (5) the 2 profiles constrained to have high drug severity and low alcohol severity would have means equal to each other; and (6) 2 profiles with low drug use severity and high alcohol use severity were constrained to have means equivalent to each other. The second 4-profile model utilized the same constraints as the first model with the exception that the standardized means of PHQ, GAD, and PCL were not constrained to be equal to one another within each profile. Syan et al found similar means of PHQ-9, GAD-7, and PCL-5 within each profile, however, an additional model that allows the means to vary from one another was tested to explore whether a better model fit would result. Additional models with 1-, 2-, and 3-profile solutions were examined as well for comparison. All models were run using maximum likelihood robust estimation in MPlus.35 To determine an optimal profile solution, the 4-profile solution models were compared to the models with 1, 2, and 3 profile structures to test for best model fit. The Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), sample size adjusted BIC, Bootstrapped Likelihood Ratio Test, and entropy were used to assess model fit.36 Smaller AIC and BIC represent better fit.37 Bootstrap likelihood ratio test (BLRT) was used to compare whether the current number of profiles (k) is a better fit model compared to a model with k−1 profiles; a significant test indicates that k-profile model fits the observed data significantly better than the k−1 profile model. Last, entropy represents overall classification quality with values closer to 1 indicating better model classification.38 An optimal profile solution was selected using entropy, posterior profile probabilities, BLRT, and prior theoretical considerations. The second objective was to examine whether the resulting groups differed in terms of treatment mechanisms. For this, Wald’s χ2 difference test using the 3-step approach39 was employed to examine differences in impulsive personality traits, delay discounting, and craving. For the delay discounting task, each participants’ derived discounting parameter (k) was calculated and to correct for positive skewness, logn transformed. A type I error rate of P < .005 was used in the follow-up analyses to adjust for multiple comparisons.
Results
Confirmatory latent profile analysis
The fit statistics for the 5 models can be found in Table 2. The CLPA revealed that a 4-profile solution (Model #1) was the best fit and confirmed the previously identified 4-profile solution. The 4-profile solution was deemed the optimal profile solution due to the following reasons: (1) the highest entropy value; (2) significant BLRT test; (3) the average latent profile probabilities for most likely profile membership was very high, ranging from 0.92 to 0.96 (Table 3); and (4) theoretical considerations (confirming the profiles obtained by Syan et al11).
Table 2.
Model fit statistics for competing models.
| Model fit | 1 | 2 | 3 | 4 | 4 |
|---|---|---|---|---|---|
| Model #1 | Model #2 | ||||
| AIC | 10 122.842 | 9121.039 | 8826.140 | 8505.513 | 8505.195 |
| BIC | 10 168.523 | 9194.128 | 8926.638 | 8569.466 | 8587.421 |
| BIC (sample size adjusted) | 10 136.771 | 9143.324 | 8856.783 | 8525.012 | 8530.266 |
| Entropy | NA | 0.85 | 0.83 | 0.90 | 0.90 |
| BLRT | |||||
| Value | NA | 1013.804 | 306.898 | 643.573 | 642.443 |
| P-value | NA | <.0001 | <.0001 | <.0001 | <.0001 |
| N/profile | C1 = 712 (100%) | C1 = 346 (48.6%) | C1 = 219 (30.8%) | C1 = 229 (32.2%) | C1 = 229 (32.2%) |
| C2 = 366 (51.4%) | C2 = 222 (31.2%) | C2 = 193 (27.1%) | C2 = 195 (27.4%) | ||
| C3 = 271 (38.0%) | C3 = 160 (22.5%) | C3 = 160 (22.5%) | |||
| C4 = 130 (18.3%) | C4 = 128 (18.0%) | ||||
Table 3.
Average latent profile probabilities for most likely latent profile membership N (row) by latent profile C (column).
