Abstract
Background
Nonadherence to diet and medical therapies in heart failure (HF) contributes to poor HF outcomes. Mobile apps may be a promising way to improve adherence because they increase knowledge and behavior change via education and monitoring. Well-designed apps with input from health care providers (HCPs) can lead to successful adoption of such apps in practice. However, little is known about HCPs’ perspectives on the use of mobile apps to support HF management.
Objective
The aim of this study is to determine HCPs’ perspectives (needs, motivations, and challenges) on the use of mobile apps to support patients with HF management.
Methods
A qualitative descriptive study using one-on-one semistructured interviews, informed by the diffusion of innovation theory, was conducted among HF HCPs, including cardiologists, nurses, and nurse practitioners. Transcripts were independently coded by 2 researchers and analyzed using content analysis.
Results
The 21 HCPs (cardiologists: n=8, 38%; nurses: n=6, 29%; and nurse practitioners: n=7, 33%) identified challenges and opportunities for app adoption across 5 themes: participant-perceived factors that affect app adoption—these include patient age, technology savviness, technology access, and ease of use; improved delivery of care—apps can support remote care; collect, share, and assess health information; identify adverse events; prevent hospitalizations; and limit clinic visits; facilitating patient engagement in care—apps can provide feedback and reinforcement, facilitate connection and communication between patients and their HCPs, support monitoring, and track self-care; providing patient support through education—apps can provide HF-related information (ie, diet and medications); and participant views on app features for their patients—HCPs felt that useful apps would have reminders and alarms and participative elements (gamification, food scanner, and quizzes).
Conclusions
HCPs had positive views on the use of mobile apps to support patients with HF management. These findings can inform effective development and implementation strategies of HF management apps in clinical practice.
Keywords: heart failure, mobile health, mHealth, eHealth, mobile apps, adherence, self-management, mobile phone
Introduction
Background
Heart failure (HF) is a progressive clinical syndrome in which abnormalities in heart function, marked by reduced cardiac output and congestion [1], often result in periods of acute decompensation. HF is managed through pharmacological therapies, accompanied by self-care recommendations that emphasize dietary modification and daily weight and symptom monitoring [1,2]. However, patient adherence to these treatments can be challenging, with medication and dietary nonadherence rates being 50% and 22% to 50%, respectively [3-7]. Nonadherence is associated with increased risk of HF hospitalizations and mortality, which contribute to the growing economic burden of HF [8].
Currently, a significant amount of behavioral and nutritional counseling occurs in the clinical setting, with the counseling provided by health care providers (HCPs), including physicians and nurses, with consultation from pharmacists and registered dietitians as needed, to support patients with HF management and adherence [9-12]. The delivery of this education can be limited by HCPs’ lack of knowledge, time, and compensation [13]. In addition, patients with HF, especially those living in rural and remote regions, may not have access to these professionals, and even if they do, HCPs are unable to monitor the patients and provide feedback in real time and on day-to-day progress. Given the clinical relevance of treatment adherence to HF outcomes and the real-life challenges that patients may experience, it is not surprising that initiatives to support adherence are highlighted as a priority action area by the American Heart Association [14].
Mobile health (mHealth) technologies present opportunities to improve adherence and support HF management. Several randomized controlled trials examining the impact of mHealth-based interventions in HF have reported significant improvements in cardiovascular and all-cause mortality, New York Heart Association class, left ventricular ejection fraction, quality of life, and physical functioning [15-18]. mHealth-based interventions improve outcomes by supporting the delivery and continuity of care in HF by relaying health information, monitoring patient symptoms outside of clinical setting, and supporting patient education [19,20]. Modern mHealth tools such as mobile apps are also able to provide real-time feedback in a way that is less resource intensive than other eHealth interventions (eg, telemonitoring) [19,20]. Multiple systematic reviews have reported that mHealth apps for HF improve engagement in self-care behaviors as well as patient self-efficacy, self-confidence, and communication with HCPs, offering a potential cost-effective solution to support patients with HF treatment adherence and self-management [21-24].
Objectives
Among existing apps available to support HF management, few are considered high quality based on content, features, and functionality when assessed against established rating scales [24,25]. In fact, it has been suggested that many apps require redesign because of a lack of appropriate features to engage patients in self-care and failure to meet the needs and motivations of the population with HF [24]. In contrast, well-designed mHealth apps that integrate input from both patients and HCPs are more likely to also meet HCPs’ needs, leading to overall better acceptability and HCPs’ willingness to adopt and recommend such tools to their patients [26]. Moreover, HCPs have a unique understanding of what is required to support patients in HF management [27]. A few studies have explored HCPs’ perceptions on the use of technology-based interventions for HF management [28-30]. However, these studies have only focused on mobile phone–based interventions for wireless Bluetooth-enabled remote monitoring of patient symptoms, SMS text messaging, and sensor-focused mHealth apps and do not capture HCPs’ perceptions on mHealth interventions using more advanced applications, which have unique opportunities and challenges of their own. Determining HCPs’ perspectives and attitudes on the use of mobile apps for HF management can inform the effective design of such apps, including their features and content, increasing the likelihood of app adoption in this population. Therefore, the objective of this qualitative descriptive study was to determine HCPs’ perspectives (needs, motivations, and challenges) on the use of mHealth apps to support patients with HF management. For the purposes of this study, HCPs included cardiologists, nurses, and nurse practitioners.
Methods
Study Design and Research Team
This study followed a qualitative descriptive design. Rooted in naturalist inquiry, this design allows for meaningful summarization of the data in everyday terms and has been used to inform development of health interventions [31]. The study followed the COREQ (Consolidated Criteria for Reporting Qualitative Research) guidelines for qualitative research [32]. The research team included a PhD graduate student (BS); 2 faculty members with expertise in HF, digital intervention research, and qualitative methods (JA and ML); an HF cardiologist (SM); and a social scientist with qualitative expertise (MS). There was no prior relationship between the interviewer and the participants.
Ethics Approval
The study was approved by the research ethics board of Ontario Tech University (14882), and informed consent was obtained from all participants.
Study Participants and Recruitment
Purposive sampling was used to recruit cardiologists, nurses, and nurse practitioners who work in outpatient HF programs in Canada. Registered dietitians and pharmacists were excluded because they are not the primary point of care for patients with HF. Recruitment was conducted with advertisements and emails circulated by the Canadian Heart Failure Society as well as with a snowball sampling approach. Eligible participants were invited to participate via an email invitation. Participants completed a web-based consent form. Participants were compensated CAD $20 (US $15) in the form of a gift card for their participation in the study.
Data Collection
One-on-one 15-minute telephone interviews were conducted in English with participants between February 4, 2019, and June 4, 2020. Telephone interviews allow for flexibility and convenience for both researchers and participants and is an acceptable method for qualitative data collection [33,34]. The interviewer (BS) recorded field notes during and after each interview, which included reflective memos on unique ideas and insights as well as their interview experience. Participants were sent the interview questions before the interview.
The interviews were directed by a semistructured interview guide (Multimedia Appendix 1) that consisted of 8 open-ended questions that reflected the aim of the study. These questions were supplemented with research probes and paraphrasing to generate further clarification of participant responses and promote discussion. The interview guide was developed by expert consensus and informed by the diffusion of innovation theory [35], which is widely used in guiding the development and evaluation of innovations. The interview questions reflected the five main factors that influence the adoption of an innovation: (1) relative advantage refers to the degree to which an innovation is seen as better than standard care, (2) compatibility refers to how consistent the innovation is with the needs and values of the adopter (eg, patients), (3) complexity refers to the difficulty of the innovation, (4) trialability refers to the extent to which the innovation can be tested before use by users, and (5) observability refers to the extent to which the innovation provides results. The interview guide was reviewed and approved by members of the research team to ensure clarity and appropriateness of questions and probes. The guide was pilot-tested with an HF cardiologist external to the research team.
