Abstract
An Online Survey among Interventional Cardiologists (IC) assessed the knowledge (five questions) and practice of radiation safety (eleven questions). Out of 185 respondents, knowledge of annual radiation dose (2% knew), LAO cranial view giving maximum radiation (48%) and benefit of assessment of radiation exposure with dose area product (31%) was limited. Radiation safety was practiced “whenever I remember” in 37–59%. Radiation safety practices were optimal frame rate selection (32%), distancing from x-ray unit (17%), collimation use (30%), positioning the image detector close to chest (91%) and personal dosimeters use (40%). A major gap exists between knowledge and practice of radiation safety.
Keywords: Radiation safety, Ionizing radiation, Interventional cardiologist
1. Introduction
Ionizing radiation in the Catherization laboratory (CL) is an unrecognized hazard producing both stochastic and tissue reactions (non-stochastic effects); the former has a linear dose response, and the latter has a threshold. Stochastic effect damages the genetic material of the cell and reprograms the cell to dysfunction – the important stochastic effect is radiation induced cancer. Tissue, non-stochastic or deterministic effect is due to radiation dose dependent cell injury and necrosis. Skin injury, cataract, bone marrow damage are examples of tissue injury.1 There is also an overlap category with diseases like cataract and thyroid malignancies.2
Knowledge and practice of radiation safety among Interventional Cardiologists (ICs) is personal and is neither standardized nor mandated. The knowledge and current practice in radiation safety among ICs is analysed in the present study with an intention to overcome the lacuna in knowledge and practice of radiation safety among ICs.
2. Methods
An online questionnaire contained three subheadings, namely, the nature of interventional work, knowledge of radiation protection and the current practice by the ICs. Knowledge was assessed by five questions: advantage of collimation, most hazardous view during angiography, how frequently should the machine be calibrated, most useful parameter for prediction of radiation exposure, and the recommended dose limit for persons exposed to radiation. Radiation safety practices were assessed based on eleven parameters: use of low fluoroscopy mode, frame rate selection, timely termination of cine recording, collimation use, moving away from the unit, positioning the image detector closer to patient's chest, use of table and ceiling mounted shields, placement and follow up of personal dosimeters, use of personal protective equipment (PPE) – lead goggles, thyroid shield, lead apron, lead cap, forearm, and leg shields.
The link to the questionnaire was circulated among ICs and their responses were analysed.
3. Results
The link to the questionnaire was circulated among nearly 500 cardiologists by e-mail and messaging services and elicited 218 responses. The 33 duplicate entries were removed and 185 responses were analysed. Most of the ICs 173 (93%) performed coronary interventions. Four cardiologists performed only diagnostic angiography, seven did only electrophysiology work and one performed only structural interventions.
Results of the knowledge of radiation safety measures and practice of radiation safety are given in Table 1.
Table 1.
Knowledge and Safety practice by Interventional Cardiologists.
| Knowledge based question | Awareness | Lacking awareness |
|---|---|---|
| 1. Advantage of using collimation: Reduced area of exposure to the patient; Reduced scatter radiation to the operator and staff; Improved quality of image | 151 (82%) | 34 (18%) |
| 2. Left anterior oblique cranial (LAO cranial) was mentioned as the most hazardous for radiation exposure (others mentioned different views) | 97 (52%) | 88 (48%) |
| 3. Optimal frequency for equipment calibration (once in 6 months to one year) | 141 (76%) | 44 – not done (24%) |
| 4. The most useful predictor of radiation exposure to patient and the staff is DAP (Dose area product), Air Kerma compared to fluoroscopy time | 128 (69%) | 54 fluorotime (29%), 3 not aware (2%) |
