Abstract
BACKGROUND
Few adolescents with depression receive treatment in accordance with national guidelines. This quality improvement project took place in 11 primary care practices with the primary aim of increasing the percentage of teens with depression who received follow-up care within 6 weeks of diagnosis and within 3 months, once stable.
METHODS
The primary strategy was external practice facilitation for 12 months. The change process used goal setting and plan-do-study-act cycles to identify and implement change ideas. A preanalysis and postanalysis was completed to evaluate process change, provider confidence, and patient improvement.
RESULTS
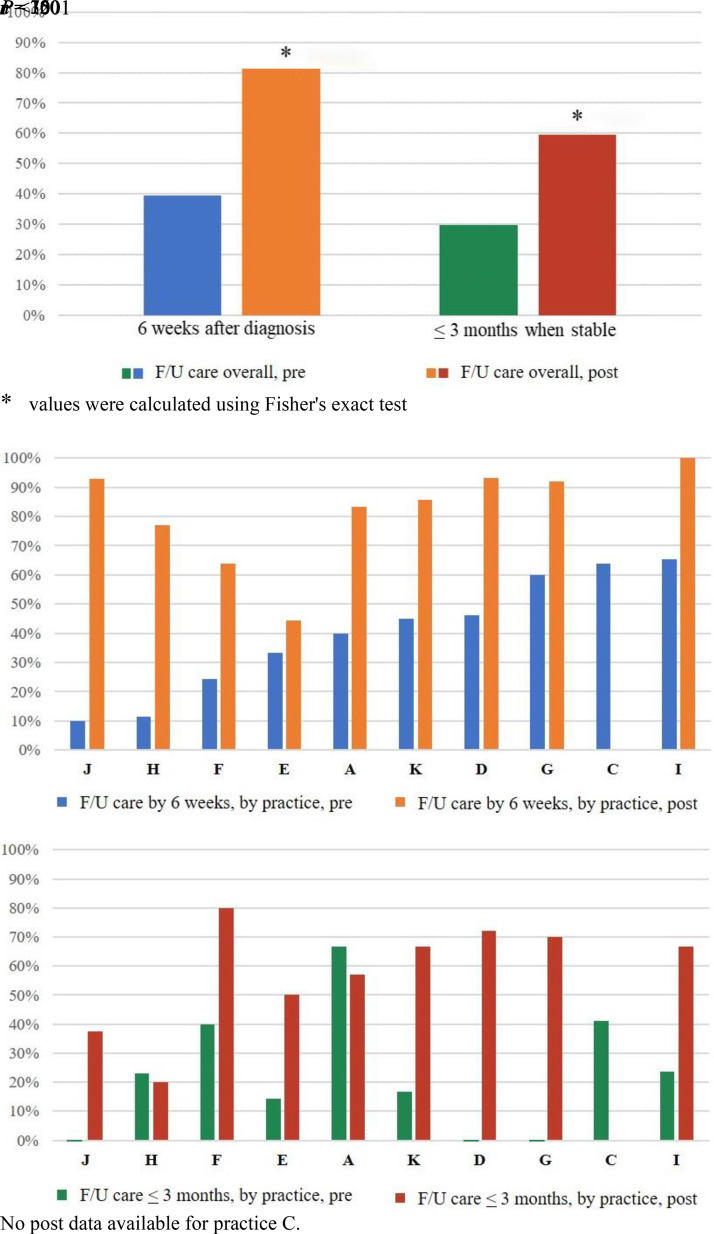
Randomly selected samples of 199 and 217 charts of teens newly diagnosed with depression were reviewed before and after the intervention, respectively. Chart data for these measurements was provided by 10 and 9 practices, respectively. The percentage of patients with follow-up care within 6 weeks after diagnosis increased from 40% to 81% (P < .001), the percentage with a follow-up visit within 3 months once stable increased from 30% to 60% (P < .001), and the percentage in remission at 6 months increased from 7% to 21% (P < .001). Providers reported increased confidence to diagnose and manage depression, assess severity, provide pharmacotherapy, and educate families.
CONCLUSIONS
Practices improved follow-up care for teens with depression. In addition, providers experienced an improvement in their confidence to diagnose and manage depression. Working with a facilitator, each practice implemented standardized systems to provide effective care in the medical home, increase providers’ confidence to address this common problem, and improve patient outcomes.
Adolescent depression is a common problem.1,2 Effective treatments are available, including selective serotonin reuptake inhibitors (SSRIs) and psychotherapy, but are underused,3,4 increasing risk for school dropout, substance abuse, and suicide.5–8 In 2018, suicide rates among adolescents in the United States had reached their highest level in 20 years, making suicide the second-highest cause of death in this age group.9–11 Most recently, the coronavirus disease 2019 (COVID-19) pandemic has exacerbated the need for widespread access to mental health care.12 For many teens, fear, loss, and isolation associated with the pandemic have increased stress, depression, anxiety, and suicide risk.13 The need to provide these teens with effective treatment is urgent and growing.
