Abstract
This cohort study examines racial and ethnic differences in the duration of buprenorphine treatment for opioid use disorder in the US from 2006 to 2020.
Buprenorphine is used to treat opioid use disorder (OUD) and reduce overdose risk.1 Duration of buprenorphine treatment is a measure of quality of care2; longer retention is associated with superior clinical outcomes.3 Racial and ethnic minority patients are more likely to discontinue buprenorphine treatment earlier than White patients.4 To our knowledge, no nationally representative studies have examined buprenorphine treatment duration over time across racial and ethnic groups. This information is needed to close the racial and ethnic gap in treatment retention for OUD.
Methods
This cohort study analyzed a random sample of buprenorphine prescriptions in IQVIA Longitudinal Prescription Data that included race and ethnicity information and were filled from January 2006 to December 2020 (eMethods in the Supplement). The Mass General Brigham institutional review board exempted the study from review and waived informed consent because data were not obtained through participant interaction. We followed the STROBE reporting guideline.
The start of a new treatment episode was defined as the date a prescription was filled after more than 14 days (30 and 60 days in sensitivity analyses) without a buprenorphine supply. If 2 or more prescription claims overlapped, the overlapped days were added to the end of the final prescription to determine episode duration. Since the distribution of episode duration was right-skewed, we investigated the median value over time. We also examined the percentage of buprenorphine episodes lasting at least 180 days.2 We compared both outcome measures across racial and ethnic groups using analysis of variance. Locally weighted scatterplot smoothing was used to visualize trends over time. Secondary analyses examined disparities stratified by age and sex. Data were analyzed with R, version 4.13.
Results
Among 11 250 354 buprenorphine prescriptions, 866 904 treatment episodes (Table) were contributed by 240 923 patients (median age, 37 years [range, 12-85 years]; 57.2% male); 8.1% were Black, 6.3% Hispanic, 84.1% White, and 1.5% other race and ethnicity. The median number of sequential prescriptions in a treatment episode was 3 (IQR, 1-10); median prescription duration was 14 days (IQR, 7-30 days).
Table. Demographic Characteristics and Number of Buprenorphine Treatment Episodes From 2006 to 2020, Stratified by Racial and Ethnic Groups.
| Characteristic | Treatment episodes, No. (%) | ||||
|---|---|---|---|---|---|
| All (N = 866 904) | Black patients (n = 70 402) | Hispanic patients (n = 54 820) | White patients (n = 729 166) | Other patients (n = 12 516)a | |
| Age at episode start, y | |||||
| 12-34 | 369 729 (42.6) | 25 673 (36.5) | 22 268 (40.6) | 316 356 (43.4) | 5432 (43.4) |
| 35-54 | 368 493 (42.5) | 31 367 (44.6) | 24 733 (45.1) | 307 079 (42.1) | 5314 (42.5) |
| 55-85 | 128 682 (14.8) | 13 362 (19.0) | 7819 (14.3) | 105 731 (14.5) | 1770 (14.1) |
| Sex | |||||
| Female | 371 149 (42.8) | 36 175 (51.4) | 23 316 (42.5) | 306 207 (42.0) | 5451 (43.6) |
| Male | 495 750 (57.2) | 34 227 (48.6) | 31 504 (57.5) | 422 954 (58.0) | 7065 (56.4) |
| Unspecified | 5 (0.0) | 0 | 0 | 5 (0.0) | 0 |
| Region | |||||