The interviews were audio recorded using a voice recorder, and the recordings were manually transcribed verbatim (BS and SG). Pseudonyms were used in the transcripts to protect the identity and maintain anonymity of the participants. All identifiable information was removed from the transcripts. The verbatim transcripts were verified by a research assistant by comparing the transcripts with the audio recordings to ensure accuracy.
Before the telephone interview, participants completed a short web-based questionnaire that asked about their views on using technology for managing HF as well as barriers related to supporting patients’ diet and medication adherence. The questions were informed by what is known in the literature about barriers and facilitators related to medication and dietary adherence. The questionnaire consisted of 10 Likert scale–style questions, with answer choices ranging from 0 to 3 (I don’t know, agree, neutral, and disagree). Sociodemographic information, including age, sex, years of practice, and professional role, was also collected. The questionnaire was validated by the research team for face and content validity.
Data Analysis
Preceding analyses, all participants received their transcript for member checking, as described by Lincoln and Guba [36], to approve the verbatim transcripts and verify accuracy. Only minor amendments were received and integrated into the final transcripts, ensuring credibility of data. To prepare for data analysis, the audio recording, transcript, and field notes of each interview were reviewed multiple times. The transcripts were imported into NVivo software (version 12.0; QSR International), which supported the content analysis. The transcripts were inductively coded by 2 independent researchers (BS and MS). This was followed by comparison of coding, collaborative discussion of codes (for intercoder agreement), expansion of codes to capture subcodes, and ultimately the grouping of codes into common themes. For the purpose of this study, a theme reflected participant accounts related to their views (needs, motivations, and challenges) regarding the use of mobile apps for HF management. Themes were reviewed and finalized in discussion with a qualitative expert on the research team (ML) as well as the principal investigator (JA).
The questionnaire data were summarized using descriptive statistics. Categorical variables were presented as frequencies and percentages, and continuous variables were described as means and SDs.
Results
Overview
A total of 21 HCPs (cardiologists: n=8, 38%; nurses: n=6, 29%; and nurse practitioners: n=7, 33%) participated. The mean age of the participants was 42.9 (SD 8.6) years, and 81% (17/21) were women. Participants’ years of practice as HCPs included 1 to 5 years (1/21, 5%), 6 to 10 years (6/21, 29%), 11 to 15 years (5/21, 24%), 16 to 20 years (1/21, 5%), and >20 years (8/21, 38%).
The questionnaire data indicated that the HCPs agreed that technology can be effective in helping patients to adhere to their prescribed medications (19/21, 90%) and dietary requirements (16/21, 76%; Figure 1). Barriers to supporting patients’ diet and medication adherence included medication cost and financial burden (16/21, 76%), difficulties with reading food labels and identifying low-sodium products (11/21, 52%), and patients not being truthful about taking their medications (14/21, 67%) or their dietary intake (17/21, 81%; Figures 2 and 3).
Figure 1.
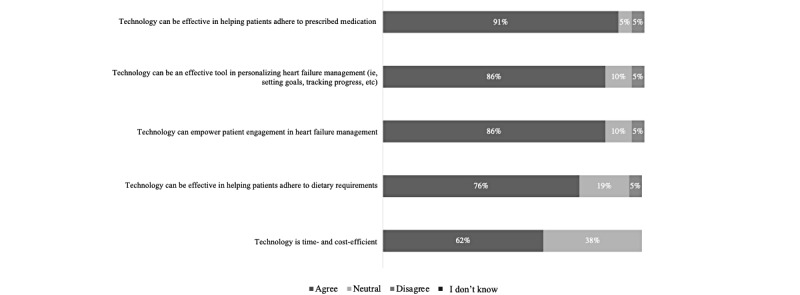
Health care providers’ views on the use of technology to aid in managing heart failure (N=21).
Figure 2.
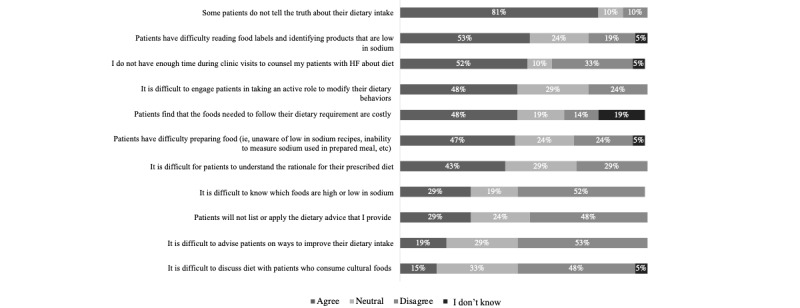
Barriers faced by health care providers when supporting patients’ dietary adherence (N=21).
Figure 3.
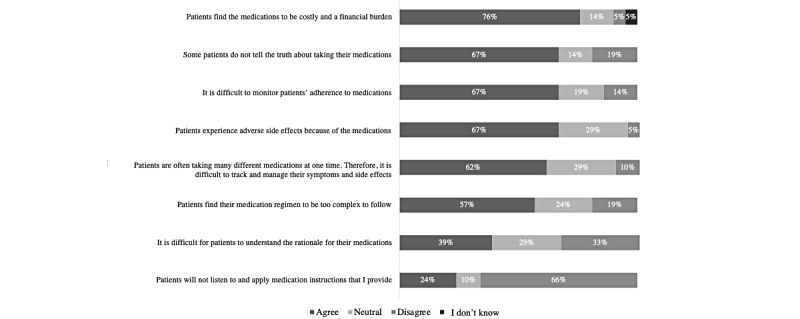
Barriers faced by health care providers when supporting patients’ medication adherence (N=21).
Five themes were identified from the telephone interviews that reflect participant perspectives on the use of mobile apps for HF management. These included participant-perceived factors that affect app adoption, improved delivery of care, facilitating patient engagement in care, providing patient support through education, and participant views on app features for their patients.
Participant-Perceived Factors That Affect App Adoption
Patient-Related Factors Affecting App Adoption
Participants described several factors that may affect the use of mobile apps by patients with HF, including patient age, access to mobile phones and internet, how technology savvy patients are, physical and cognitive function of patients, and their level of engagement in HF self-management. Participants viewed apps as being more favorable among “younger” patients with HF, suggesting that the majority of patients with HF were older adults (aged >70 years), and thus they would be unfamiliar with using technology. One participant stated as follows:
I don’t like to peg people into categories, but certainly it seems like the younger crowd for which is like 50s, 60s, they might be the ones more interested in using [apps]. We certainly have a high number of elderly, or frail elderly in our clinic so a lot of them aren’t, you know, on email or internet or things like that.
Participant 9
In addition, characteristics associated with aging, such as decline in physical and cognitive functioning, were considered barriers to app use. There was also concern that patients may lack access to mobile phones and internet needed to use apps, particularly in northern and rural communities. Participants expressed that some patients may lack motor function, have arthritis, be missing digits, have difficulty with their vision, or experience cognitive challenges, which would impede their ability to use apps. Participants also identified that adoption of apps required a certain level of motivation from patients and that those who are highly engaged in HF self-management would likely benefit from using such tools.
