Abstract
People with obsessive-compulsive disorder (OCD) tend to distrust their memory, perception, and other cognitive functions, and many OCD symptoms can be traced to diminished confidence in one's cognitive processes. For example, poor confidence in recall accuracy can cause doubt about one's memory and motivate repeated checking. At the same time, people with OCD also display performance deficits in a variety of cognitive tasks, so their reduced confidence must be evaluated in relation to their actual performance. To that end, we conducted an exhaustive review and meta-analysis of studies in which OCD participants and non-clinical control participants performed cognitive tasks and reported their confidence in their performance. Our search resulted in 19 studies that met criteria for inclusion in the quantitative analysis, with all studies addressing either memory or perception. We found that both performance and reported confidence were lower in OCD than in control participants. Importantly, however, confidence was more impaired than performance in participants with OCD. These findings suggest that people with OCD are less confident in their memory and perception than they should be, indicating a genuine under-confidence in this population. We discuss potential mechanisms that might account for this finding and suggest avenues for further research into under-confidence and related meta-cognitive characteristics of OCD.
Key words: Confidence, doubt, memory, metacognition, obsessive-compulsive disorder, perception
Introduction
Obsessive-compulsive disorder (OCD) was described more than a century ago as a disorder of doubt (Janet, 1903), with later theories of OCD agreeing on the central place of doubt in the disorder (e.g. Boyer & Lienard, 2006; Rapoport, 1989; Reed, 1985; Shapiro, 1965). In particular, people with OCD often distrust their memory, perception, and other cognitive functions, and many OCD symptoms can be understood in terms of diminished cognitive confidence. For example, individuals with OCD may attempt to reconstruct what they had experienced while driving to work, in an attempt to convince themselves that they have not accidentally run over an innocent pedestrian. Others may engage in repeated checking of doors and windows before leaving the house, because they cannot feel certain that they have properly closed them just a few minutes earlier.†,1
Consistent with these observations, questionnaire-based studies have consistently found that people with OCD report a distrust in their own cognitive processes, particularly in their memory and perception (e.g. Cougle, Salkovskis, & Wahl, 2007; Hermans et al., 2008; Hermans, Martens, De Cort, Pieters, & Eelen, 2003; Nedeljkovic & Kyrios, 2007; Nedeljkovic, Moulding, Kyrios, & Doron, 2009). While these studies documented the general tendency of individuals with OCD to distrust their cognitive processes, several experimental studies directly examined the extent to which people with OCD feel confident about their performance in a variety of cognitive tasks. In these studies, participants with OCD and non-clinical control participants performed tasks that assess memory, perception, decision making, or general knowledge, and were then asked to rate their confidence in their own performance. Whereas some studies have found that participants with OCD reported lower levels of confidence as compared with control participants (e.g. Cougle, Salkovskis, & Thorpe, 2008; Dar, 2004; Dar, Rish, Hermesh, Taub, & Fux, 2000; Marton et al., 2019; Zitterl et al., 2001), no group differences were found in other studies (e.g. Cabrera, McNally, & Savage, 2001; Göz, Karahan, & Tekcan, 2016; Tekcan, Topçuoğlu, & Kaya, 2007).
Notably, most of the studies that assessed participants' subjective confidence in their performance have not examined these confidence ratings in relation to participants' actual performance. We are aware of only two studies that directly examined confidence ratings in relation to actual performance (Dar, 2004; Dar et al., 2000). In these studies, participants with OCD and non-clinical control participants completed a two-choice general knowledge test (e.g. ‘Which scientist is associated with quantum mechanics? 1. Albert Einstein; 2. Niels Bohr’). After indicating their answer to each item, participants were asked to rate the probability that their answer was correct. In addition, at the end of the test, participants were asked to estimate the number of items they had answered correctly. As predicted, participants with OCD were significantly less confident in their performance than non-clinical participants, both in terms of the mean probability that their answers were correct and in terms of their global estimation of their performance. In addition, direct comparisons of confidence and performance showed that participants with OCD underestimated their actual performance on the general knowledge test, which was in fact equal to that of the non-clinical participants.
As these results demonstrate, it is critical to assess not only subjective confidence, but also actual performance in these types of tasks. If performance is not assessed or considered (as was the case in a recent review; Ouellet-Courtois, Wilson, and O'Connor, 2018), it is impossible to rule out the possibility that the reduced confidence in OCD may actually reflect an accurate assessment of impaired performance. Put differently, the question is whether the lower reported confidence of people with OCD is in fact too low in relation to their actual performance in the relevant tasks. As documented above for confidence/doubt, however, the evidence regarding actual task performance of people with OCD in various cognitive domains is also mixed. Some of these studies have found the performance of OCD participants to be unimpaired (e.g. Boschen & Vuksanovic, 2007; Göz et al., 2016; Moritz et al., 2007; Tekcan et al., 2007), whereas others found OCD participants to display deficient performance in cognitive and perceptual tasks compared to controls (e.g. Moritz, Rietschel, Jelinek, & Bauml, 2011; Radomsky, Dugas, Alcolado, & Lavoie, 2014; Zitterl et al., 2001). Consistent with these latter reports, meta-analyses of actual cognitive performance in OCD concluded that people with OCD exhibit deficits in both verbal and non-verbal memory (Abramovitch, Abramowitz, & Mittelman, 2013; Shin, Lee, Kim, & Kwon, 2014).
The present review and meta-analysis were designed to evaluate the self-reported confidence of people with OCD in their cognitive performance in relation to their actual performance. Toward this aim, we reviewed all research articles that assessed both performance and confidence in participants with OCD as compared to non-clinical control participants. This allowed us to evaluate three major questions: (1) Is OCD associated with impaired performance, relative to controls, in tasks that assess memory and perception? (2) Do OCD participants report lower confidence in their performance in such tasks relative to control participants? and (3) Are individuals with OCD characterized with under-confidence in these domains? In other words, is their deficit in reported confidence larger than their deficit in actual performance?
Method
Search strategy
The systematic review protocol was registered in Prospero before undertaking the review (Dar, Lazarov, & Yardeni, 2020). The present report conforms to PRISMA guidelines (Moher, Liberati, Tetzlaff, & Altman, 2009). Studies were selected following a systematic search for publications at the end of July 2020, complemented by a second search in October of 2021 to check for any studies that might have been published in the interim period (none were found). The search covered PubMed, PsycNet, and ISI Web of Science. All relevant subject headings and free-text terms were used to represent OCD and confidence, using the following search terms (asterisk denotes truncation designed to capture grammatical variability): ‘obsessiv*, compulsiv*’ with ‘confiden*’, ‘certain*’, ‘doubt*’, ‘decision*’, ‘source monitoring’, ‘monitor*’, ‘meta cognit*’, ‘memory*’, ‘signal detect*’* and ‘calibrat*’. Additional records were identified by employing the Similar Articles feature in PubMed, and the Cited Reference Search in ISI Web of Science. Reference sections of review articles, book chapters, and studies selected for inclusion were searched for further studies.