Pediatric primary care providers (PCPs) are well-positioned to provide care for adolescents with depression because they typically have a longstanding, trusting relationship with the patient and family.14 However, with limited mental health training for pediatricians, PCPs have been reluctant to provide depression care.4,15 The American Academy of Pediatrics has encouraged practice change by publishing resources and guidelines to support the delivery of effective mental health care including for depression,4,16–18 but few pediatric providers are aware of these resources and uptake is modest.16
We surveyed local PCPs in 2011 and 201719,20 and found an increasing willingness to provide depression care, perhaps because they see the distress in their patients and have experienced difficulty accessing care from child psychiatrists and therapists.17 In 2017, by self-report, 76% screened for depression with a validated tool and 95% prescribed SSRIs. However, only 47%, felt confident in providing depression care, 46% expected patients to return for follow-up visits, and 26% were aware of national guidelines.20 Their uncertainty about the adequacy of their efforts to provide care for adolescent depression led to a quality improvement (QI) initiative within our practice-based research network.
A 6-member advisory board of 4 general pediatricians, 1 parent, and 1 psychologist convened for the project and considered opportunities for improvement informed by their experience, the local survey data,19,20 and the Guidelines for Adolescent Depression in Primary Care (GLAD-PC), published in 2018.4,17 They decided to focus initial improvement efforts on implementing systematic follow-up care because they identified follow-up care as a care gap that was in urgent need of improvement, critical to improving patient outcomes, and feasible to address with a QI approach. GLAD-PC-recommended follow-up activities are summarized in Table 1. Because most primary care practices lack the resources to participate in meaningful QI endeavors,21,22 the primary strategy of the project was external practice facilitation to enable providers and staff to successfully engage in the change process together. The change process, guided by the Institute for Healthcare Improvement Model for Improvement, used key driver diagrams, goal setting, and plan-do-study-act (PDSA) cycles to identify and implement change ideas.23 The primary aim of the project was to increase the percentage of teens who received follow-up care within 6 weeks of diagnosis of depression and within 3 months, once stabilized.4,24 Secondary aims were to assess the use of a quantitative tool (the Patient Health Questionnaire-9 Modified for Adolescents [PHQ-A]25–27) to monitor symptoms at follow-up visits, patient outcomes and assess provider confidence for depression care activities.
TABLE 1.
GLAD-PC Recommendations Relevant for Follow-Up Care for an Adolescent Newly Diagnosed With Depression
| Initial management |
| Educate and counsel families and patients about depression and treatment optionsa |
| Establish a safety plan which includes restricting lethal means, engaging a concerned third party, and developing an emergency communication mechanisma |
| Develop a treatment plan, set treatment goals and initiate treatmenta |
| Assess for suicidal ideation and riska |
| Facilitate patient and parental self-managementa |
| Follow-up management |
| Develop a regular and frequent monitoring schedule for emergence of adverse events, ongoing depressive symptoms, risk of suicide, adherence to treatment, new or ongoing environmental stressorsa |
| Perform systematic and regular tracking of goals and outcomes from treatment. Once stabilized, follow-up appointments should occur monthly initially, but no longer than every 3-moa |
| Monitor symptoms during treatment with a quantitative tool such as PHQ-9a,b |
| Check-in within 1-wk of starting treatmena |
| Assess response to change in medication every 2–4 wka |
| Reassess diagnosis and treatment if no improvement by 6–8 wka |
| Continue medication for 6–12 mo after full resolution of symptomsa |
| Management adjustment if symptom remission not reached |
| If using antidepressant medication, increase to maximum dosage as needed and tolerated, monitoring for side-effects, symptom resolution and improved functioninga |
| Change to another medication or add therapy if maximum dose is reached for 4–6 wk and no or partial response, or side-effects occur.a Follow a tapering or switching schedulea |
| If not improved or partially improved, consider consultation with mental health specialista |
From American Psychiatric Association Mental Health Performance Measures (https://www.psychiatry.org/psychiatrists/practice/quality-improvement/mental-health-performance-measures).
Methods
Context
The Washington University Pediatric and Adolescent Ambulatory Research Consortium (WU PAARC), a practice-based research network of community pediatricians established in 2002, was the site for the QI initiative. WU PAARC comprises 36 community-based practices that serve demographically diverse pediatric patients in the St. Louis metropolitan area. All practices were invited to participate and informed that participants who had meaningful participation in the change effort were eligible for points toward Maintenance of Certification Part 4 requirements.28 No other incentives were provided.
Eleven practices (53 providers) volunteered between October 2018 and April 2019 (Table 2). Two practices provided access to an on-site licensed counselor for care coordination, care plan management, and counseling.
TABLE 2.
Characteristics of Participating Practices
| Patient Demographicsa | ||||||
|---|---|---|---|---|---|---|
| Practice | Participating Providers | Total Providers | Location | Medical Record | Medicaid (%) | African American (%) |
| J | 2 MD/1 PA | 3 | Suburban | EMR | 13 | 13 |
| H | 6 MD | 7 | Urban | EMR | 18 | 42 |
| F | 3 MD | 3 | Suburban | EMR | 7 | <10 |
| E | 4 MD/1 PNP | 5 | Suburban | Paper | 0 | 5 |
| A | 2 MD | 2 | Suburban | Paper | 0 | 20 |
| Kb | 3 MD/1 PNP | 4 | Suburban | EMR | 18 | 9 |
| D | 6 MD/2 PNP | 9 | Suburban | EMR | 20 | Not available |
| G | 4 MD/1 PNP | 5 | Suburban | EMR | 35 | 10 |
| C | 3 MD/1 PNP | 6 | Suburban | EMR | 20 | 20 |
| Ib | 5 MD/1 PNP | 7 | Urban | EMR | 2 | 5 |
| B | 7 MD | 9 | Suburban | Paper | 3 | 15 |
EMR, electronic medical record; MD, medical doctor; PA, physician assistant; PF QI, prior QI project with practice facilitation; PNP, pediatric nurse practitioner.
