Abstract
Background:
Liver transplantation is one of the most effective treatments for acute liver failure, chronic liver cirrhosis, and hepatocellular carcinoma. This study was implemented to evaluate the survival rate of liver transplant in Asia.
Methods:
Studies that investigated the survival rate of liver transplant were selected using a systematic search strategy in the following databases: Medline, Embase, Scopus, ProQuest, ISI Web of Science, and Cochrane to Nov 30th, 2020. Pooled survival rate and 95% confidence intervals were calculated using Der-Simonian and Laird method. Stata 16.0 (Stata Corp, College Station, TX, USA) was used for analysis.
Results:
One, 2, 3, 5, and 10-year survival rates of liver transplant were estimated to be 85%, 80%, 75%, 73%, and 71%, respectively. The results of the univariate meta-regression for defining the sources of heterogeneity for one-Year survival rate (SR) showed significant effects of bias (β high risk/moderate risk =0.059, 95% CI: 0.002, 0.115, P-Value=0.04) and follow up time (β= −0.0002, 95% CI: −0.0003, −0.00, P-Value=0.02) on heterogeneity.
Conclusion:
The survival rate of liver transplant in Asia is comparable with the corresponding rate reported in the United States and Europe. This study provides a better view of the efficiency of medical cares, regarding liver transplantation. Medical care be enhanced to increase the survival of liver transplant patients.
Keywords: Liver transplantation, Survival analysis, Meta-analysis, Asia
Introduction
Liver Transplantation (LT) has been identified as one of the most effective treatments for acute liver failure, chronic liver cirrhosis, and hepatocellular carcinoma (1, 2). Since then, liver transplantation has evolved rapidly, and the survival rate is being improved significantly over the past 25 years (lately 96% and 71% for 1-year and 10-year survival respectively) (3). In 2016, a global estimate suggested that the United States and China had the first and second largest number of liver transplantation with 7496 and 3264 cases, respectively (1). In addition, an increasing trend in LTs has been reported from different countries (4).
As a global average, the one, 10, and 18-year survival rates of liver transplantation are reported to be between 83%–88%, 68%–72%, and 48%–55%, respectively (5). In addition, the 5-year survival rates of liver transplantation for Asian, Spanish, white, and black patients were 74%, 65%, 68%, and 57% respectively (6). Moreover, in 2020 years LT in Europe achieved respectable 1- and 5-year overall survival rates of 86% and 74% (7, 8). In the United States, years one- and 5-year graft survivals for LDLT recipients were 88.4% and 78.1%, respectively, compared with 92.5% and 80.7% in propensity-score matched DBD recipients (P=0.005), respectively. Older donor age, recipient diabetes and life support requirement were significantly associated with graft failure among LDLT recipients (P<0.05)(9). Various factors such as age, sex, ethnicity, surgical techniques, type of immunosuppressive drugs, and even the individual's economic and social status affect the survival rate of liver-transplanted patients (10, 11).
Liver transplantation has revolutionized the acute prognosis of liver failure via increasing the survival of patients by 20% to 80% in 1-year and 70% in 5-year survival of the patients (3). Understanding the survival rate of liver transplants in Asia can provide valuable information on the effectiveness of the treatment strategies and determinants of the transplantation outcome. We found no comprehensive study on liver transplantation's survival rate in Asian countries.
We aimed to do a systematic review and meta-analysis on the published studies to determine the survival rate and its general determinants of liver transplantation in Asia.
Methods
The Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) guidelines were followed for the current study (12).
Search strategy
Studies that investigated the survival rate of patients with liver transplant were identified using a defined search strategy in the following databases: Medline, Embase, Scopus, ProQuest, ISI Web of Science, and Cochrane to November 30th, 2020. Moreover, we reviewed the reference lists from retrieved articles to search for further relevant studies.
Eligibility criteria
Each identified study was independently reviewed by two reviewers (FM and RKH) to determine whether the study was eligible for being included in the meta-analysis. The inclusion criteria were as follow: 1) prospective design; 2) all studies conducted on the SR of liver transplantation patients in Asia; 3) only articles published in English were included, and 4) animal studies, reviews, comments, and editorials were excluded. This study was approved by the research Ethics Committee of Shiraz University of Medical Sciences (IR.SUMS.REC.1400.257).
Data extraction and quality assessment
From each included study, the following data were extracted: first author, publication year of the study, where the study was performed, characteristics of the study population, follow up time, patients’ average age, the study sample size, and the study results.
The quality of the included studies were defined by Hoy’s checklist (13). The studies were categorized as low, moderate, and high risk of bias if their scores were equal or more than 7, between 4 and 6, and less than 4 respectively.
Statistical analysis
For estimating the pooled survival rates, we used random-effects meta-analysis. Cochran Q test was performed (P<0.001, CI 95%) to evaluate the heterogeneity among the studies and the presence of heterogeneity was analyzed using inconsistency test (I2>50%) (Higgins and Thompson 2002). Subgroup analysis was performed based on country and risk of bias. We did meta-regression analyses to identify factors that modify the survival rate of the patients and contribute to heterogeneity between the studies’ results (14). Publication bias was assessed by funnel plot and trim and fill analysis (15). The Stata 16.0 (Stata Corp, College Station, TX, USA) was used for analysis.
Results
Description of studies
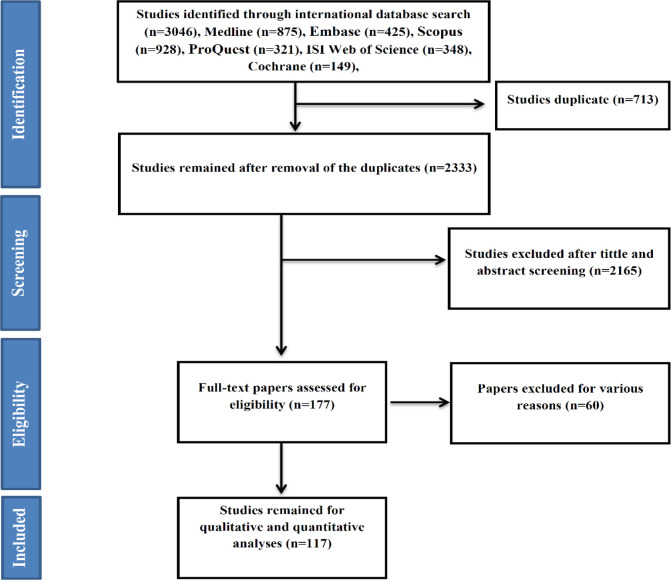
The search identified 3046 studies. In total, 713 were duplicates, 2156 defined irrelevant after reading their titles and abstracts, and 60 articles were not original (i.e. letter, commentary, review) or did not meet the inclusion criteria. As such, 117 studies (16–127), recruiting 406,464 participants, were included in this meta-analysis (Fig. 1).