Search selection process
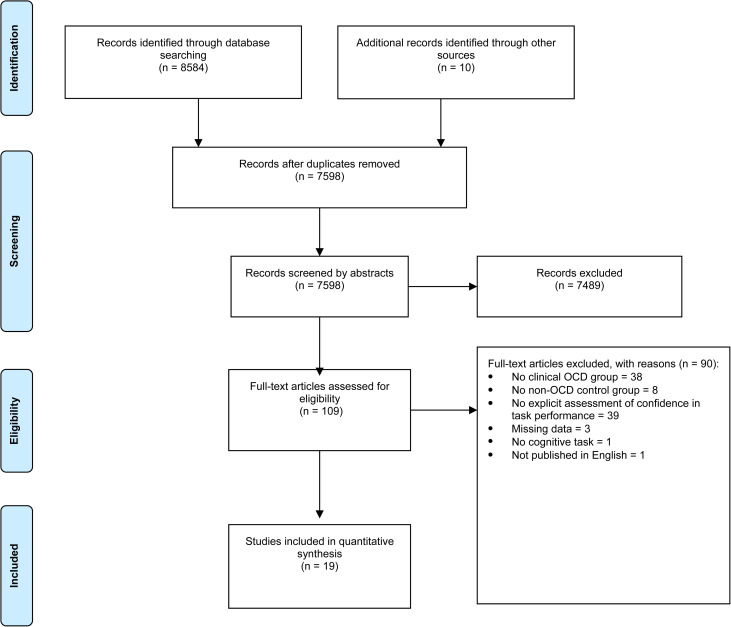
Titles and abstracts were independently screened by two reviewers using Covidence systematic review software (Babineau, 2014), based on the inclusion and exclusion criteria outlined below. Discrepancies were resolved by discussion between the two reviewers. Full articles were then independently screened by each of the two reviewers. Inter-rater reliability was calculated, and where disagreements occurred, a consensus meeting was held to decide on study inclusion. Study selection process and reasons for exclusions are described in Fig. 1.
Fig. 1.
PRISMA flowchart of paper selection. Study selection process and reasons for exclusions.
A study was included if: (1) OCD was assessed using a valid and accepted tool, including a diagnosis made by a clinician; (2) the performance of the OCD participants was compared to that of a control group – either healthy participants with no psychiatric disorder, or participants with another psychiatric disorder (e.g. anxiety disorders); (3) the study assessed both objective task performance and participants' explicit self-reported confidence as to their performance on the task; (4) the study included adult participants (aged >18); and (5) the study was published in English. Studies were excluded on the following grounds: (1) they were a review article, case study, or book chapter; (2) clinically relevant symptoms of OCD were not used in defining study groups; (3) the OCD group was not specifically identified; (4) lack of a non-OCD control group; (5) using ‘analog’ participants (i.e. non-selected participants, participants with subclinical OCD, or comparing high v. low scorers on OCD symptoms); and (6) assessing confidence only indirectly, with no explicit reporting of confidence levels.
Data extraction
Data extraction was undertaken by the two reviewers and checked by the principal investigator (RD) for errors. Study characteristics extracted from reviewed studies included: (1) publication year; (2) sample size; (3) age of the OCD group; (4) gender ratio; (5) OCD subtype, if relevant; (6) comparison group/s (healthy controls, anxiety disorders)2; and (7) paradigm/task used (e.g. memory test, decision making, perceptual search, etc.). Table 1 lists the basic characteristics of the studies included in our analysis, and Table 2 details the performance and confidence measures used in each study.
Table 1.
Study characteristics
| Study | N OCD | N Control | % Females | Mean age (sd) | Task |
|---|---|---|---|---|---|
| Boschen and Vuksanovic (2007) | 14 | 40 | 86 | 38.8 (−) | Stovetop repeated checking (free recall) |
| Cabrera et al. (2001) | 21 | 21 | 52 | 32.2 (10.3) | Semantic integration |
| Cougle et al. (2008) | 21 | 24 | 62 | 37.29 (10.0) | Reality monitoring |
| Dar et al. (2000) | 20 | 20 | 30 | 36.85 (12.17) | General knowledge |
| Dar (2004) | 15 | 15 | 13 | – | General knowledge |
| Foa et al. (1997) | 15 | 15 | – | 34.9 (12.9) | Noise rating task (with recognition phase) |
| Göz et al. (2016) | Checkers: 28 | 30 | 63–75 | 31.53 (10.81) | False memory task (DRM) |
| Non-checkers: 32 | 34.34 (9.69) | ||||
| Karadag et al. (2005) | 32 | 31 | 75 | 34.28 (10.95) | Recognition of sentences task (neutral and OC related) |
| Korotitsch (2004) | 25 | 25 | 64 | 37.0 (12.9) | Memory recognition test – words were either read or heard |
| Marton et al. (2019) | 26 | 44 | – | – | The random dot motion task |
| McNally and Kohlbeck (1993) | Checkers: 12 | 12 | 58 | 31.4 (7.8) | Recognition of words and drawings |
| Non-checkers: 12 | 12 | 31.2 (10.7) | |||
| Moritz et al. (2006) | 27 | 51 | 63 | 32.43 (8.86) | Source memory recognition task |
| Moritz et al. (2007) | 28 | 28 | 54 | 33.07 (11.94) | Recognition of words |
| Moritz et al. (2009a) | 43 | 46 | 74 | 32.74 (9.96) | Picture word memory test (recognition) |
| Moritz et al. (2009b) | 32 | 32 | 72 | 34.00 (10.88) | Action memory task |
| Moritz et al. (2011) | 30 | 20 | 60 | 30.03 (7.04) | Directed forgetting paradigm |
| Radomsky et al. (2014) | 30 | 30 | 47 | 33.1 (10.2) | Stovetop repeated checking (free recall) |
| Tekcan et al. (2007) | Checkers: 25 | 27 | – | 30.76 (9.75) | General knowledge |
| Non-checkers: 16 | 34.00 (11.30) | ||||
| Zitterl et al. (2001) | 27 | 27 | 48 | 38.9 (12.3) | LGT-3: verbal, nonverbal and general memory |
Note. The minus sign (−) represents data that were not available in the paper.
Table 2.
