Abstract
Video Abstract
The authors of this study developed, via the Delphi method, recommendations for shared decision-making (SDM) in pediatrics for both simple and complex decisions.
OBJECTIVE
To develop recommendations for pediatric shared decision-making (SDM).
METHODS
We conducted a Delphi method study from 2020 to 2021 with an international panel (n = 21) of clinicians, researchers, and parents with expertise in pediatric SDM. We conducted semistructured interviews to identify the key processes of pediatric SDM. We coded the interviews using content analysis and developed a questionnaire on the potential processes of pediatric SDM. Using a Likert scale, panelists evaluated each process twice, once for simple decisions and once for complex decisions. Panelists were provided with a summary of the results and evaluated each process again. The processes that were agreed on for simple and complex decisions were reported as “fundamental processes.” The processes that were agreed on for complex decisions were reported as “additional processes.”
RESULTS
A total of 79 recommendations were developed, including 29 fundamental processes and 14 additional processes for complex decisions. A recurring theme was the importance of personalizing the decision-making process. For example, the panel recommended that physicians should assess the family and child’s desired roles in the decision-making process, assess their desired level of directiveness, and elicit and clarify their values, preferences, and goals. The panel also disagreed on several subprocesses, such as how to determine the child’s role and the appropriate level of directiveness.
CONCLUSIONS
An international expert panel developed recommendations for pediatric SDM for both simple and complex decisions. The recommendations highlight the importance of personalizing the decision-making process.
What’s Known On This Subject
Although SDM is widely accepted in pediatrics, there is currently no consensus on specific processes unique to pediatrics, resulting in wide variation in clinical practice and research.
What This Study Adds
Using Delphi methodology, an international expert panel reached a consensus on the processes involved in pediatric SDM and generated recommendations on how to facilitate and achieve pediatric SDM for both simple and complex decisions.
Pediatric shared decision-making (SDM) is the set of processes by which health care decisions are made through a respectful collaboration between clinicians and patients (to the degree that they can or want to participate) and their parents or guardians. SDM is recognized as a key component of family-centered care1,2 and endorsed by the American Academy of Pediatrics,2 as well as other United States and international organizations.3–5 Despite these endorsements, SDM may not be as widely implemented in pediatrics as is recommended.6,7 One study revealed that neonatologists rarely honored parental preferences around resuscitation at extreme prematurity8 and made most clinical decisions themselves.9 Another study revealed that, even after receiving SDM training, only 8% of pediatric clinicians reported frequently using SDM in their clinical practice.10
Suboptimal use of SDM may be due to a lack of clinician training in best SDM processes, insufficient time, power imbalances, and clinician bias.11 One of the most important factors inhibiting the implementation of pediatric SDM, however, is the basic lack of clarity and consensus about what specific processes constitute high-quality SDM. Nearly all models of SDM are adult-medicine-focused.12–16 Yet, key differences exist between adult and pediatric medical decision-making, the most obvious being that many adult patients engage in decision-making for themselves, whereas, in pediatrics, parents of pediatric patients often make decisions on behalf of their children. Although the authors of many pediatric SDM studies adapt and use adult SDM models, how they do so varies, impeding comparisons of data and conclusions.
To address the problems arising from the lack of a consensus processes-oriented model of pediatric SDM, the objective of this study was to develop an expert consensus model of pediatric SDM that incorporates all the processes that are fundamental to pediatric SDM.
Methods
Study Design
We conducted an international Delphi study between November 2020 and May 2021. The Delphi method is a widely used technique to develop health care recommendations using iterative rounds of questionnaires, anonymous rating of items (to prevent panelists from unduly influencing each other), incorporation of panelist feedback between rounds, and sharing with panelists the finding of previous rounds of questions.17,18
The conduct of this study was approved by the institutional ethics review board at the University of Zurich. All participants provided written informed consent.
Expert Panel
The expert panel included clinicians, researchers, and parents. We first identified clinicians and researchers by searching PubMed to identify authors who had published ≥5 manuscripts on pediatric SDM between 2000 and 2019. Potential candidates were invited to participate via E-mail. During initial interviews, participants were asked to nominate other experts in the field of pediatric SDM. This snowball sampling identified additional experts in the field of pediatric SDM who may not have published extensively yet. All panelists recommended via snowball sampling had published ≥2 manuscripts on pediatric SDM.
Potential parent panelists included parents who presented on pediatric SDM at the International Conference on Patient and Family Centered Care or who participated in hospital or national health care organizations’ parent advisory committees. Additional parent panelists who had participated in previous pediatric SDM projects were identified via snowball sampling as described above.
Data Collection
Round 1
In this initial round, 1 researcher (SE) conducted individual semistructured, open-ended interviews with panelists via internet-based video meetings to explore their perspectives on the essential processes of pediatric SDM. The same researcher (SE) then deidentified, transcribed, entered into NVivo,19 and coded the interviews using content analysis. Twenty percent of the interviews were double-coded and checked for agreement between 2 team members (SE and JS). All disagreements were discussed and resolved. Ninety-eight processes were developed from the codes. All processes were reviewed by 2 team members (SE and JS), and all disagreements were discussed and resolved.
Mini Round
In Round 1, panelists used a variety of definitions for pediatric SDM. To ensure consistency, we established a common definition of pediatric SDM to use in Rounds 2 and 3. We used data from Round 1 to develop 4 potential definitions of pediatric SDM. Participants selected their preferred definition and were able to provide feedback through an optional free response.
Each panelist was provided with the results of the Mini Round (that specific panelist’s selection, the panel’s aggregate results, and a summary of the comments) via e-mail before Round 2. Panelists were instructed to use the agreed on definition of pediatric SDM as a framework for Round 2.
Round 2
In Round 2 we evaluated group consensus on the definition and processes required for pediatric SDM. We used an internet-administered questionnaire (see the Supplemental Information) in which panelists evaluated 45 potential processes of pediatric SDM via a Likert scale (Strongly Disagree [1] to Strongly Agree [9]). Some processes also had corresponding “subprocesses.” For example, the process “determine the child’s role” contained several subprocesses about the factors that should be considered when doing so. During this round, panelists also evaluated 6 aspects of the definition of pediatric SDM. The subprocesses and definition processes were also evaluated by a Likert scale. Panelists had an optional free response box for each process to provide general comments, suggest revisions, or propose new processes. All processes were evaluated twice, once in the context of simple decisions and once in the context of complex decisions. We used this approach because, during Round 1, many panelists stated that the processes of pediatric SDM vary based on the decision’s complexity.
On the basis of the comments from Round 2, we revised 17 processes and 3 subprocesses (mostly minor wording changes) and added 2 processes and 15 subprocesses for Round 3.
Round 3
In Round 3, the panelists were provided with the results of Round 2, including the panelist’s previous response, a boxplot depicting the median, interquartile range, and range of the panelists’ ratings, and a summary of comments. The results also included the final definition of pediatric SDM (which remained unchanged), with instructions to use this definition for Round 3.
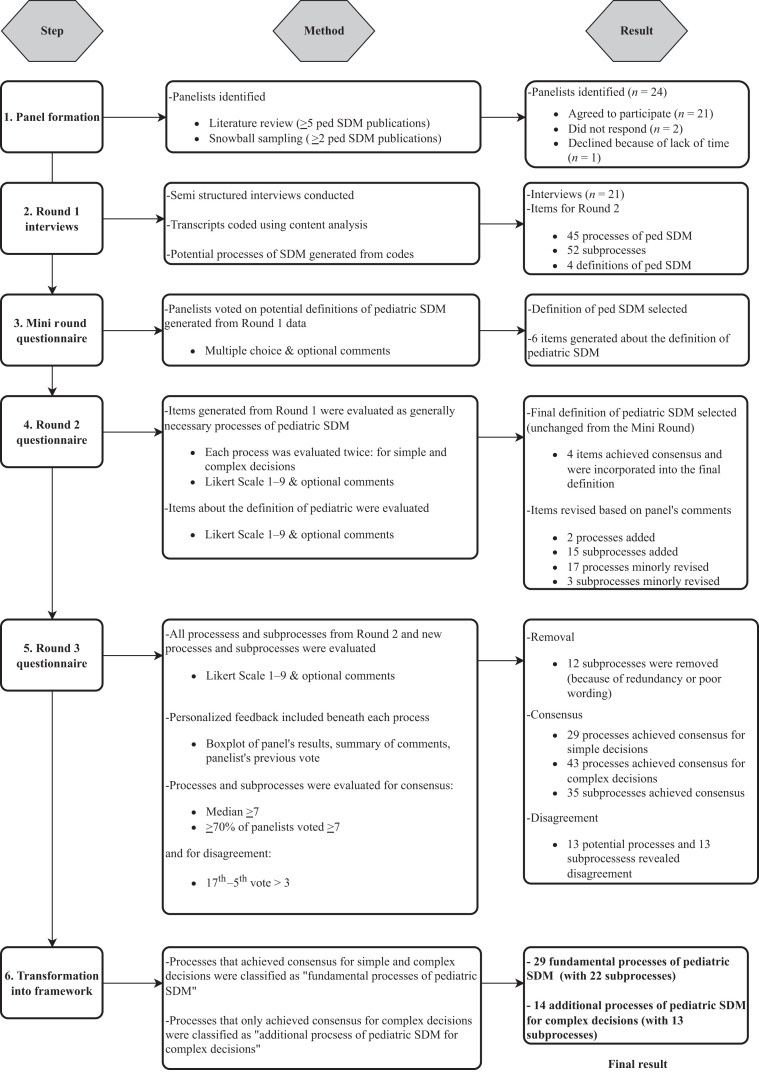
As in Round 2, processes were evaluated independently for simple and complex decisions. All SDM processes and subprocesses from Round 2, as well as new processes and subprocesses generated from the comments, were included (Fig 1). Revised and new processes were color-coded to ensure panelists paid special attention to the changes.