| C = 1 | C = 2 | C = 3 | C = 4 | |
|---|---|---|---|---|
| N = 1 | 0.950 | 0.001 | 0.037 | 0.012 |
| N = 2 | 0.001 | 0.956 | 0.006 | 0.037 |
| N = 3 | 0.050 | 0.014 | 0.936 | 0.000 |
| N = 4 | 0.013 | 0.063 | 0.000 | 0.924 |
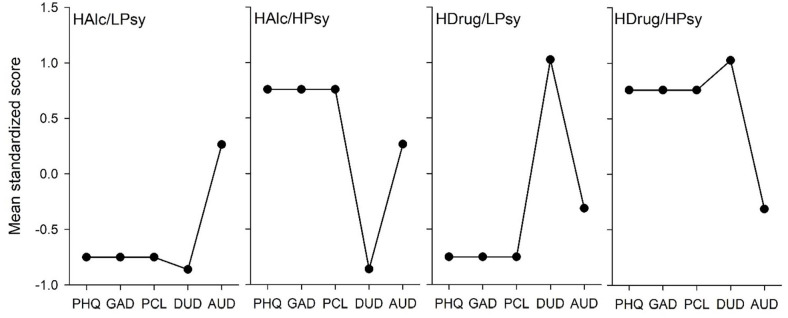
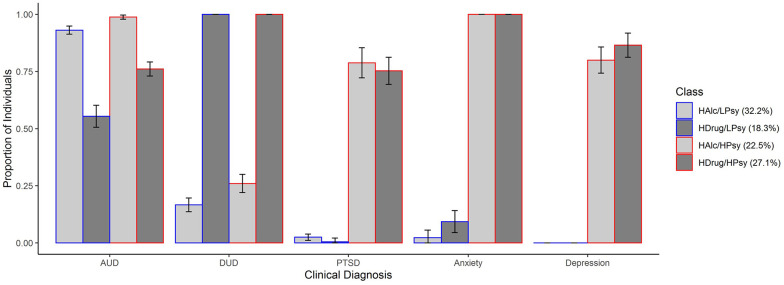
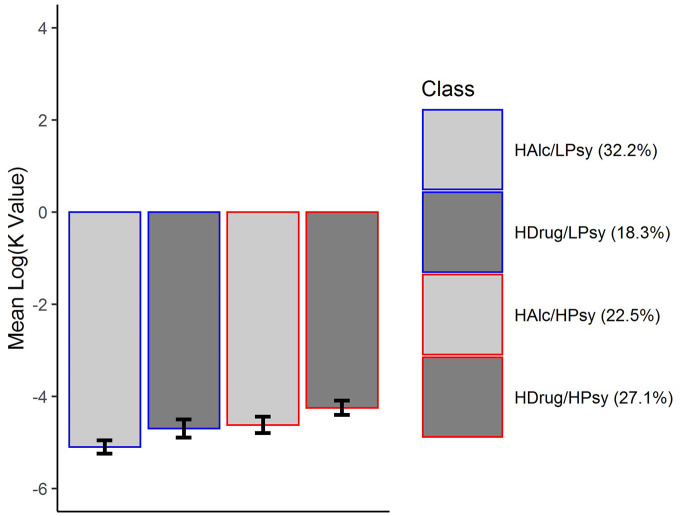
Profile 1 was the largest (32.2%) and was characterized by high alcohol severity, low drug and psychiatric severity (ie, depression, anxiety, and PTSD), therefore was designated as High Alcohol/Low Psychiatric Severity (HALc/LPsy). Profile 2 (27.1%) was characterized by low alcohol severity, high drug, and psychiatric severity, therefore was designated as High Drug/High Psychiatric Severity (HDrug/HPsy). Profile 3 (22.5%) was characterized by high alcohol severity, low drug severity, and high psychiatric severity therefore was designated as High Alcohol/High Psychiatric Severity (HAlc/HPsy). Profile 4 (18.3%) was characterized by low alcohol severity, high drug severity, and low psychiatric severity and therefore was designated as High Drug/Low Psychiatric Severity (HDrug/LPsy). Figure 1 presents the estimated standardized indicator means for this profile solution and Figure 2 presents the proportion of individuals meeting the clinical threshold for each substance use and mental health indicator within each profile and to further validate profile membership. Comparisons of demographic characteristics between latent profiles are in Supplemental Material. Overall, those in the high drug severity group were younger.
Figure 1.
Estimated standard mean (SEM) of latent profile indicators for the High Alcohol/Low Psychiatric Severity (HALc/LPsy; 32.2%), High Drug/High Psychiatric Severity (HDrug/HPsy; 27.1%), High Alcohol/High Psychiatric Severity (HAlc/HPsy; 22.5%), and High Drug/Low Psychiatric Severity (HDrug/LPsy; 18.3%) groups.
Abbreviations: ADHD, adult attention deficit hyperactivity disorder; AUD, alcohol use disorder; DUD, drug use disorder; GAD, generalized anxiety disorder; PCL, post-traumatic stress disorders checklist; PHQ, Patient Health Questionnaire-9; PTSD, post-traumatic stress disorder.
Figure 2.
Proportions of individuals meeting the clinical thresholds for alcohol use disorder, drug use disorder, anxiety disorder, major depressive disorder, and post-traumatic stress disorder.
Abbreviations: AUD, alcohol use disorder; DUD, drug use disorder.
