Abstract
Background:
Scarce resource allocation policies vary across the United States. Little is known about regional variation in resource allocation protocols and variation in their application. We sought to evaluate how Covid-19 scarce resource allocation policies vary throughout the Chicago metropolitan area and whether there are differences in policy application within hospitals when prioritizing hypothetical patients who need critical care resources.
Methods:
Two cross-sectional surveys were distributed to Chicago metropolitan area hospital representatives and triage officers. Survey responses and categorical variables are described by frequency of occurrence. Intra- and interhospital variation in ranking of hypothetical patients was assessed using Fleiss’s Kappa coefficients.
Results:
Eight Chicago-area hospitals responded to the survey assessing scarce resource allocation protocols (N = 8/18, response rate 44%). For hospitals willing to describe their ventilator allocation protocol (N = 7), most used the sequential organ failure assessment (SOFA) score (N = 6/7, 86%) and medical comorbidities (N = 4/7, 57%) for initial scoring of patients. A majority gave priority in initial scoring to pre-defined groups (N = 5/7, 71%), all discussed withdrawal of mechanical ventilation for adult patients (N = 7/7, 100%), and a minority had exclusion criteria (N = 3/7, 43%). Forty-nine triage officers from nine hospitals responded to the second survey (N = 9/10 hospitals, response rate 90%). Their rankings of hypothetical patients showed only slight agreement amongst all hospitals (Kappa 0.158) and fair agreement within two hospitals with the most respondents (Kappa 0.21 and 0.25). Almost half used tiebreakers to rank patients (N = 23/49, 47%).
Conclusions:
Although most respondents from Chicago-area hospitals described policies for resource allocation during the COVID-19 pandemic, the substance and application of these protocols varied. There was little agreement when prioritizing hypothetical patients to receive scarce resources, even among people from the same hospital. Variations in resource allocation protocols and their application could lead to inequitable distribution of resources, further exacerbating community distrust and disparities in health.
Keywords: Bioethics, public health, empirical research, survey, health policy, Covid-19
Introduction
Concern about scarcity of resources such as mechanical ventilators during the Coronavirus Disease 2019 (COVID-19) pandemic required United States (US) hospitals to create resource allocation policies in preparation for critical care shortages. Experts proposed multiple ideas for equitably allocating ventilators (Biddison et al. 2018; Daugherty Biddison et al. 2019; Emanuel et al. 2020; Silva 2020; White et al. 2009; Ramachandran et al. 2020; Maves et al. 2020; Truog, Mitchell, and Daley 2020) without consensus. US State resource allocation policies vary widely (Piscitello et al. 2020; Task Force of the Association of Bioethics Program Directors 2020), but differences in these protocols within states or individual cities is not well known. If meaningful differences in scarce resource allocation policies exist within a city or region, this could significantly affect whether a patient is allocated a resource simply based on where they live within the region. This is especially a concern in cities like Chicago where substantial segregation by race and socioeconomic status exists, and variations in resource allocation by location may exacerbate known racial health disparities present prior to and during the COVID-19 pandemic (Chicago Department of Public Health 2021). In addition, little is known about the reliability in implementation of these protocols by those asked to utilize them. Although previous studies have found variability in scarce resource allocation policies across the US (Piscitello et al. 2020), these studies assessed differences between written protocols rather than the accuracy of implementing specific protocols, which may be impacted by triage officer biases or variation in interpreting the protocol’s language. If individual policies cannot be implemented consistently and accurately, this has the potential to cause capricious scarce resource allocation worldwide.
The Illinois Department of Public Health (IDPH) made general recommendations for triage of scarce resources, including ventilators, requesting equity in allocation, but did not offer a specific allocation protocol for how to triage ventilators, deferring this to individual healthcare institutions (Guidelines on Hospital Emergency Preparedness During COVID-19 | IDPH 2020). It is not known whether hospitals chose to follow these general guidelines provided by IDPH. Like other metropolitan areas, Chicago has many hospitals ranging from community hospitals to large tertiary care centers (Illinois Department of Public Health 2020). Often patients receive care at more than one hospital. Large variation in resource allocation – especially critical care resources – amongst hospitals in the same region, could have important consequences, including inequitable treatment of certain populations (Health Equity Considerations and Racial and Ethnic Minority Groups 2021). Furthermore, the principled reasoning behind creating resource allocation policies could be rendered obsolete if patients choose to go a hospital where they knew they would get priority.
There is significant concern that variability in COVID-19 scarce resource allocation policies and their potential implementation at Chicago area hospitals exists, similar to that seen amongst US States, which may lead to inequity in scarce resource distribution. This study aims to evaluate these concerns.
Methods
A cross-sectional survey study was used to evaluate scarce resource allocation protocols at hospitals or hospital systems in and near Chicago, Illinois. This study has two objectives: to evaluate variation among (1) COVID-19 scarce resource allocation policies and (2) triage officers’ rankings of hypothetical patients in the Chicago metropolitan area.
Recruitment of participants and survey design
Two surveys were designed using best practice after completing a literature review (Artino et al. 2014). These surveys were primarily designed by a group of physicians including a palliative medicine physician, a pediatric cardiologist and a pulmonary critical care physician all of whom have experience in ethics and contributed to developing their own hospital resource allocation protocols. Both surveys were piloted by 10 ethicists from 6 different Chicago area hospitals for content and readability prior to being sent to survey participants. Survey participants at each hospital were identified using personal connections through the Chicago Bioethics Coalition, a group of over 50 ethicists in the Chicago-area representing over 20 hospitals, to identify one person at each hospital who contributed to the creation of scarce resource allocation policies. The Chicago metropolitan area was defined as any hospital within a 30-mile radius of the city of Chicago. We chose to utilize surveys to evaluate scarce resource allocation policies rather than actual institutional protocols due to intrahospital legal restrictions that prevented us from obtaining the policies. Institutional review board (IRB) exemption was granted.