HCP-Related Factors Affecting App Adoption
HCPs’ buy-in and familiarity with HF apps as well as level of time, compensation, and workload burden for HCPs were perceived as factors that may affect their app use. Although some of the participants had experience using mobile apps in their clinical practice to monitor patient care, the majority were unaware of credible HF management apps to recommend to their patients. Moreover, buy-in from HCPs and clinical staff may be a challenge to app adoption in the clinical setting. A participant observed as follows:
I don’t know how we’ve gotten to this place but so many people are, they are negative nellies. They are not willing to try new things, because “oh, it’s not going to work,” “oh I’ve seen this, it’s not going to work.” How do we know unless we try? It’s something new. Technology is where it’s at, we all know that. So, I think the buy-in from staff is going to be part of the challenge.
Participant 11
Participants indicated that the time and workload required to teach patients how to use the app, interacting with patients through an app interface, and interpreting patient data from an app may interfere with app use. If app use was time consuming, it was felt that a lack of compensation for their time can prevent HCPs from using apps in their clinical practice. One participant stated as follows:
If I need to spend hours in each clinic appointment educating the patient on how to use it [app], it’s going to fall at the first hurdle. I don’t have the time; I don’t have the money.
Participant 13
App-Related Factors Affecting App Adoption
The perceived app-related factors affecting adoption included information provided by apps, user-friendliness of apps, level of technical support and guidance provided for app use, app availability across multiple devices, level of privacy and protection for patient information, and integration into clinical practice and health care system as well as language and costs associated with app use. Participants felt that apps providing personalized and tailored information to patients were valuable compared with apps presenting generalized information about HF. Apps also need to provide simple, practical, and meaningful information as well as be easy to use, simple, user-friendly, and compatible with different types of devices and platforms (smartphones, tablet devices, and web). Moreover, technical support and reasonable support and guidance on how to navigate the app should be provided. Participants felt that HF apps need to be encrypted, safe, and secure to ensure confidentiality of personal information. In addition, it would be beneficial to have apps be integrated into practice and the health care system, including the hospital, care team, and electronic medical records. A participant made the following observation:
Now to use it [app], our whole team would have to adopt it. Meaning they would have to have a consensus on its use and then if we wanted to have data sent to us then obviously, that would be a whole system, how do you receive this information, how do you use this information, what’s the protocol for receiving it and then acting on it, type of thing.
Participant 6
By contrast, some factors were identified as barriers to app use. Participants felt that language can be a barrier because not all patients with HF may be comfortable using apps that are primarily in English. Costs involved in downloading and using apps were also seen as a barrier. In addition, participants were concerned that the use of technologies such as apps may promote the use of appointments via telephone or videoconference, which they feel can be challenging because of the lack of in-person interaction.
Improved Delivery of Care
Most participants felt that apps may positively affect their ability to provide remote and timely care, including remote monitoring, titration of medications, and check-ups, all of which may allow for timely delivery of care. It was also viewed that by providing opportunities for remote care, apps could limit clinic visits and save patient time and resources, including travel and parking costs associated with clinic visits. It was expressed that sometimes patients face difficulties with scheduling and clinic appointment travel; thus, apps may make care more accessible. One HCP provided an example of how an app supported remote care in their practice:
Well for example I have a specific patient that is on [name of app]...cardiac failure that is related to myeloma, but [patient] is very sick and is on chemotherapy so by using the app I have been able to keep [patient] at home without coming to hospital. I don’t know how much time they have, but the family is really happy that [patient] stays at home. And we have been asking for weight changes very quickly to try to keep them at home.
Participant 1
Apps may also provide additional benefits when compared with traditional telehealth services. A participant expressed the following view:
The benefit is for sure we have maybe more information than the usual phone call. So, if you can incorporate things that the patient can, let’s say, send a picture or sharing how they look like. So, we have that visual, you know, presentation in front of you.
Participant 7
In addition, they can potentially collect and assess real-time health information and prevent adverse events. Participants felt that apps can collect real-time and day-to-day data on HF signs and symptoms that can be shared with HCPs, as needed. Specific data considered important by participants were weight, blood pressure, common HF symptoms (ie, swelling and shortness of breath), step count, and daily sodium and fluid intake. Apps could allow HCPs to gauge trends in these data to better assess the patient. An HCP stated as follows:
It’s also helpful to have the data when the patient comes to clinic because we can clearly sort of go back and say, “hey you know, this is what trend of this vital sign has been” and that’s helpful information when you’re seeing someone.
Participant 3
Participants felt that, ultimately, by being able to collect, share, and assess health information remotely, apps have the potential to identify worsening clinical signs and symptoms and precipitating factors for adverse clinical events, allowing for early intervention and the prevention of HF hospitalizations. A participant made the following observation:
The device would let the attending physicians know when the patient was not doing that well...maybe some complications could be caught on time before they got really sick.
Participant 17
In addition, it was perceived that apps that use artificial intelligence could alert HCPs of patients who require immediate care. One HCP stated as follows:
...patient-reported symptoms that are algorithmically determined at which point they create an alert...so you know worsening clinical symptoms create an alert that alert is then sent to a nurse or physician.
Participant 15
Facilitating Patient Engagement in Care
Participants felt that apps can be used to foster independence, awareness, and confidence among patients because they can support establishment of health goals and provide feedback and reinforcement. Apps could encourage patients to take “ownership of their disease” and “empower” them to engage in self-care activities. In addition, they can allow patients to have awareness of their disease and health status. It was expressed that apps can support patients in goal setting and “guide them to make SMART goals” (ie, goals that are specific, measurable, achievable, relevant, and timely), as well as challenge patients in improving their health behaviors over time. A participant noted as follows:
I think it’s a great example that maybe you set a goal, okay so yesterday I can walk about a block before I’m getting shortness of breath maybe today let me try to walk one and a quarter block and see how I feel something like that.
Participant 18
Moreover, participants felt that apps present an opportunity for patients to “have ongoing reinforcement of the heart failure education of the diet and medication that are recommended for them.” Apps can also generate automated feedback for patients based on their HF symptoms and specific medication and dietary intake behaviors that would otherwise be difficult to provide during clinic visits. Participants made the following observations:
...so that way they would have feedback, you know, “this week you actually missed your medication three times.” Perhaps prompting with a screen that says “you require a compliance of at least 90% to see effectiveness in this goal, this goal and this goal.” So, kind of providing them with some research feedback.
Participant 21
...you can say did you know that the choices, the ones you made are more higher in salt or you know you can give them more feedback, that structure is hard to do one on one in person visit.
Participant 19
Several participants thought that app adoption for HF management can facilitate connection and communication between patients and their HCPs. This could include the incorporation of a messaging feature for patients and HCPs, which can serve as a more efficient communication method than traditional telephone calls. An HCP commented as follows:
...having the possibility of communicating with patients outside of phone call could be very helpful, a way to just send message that could be faster than having us to call back to answer questions or to confirm an information.
Participant 4
This type of communication may allow patients to write down questions in real time and engage in back-to-back communication with their HCPs, which can lead to more open conversations about their care. A participant observed as follows:
Also, it may allow patients to kind of write down questions or they may be more open to discussing, what their intents are in the written form as opposed to face-to-face and they don’t have to think about it. So, it’s that extra time, it’s not done by, for instance, where they have messages that go back and forth or what have you. It can allow them to kind of open up more, to think more about what they want to ask, and what kind of care do they want to have in the future.
Participant 5
One of the frequently mentioned opportunities for the use of HF mobile apps was that they can help patients monitor and track self-care activities and indicators. Participants felt that it may be beneficial if HF apps allowed patients to track their diet, including sodium and fluid intake, through manually entering food intake and scanning food labels. Participants stated as follows:
I think what would be very valuable is a way to actually track, the way that um the way that weight loss apps track you sort of have an ongoing diary of how much you eat and then it spits out your calories similarly, I think having um an ongoing tracking system of fluid intake would be particularly useful.
Participant 15
So, I think putting in milligrams of sodium is a nice way in some kind of visual way where a lot of what looks like a battery and it’s full at the beginning of the day and that represents your 2000 mg and then you have breakfast and you can sort of calculate it, depending on how good or bad you are at that, and then it’s going to deplete some of that energy or sodium allowance per se.
Participant 6
In addition to tracking dietary intake, participants also saw opportunity for an app to track patients’ physical activity (ie, step count) as well as patient symptoms (ie, daily weight, blood pressure, and pulse). It was suggested that an app for HF can be linked directly to other apps that track symptoms, diet, or exercise (eg, MyFitnessPal), allowing patients to have all information in “one spot.”
Providing Patient Support Through Education
Apps were viewed as a medium for patients to obtain access to resources. This included information about HF, HF guidelines and symptoms, and mental health support. Some of the participants felt that HF management resources available on the web (eg, the Heart and Stroke Foundation of Canada website) would be beneficial to patients in an app form because apps can present information in a more engaging way through visuals, interactions, and videos. One participant saw a unique opportunity for apps to tailor patient resources based on their geographical location:
I was thinking about an app and how great it would be if that app you could plug in your geographic location and it would give you local access or national online access to information on any types of events, webinars, support groups.
Participant 6
A commonly perceived benefit to using an app for HF management was the potential for apps to facilitate nutrition-related education. As sodium restriction was a focal point of dietary education for HF management, it was felt that an app could teach patients about sodium intake recommendations, common dietary sources of sodium, and the sodium content in foods. Dietary potassium was also identified as an important part of education for patients with HF. Participants made the following observations:
Salt restriction, giving them an idea of you know how much salt is recommended and then an example of what you know I always give this example to my patients the limitation is 2000 mg a day for the cardiac and a dill pickle is 550 so a quarter of the salt intake is in one dill pickle. So, it gives them real perspective.
Participant 16
...kind of a dictionary where they could enter the name of food and see how much sodium...so they could see that oh well a bag of pretzel is 2 grams of salt and realize oh no I should not eat that because of the salt in it.
Participant 4
...foods that would be high in potassium, so sometimes our patients have higher potassium that limits our ability to get them on guideline directed medical therapy or up-titrated and so knowing what foods were higher in potassium might be helpful because if we said to the patient “we want you to eat foods that are lower in potassium,” they always want to know what those are.
Participant 3
Apps could also support food skills development such as reading food labels on packaged foods, food preparation, and “culinary literacy.” It was also identified by several participants that apps can have information to guide patients about foods to consume versus foods to avoid, as well as provide dietary tips (eg, managing sodium intake on cheat days and managing dry mouth), acceptable low-sodium substitutions, and low-sodium recipes:
But if there would be little tips and tricks on things, if you have to buy canned green beans just rinse them off. Get rid of a lot of that sodium. Have tips like that on there...I think would be very helpful for people.
Participant 11
Providing access to medication-related information was another perceived benefit of apps. Multiple participants identified that patients may be better adherent to their HF medications if they are aware of the purpose for which the medications are prescribed and the “risk of skipping a couple of doses”:
...you know, in a much more basic level, why you are taking these drugs and why you are not to stop your ramipril just because your systolic only 100, you feel fine and you’re not dizzy and you keep taking it because it’s not for blood pressure...so having a bit of content in the background of why these medications are helpful, I think would be a little bit important for content inclusion for an app.
Participant 6
...benefits of the medication, like a little blurb on why it is important that you take this medication, and all the ACE [angiotensin-converting enzyme] inhibitors decrease the mortality of HF by 30%, those things help the patient to be compliant.
Participant 4
Other medication-related information considered beneficial included a personalized medication list with relevant information such as name (ie, brand and generic drug names) and dosage as well as information on medication interactions and side effects for prescribed and over-the-counter medications. Participants stated as follows:
Common side effects that they may anticipate, from the different families. You know they can go into ACE [angiotensin-converting enzyme] inhibitors, beta blockers, MRAs [mineralocorticoid receptor antagonists], they can go with all those different categories and look at, and self-education about the medication they are on so they know about it and know what side effects could possibly come up.
Participant 8
...interaction of medications is always a useful thing to have, especially over the counter and the normal medication.
Participant 5
Participant Views on App Features for Their Patients
App features perceived by participants as useful for patients included gamification, reminders and alarms, and food scanners. Participants had mixed views on the gamification of apps. Some of them felt that gamifying an app for HF may appeal to certain patients and if designed well it can be “fun,” “enjoyable,” “engaging,” and “interactive,” which can promote learning. One such example was embedding quizzes into the app that test patient knowledge on disease management. Other participants questioned the benefits to incentivizing someone’s health and whether patients would want to play a game, viewing it as an added task. A participant stated that they had “never seen a successful cardiovascular gamification in an app.” It was noted that gamification can be an attractive feature, especially for “young” patients with HF; however, it may be “demeaning” or not suitable for patients with HF, who are on average older. The HCPs felt that if an app for HF were gamified, it needs to be designed in a “mature” way. Participants made the following observations:
Obviously like, interaction helps to promote education at all ages. You might have a hard time getting buy in from the older population. Just because you get that “I’ve been alive for 80 years I know what I am doing” type of thing. But that’s okay it’s never perfect for everybody. But I think would help with engagement.
Participant 6
I think it’s great. My kids use educational apps that are kind of in a game format. So, I think it has a purpose. The question is, how do you do it for a mature adult? You know, are they going to find it too childish or are they going to actually enjoy it? If it’s done well, I think it’s great to keep patients engaged potentially.
Participant 5
You know our population is elderly, they are frail, English is another language of theirs, they are hard of hearing, they are visually challenged. So, yeah. I mean they are not playing cards on their phones.
Participant 20
Participants expressed that integrating reminders and alarms in an app to reinforce daily weighing, fluid intake, and exercise as well as prescription refills and physician’s appointments would be helpful. Nearly all participants agreed that reminders in an app for taking pills would be useful for patients, with some suggesting the option for patients to personalize the reminders and alarms (ie, turn them off). It was mentioned that patients are often prescribed multiple medications, to be taken multiple times a day, for their HF as well as other comorbidities; thus, they may have difficulties with medication adherence because of forgetfulness. One HCP commented as follows:
I was thinking about the medications. Like trying to make it compliant for the patients with their medications. If there was some sort of alarm, you know, within the app that would automatically remind them: “Okay it’s time to take your pills.”
Participant 11
Another feature that participants considered useful in an app was the integration of a food scanner, whereby patients can take a picture of their food plate or scan a food label (ie, nutritional facts table), which will then display nutritional information such as sodium content and calories:
I think it’s important, you know, the scanning of labels and then that calculates your salt content based on serving size and that would be a visual reminder of how much salt is actually in that and I think that when people scan enough labels, they’ll realize what they can and cannot eat.
Participant 14
Discussion
Principal Findings
To our knowledge, this is one of the first studies to determine the perspectives of HF cardiologists, nurses, and nurse practitioners on the use of mobile apps for HF management. Overall, participants had positive views about using mobile apps to support their patients with managing HF. They identified factors affecting app adoption (eg, patient age and technology access) and opportunities for app use, such as improving delivery of care, providing patient support through education, and facilitating patient engagement in care. App features such as gamification and quizzes were also identified by participants as being useful for patients. Our findings support previous research reporting that mHealth apps have the potential to be cost-effective interventions that optimize provision of care and support patients in HF self-management [22,25].