Measures of accuracy and confidence in the studies included in the analysis
| Study | Task | Measure of accuracy | Measure of confidence | Confidence scale |
|---|---|---|---|---|
| Boschen and Vuksanovic (2007) | Stovetop repeated checking (free recall) | Number of recall errors | Confidence in memory accuracy | Visual analog scale (1–10) |
| Cabrera et al. (2001) | Semantic integration | Sentence recognition – old/new | Confidence in recognition decision | For sentences judged old: +1 to +6 For sentences judged new: −1 to −6 |
| Cougle et al. (2008) | Reality monitoring | Memory for whether actions were performed or imagined | Confidence in memory rating | Visual analog scale (0–100) |
| Dar et al. (2000) | General knowledge | Mean number of correct answers | Confidence in answer | 5–100% with 5% intervals |
| Dar (2004) | General knowledge | Mean number of correct answers | Confidence in answer | 5–100% with 5% intervals |
| Foa et al. (1997) | Noise rating task (with recognition phase) | Sentence recognition – old/new | Confidence in recognition | 3-point scale with 1 indicating confidence and 3 indicating guessing |
| Göz et al. (2016) | False memory task (DRM) | Words recognition – old/new | Confidence in recognition | 4-point scale: 1 – not confident at all to 4 – very confident |
| Karadag et al. (2005) | Recognition of sentences task (neutral and OC related) | Sentence recognition – old/new | Confidence in recognition | 2-point scale: 1 indicating ‘I am completely confident’ and 0 indicating ‘I am not confident or I suspect’ |
| Korotitsch (2004) | Memory recognition test – words were either read or heard | Words recognition – old/new | Confidence in recognition | 3-point scale: 1 = not sure, 2 = fairly sure, 3 = sure |
| Marton et al. (2019) | The random dot motion task | Determine whether the dot cloud appeared to be moving to the right or left | Confidence in decision | 7-point scale from 1 – low certainty to 7 – high certainty |
| McNally and Kohlbeck (1993) | Recognition of words and drawings | Recognition – old/new | Confidence in recognition | 3-point scale: from 1 – guessing to 3 – certain |
| Moritz et al. (2006) | Source memory recognition task | Recognition – old/new/self-generated | Confidence in recognition | 4-point scale: from 1 – guessing to 4 – entirely certain |
| Moritz et al. (2007) | Recognition of words | Words recognition – old/new | Confidence in recognition | 6-point scale: entirely sure yes (100%), quite sure yes (80%), unsure yes (60%), unsure no (40%), quite sure no (20%), and entirely sure no (0%) |
| Moritz et al. (2009a) | Picture word memory test (recognition) | Recognition – old /new | Confidence in recognition | 4-point scale: 1 = guessing, 2 = rather unsure, 3 = rather sure, 4 = entirely sure |
| Moritz et al. (2009b) | Action memory task | Recognition – verbal/nonverbal/novel (external source memory) | Confidence in recognition | 4-point scale: from 1 – 100% certain to 4 – extremely uncertain |
| Moritz et al. (2011) | Directed forgetting paradigm | Recognition – old /new | Confidence was assessed together with the accuracy | 6-point scale: 1 = 100% old, 2 = rather sure old, 3 = unsure old, 4 = unsure new, 5 = rather sure new, 6 = 100% new |
| Radomsky et al. (2014) | Stovetop repeated checking (free recall) | Recall – the number of knobs (out of 3) correctly recalled | Verbally rate confidence in decision | 100-point scales, with 0 representing ‘not at all’ and 100 representing ‘extremely’ |
| Tekcan et al. (2007) | General knowledge | Recognition – multiple choice | Confidence in recognition decision | 0–100% with 20% intervals |
| Zitterl et al. (2001) | LGT-3: verbal, nonverbal and general memory | Scores on the LGT-3 test | Confidence in memory ability | 5-point scale |
Note: None of the studies provided feedback to participants on their performance in the tasks.
Data analysis
We analyzed the data using Comprehensive Meta-Analysis, Version 3 (CMA; Borenstein, Hedges, Higgins, and Rothstein, 2015). Hedges' g was used as the effect size measure. The data on accuracy and on confidence were analyzed separately. Main effects (differences between OCD and control participants) were calculated using a random effect model, whereas the interaction effect (differences between the effects of accuracy and confidence) was calculated based on a mixed-effect model, as recommended by Borenstein and his colleagues (Borenstein, 2019; Borenstein, Hedges, Higgins, & Rothstein, 2009). In studies that measured accuracy and confidence using more than a single task (e.g. for both verbal and non-verbal stimuli, or for both OCD-relevant and irrelevant stimuli), the data of the two tasks were combined. In studies which included two groups of OCD participants (‘checkers’ and ‘non-checkers’), both of which were compared to the same control group, the N of the control group was divided by two to avoid inflation of type I error (Borenstein, 2019). In a series of secondary analyses, we examined the pattern of the results specifically in the subgroup of OCD ‘checkers’, as well as the potential effects of anxiety, depression, and medication status on the results.
Publication bias was examined (Sterne, Egger, & Smith, 2001), for both accuracy and confidence, using funnel plots with one-tailed Egger tests (Egger, Smith, Schneider, & Minder, 1997). The potential impact of such a bias on the results of the analysis was estimated using the Duval and Tweedie trim and fill method (Duval & Tweedie, 2000).
Results
Task performance and confidence
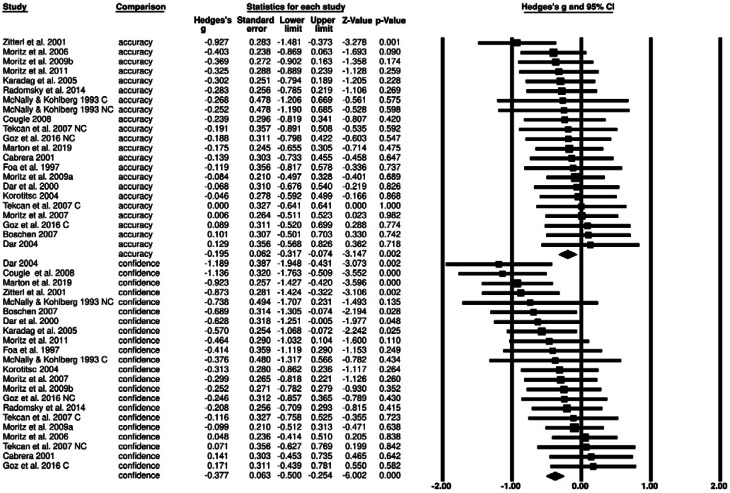
Our analysis indicated that overall, OCD participants performed significantly worse than non-clinical participants on the cognitive tasks examined in the included studies (g = −0.20, Z = −3.15, p = 0.002, 95% confidence interval (CI) [−0.32 to 0.01]). As can be seen in Fig. 2, this effect was relatively homogeneous across studies. This observation is supported by the non-significant Q statistic (12.786, df = 21, p = 0.916), indicating that the assumption of a common true effect in this body of studies could not be rejected.
