Abstract
OBJECTIVES
Masking is an essential coronavirus 2019 mitigation tool assisting in the safe return of kindergarten through 12th grade children and staff to in-person instruction; however, masking adherence, compliance evaluation methods, and potential consequences of surveillance are currently unknown. We describe 2 school districts’ approaches to promote in-school masking and the consequent impact on severe acute respiratory syndrome coronavirus 2 secondary transmission.
METHODS
Two North Carolina school districts developed surveillance programs with daily versus weekly interventions to monitor in-school masking adherence. Safety teams recorded the proportion of students and staff appropriately wearing masks and provided real-time education after observation of improper masking. Primary infections, within-school transmission, and county-level severe acute respiratory syndrome coronavirus 2 infection rates were assessed.
RESULTS
Proper mask use was high in both intervention groups and districts. There were variations by grade level, with lower rates in elementary schools, and proper adherence being higher in the weekly surveillance group. Rates of secondary transmission were low in both districts with surveillance programs, regardless of intervention frequency.
CONCLUSIONS
Masking surveillance interventions are effective at ensuring appropriate masking at all school levels. Creating a culture of safety within schools led by local leadership is important and a feasible opportunity for school districts with return to in-person school. In our study of schools with high masking adherence, secondary transmission was low.
What’s Known on This Subject:
Masking is an effective method to limit severe acute respiratory syndrome coronavirus 2 transmission in schools. Public health and child health organizations recommend universal masking in schools, given increasing rates of highly transmissible variants and the fact that most children are not yet eligible for vaccination.
What This Study Adds:
Masking surveillance interventions are effective at ensuring highly consistent masking at all grade levels. Creating a culture of safety within schools may be feasible through adherence evaluations. Secondary transmission rates are low when school communities have high masking adherence.
During the coronavirus 2019 (COVID-19) pandemic, masking has been an effective strategy for controlling transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).1 Similarly, masking has been an essential component for the safe return of kindergarten through 12th grade (K–12) schoolchildren and staff to in-person classrooms, particularly because children younger than 12 years of age are currently ineligible for vaccination.2–5 Masking is effective, even in settings of poor ventilation, emerging viral variants, and under circumstances of reduced physical distancing (<6 ft) between students and/or staff.2,6–8 Nevertheless, masking remains one of the most controversial topics both within and outside of the K–12 school community.
In May 2021, the Centers for Disease Control and Prevention (CDC) revised its guidance to only recommend mask use in some settings according to vaccination status. In early July 2021, the CDC suggested that only those who were unvaccinated should mask in the school setting.9 This guidance prompted a “return to normal” with subsequent lifting of many statewide masking mandates, physical distancing requirements, and capacity limits for indoor activities. Recently, spread of the highly transmissible SARS-CoV-2 variant, B.1.617.2 (ie, Delta variant), has led to increased COVID-19 cases worldwide, particularly among those who are unvaccinated. The CDC issued revised guidance in late July 2021 that aligned with the American Academy of Pediatrics, recommending masking for all individuals in K–12 schools, regardless of vaccination status, given the rapid spread of the Delta variant and lack of vaccine eligibility for those <12 years of age. The discrepancies in masking recommendations from public health organizations has created even more confusion for those who are working to maintain a safe environment for return to in-person school during the upcoming school semester, which happens to coincide with respiratory illness season. Additionally, school staff and many parents of children <12 years remain adamant that masking in schools must occur for them to feel that school buildings are safe, yet schools are struggling to contend with increasing opposition to masking in their surrounding communities.
There is substantial evidence to support the use of masking as an effective method to limit SARS-CoV-2 transmission in schools.2,4,5 However, student and staff adherence to masking, optimal methods to evaluate and encourage masking on the basis of surveillance, and potential consequences of masking surveillance within school buildings are currently unknown, particularly given the rapidly changing public health guidance and increasing opposition within local communities. In this article, we describe 2 school districts’ approaches to evaluate and encourage masking in schools during the fourth quarter of the 2020–2021 school year. We also characterize the relationship between masking evaluation method and adherence.
Methods
Target Population
The ABC Science Collaborative (ABCs) worked with 2 large (>15 000 students) traditional public school districts in North Carolina to design and evaluate masking interventions. District 1 initially returned prekindergarten students to in-person classrooms in September 2020, followed by other elementary school students and a small number of high school students. All phase-in activities for these students were completed by mid-November 2020, and ∼20 000 students returned to in-person class 5 days a week. Grades 6–12 were subsequently phased in by using a hybrid model that combined virtual learning and in-person school starting in late February 2021 and transitioned to in-person class 5 days per week by mid-April 2021.
