Abstract
OBJECTIVES
We evaluated the impact of distancing practices on secondary transmission of severe acute respiratory syndrome coronavirus 2 and the degree of sports-associated secondary transmission across a large diverse cohort of schools during spring 2021.
METHODS
Participating districts in North Carolina and Wisconsin and North Carolina charter schools offering in-person instruction between March 15, 2021 and June 25, 2021 reported on distancing policies, community- and school-acquired infections, quarantines, and infections associated with school-sponsored sports. We calculated the ratio of school-acquired to community-acquired infection, secondary attack rates, and the proportion of secondary transmission events associated with sports. To estimate the effect of distancing and bus practices on student secondary transmission, we used a quasi–Poisson regression model with the number of primary student cases as the denominator.
RESULTS
During the study period, 1 102 039 students and staff attended in-person instruction in 100 North Carolina school districts, 13 Wisconsin school districts, and 14 North Carolina charter schools. Students and staff had 7865 primary infections, 386 secondary infections, and 48 313 quarantines. For every 20 community-acquired infections, there was 1 within-school transmission event. Secondary transmissions associated with school sports composed 46% of secondary transmission events in middle and high schools. Relaxed distancing practices (<3 ft, 3 ft) and increased children per bus seat were not associated with increased relative risk of secondary transmission.
CONCLUSIONS
With universal masking, in-person education was associated with low rates of secondary transmission, even with less stringent distancing and bus practices. Given the rates of sports-associated secondary transmission, additional mitigation may be warranted.
What’s Known on This Subject:
Within-school transmission of severe acute respiratory syndrome coronavirus 2 is rare. With more children returning to school for the 2021–2022 academic year, distancing and decreased capacity on buses will be difficult.
What This Study Adds:
Among >1 million students and staff attending in-person school in North Carolina and Wisconsin, <1% exposed to severe acute respiratory syndrome coronavirus 2 subsequently developed infection. Distancing and bussing policies were not associated with secondary transmission; however, substantial transmission was associated with athletics.
After initial widespread school closures, many kindergarten through 12th grade (K–12) schools in the United States gradually reopened for in-person learning during the 2020–2021 academic year. Most adopted various mitigation measures to slow the spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) on the basis of early data revealing that layered mitigation measures were associated with minimal spread, even in the setting of high community transmission.1–3 Early methods to reduce transmission included a focus on reduced classroom capacity and hybrid instruction. Nevertheless, as time passed, schools have been shown to be demonstrably safe if mitigation measures are followed, so the emphasis for the 2021–2022 academic year has been to optimize access to education and resources by returning as many children as possible to school buildings for in-person learning. Importantly, when returning children to schools, distancing to the degree implemented early on is not feasible because of space constraints. Preliminary data suggested that distancing of >3 vs >6 ft did not make a difference in rates of coronavirus disease 2019 (COVID-19) infections4; however, total school case counts and community transmission were examined, not the impact of reduced distancing on within-school transmission, which is the most important metric for determining if schools can successfully keep students and staff safe.
To optimize the safe and full return of children to K–12 schools in the current academic year, the relative impact that mitigation measures (including distancing practices) will have on minimizing in-school exposure to SARS-CoV-2 must be considered. Additionally, an understanding of specific activities that are associated with increased risk of secondary transmission of SARS-CoV-2 in schools, such as participation in sports, may have important policy implications, including the places where and situations in which SARS-CoV-2 testing and vaccination should be most strongly emphasized.
We examined the impact of distancing practices, bus seat occupancy, and participation in athletics on secondary transmission of SARS-CoV-2 across a large diverse cohort of schools during the spring of 2021.