Fig. 2.
Effect sizes forest plot. Forest plot depicting effect sizes for accuracy and confidence.
Note. Negative values of Hedges' g indicate lower scores of OCD participants as compared to control participants.
Across studies, OCD participants were also significantly less confident than non-clinical control participants in their performance (g = −0.38, Z = −6.00, p < 0.001, 95% CI −0.50 to −0.25). In contrast to the performance results reported above, this effect was heterogeneous across studies, as indicated by the significant Q statistic (34.71, df = 21, p = 0.03).
As noted in the Introduction, the present meta-analysis also aimed at examining whether people with OCD are truly under-confident, that is, if they are less confident than they should be given their performance. In meta-analyses, the relevant statistic for answering this question is the Z-value that reflects the difference between the group effects of performance (g = −0.20) and confidence (g = −0.38). This value was statistically significant, Z = 1.99, p = 0.048, indicating that the overall difference between participants with OCD and non-clinical control participants in reported confidence was larger than the corresponding difference in performance.
We should note that the above value of Z for the interaction between performance and confidence is likely an underestimate of the true effect statistic. In CMA, this Z value assumes that the correlation between performance and confidence is zero (Borenstein et al., 2015). However, the few studies that reported the relevant correlation coefficients (Boschen & Vuksanovic, 2007; Cougle et al., 2008; Dar et al., 2000; Tekcan et al., 2007) found them to range between 0.16 and 0.91. As seen in Table 3, as the correlation coefficient between confidence and accuracy increases, the value of Z increases (and the p value decreases). If the correlation is assumed to be 0.3, Z becomes 2.38, with a p = 0.02. With a correlation of 0.5, which is in the middle of the range of correlations actually reported in this body of studies, the value of Z becomes 2.82, with p = 0.005.
Table 3.
Significance tests of the differences between accuracy and confidence by assumed correlation between them
| Assumed correlation | Z | p value |
|---|---|---|
| 0 | 1.99 | 0.047 |
| 0.10 | 2.10 | 0.036 |
| 0.20 | 2.23 | 0.026 |
| 0.30 | 2.38 | 0.017 |
| 0.40 | 2.57 | 0.010 |
| 0.50 | 2.82 | 0.005 |
| 0.60 | 3.15 | 0.002 |
| 0.70 | 3.63 | 0>.001 |
| 0.80 | 4.45 | 0>.001 |
| 0.90 | 6.30 | 0>.001 |
| 0.99 | 1.42 × 108 | 0>.001 |
Secondary analyses
We conducted a secondary analysis including only samples of OCD participants that were selected on the basis of having primary checking symptoms (so-called ‘checkers; N = 8). The pattern of the results was very similar for this subgroup, but due to the small N, only the effect of confidence reached statistical significance (g = −0.55, Z = −3.44, p = 0.001, 95% CI −0.86 to −0.24).
Next, we examined whether confidence was related to anxiety or depression in our meta-analysis data. Unfortunately, very few studies reported the anxiety scores of the OCD participants. However, 14 studies did report depression scores for the OCD participants, either with Beck Depression Inventory (BDI) or the Hamilton Depression Rating Scale (seven studies each). To combine these two measures, we transformed all the scores into the BDI using the conversion table created by Furukawa et al. (2020). To test whether depression might have contributed to the differences between OCD and control participants in reported confidence, we computed the correlation between the effect sizes (i.e. Hedges’ g of the differences between OCD and control participants) and the unified depression scores. Depression was negatively correlated with the effect size for performance, r = 0.477, p = 0.021, but not for confidence, r = 0.148, p = 0.51, indicating that depression did not account for the differences in confidence between OCD and control participants in our data.
Finally, we attempted to assess the role of medication use in our results. Of the studies included in our analysis, only six reported the medication use status of the OCD participants (Dar et al., 2000; Korotitsch, 2004; Moritz, Jacobsen, Willenborg, Jelinek, & Fricke, 2006, 2007; Radomsky et al., 2014; Zitterl et al., 2001). Unfortunately, even these six studies did not provide sufficient details about the type and doses of the medications to allow an analysis of their potential effect on the dependent variables. It is worth noting, however, that two of the studies mentioned above (Moritz et al., 2006, 2007) did include medication status as a moderator in their analysis and found no effect of medication use on any of the dependent variables.
Publication bias
With regard to confidence, an examination of the funnel plot suggested a small study effect, with smaller studies reporting larger effects. Consistent with this impression, the Begg and Mazumdar rank correlation test was significant, with a Kendall's tau correlation coefficient of −0.36 between sample size and effect size, p(1-tailed) = 0.008. Egger's regression was also significant in a one-tailed t test, t(21) = 2.39, p = 0.018. The trim and fill algorithm, which estimates publication bias, produced an adjusted effect size of −0.22, 95% CI −0.39 to −0.04. Notably, this adjusted CI did not include zero, so the differences between OCD and control participants in reported confidence remain significant after this correction. An examination of the funnel plot of the accuracy data did not suggest a small study effect, and none of the bias indicators were statistically significant.
Discussion
The present meta-analysis is the first to examine the reported confidence of participants with OCD, as compared to non-clinical control participants, in relation to their performance on various cognitive tasks. We found that both performance and reported confidence were lower in OCD than in control participants. Importantly, however, our analysis indicates that confidence was more impaired than performance in participants with OCD. Put differently, OCD participants exhibit a larger reduction in confidence than in actual performance compared with non-clinical control participants. These findings imply that people with OCD are under-confident (i.e. less confident than they should be) regarding their performance.
The finding of cognitive under-confidence in OCD participants is particularly important in light of the observation that humans generally tend to be over-confident in their abilities and performance (e.g. Ehrlinger, Mitchum, & Dweck, 2016; Koriat, Lichtenstein, & Fischhoff, 1980; Moore & Healy, 2008; Prims & Moore, 2017). As a rule, then, the confidence of most people in their performance and abilities is too high given their actual performance or abilities. Overconfidence has been documented across many domains – people are likely to overestimate their success in a test, their driving skills, or their chances of doing well in the stock market. Experimental studies using methods such as those described in the Introduction, where participants answer multiple choice questions, consistently found participants from the general population to be overconfident in their answers. For example, in a series of studies by Fischhoff, Slovic, and Lichtenstein (1977), even answers that participants were absolutely certain about (i.e. rated the probability that they were correct as 1.00) were in reality erroneous about 20% of the time. Participants in these studies were clearly unaware that their confidence in their performance was excessive, as evidenced by their willingness to bet money on their answers. Overconfidence is assumed to be a universal bias, proposed to have an evolutionary basis and to be adaptive for optimal functioning (Johnson & Fowler, 2011; Tobena, Marks, & Dar, 1999). Against this backdrop, the current findings of under-confidence in individual with OCD appears to be unique,3 suggesting not merely a lack of a protective normative bias in OCD, but rather the existence of a negative bias in the opposite direction.