Fig. 1:
Flow chart of the included eligible studies in systematic review
All studies were cohort. Of 117 studies included in this meta-analysis, 113, 22, 75, 88, and 16 reported one-year, two-year, three-year, five-year, and ten-year survival rates, respectively. Of the included studies, 39 were from China, 30 from Japan, 14 from Iran and the remaining studies (n=34) were from other countries in the Asia continent.
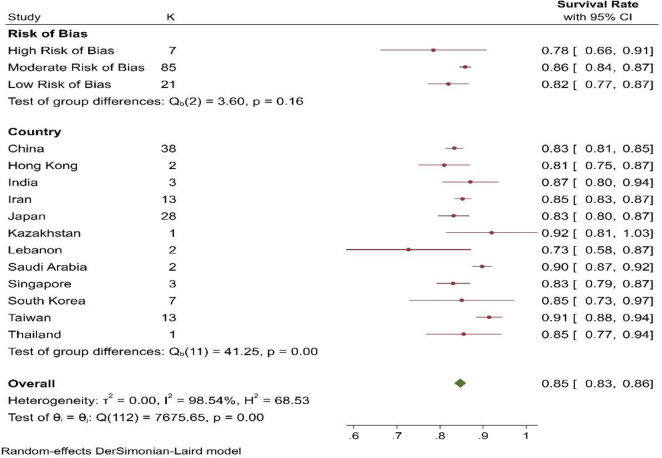
Assessment of the Risk of Bias
The risk of bias of the included studies, 10 were in the high risk of bias category, 85 studies in moderate risk and 22 studies were in the low risk of bias.
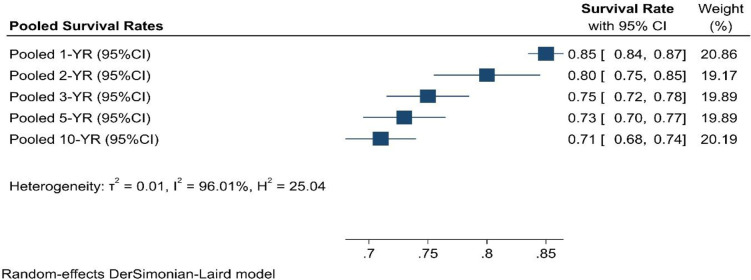
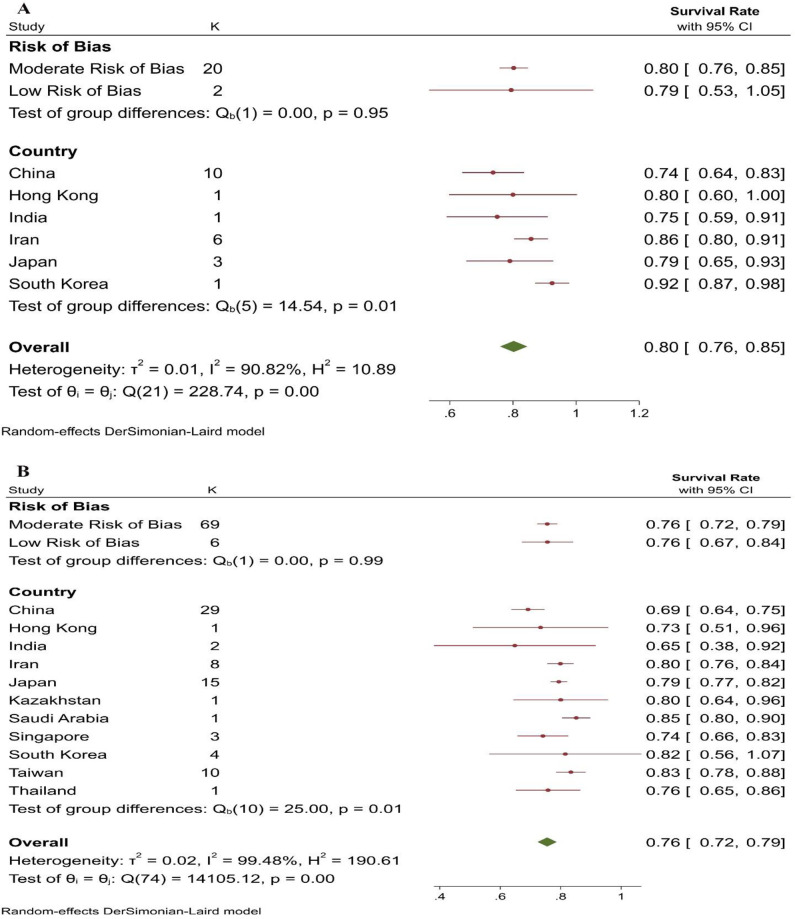
Survival rate
In this study one, 2, 3, 5, and 10-year survival rates (SR) of liver transplant were estimated to be 85%, 80%, 75%, 73%, and 71%, respectively (Fig. 2). Also, the result of test for group difference was not significant (Q=Chi2(2)=6.60, P-Value=0.16 (Fig. 3). Survival rates of liver transplantation for different times according to countries and quality of studies are presented in Fig. 4.
Fig. 2:
Pooled survival rate of liver transplantation
Fig. 3:
One-year survival rate of liver transplantation
Fig. 4:
A: 2-years survival rate of liver transplantation, B: 3-years survival rate of liver transplantation
Meta-regression analyses
The results of the univariate meta-regression for defining the sources of heterogeneity for one-Year SR showed significant effects of bias (β high risk/moderate risk =0.059, P-Value=0.04) and follow up time (β= −0.0002, P-Value=0.02) on heterogeneity. The sources of heterogeneity for three-Year SR were time (β2005-2010/before 2005 =−0.102, P-Value=0.03) and the length of follow up time (β=0.0014, P-Value=0.001). None of the covariates had a significant effect on heterogeneity of five-Year SR (Table 1).