| 5. Annual occupational dose limits for cath lab personnel? International recommendations: 20mSv/year averaged over defined periods of 5 years with no individual annual exposure to exceed 30 mSv. Lens of the eye 100 mSv 5 years (20 mSv/year) Skin 500 mSv/year Hands and feet 500 mSv/year |
Only 4 correct (2%) others aware 169 (91%) |
12 (6%) |
|
Safety measures or techniques |
Practiced |
Not practiced |
| 1. Low Fluoroscopy mode | 79 always (43%) 76 not always (41%) |
30 (16%) |
| 2. Frame rate selection for fluoroscopy and cine angiography | 60 routinely (32%) 86 whenever I remember (46%) |
40 (22%) |
| 3. Timely termination of Cine recording | 156∗ (84%) | 28 (16%) |
| 4. Collimation | 56 always (30%) 108 not always (59%) |
21 not using (11%) |
| 5. Moving away from X-ray unit | 32 always (17%) 74 whenever I remember (40%) |
79 (43%) |
| 6. Positioning image detector closer to patient's chest | 168 (91%) | 17 (9%) |
| 7. Proper use of table and ceiling mounted shields | 91 (49%) 76 not always (41%) |
18 – never or Not available (10%) |
| 8. Use of dosimeters/Thermoluminescence Dosimetry (TLD) badge | 75 (40%) Whenever remembered 68 (37%) |
42 (23%) |
| 9. Placement of dosimeters | ||
| Chest underneath the lead apron | 119/143 – (83%) | |
| Collar dosimeter | 19/143 –(13%) | |
| Ring badge/forearm dosimeter | 5/143 (4%) | |
| 10. Follow up of dosimeter readings | 71/143 always, (50%) 64/143 occasionally (45%) |
8/143 (5%) |
| 11. Use of PPE (Personal protective equipment) | ||
| Lead apron (0.5 mm or 1.0 mm) | 185 (100%) | |
| Thyroid shield | 164 (87%) | |
| Lead goggles | 65 (35%) | |
| Lead cap | 84 (45%) | |
| Lead apron + Thyroid shield + Lead cap + Leg shield and/or forearm shield | 1 (0.5%) | |
| Leg and or forearm shield | 10 (5%) |
4. Discussion
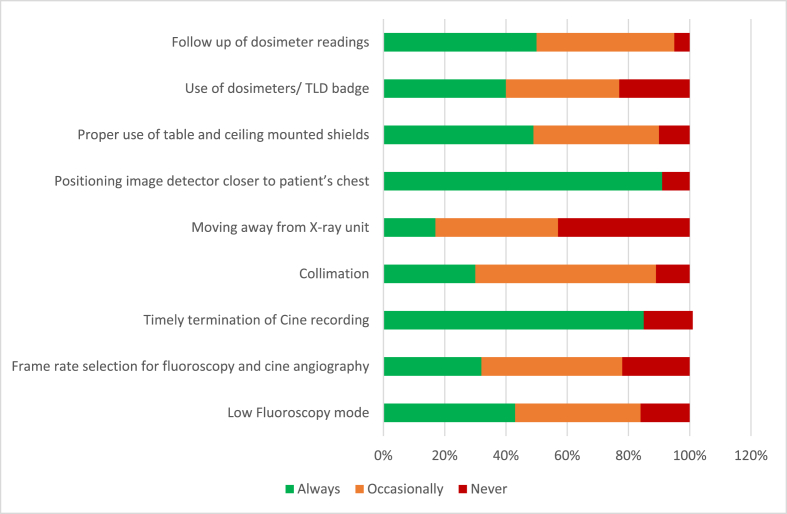
The basic principles of radiation safety are time, distance and shielding. Radiation exposure in the CL is of two types – fluoroscopy and cine angiography. Last fluoroscopy hold (a.k.a fluoro save) compared to cineangiography was associated with lower contrast use, fluoroscopy time and dose area product (DAP) without compromising the estimation of stenosis.3 The KAR-RAD study noted that low dose radiation (frame rate of 7.5/second) versus standard dose radiation (frame rate ≥10 frames/second) significantly reduced the DAP (723.60 μGy·m2 [IQR, 313.09–2328.22 μGy·m2] vs. 5203.40 μGy·m2 [IQR, 2743.55–10064.71 μGy·m2]; P < .001) without any significant change in the contrast dose or fluoroscopy time.4 In the present study, regular practice of low fluoroscopy mode and frame rate selection were 43% and 32% respectively whereas 41% and 46% practiced occasionally. The inconsistencies in practice of radiation safety measures in the CL is shown in Fig. 1.
Fig. 1.
The consistency of practice of different radiation safety measures among Interventional Cardiologists. TLD – Thermoluminescent Dosimeter.
Measurement of exposure to radiation is important. Fluoroscopy time underestimates the radiation exposure and does not include acquisition. Kinetic energy released in material (Kerma) measured in Gray (Gy) represents one joule energy released per kilogram of absorbing material. Air kerma uses air as the absorbing material. Cumulative Air kerma measures the radiation at the spot and correlates with deterministic or tissue effects.1 Air kerma area product or Dose Area Product (DAP) is the sum of air kerma and area of exposure and correlates with the stochastic effects. Effective dose, expressed in Sievert is a reliable measure of radiation and organ specific damage. In our data, 69% of ICs had some knowledge about air kerma and DAP, whereas 29% used fluoroscopy time.
Collimation is the restriction of radiation to the area of interest using lead shutters within the x-ray tube.5 In this study, 82% were aware of collimation while only 32% practiced it routinely, exposing the knowledge-practice gap. Routine calibration of the CL every 6–12 months is important since leaks in the X-ray tube increases the radiation exposure. This practice was adopted by 69% in the present study.