Patient demographics by self-report from practice-based research network database.
Practice had a licensed counsellor in-house.
Concurrent with the launch of our QI project, was the start of the Missouri Child Psychiatry Access Project (MO-CPAP). This initiative, modeled on the Massachusetts Child Psychiatry Access Project,29 provides free, same-day, telephonic psychiatry consultations for PCPs caring for mental health issues. WU PAARC encouraged all PCPs to use this resource and facilitated enrollment to the service. For this project, we did not track MO-CPAP use.
Intervention Development
Resources to support the QI intervention (Table 3 and Supplemental Information) were identified and developed by the WU PAARC team and physician advisors, including an expert in adolescent medicine. The advisory board reviewed educational materials for adolescents and families available from multiple sources, including the GLAD-PC toolkit,24 and selected some for adoption. New tools were developed to address providers’ needs, as well as brief educational videos for providers and staff. Two pediatricians pilot tested these resources. As reported by the facilitators, these support materials were appreciated by providers. Popular resources included the 1-page guides for pharmacotherapy and assessment of suicidal risk and the Excel spreadsheet to use for patient tracking.
TABLE 3.
Resources and Tools Developed to Support Practice Facilitation
| Purpose | Resource/Tool |
|---|---|
| Goal selection | Management of adolescent Depression in Primary Care Key Driver diagram. Aim 1 and Aim 2a |
| Guidelines for Adolescent Depression in Primary Care (GLAD-PC): Part 1 and Part 24,17 | |
| Summary of GLAD-PC Part 1 and 2 Recommendationsa | |
| Adolescent Depression Treatment Planss | |
| IHI Model for Improvement (http://www.ihi.org/resources/Pages/HowtoImprove/default.aspx) | |
| Baseline data reporta | |
| Depression management | SSRI Recommendations and Dosinga |
| Recommendations for Discontinuing SSRIs for Adolescent Depressiona | |
| Guidance for Black Box Warning for Anti-Depressantsa | |
| Videos | |
| Screening for Depressiona | |
| Interpreting Screener Resultsa | |
| Making a Treatment Plana | |
| Two-Week Follow-Upa | |
| Four-Week Follow-Upa | |
| When Patients and Caregivers Disagreea | |
| Patient Care Resources | |
| Provider Depression Follow-up Visit Checklista | |
| Protocol for 2-Week Follow-Up Phone Call a | |
| Provider Depression Monitoring Sheeta | |
| Safety Planning for Depressed Adolescents (https://www.thereachinstitute.org/images/pdfs/glad-pc-toolkit-2018.pdf) | |
| Linkage to MO-CPAP for provider consultations, patient care coordination, and provider education | |
| Psychotherapy support | Videos |
| Evidence-based Therapies for Adolescent Depressiona | |
| Cognitive Behavioral Therapy (CBT)a | |
| Selecting a CBT Therapista | |
| How to Know if Therapy is Workinga | |
| Suicide risk assessment and management | Assess For Safety and Suicide Risk Flowcharta |
| Validated tools: | |
| ASQ: Suicide Risk Screening Tool (https://www.nimh.nih.gov/sites/default/files/documents/research/research-conducted-at-nimh/asq-toolkit-materials/asq-tool/screening_tool_asq_nimh_toolkit.pdf) | |
| PHQ-9: Modified for Teens – (PHQ-A) (http://www.pedpsychiatry.org/pdf/depression/PHQ-9%20Modified%20for%20Teens.pdf) | |
| Videos: | |
| Addressing Suicidality and Referrala | |
| Assessing Suicidalitya | |
| Behavioral Health Response Crisis Hotlines (bhrstl.org) | |
| Communication with patients and families | Examples of scripts/documents to use to set expectations for care |
| Depression Care Plan for Parentsa | |
| Depression Care Plan for Adolescentsa | |
| Educational handouts, websites etc | |
| Tips for Helping a Depressed Teenager (Helpguide.org) | |
| Behavioral Health Response services (bhrstl.org) | |
| Self-Care Success! (https://www.thereachinstitute.org/images/pdfs/glad-pc-toolkit-2018.pdf)(updated version) | |
| Depression Care Plan for Parents * | |
| Depression Care Plan for Adolescents* | |
| Suicide: What Should I Know? (https://www.thereachinstitute.org/images/pdfs/glad-pc-toolkit-2018.pdf) | |
| Preventing Adolescent Suicide (https://jamanetwork.com/journals/jamapediatrics/fullarticle/2553099?resultClick=1) | |
| Videos: | |
| Selecting a CBT Therapista | |
| Making a Treatment Plana | |
| What Should I Do When Patients and Caregivers Disagree on Treatment Plan?a | |
| Patient tracking | Mental Health QI Tracking Worksheeta |
| Billing | Chapter IX: Billing: AAP Depression Coding Fact Sheet for Primary Care Clinicians (https://www.thereachinstitute.org/images/pdfs/glad-pc-toolkit-2018.pdf) |
| Billing for Adolescent Depression Carea |
AAP, American Academy of Pediatrics; ASQ, Ask Suicide-Screening Questions; BHR, Behavioral Health Response; CBT, Cognitive Behavioral Therapy; GLAD-PC, Guidelines for Adolescent Depression in Primary Care; IHI, Institute for Healthcare Improvement; MO CPAP, Missouri Child Psychiatry Access Project; PHQ-9, Patient Health Questionnaire-9; QI, quality improvement; SSRI, selective serotonin reuptake inhibitor.