Table 1:
Meta-regression results for one, three, and five-Year survival rates of liver transplant
| Variables | 1-YSR | 3-YSR | 5-YSR | |||
|---|---|---|---|---|---|---|
| β (95% CI) | P-value | β (95% CI) | P-value | β (95% CI) | P-value | |
| Risk of bias | ||||||
| High risk of bias | Ref | - | Ref | |||
| Moderate Risk of Bias | 0.059 (0.002, 0.115) | 0.04 | Ref | −0.044 (−0.200, 0.111) | 0.56 | |
| Low risk of bias | 0.015 (−0.048, 0.079) | 0.63 | −0.013 (−0.14, 0.12) | 0.84 | −0.063 (−0.240, 0.114) | 0.48 |
| Date of publication | ||||||
| Before 2005 | Ref | Ref | Ref | |||
| 2005–2010 | 0.025 (−0.016, 0.066) | 0.23 | −0.102 (−0.19, −0.008) | 0.03 | −0.0073 (−0.126, 0.112) | 0.90 |
| After 2010 | 0.015 (−0.024, 0.055) | 0.44 | −0.054 (−0.14, 0.034) | 0.23 | 0.0103 (−0.102, 0.123) | 0.85 |
| Follow up time | −0.0002 (−0.0003, −0.00) | 0.02 | 0.0014 (0.0006, 0.002) | 0.001 | 0.0003 (−0.00007, 0.0008) | 0.10 |
| Year of publication | 0.0014 (−0.002, 0.004) | 0.40 | 0.0000 (−0.008, 0.008) | 0.99 | 0.0026 (−0.0071, 0.012) | 0.59 |
| Sample size | −1.24e-08 (−5.94e-07 5.69e-07) | 0.96 | −2.37e−07 (−1.44e-06 9.63e-07) | 0.69 | −1.78e-07 (−1.61e-06, 1.25e-06) | 0.80 |
Publication bias
When we plotted the one, three, and five-Year survival rate; there was no publication bias. Based on the Trim and fill method no study was identified to collaborate publication bias for any survival time.
Discussion
In this meta-analysis, the probability of progression from liver transplant to the transplant rejection in 1, 2, 3, 5, and 10 years was estimated to be 85%, 80%, 75%, 73%, and 71%, respectively. The liver transplantation survival rate in Asia is comparable with the corresponding rate reported from the USA and Europe.
Factors that can affect the survival of liver transplant include disease type, clinical features, and the age of the patients. In more details, the chance of survival of patients is strongly related to the type of disease. Patients with fulminant and chronic types of disease are considerably different with regard to the survival rate, as most deaths occur in the first six months after transplantation among patients with acute liver failure (128, 129). Age is another influential variable as the function of organs, such as the liver, reduces with age (1). However, there is no cut-point recommended for the age of recipients and donors for longer survival of liver transplantation.
In addition, it is essential to consider the cause of death following each transplant. The leading causes of death are secondary to recurrent primary liver disease, especially malignancy and cirrhosis due to hepatitis C virus (HCV) (130). Graft dysfunction, technical obstacles, and infection are among the other reasons for mortality following liver transplant (131).
The highest risk of mortality associated with hepatic transplantation is during the first year post-operation, especially the first three months (132). Men and patients older than 60 year had poorer outcomes than women and younger cases (133). However, the cause of transplantation and the epidemiology of liver disease are increasingly evolving and becoming more weighted by HCV, causing a lower survival rate, compared to many other diseases. In other words, patients with HCV are distinct from the cases of primary biliary cirrhosis or primary sclerosing cholangitis (PSC), a phenomenon that makes this issue even more complex (7, 128). Although the comparable survival rates in the USA, Europe, and Asia are due to the similarity in health care practices and the expertise of surgeons, a much wider view is needed to reach a defined conclusion.
Comparing the results of studies based on their publication year, we found that the publication time of the articles was one of the factors influencing the heterogeneity of the results suggesting survival is being improved with the time goes by Smits et al. reported the same pattern in the survival of patients. The authors also reported the age of donor and recipient and blood type compatibility as significant predictors of the transplant’s survival (4, 134). According to the studies published in recent years, the transplant survival rates of European and American patients are catching up, and as observed in our study, the survival rate in Asia is becoming comparable. The improving patients’ survival rate seems to continue over time if transplantations at various times are conducted among patients with more desirable clinical conditions (9, 128).
Therefore, factors related to the donor, recipient, perioperative, and postoperative phases of transplantation may influence the survival rate of the grafts (135). For example, the donor’s characteristics that may result in poorer outcomes include older age, high body mass index, length of hospitalization, usage of vasopressors, and the presence of infection. Perioperative factors encompass cold and warm ischemia time, blood product requirements, and surgical difficulties are other factors that affect the survival of the graft (135, 136). Finally, postoperative factors are primary non-function, renal dysfunction, center experience, need for mechanical ventilation, and prolonged stay in an intensive care unit.
Strengths and Limitations
The risk of bias and the period of the study did significantly affect the survival rate of the patients. Moreover, we assessed follow-up time, year of publication, and sample size. We had few limitations in our meta-analysis. The studies on the subject did not report the characteristics of donors and recipients and the type of the selected surgical procedures, factors that can be effective in the survival of transplant. We observed statistical heterogeneity in our study.
Conclusion
Our results presented the survival rate of liver transplantation in Asia and revealed that the survival rate is comparable to that in the US and European countries. In addition, the 1 and 5-year survival rates reported in the Eastern Mediterranean countries were similar to the United States. We need further studies to define the determinants of survival of liver transplant patients. We need to consider these factors when comparing the survival of the patients. Further studies considering these factors in different subgroups are needed for estimating the survival of the grafts in different geographical locations. Medical care be enhanced to increase the survival of liver transplant patients.
Journalism Ethics considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgements
This study was supported financially by Shiraz University of Medical Sciences, Shiraz, Iran (Grant Number: 22745). Additional information is available from the corresponding author and can contact the corresponding author.
Footnotes
Conflict of interest
The authors declare that there is no conflict of interest.