Surveys were sent by email during August and September 2020 using REDCap (Harris et al. 2009; Harris et al. 2019). The first survey aimed to evaluate specific details of ventilator and other scarce resource allocation policies. This survey included 53 multiple choice and free-response questions on the initial scoring system, exclusion criteria, initial priority groups, and tiebreakers of allocation protocols. For each hospital, this survey was sent to a physician or ethicist who had access to their respective institution’s ventilator allocation protocol. Surveys did not request information that would identify the source hospital, healthcare system, or respondent. Each hospital was provided a unique link to the first survey and only one response was provided by each hospital.
The second survey evaluated triage officers’ execution of their institution’s resource allocation protocol and was sent to hospitals where a resource allocation policy was known to exist. Using the Chicago Bioethics Coalition, the authors identified one person at Chicago-area institutions where a resource allocation protocol was known to exist and asked that person to distribute the survey to people that the hospital identified to participate in triaging patients (i.e., triage officers). This method was used to maximize the response rate as it allowed the respondents (i.e., triage officers) to remain completely anonymous, even to the authors, all of whom are employed by at least one of the hospitals surveyed. Each hospital representative received a unique survey link to send to its triage officers which allowed us to compare how triage offers within the same institution, using the same policy, would respond to the survey. The survey included 17 multiple choice and free-response questions including a question asking the respondent to rank 6 hypothetical patients from 1–6 (highest to lowest priority) for receiving scarce resources using their own institution’s allocation policy. We created 6 hypothetical patients with variability in criteria that we knew many hospital policies used to distinguish between patients and thereby determine how priority scores were allocated. For each hypothetical patient, age, job description, brief past medical history and current sequential organ failure assessment (SOFA) (Vincent et al. 1996) score were provided (Table 1). A higher SOFA score correlates with higher likelihood of mortality (Vincent et al. 1996). Age and job description were included because some hospital protocols were thought to be likely to use these when determining priority scores or as tiebreakers if two patients were of equal priority. For the hypothetical pediatric patient, several different pediatric prognostic scores found in the literature (Matics and Sanchez-Pinto 2017; Richardson et al. 2001; Pollack, Ruttimann, and Getson 1988; Leteurtre et al. 2006; Schlapbach et al. 2018) were provided along with a mortality estimate since there was more variability among pediatric protocol scoring systems (Piscitello et al. 2020).
Table 1.
Six hypothetical Patients.
| A | 91-year-old retired doctor with a past medical history of coronary artery disease, history of stroke 10 years ago with no residual disease. SOFA: 6 |
| B | 65-year-old retired daycare teacher with a past medical history of poorly controlled diabetes. SOFA: 7 |
| C | 45-year-old ED nurse with active breast cancer (receiving chemotherapy with curative intent) and is currently immunocompromised. SOFA: 11 |
| D | 35-year-old city bus driver with stage IV lung cancer, participating in clinical trial for lung cancer through the medical center where he receives care. SOFA: 12 |
| E | 25-year-old graduate student with hypertension, 30 weeks pregnant. SOFA: 14 |
| F | 12-year-old with a past medical history of hypoxic ischemic encephalopathy resulting in severe cognitive disabilities and severe asthma. she does not speak, is wheelchair bound, and communicates with her family by smiling. her mother is a physician. SOFA: 3, PELOD-2: 8, pSOFA: 5, estimated mortality <5% |
SOFA Sequential Organ Failure Assessment; PELOD-2 Pediatric Logistic Organ Dysfunction-2; Pediatric Sequential Organ Failure Assessment.
Statistical analysis
Survey responses and categorical variables are described by frequency of occurrence. For each hypothetical patient, the median, mean, and modal rank were determined. Because each rater scored 6 patients on an ordinal scale, Fleiss’s kappa coefficients were calculated to assess for agreement among respondents (Fleiss 1971). A kappa of less than or equal to zero indicates no agreement (other than what would be expected by chance) and a kappa of one indicates complete agreement. All analyses were conducted using R version 3.6.1 (The R Foundation for Statistical Computing, Vienna, Austria). All statistical testing was 2-sided with a P-value threshold of < 0.05.
Results
Hospital characteristics
Eight Chicago area hospitals or hospital systems responded to the first survey (N = 8/18, response rate 44%). Nine Chicago-area hospitals had a total of 49 triage officers who responded to the second survey (N = 9/10, hospital response rate 90%). The majority of respondent hospital or hospital systems were private (75%) and academic (100%), and they all trained medical students, residents or fellows (100%). Half had a religious affiliation, and 88% offered clinical trials related to COVID-19 to patients (e-Table 1).