Subgroup differences
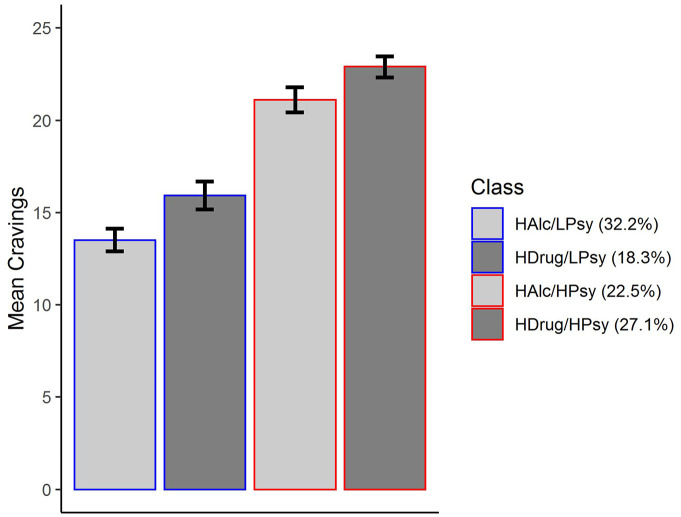
Cravings
The differences in cravings for the latent profiles are in Table 4 and Figure 3. Overall, individuals belonging to the high psychiatric severity subgroups (HDrug/HPsy and HAlc/HPsy) exhibited significantly higher craving than those belonging to the low psychiatric severity groups (HAlc/LPsyc and HDrug/LPsy). No other differences in craving existed between subgroups.
Table 4.
Profile differences based on the impulsivity, delay discounting, and craving.
| HAlc/LPsy vs HDrug/HPsy | HAlc/LPsy vs HAlc/HPsy | HAlc/ LPsy vs HDrug/LPsy | HDrug/HPsy vs HAlc/HPsy | HDrug/HPsy vs HDrug/LPsy | HAlc/HPsy vs HDrug/LPsy | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| χ2 | P | χ2 | P | χ2 | P | χ2 | P | χ2 | P | χ2 | P | |
| Craving | 128.19 | <.001 | 63.21 | <.001 | 5.95 | .02 | 3.97 | .046 | 49.57 | <.001 | 25.75 | <.001 |
| Perseverance (lack) | 20.33 | <.001 | 0.63 | .43 | 2.76 | .10 | 9.79 | .002 | 4.35 | .04 | 0.65 | .42 |
| Premeditation (lack) | 80.21 | <.001 | 15.15 | <.001 | 7.48 | .01 | 17.60 | <.001 | 20.35 | <.001 | 0.64 | .43 |
| Negative urgency | 138.37 | <.001 | 57.34 | <.001 | 6.31 | .01 | 8.86 | .003 | 44.82 | <.001 | 17.47 | <.001 |
| Positive urgency | 141.06 | <.001 | 20.48 | <.001 | 16.69 | <.001 | 34.77 | <.001 | 25.07 | <.001 | 0.01 | .97 |
| Sensation seeking | 16.65 | <.001 | 0.03 | .85 | 17.36 | <.001 | 11.14 | .001 | 0.61 | .44 | 13.46 | <.001 |
| Log MCQ (k) | 16.37 | <.001 | 4.06 | .04 | 2.66 | .10 | 2.38 | .12 | 2.94 | .09 | 0.09 | .76 |
Figure 3.
Mean craving scores across 4 profile solution. Error bars represent ±1 SE of the mean.
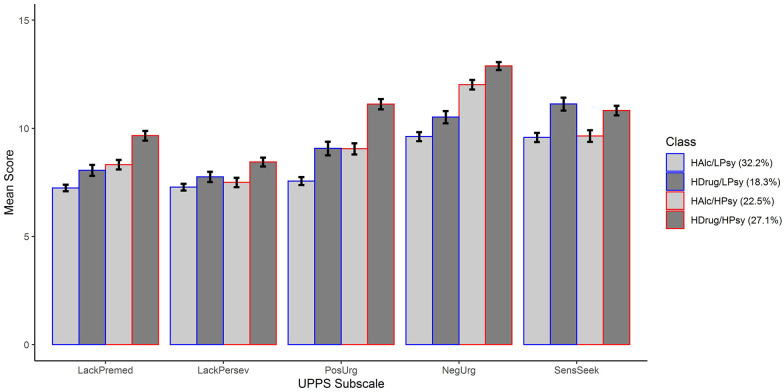
Impulsive personality traits
The differences in impulsivity for the latent profiles are in Table 4 and Figure 4. Overall, there was a common theme that those with high illicit drug use disorder (DUD) severity and comorbid psychiatric severity exhibited the highest levels of impulsivity, whereas those with alcohol use disorder (AUD) and no comorbid psychiatric severity exhibited the lowest levels of impulsivity. The 2 other subgroups tended to fall in between.
Figure 4.
Mean UPPS scores across the 4-profile solution. Error bars represent ±1 SE of the mean.