| Midwest | 150 754 (17.4) | 13 309 (18.9) | 5231 (9.5) | 130 287 (17.9) | 1927 (15.4) |
| Northeast | 178 985 (20.6) | 10 760 (15.3) | 12 603 (23.0) | 153 564 (21.1) | 2058 (16.4) |
| South | 316 296 (36.5) | 35 916 (51.0) | 15 652 (28.6) | 261 220 (35.8) | 3508 (28.0) |
| West | 122 498 (14.1) | 3613 (5.1) | 15 496 (28.3) | 99 596 (13.6) | 3793 (30.3) |
| Unspecified | 98 371 (11.3) | 6804 (9.7) | 5838 (10.6) | 84 499 (11.6) | 1230 (9.8) |
| Payment type | |||||
| Cash | 111 450 (12.9) | 8437 (12.0) | 6409 (11.7) | 94 990 (13.0) | 1614 (12.9) |
| Medicaid | 72 537 (8.4) | 7699 (10.9) | 6257 (11.4) | 57 109 (7.8) | 1472 (11.8) |
| Medicare | 163 (0.0) | 7 (0.0) | 14 (0.0) | 140 (0.0) | 2 (0.0) |
| Medicare Part D | 66 487 (7.7) | 7212 (10.2) | 4394 (8.0) | 53 946 (7.4) | 935 (7.5) |
| Third party | 616 267 (71.1) | 47 047 (66.8) | 37 746 (68.9) | 522 981 (71.7) | 8493 (67.9) |
| Episode duration ≥180 d | 218 433 (25.2) | 16 555 (23.5) | 12 062 (22.0) | 186 943 (25.6) | 2873 (23.0) |
| Calendar year | |||||
| 2006 | 7343 (0.8) | 405 (0.6) | 395 (0.7) | 6426 (0.9) | 117 (0.9) |
| 2007 | 14 870 (1.7) | 965 (1.4) | 782 (1.4) | 12 944 (1.8) | 179 (1.4) |
| 2008 | 22 919 (2.6) | 1543 (2.2) | 1295 (2.4) | 19 815 (2.7) | 266 (2.1) |
| 2009 | 31 578 (3.6) | 2209 (3.1) | 1685 (3.1) | 27 338 (3.7) | 346 (2.8) |
| 2010 | 40 726 (4.7) | 2773 (3.9) | 2340 (4.3) | 35 079 (4.8) | 534 (4.3) |
| 2011 | 52 616 (6.1) | 3662 (5.2) | 2883 (5.3) | 45 395 (6.2) | 676 (5.4) |
| 2012 | 60 982 (7.0) | 4375 (6.2) | 3524 (6.4) | 52 234 (7.2) | 849 (6.8) |
| 2013 | 68 397 (7.9) | 5104 (7.2) | 4118 (7.5) | 58 259 (8.0) | 916 (7.3) |
| 2014 | 70 456 (8.1) | 5280 (7.5) | 4419 (8.1) | 59 793 (8.2) | 964 (7.7) |
| 2015 | 71 081 (8.2) | 5521 (7.8) | 4526 (8.3) | 60 033 (8.2) | 1001 (8.0) |
| 2016 | 73 493 (8.5) | 6121 (8.7) | 4678 (8.5) | 61 604 (8.4) | 1090 (8.7) |
| 2017 | 78 528 (9.1) | 6820 (9.7) | 4994 (9.1) | 65 494 (9.0) | 1220 (9.7) |
| 2018 | 83 922 (9.7) | 7665 (10.9) | 5641 (10.3) | 69 337 (9.5) | 1279 (10.2) |
| 2019 | 94 372 (10.9) | 8914 (12.7) | 6591 (12.0) | 77 398 (10.6) | 1469 (11.7) |
| 2020 | 95 621 (11.0) | 9045 (12.8) | 6949 (12.7) | 78 017 (10.7) | 1610 (12.9) |
Other patients include Central Asian, East Asian, South Asian, Southeast Asian, Caribbean non-Hispanic, Polynesian, and Native American. Race and ethnicity were ascertained from IQVIA Longitudinal Prescription Data.
The overall median treatment duration was 50 days (IQR, 48-51 days) (Figure, A), with a slightly increasing trend from 2017 to 2020. Durations differed significantly across racial and ethnic groups, with White patients consistently having the longest durations. Moreover, treatment duration among White patients increased starting in 2017 but consistently decreased among Black patients from 2014 and Hispanic patients from 2009. Disparities remained when examining mean treatment duration over time.
Figure. Trends in Buprenorphine Episode Duration in the US From 2006 to 2020, Aggregated and Stratified by Racial and Ethnic Groups .
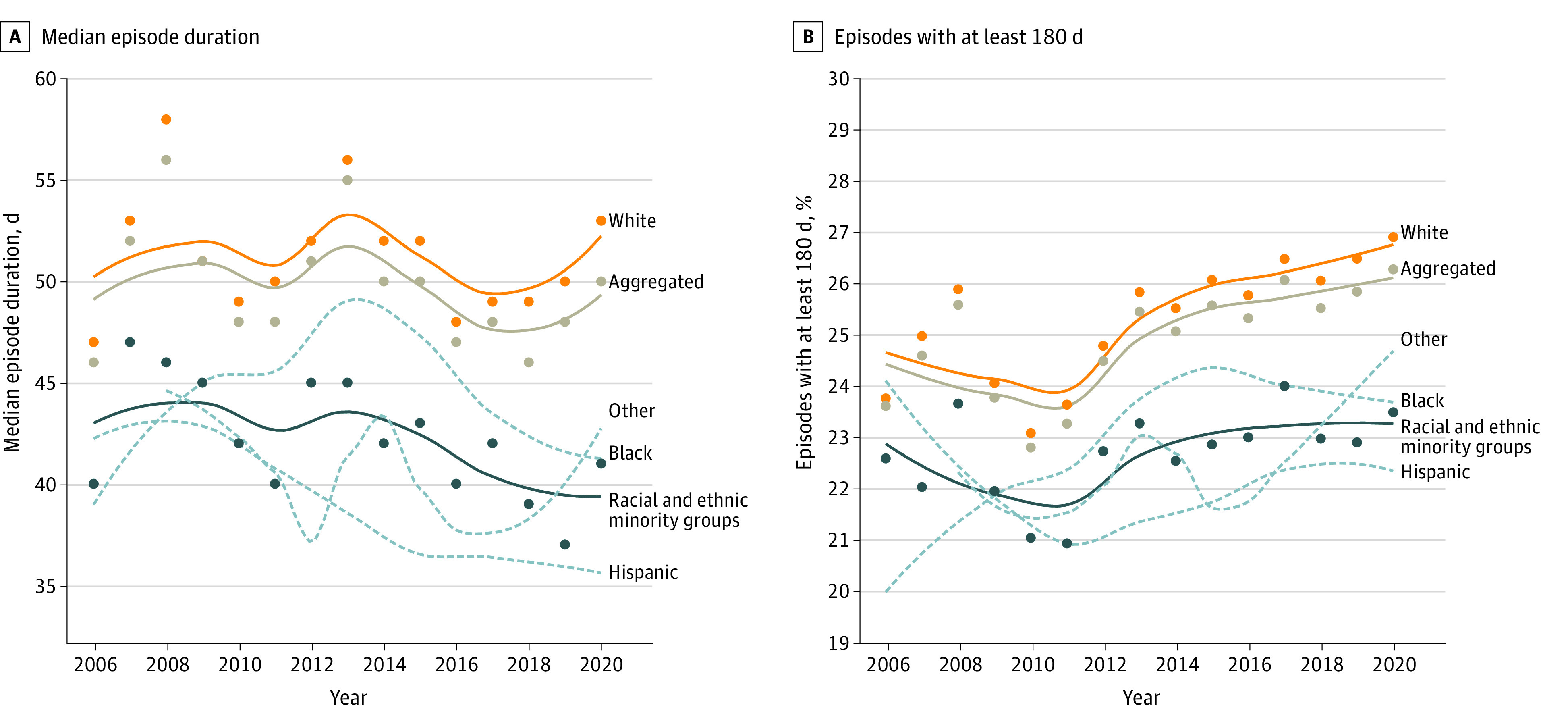
Other includes Central Asian, East Asian, South Asian, Southeast Asian, Caribbean non-Hispanic, Polynesian, and Native American. Data points for other racial and ethnic groups in 2006 and 2007 are not presented due to the small sample size.