District 2 opened school buildings in mid-August 2020 for in-person learning, 5 days per week for prekindergarten to fifth grade and 2 days per week for sixth to 12th grade. All students returned to in-person classes 5 days a week in early April 2021. Both schools followed guidance outlined in the StrongSchoolsNC Public Health Toolkit (K–12).10 Schools were encouraged to maintain a minimum of 3 ft of distance between K–12 students, whenever possible. Neither district 1 nor district 2 had major changes to their ventilation systems, and students and staff did not undergo routine surveillance testing for SARS-CoV-2.
Interventions
From April 5, 2021, to May 21, 2021, each district implemented their own surveillance program to monitor masking adherence within school buildings (Table 1). The CDC’s guidance change to masking based on vaccination status occurred on May 13, 2021, which was at the end of week 6 of the 7-week study period.
TABLE 1.
Masking Surveillance Program Descriptions
| District 1 | District 2 | |
|---|---|---|
| Leadership | Local teachers’ organization and local school leadership | School district administration |
| School levels | Elementary schools (9) | Elementary (17), middle (9), and high schools (9) |
| Education | Teachers’ organization educating school leaders, safety teams, video on proper masking | ABCs provided education on proper masking to district administrators |
| Intervention | Safety team member reminding individuals of correct masking in real time | Administrator reminding individuals of correct masking in real time |
| Monitoring frequency | Daily (4 schools), weekly (2 schools), none/control (3 schools) | Daily in 20% of students and staff at all schools in district |
| Weeks of intervention | Weeks 1–6 (April 5, 2021–May 14, 2021) | Weeks 3–7 (April 19, 2021–May 21, 2021) |
In district 1, the mask adherence surveillance plan was developed by the local teachers’ organization that included staff (ie, teachers, school administrators) from each school in the district. On return to in-person education, local school leadership (ie, teachers, administrators, and staff) served as a safety team to encourage and monitor appropriate safety measures, including masking. This grassroots effort was led and designed by school leadership to best fit the needs of their school, staff, and students. The teachers’ organization collaborated with ABCs to develop a video on the specific criteria for proper mask use (cloth or medical mask worn over the nose, mouth, and chin) and designed the 6-week pilot intervention to monitor masking adherence.
Nine of eleven elementary schools in district 1 participated in the pilot intervention. District 1 schools conducted surveillance during weeks 1–6 of the study period. Safety team leaders at 4 school buildings performed daily walkthroughs to document the proportion of students and staff properly wearing masks. When students and staff were identified without masks or with improper mask use (eg, not fully covering the nose, mouth, and chin), the safety team member gently reminded these individuals of the importance of correct masking and asked for the mask to be worn appropriately.11 At 2 schools, walkthroughs and mask evaluations occurred once per week. At the end of each week, the safety teams reported their findings to school administrators; if <90% masking adherence within a school building was documented over the course of a week, then a remediation plan was developed.
In collaboration with ABCs, district 2 administrators developed the masking adherence pilot intervention in elementary, middle, and high schools in response to rising rates of within-school transmission. Similar to district 1, this was a grassroots effort tailored to the school district with the input of school administrators. District 2 schools conducted masking surveillance during weeks 3–7 of the study period. During the 5-week study period, district administrators evaluated daily mask use in a randomly selected 20% of students and staff at each school. Administrators recorded the portion of evaluated students and staff that were appropriately wearing masks during walkthroughs. If improper masking was observed, then administrators provided a real-time, verbal reminder to these students and staff of the importance of proper masking and asked for the mask to be adjusted accordingly. Notably, although researchers in previous studies have used more standardized and structured observational methods, the school districts in our study designed feasible, observational methods tailored to the needs and capacities of their specific district and school population that aligned with CDC guidance.12–14
Additional Data Sources
To characterize county-level COVID-19 rates during the study period in districts 1 and 2, in-school attendance, and school demographics, we used state-level data from 3 publicly available online databases: the John Hopkins University Coronavirus Resource Center,15 the North Carolina Department of Public Instruction’s Principal’s Monthly Report,16 and the Public Schools of North Carolina Statistical Profile.17 Primary SARS-CoV-2 infections and within-school transmission were obtained from a concurrent study performing weekly surveillance of these metrics by school in 100 public school districts in North Carolina over a 12-week period (ABCs of North Carolina’s Plan A, Duke University Institutional Review Board, Pro00108073).
Outcome Measures
The primary study outcome was the proportion of observed students and staff with appropriate mask use. The secondary outcome was secondary transmission rates within schools participating in the masking project.
Statistical Analysis
We used SAS v9.4 (SAS Institute, Inc, Cary, NC) for all statistical analyses. We used descriptive statistics to analyze appropriate mask use overall, by week, by district, and by study cohort (daily evaluation by staff, daily evaluation by administrators, weekly evaluation by staff). We used generalized estimating equations with an independent correlation structure to estimate predictors of masking adherence.