Methods
Study Setting
The study occurred in K–12 schools across the state of North Carolina and in south central Wisconsin between March 15, 2021, and June 25, 2021. On March 11, 2021, the governor of North Carolina signed the Reopen Our Schools Act of 2021 (Senate Bill 220 or Session Law 2021-4) into law, which required that all public elementary schools return to full in-person instruction and that each district offer, at minimum, hybrid instruction for all public middle and high schools.5 All 115 North Carolina local education agencies (LEAs), or school districts, and 200 North Carolina charter schools were eligible to participate in the study if they complied with North Carolina state legislation (Session Law 2021-4) and opted to sign data use agreements with The ABC Science Collaborative (ABCs), a partnership between scientists and school leadership that uses evidence and research to safely return children to schools.6
Public schools in North Carolina followed the North Carolina Department of Health and Human Services StrongSchoolsNC Toolkit and implemented various mitigation measures, including universal masking of students and staff regardless of vaccination status and hand-washing.7 Importantly, 3 ft of physical distancing was recommended between students, but no minimum distancing was mandated. In Wisconsin, 2 ABCs investigator partners (S.M.B. and G.P.D.) collaborated with districts in and surrounding Dane County, Wisconsin, throughout the 2020–2021 academic year; data were requested from these 20 Wisconsin school districts. An emergency order initially issued by the Dane County Public Health Department on August 21, 2020, that restricted in-person education to solely kindergarten through second grade8 was later reversed on December 15, 2020,9 when restrictions to in-person instruction for all grades were lifted. Individual school districts then decided on instructional models for grades K–12 for the remainder of the school year, with the majority developing plans to transition to in-person instruction between January 2021 and June 2021. By March 15, 2021, and through the end of the study period, schools operated under a combination of in-person and virtual instructional models owing to state laws allowing for local control by public school districts and delegation of authority to county health departments. All collaborating Wisconsin school districts offered in-person instruction to elementary schoolchildren. Most collaborating school districts began to phase in in-person instruction for middle and high school students by April 2021; all districts offered in-person hybrid instruction, at minimum, to all grades by early May 2021. The county public health department continued to require face coverings in all school buildings until June 2, 2021; all collaborating Wisconsin school districts continued to require face coverings in their buildings through the end of the study period. Information on sports policies and a list of sports in which at least 1 game was played in at least 1 district during the study period is provided in the Supplemental Information.
Data Sources
Data from North Carolina schools were obtained from LEAs and charter schools offering full in-person instruction to elementary, middle, and high school students from March 2021 to June 2021 that opted to sign data use agreements. For both North Carolina and Wisconsin participating school districts, investigators used publicly available sources to obtain demographic data, including enrollment information, size of district, number of schools, and racial and ethnic student composition.10–13 In both North Carolina and Wisconsin, participating districts provided aggregate school-level data that included no identifiable personal information. At the initiation of the study, districts completed an initial survey that forecasted the number of in-person students and staff and detailed mitigation policies, including the number of children per school bus seat and distancing within the classroom. For the duration of the study period, districts and charters reported weekly COVID-19 case counts for both students and staff at the school level. At the end of the study period, districts completed a final survey that included the number of in-person students and staff during the study period by school level (elementary, middle, high), the number of quarantined students and staff during the study period, reasons for quarantine (community versus in-school exposure), and numbers of cases and quarantines attributed to school-based athletic and extracurricular activities.
Definitions and Outcomes
Primary infections were those deemed to be community acquired, and secondary infections were those acquired within school or after a school-related exposure; infection source was adjudicated by school staff, as well as local health department contact tracing efforts and SARS-CoV-2 testing. A quarantine occurrence was any exclusion of a student or staff from school after exposure to SARS-CoV-2, but only quarantine occurrences after school-related SARS-CoV-2 exposures were included in these analyses. School-related exposures could include exposures occurring in school buildings, in school sports activities, or through school-sponsored extracurricular activities. Secondary attack rates were calculated as the number of acquired secondary infections among those who were exposed to primary infections, with quarantine as the proxy for exposure. For districts where quarantine data were missing or incomplete, secondary attack rates could not be calculated; therefore, secondary infections in these districts were excluded from analyses. Secondary/primary infection ratio was calculated as the number of secondary (within school) infections generated from primary (community acquired) infections.
Statistical Analyses
We conducted descriptive statistical analyses on the demographics of participating districts and charter schools. To analyze beyond demographics, all 14 charter schools were combined into 1 “district,” thereby totaling 101 North Carolina districts. We also described the number of in-person students and staff, the number of primary (community acquired) and secondary (acquired within school) infections, and the quarantine occurrences, including reasons for quarantine of students and staff during the reporting period. We estimated secondary attack rates as the number of secondary (acquired within school) infections divided by the total estimated number of those who were exposed, represented by the number quarantined for school-related exposure. To estimate the number of within-school–acquired infections that originated from all community-acquired infections that entered schools, we calculated a secondary/primary infection ratio for the overall cohort and by district. We examined the proportion of middle and high school student secondary infections that were attributed to sports-associated exposure in districts that reported sports-specific secondary transmission.
We then analyzed primary and secondary transmission within districts on the basis of physical distancing policy category and number of students per bus seat. To estimate the effect of distancing and bus practices on student secondary transmission, we used a quasi–Poisson regression model with the number of primary student cases as the denominator. For these analyses, we used conservative distancing policies (eg, 1 child per bus seat and 6 ft of distancing) as the reference categories. We then conducted a sensitivity analysis in which, under the assumption that contact tracing is imperfect, we classified 10% of primary cases as secondary cases and reran the regression analysis. We performed descriptive analyses in Stata version 16.1 (Stata Corp, College Station, TX) and quasi Poisson regression in R version 4.0.2.14 North Carolina data collection and analysis was performed under the ABCs of North Carolina Plan A protocol (Pro00108073), deemed exempt by the Duke University Institutional Review Board. Wisconsin data collection and analysis was performed under a protocol (IRB00070029) deemed exempt by the University of Wisconsin Institutional Review Board.
Results
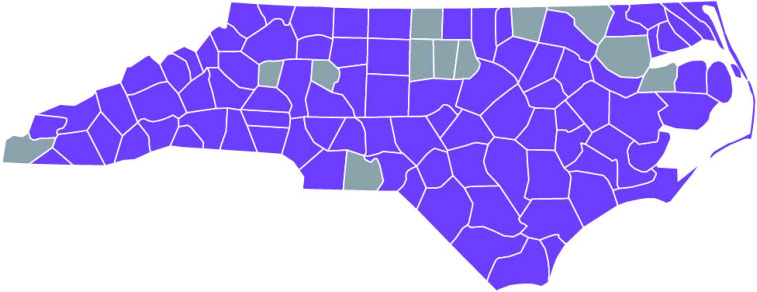
One hundred North Carolina LEAs, 14 North Carolina charter schools, and 13 Wisconsin school districts participated in the study. These districts enrolled a population of >1.3 million students in 2334 schools (2221 in North Carolina, 95%). Demographics of enrolled students are shown in Table 1. The districts were located in urban, suburban, and rural settings and were diverse in size: 45% of districts had <5000 students (small districts), 35% of districts had 5000 to 15 000 students (medium-sized districts), and 20% of districts had >15 000 students (large districts). North Carolina counties with at least 1 school district reporting are displayed in Fig 1. During the study period, 948 272 students (70% of total enrolled) and 153 767 staff attended in-person instruction in the 113 districts (North Carolina and Wisconsin) and 14 North Carolina charter schools (Table 2).
TABLE 1.
Demographics of All Students in Participating Districts
| Race and Ethnicitya | Total | Wisconsin Districtsb (n = 13) | North Carolina LEAsc (n = 100) | North Carolina Charter Schoolsd (n = 14) |
|---|---|---|---|---|
| American Indian, n (%) | 15 450 (1) | 200 (<1) | 15 230 (1) | 20 (<1) |
| Asian American, n (%) | 53 717 (4) | 4758 (7) | 48 629 (4) | 330 (3) |
| Black, n (%) | 318 402 (24) | 7290 (10) | 309 923 (24) | 1189 (12) |
| Hispanic, n (%) | 258 760 (19) | 10 203 (14) | 247 508 (20) | 1049 (10) |
| Pacific Islander, n (%) | 1845 (<1) | 39 (<1) | 1799 (<1) | 7 (<1) |
| White, n (%) | 634 373 (47) | 44 772 (62) | 582 508 (46) | 7093 (69) |
| ≥2, n (%) | 67 025 (5) | 5329 (7) | 61 077 (5) | 619 (6) |
| Sum | 1 349 572 | 72 591 | 1 266 674 | 10 307 |
In both Wisconsin and North Carolina, demographics are reported at the beginning of the academic year and include all students who were enrolled. Therefore, the numbers reported here do not equal the number of in-person learners.
In both Wisconsin and North Carolina, race and ethnicity are combined for reporting purposes.
Data obtained from the Wisconsin District of Public Instruction.13
Data obtained from the North Carolina Department of Public Instruction.10
Data obtained from the North Carolina Department of Public Instruction.11
FIGURE 1.
North Carolina reporting counties: representative map of North Carolina counties with at least 1 district reporting. Counties highlighted in purple had at least one school district reporting data to this study; counties in grey did not have any school districts reporting.
TABLE 2.
District Characteristics and Quarantine
| District Characteristics and Quarantine | Districts (127 Total), n (%) | Studentsa (948 272 Total), n (%) | Staffb (153 767 Total), n (%) |
|---|---|---|---|
| North Carolina LEAs | 100 (78) | 897 327 (95) | 143 304 (93) |
| North Carolina charter schools | 14 (11) | 5338 (<1) | 904 (<1) |
| Wisconsin school districts | 13 (10) | 45 607 (5) | 10 309 (7) |
| LEA sizec | |||
| Small (<5000) | 51 (45) | 118 870 (13) | 20 347 (13) |
| Medium (5000–15 000) | 40 (35) | 261 983 (27) | 42 864 (28) |
| Large (>15 000) | 23 (20) | 567 419 (60) | 91 306 (59) |
| School-related quarantined | 48 313 (4) | 45 097 (5) | 3216 (2) |
These numbers represent in-person students.
These numbers represent in-person staff.
Composite charter schools district is included as one small LEA.
Total quarantine reported for each incidence of quarantine (may not be mutually exclusive).
COVID-19 Infections, School-Related Quarantines, and Secondary Attack Rates
The incidences of primary (community acquired) infections and secondary (acquired within school) infections are shown in Table 3. Students and staff had 7865 primary infections and 386 secondary infections during the study period. School-related exposures resulted in 48 313 quarantine incidences; 45 097 (5%) students attending in-person instruction were quarantined during the study. These quarantine occurrences represented an estimated 360 776 missed days of school, or 8 days of missed in-person education for each quarantine.
TABLE 3.
District Primary and Secondary Infections
| COVID-19 Cases | Total, n | Students Infected, n | Staff Infected, n |
|---|---|---|---|
| Primary infections | 7865 | 6726 | 1139 |
| North Carolina | 7466 | 6373 | 1093 |
| Wisconsin | 399 | 353 | 46 |
| Secondary transmission | 386 | 331 | 55 |
| North Carolina | 359 | 304 | 55 |
| Wisconsin | 26 | 26 | 0 |
Across all districts and charter schools, despite the high burden of quarantine, the ratio of within-school–acquired/community-acquired infections was 0.05, meaning that for every 20 primary infections, there was 1 secondary transmission event (range of secondary/primary infection ratio per district was 0–0.875; mean 0.06). Among 102 districts where school-related quarantine data were reported for both students and staff, an estimated overall secondary attack rate across districts was 0.7% (344 secondary infections among 48 142 school-related quarantines); this varied by district with a range of 0% to 33% (mean: 2%).