Abbreviations: LackPersev, lack of perseverance; LackPremed, lack of premeditation; NegUrg, negative urgency; PosUrg, positive urgency; SensSeek, sensation seeking.
Specifically, for negative urgency, individuals belonging to the co-morbid high drug and psychiatric severity (HDrug/HPsy) group exhibited significantly higher urgency than those belonging to the low psychiatric severity groups (HAlc/LPsyc and HDrug/LPsy) and those with high alcohol and psychiatric severity (HAlc/HPsy). Similarly, individuals belonging to the co-morbid alcohol and psychiatric severity (HAlc/HPsy) group exhibited significantly higher urgency than those with low psychiatric severity (HAlc/LPsyc and HDrug/LPsy).
For positive urgency and lack of premeditation, parallel patterns were present. Individuals belonging to the co-morbid high drug and psychiatric severity (HDrug/HPsy) group exhibited significantly higher impulsivity than those belonging to the low psychiatric severity groups (HAlc/LPsy and HDrug/LPsy) and those with co-morbid high alcohol and psychiatric severity (HAlc/HPsy). Additionally, individuals with co-morbid high alcohol and psychiatric severity (HAlc/HPsy) exhibited significantly higher positive urgency and lack of premeditation than those with only high alcohol severity (HAlc/LPsy). For positive urgency those with only high drug severity (HDrug/LPsy) displayed greater urgency than those with only high alcohol severity (HAlc/LPsy).
For lack of perseverance and sensation seeking, parallel patterns were also present. Individuals belonging to the co-morbid high drug and psychiatric severity (HDrug/HPsy) group exhibited significantly higher lack of perseverance and sensation seeking than those belonging to the high alcohol severity groups (HAlc/LPsy and HAlc/HPsy). Furthermore, those with only high drug severity (HDrug/LPsy) displayed higher sensation seeking than those with high alcohol severity (HPsy/HAlc and LPsy/HAlc).
Impulsive choice
The differences in impulsivity for the latent profiles are in Table 4 and Figure 5. For delay discounting, those with co-morbid high drug and psychiatric severity (HDrug/Hpsy) exhibited significantly higher future discounting than those with only high alcohol severity (HAlc/Lpsy), but no other contrasts were significant.
Figure 5.
Mean delayed discounting (log k) across 4 profile solution. Error bars represent ±1 SE of the mean.
Discussion
Given the considerable variability in clinical presentations among individuals with SUDs, the current study sought to characterize this heterogeneity in a large clinical sample at admission to an addiction treatment program. Specifically, the study employed a person-centered approach, confirmatory latent profile analysis, to classify individuals based on substance (alcohol or illicit drug) use severity and psychiatric severity. The resulting subgroups were further characterized with respect to motivational mechanisms. The first major finding was that results replicated the same 4 profiles of substance (drug or alcohol) and psychiatric co-morbidity previously observed.11 Parallel to the earlier report, these profiles were characterized as: High Drug/High Psychiatric Severity (HDrug/HPsy), High Alcohol/High Psychiatric Severity (HAlc/HPsy), High Drug/Low Psychiatric Severity (HDrug/LPsy), and High Alcohol/Low Psychiatric Severity (HALc/LPsy).
The second major finding from this study was that the latent subgroups significantly differed on measures of craving and impulsivity, 2 key SUD motivational mechanisms. For craving, high co-morbid psychiatric severity in conjunction with alcohol or illicit drug use disorder was associated with notably higher scores. These results are consistent with findings that, in those with co-morbid substance and mood/anxiety disorders, craving was a mediator of substance use and co-morbidity was associated with greater craving intensity.40 These findings imply that individuals with SUD and commonly comorbid psychiatric conditions may benefit from interventions that directly target craving management.
With regard to impulsivity, a number of patterns emerged. One common theme was that, of all subgroups, patients endorsing high illicit drug use and high psychiatric severity (HDrug/HPsy) displayed the highest impulsivity across indices. In contrast, those with high alcohol severity and low psychiatric severity (HAlc/LPsy), a group that could be described clinically as uncomplicated AUD (ie, AUD without significant comorbidities), were the least impulsive in general. Overall patterns also revealed that those with high psychiatric severity specifically exhibited a greater lack of premeditation, positive urgency, and negative urgency. Difficulty regulating responses to intense emotions (urgency) has been linked to symptoms of depression and anxiety41 and so perhaps it would logically follow that urgency would be elevated in the high psychiatric severity groups. The findings with respect to lack of premeditation were somewhat surprising as high scores on anxiety and depression indices have found to be negatively associated with lack of premeditation.42 That being said, individuals with co-morbid SUD and PTSD report higher levels of lack of premeditation43; therefore, the presence of PTSD may be driving the observed relationship. Previous research has demonstrated that co-occurring mental health and SUDs lead to a more chronic treatment-resistant trajectory and increased treatment dropout.11,44
It was also notable that those with high drug severity exhibited higher sensation seeking and in some cases urgency (positive or negative) than their high alcohol severity counterparts. Consistently previous findings demonstrate that sensation-seeking was a strong predictor of drug use,45,46 whereas for alcohol use the mean weighted correlation was small to moderate.47 Sensation seeking was also shown to significantly predict DUD 7 years later even after controlling for AUD.48 Another finding in the current study was that those with higher drug severity also exhibited higher sensation seeking than the high psychiatric severity groups. This is not surprising as sensation seeking was found to be either negatively associated with GAD41 or exhibit only small positive correlations with depression and anxiety disorders.49 Overall, results suggest that those with high drug use severity are particularly elevated in terms of sensation seeking, suggesting treatments may need to emphasize alternative reinforcements that provide novel or exciting activities, independent of substance use.