FIGURE 1.
Methodology and results.
Data Analysis
We analyzed the responses provided by respondents for each process and subprocess, focusing on 2 different attributes, namely the degree to which the scores typically endorsed the process (called “consensus” in the Delphi literature) and the degree to which the scores, whether high or low, were consistent across respondents (called “agreement” in this study). Consensus endorsement was defined a priori by 2 criteria: (1) ≥70% of the panelists scored the process ≥7 and (2) the median score was ≥7. This is the most frequently used definition of consensus in Delphi studies.20 Processes that were agreed on for both simple and complex decisions were classified as “fundamental processes of pediatric SDM.” Processes that were only agreed on for complex decisions were classified as “additional processes of pediatric SDM for complex decisions.”
We assessed the degree of agreement of the responses across panelists by examining the dispersion of the scores. Many Delphi studies define disagreement as when the following are both true: (1) ≥30% of the votes ≥7 and (2) ≥30% of the votes ≤3. In our study, although scores ≤3 were uncommon, many processes achieved a preponderance of scores ≥7, yet the panelists’ open-ended comments demonstrated substantial disagreement. Therefore, interrater disagreement was defined as being present if <50% of the scores fell within a 3-point range on the 9-point Likert scale (that is, >50% of scores were ≥4 points apart from each other).
Results
Expert Panel
The final panel (n = 21) consisted of clinicians/researchers (n = 16) and parents (n = 5) from the United States (n = 13), Canada (n = 3), the Netherlands (n = 3), the United Kingdom (n = 1), and Australia (n = 1). The panel included primary care (n = 5), pediatric intensive care (n = 3), and neonatology (n = 7) clinicians.
All 3 rounds had a 100% completion rate.
Definition of Pediatric SDM
In the Mini Round, 4 potential definitions of pediatric SDM were evaluated by the panelists, who identified 6 attributes within the various definitions of pediatric SDM. In Round 2, 4 of the 6 attributes were agreed on and were incorporated into the final definition:
Pediatric SDM is a process of respectful collaboration between clinicians, patients, and their parents or guardians to make health care decisions based on clinical expertise and the family’s values, preferences, and goals.
Processes of Pediatric SDM With Consensus Endorsement
In Round 1, 45 potential processes of pediatric SDM and 52 subprocesses were generated and then evaluated in Round 2. Based on the panelists’ comments from Round 2, 2 potential processes and 15 subprocesses were added, and minor wording changes were made to 17 potential processes and 3 subprocesses. All the new and original potential processes and subprocesses (with revisions) from Round 2 were included in Round 3. After Round 3, 12 subprocesses were removed (10 because of panelists interpreting the question stem differently, as demonstrated by their comments, 1 because of poor wording and 1 removed because of redundancy). In total, 47 potential processes and 55 subprocesses were analyzed.
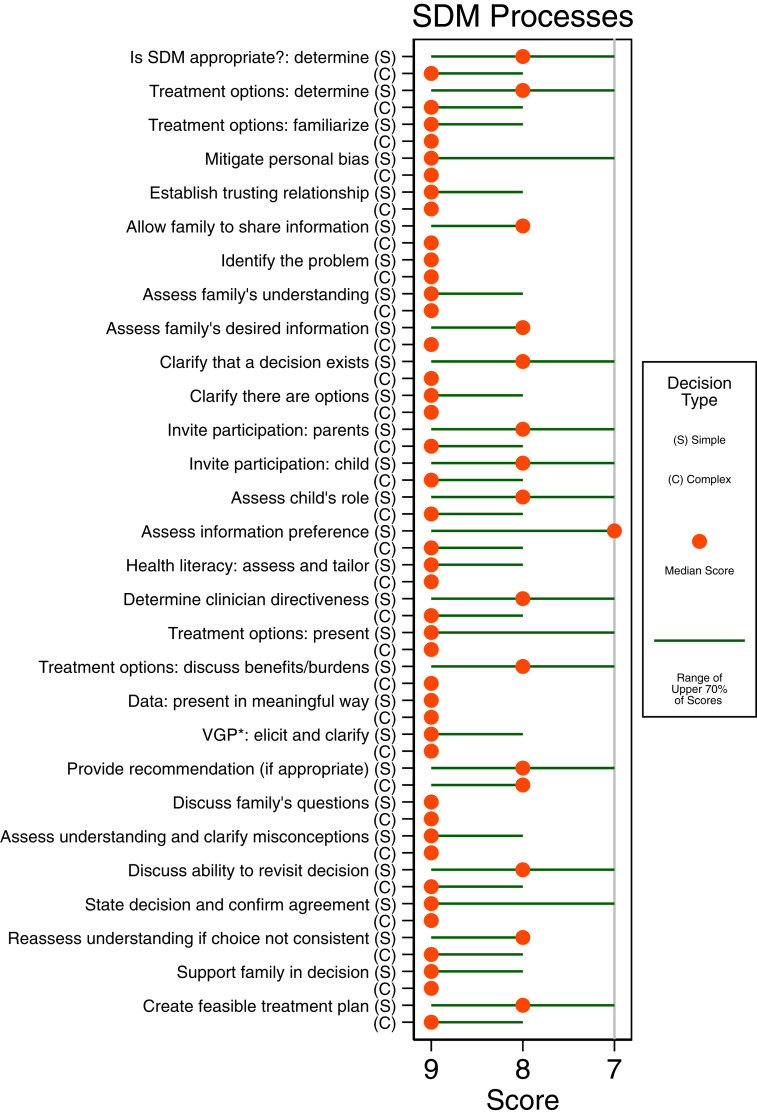
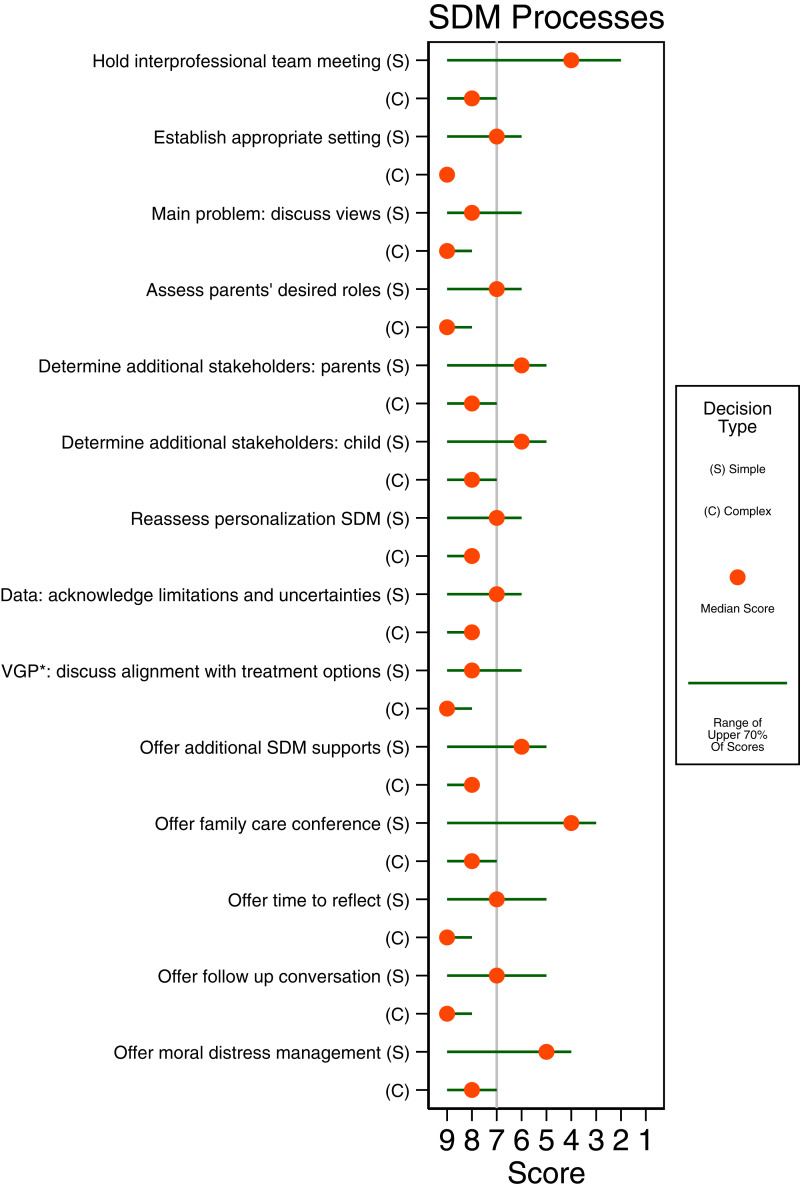
Overall, 29 processes achieved consensus endorsement for both simple and complex decisions and were classified as “fundamental processes of pediatric SDM”; these processes are listed in Table 1, and their scores are displayed in Fig 2. Fourteen processes achieved consensus for only complex decisions and were classified as “additional processes of pediatric SDM for complex decisions” (Table 2 and Fig 3). Thirty-five subprocesses achieved consensus: 22 for fundamental processes and 13 for additional processes for complex decisions.
TABLE 1.