4.1. Personal protective equipment
The Atomic Energy Regulatory Board (AERB) specifies a whole body dose limit of 20 mSv/year averaged over five years or 30 mSv in a single year. Equivalent dose for the lens is 150 mSv/year, and for the skin and extremities the dose is 500 mSv/year.6 Only the lead apron was routinely being used in the present study. RELID study revealed 45% of ICs had posterior subcapsular lens changes (attributable to radiation); 57% never/infrequently used lead goggles. 32% of paramedical staff and 12% of controls had posterior lens changes.7 In the present study, 65% did not use lead goggles. The table and ceiling mounted shield was used by 90% in the present study while the usage was 49% in the RELID study.8
The limitations of the study are the small number of responders and non-availability of the dose of radiation exposure which can be correlated with the knowledge of radiation safety. Future follow up radiation safety and practice with larger number of responders is planned at IC conferences.
5. Conclusion
ALARA (As Low As Reasonably Achievable) is the motto of radiation safety along with optimal use of protective equipment – both personal and general. Hardware improvements, software improvements, personal measures and operator technique must be emphasized to reduce radiation exposure to the ICs are summarized I Table 2 9 Dissemination of this knowledge to the ICs and CL personnel can improve radiation safety within the catheterization laboratory.
Table 2.
Safety measures that can be practiced by Interventional Cardiologists to limit radiation injury.
| Hardware Measures | Software Measures | Personal Measures | Procedural Measures |
|---|---|---|---|
| Pulsed fluoroscopy | Automated exposure control | Regular PPE usea | Use low fluoroscopy mode |
| Flat panel detectors | Last fluoroscopy Save | Proper use of dosimeter in the collar | Lower frame rate selection |
| Regular q6 months service of the equipment | Record the DAP for each patient | Regular interrogation of personal dosimeter | Proper collimation |
| Use the table and ceiling mounted shield | Keep the image detector close to patient | ||
| Move away from radiation | Less use of LAO cranial oblique views | ||
| Timely termination of angio fluoroscopy |
-lead apron, cap, goggles, thyroid, forearm and leg shield; PPE – personal protective equipment. LAO – left anterior oblique.
Contributor Information
Prabhakar Dorairaj, Email: prabhud19@gmail.com.
Shanmugasundaram Somasundaram, Email: prabhud19@gmail.com.
References
- 1.Hirshfeld J.W., Ferrari V.A., Bengel F.M., et al. ACC/HRS/NASCI/SCAI/SCCT expert consensus document on optimal use of ionizing radiation in cardiovascular imaging: best practices for safety and effectiveness. J Am Coll Cardiol. 2018 Jun 19;71(24):e283–e351. doi: 10.1016/j.jacc.2018.02.016. 2018. [DOI] [PubMed] [Google Scholar]
- 2.Hamada N., Fujimichi Y. Classification of radiation effects for dose limitation purposes: history, current situation and future prospects. J Radiat Res. 2014 Jul;55(4):629–640. doi: 10.1093/jrr/rru019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Olcay A., Guler E., Karaca I.O., et al. Comparison of fluoro and cine coronary angiography: balancing acceptable outcomes with a reduction in radiation dose. J Invasive Cardiol. 2015 Apr;27(4):199–202. [PubMed] [Google Scholar]
- 4.Kar S., Teleb M., Albaghdadi A., Ibrahim A., Mukherjee D. Efficacy of low-dose compared with standard-dose radiation for cardiac catheterization and intervention (KAR RAD study) J Invasive Cardiol. 2019 Jun;31(6):187–194. [PubMed] [Google Scholar]
- 5.Bomer J., Wiersma-Deijl L., Holscher H.C. Electronic collimation and radiation protection in paediatric digital radiography: revival of the silver lining. Insights Imaging. 2013 Aug 28;4(5):723–727. doi: 10.1007/s13244-013-0281-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Radiation Protection Principle https://www.aerb.gov.in/english/radiation-protection-principle [Internet], [cited 2022 Jan 25]. Available from:
- 7.Papp C., Romano-Miller M., Descalzo A., et al. Results of RELID study 2014-BUENOS aires, Argentina retrospective evaluation of lens injuries and dose. Radiat Protect Dosim. 2017 Apr 1;173(1–3):212–217. doi: 10.1093/rpd/ncw339. [DOI] [PubMed] [Google Scholar]
- 8.https://www.jacc.org/doi/pdf/10.1016/S0735-1097%2811%2961951-7 Full Text PDF [Internet]. [cited 2022 Jan 20]. Available from:
- 9.Hilton Jonathan. https://www.britishcardiovascularsociety.org/resources/editorials/articles/radiation-safety-in-the-cath-lab-does-it-still-matter Radiation safety in the cath lab: does it still matter? [Internet]. BCS. corporateName: [site name]; 2020 [cited 2022 Jan 23]. Available from: