Abstract
Interstitial pregnancy is a rare type of ectopic pregnancy that commonly results in uterine rupture and life-threatening haemorrhage. Interstitial ectopic pregnancies are associated with a 2–5% mortality rate and a high risk of uterine rupture before 12 weeks of gestation when compared to tubal pregnancy. Due to the thickness and distensibility of the interstitial segment of the Fallopian tube, ectopic pregnancy in this location attains a considerable size before complications arise. Unfortunately, this clinical entity may prove to be a diagnostic challenge, leading to delays in treatment and significant morbidity and mortality in women of reproductive age. Herein, we report a case of a ruptured interstitial ectopic pregnancy occurring at 17 weeks of gestation that was successfully managed with surgical intervention, after proving to be a diagnostic challenge.
Keywords: Interstitial pregnancy, Ectopic pregnancy, Uterine rupture, Cornual wedge resection, Cornuostomy
Abbreviations: CT, Computed tomography; B-hCG, Beta-human chorionic gonadotropin; CBC, Complete blood count
Highlights
-
•
Interstitial ectopic pregnancy is commonly associated with uterine rupture before 12 weeks of gestation.
-
•
Ruptured interstitial ectopic pregnancy is best treated surgically.
-
•
Follow-up should include serial B-hCG measurements to exclude the persistence of trophoblastic tissue.
1. Introduction
Interstitial pregnancy is a rare form of ectopic pregnancy, with a reported incidence of 2–3% [1]. It is defined as the implantation of a blastocyst in the proximal portion of the Fallopian tube that penetrates the uterine myometrium [2]. Due to its thickness and the rich vascular anastomoses between the uterine and ovarian arteries, the interstitial segment of the Fallopian tube possesses a significantly greater capacity to expand and can lead to massive, life-threatening haemorrhage if rupture occurs [3]. The mortality rate associated with ruptured interstitial ectopic pregnancy is approximately 2–5% (3).
Most cases of interstitial ectopic pregnancy rupture occur around 12 weeks of gestation [4]. In this regard, early detection and treatment are pivotal in decreasing the significant maternal morbidity and mortality [4]. However, this clinical entity poses a unique diagnostic challenge, because it is often misdiagnosed as an intrauterine pregnancy as the myometrium becomes significantly distended. This ultimately leads to delays in treatment [3].
Herein, we report a case of a surgically managed ruptured interstitial ectopic pregnancy occurring at 17 weeks of gestation.
2. Case Presentation
A previously healthy nulliparous woman presented at 15 weeks of gestation by dates. She presented with pain in the epigastrium and lower abdomen, a two-day history of difficulty in breathing, and vomiting. No vaginal bleeding was reported. She also gave a history of cigarette and marijuana smoking. An ultrasound scan done about ten days prior to the onset of symptoms showed a live intrauterine gestation of 12 weeks and 6 days. The patient was hemodynamically stable on examination with rebound tenderness in the suprapubic area. Vaginal examination revealed right adnexal tenderness and no cervical excitation.
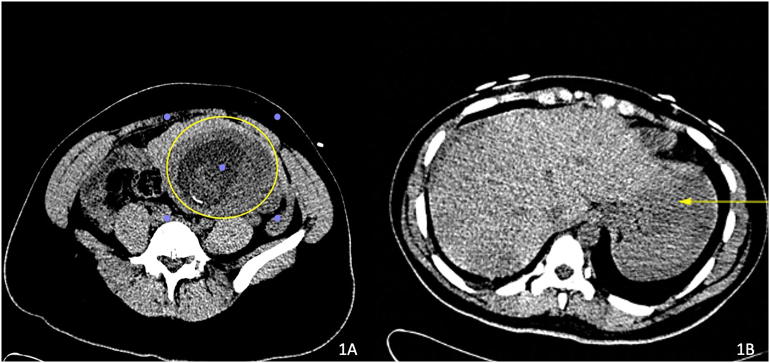
A complete blood count (CBC) showed a haemoglobin level of 9.9 g/dl. Liver and renal function tests were within normal ranges. A mid-stream urine collection revealed no evidence of bacterial growth. An ultrasound scan demonstrated a live intrauterine gestation of about 15 weeks with significant free fluid throughout the abdomen and an impression that heterotopic pregnancy could not be excluded. Serial CBC tests did not reveal any significant drop in the patient's haemoglobin over her two-day inpatient stay. A computed tomography (CT) scan of the abdomen and pelvis was requested due to a suspicion of a non-gynaecological cause for her symptoms. Abdominal CT demonstrated a small quantity of free fluid in the upper abdomen, possibly due to a ruptured corpus luteal cyst and an intrauterine pregnancy; there were no other significant findings (Fig. 1). The patient was treated with intravenous fluids and analgesia. Her pain improved and she was discharged two days after admission.