Asking someone to appraise their own performance on a task in the absence of feedback presents a challenging task for most people. Indeed, a recent meta-synthesis found that the mean correlation between self-evaluation and actual performance reported in meta-analyses across a variety of performance domains was only moderate (r = 0.29; Zell and Krizan, 2014). A recent novel model of OCD suggests that in OCD, these internal appraisals may be particularly challenging. According to the Seeking Proxies for Internal States (SPIS) model (Dar, Lazarov, & Liberman, 2021), OCD symptoms are associated with attenuated access to internal states. Evidence supporting this hypothesis was obtained in relation to several internal states, including muscle tension (Lazarov, Dar, Liberman, & Oded, 2012b; Lazarov, Liberman, Hermesh, & Dar, 2014), emotions (Dar, Lazarov, & Liberman, 2016; Lazarov, Friedman, Comay, Liberman, & Dar, 2020), interoception (Ezrati, Friedman, & Dar, 2019; Ezrati, Sherman, & Dar, 2018), and a sense of understanding (Dar, Eden, van Dongen, Hauschildt, & Liberman, 2019). As estimating one's performance requires accessing an internal state (in the current review, particularly one's memory), the under-confidence seen in our analysis might be an expression of a general difficulty in accessing these states in OCD. Moreover, according to the SPIS model, the process of self-doubt that results from attenuated access to internal states may lead, in turn, to actual performance deficits. For example, instructions that undermined unselected participants' confidence in their ability to assess their own muscle tension (Lazarov, Cohen, Liberman, & Dar, 2015; Lazarov, Dar, Liberman, & Oded, 2012a) or emotions (Dar et al., 2016) led to actual impairment in the relevant task performance. These findings may suggest that the performance deficits in cognitive tasks documented in our meta-analysis (see also Abramovitch et al., 2013; Shin et al., 2014) may be partially caused by the impaired confidence of OCD participants.
From another theoretical perspective, over- and under-confidence are both examples of biases in metacognition (i.e. the process of monitoring one's own cognitive processes). Resonating with our findings, several researchers have suggested that OCD is associated with deficits in metacognition (e.g. Ben Shachar, Lazarov, Goldsmith, Moran, & Dar, 2013; Hauser, Allen, Consortium, Rees, & Dolan, 2017). In current theorizing, metacognition is typically broken down into two distinct components – bias, as reported here, and sensitivity, which is the ability to discriminate accurate from inaccurate performance (Fleming & Lau, 2014). According to a recent hierarchical model of metacognition (Seow, Rouault, Gillan, & Fleming, 2021), metacognition is shaped through an interplay between multiple hierarchical levels of metacognitive estimation; hence a confidence bias, as detected in our analysis, can result from an impaired local level sensitivity component affecting up-stream a more global bias. As far as we know, only two experimental studies have attempted to measure specific components of metacognition in relation to OCD (Ben Shachar et al., 2013; Hauser et al., 2017). Unfortunately, these studies, which relied on non-clinical samples, used different tasks and assessment methods and reached contradicting results – whereas Hauser et al. (2017) concluded that high-OCD participants had deficient metacognitive sensitivity, Ben Shachar et al. (2013) did not.
The finding of under-confidence in OCD may also indicate that in judging their own behavior, participants with OCD were more influenced by their prior beliefs than by directly observed data (such as task difficulty and task performance). As noted above, several studies have documented that people with OCD tend to distrust their cognitive functions (e.g. Cougle et al., 2007; Hermans et al., 2008, 2003; Nedeljkovic et al., 2009; Nedeljkovic & Kyrios, 2007). Such prior beliefs can have a top-down effect on the interpretation of sensory evidence, diminishing its weight in the inferential process (Knill & Pouget, 2004; Sherman, Seth, Barrett, & Kanai, 2015). Similar processes have been integrated into a recent hierarchical model of metacognition (Seow et al., 2021), which assumes that global self-belief can influence downstream the local components of performance estimation, leading to biased meta-cognitive estimates.
At present, the ideas sketched above are clearly speculative, and their examination requires much further study. Specifically, research using newly developed computational models (Hauser et al., 2017; Seow & Gillan, 2020; Vaghi et al., 2017) might lead to more precise delineation of the underlying components and processes making up the apparent metacognitive deficit in OCD. We believe that a better mapping of these metacognitive deficits is important for understanding the pervasive doubt experienced by many individuals suffering from OCD. Down the road, it might also guide attempts to help OCD clients to cope with their doubts and related symptoms, such as repeated checking and requests for reassurance. For example, understanding the role of difficulties in accessing internal states on confidence in cognitive performance may lead to interventions designed to improve access to internal states. To the extent that people with OCD rely on prior beliefs regarding their cognitive function rather than on observed or experienced evidence, they might be encouraged and even trained to increase reliance on bottom-up processes by focusing on their present experience (e.g. by learning mindfulness techniques; see discussion in Dar et al., 2021).
In conclusion, the present review and meta-analysis indicates that people with OCD display both performance deficits and under-confidence in a variety of cognitive tasks. Future research might provide more fine-tuned data in regard to both of these effects, explore the causal relationships between them, and suggest ways in which such findings can be used to facilitate the understanding and treatment of people with OCD.
Acknowledgements
We thank Avital Horev for her invaluable help with searching and screening the studies. We are also grateful to Michael Borenstein for consulting on the meta-analysis and commenting on earlier drafts of the manuscript.
The notes appear after the main text.
Notes
Notably, checking may be motivated by other factors, such as fear of causing harm, the wish to avoid guilt, or reducing ‘not just right’ feelings (for a recent review see Strauss et al., 2020).
In fact, only one study of those included in the analysis (Dar et al., 2000) incorporated a comparison group with anxiety disorders; all others included only non-clinical control groups.
While other mental disorders may also be associated with abnormalities in confidence, most of these abnormalities are in the direction of exaggerated overconfidence (Hoven et al., 2019). The only exception appears to be major depression, but extant evidence is sparse and inconsistent.