Perceived factors affecting app adoption related to the patient, clinical practice setting, and the apps themselves are consistent with findings from past studies [37-39]. One of the most frequently mentioned factors that affect app adoption, as perceived by our participants, was patient age. Findings from several studies also cite age as an individual-level factor affecting acceptance and use of mHealth apps [37,40-42] because most individuals using such technologies are often younger (aged <35 years), with those aged >70 years using mobile apps at the lowest frequency [40]. These findings are explained by Cajita et al [43] who found that older adults (aged ≥65 years) tended to lack knowledge on how to use mobile technologies. Evidence also suggests that older adults’ self-efficacy is low when learning to use mHealth apps [44]. Despite such findings, smartphone ownership among people with HF is relatively high among all age groups (eg, 84% in those aged 50-64 years), with older patients with HF also showing willingness to use mHealth apps to support HF management [45]. As the use of mHealth technologies for health-related activities is an emerging field, it is expected that older adults may face some difficulty and require support when using apps for HF management. However, the capability of patients with HF to use mobile apps should not be based on age alone; rather, factors associated with aging, such as visual impairment and cognitive dysfunction, may be more influential in the use of apps to support HF management. Regardless, accessibility features to accommodate users with special needs should be considered when designing and developing apps. It is imperative to keep this in mind to close the digital divide among older adults and promote more equitable use and distribution of mHealth technologies [43,45].
A lack of time and workload burden for HCPs as well as the ability of an app to be integrated into clinical workflows were identified as factors influencing app adoption for HF management, particularly for apps that have features for clinical monitoring and patient-clinician interaction. These data are supported by 2 recent reviews, where increased work and responsibilities as well as lack of integration with electronic medical records were among the most frequently identified clinician-level barriers to digital health adoption [38,39]. The majority of mHealth tools for HF management focus on telemonitoring, which HCPs consider to be time and resource intensive because these tools can produce more web-based data, additional administrative work, and increased communication and interactions with patients [29]. It is unknown whether mobile apps supporting various other functions such as education and behavior change have similar challenges within the context of HF management, although several of these workload concerns may be common when using technology for health care delivery in general. HCPs may also need to provide patients with training to support the use of mHealth tools, a concern identified by participants in our study. Evidence suggests that clinicians are less likely to adopt mHealth technologies if they believe that such tools do not reduce their workload [46,47]. This has direct impact on mHealth uptake among patients because patient adoption of these tools is often dependent on HCPs’ recommendations [48]. To address HCPs’ concerns regarding mHealth workload, it is imperative that they are recognized as stakeholders in mHealth technology development and implementation. In line with recommendations by Davis et al [49] and Radhakrishnan et al [50] for remote monitoring and telehealth technologies, we emphasize the importance of involving HCPs during the design, development, and implementation stages of mHealth apps to maximize the relevance and usability of such apps, which can result in overall better uptake and adoption. Moreover, practicing and in-training HCPs should receive adequate education on the use of digital health technologies [38] to increase their familiarity and comfort with such tools, which can increase their acceptance and uptake [51]. Proper integration with electronic medical records and clinical workflow can also facilitate mHealth app adoption [38,49].
Participants in this study saw several opportunities for using apps for HF management. Notably, participants felt that apps can support patients with HF by providing access to dietary and nutritional information as well as medication-related information. However, by contrast, most HF management apps are focused on daily monitoring of symptoms, with only a few addressing diet and medication [24,25,52]. Moreover, of the apps that include diet and medication, the focus is on tracking behaviors, and these apps fail to incorporate key diet- and treatment-related knowledge and skills, such as low-sodium diet and interpreting food labels as well as information on medication interactions and side effects, which are important features identified by participants in this study; for example, according to our questionnaire data, 52% (11/21) of the participants agreed that patients have difficulty reading food labels and identifying low-sodium products. Although these are not patient-reported data, this is an indication that HCPs see opportunities for mHealth apps beyond symptom monitoring. Albeit, such objective measures related to diet and medication would be supportive in promoting adherence, facilitating targeted behavior change, and supporting patients in forming fundamental skills and habits for managing HF.
This study uniquely explored HCP perceptions on features that may be useful to incorporate in an HF mobile app. One such feature that was widely discussed was gamification. Gamification is the use of game design mechanics in real-life, nongame environments [53]. The use of game techniques is an effective way to engage, motivate, and sustain health behavior change in individuals [54-56], and such techniques (eg, goal setting, reinforcement, and social connectivity) are closely related to proven health behavior change techniques [53]. However, the use of gamification in mHealth is an emerging concept and is being explored in the context of nutrition, physical activity, diabetes, mental health, and cardiovascular disease, including HF. The perspectives related to gamification for patients with HF in our study were mixed, with some of the participants recognizing that it can be an engaging and participative app feature and others questioning its appropriateness for the older population with HF. Interestingly, Radhakrishnan et al [57] conducted prototype testing of an HF mobile app integrated with contemporary game technology among older adults with HF (aged ≥55 years) and reported that the HF digital game was easy to play, enjoyable, and helpful in learning about HF and resulted in significant improvements in HF self-management knowledge. This study [57] and others [58-60] suggest the potential of gamification to be an effective medium to increase disease-related knowledge and support self-management of HF, even among older adults [61,62].
Limitations
Our study includes potential limitations that warrant discussion. Although telephone interviews produce data comparable with those produced in face-to-face interviews, a few limitations to this method of qualitative interviewing exist, including the inability to observe and respond to visual cues, lack of contextual data, and potential challenges to establishing participant-interviewer rapport [33]. Despite these limitations, the use of telephone interviews was favorable in our study because it allowed for geographical flexibility and an efficient cost- and time-saving method that accommodated participants’ schedules. Moreover, a part of our data collection period coincided with the COVID-19 pandemic, which may have shifted HCPs’ perspectives on the use of technology in clinical practice because of the necessary transition to remote care and telehealth use. In addition, many of our participants were women, albeit the perspectives of cardiologists, nurses, and nurse practitioners were equally represented. The perspectives of HCPs in this study are limited to those of cardiologists, nurses, and nurse practitioners. We acknowledge that other health care professionals such as family physicians, dietitians, and pharmacists may hold different views. Finally, we recognize that our own beliefs and assumptions could have biased study findings; however, steps were taken to minimize these biases. These steps included expert review of the interview guide, use of multiple data sources (interview and questionnaire), field notes by the interviewer, and independent coding by 2 researchers. We have also presented participant quotes that substantiate our findings and interpretations.
Conclusions
This study demonstrated that cardiologists, nurses, and nurse practitioners generally have positive views on the use of mHealth apps to support patients with HF management. Several challenges and opportunities for app adoption were also identified. HCPs are gatekeepers of health care delivery; thus, they are an integral part of the successful adoption and implementation of mHealth technologies in practice. Although HCPs may not be the primary users of mHealth apps, their views on these apps’ perceived advantages and their degree of compatibility with patient care and needs combined with the HCPs’ unique understanding of what is required to support patients in HF management will influence patients’ decision to use such apps for the management of their condition. Our findings support the importance of including the perspectives of HCPs, who are key stakeholders in integrating such technologies into routine clinical practice, in the development and implementation of mHealth apps.
Acknowledgments
This work was supported by the Canadian Institutes of Health Research. The authors extend their gratitude to the following individuals for their help with transcript and manuscript preparation: Carlissa Townson and Shobana Ranjit.
Abbreviations
- COREQ
Consolidated Criteria for Reporting Qualitative Research
- HCP
health care provider
- HF
heart failure
- mHealth
mobile health
Interview guide.
