Abstract
Video Abstract
OBJECTIVES
We describe the change in the percentage of children lacking continuous and adequate health insurance (underinsurance) from 2016 to 2019. We also examine the relationships between child health complexity and insurance type with underinsurance.
METHODS
Secondary analysis of US children in the National Survey of Children’s Health combined 2016–2019 dataset who had continuous and adequate health insurance. We calculated differences in point estimates, with 95% confidence intervals (CIs), to describe changes in our outcomes over the study period. We used multivariable logistic regression adjusted for sociodemographic characteristics and examined relationships between child health complexity and insurance type with underinsurance.
RESULTS
From 2016 to 2019, the proportion of US children experiencing underinsurance rose from 30.6% to 34.0% (+3.4%; 95% CI, +1.9% to +4.9%), an additional 2.4 million children. This trend was driven by rising insurance inadequacy (24.8% to 27.9% [+3.1%; 95% CI, +1.7% to +4.5%]), which was mainly experienced as unreasonable out-of-pocket medical expenses. Although the estimate of children lacking continuous insurance coverage rose from 8.1% to 8.7% (+0.6%), it was not significant at the 95% CI (−0.5% to +1.7%). We observed significant growth in underinsurance among White and multiracial children, children living in households with income ≥200% of the federal poverty limit, and those with private health insurance. Increased child health complexity and private insurance were significantly associated with experiencing underinsurance (adjusted odds ratio, 1.9 and 3.5, respectively).
CONCLUSIONS
Underinsurance is increasing among US children because of rising inadequacy. Reforms to the child health insurance system are necessary to curb this problem.
What’s Known on This Subject:
Continuous and adequate health insurance is critical to child health. In recent years, child uninsurance has increased, and participation in Medicaid and the Children’s Health Insurance Program has fallen. Research examining whether these trends also apply to child underinsurance is needed.
What This Study Adds:
From 2016 to 2019, underinsurance rose significantly among US children because of increased rates of insurance inadequacy. Increased health complexity and private insurance were associated with being underinsured. Notably, underinsurance grew significantly among White children living in middle-income families.
Continuous and adequate insurance coverage is critical to ensuring the health and flourishing of US children. Children with inconsistent insurance coverage experience difficulty receiving preventive well-child care and often delay, sometimes even forgoing, needed medical care.1,2 Inadequate insurance is associated with receiving lower-quality care, experiencing lower family satisfaction, and having unmet health care needs (eg, prescription medications).3,4 For these reasons, one of the Maternal and Child Health Bureau’s national performance goals calls for increasing the proportion of children with continuous and adequate insurance coverage, a target endorsed by the American Academy of Pediatrics and Healthy People 2030 national guidelines.5,6 In recent work, however, researchers have raised serious concerns that progress in child health insurance achieved after implementation of the Affordable Care Act (ACA) (and related expansion of Medicaid and the Children’s Health Insurance Program [CHIP]) has stalled or even reversed. Analyses of the American Community Survey have revealed increasing child uninsurance and declining Medicaid and/or CHIP participation among eligible children since 2016.7,8
It is unclear whether these concerning trends apply to other dimensions of child insurance: insurance consistency and adequacy. To our knowledge, these aspects of insurance have not been fully described since the 2010 analysis of child underinsurance by Kogan et al.3 Furthermore, given the increasing prevalence and impact on health care systems of children with special health care needs (CSHCN), including children with more complex chronic health conditions, it is especially important to characterize any changes among these pediatric populations.9,10 Continuous and adequate health insurance is critical for access to and use of health care services that reduce this vulnerable group’s risk of future complications and poor health outcomes.11,12 Recent shifts in the sources of children’s insurance coverage away from Medicaid and/or CHIP to parental employer-based health insurance make reexamining the relationships between insurance type (ie, public versus private) with insurance consistency and adequacy imperative as well.7 Historically, public insurance coverage has been connected with better protection against out-of-pocket costs, as well as improved access to and satisfaction with health care.3,12,13
Therefore, we examined responses to the National Survey of Children’s Health (NSCH) to (1) describe the proportion of US children lacking continuous and adequate insurance coverage (henceforth referred to as underinsurance) using measures contained in the NSCH’s combined 2016–2019 data sets, (2) examine how child underinsurance (and its component indicators) changed from 2016 to 2019, (3) investigate which specific pediatric populations experienced significant changes in underinsurance over this time period, and (4) study how child health complexity and insurance type are related to being underinsured. We hypothesized that increased health complexity and private insurance coverage (eg, employer-sponsored insurance) would be associated with higher risk of being underinsured.
Methods
Study Design and Data Source
This is a secondary analysis of the combined 2016–2019 data sets of the NSCH. This survey is designed and funded by the Maternal and Child Health Bureau of the Health Resources and Services Administration. Since 2016, it has been conducted annually by the US Census Bureau using mail- and Web-based instruments.14 The NSCH consists of >150 items and produces national- and state-level data on the physical and emotional health of all American children (aged 0–17 years). Respondents were typically biological or adoptive parents (>90%). Additional details about survey administration, sampling strategy, and response rates have been previously described elsewhere.15 Of note, a new cross-sectional sample is recruited each year for the NSCH, so longitudinal data are not collected in the survey. This study received exempt status from our university’s institutional review board.