Survey 1: Ventilator allocation protocols
Most respondents (N = 7/8, 88%) reported the creation of a ventilator allocation protocol at their hospital or hospital system that considered adult and pediatric patients. A minority of protocols had exclusion criteria (N = 3/7, 43%) with specific exclusion criteria varying by hospital (e-Table 2). These exclusion criteria remove patients with certain diagnoses from consideration of mechanical ventilation, such as patients with persistent coma or vegetative states or severe burns with less than 10% chance of survival. Most protocols included priority groups in their initial scoring system before tiebreakers are considered (N = 5/7, 71%). These priority groups are defined groups that receive additional priority in the initial scoring system. A majority of hospitals had measures to give priority to pregnant patients (N = 4/7, 57%) and a minority to give priority to healthcare workers (N = 2/7, 29%), other essential workers (N = 1/7, 14%) or families of essential workers (N = 1/7, 14%) (e-Table 3). For hospitals with allocation policies, the initial scoring system used varied, with most utilizing the SOFA score (N = 6/7, 86%) and one using the modified SOFA score (N = 1/7, 14%). Most also utilized medical comorbidities in the initial scoring system (N = 4/7, 57%) (Table 2). Half of the protocols had unique criteria to triage pediatric patients (e-Table 4), with one hospital giving pediatric patients priority over all other patients (e-Table 3). Tiebreakers, the strategy to allocate ventilators when priority levels were the same amongst multiple patients, varied greatly amongst hospitals with some hospitals giving priority to certain groups in a tie, such as younger patients (N = 3/7, 43%), patients who were COVID-19 research subjects (N = 1/7, 14%), or their own hospital system front line workers (N = 1/7, 14%), and most using random allocation as the final tiebreaker (N = 4/7, 57%) (e-Table 5). The method of random allocation was not identified in any of the protocols. All discussed withdrawal of mechanical ventilation for adult patients (N = 7/7, 100%). At these hospitals, ventilator withdrawal would be considered if a shortage occurred, and a new patient came to the hospital with higher likelihood of recovery than a patient who was currently intubated. The method to withdraw ventilators varied by hospital (e-Table 6). No mention of nondiscrimination statements promoting equitable allocation of ventilators was mentioned in any of the protocols.
Table 2.
Ventilator allocation protocol components.
| Initial Scoring System | Exclusion Criteria | Initial Priority Groups | Withdrawal of Mechanical Ventilation for Adult Patients Discussed | Triage Committee Created | Unique Criteria for Pediatric Patients | |
|---|---|---|---|---|---|---|
|
| ||||||
| Hospital 1 | mSOFA | No | Pregnancy | Yes | Yes | No |
| Hospital 2 | No scoring system, did not make a ventilator allocation protocol | N/A | N/A | N/A | N/A | N/A |
| Hospital 3 | SOFA & poor short term prognosis due to comorbidities | Yes | Pregnancy | Yes | Yes | Yes |
| Hospital 4 | SOFA & poor short term prognosis due to comorbidities | No | Pregnancy, healthcare workers, essential workers, families of essential workers | Yes | Yes | No |
| Hospital 5 | SOFA | Yes | Pediatric patients | Yes | Yes | Yes |
| Hospital 6 | SOFA | Yes | No | Yes | Yes | Yes |
| Hospital 7 | SOFA & evaluation of medical comorbidities | No | No | Yes | Yes | Yes |
| Hospital 8 | SOFA & evaluation of medical comorbidities | No | Pregnancy, healthcare workers | Yes | No | No |
mSOFA Modified Sequential Organ Failure Assessment; SOFA Sequential Organ Failure Assessment.
Creation of ventilator allocation protocol
Protocols were created by multidisciplinary groups at each hospital (e-Table 7). Only two hospitals included community input in formation of the protocol (N = 2/7, 29%) and a minority had a plan in place to discuss their approach to allocate ventilators with the public (N = 3/7, 43%). No institution’s protocol was publicly available and few (N = 3/4, 43%) had a plan in place to explain the triage mechanism to the public. Only two hospitals rehearsed use of their protocol, e.g., doing trial runs with hypothetical patients (N = 2/7, 29%), and no hospital had used their protocol in practice (e-Table 7). Almost all protocols created a triage committee to allocate ventilators (N = 6/7, 86%) with the majority of triage officers restricted from direct patient care of patients needing scarce resources (N = 4/7, 57%). The composition of the triage committees varied by hospital, with some recommending inclusion of a critical care physician (N = 5/7, 71%), an ethicist (N = 4/7, 57%) and a nurse (3/7, 43%). The plan to provide information to triage committees varied by hospital with some hospitals blinding certain information such as patient name, race and ethnicity (N = 2/7, 29%). Some hospital policies recommended providing data to the triage committee through the medical record (N = 2/7, 29%) while others recommended that the primary medical team provide the data (N = 2/7, 29%). In addition to ventilator allocation policies, most hospitals (N = 6/8, 75%) created other scarce resource policies. Some of these policies were actually used in practice, such as allocation strategies for Remdesivir (N = 2/7, 29%) and extracorporeal membrane oxygenation (N = 2/7, 29%).
Survey 2: Variation in allocation amongst hospital protocols
Forty-nine triage officers from 9 hospitals responded to the second survey. One respondent indicated that she/he had ranked the hypothetical patients at random. This survey was removed from analysis post hoc because the research team felt it was equivalent to leaving the ranking question blank. The largest number of responses from any one hospital was 20. Twenty-nine respondents were physicians (59%), 8 were nurses or advanced practice nurses (16%), 4 were hospital administrators (8%), and 8 identified as ethicists (16%). Almost all respondents reported being familiar or very familiar with their hospital resource allocation protocol (N = 43/49, 88%) and noted that their institution’s policy provided sufficient guidance to rank the given hypothetical patients (N = 43/49, 88%). Few respondents thought that their institution’s policy disadvantaged any group (N = 5/49, 10%) and listed racial minorities (N = 3/49, 6%), low socioeconomic status (N = 3/49, 6%), elderly age (N = 4/49, 8%), people with comorbidities (N = 1/49, 2%), people with disabilities (N = 1/49, 2%), and women (N = 1/49, 2%) as the groups affected. Most respondents agreed with their institution’s policy to give priority to specific groups such as healthcare workers, pregnant patients or pediatric patients (N = 38/49, 78%) and only a minority stated that their institution did not give priority to specific groups (N = 10/49, 20%). Only 1 respondent disagreed with how his/her institution gave priority to certain groups.
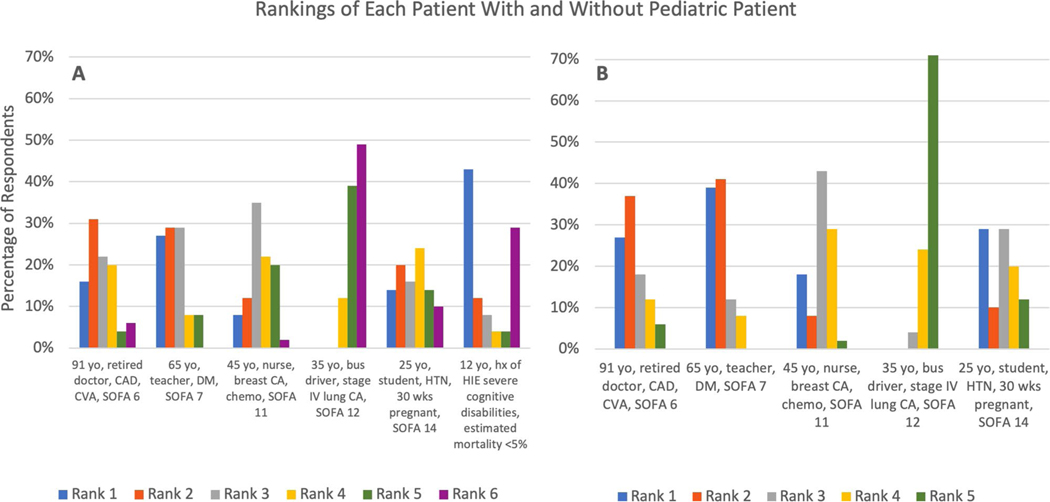
Ranking of six theoretical patients
There was pronounced variation amongst respondents’ ranking of the six hypothetical patients (Figure 1). Patient A, a 91-year-old, retired doctor with coronary artery disease and history of a stroke 10 years ago, and SOFA score of 6 was most frequently ranked second (31%). Patient B, a 65-yearold retired daycare teacher with poor controlled diabetes and SOFA 7 was most frequently ranked second and third (29% of the time). Patient C, a 45-year-old ED nurse with active breast cancer, receiving chemotherapy and immunocompromised with SOFA 11 was most often ranked third (35% of the time). Patient D, a 35-year-old, city bus driver with stage IV lung cancer, participating in a clinic trial with SOFA 12 was most often ranked last (49% of the time). Patient E, a 25-year-old graduate student with hypertension and 30-weeks pregnant with SOFA 14 was most often ranked fourth (24% of the time). Finally, patient F, a 12-year-old with hypoxic ischemic encephalopathy, severe cognitive disabilities, who communicates only by smiling, with asthma and estimated mortality <5%, was most often ranked first (43% of the time). The mean and median rank for each patient is reported in Table 3.
Figure 1.
Variation in how all respondents ranked the hypothetical patients. (yo = year old, CAD = coronary artery disease, CVA = cerebral vascular accident, SOFA = sequential organ failure assessment, CA = cancer, chemo = chemotherapy, HTN = hypertension, wks = weeks, HIE = hypoxic ischemic injury.).
Table 3.
Mean and median rank for each hypothetical patient with and without pediatric patient F.
| With Pediatric Patient Included |
Without Pediatric Patient |
|||
|---|---|---|---|---|
| Patient | Mean | Median | Mean | Median |
|
| ||||
| A | 2.84 | 3 | 2.35 | 2 |
| B | 2.43 | 2 | 1.9 | 2 |
| C | 3.41 | 3 | 2.88 | 3 |
| D | 5.37 | 5 | 4.67 | 5 |
| E | 3.35 | 3 | 2.78 | 3 |
| F | 3 | 2 | N/A | N/A |
Patient F, the pediatric patient, was excluded from entering the allocation protocol according to some respondents due to the patient’s described encephalopathy and therefore, given lowest priority. Other respondents excluded this patient from their allocation protocol because she was a pediatric patient and therefore gave this patient the highest priority. Figure e-1 shows the distribution of ranking for the pediatric patient with most respondents ranking this patient either 1 or 6. After seeing this wide variation in ranking the pediatric patient, a post-hoc sub analysis was done excluding patient F. When patient F was removed, and the other patients re-ordered as though F had not been a choice, there was slightly less variability (Figure 1). Agreement among respondents using Kappa was 0.095 when the pediatric patient was included, and 0.158 when the pediatric patient was excluded (0 = completely random, 1 = fully in agreement) consistent with slight agreement among respondents. Kappa for each rank position when the pediatric patient was excluded was: rank 1 = 0.078, rank 2 = 0.156, rank 3 = 0.090, rank 4 = 0.018, and rank 5 = 0.470 showing that the most agreement was for rank 5 as patient D was most consistently ranked fifth.
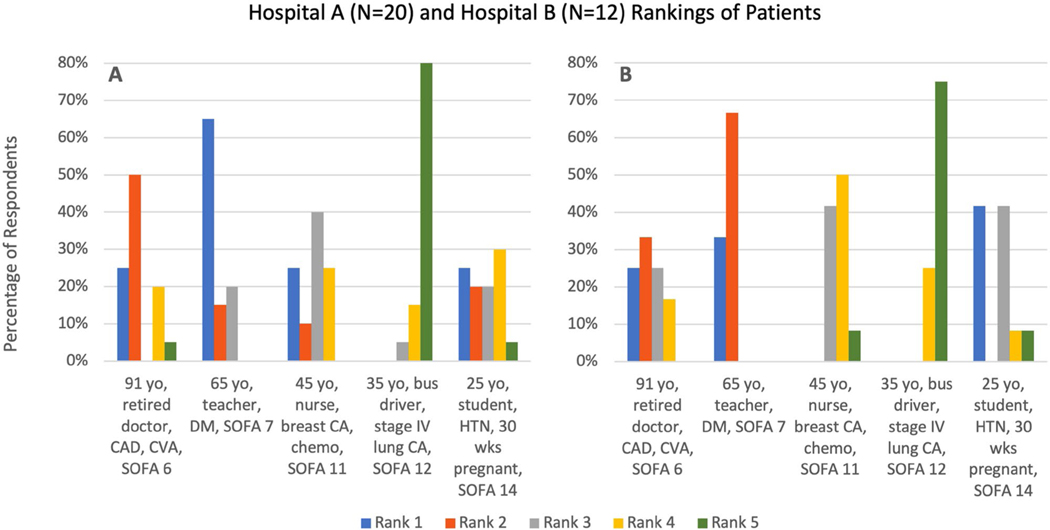
In a sub-analysis, data from the 2 hospitals with the most respondents (N = 20 and N = 12) demonstrated that even within the same hospital, there was little agreement amongst respondents (Figure 2). Kappa was 0.21 and 0.25 respectively, consistent with only fair agreement amongst respondents.
Figure 2.
Variation in ranking of the hypothetical patients by respondents from hospitals A and B. (yo = year old, CAD = coronary artery disease, CVA = cerebral vascular accident, SOFA = sequential organ failure assessment, CA = cancer, chemo = chemotherapy, HTN = hypertension, wks = weeks.).
Almost half of the respondents reported using tiebreakers to assist with the rankings (N = 23/49, 47%) and listed using tiebreakers most often between patients C and E (N = 7/23, 30%) and patients A and B (N = 6/23, 26%). Ties between three or more patients were identified 22% of the time. Respondents used the following criteria to break the ties: age, greatest likelihood of positive outcome, reciprocity, healthcare worker, pregnancy, and lottery.
Discussion
Ventilator allocation policies varied widely amongst hospitals in the Chicago metropolitan area. Most hospitals used SOFA in their initial scoring system, and only half also utilized assessment of medical comorbidities in their scoring system. Most protocols gave priority to certain groups such as pregnant patients or healthcare providers. Few protocols were created with community input, and no protocol was available for public review. There was also significant variation in the implementation of resource allocation protocols. There was only slight agreement on the ranking of hypothetical patients among all triage officers, and within a subanalysis of two hospitals there was only fair agreement among triage officers. Almost half of triage officer respondents reported using tiebreakers to assist with the rankings.
Although the IDPH Guidelines on Hospital Emergency Preparedness During COVID-19 made general recommendations about scarce resource allocation guidelines, the data revealed that Illinois hospital protocols do not uniformly reflect these recommendations. The IDPH recommended hospitals make crisis standards of care processes transparent, however no hospital in this study allowed their ventilator allocation policies to be available for public review (Guidelines on Hospital Emergency Preparedness During COVID-19 | IDPH 2020). The IDPH guidelines also recommend equity in allocation that does not discriminate based on race, ethnicity, and socioeconomic status, however the majority of ventilator allocation policies utilized medical comorbidities which may lower priority for people of color and lower socioeconomic status. No protocols introduced efforts to reduce the impact of baseline structural inequities as some experts and ethicists now support (White and Lo 2021). The IDPH guidelines recommend creating a triage team consisting of an infectious disease physician, nursing staff, hospital administration and a medical ethicist. Survey results showed that although 86% of hospitals created a triage team, only 29% of policies included the members recommended by IDPH.
Seventy-one percent of surveyed Chicago area hospitals had initial priority groups, much higher than the 23% of US state ventilator allocation guidelines which recommend priority groups (Piscitello et al. 2020). Of the hospitals with ventilator allocation guidelines, 43% gave priority to prioritize healthcare workers either in the initial scoring system (as a “priority group”) or in tiebreaker situations. We speculate that individual hospitals might feel a higher obligation to prioritize members of their own medical staff whom they are directly responsible for when compared to the creators of US state guidelines. Some hospitals prioritized multiple groups including one hospital whose protocol gives priority to pregnant patients, healthcare workers, essential workers, and families of essential workers. With so many prioritized groups, there is a concern that those not in a priority group may have inequitable access to mechanical ventilation if a shortage occurs (New York State Task Force on Life and the Law and the Law New York State Department of Health 2015).