References
- 1.Madreseh E, Mahmoudi M, Nassiri-Toosi M, et al. (2020). Post Liver Transplantation Survival and Related Prognostic Factors among Adult Recipients in Tehran Liver Transplant Center; 2002–2019. Arch Iran Med, 23(5):326–34. [DOI] [PubMed] [Google Scholar]
- 2.Ghelichi-Ghojogh M, Javanian M, Amiri S, et al. (2022). The survival rate of liver transplantation in children: a systematic review and meta-analysis. Pediatr Surg Int, 38(9):1177–1186. [DOI] [PubMed] [Google Scholar]
- 3.Burra P, Burroughs A, Graziadei I, et al. (2016). EASL clinical practice guidelines: liver transplantation. J Hepatol, 64(2):433–85. [DOI] [PubMed] [Google Scholar]
- 4.Wahid NA, Rosenblatt R, Brown RS., Jr (2021). A review of the current state of liver transplantation disparities. Liver Transpl, 27(3):434–43. [DOI] [PubMed] [Google Scholar]
- 5.Yang LS, Shan LL, Saxena A, et al. (2014). Liver transplantation: a systematic review of long- term quality of life. Liver Int, 34(9):1298–313. [DOI] [PubMed] [Google Scholar]
- 6.Kemmer NM, Neff GWJT. (2009). Liver transplantation trends and survival in the Asian population. Transplantation, 88(3):392–4. [DOI] [PubMed] [Google Scholar]
- 7.Müller PC, Kabacam G, Vibert E, et al. (2020). Current status of liver transplantation in Europe. Int J Surg, 82S:22–9. [DOI] [PubMed] [Google Scholar]
- 8.Germani G, Zeni N, Zanetto A, et al. (2020). Influence of donor and recipient gender on liver transplantation outcomes in Europe. Liver Int, 40(8):1961–71. [DOI] [PubMed] [Google Scholar]
- 9.Cotter TG, Minhem M, Wang J, et al. (2021). Living-Donor Liver Transplantation in the United States: Evolution of Frequency, Outcomes, Center Volumes and Factors Associated with Outcomes. Liver Transpl, 27(7):1019–1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Åberg F, Gissler M, Karlsen TH, et al. (2015). Differences in long-term survival among liver transplant recipients and the general population: a population-based Nordic study. Hepatology, 61(2):668–77. [DOI] [PubMed] [Google Scholar]
- 11.Kaido T. (2020). Recent evolution of living donor liver transplantation at Kyoto University: How to achieve a one-year overall survival rate of 99%? Hepatobiliary Pancreat Dis Int, 19(4):328–33. [DOI] [PubMed] [Google Scholar]
- 12.Moher D, Liberati A, Tetzlaff J, Altman DG. (2010). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg, 8(5):336–41. [DOI] [PubMed] [Google Scholar]
- 13.Hoy D, Brooks P, Woolf A, et al. (2012). Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol, 65(9):934–9. [DOI] [PubMed] [Google Scholar]
- 14.Thompson SG, Higgins JPJSim. (2002). How should meta-regression analyses be undertaken and interpreted? Stat Med, 21(11):1559–73. [DOI] [PubMed] [Google Scholar]
- 15.Mavridis D, Salanti G. (2014). How to assess publication bias: funnel plot, trim-and-fill method and selection models. Evid Based Ment Health, 17(1):30. [DOI] [PubMed] [Google Scholar]
- 16.Hirata M, Sugawara Y, Makuuchi M. (2002). Living-donor liver transplantation at Tokyo University. Clin Transpl, 215–9. [PubMed] [Google Scholar]
- 17.Ikegami T, Kawasaki S. (2002). Liver transplantation for fulminant hepatitis. Nihon Geka Gakkai Zasshi, 103(5):401–7. [PubMed] [Google Scholar]
- 18.Wei W, Tsoi N, Ng I, et al. (2002). Ten-year experience with liver transplantation at Queen Mary Hospital: retrospective study. Hong Kong Med J, 8(4):240–4. [PubMed] [Google Scholar]
- 19.Zheng S-S, Liang T-B, Wang W-L, et al. (2002). Clinical experience in liver transplantation from an organ transplantation center in China. Hepatobiliary Pancreat Dis Int, 1(4):487–91. [PubMed] [Google Scholar]
- 20.Sugawara Y, Makuuchi M, Kaneko J, et al. (2003). Living-donor liver transplantation in adults: Tokyo University experience. J Hepatobiliary Pancreat Surg, 10(1):1–4. [DOI] [PubMed] [Google Scholar]
- 21.Wong A, Lo C, Liu C. (2003). Outcome for Hong Kong residents undergoing cadaveric liver transplantation in mainland China. Hong Kong Med J, 9(3):165–70. [PubMed] [Google Scholar]
- 22.Hashikura Y, Kawasaki S. (2004). Living donor liver transplantation: issues regarding left liver grafts. HPB (Oxford), 6(2):99–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hasegawa K, Sugawara Y, Imamura H, et al. (2005). Living donor liver transplantation for primary biliary cirrhosis: retrospective analysis of 50 patients in a single center. Transpl Int, 18(7):794–9. [DOI] [PubMed] [Google Scholar]
- 24.Malek-Hosseini S, Mehdizadeh A, Salahi H, et al. (2005). Results of liver transplantation: analysis of 140 cases at a single center. Transplant Proc, 37(7):3157–8. [DOI] [PubMed] [Google Scholar]
- 25.Yong C-C, Chen Y-S, Wang, et al. (2005). Deceased-donor liver transplantation: 10 years’ experience at Change Gung Memorial Hospital-Kaohsiung Medical Center. Chang Gung Med J, 28(3):133–41. [PubMed] [Google Scholar]
- 26.Zhou J, Fan J, Wu Z-q, et al. (2005). Liver transplantation for patients with hepatocellular carcinoma at the Liver Cancer Institute of Fudan University, China. Chin Med J (Engl), 118(08):654–9. [PubMed] [Google Scholar]
- 27.Bharat A, Brown DB, Crippin JS, et al. (2006). Pre-liver transplantation locoregional adjuvant therapy for hepatocellular carcinoma as a strategy to improve longterm survival. J Am Coll Surg, 203(4):411–20. [DOI] [PubMed] [Google Scholar]
- 28.Fan J, Zhou J, Xu Y, et al. (2006). Indication of liver transplantation for hepatocellular carcinoma: Shanghai Fudan Criteria. Zhonghua Yi Xue Za Zhi, 86(18):1227–31. [PubMed] [Google Scholar]
- 29.Wai C, Lee Y, Selamat D, et al. (2006). Liver transplantation in Singapore. Singapore Med J, 47(7):580–3. [PubMed] [Google Scholar]
- 30.Wang X-h, Yan L-n, Zhang F, et al. (2006). Early experiences on living donor liver transplantation in China: multicenter report. Chin Med J (Engl), 119(12):1003–9. [PubMed] [Google Scholar]