Outcomes
We used the Title V Maternal and Child Health Services Block Grant Program National Performance Measure (NPM) 15 (“Percent of children ages 0 through 17 years who are continuously and adequately insured”) for our primary outcome.15,16 To qualify on this measure, a child had to meet 2 criteria: (1) did the child have continuous insurance coverage over the previous 12 months, and (2) did she or her have adequate health insurance? A child’s insurance was considered to be continuous if they were insured at the time of the survey and consistently insured throughout the previous year (ie, child had no periods without insurance). Insurance adequacy was a composite variable with 3 component questions (each with ordinal response options). Insurance was considered adequate if the insurance benefits “usually” or “always” met the child’s needs, usually or always allowed the child to see needed providers, and the child either had no out-of-pocket expenses or out-of-pocket expenses were usually or always reasonable. If a caregiver respondent answered “sometimes” or “never” to any of the 3 adequacy components, we categorized the child’s insurance as inadequate. Children without continuous insurance and/or had inadequate insurance were classified as underinsured.17
Child and Family Characteristics
We examined child health and personal factors, as well as family characteristics, in relation to our outcomes. Child factors included complexity of health needs, age, sex, race and ethnicity, nativity status (born in the United States), and insurance type. Family characteristics included household income (categorized by percentages of the federal poverty limit [FPL]), family structure, and parental educational attainment. Recognizing that race and ethnicity are complex social constructs, child race and ethnicity were grouped into categories specified by the US Census Bureau and included as covariates in multivariable analyses to account for well-documented disparities in access to medical care among children who are not White.18,19
To classify children in the sample by complexity of their health care needs, we used the Data Resource Center for Child and Adolescent Health approach.17 This method uses items from the CSHCN Screener questionnaire in the NSCH to divide the study population into 3 groups: (1) children with no special health care needs (non-CSHCN), (2) less complex CSHCN, and (3) more complex CSHCN.20 Less complex CSHCN were children with chronic (lasting >12 months) health conditions managed primarily through prescription medication. More complex CSHCN were children with chronic conditions resulting in ≥1 of the following health consequences: (1) elevated need or use of medical services, (2) limitations in day-to-day activities, (3) need or use of specialized therapies (eg, physical and occupational therapy), and/or (4) need or use of treatment of an emotional, behavioral, or developmental condition.21
We used the Data Resource Center for Child and Adolescent Health approach to categorize children by insurance type as well.17 Children whose coverage came from any form of government assistance (eg, Medicaid and Medical Assistance) were classified as having public insurance. Private insurance was defined as coverage through a family member’s current or former employer or union, the ACA, direct purchase from an insurance company, or TRICARE or other military health care. Children who lacked insurance at time of the survey or only had Indian Health Services or a religious health share as an insurance type were considered to be uninsured. A combined category of public and private insurance included children with both public and private forms of coverage.
Analysis
We summarized our primary outcome (underinsurance), its component indicators, and overall child and/or family characteristics using descriptive statistics. We examined the relationships between our primary outcome and child and/or family characteristics using χ2 tests of association. To describe changes in underinsurance and its component indicators over the study period, we calculated differences in point estimates, along with 95% confidence intervals (CIs). To examine if child health complexity and insurance type were independently associated with underinsurance, we included only child and/or family characteristics significant in χ2 testing (P < .01) in a multivariable, adjusted logistic regression analysis, in which our primary outcome was the dependent variable.
In all analyses, we used person-level and survey weights provided by the NSCH to generate national, multiyear estimates. Missing values for household family income were multiply imputed using sequential regression methods by NSCH administrators; therefore, the analyses involving the income variable were run across all data set imputations and combined to generate more conservative estimates.17 Statistical analyses were performed with Stata version 16.0 (Stata Corp, College Station, TX).
Results
Among 73.3 million children aged 0 to 17 years in the United States in 2016–2019, just over two-thirds (67.6%; 95% CI, 67.0% to 68.1%) had continuous and adequate insurance coverage, whereas almost one-third (32.4% [23.7 million]), did not meet criteria for this outcome and were classified as underinsured (Table 1). Examining the 2 component criteria, 93.6% (68.3 million) of children were insured at the time of the survey, 91.5% (66.4 million) were consistently insured throughout the year before the survey, and 73.7% (50.3 million) had adequate insurance. In χ2 analysis, underinsurance was significantly associated with increased health complexity, private insurance coverage, older child age (≥6 years of age), non-Black racial identity, US nonnative status, and family income ≥100% FPL (all P < .001).
TABLE 1.
US Children Who Were Insured at Time of Survey, Consistently Insured, Adequately Insured, and Adequately and Continuously Insured in 2016–2019, by Child and Family Characteristics
| Characteristic | Overall 2016–2019, Weighted n (Column %) | Insured at Time of Survey, Weighted n (Row %) | Consistently Insured Over Past Year, Weighted n (Row %) | Adequate Insurance Coverage, Weighted n (Row %) | Adequately and Continuously Insured, Weighted n (Row %) |
|---|---|---|---|---|---|
| All Children | 73 335 159 | 68 292 897 (93.6) | 66 395 741 (91.5) | 50 269 452 (73.7) | 49 323 573 (67.6) |
| Child health complexity | *** | *** | *** | *** | |
| Non-CSHCN | 59 518 364 (81.2) | 55 076 827 (93.1) | 53 615 174 (91.1) | 41 369 384 (75.3) | 40 643 461 (68.7) |
| Less complex CSHCN | 4 041 891 (5.5) | 3 894 653 (96.8) | 3 775 255 (93.9) | 2 802 922 (72.0) | 2 730 904 (67.8) |
| More complex CSHCN | 9 774 904 (13.3) | 9 321 416 (95.8) | 9 005 312 (92.7) | 6 097 147 (65.5) | 5 949 208 (61.1) |
| Child insurance type | *** | *** | *** | *** | |
| Public only | 22 207 679 (30.8) | 22 207 679 (100.0) | 21 079 072 (95.2) | 19 531 920 (88.0) | 18 812 197 (84.7) |
| Private only | 41 709 803 (57.8) | 41 709 803 (100.0) | 41 086 339 (98.5) | 27 634 250 (66.3) | 27 430 137 (65.8) |
| Public and private | 3 289 876 (4.6) | 3 289 876 (100.0) | 3 186 818 (97.0) | 2 327 670 (70.8) | 2 274 884 (69.2) |
| Uninsured | 4 941 778 (6.8) | — | — | — | — |
| Household income (% FPL) | *** | *** | *** | *** | |
| <100 | 14 813 702 (20.2) | 13 281 414 (89.7) | 12 763 543 (86.2) | 12 275 966 (82.9) | 10 662 984 (72.0) |
| 100–199 | 15 987 064 (21.8) | 14 625 562 (91.5) | 14 105 861 (88.2) | 12 449 380 (77.9) | 11 032 268 (69.0) |
| 200–399 | 20 093 833 (27.4) | 18 925 350 (94.2) | 18 482 126 (92.0) | 13 635 863 (67.9) | 12 565 035 (62.5) |
| ≥400 | 22 440 558 (30.6) | 21 832 021 (97.3) | 21 709 996 (96.7) | 15 822 440 (70.5) | 15 307 871 (68.2) |
| Child age, y | *** | P = .008 | *** | *** | |
| 0–5 | 23 617 969 (32.2) | 22 269 560 (94.7) | 21 598 631 (92.3) | 17 197 874 (77.3) | 16 840 790 (71.6) |
| 6–11 | 24 767 317 (33.8) | 23 058 945 (93.7) | 22 400 281 (91.4) | 16 869 650 (73.2) | 16 523 944 (67.1) |
| 12–17 | 24 949 873 (34.0) | 22 964 391 (92.6) | 22 396 829 (90.7) | 16 201 928 (70.7) | 15 958 839 (64.3) |
| Sex | P = .92 | P = .95 | P = .72 | P = .87 | |
| Male | 37 481 907 (51.1) | 34 891 514 (93.6) | 33 907 009 (91.5) | 25 647 704 (73.6) | 25 186 092 (67.5) |
| Female | 35 853 252 (48.9) | 33 401 383 (93.7) | 32 488 732 (91.4) | 24 621 748 (73.8) | 24 137 481 (67.6) |
| Child race and ethnicity | *** | *** | *** | *** | |
| Hispanic | 18 397 567 (25.1) | 16 509 175 (90.3) | 15 850 946 (86.9) | 12 448 279 (75.5) | 12 090 075 (66.1) |
| White, non-Hispanic | 37 321 140 (50.9) | 35 440 993 (95.3) | 34 739 935 (94.0) | 25 230 036 (71.3) | 24 913 996 (67.0) |
| Black, non-Hispanic | 9 676 323 (13.2) | 8 902 309 (93.0) | 8 538 975 (89.4) | 7 114 405 (80.1) | 6 920 203 (72.2) |
| Other/multiracial | 7 940 128 (10.8) | 7 440 419 (94.3) | 7 265 885 (92.6) | 5 476 733 (73.8) | 5 399 299 (68.4) |
| Child born in the United States | *** | *** | *** | *** | |
| Yes | 69 851 327 (95.9) | 65 498 818 (94.1) | 63 718 738 (92.0) | 48 322 331 (73.9) | 47 404 133 (68.1) |
| No | 2 974 936 (4.1) | 2 459 516 (83.7) | 2 355 164 (80.2) | 1 707 765 (69.5) | 1 666 146 (56.5) |
| Family structure | *** | *** | *** | *** | |
| Two parents, married | 46 654 132 (65.5) | 43 995 208 (94.5) | 43 054 521 (93.0) | 31 323 468 (71.3) | 30 822 219 (66.2) |
| Two parents, not married | 6 260 099 (8.8) | 5 758 147 (92.6) | 5 532 636 (89.2) | 4 453 946 (77.5) | 4 350 188 (69.9) |
| Single parent | 13 514 839 (19.0) | 12 464 674 (92.7) | 11 948 384 (89.0) | 9 567 481 (76.9) | 9 287 398 (69.0) |
| Grandparent | 2 233 051 (3.1) | 2 020 144 (92.1) | 1 953 468 (89.9) | 1 724 926 (85.6) | 1 702 588 (77.4) |
| Other | 2 574 627 (3.6) | 2 278 334 (89.8) | 2 174 180 (86.2) | 1 878 267 (82.5) | 1 819 192 (71.6) |
| Highest parental educational attainment | *** | *** | *** | *** | |
| Less than high school | 6 722 963 (9.2) | 5 362 123 (80.9) | 5 130 744 (78.4) | 4 382 877 (81.8) | 4 248 852 (64.0) |
| High school | 14 026 904 (19.1) | 12 682 702 (91.0) | 12 178 549 (87.8) | 10 142 135 (80.1) | 9 852 003 (70.6) |
| Some college | 16 092 256 (21.9) | 15 083 016 (94.2) | 14 518 078 (90.9) | 11 171 538 (74.2) | 10 886 095 (67.9) |
| College or more | 35 845 273 (48.9) | 34 601 515 (96.8) | 34 015 345 (95.5) | 24 152 357 (69.9) | 23 899 286 (66.9) |
In all analyses, we used person-level and survey-year weights provided by the NSCH to generate estimates of population size and prevalence; —, not applicable.
P < .001 in χ2 analysis.
Table 2 shows how the proportion of children who had continuous and adequate insurance coverage, and this outcome’s component variables, changed from 2016 to 2019. Over this time period, underinsurance among all US children rose from 30.6% to 34.0% (+3.4% [95% CI, +1.9% to +4.9%), a relative increase of 11.1%, representing an additional 2.4 million children. The percentage of children who lacked continuous insurance coverage increased from 8.1% to 8.7% (representing >400 000 children). Although this difference (+0.6%) was not significant at the 95% CI (−0.5% to +1.7%), this trend appeared to reflect a rise in children who were uninsured the entire 12 months before the survey (+0.6% [95% CI, −0.3% to +1.5%]). In contrast, the percentage of children with inadequate insurance significantly increased (+3.1% [95% CI, +1.7% to +4.5%]) to 27.9% in 2019, a relative increase of 12.5%, corresponding to 2.3 million children. The increase in the proportion of children who had unreasonable out-of-pocket medical expenses (+2.9% [95% CI, +1.5% +4.2%]) mainly drove the rise in insurance inadequacy. Table 2 also displays the change in child insurance type from 2016 to 2019. Both the decrease in the children with public-only insurance (−2.3% [95% CI, −0.8% to −3.9%]) and increase in children with private-only insurance (+2.5% [95% CI, +0.8% to +4.2%]) were significant at the 95% CI. The percentage of change in the shift to private-only health insurance represented an increase of >1.8 million children.
TABLE 2.
Change in NPM 15, Insurance Continuity, Adequacy, and Type From 2016 to 2019, by Year
| Outcome | 2016 (% [95% CI]) | 2017 (% [95% CI]) | 2018 (% [95% CI]) | 2019 (% [95% CI]) | Difference 2016–2019 (% [95% CI]) |
|---|---|---|---|---|---|
| NPM 15 | |||||
| Had continuous and adequate insurance | 69.4 (68.4 to 70.3) | 67.5 (66.1 to 68.8) | 67.5 (66.4 to 68.6) | 66.0 (64.8 to 67.2) | −3.4 (−1.9 to −4.9) |
| Consistently insured throughout past year | 91.9 (91.2 to 92.5) | 91.8 (90.8 to 92.7) | 90.8 (90.0 to 91.6) | 91.3 (90.4 to 92.1) | −0.6 (−1.7 to 0.5) |
| Insured at time of survey | 94.0 (93.4 to 94.6) | 93.8 (92.8 to 94.6) | 93.4 (92.7 to 94.1) | 93.3 (92.5 to 94.0) | −0.7 (−1.7 to 0.2) |
| Insured all 12 mo | 91.9 (91.2 to 92.5) | 91.8 (90.8 to 92.7) | 90.8 (90.0 to 91.6) | 91.3 (90.4 to 92.1) | −0.6 (−1.7 to 0.5) |
| Insured but with gaps | 3.4 (3.0 to 3.8) | 4.2 (3.6 to 4.9) | 3.9 (3.4 to 4.4) | 3.4 (2.9 to 3.9) | 0.0 (−0.6 to 0.7) |
| No coverage entire past 12 mo | 4.7 (4.2 to 5.3) | 4.2 (3.6 to 4.9) | 5.3 (4.7 to 6.0) | 5.3 (4.7 to 6.1) | +0.6 (−0.3 to 1.5) |
| Adequate insurance coverage | 75.2 (74.4 to 76.0) | 73.5 (72.2 to 74.7) | 74.0 (73.0 to 75.0) | 72.1 (71.0 to 73.2) | −3.1 (−4.5 to −1.7) |
| Current insurance meets child’s needs | |||||
| Always | 67.6 (66.7 to 68.6) | 67.5 (66.1 to 68.8) | 67.1 (66.0 to 68.2) | 65.9 (64.6 to 67.1) | −1.8 (−3.3 to −0.2) |
| Usually | 26.3 (25.4 to 27.2) | 26.0 (24.8 to 27.3) | 26.3 (25.3 to 27.4) | 27.1 (26.0 to 28.3) | +0.8 (0.6 to 2.2) |
| Sometimes or never | 6.0 (5.6 to 6.5) | 6.5 (5.8 to 7.3) | 6.6 (5.9 to 7.2) | 7.0 (6.3 to 7.8) | +1.0 (0.1 to 1.8) |
| Child able to see needed providers | |||||
| Always | 79.7 (78.9 to 80.5) | 78.7 (77.4 to 79.8) | 78.4 (77.3 to 79.4) | 76.6 (75.5 to 77.7) | −3.0 (−4.4 to −1.7) |
| Usually | 16.7 (16.0 to 17.5) | 17.2 (16.1 to 18.3) | 18.0 (17.1 to 18.9) | 19.2 (18.2 to 20.3) | +2.5 (1.2 to 3.8) |
| Sometimes or never | 3.6 (3.2 to 4.0) | 4.1 (3.6 to 4.8) | 3.6 (3.2 to 4.2) | 4.1 (3.7 to 4.7) | +0.5 (−0.1 to 1.2) |
| Out-of-pocket expenses reasonable | |||||
| Always | 16.3 (15.6 to 16.9) | 17.3 (16.3 to 18.5) | 15.2 (14.4 to 16.0) | 14.7 (13.9 to 15.6) | −1.6 (−2.6 to −0.5) |
| Usually | 27.5 (26.7 to 28.3) | 26.3 (25.2 to 27.5) | 27.8 (26.9 to 28.8) | 26.4 (25.4 to 27.5) | −1.0 (−2.3 to −0.3) |
| Sometimes or never | 22.2 (21.5 to 23.0) | 23.6 (22.4 to 24.7) | 23.0 (22.0 to 23.9) | 25.1 (24.0 to 26.2) | +2.9 (1.5 to 4.2) |
| No out-of-pocket costs | 34.1 (33.0 to 35.1) | 32.8 (31.3 to 34.4) | 34.0 (32.7 to 35.3) | 33.8 (32.5 to 35.1) | −0.3 (−2.0 to 1.4) |
| Insurance type | |||||
| Public only | 31.7 (30.7 to 32.8) | 30.8 (29.3 to 32.3) | 31.2 (30.0 to 32.4) | 29.4 (28.2 to 30.7) | −2.3 (−0.8 to −3.9) |
| Private only | 56.4 (55.4 to 57.4) | 57.9 (56.4 to 59.4) | 58.1 (56.8 to 59.3) | 58.9 (57.6 to 60.2) | +2.5 (0.8 to 4.2) |
| Public and private | 4.3 (3.9 to 4.7) | 5.0 (4.3 to 5.8) | 4.1 (3.6 to 4.6) | 4.9 (4.3 to 5.6) | +0.6 (−0.1 to 1.4) |
NPM 15 is the percentage of children aged 0 to 17 y who are continuously and adequately insured. To qualify on this measure, a child had to (1) have insurance coverage at the time of the survey and consistently over the previous 12 mo and (2) have insurance benefits that usually or always (a) meets a child’s needs, (b) allows a child to see needed providers, and (c) had reasonable out-of-pocket medical expenses (or no out-of-pocket costs).
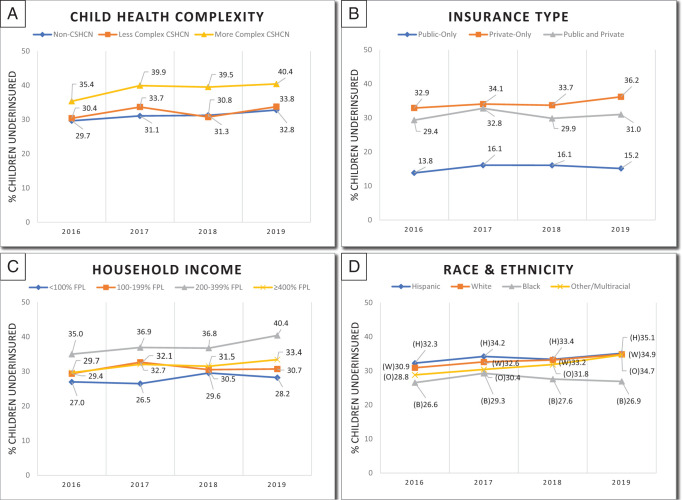
The second column of Table 3 summarizes how the prevalence of underinsurance changed for child health and child and/or family sociodemographic subgroups over the study period. With regard to child health complexity, underinsurance increased significantly for non-CSHCN (+3.1%) and more complex CSHCN (+5.1%) but not for less complex CSHCN. Although the increase in underinsurance among children with private-only health insurance was significant at the 95% CI (+3.3% [+1.6% to +5.0%]), this was not the case among children with public-only health insurance (+3.3% [95% CI, −1.0% to +3.7%]). We also observed significant growth in underinsurance among children identified as White or other and/or multiracial, born in the United States, living in households with family income ≥200% FPL, living with 2 married parents, and whose parent(s) have a college degree or higher. Year-by-year changes in the proportion of children lacking continuous and adequate insurance coverage by select child demographics are demonstrated in Fig 1.
TABLE 3.
Factors Associated With Child Underinsurance (Lacking Continuous and Adequate Insurance Coverage)
| Characteristic | Child Underinsurance | ||
|---|---|---|---|
| Change From 2016 to 2019, % (95% CI) | Pooled 2016–2019, No. (% [95% CI])a | Likelihood, aOR (95% CI)b | |
| Overall Sample | +3.4 (1.9 to 4.9) | 23 652 955 (32.4 [31.8 to 33.0]) | |
| Child health complexity | *** | ||
| Non-CSHCN | +3.1 (1.4 to 4.8) | 18 561 908 (31.4 [30.7 to 32.0]) | Reference |
| Less complex CSHCN | +3.3 (−2.3 to 8.9) | 1 298 337 (32.2 [30.2 to 34.3]) | 1.2 (1.1 to 1.3) |
| More complex CSHCN | +5.1 (1.4 to 8.9) | 3 792 137 (38.9 [37.4 to 40.5]) | 1.9 (1.8 to 2.1) |
| Insurance type | *** | ||
| Public | +1.3 (−1.0 to 3.7) | 3 394 549 (15.3 [14.4 to 16.3]) | Reference |
| Private | +3.3 (1.6 to 5.0) | 14 279 667 (34.2 [33.6 to 34.9]) | 3.5 (3.1 to 3.9) |
| Public and private | +1.6 (−6.1 to 9.4) | 1 014 992 (30.9 [27.9 to 33.9]) | 2.3 (2.0 to 2.8) |
| Household income (% FPL) | *** | ||
| ≥400 | +3.7 (1.5 to 6.0) | 7 132 686 (31.8 [30.9 to 32.6]) | Reference |
| <100 | +1.2 (−2.8 to 5.2) | 4 150 718 (28.0 [26.4 to 29.6]) | 1.3 (1.1 to 1.4) |
| 100–199 | +1.3 (−2.1 to 4.8) | 4 954 796 (31.0 [29.6 to 32.4]) | 1.3 (1.2 to 1.5) |
| 200–399 | +5.4 (2.6 to 8.2) | 7 528 798 (37.5 [36.4 to 38.5]) | 1.4 (1.3 to 1.5) |
| Child age, y | *** | ||
| 0 − 5 | +3.9 (1.3 to 6.5) | 6 691 866 (28.4 [27.5 to 29.4]) | Reference |
| 6 − 11 | +1.9 (−0.8 to 4.6) | 8 096 995 (32.9 [31.9 to 33.9]) | 1.1 (1.1 to 1.2) |
| 12 − 17 | +4.3 (1.8 to 6.8) | 8 863 521 (35.7 [34.8 to 36.7]) | 1.2 (1.1 to 1.3) |
| Sex | P = .85 | ||
| Male | +3.3 (1.3 to 5.4) | 12 103 123 (32.5 [31.7 to 33.3]) | — |
| Female | +3.4 (1.3 to 5.6) | 11 549 259 (32.4 [31.5 to 33.2]) | — |
| Child race and ethnicity | *** | ||
| White, non−Hispanic | +4.0 (2.5 to 5.5) | 12 272 596 (33.0 [32.4 to 33.6]) | Reference |
| Hispanic | +2.7 (−1.5 to 7.0) | 6 212 872 (33.9 [32.3 to 35.6]) | 1.1 (1.0 to 1.3) |
| Black, non−Hispanic | +0.3 (−3.8 to 4.4) | 2 670 412 (27.8 [26.2 to 29.5]) | 0.9 (0.8 to 1.0) |
| Other/multiracial | +5.8 (1.9 to 9.7) | 2 496 502 (31.6 [30.2 to 33.1]) | 1.0 (0.9 to 1.0) |
| Child born in the United States | *** | ||
| Yes | +3.6 (2.1 to 5.1) | 22 217 145 (31.9 [31.3 to 32.5]) | Reference |
| No | −1.1 (−10.0 to 7.8) | 1 284 377 (43.5 [40.3 to 46.9]) | 1.3 (1.1 to 1.5) |
| Family structure | *** | ||
| Two parents, married | +2.9 (1.1 to 4.6) | 15 727 591 (33.8 [33.1 to 34.5]) | Reference |
| Two parents, not married | +4.9 (−1.0 to 10.8) | 1 873 560 (30.1 [28.0 to 32.3]) | 1.0 (0.9 to 1.2) |
| Single parent | +4.0 (0.5 to 7.5) | 4 169 834 (31.0 [29.7 to 32.4]) | 1.1 (1.0 to 1.2) |
| Grandparent | c | 497 346 (22.6 [19.4 to 26.2]) | 0.7 (0.5 to 0.9) |
| Other | +12.5 (−0.3 to 25.3) | 720 372 (28.4 [25.3 to 31.6]) | 0.9 (0.8 to 1.1) |
| Highest parental educational attainment | *** | ||
| College or more | +4.5 (2.8 to 6.3) | 11 848 484 (33.1 [32.5 to 33.8]) | Reference |
| Less than high school | +6.5 (−1.6 to 14.5) | 2 387 649 (36.0 [33.0 to 39.1]) | 1.0 (0.8 to 1.2) |
| High school | +0.9 (−2.8 to 4.5) | 4 097 081 (29.4 [27.9 to 30.9]) | 1.0 (0.9 to 1.1) |
| Some college | +1.2 (−1.8 to 4.2) | 5 141 484 (32.1 [31.0 to 33.2]) | 1.1 (1.0 to 1.1) |
Row percentages unless otherwise noted. aOR, adjusted odds ratio; —, not applicable.
χ2 analysis.
Multivariable logistic regression analysis adjusted for all variables included in the final model.
Unable to trend grandparent-led household because this response option was not included in the 2016 survey.
p<.001
FIGURE 1.
Percentage of children underinsured by demographic characteristics. A, CSHCN were identified by presence of at least 1 of 5 screening criteria: use of a prescription medication, elevated use of medical services, need or use of specialized therapies, presence of functional limitation(s), or developmental and/or behavioral treatment. Less complex CSHCN were those who had chronic health conditions managed solely with prescription medications, whereas more complex CSHCN met ≥1 of the other 4 screening criteria. B, Differences by child insurance type. C, household income as a percentage of the FPL. D, differences by child race and ethnicity categories.
In adjusted multivariable regression (Table 3), child health complexity and insurance type were significantly associated with experiencing underinsurance. Compared with non-CSHCN, the odds of being underinsured were significantly higher among less complex CSHCN (odds ratio [OR], 1.2; 95% CI, 1.1 to 1.3) and more complex CSHCN (OR, 1.9; 95% CI, 1.8 to 2.1). Regarding insurance type, children with private-only health insurance were >3 times as likely to be underinsured (OR, 3.5; 95% CI, 3.1 to 3.9) than children with public-only insurance. Similarly, children with a mix of private and public insurance had more than twice the odds of being underinsured than children with public-only insurance. Child age, nativity status, and household family income also were independently associated with our primary outcome in adjusted analysis, however, with smaller effect sizes.
Discussion
In this analysis of the combined 2016–2019 data sets of the NSCH, the proportion of children lacking continuous and adequate insurance coverage rose from 2016 to 2019. Rising insurance inadequacy primarily drove the observed increase in underinsurance, mainly because caregivers reported their insurance did not adequately cover their child’s medical expenses or protect them from unreasonable out-of-pocket costs. Notably, we observed significant growth in underinsurance among more complex CSHCN and children with private insurance. We also demonstrate increased underinsurance among White and multiracial children living in households with family income ≥200% FPL, 2 married parents, and high parental educational attainment. Lastly, we found increased health complexity and private insurance coverage were significant predictors of being underinsured, as were older age, being born outside of the United States, and living below 400% FPL.
This study adds to the growing concern about the current state of US children’s health insurance. We show loss of any gains in underinsurance achieved after the passage of the ACA. The proportion of children with continuous and adequate health insurance coverage in 2019 is now within the SE of the Kogan et al3 pre-ACA examination of underinsurance which used data from the 2007 NSCH. Although our observed increase in the percentage of children lacking insurance at time of the survey was not significant at the 95% CI (+0.7%), our overall findings parallel recent analyses of the American Community Survey that demonstrate child uninsurance rose by a full percentage point (to 5.7%) from 2016 to 2019.7,22
By examining how component indicators of underinsurance changed over time, we are able to identify drivers of child underinsurance. We found that insurance inadequacy experienced as unreasonable out-of-pocket medical expenses increased significantly, in line with studies of US adult underinsurance showing a doubling of insurance inadequacy because of high out-of-pocket costs in the past decade.23 High out-of-pocket costs are problematic because they increase the risk of forgone care and the burden on a family’s finances.24,25 This rise in unreasonable out-of-pocket expenses is likely due to the broader pattern of commercial insurance plans becoming more expensive and transferring costs to individuals and families.26 Employer-sponsored insurance plans now account for >11% of the national median household income (families in non-Medicaid expansion states experience even higher cost-sharing burdens) because of increases in premiums, copayments, and deductibles.27 High-deductible health plans have also come to dominate marketplace products, with almost 90% of marketplace enrollees selecting high-deductible products.28–30 These trends also help explain why we found children with private insurance were significantly more likely to be underinsured, further building the evidence base that public insurance better protects families from out-of-pocket costs.3,31,32
With this in mind, we also observed a significant increase in the proportion of children with commercial insurance products over our study period. This shift toward private insurance is consistent with work showing the proportion of US children eligible and participating in Medicaid and/or CHIP has recently decreased.8 In a study of the American Community Survey, Alker and Corcoran7 demonstrated that from 2017 to 2019, the percentage of children enrolled into Medicaid and/or CHIP decreased by 0.9% (to 33.5%), whereas children covered by employer-sponsored insurance increased by +0.7% (to 48.1%). This was likely due to the coupled effects of (1) gains in family employment and income (before the coronavirus disease 2019 pandemic) pushing children over Medicaid and/or CHIP income eligibility cutoffs and (2) concerted policy efforts to undermine Medicaid and/or CHIP outreach, enrollment, and benefit renewal.22,33 These changes in the sources of child insurance also potentially explain our notable finding that underinsurance rose significantly among children traditionally viewed as more socioeconomically advantaged, that is, White children living in middle-income households with high parental educational attainment.
Our adjusted regression analyses demonstrate that child health complexity was independently predictive of underinsurance. We found that more complex CSHCN had nearly twice the odds of being underinsured than non-CSHCN. Underinsurance rose by >5 percent in 4 years among more complex CSHCN, a relative increase larger than what was observed among less complex CSHCN and non-CSHCN (13.1% vs 10.2% and 9.9%, respectively). The proportion of more complex CSHCN lacking continuous and adequate insurance is now similar to levels reported in the pre-ACA 2001 and 2005 National Survey of CSHCN.31,34 This is concerning because more complex CSHCN are the children for whom continuous and adequate insurance is most critical given their extensive health service needs.35,36 Among this population, underinsurance is linked to reduced access to high-quality medical care and high rates of unmet needs, resulting in greater risk for morbidity and mortality, adverse functional outcomes, and increased emergency department use.37,38 Families of more complex CSHCN are also more vulnerable to financial adversities related to high deductibles and copayments.32,39 Further research directions include (1) better delineating the relationships between underinsurance and quality of care, health care use, and health outcomes among more complex CSHCN, (2) identifying subgroups of more complex CSHCN at higher risk for underinsurance, and (3) examining differences between underinsured versus uninsured more complex CSHCN.