Institutional Review Board Approval
This work was declared as exempt research under the ABCs research program by the Duke University Institutional Review Board (Pro00108127).
Results
Study Population
In District 1, the 6 elementary schools with masking surveillance interventions enrolled a total of ∼2400 students. District 2 included 17 elementary schools, 9 middle schools, and 9 high schools, with a total enrollment of ∼20 000 students (Table 2). The district 1 schools enrolled fewer White students than district 2 schools (22% vs 63% respectively; Table 2). The 2 school districts had similar overall percentage of students on-site for in-person instruction (78.2% district 1 vs 81% district 2; Table 2); however, district 2 had variable percentages of learners on-site, depending on school and grade level (eg, (80% to 94% in middle and 46% to 100% in high school; Table 2).
TABLE 2.
School Demographics
| Total Enrolled, n (%) | Male, n (%) | White, n (%) | On-Site, n (%) | |
|---|---|---|---|---|
| All schools | 22 325 | 11 464 (51) | 13 015 (58) | 17 706/21 983 (81) |
| District 1 | 2405 | 1 238 (52) | 535 (22) | 1880/2405 (78) |
| School 1-1 | 419 | 208 (50) | 8 (2) | 323/419 (77) |
| School 1-2 | 159 | 79 (50) | 4 (3) | 111/159 (70) |
| School 1-3 | 448 | 226 (50) | 22 (5) | 345/448 (77) |
| School 1-4 | 465 | 244 (53) | 20 (4) | 353/465 (76) |
| School 1-5 | 651 | 340 (52) | 477 (73) | 514/651 (79) |
| School 1-6 | 263 | 141 (54) | 4 (2) | 234/263 (89) |
| District 2 | 19 920 | 10 226 (51) | 12 480 (63) | 15 826/19 578 (81) |
| Elementary schools | 8107 | 4229 (52) | 4906 (61) | 7470/8375 (89) |
| School 2.1-1 | 365 | 197 (54) | 48 (13) | 331/374 (89) |
| School 2.1-2 | 713 | 381 (53) | 221 (31) | 579/707 (82) |
| School 2.1-3 | 322 | 167 (52) | 162 (50) | 310/325 (95) |
| School 2.1-4 | 332 | 168 (51) | 231 (70) | 335/352 (95) |
| School 2.1-5 | 514 | 278 (54) | 163 (32) | 488/547 (89) |
| School 2.1-6 | 651 | 334 (51) | 440 (68) | 608/687 (89) |
| School 2.1-7 | 243 | 123 (51) | 188 (77) | 222/237 (94) |
| School 2.1-8 | 228 | 113 (50) | 175 (77) | 188/234 (80) |
| School 2.1-9 | 608 | 310 (51) | 417 (69) | 536/639 (84) |
| School 2.1-10 | 487 | 229 (47) | 186 (38) | 436/480 (91) |
| School 2.1-11 | 524 | 285 (54) | 387 (74) | 513/569 (90) |
| School 2.1-12 | 469 | 261 (56) | 316 (67) | 463/492 (94) |
| School 2.1-13 | 641 | 338 (53) | 526 (82) | 628/681 (92) |
| School 2.1-14 | 622 | 329 (53) | 383 (62) | 570/625 (91) |
| Middle schools | 4756 | 2429 (51) | 2925 (62) | 4201/4781 (88) |
| School 2.1-15 | 352 | 159 (45) | 317 (90) | 338/361 (94) |
| School 2.1-16 | 395 | 209 (53) | 255 (65) | 339/388 (87) |
| School 2.1-17 | 641 | 348 (54) | 491 (77) | 586/677 (87) |
| School 2.2-1 | 489 | 209 (43) | 317 (65) | 403/465 (87) |
| School 2.2-2 | 590 | 303 (51) | 440 (75) | 527/571 (92) |
| School 2.2-3 | 379 | 201 (53) | 241 (64) | 341/385 (89) |
| School 2.2-4 | 632 | 325 (51) | 465 (74) | 573/663 (86) |
| School 2.2-5 | 467 | 236 (51) | 92 (20) | 454/490 (93) |
| School 2.2-6 | 545 | 253 (46) | 412 (76) | 429/534 (80) |
| High schools | 7057 | 3568 (51) | 4649 (66) | 4155/6422 (65) |
| School 2.2-7 | 621 | 337 (54) | 483 (78) | 548/626 (88) |
| School 2.2-8 | 620 | 340 (55) | 341 (55) | 565/620 (91) |
| School 2.2-9 | 413 | 225 (55) | 134 (32) | 361/427 (85) |
| School 2.3-1 | 1980 | 1052 (53) | 1563 (79) | 900/1970 (46) |
| School 2.3-2 | 1600 | 812 (51) | 1143 (71) | 1061/1519 (70) |
| School 2.3-3 | 246 | 102 (42) | 175 (71) | 138/138 (100) |
| School 2.3-4 | 854 | 416 (49) | 193 (23) | 601/828 (73) |
| School 2.3-5 | 923 | 493 (53) | 635 (69) | 597/845 (71) |
| School 2.3-6 | 230 | 119 (52) | 140 (61) | 65/65 (100) |
| School 2.3-7 | 133 | 61 (46) | 119 (90) | 128/128 (100) |
| School 2.3-8 | 817 | 427 (52) | 525 (64) | 534/798 (67) |
| School 2.3-9 | 274 | 86 (31) | 156 (57) | 131/131 (100) |
Total percentages may not add to 100% because of rounding.
Primary Cases and Secondary Transmission
Within the 2 school districts, 127 primary SARS-CoV-2 infections (ie, community-acquired) were documented by diagnostic testing during the study period; however, there were only 14 cases of secondary (ie, within school) transmission in the 2 districts during the study period (Table 3). There were 10 primary infections (0.42%) and only 1 secondary infection in district 1–participating schools. District 2 had 117 documented primary infections (0.58%) across all participating schools. There were 13 secondary infections in district 2 in four different schools, all of which occurred during weeks 3 to 7; 11 occurred in middle schools and 2 occurred in 1 high school. During the study period, county-level rates of infection remained low in both districts (county 1, 0.06% to 0.18%; county 2, 0.07% to 0.14%; Table 2).
TABLE 3.
Within-School and District-Level Infections During Study Period
| Week 1, n (%) | Week 2, n (%) | Week 3, n (%) | Week 4, n (%) | Week 5, n (%) | Week 6, n (%) | Week 7, n (%) | |
|---|---|---|---|---|---|---|---|
| All schools | |||||||
| Primary infections | 3/17 706 (0.02) | 26/17 706 (0.15) | 26/17 706 (0.15) | 17/17 706 (0.10) | 13/17 706 (0.07) | 28/17 706 (0.16) | 14/17 706 (0.08) |
| Secondary infections | 0 | 0 | 2/17 706 (0.01) | 5/17 706 (0.03) | 0 | 5/17 706 (0.03) | 2/17 706 (0.01) |
| District 1 | |||||||
| County infection rate | 927/537 174 (0.17) | 980/537 174 (0.18) | 855/537 174 (0.16) | 679/537 174 (0.13) | 536/537 174 (0.10) | 592/537 174 (0.11) | 327/537 174 (0.06) |
| Elementary schools | |||||||
| Primary infections | 0 | 0 | 4/1880 (0.21) | 1/1880 (0.05) | 1/1880 (0.05) | 3/1880 (0.16) | 1/1880 (0.05) |
| Secondary infections | 0 | 0 | 0 | 0 | 0 | 1/1880 (0.05) | 0 |
| District 2 | |||||||
| County infection rate | 198/181 806 (0.11) | 251/181 806 (0.14) | 247/181 806 (0.14) | 222/181 806 (0.12) | 205/181 806 (0.11) | 208/181 806 (0.11) | 131/181 806 (0.07) |
| Primary infections | 3/15 826 (0.02) | 26/15 826 (0.16) | 22/15 826 (0.14) | 16/15 826 (0.10) | 12/15 826 (0.08) | 25/15 826 (0.16) | 13/15 826 (0.08) |
| Secondary infections | 0 | 0 | 2/15 826 (0.01) | 5/15 826 (0.03) | 0 | 4/15 826 (0.03) | 2/15 826 (0.01) |
| Elementary schools | |||||||
| Primary infections | 1/7470 (0.01) | 6/7470 (0.08) | 9/7470 (0.12) | 7/7470 (0.09) | 5/7470 (0.07) | 7/7 470 (0.09) | 3/7470 (0.04) |
| Secondary infections | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Middle schools | |||||||
| Primary infections | 1/4201 (0.02) | 10/4201 (0.24) | 5/4201 (0.12) | ¼201 (0.02) | 5/4201 (0.12) | 8/4201 (0.19) | 5/4201 (0.12) |
| Secondary infections | 0 | 0 | 2/4201 (0.05) | 5/4201 (0.12) | 0 | 4/4201 (0.10) | 0 |
| High schools | |||||||
| Primary infections | 1/4155 (0.02) | 10/4155 (0.24) | 8/4155 (0.19) | 8/4155 (0.19) | 2/4155 (0.05) | 10/4155 (0.24) | 5/4155 (0.12) |
| Secondary infections | 0 | 0 | 0 | 0 | 0 | 0 | 2/4155 (0.05) |
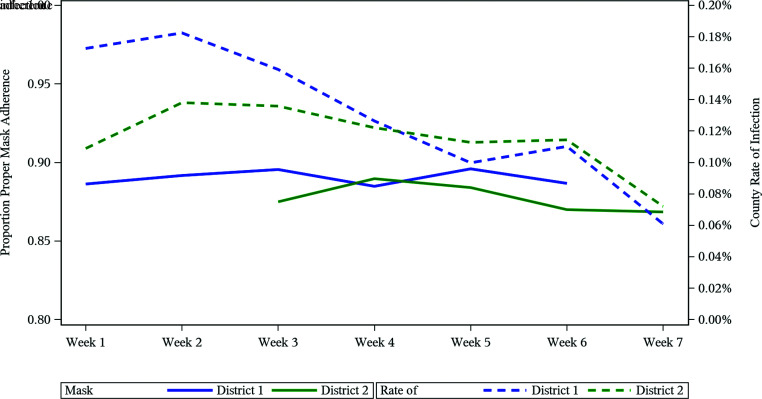
Masking Adherence Over Time by District, School Level, and Surveillance Program
There was high masking adherence (>80%) in both school districts at all school levels (elementary, middle, and high school). Proper mask adherence remained consistently high over the study period, despite changes in CDC guidance and county rates of infection (Fig 1). The percentage of students and staff properly masked at all elementary schools ranged from 89% in week 1% to 82% in week 7 and were similar in district 1 (88% to 90%) and district 2 (81% to 85%); Table 4. In district 2, the percentage of proper masking adherence was 81% to 95%, and it was similar in middle and high schools for students, staff, and overall (Table 4).
FIGURE 1.
Proper masking proportion. Proper masking proportion and county rates of infections over time by district.
TABLE 4.
Proportion of Students and Staff Properly Masked During Study Period
| Week 1 | Week 2 | Week 3 | Week 4 | Week 5 | Week 6 | Week 7 | |
|---|---|---|---|---|---|---|---|
| By school level | |||||||
| All districts | |||||||
| Elementary schools | 0.89 | 0.89 | 0.84 | 0.85 | 0.86 | 0.84 | 0.82 |
| Middle schools | N/A | N/A | 0.92 | 0.93 | 0.92 | 0.90 | 0.90 |
| High schools | N/A | N/A | 0.92 | 0.95 | 0.91 | 0.91 | 0.93 |
| District 1 | |||||||
| Elementary schools | 0.89 | 0.89 | 0.90 | 0.88 | 0.90 | 0.89 | N/A |
| District 2 | |||||||
| Overall | |||||||
| Elementary schools | N/A | N/A | 0.81 | 0.84 | 0.85 | 0.83 | 0.82 |
| Middle schools | N/A | N/A | 0.92 | 0.93 | 0.92 | 0.90 | 0.90 |
| High schools | N/A | N/A | 0.92 | 0.95 | 0.91 | 0.91 | 0.93 |
| Students | |||||||
| Elementary schools | N/A | N/A | 0.81 | 0.83 | 0.85 | 0.82 | 0.82 |
| Middle schools | N/A | N/A | 0.92 | 0.93 | 0.92 | 0.90 | 0.89 |
| High schools | N/A | N/A | 0.91 | 0.95 | 0.91 | 0.90 | 0.93 |
| Staff | |||||||
| Elementary schools | N/A | N/A | 0.88 | 0.90 | 0.92 | 0.91 | 0.88 |
| Middle schools | N/A | N/A | 0.93 | 0.96 | 0.94 | 0.96 | 0.96 |
| High schools | N/A | N/A | 0.98 | 0.98 | 0.95 | 0.96 | 0.95 |
| By evaluation type | |||||||
| District 1 | |||||||
| Daily | 0.88 | 0.88 | 0.88 | 0.88 | 0.89 | 0.88 | N/A |
| Weekly | 0.92 | 0.94 | 0.95 | 0.92 | 0.92 | 0.94 | N/A |
N/A, not applicable.
In district 1, the weekly surveillance cohort had a higher proportion of students and staff with appropriate masking than the daily surveillance cohort (1.82 [95% confidence interval: 1.22–2.72]; Table 5). Higher grade level was a predictor of masking adherence (Table 5).
TABLE 5.
Predictors of Masking Adherence
| Predictor | Estimate (95% CI) |
|---|---|
| All districts | |
| CDC guidance change | 0.93 (0.82–1.05) |
| County infection rate | 1.09 (0.92–1.29) |
| District 1 | |
| County infection rate | 1.06 (0.89–1.25) |
| Weekly evaluation type (versus daily) | 1.82 (1.22–2.72) |
| District 2 | |
| CDC guidance change | 0.93 (0.82–1.05) |
| County infection rate | 1.08 (0.86–1.36) |
| Middle school (versus elementary school) | 1.87 (1.15–3.07) |
| High school (versus elementary school) | 2.21 (1.18–4.13) |
| School secondary transmission rate | 0.72 (0.40–1.29) |
CI, confidence interval.
Discussion
With this study, we assessed the effect of masking surveillance interventions on appropriate mask adherence in school settings and evaluated the relationship between masking adherence and secondary transmission of SARS-CoV-2 amid changing public health guidance and increasing community opposition to masking. We found that masking adherence was high in both daily and weekly surveillance groups (88% to 95%) and across varying grade levels in both districts (82% to 95%). There were variations by grade level, with lower rates of proper masking in elementary schools, and higher proper masking adherence in the weekly surveillance group, which may reflect that our study captured variability in multiple, different cohorts. Rates of secondary transmission were low in daily and weekly masking intervention cohorts and in both districts. Our findings also suggest that elementary school students should have close surveillance of masking adherence, particularly with the spread of variants and lack of vaccine availability in this age group. Lessons learned from this evaluation may be useful going forward as school districts plan for in-person school attendance in the middle of an ever-changing pandemic.
The effects of surveillance and real-time education on proper mask adherence have not previously been studied. Additionally, the efficacy of a grassroots intervention such as ours in mitigating in-school spread has not previously been measured. Researchers in an observational study in Georgia elementary schools who assessed the period of time that an entire class was appropriately masked found that younger, elementary-aged students had lower adherence but could reliably wear masks during the school day.18 We found that middle and high school students had a higher percentage of proper masking when compared with elementary school students; however, adherence reached 90% in some elementary schools, and surveillance interventions may increase adherence. The groups studied had high adherence to masking; therefore, we did not see changes in adherence reflected over time. The sampling structure of our study, particularly in district 2, may not wholly reflect subtle improvements in masking adherence because it is possible that the same group of students were not re-evaluated given random sampling. Nevertheless, in some settings, just-in-time education may ensure appropriate mask use and, as a result, prevent in-school COVID-19 spread. Our study continues to support existing data on low secondary transmission rates in schools that implemented various mitigation strategies.4
CDC guidance regarding masking in communities and within schools is ever-changing on the basis of the prevalence of COVID-19 transmission. During this study, although CDC masking guidance in community settings changed, masking adherence within these schools did not. County-level transmission rates also had no impact on in-school mask adherence. These data suggest that staff members were adept at maintaining consistent and high levels of mask adherence, even as guidance and community infection rates fluctuated.
Because masking remains a divisive issue in the United States, regular internal surveillance may set a tone of unity and empowerment that improves the overall culture of safety for staff and students. In district 1, weekly evaluations had higher levels of masking adherence when compared with daily evaluations; because observations only occurred at 1 weekly time point, students and staff may have been more cognizant of their masking and anticipated evaluation. Conversely, those in daily surveillance cohorts had many more opportunities for observation and may have been identified during moments of masking fatigue. Additionally, perhaps daily evaluations captured more variability in adherence in different cohorts, as opposed to weekly adherence, which may reflect a snapshot of a singular cohort given the random sampling in the weekly intervention group.
As schools return to in-person learning, staff are understandably concerned about school safety.19 Researchers have suggested that improper masking can increase teachers’ risk of anxiety.20 These grassroots interventions were developed to allow teachers and school administration to be empowered and play a role in creating a safe learning environment. Work done to create a culture of safety and trust in the school setting may have contributed to excellent masking. Employees who perceived their jobs as safe have been shown to comply with safety behaviors at work more frequently.21 There was no clear difference in adherence between evaluations conducted by internal school staff (ie, district 1) and administrators (ie, district 2). Therefore, tasking either school leadership and/or administration to lead internal surveillance of appropriate adherence to safety measures may be effective in ensuring appropriate mask use. Researchers in other studies have demonstrated that work safety climate is influenced by leadership and co-worker commitment to safety; such a climate is associated with improved employee satisfaction and stronger employee–employer relationships.22,23 Schools need to create an environment where staff feel comfortable. Further study is needed to evaluate the impact of school-led masking adherence and safety initiatives on teacher anxiety and co-worker perceptions of safety.
Our study had several limitations. First, data on masking adherence were collected by school leadership. There are limitations to self-reporting (including bias), potential reliability issues related to perception of appropriate mask adherence, and missing data. Second, school-level demographics were obtained from state databases that may have errors or missing data. Third, school participation in the ABCs was voluntary, and data submission may have resulted in selection bias of schools that enforce mitigation strategies and/or greater data transparency. We acknowledge that we have no comparison data regarding masking adherence in nonintervention schools. Our sampling strategy may not have allowed for a complete assessment of the impact of real-time education; however, these interventions were not initially designed with that in mind and rather focused on staff empowerment. Finally, secondary transmission rates were adjudicated by local health department staff in each district with varying resource capabilities, and exposure testing was not required for return to school in North Carolina, potentially leading to underreporting of secondary transmission. Nonetheless, rates observed in this study were similar to those reported outside of North Carolina when testing has been conducted.2–4 Notably, community transmission was relatively low during this short study period and may increase in fall and winter 2021 because of surges of variant strains and loosening of masking requirements in communities. Secondary transmission could increase in the school setting if school masking guidelines are changed.
Conclusions
Masking surveillance interventions are effective at ensuring highly consistent masking at all grade levels. Creating a culture of safety within schools through surveillance led by local leadership can assist in decreasing spread of in-school infections. With this study, we also add to the previously noted evidence that secondary transmission rates are low when school communities have high masking adherence. Masking adherence is more important than ever as more transmissible variants circulate and rates of COVID-19 infections in unvaccinated children increase. Our findings contribute to keeping school settings safe as districts transition to in-person learning during an ever-changing pandemic with fluctuating masking guidelines for community and school settings.
Acknowledgment
We thank Erin Campbell, MS, for providing editorial review and submission.
Glossary
- ABCs
ABC Science Collaborative
- CDC
Centers for Disease Control and Prevention
- COVID-19
coronavirus 2019
- K–12
kindergarten through 12th grade
- SARS-CoV-2
severe acute respiratory syndrome coronavirus 2
Footnotes
Dr Kalu conceptualized and designed the study, drafted the initial manuscript, and reviewed and revised the manuscript; Mr Warren, Mr Garcés, and Ms Pendleton conceptualized and designed the study, drafted the initial manuscript, designed the data collection instruments, collected data, conducted the initial analyses, and reviewed and revised the manuscript; Dr Brookhart conducted the initial analyses and reviewed and revised the manuscript; Ms Edwards designed the data collection instruments, collected data, conducted the initial analyses, and reviewed and revised the manuscript; Drs Benjamin, Boutzoukas, Corneli, Jackman, Weber, Maradiaga Panayotti, and Ms Blakemore reviewed and revised the manuscript; Drs Moorthy, Mann, and Zimmerman, conceptualized and designed the study, drafted the initial manuscript, coordinated and supervised data collection, designed the data collection instruments, collected data, conducted the initial analyses, and critically reviewed the manuscript for important intellectual content; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FUNDING: This research was funded in part by the Rapid Acceleration of Diagnostics Underserved Populations (U24 MD016258; National Institutes of Health [NIH] Agreement No.’s 1 OT2 HD107543-01, 1 OT2 HD107544-01, 1 OT2 HD107553-01, 1 OT2 HD107555-01, 1 OT2 HD107556-01, 1 OT2 HD107557-01, 1 OT2 HD107558-01, 1 OT2 HD107559-01); the Trial Innovation Network, which is an innovative collaboration addressing critical roadblocks in clinical research and accelerating the translation of novel interventions into life-saving therapies; and the National Institute of Child Health and Human Development contract (HHSN275201000003I) for the Pediatric Trials Network (principal investigator, Daniel Benjamin). Dr Moorthy receives salary support through the US government National Institute of Child Health and Human Development T32 training grant (1T32HD094671). Dr Boutzoukas receives salary support through the US government National Institute of Child Health and Human Development T32 training grant (1T32HD094671). The views and conclusions contained in this document are those of the authors and should not be interpreted as representing the official policies, either expressed or implied, of the NIH. Funded by the National Institutes of Health (NIH).
CONFLICT OF INTEREST DISCLOSURES: Dr Weber reports consulting for Pfizer, Merck, Sanofi, PDI, UVinnovators, Gemitec. Dr Kalu reports CDC Epicenter; consulting for IPEC Experts, Wayfair. Dr Benjamin reports consultancy for Allergan, Melinta Therapeutics, Sun Pharma Advanced Research Co. Dr Zimmerman reports funding from the National Institutes of Health and US Food and Drug Administration. Dr Brookhart serves on scientific advisory committees for American Academy of Allergy, Asthma & Immunology, AbbVie, Amgen, Atara Biotherapeutics, Brigham and Women’s Hospital, Gilead, US Renal Data System, and Vertex; he receives consulting fees and own equity in NoviSci/Target RWE.
References
- 1. Joo H, Miller GF, Sunshine G, et al. Decline in COVID-19 hospitalization growth rates associated with statewide mask mandates – 10 states, March-October 2020. MMWR Morb Mortal Wkly Rep. 2021;70(6):212–216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dawson P, Worrell MC, Malone S, et al. ; CDC COVID-19 Surge Laboratory Group . Pilot investigation of SARS-CoV-2 secondary transmission in kindergarten through grade 12 schools implementing mitigation strategies - St. Louis County and City of Springfield, Missouri, December 2020. MMWR Morb Mortal Wkly Rep. 2021;70(12):449–455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Falk A, Benda A, Falk P, Steffen S, Wallace Z, Høeg TB. COVID-19 cases and transmission in 17 K-12 schools - Wood County, Wisconsin, August 31-November 29, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(4):136–140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hershow RB, Wu K, Lewis NM, et al. low sars-cov-2 transmission in elementary schools - Salt Lake County, Utah, December 3, 2020-January 31, 2021. MMWR Morb Mortal Wkly Rep. 2021; 70(12):442–448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zimmerman KO, Akinboyo IC, Brookhart MA, et al. ; ABC SCIENCE COLLABORATIVE . Incidence and secondary transmission of SARS-CoV-2 infections in schools. Pediatrics. 2021;147(4):e2020048090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Goldhaber D, Imberman SA, Strunk KO, et al. To what extent does in-person schooling contribute to the spread of COVID-19? Evidence from Michigan and Washington. Working paper no. 247-1220-3. 2021. Available at: https://caldercenter.org/sites/default/files/CALDER%20WP%20247-1220-2_0.pdf. Accessed August 11, 2021
- 7. Ohio Department of Health; The Ohio Schools COVID-19 Evaluation Research Team . Ohio schools COVID-19 evaluation: final report. Available at: https://coronavirus.ohio.gov/static/responsible/schools/OSCE_evaluation.pdf. Accessed August 11, 2021
- 8. Doyle T, Kendrick K, Troelstrup T, et al. COVID-19 in primary and secondary school settings during the first semester of school reopening — Florida, August–December 2020. MMWR Morb Mortal Wkly Rep. 2021;70(12):437–441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Centers for Disease Control and Prevention . Guidance for COVID-19 prevention in K-12 schools. Available at: https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/k-12-guidance.html. Accessed August 11, 2021
- 10. North Carolina Department of Health and Human Services . StrongSchoolsNC Public Health Toolkit (K-12): Interim Guidance. Available at: https://covid19.ncdhhs.gov/media/164/open. Accessed October 6, 2021
- 11. Centers for Disease Control and Prevention . Guidance for wearing masks. Available at: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cloth-face-cover-guidance.html. 2021. Accessed August 11, 2021
- 12. Kaiser Permanente Department of Research & Evaluation Southern California . Systematic observation of mask adherence and distancing (SOMAD). Available at: https://www.kp-scalresearch.org/somad/. Accessed October 6, 2021
- 13. Karimi SM, Salunkhe SS, White KB, et al. Prevalence of unmasked and improperly masked behavior in indoor public areas during the COVID-19 pandemic: Analysis of a stratified random sample from Louisville, Kentucky. PLoS One. 2021;16(7):e0248324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Centers for Disease Control and Prevention . Monitoring and evaluation action guide: wearing masks as a COVID-19 community mitigation strategy. Available at: https://www.cdc.gov/coronavirus/2019-ncov/php/mask-evaluation.html. Accessed October 6, 2021
- 15. Johns Hopkins University & Medicine . Coronavirus resource center. Available at: https://coronavirus.jhu.edu. Accessed August 11, 2021
- 16. North Carolina Department of Public Instruction . Student accounting data, principal’s monthly report data. Available at: https://www.dpi.nc.gov/districts-schools/district-operations/financial-and-business-services/demographics-and-finances/student-accounting-data. Accessed August 11, 2021
- 17. Public Schools of North Carolina . Statistical profile. Available at: http://apps.schools.nc.gov/ords/f?p=145:1. Accessed August 11, 2021
- 18. Mickells GE, Figueroa J, West KW, Wood A, McElhanon BO. Adherence to masking requirement during the COVID-19 pandemic in early elementary school children. J Sch Health. 2021;91(7):555–561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wakui N, Abe S, Shirozu S, et al. Causes of anxiety among teachers giving face-to-face lessons after the reopening of schools during the COVID-19 pandemic: a cross-sectional study. BMC Public Health. 2021;21(1):1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Li Q, Tarimo CS, Miao Y, Zeng X, Wu C, Wu J. Effects of mask wearing on anxiety of teachers affected by COVID-19: A large cross-sectional study in China. J Affect Disord. 2021;281:574–580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Murphy LR, Sturdivant K, Gershon RM. Organizational and employee characteristics predict compliance with universal precautions. In: Annual Meeting of the American Psychological Society, June 25–28, 1993; Chicago, IL [Google Scholar]
- 22. Katz AS, Pronk NP, McLellan D, Dennerlein J, Katz JN. Perceived workplace health and safety climates: associations with worker outcomes and productivity. Am J Prev Med. 2019;57(4):487–494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Stackhouse M, Turner N. How do organizational practices relate to perceived system safety effectiveness? Perceptions of safety climate and co-worker commitment to safety as workplace safety signals. J Safety Res. 2019; 70:59–69 [DOI] [PubMed] [Google Scholar]