- 31.Yokoi H, Isaji S, Yamagiwa K, et al. (2006). The role of living-donor liver transplantation in surgical treatment for hepatocellular carcinoma. J Hepatobiliary Pancreat Surg, 13(2):123–30. [DOI] [PubMed] [Google Scholar]
- 32.Huang J. (2007). Ethical and legislative perspectives on liver transplantation in the People's Republic of China. Liver Transpl, 13(2):193–6. [DOI] [PubMed] [Google Scholar]
- 33.Morioka D, Egawa H, Kasahara M, et al. (2007). Outcomes of adult-to-adult living donor liver transplantation: a single institution's experience with 335 consecutive cases. Ann Surg, 245(2):315–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rakela J, Fung JJ. (2007). Liver transplantation in China. Liver Transpl, 13(2):182. [DOI] [PubMed] [Google Scholar]
- 35.Concejero A, Chen C-L, Wang C-C, et al. (2008). Living donor liver transplantation for hepatocellular carcinoma: a single-center experience in Taiwan. Transplantation, 85(3):398–406. [DOI] [PubMed] [Google Scholar]
- 36.Eguchi S, Takatsuki M, Hidaka M, et al. (2008). Evolution of living donor liver transplantation over 10 years: experience of a single center. Surg Today, 38(9):795–800. [DOI] [PubMed] [Google Scholar]
- 37.Ikegami T, Taketomi A, Soejima Y, et al. (2008). Living donor liver transplantation for acute liver failure: a 10-year experience in a single center. J Am Coll Surg, 206(3):412–8. [DOI] [PubMed] [Google Scholar]
- 38.Lin N-C, Hsia C-Y, Loong C-C, et al. (2008). Liver transplantation at a small-volume procedure center—preliminary results from Taipei Veterans General Hospital. J Chin Med Assoc, 71(4):186–90. [DOI] [PubMed] [Google Scholar]
- 39.Pandey D, Wai CT, Lee KH, Tan KC. (2008). Living donor liver transplantation for hepatocellular carcinoma: a single centre experience. Indian J Gastroenterol, 27:148–52. [PubMed] [Google Scholar]
- 40.Shen Z-y, Wang Z-f, Zhu Z-j, et al. (2008). Pediatric liver transplantation in 31 consecutive children. Chin Med J (Engl), 121(20):2001–3. [PubMed] [Google Scholar]
- 41.Chan KL, Fan ST, Lo CM, et al. (2009). Pediatric liver transplantation in Hong Kong-a domain with scarce deceased donors. J Pediatr Surg, 44(12):2316–21. [DOI] [PubMed] [Google Scholar]
- 42.Chen GH. (2009). Liver transplantation in China: retrospect and prospect. Chin Med J (Engl), 122(19):2229–30. [PubMed] [Google Scholar]
- 43.Cheng F, Li GQ, Zhang F, et al. (2009). Outcomes of living-related liver transplantation for Wilson's disease: a single-center experience in China. Transplantation, 87(5):751–7. [DOI] [PubMed] [Google Scholar]
- 44.García-Valdecasas JC, Fuster J, Fondevila C, Calatayud D. (2009). Adult living-donor liver transplantation. Gastroenterol Hepatol, 32(8):577–83. [DOI] [PubMed] [Google Scholar]
- 45.Fan ST, Wang H, Lam BK. (2009). Follow-up of Chinese liver transplant recipients in Hong Kong. Liver Transpl, 15(5):544–50. [DOI] [PubMed] [Google Scholar]
- 46.Kuo WT, Hsia CY, Loong CC, et al. (2009). Outcome of foreign residents undergoing deceased donor liver transplantation in China: a single-center experience in Taiwan. Liver Transpl, 15(11):1579–85. [DOI] [PubMed] [Google Scholar]
- 47.Li J, Yan LN, Yang J, et al. (2009). Indicators of prognosis after liver transplantation in Chinese hepatocellular carcinoma patients. World J Gastroenterol, 15(33):4170–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sabet B, Rajaeefard A, Nikeghbalian S, Malek-Hosseini SA. (2009). Six years liver transplants outcome in Shiraz transplant center. J Isfahan Med School, 27(99):543–50. [Google Scholar]
- 49.Xiao L, Fu ZR, Ding GS, et al. (2009). Liver transplantation for hepatitis B virus-related hepatocellular carcinoma: one center's experience in China. Transplant Proc, 41(5):1717–21. [DOI] [PubMed] [Google Scholar]
- 50.Xiao L, Fu ZR, Ding GS, et al. (2009). Prediction of survival after liver transplantation for chronic severe hepatitis B based on preoperative prognostic scores: a single center's experience in China. World J Surg, 33(11):2420–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yoshitoshi EY, Takada Y, Oike F, et al. (2009). Long-term outcomes for 32 cases of Wilson's disease after living-donor liver transplantation. Transplantation, 87(2):261–7. [DOI] [PubMed] [Google Scholar]
- 52.Allam N, Al Saghier M, El Sheikh Y, et al. (2010). Clinical outcomes for Saudi and Egyptian patients receiving deceased donor liver transplantation in China. Am J Transplant, 10(8):1834–41. [DOI] [PubMed] [Google Scholar]
- 53.Chen CL, Concejero AM. (2010). Liver transplantation for hepatocellular carcinoma in the world: the Taiwan experience. J Hepatobiliary Pancreat Sci, 17(5):555–8. [DOI] [PubMed] [Google Scholar]
- 54.Mohamed El Moghazy W, Ogura Y, Mutsuko M, et al. (2010). Pediatric living-donor liver transplantation for acute liver failure: analysis of 57 cases. Transpl Int, 23(8):823–30. [DOI] [PubMed] [Google Scholar]
- 55.Faraj W, Deborah M, ukherji D, Fakih H, et al. (2010). Liver transplantation in Lebanon: A hard lesson to learn. Ann Transplant, 15(3):25–9. [PubMed] [Google Scholar]
- 56.Ikegami T, Soejima Y, Shirabe K, et al. (2010). Evolving strategies to prevent biliary strictures after living donor liver transplantation. Transplant Proc, 42(9):3624–9. [DOI] [PubMed] [Google Scholar]
- 57.Zhu M, Li Y, Xia Q, et al. (2010). Strong impact of acute kidney injury on survival after liver transplantation. Transplant Proc, 42(9):3634–8. [DOI] [PubMed] [Google Scholar]
- 58.Gwon DI, Sung KB, Ko GY, et al. (2011). Dual catheter placement technique for treatment of biliary anastomotic strictures after liver transplantation. Liver Transpl, 17(2):159–66. [DOI] [PubMed] [Google Scholar]
- 59.Hu X-X, Yan L-N. (2011). Retrospective analysis of prognostic factors after liver transplantation for intrahepatic cholangiocarcinoma in China: a single-center experience. Hepatogastroenterology, 58(109):1255–9. [DOI] [PubMed] [Google Scholar]
- 60.Hu Z, Zhou J, Xu X, et al. (2012). Salvage liver transplantation is a reasonable option for selected patients who have recurrent hepatocellular carcinoma after liver resection. PLoS One, 7(5):e36587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kim J, Kwon C, Joh J-W, et al. (2012). Effectiveness of locoregional therapy before living donor liver transplantation in patients with hepatocellular carcinoma who meet the Milan criteria. Transplant Proc, 44(2):403–8. [DOI] [PubMed] [Google Scholar]
- 62.Lee H-J, Hwang S, Ahn C-S, et al. (2012). Long-term outcomes of portal Y-graft interposition for anomalous right portal veins in living donor liver transplantation. Transplant Proc, 44(2):454–6. [DOI] [PubMed] [Google Scholar]
- 63.Mizuta K, Urahashi T, Ihara Y, et al. (2012). Living donor liver transplantation in children with cholestatic liver disease: a single-center experience. Transplant Proc, 44(2):469–72. [DOI] [PubMed] [Google Scholar]
- 64.Oh S, Kim K, Kim D, et al. (2012). Clinical experience of more than 200 cases of pediatric liver transplantation at a single center: improved patient survival. Transplant Proc, 44(2):484–6. [DOI] [PubMed] [Google Scholar]
- 65.Poon K-S, Chen T-H, Jeng L-B, et al. (2012). A high model for end-stage liver disease score should not be considered a contraindication to living donor liver transplantation. Transplant Proc, 44(2):316–9. [DOI] [PubMed] [Google Scholar]
- 66.Wai C-T, Woon W-A, Tan Y-M, et al. (2012). Younger age and presence of macrovascular invasion were independent significant factors associated with poor disease-free survival in hepatocellular carcinoma patients undergoing living donor liver transplantation. Transplant Proc, 44(2):516–9. [DOI] [PubMed] [Google Scholar]
- 67.Wai C-T, Woon W-A, Tan Y-M, et al. (2012). Pretransplant Model for End-stage Liver Disease score has no impact on posttransplant survival in living donor liver transplantation. Transplant Proc, 44(2):396–8. [DOI] [PubMed] [Google Scholar]
- 68.Xu L, Xu M-Q, Yan L-N, et al. (2012). Causes of mortality after liver transplantation: a single center experience in mainland china. Hepatogastroenterology, 59(114):481–4. [DOI] [PubMed] [Google Scholar]
- 69.Yoshizumi T, Shirabe K, Ikegami T, et al. (2012). Impact of human T cell leukemia virus type 1 in living donor liver transplantation. Am J Transplant, 12(6):1479–85. [DOI] [PubMed] [Google Scholar]
- 70.Yu C-Y, Ou H-Y, Huang T-L, et al. (2012). Hepatocellular carcinoma downstaging in liver transplantation. Transplant Proc, 44(2):412–4. [DOI] [PubMed] [Google Scholar]
- 71.Haseli N, Hassanzade J, Dehghani SM, et al. (2013). Living related donor liver transplantation in Iranian children: a 12-year experience. Gastroenterol Hepatol Bed Bench, 6(4):183–9. [PMC free article] [PubMed] [Google Scholar]
- 72.Haseli N, Hassanzadeh J, Dehghani SM, et al. (2013). Long-term survival and its related factors in pediatric liver transplant recipients of shiraz transplant center, shiraz, iran in 2012. Hepat Mon, 13(7) :e10257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hu Z, Zhou J, Wang H, et al. (2013). Survival in liver transplant recipients with hepatitis B-or hepatitis C-associated hepatocellular carcinoma: the Chinese experience from 1999 to 2010. PLoS One, 8(4):e61620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jiang L, Yan L-N, Wen T-F, et al. (2013). Comparison of hepatitis B prophylactic outcomes in living donor liver transplantation recipients who meet the Milan or UCSF criteria. Hepatobiliary Pancreat Dis Int, 12(5):494–9. [DOI] [PubMed] [Google Scholar]
- 75.Kasahara M, Umeshita K, Inomata Y, et al. (2013). Long-term outcomes of pediatric living donor liver transplantation in Japan: an analysis of more than 2200 cases listed in the registry of the Japanese Liver Transplantation Society. Am J Transplant, 13(7):1830–9. [DOI] [PubMed] [Google Scholar]
- 76.Kim JM, Kim KM, Yi N-J, et al. (2013). Pediatric liver transplantation outcomes in Korea. J Korean Med Sci, 28(1):42–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Pillai VG, Chen C-L. (2016). Living donor liver transplantation in Taiwan—challenges beyond surgery. Hepatobiliary Surg Nutr, 5(2):145–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lei J, Yan L. (2013). Outcome comparisons among the Hangzhou, Chengdu, and UCSF criteria for hepatocellular carcinoma liver transplantation after successful downstaging therapies. J Gastrointest Surg, 17(6):1116–22. [DOI] [PubMed] [Google Scholar]
- 79.Lei J-Y, Wang W-T, Yan L-N. (2013). Up-to-seven criteria for hepatocellular carcinoma liver transplantation: a single center analysis. World J Gastroenterol, 19(36):6077–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Li C-T, Luo J, Zhang Z-W. (2013). Risk factors for massive ascites after living donor liver transplantation in adult and impact of massive ascites on patient survival. Sichuan Da Xue Xue Bao Yi Xue Ban, 44(4):632–6. [PubMed] [Google Scholar]
- 81.Sun L-Y, Yang Y-S, Zhu Z-J, et al. (2013). Outcomes in children with biliary atresia following liver transplantation. Hepatobiliary Pancreat Dis Int, 12(2):143–8. [DOI] [PubMed] [Google Scholar]
- 82.Takada Y, Uemoto S. (2013). Living donor liver transplantation for hepatitis C. Surg Today, 43(7):709–14. [DOI] [PubMed] [Google Scholar]
- 83.Yoshizumi T, Ikegami T, Yoshiya S, et al. (2013). Impact of tumor size, number of tumors and neutrophil-to-lymphocyte ratio in liver transplantation for recurrent hepatocellular carcinoma. Hepatol Res, 43(7):709–16. [DOI] [PubMed] [Google Scholar]
