Surgical necrotizing enterocolitis and spontaneous intestinal perforation might be associated with growth impairment but is not associated with adverse neurodevelopmental outcomes in ages 10 and 15 years.
Abstract
OBJECTIVES
Necrotizing enterocolitis (NEC) and spontaneous intestinal perforation (SIP) are complications in preterm infants associated with high morbidity, mortality, impaired growth, and neurodevelopmental (ND) outcomes. Few studies have reported growth or ND outcomes of infants born extremely preterm with NEC/SIP beyond early childhood. Here, we compared anthropometric and ND outcomes, at 10 and 15 years, for children with medical NEC, surgical NEC, SIP, and neither NEC nor SIP.
METHODS
Participants from the prospective longitudinal extremely low gestational age newborns study were evaluated at ages 10 and 15 years for anthropometrics, neurocognition, attention-deficit/hyperactivity disorder, epilepsy, and gross motor function.
RESULTS
At age 10 years, 889 children were followed-up (medical NEC = 138, surgical NEC = 33, SIP = 29, no NEC/SIP = 689), and 694 children were followed up-at 15 years. Children with medical NEC had similar weight, BMI, height, and head circumference compared with controls at both 10 and 15 years. At 15 years, children with surgical NEC had lower weight z-score (adjusted β: −0.75, 95% confidence interval [CI]: −1.25 to −0.25), lower BMI z-score (adjusted β: −0.55, 95% CI: −1.09 to −0.01), and lower height z-score (adjusted β: −0.65, 95% CI: −1.16 to −0.14). Children with SIP had lower weight and height z-scores at age 10 years when adjusted for sample attrition, but these differences were not significant when adjusted for confounders. We observed no differences in long-term ND outcomes.
CONCLUSIONS
Surgical NEC- and SIP-associated growth impairment may persist through late childhood. ND outcomes among school-aged children born extremely preterm with any NEC or SIP are no different from children without NEC/SIP.
What’s Known on the Subject:
The adverse impact of necrotizing enterocolitis (NEC) and spontaneous intestinal perforation in early childhood are well established, but less is known about outcomes in late childhood.
What This Study Adds:
We found that growth impairment associated with NEC and spontaneous intestinal perforation (SIP) may persist through late childhood. Neurodevelopmental outcomes in children with NEC or SIP were not different from children with no NEC/SIP.
Necrotizing enterocolitis (NEC) and spontaneous intestinal perforation (SIP) are gastrointestinal complications in preterm infants associated with high morbidity and mortality in extremely low birth weight (ELBW) infants.1 NEC is characterized by ischemic necrosis of the intestinal mucosa, severe inflammation, invasion by enteric gas-forming organisms, and dissection of gas into the bowel wall and portal venous system.2 Pathophysiology of SIP is distinct from NEC and typically presents as a focal intestinal perforation at the terminal ileum.3 Among ELBW infants, the incidence of NEC is ∼7%, whereas the incidence of SIP is 3% to 8%.4
Both NEC and SIP have been associated with increased risk of neurodevelopmental (ND) impairment (NDI). Severe NDI affects 25% to 59% of surviving infants with medical or surgical NEC, with most studies reporting outcomes up to 18 to 24 months.5–7 SIP is also associated with NDI, although most studies have been limited to 12 to 24 months follow-up.6,8 Few studies have reported ND outcomes with NEC and SIP in later childhood or at school age up to age 10 years with concerns for long-term NDI.9–14 NEC has also been associated with longer-term growth impairment, but data are conflicting. Two studies found no association between NEC and severe growth failure,11,15 whereas another study found poor growth outcomes at 18 to 22 months’ corrected age in infants with surgical NEC compared with infants without NEC.16
The objective of this study is to compare growth and ND outcomes at 10- and 15-years follow-up for school-aged children born extremely preterm (EP) who developed NEC or SIP during their NICU stay with controls who had neither NEC nor SIP. We hypothesized that both SIP and NEC would be associated with worse growth and ND outcomes when compared with infants with neither NEC nor SIP; and surgical NEC would be associated with worse growth and ND outcomes when compared with infants with medical NEC or SIP alone.
Methods
Data were derived from the extremely low gestational age newborns (ELGAN) study, a prospective, longitudinal study designed to identify characteristics and exposures that increase the risk of structural and functional neurologic disorders in ELGANs born preterm at 23 to 27 weeks’ gestational age (GA). Between 2002 and 2004, 1506 infants born in 14 participating institutions across 5 states in the United States were enrolled.17 The study protocol was approved by the institutional review board in each participating institution. The participants were followed up at 2,18 10,19 and 15 years of age.
Participants
Of 1222 infants who survived until discharge, 966 were eligible for follow-up assessment at age 10 years (on the basis of availability of data on levels of protein biomarkers in the first 2 postnatal weeks). A total of 889 (92%) participated in comprehensive ND and neurobehavioral assessments at 10 years and 694 (71.8%) completed the 15-year assessments. For the current study, children were categorized into 4 groups: medical NEC, surgical NEC, SIP, and no NEC/SIP, on the basis of diagnoses made during the NICU hospitalization. After infants were discharged from neonatal intensive care, research assistants reviewed their medical records and recorded whether a diagnosis was made of either NEC or SIP. For infants with NEC, a Bell’s classification stated in the medical record was recorded. Despite Bell’s classification having its own limitations of varying sensitivity and specificity, it is the most commonly used definition for NEC.20 If an infant had NEC but no Bell’s classification was listed, the research assistant assigned a classification using a manual containing descriptions of stages of NEC (stages I, IIa, IIb, and IIIa) or surgical (stage IIIb) on the basis of modified Bell’s classification.21 The study manual specified that infants without NEC be classified as having SIP if they “had a gastrointestinal perforation documented on radiograph and an isolated intestinal perforation was confirmed at the time of exploratory laparotomy or strongly suspected clinically (if managed with Penrose drain and exploratory laparotomy was not done).”
Growth Outcome at 10 and 15 Years
Height, weight, and head circumference (HC) were collected by a research assistant after all outer garments such as coats and shoes were removed. If children were unable to stand unsupported, either a wheelchair scale or the difference of the parent’s weight, plus child’s weight, and the parent’s weight alone was used for weight measurements. As a substitute for height in these subjects, the child’s length was measured while lying down. BMI was calculated using the following formula: BMI = weight in kilograms/(height in meters × height in meters). Height, weight, and HC were converted to z-scores on the basis of standard Centers for Disease Control and Prevention growth curves (https://www.cdc.gov/growthcharts/html_charts/bmiagerev.htm; https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm) using the Statistical Analysis Software program, and z-scores were used for further analysis. BMI, weight, and height at ages 10 and 15 years were transformed to z-scores using the LMS method (L: λ, M: μ, and S: σ method) in the Centers for Disease Control and Prevention Statistical Analysis Software macro.
Neurodevelopmental Outcomes at 10 and 15 Years
Motor function was assessed with the Gross Motor Function Classification System (GMFCS)22 at age 10 and 15 years. GMFCS classifications are level 0: normal; level 1: reduced speed or balance; level 2: difficulty walking and no ability to run or jump; level 3: walks using a handheld mobility device; level 4: self-mobility with limitations, including need of some powered mobility; and level 5: transported in a manual wheelchair. Identification of seizures and epilepsy involved a 2-stage process with initial parent’s questionnaire for seizure screening and a structured interview with a study coordinator followed by an open-ended interview with a pediatric epilepsy specialist per the study protocol.23
Cognitive outcomes at age 10 years were assessed with the School-Age Differential Ability Scales-II (DAS-II) Verbal and Nonverbal Reasoning subscales,24 which were averaged to create a full-scale IQ composite. In addition, a latent profile analysis (LPA) was conducted using DAS-II Verbal and Nonverbal Reasoning subscales, 2 DAS-II measures of working memory, and 5 NEPSY-II executive function subtests25 measuring attention, inhibitory control, and mental flexibility.26 The LPA identified 4 subgroups on the basis of similarities in profiles of IQ and executive function scores with similar patterns of performance across subtests that were classified as normal, low-normal, moderately impaired, and severely impaired. The age 10 LPA cognitive outcome classifications were dichotomized to 1, normal/low-normal, and 0, moderately impaired/severely impaired.
At age 15, full-scale IQ was assessed with Wechsler Abbreviated Scale of Intelligence-II.27 In addition, the National Institutes of Health Cognition Toolbox Battery28 was used to assess neuropsychological function, including verbal and executive control abilities. An LPA conducted on the Wechsler Abbreviated Scale of Intelligence-II verbal and nonverbal, and the 7 National Institutes of Health Cognition Toolbox Battery measures classified age 15 participants into normal, low-normal, and impaired subgroups (Table 1). LPA has been argued to provide a more sensitive assessment of cognitive function than IQ alone,26 and is likely to have better predicative value for future cognitive and adaptive function.29 The LPA variable was dichotomized to 1, normal/low-normal, and 0, severely impaired.
TABLE 1.
Baseline Demographic Characteristics of the Study Cohort
| Characteristics (N = 889) | No NEC/SIP, n = 689 | Medical NEC, n = 138 | Surgical NEC, n = 33 | SIP, n = 29 |
|---|---|---|---|---|
| Maternal age, y, n (%) | ||||
| <21 | 87 (12.6) | 23 (16.7) | 3 (9.1) | 2 (6.9) |
| 21–35 | 454 (65.9) | 92 (66.7) | 26 (78.8) | 22 (75.9) |
| >35 | 148 (21.5) | 23 (16.7) | 4 (12.1) | 5 (17.2) |
| Maternal education (12 = high school, 16 = college) | ||||
| ≤12 | 275 (41.0) | 59 (45.0) | 13 (39.4) | 8 (27.6) |
| >12−<16 | 148 (22.1) | 37 (28.2) | 7 (21.2) | 10 (34.5) |
| ≥16 | 247 (36.9) | 35 (26.7) | 13 (39.4) | 11 (37.9) |
| Maternal IQ, mean (SD) | ||||
| ≤−2 | 22 (3.4) | 7 (5.3) | 2 (6.3) | 2 (7.4) |
| >−2 to ≤−1 | 46 (7.1) | 8 (6.1) | 7 (21.9) | 1 (3.7) |
| >−1 to ≤1 | 477 (73.3) | 90 (68.7) | 18 (56.3) | 22 (81.5) |
| Public insurance, n (%) | ||||
| No | 446 (64.7) | 81 (58.7) | 26 (78.8) | 22 (75.9) |
| Yes | 243 (35.3) | 57 (41.3) | 7 (21.2) | 7 (24.1) |
| Race, n (%) | ||||
| Black | 167 (24.2) | 40 (29.2) | 8 (24.2) | 12 (42.9) |
| White | 445 (64.6) | 78 (56.9) | 23 (69.7) | 16 (57.1) |
| Other | 77 (11.2) | 19 (13.9) | 2 (6.1) | 0 (0.0) |
| Hispanic | ||||
| No | 627 (91.4) | 118 (85.5) | 27 (81.8) | 28 (96.6) |
| Yes | 59 (8.6) | 20 (14.5) | 6 (18.2) | 1 (3.4) |
| Histologic chorioamnionitis, n (%) | ||||
| Yes | 341 (53.4) | 67 (54.0) | 13 (44.8) | 18 (69.2) |
| Missing | 50 (7.3) | 14 (10.1) | 4 (12.1) | 3 (10.3) |
| Cesarean delivery, n (%) | ||||
| Yes | 466 (67.6) | 85 (61.6) | 23 (69.7) | 16 (55.2) |
| GA, wk, n (%) | ||||
| 23–24 | 131 (19.0) | 34 (24.6) | 11 (33.3) | 11 (37.9) |
| 25–26 | 305 (44.3) | 62 (44.9) | 18 (54.5) | 15 (51.7) |
| 27 | 253 (36.7) | 42 (30.4) | 4 (12.1) | 3 (10.3) |
| BW z-score, n (%) | ||||
| <−2 | 38 (5.5) | 9 (6.5) | 3 (9.1) | 3 (10.3) |
| ≥−2 to <−1 | 93 (13.5) | 20 (14.5) | 5 (15.2) | 2 (6.9) |
| Sex, n (%) | ||||
| Female | 345 (50.1) | 69 (50.0) | 10 (30.3) | 10 (34.5) |
| Male | 344 (49.9) | 69 (50.0) | 23 (69.7) | 19 (65.5) |
| WMD on neonatal ultrasound, n (%) | ||||
| Yes | 145 (21.0) | 28 (20.3) | 12 (36.4) | 3 (10.3) |
| Severe ROP, n (%) | ||||
| Yes | 78 (11.5) | 26 (19.0) | 9 (27.3) | 5 (17.2) |
| Chronic lung disease, n (%) | ||||
| Yes | 285 (41.7) | 64 (46.7) | 12 (36.4) | 19 (65.5) |
| Severe chronic lung disease, n (%) | ||||
| Yes | 56 (8.2) | 15 (10.9) | 7 (21.2) | 3 (10.3) |
| SNAP score | ||||
| <20 | 363 (53.5) | 74 (54.4) | 14 (43.8) | 9 (32.1) |
| 20–29 | 169 (24.9) | 31 (22.8) | 6 (18.8) | 9 (32.1) |
| 30+ | 146 (21.5) | 31 (22.8) | 12 (37.5) | 10 (35.7) |
| Cerebral palsy at 24 mo, n (%) | 67 (10.2) | 16 (12.2) | 5 (15.6) | 5 (18.5) |
| Bayley MDI <70 at 24 mo, n (%) | 149 (23.5) | 31 (25.2) | 11 (37.9) | 7 (29.2) |
| Bayley PDI <70 at 24 mo, n (%) | 174 (28.1) | 34 (27.9) | 14 (50.0) | 10 (43.5) |
| Mean weight z-score (SD) | −0.75 (1.34) | −0.48 (1.33) | −0.81 (1.27) | −0.80 (1.43) |
| Mean length z-score (SD) | −0.33 (1.27) | −0.22 (1.13) | −1.09 (2.84) | −0.53 (1.05) |
| Mean HC z-score (SD) | −0.22 (1.27) | −0.12 (1.45) | −0.83 (1.46) | −1.1 (1.45) |
MDI, mental developmental index; PDI, psychomotor developmental index; ROP, retinopathy of prematurity; SNAP, score for neonatal acute physiology; WMD, white matter damage.
For attention-deficit/hyperactivity (ADHD) assessment at age 10 years, 3 contexts were considered: the parent or caregiver completed the Child Symptom Inventory, Fourth Edition (CSI-4), the child’s current teacher was asked to complete the Child Symptom Inventory, Fourth Edition, Teacher Checklist, and information on the basis of the parent’s indication of the child having been diagnosed previously by a clinician to have ADHD. Participants were included in the ADHD symptom group if they met criteria in any 2 of the 3 contexts.30 At age 15, ADHD was assessed with the Mini International Neuropsychiatric Interview for Children and Adolescents. The Mini International Neuropsychiatric Interview for Children and Adolescents is a structured clinical diagnostic interview designed to assess the presence of current Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, and International Classification of Diseases, 10th Revision, psychiatric disorders in youth aged 6 to 17 years, and has been validated against the structured clinical interview for Diagnostic and Statistical Manual of Mental Disorders-III-R and against the World Health Organization-designed composite international diagnostic interview.31
Statistical Analysis
A directed acyclic graph was created on the basis of a priori knowledge, and birth weight z-score, GA, and sex were identified as variables requiring minimally sufficient adjustment. Multivariable analysis was performed, adjusting for birth weight z-score, GA, and sex, when comparing outcomes between no NEC/SIP group and medical NEC, surgical NEC, and SIP. Birth weight z-scores were derived from reference data based on 2013 Fenton preterm growth charts.32 GA was defined as a continuous variable in weeks. Because of sample attrition, inverse probability weighting was conducted to adjust for the dropout of subjects with necrotizing enterocolitis. Weights were given to each subject dependent on maternal education, maternal single status, public insurance, and severe chronic lung disease for growth outcomes. For ND outcomes, weights were dependent on the maternal education, maternal single status, public insurance, severe chronic lung disease, white matter damage, and severe retinopathy of prematurity. White matter damage was defined as the presence of either parenchymal echolucency (hypoechoic zone) and/or moderate to severe ventriculomegaly on a scan performed after the first 2 postnatal weeks.33 Generalized linear models were used for all crude, adjusted, and inverse probability weighted analyses. Differences were considered statistically significant if the corresponding P values were <.05. Confidence intervals (CIs) were constructed using α =.05.
Results
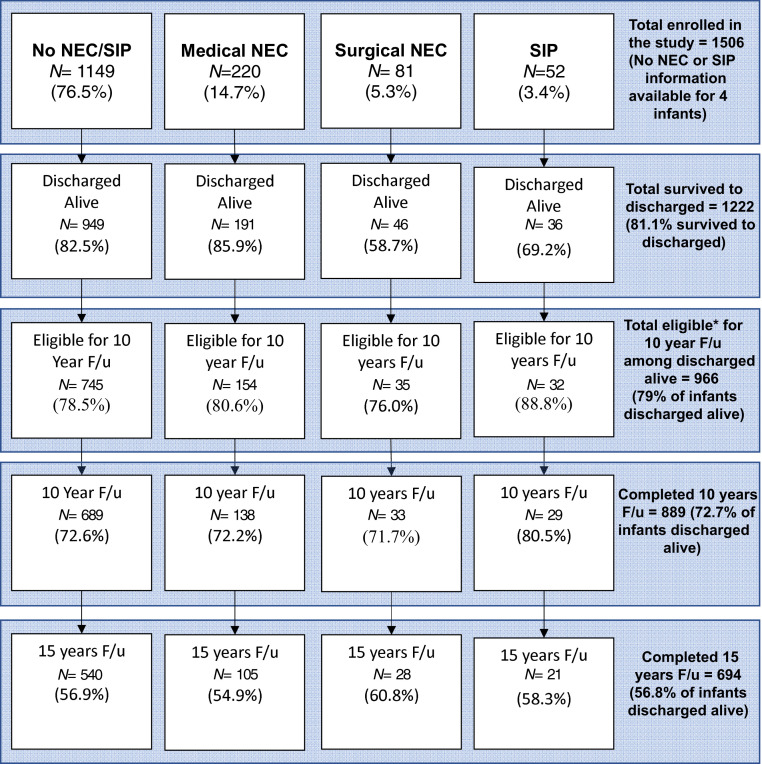
Among the 1506 infants enrolled in ELGAN study, 14.7% were diagnosed with medical NEC, 5.3% with surgical NEC, and 3.4% with SIP. Of the 1222 infants discharged alive from the NICU, 1198 survived to 10 years. Follow-up data were available from 889 (72.7%) children at 10 years and 694 (56.8%) at 15 years. A flow diagram of all participants and those who completed the follow-up visits is included (Fig 1). Among children followed up at the 10-year visit, 138 (15.5%) had medical NEC, 33 (3.7%) had surgical NEC, 29 (3.3%) had SIP, and 689 had no NEC/SIP. Among children followed up at the 15 years visit, 105 (15.1%) had medical NEC, 28 (4.0%) had surgical NEC, 21 (3.0%) had SIP, and 540 had no NEC/SIP (Fig 1).
FIGURE 1.
Flow diagram of all the patients enrolled in study and those that completed the follow-up visits. *Eligibility for follow-up assessment at 10 years of age was based on prespecified study protocols based on availability of data on levels of protein biomarkers in the first 2 postnatal weeks.
Baseline Demographic Characteristics
Infants with SIP and surgical NEC were more likely male, had lower GA, and lower birth weight compared with infants with no NEC/SIP. Infants with medical NEC had similar baseline demographic characteristics compared with infants with no NEC/SIP (Table 2).
TABLE 2.
10- and 15-Year Growth and Neurodevelopmental Outcomes
| All Mean (SD)or n (%) | No NEC/SIP, Mean (SD)or n (%) | Medical NEC, Mean (SD)or n (%) | Surgical NEC, Mean (SD)or n (%) | SIP, Mean (SD)or n (%) | |
|---|---|---|---|---|---|
| 10-y growth outcomes (N = 889) | |||||
| BMI mean (SD) | 17.8 (4.1) | 17.7 (4.0) | 18.2 (4.3) | 17.0 (3.1) | 17.3 (6.1) |
| z-score | −0.07 (1.46) | −0.06 (1.43) | 0.055 (1.58) | −0.25 (1.36) | −0.51 (1.59) |
| Weight mean (SD) | 33.5 (10.4) | 33.6 (10.2) | 34.4 (11.0) | 31.2 (7.3) | 31.2 (13.4) |
| z-score | −0.19 (1.40) | −0.18 (1.40) | −0.06 (1.33) | −0.43 (1.26) | -0.8 (1.76) |
| Height mean (SD) | 136.4 (8.8) | 136.6 (8.8) | 136.8 (8.8) | 134.8 (7.0) | 132.7 (8.3) |
| z-score | −0.27 (1.25) | −0.27 (1.24) | −0.24 (1.23) | −0.51 (0.95) | −0.8 (1.18) |
| HC mean (SD) | 52.5 (2.4) | 52.6 (2.3) | 52.5 (2.5) | 51.5 (2.2) | 51.6 (3.2) |
| 10-y ND outcomes (N = 889) | |||||
| ADHD | 152 (17.1%) | 122 (18.0%) | 20 (14.7%) | 7 (21.9%) | 3 (10.7%) |
| GMFCS >1 | 72 (8.1%) | 51 (7.7%) | 12 (9.2%) | 3 (9.7%) | 6 (22.2%) |
| Epilepsy | 66 (7.4%) | 54 (7.8%) | 9 (6.6%) | 3 (9.1%) | 0 (0.0%) |
| DAS-II FSIQ | 88.4 (20.0) | 88.9 (19.7) | 88.4 (20.0) | 84.6 (19.5) | 80.4 (24.6) |
| LPA classifications | |||||
| Normal | — | 242 (35.7%) | 43 (31.4%) | 8 (25.8%) | 7 (25.0%) |
| Low-normal | — | 280 (41.3%) | 58 (42.3%) | 12 (38.7%) | 10 (35.7%) |
| Moderate | — | 108 (15.9%) | 24 (17.5%) | 8 (25.8%) | 5 (17.9%) |
| Severely impaired | — | 48 (7.1%) | 12 (8.8%) | 3 (9.7%) | 6 (21.4%) |
| 15-y growth outcome (N = 694) | |||||
| BMI mean (SD) | 23.1 (6.3) | 23.1 (6.5) | 23.9 (5.6) | 20.8 (4.7) | 23.9 (8.8) |
| z-score | 0.41 (1.26) | 0.40 (1.26) | 0.63 (1.25) | −0.25 (1.36) | 0.35 (1.31) |
| Weight mean (SD) | 62.1 (18.7) | 62.0 (18.9) | 64.1 (18.9) | 53.1 (9.0) | 64.8 (24.6) |
| z-score | 0.23 (1.40) | 0.24 (1.36) | 0.40 (1.55) | −0.60 (1.22) | 0.14 (1.63) |
| Height mean (SD) | 163.5 (9.7) | 163.6 (9.5) | 162.9 (9.9) | 160.9 (11.0) | 164.1 (8.6) |
| z-score | −0.44 (1.15) | −0.41 (1.12) | −0.52 (1.20) | −1.07 (1.30) | −0.53 (1.05) |
| HC mean (SD) | 55.6 (2.9) | 55.5 (2.7) | 55.9 (3.5) | 54.2 (2.6) | 55.1 (4.1) |
| 15-y ND outcomes (N = 694) | |||||
| ADD or ADHD | 42 (6.0%) | 31 (6.1%) | 6 (6.1%) | 3 (11.5%) | 2 (12.5%) |
| Epilepsy | 51 (7.3%) | 40 (7.7%) | 8 (8.2%) | 2 (7.7%) | 1 (5.3%) |
| WASI-II FSIQ | 99.6 (17.9) | 100 (17.8) | 98.6 (18.1) | 92.5 (18.4) | 97.5 (18.2) |
| LPA classifications | |||||
| Severe | — | 74 (14.7%) | 19 (19.4%) | 5 (19.2%) | 6 (33.3%) |
| Low-Normal | — | 269 (53.5%) | 48 (49.0%) | 14 (53.8%) | 6 (33.3%) |
| Normal | — | 160 (31.8%) | 31 (31.6%) | 7 (26.9%) | 6 (33.3%) |
ADD, attention-deficit disorder; FSIQ: full-scale IQ; WASI-II: Wechsler Abbreviated Scale of Intelligence-II. —, not applicable.
Medical NEC and Outcomes
Children who had medical NEC had similar weight, BMI, height, and HC compared with children with no NEC/SIP at both age 10 and 15 years. This group also had similar neurodevelopmental outcomes as children with no NEC/SIP (Table 1, Table 3).
TABLE 3.
Crude Associations Between NEC and 10- and 15-Year Outcomes
| No NEC Nor SIP | Medical NEC | Surgical NEC | SIP | ||||
|---|---|---|---|---|---|---|---|
| Effect Estimate (β)/OR (95% CI) | P | Effect Estimate (β)/OR (95% CI) | P | Effect Estimate (β)/OR (95% CI) | P | ||
| Age 10 y | |||||||
| BMI z-score | Referent | 0.12 (−0.17 to 0.40) | .43 | −0.19 (−0.66 to 0.29) | .44 | −0.45 (−1.02 to 0.13) | .13 |
| Weight z-score | Referent | 0.12 (−0.12 to 0.37) | .32 | −0.25 (−0.69 to 0.19) | .27 | −0.62 (−1.26 to 0.02) | .06 |
| Height z-score | Referent | 0.03 (−0.20 to 0.25) | .81 | −0.24 (−0.57 to 0.10) | .17 | −0.53 (−0.96 to −0.09) | .02* |
| DAS-II FSIQ | Referent | −0.58 (−4.23 to 3.08) | .76 | −4.30 (−11.22 to 2.62) | .22 | −8.53 (−17.60 to 0.54) | .07 |
| LPAa | Referent | 1.21 (0.86–1.69) | .28 | 1.68 (0.87–3.24) | .12 | 2.16 (1.08–4.29) | .03* |
| Age 15 y | |||||||
| BMI z-score | Referent | 0.23 (−0.05 to 0.52) | .11 | −0.64 (−1.18 to −0.11) | .02* | −0.05 (−0.72 to 0.62) | .89 |
| Weight z-score | Referent | 0.16 (−0.19 to 0.51) | .37 | −0.84 (−1.32 to −0.35) | <.01* | −0.10 (−0.93 to 0.73) | .81 |
| Height z-score | Referent | −0.11 (−0.38 to 0.16) | .43 | −0.66 (−1.17 to −0.15) | .01* | −0.12 (−0.66 to 0.42) | .66 |
| WAS-II FSIQ | Referent | −1.83 (−5.91 to 2.25) | .38 | −7.87 (−15.3 to −0.47) | .04* | −2.88 (−11.9 to 6.18) | .53 |
| LPAb | Referent | 0.88 (0.58–1.34) | .56 | 0.77 (0.36–1.64) | .50 | 0.62 (0.25–1.53) | .30 |
FSIQ, full-scale IQ; OR, odds ratio; WASI-II, Wechsler Abbreviated Scale of Intelligence-II.
P ≤ .05.
Age-10 LPA outcome classifications were dichotomized to normal/low-normal and moderately impaired/severely impaired.
Age-15 LPA variable was dichotomized to normal/low-normal and severely impaired.
Surgical NEC and Outcome
Although children who had surgical NEC tended to weigh less and be shorter at age 10 years than children with no NEC/SIP, these differences were not statistically significant. However, at 15 years, children who had surgical NEC had lower average weight z-score (adjusted effect estimate: −0.75, 95% CI: −1.25 to −0.25), lower BMI z-score (adjusted effect estimate: −0.55, 95% CI: −1.09 to −0.01), and lower height z-score (adjusted effect estimate: −0.65, 95% CI: −1.16 to −0.14) than children with no NEC/SIP (Table 4), and these results remained significant after correcting for sample attrition via inverse probability weighting (Supplemental Table 5).
TABLE 4.
Adjusted Associations between NEC and 10- and 15-Year Outcomes
| No NEC Nor SIP | Medical NEC | Surgical NEC | SIP | ||||
|---|---|---|---|---|---|---|---|
| Effect Estimate (β)/OR (95% CI) | P | Effect Estimate (β)/OR (95% CI) | P | Effect Estimate (β)/OR (95% CI) | P | ||
| Age-10 outcome | |||||||
| BMI z-score | Referent | 0.13 (−0.16 to 0.42) | .38 | −0.17 (−0.64 to 0.31) | .49 | −0.32 (−0.91 to 0.26) | .28 |
| Weight z-score | Referent | 0.15 (−0.09 to 0.40) | .22 | −0.20 (−0.64 to 0.24) | .38 | −0.44 (−1.07 to 0.20) | .18 |
| Height z-score | Referent | 0.06 (−0.16 to 0.29) | .57 | −0.14 (−0.47 to 0.19) | .40 | −0.31 (−0.75 to 0.12) | .16 |
| DAS-II FSIQ | Referent | 0.21 (−3.32 to 3.73) | .91 | −2.04 (−9.13 to 5.05) | .57 | −3.57 (−11.8 to 4.65) | .39 |
| LPAa | Referent | 1.13 (0.80–1.59) | .49 | 1.46 (0.75–2.83) | .27 | 1.43 (0.71–2.88) | .32 |
| Age-15 outcome | |||||||
| BMI z-score | Referent | 0.24 (−0.04 to 0.53) | .10 | −0.55 (−1.09 to −0.01) | .04* | 0.08 (−0.60 to 0.75) | .83 |
| Weight z-score | Referent | 0.19 (−0.15 to 0.53) | .28 | −0.75 (−1.25 to −0.25) | <.01* | 0.09 (−0.76 to 0.93) | .84 |
| Height z-score | Referent | −0.08 (−0.34 to 0.18) | .55 | −0.65 (−1.16 to −0.14) | .01* | 0.03 (−0.53 to 0.59) | .92 |
| WASI-II FSIQ | Referent | −1.62 (−5.65 to 2.41) | .43 | −6.51 (−14.2 to 1.14) | .10 | −0.07 (−8.50 to 8.36) | .99 |
| LPAb | Referent | 0.89 (0.59–1.36) | .60 | 0.91 (0.42–1.96) | .81 | 0.90 (0.36–2.24) | .82 |
Adjusted for Fenton birth weight z-score, GA and sex. LPA OR represents the odds of a worse outcome (impaired). FSIQ, full-scale IQ; OR, odds ratio; WASI-II, Wechsler Abbreviated Scale of Intelligence-II.
P ≤ .05.
Age-10 LPA outcome classifications were dichotomized to normal/low-normal and moderately impaired/severely impaired.
Age-15 LPA variable was dichotomized to normal/low-normal and severely impaired.
When adjusted for confounding variables, no differences were found at either 10 or 15 years of age between the neurodevelopmental outcomes of children who had surgical NEC and children with neither SIP nor NEC, despite correcting for sample attrition.
SIP and Outcome
At age 10 years, children who had SIP tended to have lower weight and height compared with no NEC/SIP, but the results were not significant after adjusting for confounding variables. However, when adjusting for sample attrition, children with SIP had lower average weight (effect estimate: −0.63, 95% CI: −1.24 to −0.02) and lower height (effect estimate: −0.57, 95% CI: −0.97 to −0.16) than children with no NEC/SIP at age 10 years (Supplemental Table 5). At age 15 years, children who had SIP had similar weight, BMI, and height as children who had no NEC/SIP. Children who had SIP had IQ scores and LPA classifications that did not differ from those of children with no NEC/SIP.
Discussion
This study is 1 of the few studies to report long-term growth and ND outcomes from a large cohort of infants born EP with NEC and SIP at age 10 and 15 years. Compared with controls who had neither NEC nor SIP during initial NICU stay, infants who had NEC requiring surgery were shorter, lighter, and had lower BMI at age 15 years. There were no differences in long-term ND outcomes when comparing infants with surgical NEC to controls in our study population. Infants who had medical NEC had growth and ND outcomes that were not significantly different from infants without NEC/SIP. Infants with SIP had lower weight and height at 10 years, but there was no difference in ND outcomes when compared to infants with no NEC/SIP at 10 or 15 years of age. Overall, these findings should offer encouragement to parents and clinicians caring for EP infants who encounter the devastating short-term effects of NEC or SIP, while acknowledging that there are multiple factors after discharge from hospital that can potentially impact these outcomes and it may not be possible to adjust for all cofounders in any study.
Most previous studies in infants with medical or surgical NEC have found higher rates of NDI among smaller infants, infants who were more ill, and those who underwent surgery, in early childhood.16,34,35 Because most studies only reported outcomes up to 2 years, it is largely unknown how ND outcomes change over time, possibly enhanced by early intervention services, support from their family and schools, and “catch-up” growth for infants born EP. Our findings are consistent with a previous report in which motor function in very low birth weight neonates with surgical NEC gradually improved during the first 2 years of life.36 Similarly, in the cohort we studied, infants with surgical NEC, as compared with those without NEC or SIP, had worse scores on a standardized assessment of motor skills at age 2 years,18 but this difference was not found at ages 10 and 15 years, suggesting improvement over time. Our findings contrast with those of Roze et al, who found that infants with NEC or SIP when compared with controls had lower IQ and worse motor function at 6.2 to 13.2 years of age,13 but this study differed from ours because it only included infants between 27 and 34 weeks’ gestation and were not adjusted for confounders other than severe cerebral pathology. Because our study included patients of lower gestation (23–27 weeks), who are at increased risk of poor ND outcome at baseline even without NEC, this might have contributed to the nonsignificant difference in neurocognitive outcomes between the different groups in our study. Our results are consistent with a population-based study of children with NEC, born at average of 30 weeks’ gestation, where the authors concluded that negative consequences of NEC-associated brain injury detected in early childhood may not be important at school age,14 but the investigators used parental questionnaires, which may potentially include biased responses as stated in the limitation. Most of the studies reporting ND outcomes after early childhood among survivors of NEC were based on infants whose mean GAs were higher than our study population12,13 and had significant methodical differences in the study cohort, such as including suspected NEC cases,12 making detailed comparison between the studies very challenging.
Most studies reporting long-term outcomes in children with SIP have only reported ND outcomes at 18 to 24 months’ corrected age.6,8,37 In our cohort, children with SIP were more likely to have GMFCS classification level >1 at 10 years of age than children with neither NEC nor SIP, but otherwise had similar ND outcomes compared with children with no NEC or SIP at age 10 and 15 years.
The exact cause of NDI in children with surgical NEC and SIP is largely unknown but is probably multifactorial. Some key factors may include systemic circulation of proinflammatory proteins, illness severity, exposure to perioperative anesthetic and pain medications, poor nutrition (especially with short gut), and ongoing need for parenteral nutrition, which increases the risk for sepsis. Any surgical intervention potentially results in a proinflammatory cytokine surge, as well as exposure to anesthesia, both of which are known to be associated with ND impairment.38,39
Studies of growth outcomes in infancy among survivors of NEC are inconsistent, with some studies reporting lower weight, height, and HC at 18 to 24 months,40,41 whereas others report no significant difference in growth outcomes.11,42 Among ELBW infants, surgical NEC, but not medical NEC, was associated with significant growth delay at 18 to 22 months’ corrected age.16,43 Our findings suggest that growth delay among infants with surgical NEC persists into late childhood. A complex array of humoral responses may affect adaptation of the remaining small intestine, as well as nutritional status and/or growth.44 Many growth factors that stimulate intestinal growth, such as glucagon-like peptide-2, epidermal growth factor, growth hormone, and insulin-like growth factor-1, may have lower circulating levels secondary to bowel loss.45,46 It is plausible that the postresection intestinal adaptation47 impacts the pubertal growth spurt, which proceeds normally in children with medical NEC or no NEC/SIP as infants. Barksdale et al, in a small study of children with short bowel syndrome, demonstrated that exogenous insulin-like growth factor-1 and insulin-like growth factor–binding protein-3, but not growth hormone, may be beneficial to treat this subpopulation.48 In our study cohort, the growth outcomes for surgical NEC were not different at age 10 years but were significantly lower at age 15 years, even after adjustments, which may suggest that, if the patients have caught up in weight at early childhood up to age 10 years, they are still at risk for poor growth at phases of accelerated growth during adolescence, and thereby require closer follow-up.