Although no Chicago hospital ventilator allocation protocol was identical to any US state guideline, many showed similarities to certain states guidelines. These similarities may reflect the need by Chicago area hospitals to reference protocols from other states’ protocols for guidance since Illinois did not provide a specific state-wide allocation protocol for use. For example, two Chicago-area hospital protocols chose to use SOFA score in their initial allocation scoring system without incorporating medical comorbidities, similar to the New York State allocation policy (New York State Task Force on Life and the Law; New York State Department of Health 2015). Two other hospitals chose to use SOFA score plus evaluation of poor short-term prognosis in their initial priority score for patients, similar to the revised Pennsylvania state proposal for scarce resource allocation (Pennsylvania Department of Health 2021). Because Chicago-area hospitals did not conform to one state guideline, the resulting allocation protocols differed even amongst hospitals in close proximity to one another who may care for similar patient populations.
These results have significant implications. If critical care resources in the Chicago region are scarce, patients might, to the extent they are able, seek out hospitals where they would receive higher priority. For example, if pregnant patients or healthcare workers knew they would receive higher priority at a specific hospital, they may preferentially seek out that hospital. This could create an imbalance in hospital usage that further exacerbates resource scarcity within a hospital or healthcare system. Perhaps this is unlikely given that lack of transparency in hospital allocation protocols, as this study found that no allocation protocols were publicly available. Nevertheless, if groups within communities share experiences and unveil these differences, this could lead to a strain on some hospitals’ resources while others in the same region have excess supply.
When people require hospitalization, they do not expect to be prioritized for resources differently depending on the hospital at which they are treated. Most people rely on an ambulance to take them to the nearest hospital without thought to hospital triage protocols. However, if differences in prioritization became known in the community, those with transportation and monetary resources and who are not constrained by health insurance mandates, would be able to choose a hospital where they would get prioritized, thereby exacerbating current health disparities. Furthermore, our study results showed that the internal application of any individual hospital’s policy to hypothetical patients was also varied even though a protocol is meant to prevent arbitrary allocation. When there is significant variation in the application of a protocol, opportunities for bias, racism, and further inequalities abound. To help avoid the variable application of a resource allocation protocol, hospitals should be required to run mock drills where triage officers apply the protocol to hypothetical patients, and the hospital can check for inconsistencies in application. Mock drills are also essential to evaluate how discussions about ventilator withdrawal from a lower priority patient might occur, and whether medical staff would be willing to withdraw a ventilator from a patient in order to have enough for higher priority patients.
Results from the second survey revealed that respondents agreed most about giving the 35-year-old city bus driver who had stage IV lung cancer and a SOFA score of 12 low priority. This patient was ranked last over 70% of the time (Figure 1), showing that the concept of saving the most lives is highly reflected in most allocation protocols and that utilitarian principles underlie many of these protocols. Other than agreeing that the patient with stage IV lung cancer should be given lowest priority, however, there was little agreement among respondents for how hypothetical patients should be ranked for priority, and almost half of all respondents resorted to tiebreakers in order to rank the patients. The frequent use of tiebreakers suggests that primary scores do not adequately separate patient groups which has important ethical implications as there is some concern that the order of tiebreakers may be arbitrary and not justified by rigorous ethical analysis due to the significant variability in the order of tiebreakers observed in this study and US ventilator allocation guidelines (Piscitello et al. 2020).
Although there is data to support scarce resource policies may not contribute to racial or ethnic disparities in allocation (Gershengorn et al. 2021), this data is limited in application to Chicago as it does not evaluate the priority groups or tiebreakers used by individual hospitals in Chicago which likely would lead to differences in resource allocation. There remains significant concern that racial and ethnic minorities living in the Chicago area would be more affected by scarce resource allocation policies as Chicago has a significant proportion of Black and Latinx residents who are more likely to be hospitalized and die from COVID-19 (Risk for COVID-19 Infection, Hospitalization, and Death by Race/Ethnicity 2021).
Other findings from our results which may contribute to public distrust about inequitable allocation of scarce resources include the complete lack of transparency by all hospitals to share their allocation policies with the public, and limited inclusion of the community in creation of these policies (Upshur 2002). The public has good reason to be concerned about inequitable allocation of scarce resources, as has been well documented in the distribution of COVID-19 vaccines (Pandemic’s Racial Disparities Persist in Vaccine Rollout 2021). Given the existing mistrust of healthcare systems among certain communities, exacerbated by differences in disease burden and mortality among Black, Latinx, and Native American populations during the COVID-19 pandemic (Webb Hooper, Nápoles, and Pérez-Stable 2020; Chicago Department of Public Health 2020), avoiding further erosions in confidence is crucial. A potential solution is to bolster regional guidance for resource allocation protocols based on working groups with representation from local hospitals.