Author contributions
Reuven Dar and Amit Lazarov conceived and designed the analysis and the pre-registration. Reuven Dar and Amit Lazarov performed the analysis and wrote the first draft of the paper. Gal Yardeni conducted the systematic search and the screening process. Noam Sarna contributed to writing the paper, particularly the discussion of meta-cognition, and provided summaries of previous research studies. All authors contributed to and have approved the final manuscript.
Financial support
This study was supported by the Israeli Science Foundation (Grant number 1156/11). The Israeli Science Foundation had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Conflict of interest
All four authors declare that they have no conflict of interest.
References
- Abramovitch, A., Abramowitz, J. S., & Mittelman, A. (2013). The neuropsychology of adult obsessive-compulsive disorder: A meta-analysis. Clinical Psychology Review, 33(8), 1163–1171. 10.1016/j.cpr.2013.09.004. [DOI] [PubMed] [Google Scholar]
- Babineau, J. (2014). Product review: Covidence (systematic review software). Journal of the Canadian Health Libraries Association/Journal de l'Association des bibliothèques de la santé du Canada, 2(35), 68–71. [Google Scholar]
- Ben Shachar, A., Lazarov, A., Goldsmith, M., Moran, R., & Dar, R. (2013). Exploring metacognitive components of confidence and control in individuals with obsessive-compulsive tendencies. Journal of Behavior Therapy and Experimental Psychiatry, 44(2), 255–261. 10.1016/j.jbtep.2012.11.007. [DOI] [PubMed] [Google Scholar]
- Borenstein, M. (2019). Common mistakes in meta-analysis and how to avoid them. Englewood: Biostat. [Google Scholar]
- Borenstein, M., Hedges, L. V., Higgins, J. P., & Rothstein, H. R. (2009). Introduction to meta-analysis. Hoboken: Wiley. [Google Scholar]
- Borenstein, M., Hedges, L. V., Higgins, J. P., & Rothstein, H. R. (2015). Comprehensive meta-analysis (version 3) (software). Englewood: Biostat. [Google Scholar]
- Boschen, M. J., & Vuksanovic, D. (2007). Deteriorating memory confidence, responsibility perceptions and repeated checking: Comparisons in OCD and control samples. Behaviour Research and Therapy, 45(9), 2098–2109. 10.1016/j.brat.2007.03.009. [DOI] [PubMed] [Google Scholar]
- Boyer, P., & Lienard, P. (2006). Why ritualized behavior? Precaution systems and action parsing in developmental, pathological and cultural rituals. Behavioral and Brain Sciences, 29(6), 595–613. 10.1017/S0140525x06009332. [DOI] [PubMed] [Google Scholar]
- Cabrera, A. R., McNally, R. J., & Savage, C. R. (2001). Missing the forest for the trees? Deficient memory for linguistic gist in obsessive-compulsive disorder. Psychological Medicine, 31(6), 1089–1094. 10.1017/s0033291701004354. [DOI] [PubMed] [Google Scholar]
- Cougle, J. R., Salkovskis, P. M., & Thorpe, S. J. (2008). ‘Perhaps you only imagined doing it’: Reality-monitoring in obsessive-compulsive checkers using semi-idiographic stimuli. Journal of Behavior Therapy and Experimental Psychiatry, 39(3), 305–320. 10.1016/j.jbtep.2007.08.001. [DOI] [PubMed] [Google Scholar]
- Cougle, J. R., Salkovskis, P. M., & Wahl, K. (2007). Perception of memory ability and confidence in recollections in obsessive-compulsive checking. Journal of Anxiety Disorders, 21(1), 118–130. 10.1016/j.janxdis.2006.03.015. [DOI] [PubMed] [Google Scholar]
- Dar, R. (2004). Elucidating the mechanism of uncertainty and doubt in obsessive-compulsive checkers. Journal of Behavior Therapy and Experimental Psychiatry, 35(2), 153–163. 10.1016/j.jbtep.2004.04.006. [DOI] [PubMed] [Google Scholar]
- Dar, R., Eden, T., van Dongen, M., Hauschildt, M., & Liberman, N. (2019). Obsessive-compulsive tendencies predict seeking proxies for understanding. Journal of Behavior Therapy and Experimental Psychiatry, 64, 87–91. [DOI] [PubMed] [Google Scholar]
- Dar, R., Lazarov, A., & Liberman, N. (2016). How can I know what I'm feeling? Obsessive-compulsive tendencies and induced doubt are related to reduced access to emotional states. Journal of Behavior Therapy and Experimental Psychiatry, 52, 128–137. 10.1016/j.jbtep.2016.04.004. [DOI] [PubMed] [Google Scholar]
- Dar, R., Lazarov, A., & Liberman, N. (2021). Seeking proxies for internal states (SPIS): Towards a novel model of obsessive-compulsive disorder. Behaviour Research and Therapy, 147, 103987. 10.1016/j.brat.2021.103987. [DOI] [PubMed] [Google Scholar]
- Dar, R., Rish, S., Hermesh, H., Taub, M., & Fux, M. (2000). Realism of confidence in obsessive-compulsive checkers. Journal of Abnormal Psychology, 109(4), 673–678. [DOI] [PubMed] [Google Scholar]
- Dar, R., Lazarov A., & Yardeni G (2020). Subjective Confidence in Obsessive-Compulsive Disorder: Systematic Review and Meta-Analysis. Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020208869.