Fig. 1.
(1A) Intra-uterine gestation (yellow circle) containing fetal components eccentrically located towards the left cornua. (1B) Dense fluid (yellow arrow) within the left sub-diaphragmatic region indicative of acute haemorrhage in keeping with rupture.
Approximately two weeks after the first admission, the patient presented at 17 weeks and 1 day of gestation with a one-day history of lower abdominal pain and vomiting. She was hemodynamically stable, and examination revealed mild tenderness and voluntary guarding. Ultrasound noted a live intrauterine gestation of 17 weeks 5 days and a possible area of haemorrhage measuring 1.3 cm posterior to the placenta. The patient remained haemodynamically stable. Her haemoglobin on admission was 8.8 g/dl while her liver and renal function tests and amylase were within normal ranges. Serial haemoglobin levels were requested after her initial treatment with intravenous fluids, and analgesia and anti-emetics were started. Over the next 8 h, her pain increased, and her haemoglobin level dropped from 8.8 g/dl to 6.6 g/dl. Clinical assessment revealed a distended, tender abdomen with guarding and rebound tenderness. A bedside ultrasound scan revealed a single live intrauterine gestation with significant free intrabdominal fluid. An emergency exploratory laparotomy was scheduled based on these findings.
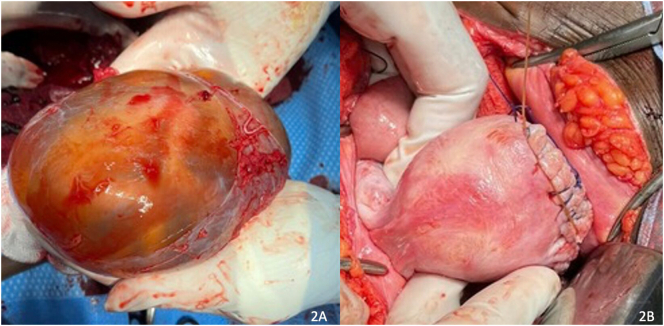
The laparotomy was performed using a midline incision. Intraoperatively, haemoperitoneum was encountered and approximately 2000 ml of blood was evacuated from the abdomen. A ruptured left interstitial ectopic pregnancy of 17 weeks' gestation en-sac was discovered with approximately 8 cm exposed on the left aspect of the uterus (Fig. 2A). Both fallopian tubes and ovaries were grossly normal and preserved. Partial wedge resection and repair of the left cornua were performed (Fig. 2B). An abdominal drain was left in situ.
Fig. 2.
(2A) Ruptured left interstitial ectopic pregnancy of 17 weeks' gestation en-sac discovered during emergency laparotomy. (2B) Partial wedge resection and repair of the left uterine cornua were performed.
Recovery after the operation was unremarkable, and the patient was discharged seven days postoperatively. The patient was followed up with serial B-hCG measurements until levels were undetectable, to exclude the presence of persistent trophoblastic tissue.