Although our study does not indicate how to address insurance inadequacy (the main driver of underinsurance), inadequate health insurance is clearly a growing problem. Our data, demonstrating a shift from public to private insurance that is more likely to be inadequate, in conjunction with existing literature linking Medicaid and/or CHIP coverage with improved access to medical care (as well as improved long-term outcomes in adulthood), should give policy makers and payers pause as they contemplate strategies to improve child health.4,40–43 Approaches to expand child access to Medicaid and/or CHIP (eg, ensuring CSHCN with commercial insurance can use Medicaid as secondary coverage) or larger-scale reforms, such as a national single-payer child health insurance plan (“Medicare for Kids”), should be seriously considered.44–46
This study has important limitations. The NSCH is cross-sectional, so we cannot infer causality between observed associations or describe changes in outcomes for any individual child. All outcomes come from parental report, making the results vulnerable to recall and sampling bias without any validation from other objective measures (eg, percentage of family income spent on health insurance). Lastly, because there is no broadly accepted definition of underinsurance, other models of this construct might have yielded different findings.
Conclusions
The proportion of US children lacking continuous and adequate health insurance (ie, underinsured) increased significantly from 2016 to 2019, mainly through rising insurance inadequacy reported largely as unreasonable out-of-pocket medical expenses. Child health complexity and private insurance coverage are independent risk factors for experiencing underinsurance. Efforts to reverse these trends and improve the insurance adequacy for CSHCN are needed.
Glossary
- ACA
Affordable Care Act
- CHIP
Children’s Health Insurance Program
- CSHCN
children with special health care needs
- NSCH
National Survey of Children’s Health
- NPM
National Performance Measure
- FPL
federal poverty limit
- CI
confidence interval
- OR
odds ratio
Footnotes
Dr Yu conceptualized and designed the study, collected data, conducted the initial analyses, helped draft the initial manuscript, and reviewed and revised the final manuscript; Dr Perrin conceptualized and designed the study, supervised data analysis, and critically reviewed the manuscript for important intellectual content; Dr Hagerman helped to conceptualize and design the study, assisted with data collection, helped draft the initial manuscript, and reviewed and revised the final manuscript; Dr Houtrow conceptualized and designed the study, supervised data collection and analysis, drafted the initial manuscript, and reviewed and revised the final manuscript; and all authors approve the final manuscript as submitted and agree to be accountable for all aspects of the work.
FUNDING: No external funding.
References
- 1. Cassedy A, Fairbrother G, Newacheck PW. The impact of insurance instability on children’s access, utilization, and satisfaction with health care. Ambul Pediatr. 2008;8(5):321–328 [DOI] [PubMed] [Google Scholar]
- 2. Halterman JS, Montes G, Shone LP, Szilagyi PG. The impact of health insurance gaps on access to care among children with asthma in the United States. Ambul Pediatr. 2008;8(1):43–49 [DOI] [PubMed] [Google Scholar]
- 3. Kogan MD, Newacheck PW, Blumberg SJ, et al. Underinsurance among children in the United States. N Engl J Med. 2010;363(9):841–851 [DOI] [PubMed] [Google Scholar]
- 4. Szilagyi PG, Shone LP, Klein JD, Bajorska A, Dick AW. Improved health care among children with special health care needs after enrollment into the State Children’s Health Insurance Program. Ambul Pediatr. 2007;7(1): 10–17 [DOI] [PubMed] [Google Scholar]
- 5. Maternal and Child Health Bureau . Federally Available Data (FAD) Resource Document. Rockville, MD: Health Resources and Services Administration; 2021 [Google Scholar]
- 6. Board on Population Health and Public Health Practice . Leading Health Indicators 2030: Advancing Health, Equity, and Well-Being. Washington, DC: National Academy of Sciences; 2020 [PubMed] [Google Scholar]
- 7. Alker J, Corcoran A. Children’s Uninsured Rate Rises by Largest Annual Jump in More Than a Decade. Washington, DC: Georgetown University Center for Children and Families; 2020 [Google Scholar]
- 8. Haley J, Kenney GM, Wang R, Pan C, Lynch V, Buettgens M. Improvements in Uninsurance and Medicaid/CHIP Participation Among Children and Parents Stalled in 2017. Washington, DC: The Urban Institute; 2019 [Google Scholar]
- 9. Berry JG. What Children With Medical Complexity, Their Families, and Healthcare Providers Deserve From an Ideal Healthcare System. Palo Alto, CA: Lucile Packard Foundation for Children's Health; 2015 [Google Scholar]
- 10. Yu JA, McKernan G, Hagerman T, Schenker Y, Houtrow A. Identifying children with medical complexity from the National Survey of Children’s Health combined 2016-17 data set. Hosp Pediatr. 2021;11(2):192–197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jeffrey AE, Newacheck PW. Role of insurance for children with special health care needs: a synthesis of the evidence. Pediatrics. 2006;118(4). Available at: www.pediatrics.org/cgi/content/full/118/4/e1027 [DOI] [PubMed] [Google Scholar]
- 12. Oswald DP, Bodurtha JN, Willis JH, Moore MB. Underinsurance and key health outcomes for children with special health care needs. Pediatrics. 2007;119(2). Available at: www.pediatrics.org/cgi/content/full/119/2/e341 [DOI] [PubMed] [Google Scholar]
- 13. King C. Disparities in access to preventive health care services among insured children in a cross sectional study. Medicine (Baltimore). 2016; 95(28):e4262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ghandour RM, Jones JR, Lebrun-Harris LA, et al. The design and implementation of the 2016 National Survey of Children’s Health. Matern Child Health J. 2018;22(8):1093–1102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Child and Adolescent Health Measurement Initiative . Title V Maternal and Child Health Services Block Grant Measures Content Map. Washington, DC: US Census Bureau; 2020 [Google Scholar]