- Duval, S., & Tweedie, R. (2000). Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics, 56(2), 455–463. 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- Egger, M., Smith, G. D., Schneider, M., & Minder, C. (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ, 315(7109), 629–634. 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehrlinger, J., Mitchum, A. L., & Dweck, C. S. (2016). Understanding overconfidence: Theories of intelligence, preferential attention, and distorted self-assessment. Journal of Experimental Social Psychology, 63, 94–100. 10.1016/j.jesp.2015.11.001. [DOI] [Google Scholar]
- Ezrati, O., Friedman, J., & Dar, R. (2019). Attenuation of access to internal states in high obsessive-compulsive individuals might increase susceptibility to false feedback: Evidence from a visuo-motor hand-reaching task. Journal of Behavior Therapy and Experimental Psychiatry, 65, 101445. [DOI] [PubMed] [Google Scholar]
- Ezrati, O., Sherman, E., & Dar, R. (2018). High obsessive-compulsive individuals may have attenuated access to internal cues associated with active movement: Evidence from a head repositioning study. Journal of Behavior Therapy and Experimental Psychiatry, 60, 1–4. 10.1016/j.jbtep.2018.02.004. [DOI] [PubMed] [Google Scholar]
- Fischhoff, B., Slovic, P., & Lichtenstein, S. (1977). Knowing with certainty: The appropriateness of extreme confidence. Journal of Experimental Psychology: Human Perception and Performance, 3(4), 552–564. 10.1037/0096-1523.3.4.552. [DOI] [Google Scholar]
- Fleming, S. M., & Lau, H. C. (2014). How to measure metacognition. Frontiers in Human Neuroscience, 8, 443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa, E. B., Amir, N., Gershuny, B., Molnar, C., & Kozak, M. J. (1997). Implicit and explicit memory in obsessive-compulsive disorder. Journal of Anxiety Disorders, 11(2), 119–129. [DOI] [PubMed] [Google Scholar]
- Furukawa, T. A., Reijnders, M., Kishimoto, S., Sakata, M., DeRubeis, R. J., Dimidjian, S., … Jarrett, R. B. (2020). Translating the BDI and BDI-II into the HAMD and vice versa with equipercentile linking. Epidemiology and Psychiatric Sciences, 29, e24, 1–13. 10.1017/S2045796019000088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Göz, İ., Karahan, S. K., & Tekcan, A. İ. (2016). Individuals with obsessive-compulsive disorder are less prone to false memories. Journal of Obsessive-Compulsive and Related Disorders, 10, 62–68. 10.1016/j.jocrd.2016.05.004. [DOI] [Google Scholar]
- Hauser, T. U., Allen, M., Consortium, N., Rees, G., & Dolan, R. J. (2017). Metacognitive impairments extend perceptual decision making weaknesses in compulsivity. Scientific Reports, 7(1), 6614. 10.1038/s41598-017-06116-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hermans, D., Engelen, U., Grouwels, L., Joos, E., Lemmens, J., & Pieters, G. (2008). Cognitive confidence in obsessive-compulsive disorder: Distrusting perception, attention and memory. Behaviour Research and Therapy, 46(1), 98–113. 10.1016/j.brat.2007.11.001. [DOI] [PubMed] [Google Scholar]
- Hermans, D., Martens, K., De Cort, K., Pieters, G., & Eelen, P. (2003). Reality monitoring and metacognitive beliefs related to cognitive confidence in obsessive-compulsive disorder. Behaviour Research and Therapy, 41(4), 383–401. 10.1016/S0005-7967(02)00015-3. [DOI] [PubMed] [Google Scholar]
- Hoven, M., Lebreton, M., Engelmann, J. B., Denys, D., Luigjes, J., & Van Holst, R. J. (2019). Abnormalities of confidence in psychiatry: An overview and future perspectives. Translational Psychiatry, 9(1), 1–18. 10.1038/s41398-019-0602-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janet, P. (1903). Les obsessions et la psychasthénie. Paris: Alcan. [Google Scholar]
- Johnson, D. D. P., & Fowler, J. H. (2011). The evolution of overconfidence. Nature, 477(7364), 317–320. 10.1038/nature10384. [DOI] [PubMed] [Google Scholar]
- Karadag, F., Oguzhanoglu, N., Ozdel, O., Atesci, F. C., & Amuk, T. (2005). Memory function in patients with obsessive compulsive disorder and the problem of confidence in their memories: A clinical study. Anxiety, 6, 8. [PubMed] [Google Scholar]
- Knill, D. C., & Pouget, A. (2004). The Bayesian brain: The role of uncertainty in neural coding and computation. Trends in Neurosciences, 27(12), 712–719. [DOI] [PubMed] [Google Scholar]
- Koriat, A., Lichtenstein, S., & Fischhoff, B. (1980). Reasons for confidence. Journal of Experimental Psychology: Human Learning and Memory, 6(2), 107–118. 10.1037/0278-7393.6.2.107. [DOI] [Google Scholar]
- Korotitsch, W. J. (2004). Subjective judgments in obsessive-compulsive disorder: Test of a cognitive model of the “feeling of incompleteness” [Doctoral dissertation]. The University of North Carolina at Greensboro. [Google Scholar]
- Lazarov, A., Cohen, T., Liberman, N., & Dar, R. (2015). Can doubt attenuate access to internal states? Implications for obsessive-compulsive disorder. Journal of Behavior Therapy and Experimental Psychiatry, 49, 150–156. 10.1016/j.jbtep.2014.11.003. [DOI] [PubMed] [Google Scholar]
- Lazarov, A., Dar, R., Liberman, N., & Oded, Y. (2012a). Obsessive-compulsive tendencies and undermined confidence are related to reliance on proxies for internal states in a false feedback paradigm. Journal of Behavior Therapy and Experimental Psychiatry, 43(1), 556–564. 10.1016/j.jbtep.2011.07.007. [DOI] [PubMed] [Google Scholar]
- Lazarov, A., Dar, R., Liberman, N., & Oded, Y. (2012b). Obsessive-compulsive tendencies may be associated with attenuated access to internal states: Evidence from a biofeedback-aided muscle tensing task. Consciousness and Cognition, 21(3), 1401–1409. 10.1016/j.concog.2012.07.002. [DOI] [PubMed] [Google Scholar]
- Lazarov, A., Friedman, A., Comay, O., Liberman, N., & Dar, R. (2020). Obsessive-compulsive symptoms are related to reduced awareness of emotional valence. Journal of Affective Disorders, 272, 28–37. [DOI] [PubMed] [Google Scholar]
- Lazarov, A., Liberman, N., Hermesh, H., & Dar, R. (2014). Seeking proxies for internal states in obsessive-compulsive disorder. Journal of Abnormal Psychology, 123(4), 695–704. 10.1037/abn0000004. [DOI] [PubMed] [Google Scholar]