For delay discounting, those with comorbid high drug severity and psychiatric severity (HDrug/HPsy) exhibited higher future discounting than the uncomplicated AUD group (HAlc/LPsy). Previous research suggests that higher delayed discounting is associated with decreased abstinence and treatment response (ie, treatment drop out).11,50,51 Thus, patients exhibiting the profile of high illicit DUD and high comorbid psychiatric severity may selectively benefit from interventions that focus on increasing future time perspectives, such as episodic future thinking.
It was notable that, individuals with high comorbid psychiatric conditions exhibited higher craving and higher positive and negative urgency. Often abused substances can act as maladaptive coping mechanisms. It is possible that in this particular subset of individuals, negative reinforcement, whereby individuals consume psychoactive substances to experience momentary relief from psychological distress, drove behavior.52,53 Perhaps in these individuals who display higher craving and negative urgency, therapy focusing on emotional regulation may be the most beneficial54 or pharmacotherapies such as atomoxetine, a nonstimulant medication used for attention-deficit hyperactivity disorder, has shown to reduce impulsive behavior without abuse potential.55,56
The study must be considered in the context of its strengths and limitations. The large sample size was a strength as it increases power to detect subgroups and the generalizability of the findings, generally increasing confidence in these findings. Another strength of the current study is the use of multiple impulsivity facets (impulsive personality traits and delay discounting), which allows for a high-resolution examination of differences in self-regulation between subgroups. However, the current results were cross-sectional, therefore it was not possible to determine temporality between co-morbidity profile membership, impulsivity, and craving. A further limitation of the current study was that it did not have substantial racial or sex diversity; it is possible that the interaction between the profiles and the motivational mechanisms could have manifested differently among individuals of different racial backgrounds, sexes, and genders. Incidentally, the current sample also included a large proportion of individuals who participated in post-secondary education. As SUD has shown to be associated with a lower education level,57 it is possible these results may not be present in a sample with lower levels of educational attainment. Finally, the comorbidities considered were restricted to just 3 domains, future studies should also consider other psychiatric conditions such as chronic psychosis, personality disorders, and attentional disorders, which have also been associated with problematic substance use.58-60 For these reasons, future studies should expand these methods to samples with higher minority representation and consider other common psychiatric conditions also. In light of the recent COVID-19 pandemic, it would also be interesting to look at more recently ascertained samples, as the COVID-19 pandemic has exacerbated substance use and drug overdoses.61
Nonetheless, the current set of findings provide further evidence of the value of clinical subtyping strategies in the treatment of SUD toward a more personalized approach. The results confirmed a previously observed latent subgroup structure and revealed that the latent cluster reflecting high illicit drug and co-morbid psychiatric severity was associated with the highest craving and impulsivity. This suggests that these individuals may require a more multifaceted approach that directly addresses these mechanisms to achieve optimal outcomes. Ultimately, by characterizing the clinical variability among patients and providing subgroup-specific programing or care paths, treatment programs may result in greater patient engagement in treatment, thereby decreasing treatment dropout, improving the quality of care offered and ultimately optimizing patient outcomes.
Supplemental Material
Supplemental material, sj-docx-1-sat-10.1177_11782218221126977 for Characterizing Clinical Heterogeneity in a Large Inpatient Addiction Treatment Sample: Confirmatory Latent Profile Analysis and Differential Levels of Craving and Impulsivity by Meenu Minhas, Alysha Cooper, Sarah Sousa, Mary Jean Costello and James MacKillop in Substance Abuse: Research and Treatment
Footnotes
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by Homewood Research Institute, the Peter Boris Chair on Addictions Research, and a Canada Research Chair in Translational Addiction Research.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: JM is a principal in Beam Diagnostics, Inc. and a consultant to Clairvoyant Therapeutics, Inc., although no related products or services were involved in this research.
Author Contributions: MM: Methodology, visualization, writing- original draft preparation. AC: Data curation, methodology, visualization, writing-review & editing. SS: Data curation , writing-review & editing. MJC: Conceptualization, funding acquisition, resources, supervision, writing-review & editing. JM: Conceptualization, funding acquisition, resources, supervision, writing-review & editing.
ORCID iDs: Meenu Minhas  https://orcid.org/0000-0001-6741-3940
https://orcid.org/0000-0001-6741-3940
James MacKillop  https://orcid.org/0000-0002-8695-1071
https://orcid.org/0000-0002-8695-1071
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Cartwright WS. Economic costs of drug abuse: financial, cost of illness, and services. J Subst Abuse Treat. 2008;34:224-233. [DOI] [PubMed] [Google Scholar]
- 2. Tracy EM, Laudet AB, Min MO, et al. Prospective patterns and correlates of quality of life among women in substance abuse treatment. Drug Alcohol Depend. 2012;124:242-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Moos RH, Moos BS. Rates and predictors of relapse after natural and treated remission from alcohol use disorders. Addiction. 2006;101:212-222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gossop M, Stewart D, Browne N, Marsden J. Factors associated with abstinence, lapse or relapse to heroin use after residential treatment: protective effect of coping responses. Addiction. 2002;97:1259-1267. [DOI] [PubMed] [Google Scholar]
- 5. Andersson HW, Wenaas M, Nordfjærn T. Relapse after inpatient substance use treatment: a prospective cohort study among users of illicit substances. Addict Behav. 2019;90:222-228. [DOI] [PubMed] [Google Scholar]
- 6. Maisto SA, Pollock NK, Cornelius JR, Lynch KG, Martin CS. Alcohol relapse as a function of relapse definition in a clinical sample of adolescents. Addict Behav. 2003;28:449-459. [DOI] [PubMed] [Google Scholar]
- 7. Witkiewitz K, Masyn KE. Drinking trajectories following an initial lapse. Psychol Addict Behav. 2008;22:157-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Khoury MJ, Galea S. Will precision medicine improve population health? JAMA. 2016;316:1357-1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cho SH, Jeon J, Kim SI. Personalized medicine in breast cancer: a systematic review. J Breast Cancer. 2012;15:265-272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ziegler A, Koch A, Krockenberger K, Grosshennig A. Personalized medicine using DNA biomarkers: a review. Hum Genet. 2012;131:1627-1638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Syan SK, Minhas M, Oshri A, et al. Predictors of premature treatment termination in a large residential addiction medicine program. J Subst Abuse Treat. 2020;117:108077. [DOI] [PubMed] [Google Scholar]
- 12. Mueller TI, Lavori PW, Keller MB, et al. Prognostic effect of the variable course of alcoholism on the 10-year course of depression. Am J Psychiatr. 1994;151:701-706. [DOI] [PubMed] [Google Scholar]
- 13. Hagnell O, Gräsbeck A. Comorbidity of anxiety and depression in the Lundby 25-Year Prospective Study: The pattern of subsequent episodes. In: Maser JD, Cloninger CR, eds. Comorbidity of Mood and Anxiety Disorders. American Psychiatric Association; 1990:139-152. [Google Scholar]
- 14. Beseler CL, Taylor LA, Kraemer DT, Leeman RF. A latent class analysis of DSM-IV alcohol use disorder criteria and binge drinking in undergraduates. Alcohol Clin Exp Res. 2011;36:153-161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Moss HB, Chen CM, Yi HY. Subtypes of alcohol dependence in a nationally representative sample. Drug Alcohol Depend. 2007;91:149-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Stohs ME, Schneekloth TD, Geske JR, Biernacka JM, Karpyak VM. Alcohol craving predicts relapse after residential addiction treatment. Alcohol Alcohol. 2019;54:167-172. [DOI] [PubMed] [Google Scholar]
- 17. Steckler G, Witkiewitz K, Marlatt GA. Relapse and lapse. In: Miller PM, ed. Principles of Addiction. 1st ed. Elsevier Inc.; 2013:125-132. [Google Scholar]
- 18. Pattij T, De Vries TJ. The role of impulsivity in relapse vulnerability. Curr Opin Neurobiol. 2013;23:700-705. [DOI] [PubMed] [Google Scholar]
- 19. Clark DB, Vanyukov M, Cornelius J. Childhood antisocial behavior and adolescent alcohol use disorders. Alcohol Res Health. 2002;26:109-115. [Google Scholar]