Data Availability
The data sets generated and analyzed during the course of conducting this study are available from the corresponding author on reasonable request.
Footnotes
Authors' Contributions: BS, ML, and JAA conceptualized and designed the study. SM helped with participant recruitment. BS led the writing of this manuscript and completed data collection and analysis. BS and SG prepared the transcripts. BS and MS conducted independent coding of transcripts. BS, ML, and JAA contributed to the interpretation of data. MS, SM, SG, ML, and JAA provided critical review of the manuscript. All authors read and approved the final version of the manuscript.
Conflicts of Interest: None declared.
References
- 1.Ezekowitz JA, O'Meara E, McDonald MA, Abrams H, Chan M, Ducharme A, Giannetti N, Grzeslo A, Hamilton PG, Heckman GA, Howlett JG, Koshman SL, Lepage S, McKelvie RS, Moe GW, Rajda M, Swiggum E, Virani SA, Zieroth S, Al-Hesayen A, Cohen-Solal A, D'Astous M, De S, Estrella-Holder E, Fremes S, Green L, Haddad H, Harkness K, Hernandez AF, Kouz S, LeBlanc MH, Masoudi FA, Ross HJ, Roussin A, Sussex B. 2017 comprehensive update of the Canadian Cardiovascular Society guidelines for the management of heart failure. Can J Cardiol. 2017 Nov;33(11):1342–433. doi: 10.1016/j.cjca.2017.08.022.S0828-282X(17)30973-X [DOI] [PubMed] [Google Scholar]
- 2.Katz AM. Heart Failure: Pathophysiology, Molecular Biology, and Clinical Management. Philadelphia, PA, USA: Lippincott Williams & Wilkins; 2000. [Google Scholar]
- 3.Dolansky MA, Schaefer JT, Hawkins MA, Gunstad J, Basuray A, Redle JD, Fang JC, Josephson RA, Moore SM, Hughes JW. The association between cognitive function and objective adherence to dietary sodium guidelines in patients with heart failure. Patient Prefer Adherence. 2016 Mar 2;10:233–41. doi: 10.2147/PPA.S95528. doi: 10.2147/PPA.S95528.ppa-10-233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mastromarino V, Casenghi M, Testa M, Gabriele E, Coluccia R, Rubattu S, Volpe M. Polypharmacy in heart failure patients. Curr Heart Fail Rep. 2014 Jun;11(2):212–9. doi: 10.1007/s11897-014-0186-8. [DOI] [PubMed] [Google Scholar]
- 5.Riegel B, Moelter ST, Ratcliffe SJ, Pressler SJ, De Geest S, Potashnik S, Fleck D, Sha D, Sayers SL, Weintraub WS, Weaver TE, Goldberg LR. Excessive daytime sleepiness is associated with poor medication adherence in adults with heart failure. J Card Fail. 2011 Apr;17(4):340–8. doi: 10.1016/j.cardfail.2010.11.002. https://europepmc.org/abstract/MED/21440873 .S1071-9164(10)01190-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Amininasab SS, Lolaty HA, Moosazadeh M, Shafipour V. Medication adherence and its predictors among patients with heart failure. Nurs Midwifery Stud. 2018;7(2):81–6. doi: 10.4103/nms.nms_9_17. [DOI] [Google Scholar]
- 7.Chung ML, Lennie TA, Mudd-Martin G, Moser DK. Adherence to a low-sodium diet in patients with heart failure is best when family members also follow the diet: a multicenter observational study. J Cardiovasc Nurs. 2015;30(1):44–50. doi: 10.1097/JCN.0000000000000089. https://europepmc.org/abstract/MED/24165698 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lesyuk W, Kriza C, Kolominsky-Rabas P. Cost-of-illness studies in heart failure: a systematic review 2004-2016. BMC Cardiovasc Disord. 2018 May 02;18(1):74. doi: 10.1186/s12872-018-0815-3. https://bmccardiovascdisord.biomedcentral.com/articles/10.1186/s12872-018-0815-3 .10.1186/s12872-018-0815-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barello S, Graffigna G, Vegni E, Savarese M, Lombardi F, Bosio AC. 'Engage me in taking care of my heart': a grounded theory study on patient-cardiologist relationship in the hospital management of heart failure. BMJ Open. 2015 Mar 16;5(3):e005582. doi: 10.1136/bmjopen-2014-005582. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=25776041 .bmjopen-2014-005582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dunn SP, Birtcher KK, Beavers CJ, Baker WL, Brouse SD, Page 2nd RL, Bittner V, Walsh MN. The role of the clinical pharmacist in the care of patients with cardiovascular disease. J Am Coll Cardiol. 2015 Nov 10;66(19):2129–39. doi: 10.1016/j.jacc.2015.09.025. https://linkinghub.elsevier.com/retrieve/pii/S0735-1097(15)06275-0 .S0735-1097(15)06275-0 [DOI] [PubMed] [Google Scholar]
- 11.McClinchy J, Williams J, Gordon L, Cairns M, Fairey G. Dietary advice and collaborative working: do pharmacists and allied health professionals other than dietitians have a role? Healthcare (Basel) 2015 Feb 12;3(1):64–77. doi: 10.3390/healthcare3010064. https://www.mdpi.com/resolver?pii=healthcare3010064 .healthcare3010064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stamp KD, Dunbar SB, Clark PC, Reilly CM, Gary RA, Higgins M, Ryan RM. Family partner intervention influences self-care confidence and treatment self-regulation in patients with heart failure. Eur J Cardiovasc Nurs. 2016 Aug;15(5):317–27. doi: 10.1177/1474515115572047. https://europepmc.org/abstract/MED/25673525 .1474515115572047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tarn DM, Mattimore TJ, Bell DS, Kravitz RL, Wenger NS. Provider views about responsibility for medication adherence and content of physician-older patient discussions. J Am Geriatr Soc. 2012 Jun;60(6):1019–26. doi: 10.1111/j.1532-5415.2012.03969.x. https://europepmc.org/abstract/MED/22646818 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peterson PN, Allen LA, Heidenreich PA, Albert NM, Piña IL, American Heart Association The American Heart Association Heart Failure Summit, Bethesda, April 12, 2017. Circ Heart Fail. 2018 Oct;11(10):e004957. doi: 10.1161/CIRCHEARTFAILURE.118.004957. https://europepmc.org/abstract/MED/30354400 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hägglund E, Lyngå P, Frie F, Ullman B, Persson H, Melin M, Hagerman I. Patient-centred home-based management of heart failure. Findings from a randomised clinical trial evaluating a tablet computer for self-care, quality of life and effects on knowledge. Scand Cardiovasc J. 2015 Aug;49(4):193–9. doi: 10.3109/14017431.2015.1035319. [DOI] [PubMed] [Google Scholar]
- 16.Piotrowicz E, Baranowski R, Bilinska M, Stepnowska M, Piotrowska M, Wójcik A, Korewicki J, Chojnowska L, Malek LA, Klopotowski M, Piotrowski W, Piotrowicz R. A new model of home-based telemonitored cardiac rehabilitation in patients with heart failure: effectiveness, quality of life, and adherence. Eur J Heart Fail. 2010 Feb;12(2):164–71. doi: 10.1093/eurjhf/hfp181. doi: 10.1093/eurjhf/hfp181.hfp181 [DOI] [PubMed] [Google Scholar]
- 17.Scherr D, Zweiker R, Kollmann A, Kastner P, Schreier G, Fruhwald FM. Mobile phone-based surveillance of cardiac patients at home. J Telemed Telecare. 2006;12(5):255–61. doi: 10.1258/135763306777889046. [DOI] [PubMed] [Google Scholar]
- 18.Scherr D, Kastner P, Kollmann A, Hallas A, Auer J, Krappinger H, Schuchlenz H, Stark G, Grander W, Jakl G, Schreier G, Fruhwald FM, MOBITEL Investigators Effect of home-based telemonitoring using mobile phone technology on the outcome of heart failure patients after an episode of acute decompensation: randomized controlled trial. J Med Internet Res. 2009 Aug 17;11(3):e34. doi: 10.2196/jmir.1252. https://www.jmir.org/2009/3/e34/ v11i3e34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Burke LE, Ma J, Azar KM, Bennett GG, Peterson ED, Zheng Y, Riley W, Stephens J, Shah SH, Suffoletto B, Turan TN, Spring B, Steinberger J, Quinn CC, American Heart Association Publications Committee of the Council on Epidemiology and Prevention, Behavior Change Committee of the Council on Cardiometabolic Health, Council on Cardiovascular and Stroke Nursing, Council on Functional Genomics and Translational Biology, Council on Quality of Care and Outcomes Research, and Stroke Council Current science on consumer use of mobile health for cardiovascular disease prevention: a scientific statement from the American Heart Association. Circulation. 2015 Sep 22;132(12):1157–213. doi: 10.1161/CIR.0000000000000232. https://europepmc.org/abstract/MED/26271892 .CIR.0000000000000232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kayyali R, Peletidi A, Ismail M, Hashim Z, Bandeira P, Bonnah J. Awareness and use of mHealth apps: a study from England. Pharmacy (Basel) 2017 Jun 14;5(2):33. doi: 10.3390/pharmacy5020033. https://www.mdpi.com/resolver?pii=pharmacy5020033 .pharmacy5020033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cajita MI, Gleason KT, Han H. A systematic review of mHealth-based heart failure interventions. J Cardiovasc Nurs. 2016;31(3):E10–22. doi: 10.1097/JCN.0000000000000305. https://europepmc.org/abstract/MED/26544175 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Coorey GM, Neubeck L, Mulley J, Redfern J. Effectiveness, acceptability and usefulness of mobile applications for cardiovascular disease self-management: systematic review with meta-synthesis of quantitative and qualitative data. Eur J Prev Cardiol. 2018 Mar;25(5):505–21. doi: 10.1177/2047487317750913. [DOI] [PubMed] [Google Scholar]
- 23.Marcolino MS, Oliveira JA, D'Agostino M, Ribeiro AL, Alkmim MB, Novillo-Ortiz D. The impact of mHealth interventions: systematic review of systematic reviews. JMIR Mhealth Uhealth. 2018 Jan 17;6(1):e23. doi: 10.2196/mhealth.8873. https://mhealth.jmir.org/2018/1/e23/ v6i1e23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wali S, Demers C, Shah H, Wali H, Lim D, Naik N, Ghany A, Vispute A, Wali M, Keshavjee K. Evaluation of heart failure apps to promote self-care: systematic app search. JMIR Mhealth Uhealth. 2019 Nov 11;7(11):e13173. doi: 10.2196/13173. https://mhealth.jmir.org/2019/11/e13173/ v7i11e13173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Athilingam P, Jenkins B. Mobile phone apps to support heart failure self-care management: integrative review. JMIR Cardio. 2018 May 02;2(1):e10057. doi: 10.2196/10057. https://cardio.jmir.org/2018/1/e10057/ v2i1e10057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fitzgerald M, McClelland T. What makes a mobile app successful in supporting health behaviour change? Health Educ J. 2016 Dec 27;76(3):373–81. doi: 10.1177/0017896916681179. [DOI] [Google Scholar]
- 27.Yang WE, Shah LM, Spaulding EM, Wang J, Xun H, Weng D, Shan R, Wongvibulsin S, Marvel FA, Martin SS. The role of a clinician amid the rise of mobile health technology. J Am Med Inform Assoc. 2019 Nov 01;26(11):1385–8. doi: 10.1093/jamia/ocz131. https://europepmc.org/abstract/MED/31373364 .5542898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Seto E, Leonard KJ, Masino C, Cafazzo JA, Barnsley J, Ross HJ. Attitudes of heart failure patients and health care providers towards mobile phone-based remote monitoring. J Med Internet Res. 2010 Nov 29;12(4):e55. doi: 10.2196/jmir.1627. https://www.jmir.org/2010/4/e55/ v12i4e55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fairbrother P, Ure J, Hanley J, McCloughan L, Denvir M, Sheikh A, McKinstry B, Telescot programme team Telemonitoring for chronic heart failure: the views of patients and healthcare professionals - a qualitative study. J Clin Nurs. 2014 Jan;23(1-2):132–44. doi: 10.1111/jocn.12137. [DOI] [PubMed] [Google Scholar]
- 30.Portz JD, Ford KL, Elsbernd K, Knoepke CE, Flint K, Bekelman DB, Boxer RS, Bull S. "I like the idea of it…but probably wouldn't use it" - health care provider perspectives on heart failure mHealth: qualitative study. JMIR Cardio. 2020 Sep 04;4(1):e18101. doi: 10.2196/18101. https://cardio.jmir.org/2020/1/e18101/ v4i1e18101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. 2000 Aug;23(4):334–40. doi: 10.1002/1098-240x(200008)23:4<334::aid-nur9>3.0.co;2-g.10.1002/1098-240X(200008)23:4<334::AID-NUR9>3.0.CO;2-G [DOI] [PubMed] [Google Scholar]
- 32.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007 Dec;19(6):349–57. doi: 10.1093/intqhc/mzm042.mzm042 [DOI] [PubMed] [Google Scholar]
- 33.Musselwhite K, Cuff L, McGregor L, King KM. The telephone interview is an effective method of data collection in clinical nursing research: a discussion paper. Int J Nurs Stud. 2007 Aug;44(6):1064–70. doi: 10.1016/j.ijnurstu.2006.05.014.S0020-7489(06)00167-2 [DOI] [PubMed] [Google Scholar]
- 34.Sturges JE, Hanrahan KJ. Comparing telephone and face-to-face qualitative interviewing: a research note. Qual Res. 2004 Apr;4(1):107–18. doi: 10.1177/1468794104041110. [DOI] [Google Scholar]
- 35.Rogers EM, Marshall LR. Diffusion of Innovations. 5th edition. New York, NY, USA: Free Press; 2003. [Google Scholar]
- 36.Lincoln YS, Guba EG. Naturalistic Inquiry. Thousand Oaks, CA, USA: Sage Publications; 1985. [Google Scholar]
- 37.Wang C, Qi H. Influencing factors of acceptance and use behavior of mobile health application users: systematic review. Healthcare (Basel) 2021 Mar 22;9(3):357. doi: 10.3390/healthcare9030357. https://www.mdpi.com/resolver?pii=healthcare9030357 .healthcare9030357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Whitelaw S, Pellegrini DM, Mamas MA, Cowie M, Van Spall HG. Barriers and facilitators of the uptake of digital health technology in cardiovascular care: a systematic scoping review. Eur Heart J Digit Health. 2021 Mar;2(1):62–74. doi: 10.1093/ehjdh/ztab005. https://europepmc.org/abstract/MED/34048508 .ztab005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jacob C, Sanchez-Vazquez A, Ivory C. Social, organizational, and technological factors impacting clinicians' adoption of mobile health tools: systematic literature review. JMIR Mhealth Uhealth. 2020 Feb 20;8(2):e15935. doi: 10.2196/15935. https://mhealth.jmir.org/2020/2/e15935/ v8i2e15935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Reddy R, Majmudar M, Dhopeshwarkar N, Vacaro V, Isselbacher E, Bhatt AB. Mobile health apps preferences and practice among ambulatory cardiovascular patients. Future Cardiol. 2018 Sep;14(5):381–8. doi: 10.2217/fca-2018-0005. [DOI] [PubMed] [Google Scholar]