- 16. Kogan MD, Dykton C, Hirai AH, et al. A new performance measurement system for maternal and child health in the United States. Matern Child Health J. 2015;19(5):945–957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. US Census Bureau . 2019 National Survey of Children’s Health: Methodology Report. Washington, DC: U.S. Census Bureau; 2020 [Google Scholar]
- 18. US Census Bureau . Population. Washington, DC: US Census Bureau; 2020 [Google Scholar]
- 19. Creamer J. Inequalities Persist Despite Decline in Poverty for All Major Race and Hispanic Origin Groups. Washington, DC: US Census Bureau; 2020 [Google Scholar]
- 20. Bethell CD, Read D, Stein RE, Blumberg SJ, Wells N, Newacheck PW. Identifying children with special health care needs: development and evaluation of a short screening instrument. Ambul Pediatr. 2002;2(1):38–48 [DOI] [PubMed] [Google Scholar]
- 21. Bethell CD, Blumberg SJ, Stein REK, Strickland B, Robertson J, Newacheck PW. Taking stock of the CSHCN screener: a review of common questions and current reflections. Acad Pediatr. 2015;15(2):165–176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. McMorrow S, Kenney GM. Recent Trends in Uninsurance Among Children. Washington, DC: The Urban Institute; 2018 [Google Scholar]
- 23. Collins SR, Gunja MZ, Aboulafia GN. U.S. Health Insurance Coverage in 2020: A Looming Crisis in Affordability. Washington, DC: The Commonwealth Fund; 2020 [Google Scholar]
- 24. Lindley LC, Mark BA. Children with special health care needs: impact of health care expenditures on family financial burden. J Child Fam Stud. 2010;19(1): 79–89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Smaldone A, Honig J, Byrne MW. Delayed and forgone care for children with special health care needs in New York State. Matern Child Health J. 2005; 9(2 Suppl):S75–S86 [DOI] [PubMed] [Google Scholar]
- 26. Claxton G, Damico A, Rae M, Young G, McDermott D, Whitmore H. Health benefits in 2020: premiums in employer-sponsored plans grow 4 percent; employers consider responses to pandemic. Health Aff (Millwood). 2020; 39(11):2018–2028 [DOI] [PubMed] [Google Scholar]
- 27. Collins SR, Radley DC, Baumgartner JC. State Trends in Employer Premiums and Deductibles, 2010-2019. Washington, DC: The Commonwealth Fund; 2020 [Google Scholar]
- 28. Chen W, Page TF. Impact of health plan deductibles and health insurance marketplace enrollment on health care experiences. Med Care Res Rev. 2020; 77(5):483–497 [DOI] [PubMed] [Google Scholar]
- 29. Dolan R. Health Policy Brief: High-Deductible Health Plans. Washington, DC: Health Affairs; 2016 [Google Scholar]
- 30. Miller GE, Vistnes JP, Rohde F, Keenan PS. High-deductible health plan enrollment increased from 2006 To 2016, employer-funded accounts grew in largest firms. Health Aff (Millwood). 2018; 37(8):1231–1237 [DOI] [PubMed] [Google Scholar]
- 31. Honberg L, McPherson M, Strickland B, Gage JC, Newacheck PW. Assuring adequate health insurance: results of the National Survey of Children with Special Health Care Needs. Pediatrics. 2005; 115(5):1233–1239 [DOI] [PubMed] [Google Scholar]
- 32. Kreider AR, French B, Aysola J, Saloner B, Noonan KG, Rubin DM. Quality of health insurance coverage and access to care for children in low-income families. JAMA Pediatr. 2016;170(1):43–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Brooks T, Park E, Roygardner L. Medicaid and CHIP Enrollment Decline Suggests the Child Uninsured Rate May Rise Again. Washington, DC: Georgetown University Center for Children and Families; 2019 [Google Scholar]
- 34. Kogan MD, Newacheck PW, Blumberg SJ, et al. State variation in underinsurance among children with special health care needs in the United States. Pediatrics. 2010;125(4):673–680 [DOI] [PubMed] [Google Scholar]
- 35. Kuo DZ, Goudie A, Cohen E, et al. Inequities in health care needs for children with medical complexity. Health Aff (Millwood). 2014;33(12):2190–2198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Parasuraman SR, Anglin TM, McLellan SE, Riley C, Mann MY. Health care utilization and unmet need among youth with special health care needs. J Adolesc Health. 2018;63(4):435–444 [DOI] [PubMed] [Google Scholar]
- 37. Lindly OJ, Chavez AE, Zuckerman KE. Unmet health services needs among US children with developmental disabilities: associations with family impact and child functioning. J Dev Behav Pediatr. 2016;37(9):712–723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Selden TM. Compliance with well-child visit recommendations: evidence from the Medical Expenditure Panel Survey, 2000-2002. Pediatrics. 2006;118(6). Available at: www.pediatrics.org/cgi/content/full/118/6/e1766 [DOI] [PubMed] [Google Scholar]
- 39. Parish SL, Rose RA, Grinstein-Weiss M, Richman EL, Andrews ME. Material hardship in U.S. families raising children with disabilities. Except Child. 2008;75(1):71–92 [Google Scholar]
- 40. Goodman-Bacon A. The Long-Run Effects of Childhood Insurance Coverage: Medicaid Implementation, Adult Health, and Labor Market Outcomes. Cambridge, MA: National Bureau of Economic Research; 2016 [Google Scholar]
- 41. Ghandour RM, Comeau M, Tobias C, et al. Assuring adequate health insurance for children with special health care needs: progress from 2001 to 2009-2010. Acad Pediatr. 2015;15(4): 451–460 [DOI] [PubMed] [Google Scholar]
- 42. Newacheck PW, Houtrow AJ, Romm DL, et al. The future of health insurance for children with special health care needs. Pediatrics. 2009;123(5). Available at: www.pediatrics.org/cgi/content/full/123/5/e940 [DOI] [PubMed] [Google Scholar]
- 43. Szilagyi PG, Dick AW, Klein JD, Shone LP, Zwanziger J, McInerny T. Improved access and quality of care after enrollment in the New York State Children’s Health Insurance Program (SCHIP). Pediatrics. 2004;113(5). Available at: www.pediatrics.org/cgi/content/full/113/5/e395 [DOI] [PubMed] [Google Scholar]
- 44. Alker JC, Kenney GM, Rosenbaum S. Children’s health insurance coverage: progress, problems, and priorities for 2021 and beyond. Health Aff (Millwood). 2020;39(10):1743–1751 [DOI] [PubMed] [Google Scholar]
- 45. Perrin JM, Kenney GM, Rosenbaum S. Medicaid and child health equity. N Engl J Med. 2020;383(27):2595–2598 [DOI] [PubMed] [Google Scholar]
- 46. Perkins J, Agrawal R. Protecting rights of children with medical complexity in an era of spending reduction. Pediatrics. 2018;141(Suppl 3):S242–S249 [DOI] [PubMed] [Google Scholar]