- 20. MacKillop J, Weafer J, C Gray J, Oshri A, Palmer A, de Wit H. The latent structure of impulsivity: impulsive choice, impulsive action, and impulsive personality traits. Psychopharmacology. 2016;233:3361-3370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Enticott PG, Ogloff JRP. Elucidation of impulsivity. Aust Psychol. 2006;41:3-14. [Google Scholar]
- 22. Hershberger AR, Um M, Cyders MA. The relationship between the UPPS-P impulsive personality traits and substance use psychotherapy outcomes: a meta-analysis. Drug Alcohol Depend. 2017;178:408-416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Syan SK, González-Roz A, Amlung M, Sweet LH, MacKillop J. Delayed reward discounting as a prognostic factor for smoking cessation treatment outcome: a systematic review. Nicotine Tob Res. 2021;23:1636-1645. [DOI] [PubMed] [Google Scholar]
- 24. American Psychiatric Association. Diagnostic and Statistical Manual of Disorders. 5th ed. American Psychiatric Association; 2013. 10.1176/appi.books.9780890425596 [DOI] [Google Scholar]
- 25. Levitt EE, Syan SK, Sousa S, et al. Optimizing screening for depression, anxiety disorders, and post-traumatic stress disorder in inpatient addiction treatment: a preliminary investigation. Addict Behav. 2021;112:106649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the gad-7. Arch Intern Med. 2006;166:1092-1097. [DOI] [PubMed] [Google Scholar]
- 27. Kroenke K, Spitzer RL, Williams JB, Löwe B. The Patient Health Questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. Gen Hosp Psychiatry. 2010;32:345-359. [DOI] [PubMed] [Google Scholar]
- 28. McDonald SD, Calhoun PS. The diagnostic accuracy of the PTSD checklist: a critical review. Clin Psychol Rev. 2010;30:976-987. [DOI] [PubMed] [Google Scholar]
- 29. Kirby KN, Petry NM, Bickel WK. Heroin addicts have higher discount rates for delayed rewards than non-drug-using controls. J Exp Psychol Gen. 1999;128:78-87. [DOI] [PubMed] [Google Scholar]
- 30. MacKillop J, Tidey JW. Cigarette demand and delayed reward discounting in nicotine-dependent individuals with schizophrenia and controls: an initial study. Psychopharmacology. 2011;216:91-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Cyders MA, Smith GT, Spillane NS, Fischer S, Annus AM, Peterson C. Integration of impulsivity and positive mood to predict risky behavior: development and validation of a measure of positive urgency. Psychol Assess. 2007;19:107-118. [DOI] [PubMed] [Google Scholar]
- 32. Whiteside SP, Lynam DR. The five factor model and impulsivity: using a structural model of personality to understand impulsivity. Pers Individ Dif. 2001;30:669-689. [Google Scholar]
- 33. Costello MJ, Viel C, Li Y, Oshri A, MacKillop J. Psychometric validation of an adaptation of the Penn Alcohol Craving scale to assess aggregated drug craving. Journal of Substance Abuse Treatment. 2020;119:108127. [DOI] [PubMed] [Google Scholar]
- 34. Flannery BA, Volpicelli JR, Pettinati HM. Psychometric properties of the Penn Alcohol Craving scale. Alcohol Clin Exp Res. 1999;23:1289-1295. [PubMed] [Google Scholar]
- 35. Muthén LK, Muthén BO. Mplus Statistical Analysis With Latent Variables User’s Guide (Version 8). Scientific Research Publishing; 2017. Accessed February 12, 2022. https://www.scirp.org/(S(czeh2tfqyw2orz553k1w0r45))/reference/ReferencesPapers.aspx?ReferenceID=2123077 [Google Scholar]
- 36. Finch WH, Bronk KC. Conducting confirmatory latent class analysis using mplus. Struct Equ Modeling. 2011;18:132-151. [Google Scholar]
- 37. Kass RE, Wasserman L. A reference Bayesian test for nested hypotheses and its relationship to the Schwarz criterion. J Am Stat Assoc. 1995;90:928-934. [Google Scholar]
- 38. McCutcheon AL. Basic Concepts and Procedures in Single- and Multiple-Group Latent Class Analysis. Hagenaars. Cambridge University Press; 2002. [Google Scholar]
- 39. Asparouhov T, Muthén B. Auxiliary Variables in Mixture Modeling: A 3-Step Approach Using Mplus. [Google Scholar]
- 40. Fatseas M, Serre F, Swendsen J, Auriacombe M. Effects of anxiety and mood disorders on craving and substance use among patients with substance use disorder: an ecological momentary assessment study. Drug Alcohol Depend. 2018;187:242-248. [DOI] [PubMed] [Google Scholar]
- 41. Miller J, Flory K, Lynam D, Leukefeld C. A test of the four-factor model of impulsivity-related traits. Pers Individ Dif. 2003;34:1403-1418. [Google Scholar]
- 42. Pawluk EJ, Koerner N. A preliminary investigation of impulsivity in generalized anxiety disorder. Pers Individ Dif. 2013;54:732-737. [Google Scholar]