Developed by project team.
The Intervention
At each site, the QI initiative was spearheaded by 1 of 2 external practice facilitators (total ∼1 full-time equivalent) trained for the project by the WU PAARC network coordinator, an experienced external facilitator. All facilitators had completed the University of Buffalo Practice Facilitator Certification Program.30
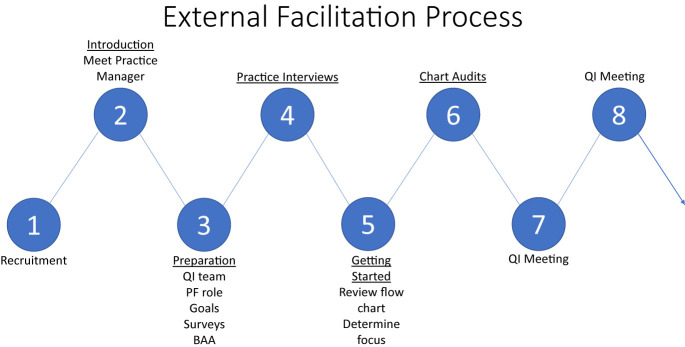
The approach to facilitation was the same at each practice (Fig 1). Initially, the WU PAARC network coordinator, who was well-known at the practices, introduced the facilitator to the practice manager and providers and briefly outlined the 12-month project. At the first QI team meeting, the facilitator introduced the providers and staff to practice facilitation, described the QI process, and set project expectations. Next, the facilitator conducted brief interviews with each provider and the practice manager with the goal of identifying their individual goals and current practice, understanding how the practice was organized, and identifying additional staff members for the QI team. This preparation work and thorough practice assessment were important to the change process as well as to initiate a relationship with the practice.
FIGURE 1.
The external facilitation process. BAA, bnusiness associates agreement; PF, practice facilitation; QI, quality improvement.
At the second QI team meeting, the facilitator presented a flowchart summary of current practice, highlighting consistencies and inconsistencies among providers. This was compared with a flowchart of GLAD-PC recommendations (see Supplemental Information) to help the team identify opportunities for improvement, set practice goals, and decide their first change idea and PDSA cycle. Concurrent to starting the QI process, the facilitator worked with the practice to measure depression care by using their medical records. Practices worked through multiple PDSA cycles to develop and implement standard protocols and office processes for follow-up care including standardizing documentation and diagnostic codes.
Throughout the change process, the facilitator arranged meetings, assisted with the collection and interpretation of data to inform decision making, and encouraged and supported the QI team, tailoring the facilitation process to the needs of the practice. In 3 practices, a 6-month assessment of progress toward project aims via a chart review (2 charts per provider) was used to increase motivation to continue. In addition, the facilitator promoted the use of the PHQ-A to monitor symptoms, identified and addressed training needs for providers and staff, shared experiences and successes among participating practices, and encouraged engagement with MO-CPAP. Interactions included monthly meetings with the QI team, as-needed individual meetings with providers and staff, training, phone calls, and E-mails. The facilitator provided meeting minutes and action plans after each QI team meeting.
Study of the Intervention
We completed a pre/post analysis. Primary and secondary outcomes were assessed by chart review and brief surveys to assess self-reported care delivery and confidence by using questions derived from previous local surveys.19,20 Measurement occurred at the start of the QI intervention and 12 months after the rollout of the facilitation process. Process measures were recorded by the facilitators. In October 2019, to support an application for funding to continue the program, all providers in practices who were close to completing the project were asked to report any benefits they felt had ensued for themselves, their practice, and their patients. Twelve providers from 7 practices replied with written statements. A summary of their feedback is provided with illustrative quotes.
Chart Review
Our goal was to get a meaningful sample from each practice, with representation from all providers. Chart review was restricted to 30 per practice because of limited resources. Eligible charts were those of patients 12 to 17 years old who were newly diagnosed with depression by their PCP and managed during the 12-month measurement period. Pre- and post measurements considered patients seen in the calendar year 2017 and 2019, respectively. For 1 practice that started the project later, the postassessment measurement was from June 1, 2019, to May 31, 2020. At each practice, eligible charts were identified by using billing data or medical records and randomly selected by the data analyst by using random numbers, balanced across providers. The facilitator reviewed charts in order from the randomized list, first confirming eligibility and then abstracting data by using a structured data collection tool. If < 30 charts were eligible for inclusion, all charts were reviewed. The number of charts varied from 15 to 30 (median 28) per practice, with ∼5 charts per provider.