- Marton, T., Samuels, J., Nestadt, P., Krasnow, J., Wang, Y., Shuler, M., … Nestadt, G. (2019). Validating a dimension of doubt in decision-making: A proposed endophenotype for obsessive-compulsive disorder. PLoS One, 14(6), e0218182. 10.1371/journal.pone.0218182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNally, R. J., & Kohlbeck, P A. (1993). Reality monitoring in obsessive-compulsive disorder. Behaviour Research and Therapy, 31(3), 249–253. [DOI] [PubMed] [Google Scholar]
- Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Annals of Internal Medicine, 151(4), 264–269. 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- Moore, D. A., & Healy, P. J. (2008). The trouble with overconfidence. Psychological Review, 115(2), 502–517. 10.1037/0033-295X.115.2.502. [DOI] [PubMed] [Google Scholar]
- Moritz, S., Jacobsen, D., Willenborg, B., Jelinek, L., & Fricke, S. (2006). A check on the memory deficit hypothesis of obsessive-compulsive checking. European Archives of Psychiatry and Clinical Neuroscience, 256(2), 82–86. [DOI] [PubMed] [Google Scholar]
- Moritz, S., Kloss, M., von Eckstaedt, F. V., & Jelinek, L. (2009a). Comparable performance of patients with obsessive-compulsive disorder (OCD) and healthy controls for verbal and nonverbal memory accuracy and confidence: Time to forget the forgetfulness hypothesis of OCD?. Psychiatry Research, 166(2-3), 247–253. [DOI] [PubMed] [Google Scholar]
- Moritz, S., Rietschel, L., Jelinek, L., & Bauml, K. H. (2011). Are patients with obsessive-compulsive disorder generally more doubtful? Doubt is warranted!. Psychiatry Research, 189(2), 265–269. 10.1016/j.psychres.2011.07.023. [DOI] [PubMed] [Google Scholar]
- Moritz, S., Ruhe, C., Jelinek, L., & Naber, D. (2009b). No deficits in nonverbal memory, metamemory and internal as well as external source memory in obsessive-compulsive disorder (OCD). Behaviour Research and Therapy, 47(4), 308–315. [DOI] [PubMed] [Google Scholar]
- Moritz, S., Wahl, K., Zurowski, B., Jelinek, L., Hand, I., & Fricke, S. (2007). Enhanced perceived responsibility decreases metamemory but not memory accuracy in obsessive-compulsive disorder (OCD). Behaviour Research and Therapy, 45(9), 2044–2052. 10.1016/j.brat.2007.03.003. [DOI] [PubMed] [Google Scholar]
- Nedeljkovic, M., & Kyrios, M. (2007). Confidence in memory and other cognitive processes in obsessive-compulsive disorder. Behaviour Research and Therapy, 45(12), 2899–2914. 10.1016/j.brat.2007.08.001. [DOI] [PubMed] [Google Scholar]
- Nedeljkovic, M., Moulding, R., Kyrios, M., & Doron, G. (2009). The relationship of cognitive confidence to OCD symptoms. Journal of Anxiety Disorders, 23(4), 463–468. 10.1016/j.janxdis.2008.10.001. [DOI] [PubMed] [Google Scholar]
- Ouellet-Courtois, C., Wilson, S., & O'Connor, K. (2018). Cognitive confidence in obsessive-compulsive disorder: A systematic review and meta-analysis. Journal of Obsessive-Compulsive and Related Disorders, 19, 77–86. 10.1016/j.jocrd.2018.08.003. [DOI] [Google Scholar]
- Prims, J. P., & Moore, D. A. (2017). Overconfidence over the lifespan. Judgment and Decision Making, 12(1), 29–41. [PMC free article] [PubMed] [Google Scholar]
- Radomsky, A. S., Dugas, M. J., Alcolado, G. M., & Lavoie, S. L. (2014). When more is less: Doubt, repetition, memory, metamemory, and compulsive checking in OCD. Behaviour Research and Therapy, 59, 30–39. 10.1016/j.brat.2014.05.008. [DOI] [PubMed] [Google Scholar]
- Rapoport, J. L. (1989). The boy who couldn't stop washing: The experience & treatment of obsessive-compulsive disorder. New York: Dutton. [Google Scholar]
- Reed, G. F. (1985). Obsessional experience and compulsive behaviour: A cognitive structural approach. New York: Academic Press. [Google Scholar]
- Seow, T. X. F., & Gillan, C. M. (2020). Transdiagnostic phenotyping reveals a host of metacognitive deficits implicated in compulsivity. Scientific Reports, 10(1), 1–11. 10.1038/s41598-020-59646-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seow, T., Rouault, M., Gillan, C. M., & Fleming, S. M. (2021). How local and global metacognition shape mental health. Biological Psychiatry, 90(7), 436–446. 10.1016/j.biopsych.2021.05.013. [DOI] [PubMed] [Google Scholar]
- Shapiro, D. (1965). Neurotic styles. New York: Basic Books. [Google Scholar]
- Sherman, M. T., Seth, A. K., Barrett, A. B., & Kanai, R. (2015). Prior expectations facilitate metacognition for perceptual decision. Consciousness and Cognition, 35, 53–65. 10.1016/j.concog.2015.04.015. [DOI] [PubMed] [Google Scholar]
- Shin, N. Y., Lee, T. Y., Kim, E., & Kwon, J. S. (2014). Cognitive functioning in obsessive-compulsive disorder: A meta-analysis. Psychological Medicine, 44(6), 1121–1130. 10.1017/s0033291713001803. [DOI] [PubMed] [Google Scholar]
- Sterne, J. A., Egger, M., & Smith, G. D. (2001). Systematic reviews in health care: Investigating and dealing with publication and other biases in meta-analysis. BMJ, 323(7304), 101–105. 10.1136/bmj.323.7304.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauss, A. Y., Fradkin, I., McNally, R. J., Linkovski, O., Anholt, G. E., & Huppert, J. D. (2020). Why check? A meta-analysis of checking in obsessive-compulsive disorder: Threat vs. distrust of senses. Clinical Psychology Review, 75, 101807. 10.1016/j.cpr.2019.101807. [DOI] [PubMed] [Google Scholar]
- Tekcan, A. İ., Topçuoğlu, V., & Kaya, B. (2007). Memory and metamemory for semantic information in obsessive-compulsive disorder. Behaviour Research and Therapy 45(9), 2164–2172. 10.1016/j.brat.2006.10.002. [DOI] [PubMed] [Google Scholar]
- Tobena, A., Marks, I., & Dar, R. (1999). Advantages of bias and prejudice: An exploration of their neurocognitive templates. Neuroscience and Biobehavioral Reviews, 23(7), 1047–1058. [DOI] [PubMed] [Google Scholar]
- Vaghi, M. M., Luyckx, F., Sule, A., Fineberg, N. A., Robbins, T. W., & De Martino, B. (2017). Compulsivity reveals a novel dissociation between action and confidence. Neuron, 96(2), 348–354. e344. 10.1016/j.neuron.2017.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zell, E., & Krizan, Z. (2014). Do people have insight into their abilities? A metasynthesis. Perspectives on Psychological Science, 9(2), 111–125. 10.1177/1745691613518075. [DOI] [PubMed] [Google Scholar]
- Zitterl, W., Urban, C., Linzmayer, L., Aigner, M., Demal, U., Semler, B., & Zitterl-Eglseer, K. (2001). Memory deficits in patients with DSM-IV obsessive-compulsive disorder. Psychopathology, 34(3), 113–117. 10.1159/000049292. [DOI] [PubMed] [Google Scholar]