Strengths of our study include a large, prospective, multicenter cohort with ND assessments by examiners who were masked to children’s neonatal histories and multivariable adjustments for confounding variables. A limitation of our study is the relatively small number of infants with any NEC or SIP. Additionally, we had sample attrition, which was particularly high among study participants whose families had indicators of lower socioeconomic position, likely resulting in selection bias, which lessens our confidence that the results apply to more diverse samples with a greater socioeconomic disadvantage. To address this, we performed inverse probability weighting, giving weight to surrogates for socioeconomic status, including maternal education, maternal single status, and public insurance. Even with these adjustments, our results were unchanged. Further, results based on those who are compliant with follow-up might result in an overestimation of adverse outcomes in ELBW survivors as reported in a previous study.49 Another limitation is lack of detailed information about exposure to anesthesia and pain medications, and the occurrence of short gut syndrome, factors that have been shown to negatively influence ND outcomes in multiple studies.50,51 One important consideration would be that our exposure variables occurred 18 to 20 years ago, and we acknowledge that numerous aspects of neonatal care may have changed over the past 2 decades, including management of NEC, nutrition, and other interventions that affect ND outcomes. Additionally, in long-term follow-up studies, there might be multiple other known or unknown confounding factors, such as nutritional intake, medication exposure, illness, among others, which would be extremely difficult to adjust for. These challenges are inherent to many long-term outcome study designs; hence, our results might not apply to more recently born individuals with NEC or SIP.
Conclusions
EP infants who developed surgical NEC were shorter, lighter, and had lower BMI at 15 years, as compared with children without NEC or SIP. Infants with SIP had lower weight and height at age 10 years, but this difference resolved by age 15. ND outcomes at 10 and 15 years of age among children born extremely preterm who developed SIP, medical NEC, or surgical NEC during infancy did not differ from children who had neither NEC nor SIP.
Supplementary Material
Acknowledgments
We thank our subjects and their families for their contributions, as well as the following colleagues: project lead for ELGAN-2 and ELGAN ECHO, Julie V. Rollins, Massachusetts site; principal investigators, Baystate Medical Center, Springfield, MA: Bhavesh Shah, MD; Boston Children’s Hospital, Boston, MA: Linda Van Marter, MD, MPH, Camilla Martin, MD, MPH, Janice Ware, PhD, Caitlin Rollins, MD; Tufts Medical Center, Boston, MA: Cynthia Cole, MD; Ellen Perrin, MD, Christina Sakai, MD; University of Massachusetts Medical School, Worcester, MA: Frank Bednarek, MD (deceased); Yale University School of Medicine, New Haven, CT: Richard Ehrenkranz, MD (deceased), Jennifer Benjamin, MD, Angela Montgomery, MD; Wake Forest University, Winston-Salem, NC: T. Michael O’Shea, MD, MPH, Lisa Washburn, MD; University of North Carolina, Chapel Hill, NC: Carl Bose, MD; Diane Warner, MD, MPH; East Carolina University, Greenville, NC: Steve Engelke, MD, Amanda Higginson, MD, Jason Higginson, MD, Kelly Bear, MD; Helen DeVos Children’s Hospital, Grand Rapids, MI: Mariel Poortenga, MD, Steve Pastyrnak, PhD; Sparrow Hospital, Lansing, MI, and Michigan State University, East Lansing, MI: Padu Karna, MD, Nigel Paneth, MD, MPH, Madeleine Lenski, MSPH; University of Chicago Medical Center, Chicago, IL: Michael Schreiber, MD, Scott Hunter, PhD; William Beaumont Hospital, Royal Oak, MI: Danny Batton, MD, Judith Klarr, MD, Young Ah Lee, MD, Rawad Obeid, MD; site study coordinators, Baystate Medical Center, Springfield, MA: Karen Christianson, RN, Deborah Klein, BSN, RN; Boston Children’s Hospital, Boston MA: Maureen Pimental, BA, Collen Hallisey, BA, Taryn Coster, BA, Maddie Dolins, Maggie Mittleman, Hannah Haile, Julia Rohde, Kaysi Herrera Pujols; Tufts Medical Center, Boston, MA: Ellen Nylen, RN, Emily Neger, MA, Kathryn Mattern, BA, Catherine Ma, Deanna Toner, Elizabeth Vitaro; University of Massachusetts Medical School, Worcester, MA: Lauren Venuti, BA, Beth Powers, RN, Ann Foley, EdM, Taylor Merk; Yale University School of Medicine, New Haven, CT: Joanne Williams, RN, Elaine Romano, APRN, Christine Henry; Wake Forest University, Winston-Salem, NC: Debbie Hiatt, BSN (deceased), Nancy Peters, RN, Patricia Brown, RN, Emily Ansusinha, BA, Jazmyne James, MS, Nou Yang, MS; University of North Carolina, Chapel Hill, NC: Gennie Bose, RN, Janice Wereszczak, MSN, Janice Bernhardt, MS, RN; East Carolina University, Greenville, NC: Joan Adams (deceased), Donna Wilson, BA, BSW, Nancy Darden-Saad, BS, RN, Bree Williams, Emily Jones, Hannah Morris; Helen DeVos Children’s Hospital, Grand Rapids, MI: Dinah Sutton, RN, Julie Rathbun, BSW, BSN, Stephanie Fagerman, William Boshoven, Jalen Johnson, Brandon James, Cynthia Gile, BS, CCRC; Sparrow Hospital, Lansing, MI, and Michigan State University, East Lansing, MI: Karen Miras, RN, BSN, Carolyn Solomon, RN, Deborah Weiland, MSN; University of Chicago Medical Center, Chicago, IL: Grace Yoon, RN, Rugile Ramoskaite, BA, Suzanne Wiggins, MA, Krissy Washington, MA, Ryan Martin, MA, Barbara Prendergast, BSN, RN, Emma Lynch, MPH, Sabina Hajdarovic; William Beaumont Hospital, Royal Oak, MI: Beth Kring, RN; psychologists, Baystate Medical Center, Springfield, MA: Anne Smith, PhD, Susan McQuiston, PhD; Boston Children’s Hospital: Samantha Butler, PhD, Rachel Wilson, PhD, Kirsten McGhee, PhD, Patricia Lee, PhD, Aimee Asgarian, PhD, Anjali Sadhwani, PhD, Brandi Henson, PsyD; Tufts Medical Center, Boston, MA: Cecelia Keller, PT, MHA, Jenifer Walkowiak, PhD, Susan Barron, PhD; University of Massachusetts Medical School, Worcester MA: Alice Miller, PT, MS, Brian Dessureau, PhD, Molly Wood, PhD, Jill Damon-Minow, PhD; Yale University School of Medicine, New Haven, CT: Elaine Romano, MSN, Linda Mayes, PhD, Kathy Tsatsanis, PhD, Katarzyna Chawarska, PhD, Sophy Kim, PhD, Susan Dieterich, PhD, Karen Bearrs, PhD; Wake Forest University Baptist Medical Center, Winston-Salem NC: Ellen Waldrep, MA, Jackie Friedman, PhD, Gail Hounshell, PhD, Debbie Allred, PhD; University Health Systems of Eastern Carolina, Greenville, NC: Rebecca Helms, PhD, Lynn Whitley, PhD, Gary Stainback, PhD; University of North Carolina at Chapel Hill, NC: Lisa Bostic, OTR/L, Amanda Jacobson, PT, Joni McKeeman, PhD, Echo Meyer, PhD; Helen DeVos Children’s Hospital, Grand Rapids, MI: Steve Pastyrnak, PhD; Sparrow Hospital, Lansing, MI, and Michigan State University, East Lansing, MI: Joan Price, EdS, Megan Lloyd, MA, EdS; University of Chicago Medical Center, Chicago, IL: Susan Plesha-Troyke, OT, Megan Scott, PhD; William Beaumont Hospital, Royal Oak, MI: Katherine M. Solomon, PhD, Kara Brooklier, PhD, Kelly Vogt, PhD.
Glossary
- ADHD
attention-deficit/hyperactivity disorder
- CI
confidence interval
- DAS-II
Differential Ability Scales-II
- ELBW
extremely low birth weight
- ELGAN
extremely low gestational age newborns
- EP
extremely preterm
- GA
gestational age
- GMFCS
Gross Motor Function Classification System
- HC
head circumference
- LPA
latent profile analysis
- ND
neurodevelopmental
- NDI
neurodevelopmental impairment
- NEC
necrotizing enterocolitis
- SIP
spontaneous intestinal perforation
Footnotes
A complete list of nonauthor contributors appears in the Acknowledgments.
Drs Vaidya and Singh conceptualized and designed the study, collected data, drafted the initial manuscript, and reviewed and revised the manuscript; Mr Yi conducted the initial analyses, and reviewed and revised the manuscript; Drs Joseph, Shenberger, O’Shea, Jensen, Gogcu, and Ms Wagner conceptualized and designed the study, and critically reviewed the manuscript for important intellectual content; Drs Msall, Thompson, Fry, and Frazier critically reviewed the manuscript for important intellectual content; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FUNDING: Supported by the National Institute of Neurologic Disorders and Stroke (grants 5U01NS040069-05 and 2R01NS040069-09) and the Office of the Director of the National Institutes of Health (grant 5UG3OD023348-06). The funder had no role in the design and conduct of the study. Funded by the National Institutes of Health (NIH).
CONFLICT OF INTEREST DISCLAIMER: The authors have indicated they have no conflicts of interest relevant to this article to disclose.
References
- 1. Stoll BJ, Hansen NI, Bell EF, et al. Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network . Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010;126(3):443–456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Neu J, Walker WA. Necrotizing enterocolitis. N Engl J Med. 2011;364(3):255–264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Pumberger W, Mayr M, Kohlhauser C, Weninger M. Spontaneous localized intestinal perforation in very-low-birth-weight infants: a distinct clinical entity different from necrotizing enterocolitis. J Am Coll Surg. 2002;195(6):796–803 [DOI] [PubMed] [Google Scholar]
- 4. Guthrie SO, Gordon PV, Thomas V, Thorp JA, Peabody J, Clark RH. Necrotizing enterocolitis among neonates in the United States. J Perinatol. 2003;23(4):278–285 [DOI] [PubMed] [Google Scholar]
- 5. Ganapathy V, Hay JW, Kim JH, Lee ML, Rechtman DJ. Long-term health care costs of infants who survived neonatal necrotizing enterocolitis: a retrospective longitudinal study among infants enrolled in Texas Medicaid. BMC Pediatr. 2013;13:127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wadhawan R, Oh W, Hintz SR, et al. NICHD Neonatal Research Network . Neurodevelopmental outcomes of extremely low birth weight infants with spontaneous intestinal perforation or surgical necrotizing enterocolitis. J Perinatol. 2014;34(1):64–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hayakawa M, Taguchi T, Urushihara N, et al. Outcome in VLBW infants with surgical intestinal disorder at 18 months of corrected age. Pediatr Int. 2015;57(4):633–638 [DOI] [PubMed] [Google Scholar]
- 8. Shah TA, Meinzen-Derr J, Gratton T, et al. Hospital and neurodevelopmental outcomes of extremely low-birth-weight infants with necrotizing enterocolitis and spontaneous intestinal perforation. J Perinatol. 2012;32(7):552–558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tobiansky R, Lui K, Roberts S, Veddovi M. Neurodevelopmental outcome in very low birthweight infants with necrotizing enterocolitis requiring surgery. J Paediatr Child Health. 1995;31(3):233–236 [DOI] [PubMed] [Google Scholar]
- 10. Han SM, Knell J, Henry O, et al. Long-term outcomes of severe surgical necrotizing enterocolitis. J Pediatr Surg. 2020;55(5):848–851 [DOI] [PubMed] [Google Scholar]
- 11. Soraisham AS, Amin HJ, Al-Hindi MY, Singhal N, Sauve RS. Does necrotizing enterocolitis impact the neurodevelopmental and growth outcomes in preterm infants with birthweight < or =1250 g? J Paediatr Child Health. 2006;42(9):499–504 [DOI] [PubMed] [Google Scholar]
- 12. Pike K, Brocklehurst P, Jones D, et al. Outcomes at 7 years for babies who developed neonatal necrotising enterocolitis: the ORACLE Children Study. Arch Dis Child Fetal Neonatal Ed. 2012;97(5):F318–F322 [DOI] [PubMed] [Google Scholar]
- 13. Roze E, Ta BD, van der Ree MH, et al. Functional impairments at school age of children with necrotizing enterocolitis or spontaneous intestinal perforation. Pediatr Res. 2011;70(6):619–625 [DOI] [PubMed] [Google Scholar]
- 14. Hansen ML, Jensen IV, Gregersen R, Juhl SM, Greisen G. Behavioural and neurodevelopmental impairment at school age following necrotizing enterocolitis in the newborn period. PLoS One. 2019;14(4):e0215220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hong CR, Fullerton BS, Mercier CE, et al. Growth morbidity in extremely low birth weight survivors of necrotizing enterocolitis at discharge and two-year follow-up. J Pediatr Surg. 2018;53(6):1197–1202 [DOI] [PubMed] [Google Scholar]
- 16. Hintz SR, Kendrick DE, Stoll BJ, et al. NICHD Neonatal Research Network . Neurodevelopmental and growth outcomes of extremely low birth weight infants after necrotizing enterocolitis. Pediatrics. 2005;115(3):696–703 [DOI] [PubMed] [Google Scholar]
- 17. O’Shea TM, Allred EN, Dammann O, et al. ELGAN study Investigators . The ELGAN study of the brain and related disorders in extremely low gestational age newborns. Early Hum Dev. 2009;85(11):719–725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Martin CR, Dammann O, Allred EN, et al. Neurodevelopment of extremely preterm infants who had necrotizing enterocolitis with or without late bacteremia. J Pediatr. 2010;157(5):751–6.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Joseph RM, O’Shea TM, Allred EN, et al. ELGAN Study Investigators . Neurocognitive and academic outcomes at age 10 years of extremely preterm newborns. Pediatrics. 2016;137(4):e20154343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Patel RM, Ferguson J, McElroy SJ, Khashu M, Caplan MS. Defining necrotizing enterocolitis: current difficulties and future opportunities. Pediatr Res. 2020;88(Suppl 1):10–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kliegman RM, Walsh MC. Neonatal necrotizing enterocolitis: pathogenesis, classification, and spectrum of illness. Curr Probl Pediatr. 1987;17(4):213–288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39(4):214–223 [DOI] [PubMed] [Google Scholar]