- 84.Al Sebayel MI, Abaalkhail FA, Al Bahili H, et al. (2014). Liver transplantation at KFSHRC: Achievement and challenges. Ann Saudi Med, 34(2):103–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kabiling CS, Chen C-L, Concejero A, et al. (2014). Section 18. Professional framework for liver transplantation for overseas patients: traveling for living donor liver transplantation. Transplantation, 97 Suppl 8:S75–9. [DOI] [PubMed] [Google Scholar]
- 86.Kumaran V. (2014). Role of liver transplantation for hepatocellular carcinoma. J Clin Exp Hepatol, 4(Suppl 3):S97–S103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lei JY, Wang WT, Yan LN. (2014). Hangzhou criteria for liver transplantation in hepatocellular carcinoma: a single-center experience. Eur J Gastroenterol Hepatol, 26(2):200–4. [DOI] [PubMed] [Google Scholar]
- 88.Liang B-y, Huang Z-y, Zhou S-j, et al. (2014). Primary results of salvage liver transplantation in the patients with unresectable recurrent hepatocellular carcinoma after initial liver resection. Hepatogastroenterology, 61(135):2014–20. [PubMed] [Google Scholar]
- 89.Wang P, Wang C, Li H, et al. (2015). Impact of age on the prognosis after liver transplantation for patients with hepatocellular carcinoma: a single-center experience. Onco Targets Ther, 8:3775–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Oh SH, Kim KM, Kim DY, et al. (2014). Improved outcomes in liver transplantation in children with acute liver failure. J Pediatr Gastroenterol Nutr, 58(1):68–73. [DOI] [PubMed] [Google Scholar]
- 91.Yabuta M, Shibata T, Shibata T, et al. (2014). Long-term outcome of percutaneous transhepatic balloon angioplasty for portal vein stenosis after pediatric living donor liver transplantation: a single institute’s experience. J Vasc Interv Radiol, 25(9):1406–12. [DOI] [PubMed] [Google Scholar]
- 92.Al Sebayel M, Abaalkhail F, Hashim A, et al. (2015). Living donor liver transplant versus cadaveric liver transplant survival in relation to model for end-stage liver disease score. Transplant Proc, 47(4):1211–3. [DOI] [PubMed] [Google Scholar]
- 93.Faraj W, Haydar A, Nounou GE, et al. (2015). Update on liver transplants in Lebanon. Prog Transplant, 25(3):271–5. [DOI] [PubMed] [Google Scholar]
- 94.Sakamoto S, Kasahara M, Ogura Y, et al. (2015). Current status of deceased donor split liver transplantation in Japan. J Hepatobiliary Pancreat Sci, 22(12):837–45. [DOI] [PubMed] [Google Scholar]
- 95.Dong J, Zhu Y, Ma F, et al. (2016). Conditional disease-free survival after liver transplantation for hepatocellular carcinoma: a two-center experience. Medicine (Baltimore), 95(31):e4383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Eguchi S, Furukawa H, Uemoto S, et al. (2016). Outcomes of living donor liver transplantation alone for patients on maintenance renal replacement therapy in Japan: results of a Nationwide Survey. Transplant Direct, 2(6):e74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Sugawara Y, Yamamoto H, Hibi T. (2018). Living donor liver transplantation for patients with hepatocellular carcinoma in Japan. Hepatoma Res,4:33. [Google Scholar]
- 98.Liu X, Wang B, Zhang X, et al. (2016). Liver transplantation using donation after brain and cardiac death: a single-center experience in China. Transplant Proc, 48(6):1879–86. [DOI] [PubMed] [Google Scholar]
- 99.Togashi J, Akamastu N, Kokudo N. (2016). Living donor liver transplantation for hepatocellular carcinoma at the University of Tokyo Hospital. Hepatobiliary Surg Nutr,5(5):399–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Hosseini SAM, Nikeghbalian S, Salahi H, et al. (2017). Evolution of liver transplantation program in Shiraz, Iran. Hepat Mon, 17(11): e60745. [Google Scholar]
- 101.Umeshita K, Eguchi S, Egawa H, et al. (2019). Liver transplantation in Japan: registry by the Japanese liver transplantation society. Hepatol Res, 49(9):964–80. [DOI] [PubMed] [Google Scholar]
- 102.Ushigome H, Nakao T, Harada S, et al. (2016). Elderly living donor liver transplant recipients over 60 Years old at a japanese single center. Transplant Proc, 48(4):1115–8. [DOI] [PubMed] [Google Scholar]
- 103.Wang T-J, Lin C-H, Chang S-N, et al. (2016). Long-term outcome of liver transplant recipients after the development of renal failure requiring dialysis: a study using the National Health Insurance Database in Taiwan. Transplant Proc, 48(4):1194–7. [DOI] [PubMed] [Google Scholar]
- 104.Yoshizumi T, Takada Y, Shirabe K, et al. (2016). Impact of human T-cell leukemia virus type 1 on living donor liver transplantation: a multi- center study in Japan. J Hepatobiliary Pancreat Sci, 23(6):333–41. [DOI] [PubMed] [Google Scholar]
- 105.Zhang Q, Deng Y-L, Liu C, et al. (2016). Diabetes mellitus may affect the long-term survival of hepatitis B virus-related hepatocellular carcinoma patients after liver transplantation. World J Gastroenterol, 22(43):9571–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Kositamongkol P, Sanphasitvong V, Sirivatanauksorn Y, et al. (2017). Outcome of liver transplantation in hepatocellular carcinoma patients at Siriraj Hospital. Transplant Proc, 49(5):1114–1117. [DOI] [PubMed] [Google Scholar]
- 107.Wei Q, Nemdharry RS, Zhuang R-Z, et al. (2017). A good prognostic predictor for liver transplantation recipients with benign end-stage liver cirrhosis. Hepatobiliary Pancreat Dis Int, 16(2):164–8. [DOI] [PubMed] [Google Scholar]
- 108.Wei L, Chen D, Zhang B, et al. (2018). Long- term outcome and recurrence of hepatitis B virus following liver transplantation from hepatitis B surface antigen-positive donors in a Chinese population. J Viral Hepat, 25(12):1576–81. [DOI] [PubMed] [Google Scholar]
- 109.Hsu C-T, Chang M-H, Ho M-C, et al. (2019). Post-transplantation lymphoproliferative disease in pediatric liver recipients in Taiwan. J Formos Med Assoc, 118(11):1537–45. [DOI] [PubMed] [Google Scholar]