- 41.Bhuyan SS, Lu N, Chandak A, Kim H, Wyant D, Bhatt J, Kedia S, Chang CF. Use of mobile health applications for health-seeking behavior among US adults. J Med Syst. 2016 Jun;40(6):153. doi: 10.1007/s10916-016-0492-7.10.1007/s10916-016-0492-7 [DOI] [PubMed] [Google Scholar]
- 42.James DC, Harville 2nd C. Barriers and motivators to participating in mHealth research among African American men. Am J Mens Health. 2017 Nov;11(6):1605–13. doi: 10.1177/1557988315620276. https://journals.sagepub.com/doi/10.1177/1557988315620276?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed .1557988315620276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cajita MI, Hodgson NA, Lam KW, Yoo S, Han HR. Facilitators of and barriers to mHealth adoption in older adults with heart failure. Comput Inform Nurs. 2018 Aug;36(8):376–82. doi: 10.1097/CIN.0000000000000442. https://europepmc.org/abstract/MED/29742549 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mercer K, Giangregorio L, Schneider E, Chilana P, Li M, Grindrod K. Acceptance of commercially available wearable activity trackers among adults aged over 50 and with chronic illness: a mixed-methods evaluation. JMIR Mhealth Uhealth. 2016 Jan 27;4(1):e7. doi: 10.2196/mhealth.4225. https://mhealth.jmir.org/2016/1/e7/ v4i1e7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Leigh JW, Gerber BS, Gans CP, Kansal MM, Kitsiou S. Smartphone ownership and interest in mobile health technologies for self-care among patients with chronic heart failure: cross-sectional survey study. JMIR Cardio. 2022 Jan 14;6(1):e31982. doi: 10.2196/31982. https://cardio.jmir.org/2022/1/e31982/ v6i1e31982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.World Health Organization. Geneva, Switzerland: World Health Organization; 2019. [2022-03-16]. WHO Guideline: Recommendations on digital interventions for health system strengthening. https://www.who.int/publications/i/item/9789241550505 . [PubMed] [Google Scholar]
- 47.NHS Health Education. London, UK: The NHS Constitution; 2019. Feb, [2022-03-16]. The Topol Review: preparing the healthcare workforce to deliver the digital future: an independent report on behalf of the secretary of state for health and social care. https://topol.hee.nhs.uk/wp-content/uploads/HEE-Topol-Review-2019.pdf . [Google Scholar]
- 48.Leigh S, Ashall-Payne L. The role of health-care providers in mHealth adoption. Lancet Digit Health. 2019 Jun;1(2):e58–9. doi: 10.1016/S2589-7500(19)30025-1. https://linkinghub.elsevier.com/retrieve/pii/S2589-7500(19)30025-1 .S2589-7500(19)30025-1 [DOI] [PubMed] [Google Scholar]
- 49.Davis MM, Freeman M, Kaye J, Vuckovic N, Buckley DI. A systematic review of clinician and staff views on the acceptability of incorporating remote monitoring technology into primary care. Telemed J E Health. 2014 May;20(5):428–38. doi: 10.1089/tmj.2013.0166. https://europepmc.org/abstract/MED/24731239 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Radhakrishnan K, Xie B, Berkley A, Kim M. Barriers and facilitators for sustainability of tele-homecare programs: a systematic review. Health Serv Res. 2016 Feb;51(1):48–75. doi: 10.1111/1475-6773.12327. https://europepmc.org/abstract/MED/26119048 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Waseh S, Dicker AP. Telemedicine training in undergraduate medical education: mixed-methods review. JMIR Med Educ. 2019 Apr 08;5(1):e12515. doi: 10.2196/12515. https://mededu.jmir.org/2019/1/e12515/ v5i1e12515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Creber RM, Reading M, Hiraldo G, Iribarren SJ. Review and analysis of existing mobile phone applications to support symptom monitoring and self-management for adults with heart failure. J Card Fail. 2016 Aug 1;22(8):S81. doi: 10.1016/j.cardfail.2016.06.259. [DOI] [Google Scholar]
- 53.Cugelman B. Gamification: what it is and why it matters to digital health behavior change developers. JMIR Serious Games. 2013 Dec 12;1(1):e3. doi: 10.2196/games.3139. https://games.jmir.org/2013/1/e3/ v1i1e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Baranowski T, Buday R, Thompson DI, Baranowski J. Playing for real: video games and stories for health-related behavior change. Am J Prev Med. 2008 Jan;34(1):74–82. doi: 10.1016/j.amepre.2007.09.027. https://europepmc.org/abstract/MED/18083454 .S0749-3797(07)00647-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Aarhus R, Grönvall E, Larsen SB, Wollsen S. Turning training into play: embodied gaming, seniors, physical training and motivation. Gerontechnology. 2011;10(2):110–20. doi: 10.4017/gt.2011.10.2.005.00. [DOI] [Google Scholar]
- 56.Deterding S. Gamification: designing for motivation. interactions. 2012 Jul;19(4):14–7. doi: 10.1145/2212877.2212883. [DOI] [Google Scholar]
- 57.Radhakrishnan K, Toprac P, O'Hair M, Bias R, Kim MT, Bradley P, Mackert M. Interactive digital e-Health game for heart failure self-management: a feasibility study. Games Health J. 2016 Dec;5(6):366–74. doi: 10.1089/g4h.2016.0038. https://europepmc.org/abstract/MED/27976955 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Dithmer M, Rasmussen JO, Grönvall E, Spindler H, Hansen J, Nielsen G, Sørensen SB, Dinesen B. "The heart game": using gamification as part of a telerehabilitation program for heart patients. Games Health J. 2016 Feb;5(1):27–33. doi: 10.1089/g4h.2015.0001. https://europepmc.org/abstract/MED/26579590 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Radhakrishnan K, Julien C, Baranowski T, O'Hair M, Lee G, Sagna De Main A, Allen C, Viswanathan B, Thomaz E, Kim M. Feasibility of a sensor-controlled digital game for heart failure self-management: randomized controlled trial. JMIR Serious Games. 2021 Nov 08;9(4):e29044. doi: 10.2196/29044. https://games.jmir.org/2021/4/e29044/ v9i4e29044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Radhakrishnan K, Baranowski T, Julien C, Thomaz E, Kim M. Role of digital games in self-management of cardiovascular diseases: a scoping review. Games Health J. 2019 Apr;8(2):65–73. doi: 10.1089/g4h.2018.0011. https://europepmc.org/abstract/MED/30199275 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Koivisto J, Malik A. Gamification for older adults: a systematic literature review. Gerontologist. 2021 Sep 13;61(7):e360–72. doi: 10.1093/geront/gnaa047. https://europepmc.org/abstract/MED/32530026 .5856423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Radhakrishnan K, Baranowski T, O'Hair M, Fournier CA, Spranger CB, Kim MT. Personalizing sensor-controlled digital gaming to self-management needs of older adults with heart failure: a qualitative study. Games Health J. 2020 Aug;9(4):304–10. doi: 10.1089/g4h.2019.0222. https://europepmc.org/abstract/MED/32155355 . [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Interview guide.
Data Availability Statement
The data sets generated and analyzed during the course of conducting this study are available from the corresponding author on reasonable request.