We acknowledge several study limitations. First, we did not have a robust survey response rate. For Survey 1, we speculate that the lower response rate may reflect reluctance from some hospitals to share information about their protocols or the reality that some hospitals did not have a protocol (Task Force of the Association of Bioethics Program Directors 2020). Despite the sample size, we still show important variation amongst ventilator allocation protocols. For Survey 2, triage officer variation could only be described within two hospitals due to the low number of respondents from other hospitals. This could have occurred because some hospitals actually had fewer triage officers. Unfortunately, we do not know how many triage officers at each hospital were invited to participate because we relied on a representative from each hospital to distribute the survey to their triage officers in order to preserved anonymity of respondents. Second, these data may not reflect the current resource allocation protocols as many hospitals are continually updating them as issues of health disparities and difficulties with applying the protocols are raised (White and Lo 2021), and as knowledge about COVID-19 treatments increases. Third, we did not ask whether nondiscrimination statements promoting equitable allocation of ventilators were included in any of the protocols. Fourth, these results may not be generalizable to other metropolitan areas where increased state guidance was provided to hospitals when allocation policies were developed (Piscitello et al. 2020; Interim Pennsylvania Crisis Standards of Care for Pandemic Guidelines 2020). Fifth, some hospital protocols may provide triage officers with additional patient data not provided in the descriptions of the hypothetical patients when determining patient priority. Finally, triage groups or committees may work together to determine patient priority and therefore, discussion and elaboration of patient data may make their choices more internally consistent.
Conclusion
Ventilator allocation policies varied widely amongst hospitals in the Chicago metropolitan area and application of protocols differed among people asked to implement them. The potential impact of such differences is unequal distribution of resources which further exacerbates community distrust and disparities in health. Efforts such as collaboration among hospitals serving the region to more closely align their resource allocation protocols, and simulated application of protocols by triage officers may help minimize these variations, and the resulting inequities.
Funding
The author(s) reported there is no funding associated with the work featured in this article.
Dr. Parker reported receiving grants from the National Heart, Lung, and Blood Institute outside the submitted work. Dr. Michelson reported receiving grants from the National Institute for Diabetes and Digestive and Kidney Disease and the National Palliative Care Research Center outside the submitted work.
Footnotes
Disclosure statement
No other potential conflict of interest was reported by the authors.
Supplemental data for this article can be accessed online at https://doi.org/10.1080/23294515.2021.1983667.
References
- Antommaria AHM, Gibb TS, McGuire AL, Wolpe PR, Wynia MK, Applewhite MK, Caplan A, Diekema DS, Hester DM, Lehmann LS, Task Force of the Association of Bioethics Program Directors, et al. 2020. Ventilator triage policies during the COVID-19 pandemic at U.S. hospitals associated with members of the association of bioethics program directors. Annals of Internal Medicine 173 (3):188–94. doi: 10.7326/M20-1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Artino AR, La Rochelle JS, Dezee KJ, and Gehlbach H. 2014. Developing questionnaires for educational research: AMEE Guide No. 87. Medical Teacher 36 (6):463–74. doi: 10.3109/0142159X.2014.889814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biddison ELD, Gwon HS, Schoch-Spana M, Regenberg AC, Juliano C, Faden RR, and Toner ES. 2018. Scarce resource allocation during disasters: A mixed-method community engagement study. Chest 153 (1):187–95. doi: 10.1016/j.chest.2017.08.001. [DOI] [PubMed] [Google Scholar]
- Chicago Department of Public Health. 2020. Latest Data. Published December 17, 2020. Accessed December 17, 2020. https://www.chicago.gov/city/en/sites/covid-19/home/latest-data.html [Google Scholar]
- Chicago Department of Public Health. 2021. Data Brief: The State of Health for Blacks in Chicago. Published online June 2021. Accessed August 13, 2021. https://www.chicago.gov/content/dam/city/depts/cdph/CDPH/Healthy%20Chicago/CDPH_BlackHealth7c_DIGITAL.pdf [Google Scholar]
- Daugherty Biddison EL, Faden R, Gwon HS, Mareiniss DP, Regenberg AC, Schoch-Spana M, Schwartz J, Toner ES. 2019. Too many patients…A framework to guide statewide allocation of scarce mechanical ventilation during disasters. Chest 155 (4):848–54. doi: 10.1016/j.chest.2018.09.025. [DOI] [PubMed] [Google Scholar]
- Emanuel EJ, Persad G, Upshur R, Thome B, Parker M, Glickman A, Zhang C, Boyle C, Smith M, and Phillips JP. 2020. Fair allocation of scarce medical resources in the time of Covid-19. The New England Journal of Medicine 382 (21):2049–55. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- Fleiss JL. 1971. Measuring nominal scale agreement among many raters. Psychological Bulletin 76 (5):378–82. doi: 10.1037/h0031619. [DOI] [Google Scholar]
- Gershengorn HB, Holt GE, Rezk A, Delgado S, Shah N, Arora A, Colucci LB, Mora B, Iyengar RS, Lopez A, et al. 2021. Assessment of disparities associated with a crisis standards of care resource allocation algorithm for patients in 2 US hospitals during the COVID-19 pandemic. JAMA Network Open 4 (3):e214149. doi: 10.1001/jamanetworkopen.2021.4149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guidelines on Hospital Emergency Preparedness During COVID-19 | IDPH. 2020. Accessed October 31, 2020. https://www.dph.illinois.gov/covid19/guidelines-emergency-preparedness-hospitals-during-covid-19 [Google Scholar]
- Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J, REDCap Consortium, et al. 2019. The REDCap consortium: Building an international community of software platform partners. Journal of Biomedical Informatics 95:103208. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, and Conde JG. 2009. Research electronic data capture (REDCap)-a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics 42 (2):377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Equity Considerations and Racial and Ethnic Minority Groups. 2021. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html [Google Scholar]
- Illinois Department of Public Health. 2020. Accessed December 3, 2020. https://www.dph.illinois.gov/data-statistics [Google Scholar]
- Interim Pennsylvania Crisis Standards of Care for Pandemic Guidelines. 2020. Published online April 2020. https://www.health.pa.gov/topics/Documents/Diseases%20and%20Conditions/COVID-19%20Interim%20Crisis%20Standards%20of%20Care.pdf [Google Scholar]
- Leteurtre S, Duhamel A, Grandbastien B, Lacroix J, and Leclerc F. 2006. Paediatric logistic organ dysfunction (PELOD) score. The Lancet 367 (9514):897. doi: 10.1016/S0140-6736(06)68371–2. [DOI] [PubMed] [Google Scholar]
- Matics TJ, and Sanchez-Pinto LN. 2017. Adaptation and validation of a pediatric sequential organ failure assessment score and evaluation of the sepsis-3 definitions in critically ill children. JAMA Pediatrics 171 (10):e172352. doi: 10.1001/jamapediatrics.2017.2352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maves RC, Downar J, Dichter JR, Hick JL, Devereaux A, Geiling JA, Kissoon N, Hupert N, Niven AS, King MA, et al. 2020. Triage of scarce critical care resources in COVID-19 an implementation guide for regional allocation: An expert panel report of the task force for mass critical care and the American College of Chest Physicians. Chest 158 (1):212–25. doi: 10.1016/j.chest.2020.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- New York State Task Force on Life and the Law and the Law New York State Department of Health. 2015. Ventilator Allocation Guidelines. Published online November 2015. Accessed March 29, 2020. https://www.health.ny.gov/regulations/task_force/reports_publications/docs/ventilator_guidelines.pdf [Google Scholar]
- New York State Task Force on Life and the Law; New York State Department of Health. 2015. Ventilator allocation guidelines. Published November 2015. Accessed April 20, 2021. https://www.health.ny.gov/regulations/task_force/reports_publications/docs/ventilator_guidelines.pdf [Google Scholar]
- Pandemic’s Racial Disparities Persist in Vaccine Rollout. 2021. https://www.nytimes.com/interactive/2021/03/05/us/vaccine-racial-disparities.html#methodology. [Google Scholar]
- Pennsylvania Department of Health. 2021. Ethical Allocation Framework for Emerging Treatments of COVID-19. https://www.health.pa.gov/topics/disease/coronavirus/Pages/Guidance/Ethical-Allocation-Framework.aspx [Google Scholar]
- Piscitello GM, Kapania EM, Miller WD, Rojas JC, Siegler M, and Parker WF. 2020. Variation in ventilator allocation guidelines by US state during the coronavirus disease 2019 pandemic: A systematic review. JAMA Network Open 3 (6):e2012606. doi: 10.1001/jamanetworkopen.2020.12606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollack MM, Ruttimann UE, and Getson PR. 1988. Pediatric risk of mortality (PRISM) score. Critical Care Medicine 16 (11):1110–6. doi: 10.1097/00003246-19881100000006. [DOI] [PubMed] [Google Scholar]
- Ramachandran P, Swamy L, Kaul V, and Agrawal A. 2020. A national strategy for ventilator and ICU resource allocation during the coronavirus disease 2019 pandemic. Chest 158 (3):887–9. doi: 10.1016/j.chest.2020.04.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson DK, Corcoran JD, Escobar GJ, and Lee SK. 2001. SNAP-II and SNAPPE-II: Simplified newborn illness severity and mortality risk scores. Journal of Pediatrics 138 (1):92–100. doi: 10.1067/mpd.2001.109608. [DOI] [PubMed] [Google Scholar]
- Risk for COVID-19 Infection, Hospitalization, and Death by Race/Ethnicity. 2021. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html [Google Scholar]
- Schlapbach LJ, Straney L, Bellomo R, MacLaren G, and Pilcher D. 2018. Prognostic accuracy of age-adapted SOFA, SIRS, PELOD-2, and qSOFA for in-hospital mortality among children with suspected infection admitted to the intensive care unit. Intensive Care Medicine 44 (2):179–88. doi: 10.1007/s00134-017-5021-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva DS. 2020. Ventilators by lottery: The least unjust form of allocation in the coronavirus disease 2019 pandemic. Chest 158 (3):890–1. doi: 10.1016/j.chest.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Truog RD, Mitchell C, and Daley GQ. 2020. The toughest triage - allocating ventilators in a pandemic. New England Journal of Medicine 382 (21):1973–5. doi: 10.1056/NEJMp2005689. [DOI] [PubMed] [Google Scholar]
- Upshur REG. 2002. Principles for the justification of public health intervention. Canadian Journal of Public Health = Revue Canadienne de Sante Publique 93 (2):101–3. doi: 10.1007/BF03404547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, Reinhart CK, Suter PM, and Thijs LG. 1996. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Medicine 22 (7):707–10. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- Webb Hooper M, Nápoles AM, and Pérez-Stable EJ. 2020. COVID-19 and racial/ethnic disparities. JAMA 323 (24):2466–7. doi: 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White DB, Katz MH, Luce JM, and Lo B. 2009. Who should receive life support during a public health emergency? Using ethical principles to improve allocation decisions. Annals of Internal Medicine 150 (2):132–8. doi: 10.7326/0003-4819-150-2-200901200-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White DB, and Lo B. 2021. Mitigating inequities and saving lives with ICU triage during the COVID-19 pandemic. American Journal of Respiratory and Critical Care Medicine 203 (3):287–95. doi: 10.1164/rccm.202010-3809CP. [DOI] [PMC free article] [PubMed] [Google Scholar]