Fundamental Processes (and Subprocesses) of Pediatric SDM for Both Simple and Complex Decisions
| The Expert Panel Recommendations |
|---|
| Determine if SDM is appropriate |
| Determine the ethically permissible treatment options |
| Possible ways to do this: |
| Use clinical judgement (if the options are obvious or standard) |
| Review the medical literature |
| Consult colleagues at the institute |
| Hold an interprofessional team meeting |
| Become familiar with the treatment options that will be offered to be able to answer the family’s questions |
| Reflect on personal biases and employ strategies to mitigate them |
| Establish a trusting relationship with the family |
| Provide an opportunity for the family to share pertinent clinical information (eg, past medical history, response to previous therapy, overall wellbeing before visit) |
| Identify the problem (diagnosis or signs and symptoms) |
| Assess the family’s current understanding of the clinical situation |
| Assess what the family wants to know (eg, more information, a second opinion, a recommendation) |
| Make clear that there are multiple treatment options |
| Make clear that there is a decision to be made |
| Explicitly invite the family (including the child, if possible and appropriate) to participate in the decision-making process |
| Determine the child’s role in the decision-making process |
| Factors that should be considered: |
| Child’s desired role |
| Child’s decision-making capacity |
| Child’s required participation in the treatment plan |
| Child’s familiarity with their illness |
| Relevant laws |
| Determine what type of information the family desires (eg, big picture or details) |
| Assess the family’s health literacy and tailor information to their individual levels of understanding |
| Determine the appropriate level of clinician directiveness |
| Factors that should be considered: |
| Parents’ desired level of directiveness |
| Clinical uncertainty |
| Preference sensitivity |
| Degree of clinical equipoise |
| Urgency |
| Present the range of ethically permissible treatment options (which may include the option of no treatment, if appropriate) |
| Discuss the benefits and burdens of each treatment option |
| Present data in a way that is useful and meaningful to the family |
| Elicit and clarify the family’s values, preferences, and goals |
| The depth of the process will vary based on: |
| Complexity of the decision |
| Family’s willingness to discuss these topics |
| Family’s needs |
| Provide the family with a recommendation (if appropriate) |
| Reflect on how personal biases may influence making a recommendation |
| For more difficult cases, consider holding an interprofessional team meeting to determine if what recommendation should be made |
| If possible, choose a recommendation that is in alignment with the family’s values, goals, and preferences |
| Discuss all ethically permissible treatment options with the family |
| If >1 ethically permissible option, give the family permission to choose alternative option |
| Ask the family what questions they have |
| Assess the family’s understanding and address any misconceptions or gaps in knowledge |
| Discuss the family’s ability to revisit the decision and change their minds at a later time (if possible) |
| If the family chooses an option that does not seem in line with their previously stated preferences, reassess their understanding |
| Clearly state the final decision (or plan if a discrete decision was not made) and confirm that the family agrees |
| Ensure the family feels supported in the decision |
| Create a feasible care plan that can be implemented and sustained |
The processes above are listed in what may be the most typical sequential order in which they might occur.
FIGURE 2.
Fundamental processes of pediatric SDM (simple and complex decisions).
TABLE 2.
Additional Processes (and Subprocesses) of Pediatric SDM for Complex Decisions
| The Expert Panel Recommendations |
|---|
| Hold an interprofessional team meeting |
| This can be used to: |
| Determine which treatment options should be offered |
| Determine the recommendation (if one is being provided) |
| Ensure the clinical team understands the reasoning for a decision |
| Ensure the clinical team is on the same page so their communications to the family are consistent |
| Manage moral distress by debriefing with the care team after a difficult case |
| Establish an appropriate setting |
| Use a quiet room that ensures privacy |
| Ensure other clinical responsibilities are covered |
| Silence phone/pager |
| Be seated |
| Have tissues available for the family |
| Face the family (not a computer) |
| Use the child’s name |
| Discuss what the clinician and the family each consider to be the main problem |
| Assess the parents’ desired roles in decision-making |
| Determine if family wishes to include additional stakeholders in the decision-making process (eg, grandparents, religious elders) |
| Invite additional stakeholders to participate in the decision-making process |
| Regularly reassess the processes of SDM that can be personalized (eg, the family’s desired level of directiveness, their desired roles, their desired type of information) |
| Explicitly acknowledge uncertainties and the limitations of data (eg, center–center variability, generalizability) |
| Discuss how each treatment option aligns with the family’s values, goals, and preferences |
| Offer the family additional multidisciplinary supports for deliberation (eg, clergy, psychological counseling, social worker, written information) |
| Assess the family’s interest in a family care conference and use, if desired |
| Offer the family time to reflect on the decision (if possible) |
| Offer a follow up conversation with the family |
| Offer moral distress management for involved clinicians |
The processes above are listed in what may be the most typical sequential order in which they might occur.
FIGURE 3.
Additional processes of pediatric SDM for complex decisions.
Finally, 13 potential processes and 13 subprocesses were found to have disagreement (Supplemental Figs 4 and 5, respectively).
Fundamental Processes With Consensus Endorsement
Processes that achieved consensus for both simple and complex decisions were classified as fundamental processes of pediatric SDM.
Personalizing the discussion(s) to the family’s needs and preferences was a common theme. Assessing the family’s (1) understanding of the clinical situation, (2) health literacy, (3) information preference (big picture or details), and (4) values, preferences, and goals was essential to tailoring the discussion. Although eliciting and clarifying the family’s values, preferences, and goals is common to many models of SDM, this panel determined that this process varies in depth depending on (1) the complexity of the decision, (2) the family’s needs (eg, if they had already clearly articulated their values), and (3) the family’s willingness to discuss their values. The panel also recommended that when clinicians determine the appropriate level of directiveness, they should consider (1) the family’s desired level of directiveness, (2) the degree of clinical uncertainty, (3) the degree of preference sensitivity, (4) the degree of clinical equipoise, and (5) the level of urgency.
The panel concluded that providing a recommendation (when appropriate) is a fundamental process of pediatric SDM. The panel also recommended that, when clinicians make recommendations, they should (1) reflect on their own biases before making a recommendation, (2) use an interprofessional team meeting to make a recommendation in more nuanced cases or when there is greater clinical equipoise, (3) ensure the recommendation is in alignment with the family’s values, preferences, and goals, (4) continue to present all permissible treatment options to the family, and (5) provide permission for the family to make a different choice without repercussions.
Additional Processes for Complex Decisions With Consensus Endorsement
This panel found that, in addition to the fundamental processes (Table 1), several additional processes are important to facilitate pediatric SDM for complex decisions (Table 2). They recommended that clinicians assess the parents’ desired roles in decision-making and explore whether the family desires to include any additional stakeholders (such as grandparents or elders). They also recommended regularly reassessing the fundamental processes that can be personalized because a family may change their preferences for different types of decisions as they become more familiar with their child’s illness and the clinical setting.
Although the panel recommended eliciting and clarifying the family’s values, preferences, and goals for all decisions, they recommended additionally discussing how each treatment option aligns with the family’s values, preferences, and goals for complex decisions.
Process With Between-Rater Disagreement
Although the panel agreed that determining the child’s role in decision-making is a fundamental process of pediatric SDM, they disagreed about whether one should consider (1) the parents’ preference for the child’s role and (2) the severity of the consequences of the decision.
Although the panel achieved endorsement consensus that determining the appropriate level of clinician directiveness is a fundamental process of pediatric SDM and reached a consensus on several factors that should influence the degree of clinician directiveness, the panel displayed interrater disagreement over whether the following factors should be considered: (1) degree of clinical uncertainty, (2) degree of clinical equipoise, (3) severity of the consequences of the decision, (4) moral uncertainty, and (5) clinician’s preference for decision-making approach (clinician’s desired level of directiveness).
Lastly, although the panel achieved endorsement consensus that providing recommendations (when appropriate) is a fundamental part of pediatric SDM, they displayed between-rater disagreement about whether the clinician should inquire if the family desires a recommendation before providing one.
Discussion
Despite numerous recommendations that SDM should be the main method for family-centered decision-making in pediatrics, the specific processes and communication techniques for achieving high-quality SDM have remained unclear. Using the Delphi method, a panel of international experts reached a consensus regarding the processes of pediatric SDM. They subsequently developed a framework that acknowledges that the SDM approach will vary depending on the complexity of the decision. The framework provides guidance for both simple and complex decisions by classifying processes as fundamental processes (to be used for all types of decisions) or as additional processes needed for more complex decisions.
Families vary in their values, preferences, and goals, including their preferred approach to making medical decisions for their children.21,22 The processes described here should be used when SDM is appropriate and desired by the family. The desired degree of collaboration will vary between families, and the processes revealed by this study should be tailored to each family’s preference.
Our main findings highlight the importance of personalizing the decision-making process to the family’s preferences and their unique clinical situation, including determining the child’s and parents’ roles in the SDM process, determining the family’s information preferences, exploring the family’s values, preferences, and goals, titrating clinician directiveness, and providing a recommendation (if appropriate) on the basis of the family’s values, preferences, and goals.
In addition to producing a novel framework for pediatric SDM, this Delphi study revealed several areas of disagreement among the panelists. For example, the panel did not agree on (1) which factors determine the child’s role in the SDM process, (2) which factors determine the appropriate level of clinician directiveness, (3) what the role of the palliative care team should be, and (4) if a family should be asked if they want a recommendation before clinicians provide one. Panelists also expressed misgivings about the word “shared” in SDM. These areas, and whether the phrase “shared” should be replaced by “personalized” or another term warrant additional exploration and discussion.
This is the first study that has examined agreement on key topics crucial to SDM among prominent experts on pediatric SDM. The resulting consensus pediatric SDM model is the first to stratify recommended processes on the basis of the clinical decision’s complexity. This proposed model of pediatric SDM is also the first developed from consensus methodology. Many recommendations in this framework are consistent with existing literature on pediatric SDM, which may follow from the fact that the panelists are prolific authors on the topic.7,23–27 Although many of these processes are discussed in other models, such as titrating clinician directiveness, we found key differences in how they should be done. For example, Kon suggests that only the parents’ desired level of directiveness should be considered,23 whereas Opel contends that the degree of clinical equipoise and preference sensitivity should also be appraised,24 yet this panel recommended that the parent’s desired level of directiveness, degree of preference sensitivity, degree of clinical uncertainty, level of urgency, and degree of clinical equipoise should all be considered. Additionally, this framework is more extensive than most SDM models and includes processes, such as determining the child’s role, that have been discussed in the literature but have not been incorporated into models of pediatric SDM.28–31
The authors of this study used an evidence-based consensus methodology and followed the recommended criteria for high-quality Delphi studies,17,20,32 including providing panelists with extensive feedback reports between rounds and recirculating all processes in every round. An additional strength of this study is the caliber and national diversity of the panel. The panel included internationally renowned experts on pediatric SDM from 5 countries and various specialties. The panel also included parents with expertise in pediatric SDM from 3 countries, resulting in a uniquely informed model of pediatric SDM because most proposed models of SDM have been developed solely by clinicians. Additionally, all panelists completed every round of the study. A limitation of this study includes the fact that, because of our recruitment criteria, we may have missed clinicians who do not publish but are experts on pediatric SDM. We attempted to address this through snowball sampling. Another limitation is that our panel was limited to experts from a limited range of countries and cultures; because the use of SDM is spreading globally,33 more work will need to be done to appraise key pediatric SDM processes in other contexts.
Conclusions
Using the Delphi methodology, an international expert panel reached a consensus on the processes involved in pediatric SDM and generated recommendations on how to facilitate and achieve pediatric SDM for both simple and complex decisions. The resulting recommendations emphasize the importance of personalizing the decision-making process while also maintaining the compatibility of clinician directiveness and recommendations with pediatric SDM. Future studies should further explore the areas of disagreement revealed by our study, such as which factors determine the appropriate level of clinician directiveness and which factors determine the child’s role in the decision-making process.
Supplementary Material
Acknowledgments
The authors wish to acknowledge the panelists Laura Boland, Desiree Collins Bradley, Mirjam de Vos, Rosa Geurtzen, Clarissa Hoover, Annie Janvier, Isabel Jordan, John Lantos, Ellen Lipstein, Douglas Opel, Quynh-An Phan, Trisha Prentice, Christopher Stille, Eduard Verhagen, Jennifer Walter, and Dominic Wilkinson. The authors also wish to thank Douglas Hill and Pamela Nathanson for their review of the manuscript.
Glossary
- SDM
shared decision-making
- VGP
values, goals, and preferences
Footnotes
Dr Eaton conceptualized and designed the study, designed the data collection instruments, collected the data, conducted the initial and final analyses, and drafted the initial manuscript; Drs Clark, Kon, Cummings, and Morrison contributed to the design of the study; Dr Feudtner contributed to the design of the study, assisted with design of the data collection instruments, conducted the final analyses, and created the graphic depictions of the results; Dr Streuli conceptualized the study, assisted with the design of the data collection instruments, and assisted with data analysis; and all authors reviewed and revised the manuscript, approved the final manuscript as submitted, and agree to be accountable for all aspects of the work.
FUNDING: Dr Cummings is supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) of the National Institutes of Health under award number R01HD094794 (CC PI) for research not related to this work.
CONFLICT OF INTEREST DISCLOSURES: The authors have indicated they have no potential conflicts of interest relevant to this article to disclose.
References
- 1. Gooding JS, Cooper LG, Blaine AI, Franck LS, Howse JL, Berns SD. Family support and family-centered care in the neonatal intensive care unit: origins, advances, impact. Semin Perinatol. 2011;35(1):20–28 [DOI] [PubMed] [Google Scholar]
- 2. Katz AL, Webb SA; Committee on Bioethics . Informed consent in decision-making in pediatric practice. Pediatrics. 2016;138(2): e20161485. [DOI] [PubMed] [Google Scholar]
- 3. National Quality Forum . NQP shared decision making action brief. In: Proceedings from the National Quality Forum; October, 2017; Washington, DC [Google Scholar]
- 4. World Health Organization . Patient Engagement: Technical Series on Safer Primary Care. Geneva, Switzerland: World Health Organization; 2016 [Google Scholar]
- 5. Michaud PA, Jucker-Kupper P, the Profiles Working Group . PROFILES: Principle Relevant Objectives and Framework for Integrated Learning and Education in Switzerland. Bern, Switzerland: Joint Commission of the Swiss Medical Schools; 2017 [Google Scholar]
- 6. Boland L, Graham ID, Légaré F, et al. Barriers and facilitators of pediatric shared decision-making: a systematic review. Implement Sci. 2019;14(1):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lantos JD. Ethical problems in decision making in the neonatal ICU. N Engl J Med. 2018;379(19):1851–1860 [DOI] [PubMed] [Google Scholar]
- 8. Singh J, Fanaroff J, Andrews B, et al. Resuscitation in the “gray zone” of viability: determining physician preferences and predicting infant outcomes. Pediatrics. 2007;120(3):519–526 [DOI] [PubMed] [Google Scholar]
- 9. Bastek TK, Richardson DK, Zupancic JA, Burns JP. Prenatal consultation practices at the border of viability: a regional survey. Pediatrics. 2005; 116(2):407–413 [DOI] [PubMed] [Google Scholar]
- 10. Boland L, Lawson ML, Graham ID, et al. Post-training shared decision making barriers and facilitators for pediatric healthcare providers: a mixed-methods study. Acad Pediatr. 2019;19(1):118–129 [DOI] [PubMed] [Google Scholar]
- 11. Wyatt KD, List B, Brinkman WB, et al. Shared decision making in pediatrics: a systematic review and meta-analysis. Acad Pediatr. 2015;15(6):573–583 [DOI] [PubMed] [Google Scholar]
- 12. Elwyn G, Frosch D, Thomson R, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27(10):1361–1367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango). Soc Sci Med. 1997;44(5):681–692 [DOI] [PubMed] [Google Scholar]
- 14. Makoul G, Clayman ML. An integrative model of shared decision making in medical encounters. Patient Educ Couns. 2006;60(3):301–312 [DOI] [PubMed] [Google Scholar]
- 15. Towle A, Godolphin W. Framework for teaching and learning informed shared decision making. BMJ. 1999;319(7212): 766–771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Stiggelbout AM, Pieterse AH, De Haes JC. Shared decision making: concepts, evidence, and practice. Patient Educ Couns. 2015;98(10):1172–1179 [DOI] [PubMed] [Google Scholar]
- 17. Boulkedid R, Abdoul H, Loustau M, %Sibony O, Alberti C. Using and reporting the Delphi method for selecting healthcare quality indicators: a systematic review. PLoS One. 2011;6(6):e20476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Keeney S, Hasson F, McKenna H. The Delphi Technique in Nursing and Health Research. Chichester, West Sussex: Wiley-Blackwell; 2011 [Google Scholar]
- 19. QSR International Pty Ltd . NVivo. Available at: https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home. Accessed November 15, 2020
- 20. Diamond IR, Grant RC, Feldman BM, et al. Defining consensus: a systematic review recommends methodologic criteria for reporting of Delphi studies. J Clin Epidemiol. 2014;67(4):401–409 [DOI] [PubMed] [Google Scholar]
- 21. Madrigal VN, Carroll KW, Hexem KR, %Faerber JA, Morrison WE, Feudtner C. Parental decision-making preferences in the pediatric intensive care unit. Crit Care Med. 2012;40(10): 2876–2882 [DOI] [PubMed] [Google Scholar]
- 22. Janvier A, Farlow B, Barrington KJ, Bourque CJ, Brazg T, Wilfond B. Building trust and improving communication with parents of children with Trisomy 13 and 18: a mixed-methods study. Palliat Med. 2020;34(3):262–271 [DOI] [PubMed] [Google Scholar]
- 23. Kon AA. The shared decision-making continuum. JAMA. 2010;304(8):903–904 [DOI] [PubMed] [Google Scholar]
- 24. Opel DJA. A 4-step framework for shared decision-making in pediatrics. Pediatrics. 2018;142(Suppl 3):S149–S156 [DOI] [PubMed] [Google Scholar]
- 25. Sullivan A, Cummings C. Historical perspectives: shared decision making in the NICU. NeoReviews. 2020;21(4): e217–e225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Haward MF, Gaucher N, Payot A, %Robson K, Janvier A. Personalized decision making: practical recommendations for antenatal counseling for fragile neonates. Clin Perinatol. 2017;44(2):429–445 [DOI] [PubMed] [Google Scholar]
- 27. Park ES, Cho IY. Shared decision-making in the paediatric field: a literature review and concept analysis. Scand J Caring Sci. 2018;32(2):478–489 [DOI] [PubMed] [Google Scholar]
- 28. Navin MC, Wasserman JA. Capacity for preferences and pediatric assent implications for pediatric practice. Hastings Cent Rep. 2019;49(1):43–51 [DOI] [PubMed] [Google Scholar]
- 29. Coyne I, Harder M. Children’s participation in decision-making: balancing protection with shared decision- making using a situational perspective. J Child Health Care. 2011;15(4): 312–319 [DOI] [PubMed] [Google Scholar]
- 30. Sabatello M, Janvier A, Verhagen E, Morrison W, Lantos J. Pediatric participation in medical decision making: optimized or personalized? Am J Bioeth. 2018;18(3):1–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Olszewski AE, Goldkind SF. The default position: optimizing pediatric participation in medical decision making. Am J Bioeth. 2018;18(3):4–9 [DOI] [PubMed] [Google Scholar]
- 32. Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique. J Adv Nurs. 2000; 32(4):1008–1015 [PubMed] [Google Scholar]
- 33. Härter M, Moumjid N, Cornuz J, Elwyn G, van der Weijden T. Shared decision making in 2017: international accomplishments in policy, research and implementation. Z Evid Fortbild Qual Gesundhwes. 2017;123–124:1–5 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.