Sports-Associated Secondary Transmission
Sixty-eight North Carolina LEAs and 13 Wisconsin districts reported the number of student secondary infections that were associated with sports and were included in the sports-associated secondary transmission subanalysis. In these districts, there were 60 student sports-associated secondary infections; sports-associated infections accounted for 46% of total secondary infections in middle and high schools (76 secondary infections in high school students; 55 secondary infections in middle school students). In North Carolina, sports-associated infections and quarantines were reported at the district level and not categorized by middle or high school; however, a subanalysis of Wisconsin data revealed that across the 13 districts, all 16 cases of secondary transmission that occurred in high schools were associated with sports. In staff, there were 8 sports-associated secondary infections in middle and high schools, accounting for 42% of total secondary infections in middle and high school staff.
Association Between Distancing, Children per Bus Seat, and Secondary Transmission
A quasi–Poisson regression analysis revealed no detectable increase in the relative rate of secondary transmission with decreased distancing of 3 or <3 ft when compared with 6-ft distancing (Table 4). Similarly, there was no notable increase in the relative rate of secondary transmission with an increasing number of students per bus seat when compared with 1 student per bus seat. In a sensitivity analysis, the incidence rate ratios remained consistent but with narrower confidence intervals (data not shown).
TABLE 4.
Impact of Distancing on Secondary SARS-CoV-2 Transmission
| Districtsa | Students | Student Primary Infections | Student Secondary Infections | Secondary/Primary Infection Ratiob | Relative Rate of Secondary Transmissionc | 95% CIsd | |
|---|---|---|---|---|---|---|---|
| Bus practice (children per seat) | |||||||
| 1 | 13 | 36 975 | 190 | 12 | 0.06 | — | — |
| 2 | 17 | 656 444 | 4388 | 210 | 0.05 | 0.76 | 0.19–2.96 |
| 3 | 17 | 205 996 | 1758 | 83 | 0.04 | 0.75 | 0.18–3.19 |
| Othere | 6 | 43 519 | 353 | 25 | 0.07 | 1.12 | 0.27–4.71 |
| Distancing, ft | |||||||
| 6 | 10 (9%) | 54 557 | 276 | 12 | 0.04 | — | — |
| 3 | 76 (67%) | 610 236 | 4140 | 207 | 0.05 | 1.15 | 0.31–4.24 |
| <3 | 27 (24%) | 278 141 | 2273 | 111 | 0.05 | 1.12 | 0.28–4.45 |
CI, confidence interval; —, reference group for Poisson regression.
This analysis excludes the composite North Carolina charter schools district because of varying practices among schools.
Calculated by the composite number of student within-school–acquired infections (secondary infections) divided by the number of student community-acquired infections (secondary infections) for districts in each category of bus practices or distancing.
Relative rate of secondary transmission for each primary infection, compared with the reference range (for bus analysis: 1 child per seat; for distancing analysis: 6 ft of distancing). Relative rates were calculated by quasi Poisson regression, with the number of primary student cases as the denominator.
Robust CIs were calculated to account for overdispersion.
“Other” category was assigned when districts could not give a policy practice for children per bus seat because of widely varying practices.
Discussion
This study is the largest known analysis of SARS-CoV-2 transmission in students and staff attending in-person education in the United States; these data represent a diverse cohort of schools in a variety of settings, including urban, suburban, and rural districts. With >1 million students and staff attending K–12 schools primarily operating under full in-person learning, we observed low rates of secondary transmission of SARS-CoV-2 in the setting of mitigation measures. These data are consistent with previous literature revealing that with mitigation measures in place, in-person schooling can be safe during the COVID-19 pandemic.1–3,15,16
Pertinent to policy in K–12 schools and consistent with a previous analysis and data from Europe,4,17 we found that in the masked environment, distancing either on buses or within classrooms was not associated with increased secondary transmission. Early requirements for 6-ft distancing effectively limited capacity for students in most classrooms, and full implementation of distancing requirements for student transportation was estimated to cost the US education system an additional $9.6 billion.1 The ability to reduce distancing between students without substantial increase in secondary transmission suggests that full return to in-person education is possible.
Our data also reveal that quarantine continues to be an issue for school districts; given the markedly low secondary attack rate, there is limited benefit to instituting quarantine in the mask-on-mask environment. After within-school contact with people infected with SARS-CoV-2, nearly 50 000 students missed school because of quarantine during the study period, representing an estimated >350 000 days of missed school and lost learning opportunities. Fortunately, the recent close contact exception for students in the K–12 classroom setting from the Centers for Disease Control and Prevention allows for continued in-person learning for students after masked exposures within K–12 schools.18 Primary cases will continue to enter schools as community rates remain substantial; however, given the low rates of secondary infection after masked exposure, elimination of quarantine in mask mitigated settings will allow for minimizing missed days of school.
As the data regarding the risk of SARS-CoV-2 spread in the K–12 environment continues to evolve, defining activities that are higher risk for secondary transmission can help inform where additional mitigation efforts should be implemented. Sports, particularly those that occur indoors, have been previously described as having a substantial amount of secondary transmission19–21; high school indoor sports accounted for 75% of secondary transmission in 13 districts in North Carolina during the winter 2021 surge.16 In this study, nearly half of middle and high school student secondary transmissions (including all high school secondary transmissions in Wisconsin) could be attributed to sports-associated exposure. Whether sports-associated secondary transmission occurred during practice, games, or team social events with lower adherence to masking is unclear. Ongoing participation of students in physical activity and organized sports is important to promote children’s health; however, focused strategies to mitigate the spread of SARS-CoV-2 are needed to protect children while participating in athletics. Data regarding the role of masking during sports to reduce secondary transmission are limited. Potential additional strategies to mitigate disease spread in higher-risk activities include vaccination and testing. Children playing school-sponsored sports who are >12 years old are currently eligible for vaccination against SARS-CoV-2. If vaccines are not required for sports participation, other mitigation measures should be considered; for example, masking and routine testing have been shown to allow ongoing sports participation with low transmission of SARS-CoV-2.22
Our study has limitations. First, the ability to perform adequate contact tracing might have differed between districts, thereby limiting accurate attribution of the infection source. However, when whole-genome sequencing has been compared with contact tracing in other studies to confirm the source of the infection, contact tracing has underestimated (rather than overestimated) within-school transmission.1 Regardless, our sensitivity analysis did not reveal a difference between secondary transmission among distancing or bus practices, even under the assumption of 10% misclassification of secondary cases. Second, we used policy data as reported by districts and did not measure adherence within schools of distancing, children per bus seat, or mask policies. Third, all districts included in our analysis implemented layered mitigation strategies, including a mask mandate for K–12 schools for the duration of the study period. As a result, we cannot estimate the impact that masking alone or any other individual mitigation factor had on secondary transmission rates. Furthermore, distancing may play a larger role in the unmasked environment. Continued study of the impact of different mitigation practices (masked and unmasked, varying distancing requirements) in the current academic year is needed. Fourth, the associations between distancing policies and secondary transmission could be confounded by other factors. Fifth, the sports subanalysis consisted of 68 of 100 LEAs plus the combined charter schools district in North Carolina. Those reporting for the sports subanalysis might have represented a biased sample of districts. Sixth, associations between distancing and bus policies could be confounded by other school system or community factors and, therefore, may not be strictly causal. Finally, the study occurred during a period of lower transmission in both North Carolina and Wisconsin and before the widespread emergence of the delta (B1.617.2) variant. Stricter adherence to mitigation strategies may play a larger role in the setting of higher community transmission or more infectious variants.
Conclusions
This study of nearly 1 million students and staff reveals that return to full in-person education was associated with low rates of secondary (within school) transmission. In the setting of universal masking, these low rates of secondary transmission were achieved even when distancing was reduced. School sports were associated with substantial secondary transmission and represent an area in which additional mitigation is warranted to prevent the spread of disease.
Supplementary Material
Acknowledgments
We acknowledge the school districts, administrators, and school nurses who worked diligently to collect and report these data in an effort to keep the children in their districts safe. We also acknowledge Helen Bristow, Vroselyn Benjamin, Brenda Franklin-Goode, and Wayne Pennachi for their efforts in ABCs program and data management and Erin Campbell, MS, who provided editorial review and submission.
Glossary
- ABCs
The ABC Science Collaborative
- COVID-19
coronavirus disease 2019
- K–12
kindergarten through 12th grade
- LEA
local education agency
- SARS-CoV-2
severe acute respiratory syndrome coronavirus 2
Footnotes
FUNDING: Funded in part by the Rapid Acceleration of Diagnostics Underserved Populations (U24 MD016258; National Institutes of Health agreements 1 OT2 HD107543-01, 1 OT2 HD107544-01, 1 OT2 HD107553-01, 1 OT2 HD107555-01, 1 OT2 HD107556-01, 1 OT2 HD107557-01, 1 OT2 HD107558-01, and 1 OT2 HD107559-01); the Trial Innovation Network, which is an innovative collaboration addressing critical roadblocks in clinical research and accelerating the translation of novel interventions into life-saving therapies; and the Eunice Kennedy Shriver National Institute of Child Health and Human Development contract (HHSN275201000003I) for the Pediatric Trials Network (principal investigator, Daniel Benjamin). The views and conclusions contained in this document are those of the authors and should not be interpreted as representing the official policies, either expressed or implied, of the National Institutes of Health. Funded by the National Institutes of Health (NIH).
CONFLICT OF INTEREST DISCLOSURES: Dr Boutzoukas receives salary support through the US Government Eunice Kennedy Shriver National Institute of Child Health and Human Development T32 training grant (1T32HD094671). Dr Zimmerman reports funding from the National Institutes of Health and US Food and Drug Administration. Dr Benjamin reports consultancy for Allergan, Melinta Therapeutics, and Sun Pharma Advanced Research Company. Dr Kalu reports funding from the Centers for Disease Control and Prevention’s Prevention Epicenters Program and consultancy for Infection Prevention Education Consultant (IP EC) Experts and Wayfair. Dr Smith reports being a site coinvestigator for Pfizer adult and pediatric vaccine trials. Dr Brookhart serves on scientific advisory committees for AbbVie, Amgen, Atara Biotherapeutics, Brigham and Women’s Hospital, Gilead, and Vertex; he receives consulting fees for and owns equity in NoviSci and TargetRWE; the other authors have indicated they have no financial relationships relevant to this article to disclose.
Drs Boutzoukas and Butteris conceptualized and designed the study, designed the data collection instruments, collected data, conducted the initial analyses, drafted the initial manuscript, and reviewed and revised the manuscript; Drs McGann, Kalu, and DeMuri designed the data collection instruments, collected data, and reviewed and revised the manuscript; Drs Smith and Brookhart and Mr Koval reviewed and revised the manuscript; Drs Zimmerman and Benjamin designed the data collection instruments, collected data, reviewed and revised the manuscript, conceptualized and designed the study, coordinated and supervised data collection, and critically reviewed the manuscript for important intellectual content; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
References
- 1. Hershow RB, Wu K, Lewis NM, et al. Low SARS-CoV-2 transmission in elementary schools - Salt Lake County, Utah, December 3, 2020-January 31, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(12):442–448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zimmerman KO, Akinboyo IC, Brookhart MA, et al. ; ABC Science Collaborative . Incidence and secondary transmission of SARS-CoV-2 infections in schools. Pediatrics. 2021;147(4):e2020048090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Falk A, Benda A, Falk P, Steffen S, Wallace Z, Høeg TB. COVID-19 cases and transmission in 17 K-12 schools - Wood County, Wisconsin, August 31-November 29, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(4):136–140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. van den Berg P, Schechter-Perkins EM, Jack RS, et al. Effectiveness of 3 versus 6 ft of physical distancing for controlling spread of coronavirus disease 2019 among primary and secondary students and staff: a retrospective, statewide cohort study. Clin Infect Dis. 2021;73(10):1871–1878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. General Assembly of North Carolina, Session 2021 . Session Law 2021-4, Senate Bill 220. Available at: https://www.ncleg.gov/Sessions/2021/Bills/Senate/PDF/S220v4.pdf. Accessed August 20, 2021