3. Discussion
Interstitial pregnancy is typically defined as a pregnancy implanted in the proximal portion of the fallopian tube that penetrates the uterine myometrium [2]. This part of the fallopian tube is approximately 2 cm long, 0.7 mm wide, with a tortuous course, and is surrounded by highly vascular myometrium [2]. The terms interstitial, cornual and angular pregnancy are sometimes used interchangeably. A cornual pregnancy is defined as a pregnancy that has implanted in one horn of a bicornuate uterus, or a rudimentary horn of a unicornuate uterus, or in the lateral half of a septated or partially septated uterus [3]. An angular pregnancy is described as an intrauterine pregnancy in which the embryo is implanted in the lateral angle of the uterine cavity. [5,6] This implantation takes place medial to the utero-tubal junction and round ligament. [5,6]
The incidence of interstitial ectopic pregnancy ranges between 1.0% and 6.3% of all ectopic pregnancies, while the average gestational age at presentation is 7–12 weeks [4]. Interstitial ectopic pregnancies have a rupture rate of approximately 15% and evidence has shown that most rupture before 12 weeks of gestation [4]. The innate ability of the myometrium to distend can allow the gestation to advance well into the second trimester, as seen in the present case. It should also be noted that this region of the uterus is supplied by a rich vascular anastomosis between the uterine and ovarian vessels [3]. As a result, a ruptured cornual/ interstitial pregnancy in the second trimester can lead to massive maternal haemorrhage, hypovolemic shock and even death [7]. Approximately 40% of deaths from ectopic pregnancies result from a cornual rupture [7]. Additionally, due to the difficulty in diagnosing interstitial ectopic pregnancies and the resulting delay in treatment, the mortality rate remains quite high, in the range of 2–2.5% [4]. This rate is approximately 7 times higher than that of other ectopic pregnancies [8]. This patient presented with a massive hemoperitoneum secondary to a left ruptured interstitial pregnancy. This ectopic pregnancy was undiagnosed at up to 17 weeks of gestation, despite prior first- and second-trimester ultrasound scans. Both ultrasound scans, as well as two second-trimester CT scans, indicated an intrauterine gestation, highlighting the diagnostic challenge associated with this clinical entity.
A ruptured ectopic pregnancy may present with a variety of symptoms, which may mimic other conditions. Patients may present with abdominal or pelvic pain, vaginal bleeding, shoulder pain, gastrointestinal symptoms, urinary symptoms, rectal pressure or pain on defecation, dizziness, fainting and syncope [8]. On physical examination, the patient may exhibit peritonism, such as rebound abdominal tenderness and cervical motion tenderness [9]. Additional examination findings include pallor, abdominal distension, an enlarged uterus sometimes beyond the calculated gestational age, and signs of shock such as tachycardia and hypotension [9]. A clinical diagnosis is made based on an evaluation of signs and symptoms, risk factors, and a high index of suspicion. Smoking was the only significant risk factor in our case.
Although routine two-dimensional ultrasonography can be suggestive, interstitial ectopic pregnancies pose a unique diagnostic challenge due to their apparent location. At an advanced gestational age, the gestational sac can be located above the uterine fundus and mistaken for an eccentric intrauterine pregnancy [2]. Ultrasound criteria in the first trimester used to diagnose interstitial ectopic pregnancies include an empty uterus, a gestational sac that measures less than 1 cm from the most lateral edge of the uterine cavity, a thin myometrial lining (less than 5 mm in all planes) surrounding gestational sac and an ‘interstitial line sign’ [10]. The interstitial line sign is a hyperechoic line which extends from the central uterine cavity to the outer margin of the interstitial gestational sac [2]. It has a sensitivity and specificity of 80% and 98% respectively in detecting interstitial ectopic pregnancies [2]. Additionally, 3D ultrasound and MRI can also be utilized to confirm the diagnosis when doubt exists. These imaging modalities were not readily available in the patient's setting. In the event of clinical suspicion of an interstitial pregnancy, a serum B-HCG test should also be carried out to assist with planning management [11]. Serum B-HCG testing does not contribute to the diagnosis of interstitial ectopic pregnancy since, in the case of a viable interstitial pregnancy, the serum B-HCG level may rise over 48 h as it would in normal intrauterine pregnancy [11]. This normal doubling of serum levels supports fetal viability but does not rule out an ectopic pregnancy [11].
Differential diagnoses for an interstitial pregnancy include an angular pregnancy or rudimentary uterine horn/cornual pregnancy [10]. Notably, both these pregnancies are intrauterine. While uterine rupture in the case of an angular pregnancy is extremely rare, there is a much higher risk of rupture in cases of the rudimentary uterine horn/cornual pregnancies [10]. Both ultrasound and intra-operative/anatomical findings can be utilized to distinguish between an interstitial and angular pregnancy.