- 43. Weiss NH, Connolly KM, Gratz KL, Tull MT. The role of impulsivity dimensions in the relation between probable posttraumatic stress disorder and aggressive behavior among substance users. J Dual Diagn. 2017;13:109-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Najt P, Fusar-Poli P, Brambilla P. Co-occurring mental and substance abuse disorders: a review on the potential predictors and clinical outcomes. Psychiatry Res. 2011;186:159-164. [DOI] [PubMed] [Google Scholar]
- 45. Arria AM, Caldeira KM, O’Grady KE, Vincent KB, Johnson EP, Wish ED. Nonmedical use of prescription stimulants among college students: associations with attention-deficit-hyperactivity disorder and polydrug use. Pharmacotherapy. 2008;28:156-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Arria AM, Caldeira KM, O’Grady KE, et al. Drug exposure opportunities and use patterns among college students: results of a longitudinal prospective cohort study. Subst Abuse. 2008;29:19-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Hittner JB, Swickert R. Sensation seeking and alcohol use: a meta-analytic review. Addict Behav. 2006;31:1383-1401. [DOI] [PubMed] [Google Scholar]
- 48. Sher KJ, Bartholow BD, Wood MD. Personality and substance use disorders: a prospective study. J Consult Clin Psychol. 2000;68:818-829. [PubMed] [Google Scholar]
- 49. Zermatten A, Van der Linden M. Impulsivity in non-clinical persons with obsessive-compulsive symptoms. Pers Individ Dif. 2008;44:1824-1830. [Google Scholar]
- 50. Black AC, Rosen MI. A money management-based substance use treatment increases valuation of future rewards. Addict Behav. 2011;36:125-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Washio Y, Higgins ST, Heil SH, et al. Delay discounting is associated with treatment response among cocaine-dependent outpatients. Exp Clin Psychopharmacol. 2011;19:243-248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Macdiarmid JI, Hetherington MM. Mood modulation by food: an exploration of affect and cravings in ‘chocolate addicts. Br J Clin Psychol. 1995;34:129-138. [DOI] [PubMed] [Google Scholar]
- 53. Fischer S, Anderson KG, Smith GT. Coping with distress by eating or drinking: role of trait urgency and expectancies. Psychol Addict Behav. 2004;18:269-274. [DOI] [PubMed] [Google Scholar]
- 54. Renna ME, Quintero JM, Fresco DM, Mennin DS. Emotion regulation therapy: a mechanism-targeted treatment for disorders of distress. Front Psychol. 2017;8:98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Upadhyaya HP, Desaiah D, Schuh KJ, et al. A review of the abuse potential assessment of atomoxetine: a nonstimulant medication for attention-deficit/hyperactivity disorder. Psychopharmacology. 2013;226:189-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Ravishankar V, Chowdappa SV, Benegal V, Muralidharan K. The efficacy of atomoxetine in treating adult attention deficit hyperactivity disorder (ADHD): a meta-analysis of controlled trials. Asian J Psychiatr. 2016;24:53-58. [DOI] [PubMed] [Google Scholar]
- 57. Gielen N, Havermans RC, Tekelenburg M, Jansen A. Prevalence of post-traumatic stress disorder among patients with substance use disorder: it is higher than clinicians think it is. Eur J Psychotraumatol. 2012;3:17734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Soyka M, Albus M, Kathmann N, et al. Prevalence of alcohol and drug abuse in schizophrenic inpatients. Eur Arch Psychiatry Clin Neurosci. 1993;242:362-372. [DOI] [PubMed] [Google Scholar]
- 59. Biederman J, Wilens TE, Mick E, Faraone SV, Spencer T. Does attention-deficit hyperactivity disorder impact the developmental course of drug and alcohol abuse and dependence? Biol Psychiatry. 1998;44:269-273. [DOI] [PubMed] [Google Scholar]
- 60. August GJ, Winters KC, Realmuto GM, Fahnhorst T, Botzet A, Lee S. Prospective study of adolescent drug use among community samples of ADHD and Non-ADHD participants. J Am Acad Child Adolesc Psychiatry. 2006;45:824-832. [DOI] [PubMed] [Google Scholar]
- 61. Chacon NC, Walia N, Allen A, et al. Substance use during COVID-19 pandemic: impact on the underserved communities. Discoveries. 2021;9:e141. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-sat-10.1177_11782218221126977 for Characterizing Clinical Heterogeneity in a Large Inpatient Addiction Treatment Sample: Confirmatory Latent Profile Analysis and Differential Levels of Craving and Impulsivity by Meenu Minhas, Alysha Cooper, Sarah Sousa, Mary Jean Costello and James MacKillop in Substance Abuse: Research and Treatment