- 23. Douglass LM, Kuban K, Tarquinio D, et al. A novel parent questionnaire for the detection of seizures in children. Pediatr Neurol. 2016;54:64–69.e1 [DOI] [PubMed] [Google Scholar]
- 24. Elliott CD, Salerno JD, Dumont R, Willis JO. Differential Ability Scales-II (DAS-II), 2nd ed. San Antonio, TX: Harcourt Assessment; 2007 [Google Scholar]
- 25. Korkman M, Kirk U, Kemp S. NEPSY II: Clinical and Interpretive Manual. San Antonio, TX: PsychCorp. Pearson Assessment; 2007 [Google Scholar]
- 26. Heeren T, Joseph RM, Allred EN, O’Shea TM, Leviton A, Kuban KCK. Cognitive functioning at the age of 10 years among children born extremely preterm: a latent profile approach. Pediatr Res. 2017;82(4):614–619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wechsler D. Wechsler Abbreviated Scale of Intelligence, Second Ed. San Antonio, Texas: Pearson[Google Scholar]. 2011 [Google Scholar]
- 28. Akshoomoff N, Beaumont JL, Bauer PJ, et al. VIII. NIH Toolbox Cognition Battery (CB): composite scores of crystallized, fluid, and overall cognition. Monogr Soc Res Child Dev. 2013;78(4):119–132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Chung PJ, Opipari VP, Koolwijk I. Executive function and extremely preterm children. Pediatr Res. 2017;82(4):565–566 [DOI] [PubMed] [Google Scholar]
- 30. Scott MN, Hunter SJ, Joseph RM, et al. Neurocognitive correlates of attention-deficit hyperactivity disorder symptoms in children born at extremely low gestational age. J Dev Behav Pediatr. 2017;38(4):249–259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sheehan DV, Sheehan KH, Shytle RD, et al. Reliability and validity of the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID). J Clin Psychiatry. 2010;71(3):313–326 [DOI] [PubMed] [Google Scholar]
- 32. Fenton TR, Kim JH. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013;13:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Campbell H, Check J, Kuban KCK, et al. Neonatal cranial ultrasound findings among infants born extremely preterm: associations with neurodevelopmental outcomes at 10 years of age. J Pediatr. 2021;237:197–205.e4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Jones IH, Hall NJ. Contemporary outcomes for infants with necrotizing enterocolitis-a systematic review. J Pediatr. 2020;220:86–92.e3 [DOI] [PubMed] [Google Scholar]
- 35. Schulzke SM, Deshpande GC, Patole SK. Neurodevelopmental outcomes of very low-birth-weight infants with necrotizing enterocolitis: a systematic review of observational studies. Arch Pediatr Adolesc Med. 2007;161(6):583–590 [DOI] [PubMed] [Google Scholar]
- 36. Simon NP, Brady NR, Stafford RL, Powell RW. The effect of abdominal incisions on early motor development of infants with necrotizing enterocolitis. Dev Med Child Neurol. 1993;35(1):49–53 [DOI] [PubMed] [Google Scholar]
- 37. Adesanya OA, O’Shea TM, Turner CS, Amoroso RM, Morgan TM, Aschner JL. Intestinal perforation in very low birth weight infants: growth and neurodevelopment at 1 year of age. J Perinatol. 2005;25(9):583–589 [DOI] [PubMed] [Google Scholar]
- 38. Blakely ML, Tyson JE, Lally KP, et al. NICHD Neonatal Research Network . Laparotomy versus peritoneal drainage for necrotizing enterocolitis or isolated intestinal perforation in extremely low birth weight infants: outcomes through 18 months adjusted age. Pediatrics. 2006;117(4):e680–e687 [DOI] [PubMed] [Google Scholar]
- 39. The Victorian Infant Collaborative Study Group . Surgery and the tiny baby: sensorineural outcome at 5 years of age. J Paediatr Child Health. 1996;32(2):167–172 [DOI] [PubMed] [Google Scholar]
- 40. Salhab WA, Perlman JM, Silver L, Sue Broyles R. Necrotizing enterocolitis and neurodevelopmental outcome in extremely low birth weight infants <1000 g. J Perinatol. 2004;24(9):534–540 [DOI] [PubMed] [Google Scholar]
- 41. Sonntag J, Grimmer I, Scholz T, Metze B, Wit J, Obladen M. Growth and neurodevelopmental outcome of very low birthweight infants with necrotizing enterocolitis. Acta Paediatr. 2000;89(5):528–532 [DOI] [PubMed] [Google Scholar]
- 42. Silveira RC, Procianoy RS, Koch MS, Benjamin AC, Schlindwein CF. Growth and neurodevelopment outcome of very low birth weight infants delivered by preeclamptic mothers. Acta Paediatr. 2007;96(12):1738–1742 [DOI] [PubMed] [Google Scholar]
- 43. McLaughlin CM, Channabasappa N, Pace J, Nguyen H, Piper HG. Growth trajectory in children with short bowel syndrome during the first 2 years of life. J Pediatr Gastroenterol Nutr. 2018;66(3):484–488 [DOI] [PubMed] [Google Scholar]
- 44. Baksheev L, Fuller PJ. Humoral factors in intestinal adaptation. Trends Endocrinol Metab. 2000;11(10):401–405 [DOI] [PubMed] [Google Scholar]
- 45. Martin GR, Beck PL, Sigalet DL. Gut hormones, and short bowel syndrome: the enigmatic role of glucagon-like peptide-2 in the regulation of intestinal adaptation. World J Gastroenterol. 2006;12(26):4117–4129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Seetharam P, Rodrigues G. Short bowel syndrome: a review of management options. Saudi J Gastroenterol. 2011;17(4):229–235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Warner BW. The pathogenesis of resection-associated intestinal adaptation. Cell Mol Gastroenterol Hepatol. 2016;2(4):429–438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Barksdale EM Jr, Koehler AN, Yaworski JA, Gardner M, Reyes J. Insulinlike growth factor 1 and insulinlike growth factor 3: indices of intestinal failure in children. J Pediatr Surg. 1999;34(5):655–661, discussion 661–662 [DOI] [PubMed] [Google Scholar]
- 49. Castro L, Yolton K, Haberman B, et al. Bias in reported neurodevelopmental outcomes among extremely low birth weight survivors. Pediatrics. 2004;114(2):404–410 [DOI] [PubMed] [Google Scholar]
- 50. Backeljauw B, Holland SK, Altaye M, Loepke AW. Cognition and brain structure following early childhood surgery with anesthesia. Pediatrics. 2015;136(1):e1–e12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Block RI, Thomas JJ, Bayman EO, Choi JY, Kimble KK, Todd MM. Are anesthesia and surgery during infancy associated with altered academic performance during childhood? Anesthesiology. 2012;117(3):494–503 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.