Management of an interstitial ectopic pregnancy is based on clinical assessment and may be expectant, medical or surgical [12]. In a clinically stable patient with no signs or evidence of rupture and a serum B-HCG level of less than 5000 IU/l, medical management of early interstitial pregnancy is possible with methotrexate [12]. Other criteria must be met to proceed with medical treatment, such as the absence of fetal cardiac activity on ultrasound, absent intrauterine pregnancy, no known methotrexate sensitivity, and a willingness to attend follow-up visits [12]. Non-surgical management was not possible in this case since the patient was hemodynamically unstable, and in the second trimester of pregnancy at a gestation of 17 weeks with a recordable fetal heart rate.
Surgical management options for an interstitial ectopic pregnancy include salpingostomy, cornuostomy, and cornual resection [13]. Laparoscopy is currently the standard approach for surgical management [13]. In applicable cases, a fertility-sparing laparoscopic approach to surgical management that includes removal of the interstitial pregnancy via cornuostomy and resection of the interstitial portion of the tube (cornual resection) should be considered [5]. Laparotomy is generally reserved for patients with hemodynamic compromise or where laparoscopic expertise is insufficient. Hysterectomy may also be considered in the treatment of interstitial pregnancies and is very often an associated complication that may arise if ongoing blood loss occurs and haemostasis cannot be adequately achieved [14]. The rate of hysterectomy in the management of interstitial pregnancies has been reported to be as high as 40% [8]. In our case, an emergency midline laparotomy was undertaken considering the patient's haemodynamic instability, uterine size and the gestational age of the pregnancy. This facilitated exteriorization and repair of the uterus and evacuation of the gestational sac with the fetus found in the abdominal cavity. Haemostasis was achieved by closing the uterine defect in layers using a No. 1 dyed polyglactin suture. Neither vasopressin nor uterine artery ligation was required in this case.
Follow-up of patients treated surgically for a ruptured interstitial pregnancy should include serial B-HCG monitoring to exclude the persistence of trophoblastic tissue, which if untreated can advance to gestational trophoblastic disease [15]. Future pregnancies may be complicated by recurrence of ectopic pregnancy, uterine rupture, morbidly adherent placenta or preterm birth [15]. Most studies have shown that the optimum mode of delivery following a ruptured interstitial pregnancy managed by cornual excision and repair is a caesarean section at 36–37 weeks of gestation [16]. This data has been extrapolated from studies done on the management of pregnancy after extensive myomectomy for uterine fibroids [16]. Multilayered suturing of the myometrium and serosa of the cornual region may prevent future uterine rupture in pregnancy [16]. These risks must be discussed with the patient and close antenatal monitoring of patients with a previous interstitial pregnancy is needed.
In conclusion, interstitial ectopic pregnancy is a rare subtype of tubal pregnancy that poses a unique diagnostic challenge, resulting in diagnostic delays and significant maternal morbidity and mortality. Interstitial ectopic pregnancies are associated with a high risk of uterine rupture and life-threatening haemorrhage. Transvaginal ultrasonography with serial serum B-hCG measurements remains the mainstay of diagnosis. This case highlights the importance of maintaining a high index of suspicion in patients presenting with vague lower abdominal symptoms in early pregnancy so that prompt management protocols can be implemented, to minimise morbidity associated with an interstitial ectopic pregnancy.
Contributors
Vishal Bahall conceived, supervised and drafted the manuscript.
Wendel Cozier was involved in performing the surgical procedure (partial wedge resection and repair of the left cornua) and contributed to drafting the manuscript.
Sarah-Ann Elias assisted in drafting the manuscript.
Petal Latchman assisted in drafting the manuscript.
Steven Sankar was involved in patient care and reporting of images, and contributed to drafting the manuscript.
All authors approved the final submitted manuscript.
Funding
No funding from an external source supported the publication of this case report.
Patient consent
Written informed consent was obtained from the patient for the publication of this case report and accompanying images.
Provenance and peer review
This article was not commissioned and was peer reviewed.
Declaration of Competing Interest
The authors declare that they have no conflict of interest regarding the publication of this case report.
Acknowledgements
The authors would like to thank all anonymous reviewers and editors for their helpful suggestions for the improvement of this paper.
References
- 1.Kalidindi M., Shahid A., Odejinmi F. Expect the unexpected: the dilemmas in the diagnosis and management of interstitial ectopic pregnancy—case report and literature review. Gynecol. Minimal. Invas. Therap. 2016;5(1):35–37. [Google Scholar]
- 2.Rastogi R., Meena G.L., Rastogi N., Rastogi V. J Hum Reprod Sci.; 2008. Interstitial ectopic pregnancy: A rare and difficult clinicosonographic diagnosis. (0974–1208 (Print)) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Corioni S., Perelli F., Bianchi C., Cozzolino M., Maggio L., Masini G., et al. J Res Med Sci.; 2015. Interstitial pregnancy treated with a single-dose of systemic methotrexate: A successful management. (1735–1995 (Print)) [PMC free article] [PubMed] [Google Scholar]
- 4.S M S, T C, Singh N.N., Singh N.B., T S N . J Clin Diagn Res.; 2013. A ruputured left cornual pregnancy: a case report. (2249-782X (Print)) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arleo Kagan E., Cornual DeFilippis M. 2014. Interstitial and angular pregnancies: clarifying the terms and a review of the literature. [DOI] [PubMed] [Google Scholar]
- 6.Finlinson A.R., Bollig K.J., Schust D. Differentiating pregnancies near the uterotubal junction (angular, cornual and interstitial): a review and recommendations. Fertil. Res. Pract. 2020;6:1–7. doi: 10.1186/s40738-020-00077-0. Article no 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Soriano D., Vicus D., Mashiach R., Schiff E., Seidman D., Goldenberg M. Fertil Steril; 2008. Laparoscopic treatment of cornual pregnancy: a series of 20 consecutive cases. (1556–5653 (Electronic)) [DOI] [PubMed] [Google Scholar]
- 8.Ahlschlager L.M., Mysona D., Beckham A.J. The elusive diagnosis and emergent management of a late-presenting ruptured interstitial pregnancy: a case report. BMC Pregnancy Childbirth. 2021;21(1):553. doi: 10.1186/s12884-021-04026-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Boujida S., M’Hamdi O., Mahfoud H., Baydada A., Kharbach A. Ann Med Surg (Lond).; 2022. Ruptured interstitial ectopic pregnancy: A case report and review of the literature. (2049–0801 (Print)) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Finlinson A.R., Bollig K.J., Schust D.J. Differentiating pregnancies near the uterotubal junction (angular, cornual, and interstitial): a review and recommendations. Fertil. Res. Pract. 2020;6(1):8. doi: 10.1186/s40738-020-00077-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kingsbury B., Sam D., Jeyasudha R., Thomas E., Rebekah G., Lionel J. J Family Med Prim Care.; 2020. Ectopic pregnancies: Catch them early, treat them wisely! (2249–4863 (Print)) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stabile G.A.-O., Romano F., Buonomo F., Zinicola G., Ricci G.A.-O. Biomed Res Int.; 2020. Conservative Treatment of Interstitial Ectopic Pregnancy with the Combination of Mifepristone and Methotrexate: Our Experience and Review of the Literature. (2314–6141 (Electronic)) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moawad N., Dayaratna S., Mahajan S. JSLS; 2009. Mini-cornual excision: a simple stepwise laparoscopic technique for the treatment of cornual pregnancy. (1086–8089 (Print)) [PMC free article] [PubMed] [Google Scholar]
- 14.Faraj R., Steel M. Management of cornual (interstitial) pregnancy. Obstet Gynecol. 2007;9(4):249–255. [Google Scholar]
- 15.Al-Maghrabi H.A.-O., Saleh D., Meliti A.A.-O. Case Rep Obstet Gynecol.; 2019. Gestational Trophoblastic Disease Presents as an Ectopic Tubal Pregnancy, a Rare Entity. (2090–6684 (Print)) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tang S., Du T., Huang J., Ye H., Zhao M., Lin J., et al. Effect of previous wedge resection for interstitial pregnancy on pregnancy and neonatal outcomes following frozen-thawed embryo transfer (FET) cycles of IVF/ICSI: a retrospective study. Reprod. Biol. Endocrinol. 2022;20(1):23. doi: 10.1186/s12958-022-00896-4. [DOI] [PMC free article] [PubMed] [Google Scholar]