- 6. The ABC Science Collaborative . About. Available at: https://abcscience collaborative.org/about/. Accessed August 20, 2021
- 7. North Carolina Department of Health and Human Services . StrongSchoolsNC public health toolkit (K-12): interim guidance. 2020. Available at: https://covid19.ncdhhs.gov/media/164/open. Accessed August 20, 2021
- 8. Public Health Madison & Dane County . Order of public health Madison & Dane County, emergency order #9. 2020. Available at: https://publichealthmdc.com/documents/2020-08-21_Order_9.pdf. Accessed August 24, 2021
- 9. Public Health Madison & Dane County . Order of public health Madison & Dane County, emergency order #11. 2020. Available at: https://publichealthmdc.com/documents/2020-12-15_Order_11.pdf. Accessed August 24, 2021
- 10. Public Schools of North Carolina . Pupils in membership by race and sex, school year 2020-21. Available at: http://apps.schools.nc.gov/ords/f?p=145:15:::NO:::. Accessed August 20, 2021
- 11. Public Schools of North Carolina . Charter and regional school membership by race and sex, school year 2020-21. Available at: http://apps.schools.nc.gov/ords/f?p=145:73:::NO:::. Accessed August 24, 2021
- 12. North Carolina Department of Public Instruction . Student accounting data. Available at: https://www.dpi.nc.gov/districts-schools/district-operations/financial-and-business-services/demographics-and-finances/student-accounting-data. Accessed August 24, 2021
- 13. WISEdash Public Portal . Enrollment. Available at: https://wisedash.dpi.wi.gov/Dashboard/dashboard/18110. Accessed August 24, 2021
- 14. Ihaka R, Gentleman R. R: a language for data analysis and graphics. J Comput Graph Stat. 1996;5(3):299–314 [Google Scholar]
- 15. Dawson P, Worrell MC, Malone S, et al. ; CDC COVID-19 Surge Laboratory Group . Pilot investigation of SARS-CoV-2 secondary transmission in kindergarten through grade 12 schools implementing mitigation strategies - St. Louis County and City of Springfield, Missouri, December 2020. MMWR Morb Mortal Wkly Rep. 2021;70(12): 449–455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zimmerman KO, Brookhart MA, Kalu IC, et al. ; ABC Science Collaborative . Community SARS-CoV-2 surge and within-school transmission. Pediatrics. 2021;148(4):e2021052686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ismail SA, Saliba V, Lopez Bernal J, Ramsay ME, Ladhani SN. SARS-CoV-2 infection and transmission in educational settings: a prospective, cross-sectional analysis of infection clusters and outbreaks in England. Lancet Infect Dis. 2021;21(3):344–353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Centers for Disease Control and Prevention . Guidance for COVID-19 prevention in K-12 schools. Available at: https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/k-12- guidance.html. Accessed August 24, 2021
- 19. Atherstone C, Siegel M, Schmitt-Matzen E, et al. SARS-CoV-2 transmission associated with high school wrestling tournaments - Florida, December 2020-January 2021. MMWR Morb Mortal Wkly Rep. 2021;70(4):141–143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gettings JR, Gold JAW, Kimball A, et al. SARS-CoV-2 transmission in a Georgia school district - United States, December 2020-January 2021 [published online ahead of print April 17, 2021]. Clin Infect Dis. doi:10.1093/cid/ciab332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Doyle T, Kendrick K, Troelstrup T, et al. COVID-19 in primary and secondary school settings during the first semester of school reopening - Florida, August-December 2020. MMWR Morb Mortal Wkly Rep. 2021;70(12):437–441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lanier WA, Babitz KD, Collingwood A, et al. COVID-19 testing to sustain in- person instruction and extracurricular activities in high schools - Utah, November 2020-March 2021. MMWR Morb Mortal Wkly Rep. 2021;70(21):785–791 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.