- 110.Zakaria HM, Sallam AN, Ayoub II, et al. (2017). Predictors of outcome of living donor liver transplantation for hepatocellular carcinoma. Indian J Surg, 79(4):299–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Morise Z. (2019). Developments and perspectives of laparoscopic liver resection in the treatment of hepatocellular carcinoma. Surg Today,49(8):649–55. [DOI] [PubMed] [Google Scholar]
- 112.Miura K, Sakamoto S, Shimata K, et al. (2017). The outcomes of pediatric liver retransplantation from a living donor: a 17-year single-center experience. Surg Today, 47(11):1405–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Zongyi Y, Baifeng L, Funian Z, et al. (2017). Risk factors of acute kidney injury after orthotopic liver transplantation in China. Sci Rep, 7:41555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kamo N, Kaido T, Yagi S, et al. (2018). Liver transplantation for intermediate-stage hepatocellular carcinoma. Liver Cancer, 7(2):179–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Kasahara M, Umeshita K, Sakamoto S, et al. (2018). Living donor liver transplantation for biliary atresia: an analysis of 2085 cases in the registry of the Japanese Liver Transplantation Society. Am J Transplant, 18(3):659–68. [DOI] [PubMed] [Google Scholar]
- 116.Lee EC, Kim SH, Shim JR, Park SJ. (2018). Small-for-size grafts increase recurrence of hepatocellular carcinoma in liver transplantation beyond milan criteria. Liver Transpl, 24(1):35–43. [DOI] [PubMed] [Google Scholar]
- 117.Lei M, Yan L-N, Yang J-Y, et al. (2018). Safety of hepatitis B virus core antibody-positive grafts in liver transplantation: A single-center experience in China. World J Gastroenterol, 24(48):5525–5536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Malek-Hosseini SA, Jafarian A, Nikeghbalian S, et al. (2018). Liver transplantation status in Iran: a multi-center report on the main transplant indicators and survival rates. Arch Iran Med, 21(7):275–82. [PubMed] [Google Scholar]
- 119.Zhong C-P, Xi Z-F, Xia Q. (2018). Clinical analysis of liver transplantation in autoimmune liver diseases. Hepatobiliary Pancreat Dis Int, 17(1):27–31. [DOI] [PubMed] [Google Scholar]
- 120.Chen W, Yadav DK, Bai X, et al. (2019). Liver transplantation from voluntary organ donor system in China: a comparison between DBD and DCD liver transplants. Gastroenterol Res Pract, 2019:5736702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Baimakhanov Z, Kaniev S, Doskhanov M, et al. (2019). Evolution of Liver Transplantation in Kazakhstan: Two-Era Experience of a Single Center, the First Report. Transplant Proc, 51(10):3360–3363. [DOI] [PubMed] [Google Scholar]
- 122.Shen Z, Gu C, Zheng H, et al. (2019). A twenty-year review of clinical liver transplantation. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue, 31(3):269–80. [DOI] [PubMed] [Google Scholar]
- 123.Kurata N, Ogura Y, Ogiso S, et al. (2019). Splenectomy in living donor liver transplantation and risk factors of portal vein thrombosis. Hepatobiliary Pancreat Dis Int, 18(4):337–42. [DOI] [PubMed] [Google Scholar]
- 124.Madreseh E, Mahmoudi M, Nassiri-Toosi M, et al. (2020). Post Liver Transplantation Survival and Related Prognostic Factors among Adult Recipients in Tehran Liver Transplant Center; 2002–2019. Arch Iran Med, 23(5):326–334. [DOI] [PubMed] [Google Scholar]
- 125.Basiratnia M, Dehghani SM, Razmjoee F, Derakhshan D. (2020). Prevalence of Renal Dysfunction Among Pediatric Liver Transplant Recipients. Iran J Kidney Dis, 14(2):119–125. [PubMed] [Google Scholar]
- 126.Malek-Hosseini SA, Habibzadeh F, Nikeghbalian S. (2019). Shiraz organ transplant center: the largest liver transplant center in the world. Transplantation, 103(8):1523–5. [DOI] [PubMed] [Google Scholar]
- 127.Nikeghbalian S, Malekhosseini SA, Kazemi K, et al. (2021). The largest single center report on pediatric liver transplantation: experiences and lessons learned. Ann Surg, 273(2):e70–e72. [DOI] [PubMed] [Google Scholar]
- 128.Roberts MS, Angus DC, Bryce CL, et al. (2004). Survival after liver transplantation in the United States: a disease-specific analysis of the UNOS database. Liver Transpl, 10(7):886–97. [DOI] [PubMed] [Google Scholar]
- 129.Dueland S, Syversveen T, Solheim JM, et al. (2020). Survival Following Liver Transplantation for Patients With Nonresectable Liver-only Colorectal Metastases. Ann Surg, 271(2):212–8. [DOI] [PubMed] [Google Scholar]
- 130.Vogt DP, Henderson JM, Carey WD, Barnes DJS. (2002). The long-term survival and causes of death in patients who survive at least 1 year after liver transplantation. Surgery, 132(4):775–80. [DOI] [PubMed] [Google Scholar]
- 131.Cuervas-Mons V, Martinez AJ, Dekker A, et al. (1986). Adult liver transplantation: an analysis of the early causes of death in 40 consecutive cases. Hepatology, 6(3):495–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Mora NP, Klintmalm GB, Solomon H, et al. (1992). Survival after liver transplantation in 300 consecutive patients: the influence of age, clinical status, and pretransplant disease. Transplant Proc, 24(1):156–7. [PubMed] [Google Scholar]
- 133.Jain A, Reyes J, Kashyap R, et al. (2000). Long-term survival after liver transplantation in 4,000 consecutive patients at a single center. Ann Surg, 232(4):490–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Smits J, De Meester J, Persijn G, et al. (1996). Long-term results of solid organ transplantation. Report from the Eurotransplant International Foundation. Clin Transpl, 109–27. [PubMed] [Google Scholar]
- 135.Saidi RF. (2012). Current status of liver transplantation. Arch Iran Med, 15(12):772–6. [PubMed] [Google Scholar]
- 136.Kadohisa M, Inomata Y, Uto K, et al. (2021). Impact of Donor Age on the Outcome of Living-donor Liver Transplantation: Special Consideration to the Feasibility of Using Elderly Donors. Transplantation, 105(2):328–37. [DOI] [PubMed] [Google Scholar]