Overall, 22.8% to 26.3% of episodes were at least 180 days (Figure, B). Racial and ethnic minority populations consistently had fewer buprenorphine episodes of at least 180 days vs White patients. From 2011, the percentage of episodes of at least 180 days increased among all racial and ethnic groups; however, beginning in 2016, this trend reversed for Black patients. The sensitivity and secondary analyses consistently showed racial and ethnic disparities in buprenorphine treatment duration.
Discussion
The results showed that racial and ethnic disparities in buprenorphine treatment duration increased between 2006 and 2020, particularly during more recent years. Trends in treatment duration identified using only aggregated data may mask underlying disparities, leading to a distorted perspective among researchers. Limitations include basing estimated durations on prescriptions dispensed rather than actual use and increasing coverage of IQVIA data over time, which may have introduced biases. We could not examine multiethnic or multiracial experiences or account for off-label use of buprenorphine to treat pain.
The observed heterogeneity in buprenorphine treatment duration among racial and ethnic groups may reflect disproportionate structural barriers in treatment retention for OUD. Racial and ethnic inequities in social determinants of health, such as access to education, employment, and medical care, could affect substance use treatment initiation, engagement, and outcomes.5,6 In addition, drug overdose mortality has recently increased, especially among racial and ethnic minority populations.6 Closing the racial and ethnic gaps in buprenorphine treatment duration could be a potential approach to reducing opioid overdoses.
eMethods
eReference
References:
- 1.Wakeman S. Shifting focus to evidence-based management of substance use disorders. Ann Intern Med. 2022;175(5):753-754. doi: 10.7326/M22-0150 [DOI] [PubMed] [Google Scholar]
- 2.National Quality Forum . Behavioral health 2016-2017: final report. August 2017. Accessed March 14, 2022. https://www.qualityforum.org/Publications/2017/08/Behavioral_Health_2016-2017_Final_Report.aspx
- 3.Williams AR, Samples H, Crystal S, Olfson M. Acute care, prescription opioid use, and overdose following discontinuation of long-term buprenorphine treatment for opioid use disorder. Am J Psychiatry. 2020;177(2):117-124. doi: 10.1176/appi.ajp.2019.19060612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weinstein ZM, Kim HW, Cheng DM, et al. Long-term retention in office based opioid treatment with buprenorphine. J Subst Abuse Treat. 2017;74:65-70. doi: 10.1016/j.jsat.2016.12.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jordan A, Quainoo S, Nich C, Babuscio TA, Funaro MC, Carroll KM. Racial and ethnic differences in alcohol, cannabis, and illicit substance use treatment: a systematic review and narrative synthesis of studies done in the USA. Lancet Psychiatry. 2022;9(8):660-675. doi: 10.1016/S2215-0366(22)00160-2 [DOI] [PubMed] [Google Scholar]
- 6.Kariisa M, Davis NL, Kumar S, et al. Vital signs: drug overdose deaths, by selected sociodemographic and social determinants of health characteristics—25 states and the District of Columbia, 2019-2020. MMWR Morb Mortal Wkly Rep. 2022;71(29):940-947. doi: 10.15585/mmwr.mm7129e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods
eReference