Measures
Primary Outcome
The primary outcome was the percentage of teens with a new diagnosis of depression who received follow-up care within 6 weeks of diagnosis and within 3 months, once stabilized.4,24
Secondary Outcomes
The secondary outcomes were (1) the percentage of teens monitored with a PHQ-A25–27 at follow-up visits, (2) remission of depression (PHQ-A score < 5) at 6 months,31 and (3) provider confidence assessed as the percentage of providers scoring ≥ 6 on 7-point confidence scale (1, not confident and 7 highly confident) for depression care activities.
Process Measures
The process measures were the implementation of the intervention (duration of and time for facilitation and number of QI team meetings) and a cost estimate.
Analysis
Outcomes were measured in independent samples. Pre- and postcomparison of the primary and secondary outcomes were compared by using Fisher’s exact test. A probability of P < .05 (2-tailed) was used to determine statistical significance. All statistical analyses were performed by using R version 4.0.3.32 Patients newly diagnosed with depression < 6 weeks before the end of the measurement period were considered ineligible for the analysis of short-term follow-up care. A similar adjustment for eligibility was made for the assessment of 3-month follow-up visits.
Time series analysis was not used because of measurement difficulties and resource limitations. Newly diagnosed depressed patients were infrequent and could not easily be identified because charting and billing behaviors varied considerably among providers within and between practices. Chart review by the facilitator was needed to confirm the diagnosis requiring a site visit, and an extended measurement period was required to assess outcomes of interest. Because of resource limitations, we restricted chart review to 2 occasions, each using a 12-month measurement period.
Ethical Considerations
Business associates agreements were enacted between each practice and WU PAARC. This QI project was determined not to be human subject research by the Washington University Human Research Protection Office.
Results
Missing Data
Eleven practices participated in the project and received facilitation, with 10 and 9 practices providing charts for review before and after the intervention, respectively. Response rates for the before and after provider assessments were both 92%.
Measurement Samples
A randomly selected sample of 199 charts (from 10 practices) and 217 charts (from 9 practices) of teens newly diagnosed with depression was reviewed for the premeasures and postmeasures, respectively. Patients in both samples were similar for sex and age: predominantly female (68%), with a median age at diagnosis of 15 years (interquartile range, 14–16 years). Outcomes are presented in Table 4.
TABLE 4.
Outcome Measures Pre- and Post-QI Intervention to Improve Follow-Up Care for Adolescents Newly Diagnosed With Depression
| Factor | Preinterventiona (N = 199) | Postinterventiona (N = 217) | P |
|---|---|---|---|
| Primary outcome | |||
| Follow-up care, n (%) | |||
| At diagnosis, follow-up care (either call or visit) within 6 wk | 70/177b (40) | 160/197b (81) | <.001 |
| Once stable, follow-up care within 3-mo | 32/108c (30) | 75/126c (60) | <.001 |
| Secondary outcomes | |||
| PHQ-A use, n (%) | |||
| Proportion with PHQ-A used at diagnostic visit | 118/199 (59) | 186/217 (86) | <.001 |
| Proportion with PHQ-A used at least 1 follow-up visit | 38/113d (34) | 148/194d (76) | <.001 |
| Proportion with PHQ-A used at every follow-up visit | 20/113d (18) | 95/194d (49) | <.001 |
| Patient improvement | |||
| Proportion with remission at 6-mo | 7/107e (7) | 41/193e(21) | <.001 |
| Provider confidencef: | (N = 49) | (N = 47) | |
| Make a diagnosis of depression, n (%) | 18 (37) | 36 (77) | <.001 |
| Assess depression severity, n (%) | 8 (16) | 28 (60) | <.001 |
| Assess for suicidal intent, n (%) | 16 (33) | 25 (53) | .06 |
| Assess treatment response, n (%) | 13 (27) | 25 (53) | .01 |
| Prescribe SSRIs for initial treatment, n (%) | 28 (57) | 40 (85) | .003 |
| Prescribe second drug if partial or no benefit with first drug, n (%) | 7 (14) | 22 (47) | <.001 |
| Ability to educate patients and families, n (%) | 10 (20) | 29 (62) | <.001 |
PHQ-A, Patient Health Questionnaire-9 modified for teens;26 QI, quality improvement; SSRI, selective serotonin reuptake inhibitor.
Denominator varies as number of patients eligible for metric varies, depending on date of diagnosis.
Excluded from denominator if diagnosed in last 6 wk of the measurement period.
Excluded from denominator if diagnosed in last 3 mo of the measurement period.
Excluded from the denominator if no follow-up visit during the measurement period.
The percentage of patients who achieved remission (PHQ-A <5) at 6 mo after the initial elevated PHQ-A score. Excluded from the denominator if no follow-up visit within 6 mo.
Percent of providers scoring confidence >6 out of 7 (1, not confident to 7, highly confident).
Primary Outcomes
The percentage of newly diagnosed patients who had follow-up care within 6 weeks after diagnosis increased from 40% to 81% (P < .001), with improvement in all 9 practices that provided post data (Fig 2). Similarly, the percentage who had follow-up care within 3 months after their condition had stabilized increased from 30% to 60% (P < .001), with improvement in 7 of 9 practices who provided post data.
FIGURE 2.
Proportion of patients receiving depression follow-up care pre-/postintervention, overall and by practice. F/U, follow-up.
Secondary Outcomes
Use of Quantitative Tool to Monitor Symptoms
The percentage of patients with the PHQ-A recorded in ≥1 follow-up visit increased from 34% to 76% and the percentage with scores recorded at every follow-up visit increased from 18% to 49% (P < .001 for both).
Remission of Depression
Remission at 6 months increased from 7% to 21% (P < .001).
Provider Confidence
Provider confidence increased for making a diagnosis of depression, educating patients and families, prescribing SSRIs, and assessing severity, suicidal intent, and treatment response. Providers also reported increased use of a protocol to monitor treatment response (47% to 94%, P < .001), a quantitative tool to monitor change (40% to 87%, P < .001), and establishing a safety plan (64% to 89%, P = .003).
Process Measures
Implementation of the Intervention
Across the 11 practices, the duration of facilitation varied from 10 months to 16 months with an average of 16 QI team meetings/practice (range 8–26). Meeting duration varied from 34 to 59 minutes (average 48) with 2 to 11 attendees (average 7). Attendance at QI team meetings was high and PCPs rarely missed them.
Cost
We did not formally assess cost but estimate the cost to implement this program at 10 practices over 12 months to be $60c000 to $65c000 (assuming the facilitator works 2 hours per week per practice, holds on-site meetings, and uses tools/resources that are already developed).
Perceived Program Benefits
As illustrated by these quotes, providers felt that care delivery became more proactive, organized, and efficient. They became confident and empowered to provide depression care, and several reported improved job satisfaction.
“It has helped us to organize an efficient way to manage our patients with depression and anxiety. We have developed a protocol for first visits and follow-up visits, including a plan for scheduling follow up phone calls and follow up office visits.”
“We are screening our patient population for depression and anxiety on an ongoing basis and NOT just when in crisis.”
“I have benefitted from a review of the current guidelines …….as well as having access to multiple resources in the community and through MO-CPAP.”
“We have learned and developed methods for navigating these complex visits so that we all feel so much more comfortable diagnosing and treating adolescents with mental health issues.”
“…. I feel that this has enhanced my pediatric practice of medicine as mental health is vital and often overlooked.
Unexpected Benefits
Practices experienced an overall improvement in the diagnosis and management of depression. For example, the percentage of newly diagnosed patients who had their PHQ-A noted at diagnosis increased from 59% to 86% (P < .001). In addition, many providers used a “transdiagnostic approach to care”14 and used their new protocols for depression care to guide the management of anxiety. Practice representatives noted that a more structured approach to depression care resulted in the standardization of the billing process and that transitioning their protocols for depression care to telehealth as necessitated by the COVID-19 pandemic was easy.
Discussion
Our pediatric primary care QI initiative to improve care for adolescents with depression was impactful. Although the target for improvement was follow-up care, which improved significantly, all practices experienced an overall improvement in the diagnosis and management of depression. Practices that participated transformed how they provided care for this common disease, standardizing their approach to follow-up care delivery within the practice and sharing the work among a team of providers and staff. Building a system to provide care in accordance with national guidelines improved patient outcomes and increased provider confidence to deliver depression care in the medical home.
To be able to successfully establish practice-wide standardization of care delivery, PCPs needed to fundamentally change their orientation to care delivery, learn how to work as a team, and share work with staff. The facilitator provided the infrastructure and support needed for practice change, allowing PCPs to actively engage in the change process and work collaboratively over time. For example, reviewing the facilitator’s practice assessment enabled the QI team to identify variations among providers in care delivery, documentation, and billing. Collaborating to address this variation catalyzed change efforts. Many PCPs were unaware of the GLAD-PC guidelines and toolkit and welcomed the pragmatic educational resources provided for the project. Guided by the facilitator, they worked together to identify opportunities to use these resources in improvement activities. In most practices, depression care had rarely been discussed among providers or with staff. Meetings with the facilitator provided the opportunity to focus these discussions on optimizing and reorganizing care. External facilitation has been used successfully in adult primary care settings to affect practice change, with sustained benefits when tailored to practice needs, values, and processes.21,33
Primary care practice change is difficult.21 As noted by the American Academy of Pediatrics Task Force on Mental Health, to provide mental health care, providers must acquire new knowledge and skills and overcome other significant barriers to change, such as office processes and culture.16 Our project was focused on follow-up care as suggested by the advisory board, and the change process was complex. The time needed for change varied among practices, depending on the challenges they faced and their willingness to engage. All practices improved 6-week follow-up care and most improved long-term follow-up, with variability in the impact of the changes accomplished. We observed that practices that found it easy to work as a team and share the work of depression care worked through the change process more quickly and achieved more substantive results. For others, progress was slower and change goals were not fully realized in the 12-month project period. These findings are consistent with the literature and support the idea of adaptive reserve: an increased capacity for change gained by change experience, which is another benefit of participation in the facilitation process.34
Limitations to this project include our inability to fully attribute improvements to the intervention because of the lack of a comparator to control for secular trends and for some practices having previous QI efforts, our inability to disaggregate the effect of MO-CPAP, and infrequent measurements. The accuracy of our estimates may be limited by missing data, incomplete assessments, and failure to systematically document care provided. Also, measures of provider confidence and behavior have not been validated.
Conclusions
Our structured approach using external practice facilitation enabled pediatric primary care providers to integrate effective depression care for adolescents into their practice. Although the target of the QI intervention was follow-up care, there was an overall improvement in many aspects of depression care. The ∼12-month facilitator-led change process encouraged a team-based approach and included education, training, and support to identify and address practice-specific barriers to change. It resulted in standardized care, increased confidence of PCPs to address this common problem, and improved patient outcomes.
An important next step is scaling this effective approach to address the urgent need to provide effective mental health care for children and adolescents. Sharing resources developed for this project (see Supplemental Information) and using technology such as virtual meetings will reduce costs, and may speed the change process, although funding for the facilitator will be needed. Our experience suggests many benefits to this investment for providers, practices, and patients.
Acknowledgments
The thank the members of the Advisory Board for their invaluable advice. They included Drs. Trina Blythe, Alla Dorfman, Jerome O’Neil, David Sonderman, Karen Ruecker, and Melanie VanDyke.
Glossary
- COVID-19
coronavirus disease 2019
- GLAD-PC
Guidelines for Adolescent Depression in Primary Care
- MO-CPAP
Missouri Child Psychiatry Access Project
- PDSA
plan, do, study, act
- PHQ-A
patient health questionnaire-9 modified for adolescents
- PCP
pediatric primary care provider
- QI
quality improvement
- SSRI
selective serotonin reuptake inhibitor
- WU PAARC
Washington University Pediatric and Adolescent Ambulatory Research Consortium
Footnotes
Dr Garbutt conceptualized the project and designed tools, drafted the initial manuscript, and reviewed and revised the manuscript; Dr Plax conceptualized the project, designed tools, and reviewed and revised the manuscript; Dr Sterkel conceptualized the project, reviewed the data analyses, and reviewed and revised the manuscript; Ms Dodd conceptualized and operationalized the project, designed tools, coordinated, and supervised data collection and reviewed and revised the manuscript; Ms Rook and Ms Graham operationalized the project, designed tools, coordinated, and supervised data collection and reviewed and revised the manuscript; Ms Wang designed the database, conducted the initial analyses, and reviewed and revised the manuscript; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FUNDING: The project reported in this publication was supported by the Washington University Institute of Clinical and Translational Sciences grant UL1TR002345 from the National Center for Advancing Translational Sciences of the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official view of the National Institute of Health. Additional funding was provided by the Department of Pediatrics, Washington University and St. Louis Children’s Hospital. The funders did not participate in the work. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICTS OF INTEREST: The authors have indicated they have no conflicts of interest relevant to this article to disclose.
References
- 1. Perou R, Bitsko RH, Blumberg SJ, et al. ; Centers for Disease Control and Prevention (CDC) . Mental health surveillance among children--United States, 2005-2011. MMWR Suppl. 2013;62(2): 1–35 [PubMed] [Google Scholar]
- 2. Mojtabai R, Olfson M, Han B. National trends in the prevalence and treatment of depression in adolescents and young adults. Pediatrics. 2016;138(6):e20161878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. O’Connor BC, Lewandowski RE, Rodriguez S, et al. Usual care for adolescent depression from symptom identification through treatment initiation. JAMA Pediatr. 2016;170(4):373–380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cheung AH, Zuckerbrot RA, Jensen PS, Laraque D, Stein REK; GLAD-PC Steering Group . Guidelines for adolescent depression in primary care (GLAD-PC): part II. Treatment and ongoing management. Pediatrics. 2018;141(3):e20174082. [DOI] [PubMed] [Google Scholar]
- 5. Clayborne ZM, Varin M, Colman I. Systematic review and meta-analysis: adolescent depression and long-term psychosocial outcomes. J Am Acad Child Adolesc Psychiatry. 2019;58(1):72–79 [DOI] [PubMed] [Google Scholar]
- 6. Asarnow JR, Jaycox LH, Duan N, et al. Depression and role impairment among adolescents in primary care clinics. J Adolesc Health. 2005;37(6):477–483 [DOI] [PubMed] [Google Scholar]
- 7. National Institute of Mental Health . Major depression. Available at: https://www.nimh.nih.gov/health/statistics/major-depression.shtml#part_155031. Accessed February 22, 2021
- 8. Shain B; Committee on Adolescence . Suicide and suicide attempts in adolescents. Pediatrics. 2016;138(1):e20161420. [DOI] [PubMed] [Google Scholar]
- 9. Heron M. Deaths: leading causes for 2017. Natl Vital Stat Rep. 2019;68(6):1–77 [PubMed] [Google Scholar]
- 10. Miron O, Yu KH, Wilf-Miron R, Kohane IS. Suicide rates among adolescents and young adults in the United States, 2000-2017. JAMA. 2019;321(23):2362–2364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Curtin SC. State suicide rates among adolescents and young adults aged 10-24: United States, 2000-2018. Natl Vital Stat Rep. 2020;69(11):1–10 [PubMed] [Google Scholar]
- 12. Czeisler ME, Lane RI, Petrosky E, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic - United States, June 24-30, 2020. MMWR Morb Mortal Wkly Rep. 2020; 69(32):1049–1057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Leeb RT, Bitsko RH, Radhakrishnan L, Martinez P, Njai R, Holland KM. Mental health-related emergency department visits among children aged <18 years during the COVID-19 Pandemic - United States, January 1-October 17, 2020. MMWR Morb Mortal Wkly Rep. 2020; 69(45):1675–1680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Foy JM, Green CM, Earls MF; Committee on Psychosocial Aspects of Child and Family Health, Mental Health Leadership Work Group . Mental health competencies for pediatric practice. Pediatrics. 2019; 144(5):e20192757. [DOI] [PubMed] [Google Scholar]
- 15. Horwitz SM, Storfer-Isser A, Kerker BD, et al. Barriers to the identification and management of psychosocial problems: changes from 2004 to 2013. Acad Pediatr. 2015;15(6):613–620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Green CM, Foy JM, Earls MF; Committee on Psychosocial Aspects of Child and Family Health, Mental Health Leadership Work Group . Achieving the pediatric mental health competencies. Pediatrics. 2019;144(5):e20192758. [DOI] [PubMed] [Google Scholar]
- 17. Zuckerbrot RA, Cheung A, Jensen PS, Stein REK, Laraque D; GLAD-PC Steering Group . Guidelines for adolescent depression in primary care (GLAD-PC): part I. Practice preparation, identification, assessment, and initial management. Pediatrics. 2018;141(3):e20174081. [DOI] [PubMed] [Google Scholar]
- 18. Foy JM; American Academy of Pediatrics Task Force on Mental Health . Enhancing pediatric mental health care: algorithms for primary care. Pediatrics. 2010; 125(Suppl 3):S109–S125 [DOI] [PubMed] [Google Scholar]
- 19. Garbutt JM, Leege E, Sterkel R, Gentry S, Strunk RC. Providing depression care in the medical home: what can we learn from attention-deficit/hyperactivity disorder? Arch Pediatr Adolesc Med. 2012; 166(7):672–673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Garbutt J, Sterkel R, Ruecker K, Dodd S, Smith E, Plax K. Ready for the challenge of depression care in the medical home. Clin Pediatr (Phila). 2019;58(7):816–818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Crabtree BF, Nutting PA, Miller WL, et al. Primary care practice transformation is hard work: insights from a 15-year developmental program of research. Med Care. 2011;49(Suppl):S28–S35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Freed GL, Moran LM, Van KD, Leslie LK; Research Advisory Committee of the American Board of Pediatrics . Current workforce of general pediatricians in the United States. Pediatrics. 2016;137(4): e20154242. [DOI] [PubMed] [Google Scholar]
- 23. Institute for Healthcare Improvement . How to improve. Available at: www.ihi.org/resources/Pages/HowtoImprove/default.aspx. Accessed January 11, 2021
- 24. The REACH Institute . Guidelines for adolescent depression in primary care (GLAD-PC) toolkit. Available at: https://www.thereachinstitute.org/guidelines- for-adolescent-depression-primary-care. Accessed February 18, 2021
- 25. Johnson JG, Harris ES, Spitzer RL, Williams JB. The patient health questionnaire for adolescents: validation of an instrument for the assessment of mental disorders among adolescent primary care patients. J Adolesc Health. 2002; 30(3):196–204 [DOI] [PubMed] [Google Scholar]
- 26. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. American Academy of Child and Adolescent Psychiatry . PHQ-9: modified for teens. Available at: https://www.aacap.org/App_Themes/AACAP/docs/member_ resources/toolbox_for_clinical_practice_ and_outcomes/symptoms/GLAD-PC_ PHQ-9.pdf. Accessed May 10, 2021
- 28. The American Board of Pediatrics . Improving professional practice — quality improvement (part 4). Available at: https://www.abp.org/content/quality-improvement-part-4. Accessed August 30, 2021
- 29. Sarvet BD, Wegner L. Developing effective child psychiatry collaboration with primary care: leadership and management strategies. Child Adolesc Psychiatr Clin N Am. 2010;19(1):139–148 [DOI] [PubMed] [Google Scholar]
- 30. Agency for Healthcare Research and Quality, Patient Centered Medical Home Resource Center . Primary care practice facilitation curriculum. Available at: https://pcmh.ahrq.gov/page/primary- care-practice-facilitation-curriculum. Accessed June 2, 2021
- 31. Agency for Healthcare Research and Quality . Depression remission or response for adolescents and adults. Available at: https://www.ahrq.gov/sites/default/files/wysiwyg/pqmp/measures/chronic/chipra-244-fullreport.pdf. Accessed June 2, 2021
- 32. R. Version 4.0.3. Vienna, Austria: R Foundation for Statistical Computing; 2020 [Google Scholar]
- 33. Baskerville NB, Liddy C, Hogg W. Systematic review and meta-analysis of practice facilitation within primary care settings. Ann Fam Med. 2012;10(1):63–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Nutting PA, Crabtree BF, Stewart EE, et al. Effect of facilitation on practice outcomes in the National Demonstration Project model of the patient-centered medical home. Ann Fam Med. 2010;8(Suppl 1): S33–S44, S92 [DOI] [PMC free article] [PubMed] [Google Scholar]