Abstract
Postural orthostatic tachycardia syndrome (POTS) is a form of dysautonomia that’s characterised by an abnormal heart rate response to a positional change. A 50-year-old female presented with lightheadedness, palpitation, and neck pain for 3 years. Lightheadedness and palpitation occurred when shifting from a prolonged seated or lying position. Standing radiographs showed spinal misalignment with cervical kyphosis and thoracic scoliosis. Continuous static stress on these minor variants could aggravate biomechanical and autonomic disorder like POTS. After ruling out cardiovascular, neurological, or vestibular pathophysiology, a multicomponent treatment approach was adopted including the use of thermal ultrasound therapy, cervical and thoracic spinal manipulation, and intermittent motorized cervicothoracic traction to manage her neck pain complaints. Following 3 months of regular treatment, the patient reported a full resolution of neck pain, dizziness, and POTS. At 12-month follow-up, all radiographic metrics showed improvement, including improvement of cervical alignment and thoracic curvature. POTS is a prevalent, under-diagnosed dysautonomia. This study might arouse the alertness of clinicians that symptoms related to POTS may be erroneously attributed to other neuro-cardiovascular disorders.
Keywords: Chiropractic manipulation, lightheadedness, palpitation, postural orthostatic tachycardia syndrome
Introduction
Postural orthostatic tachycardia syndrome (POTS) is a form of chronic dysautonomia causing an abnormal heart rate response to a positional change. Current diagnostic criteria require a heart rate (HR) increment of 30 beats/min or HR >120 beats/min in the first 10 min of standing, in the absence of orthostatic hypotension, and associated with orthostatic intolerance.[1] POTS symptoms are lightheadedness, palpitations, and tremor. POTS is also associated with headaches and neck pain as the blood is not getting to the muscles and brain. Even activities of daily living such as taking a bath or housekeeping work may significantly increase symptoms, resulting in debilitating symptoms, which has substantial functional and economic consequences.[2]
The multiple factors like moderate autonomic dysfunction, increased sympathetic tone, inadequate venous return or excessive blood venous pooling, and severe deconditioning may be responsible for POTS symptoms.[1] The mechanisms for migraine, chronic pain, and POTS symptomatology are complex and overlapped.[3] This article will help readers gain a better understanding of POTS and will assist primary care practitioners in managing it effectively. This case report was prepared with the patient’s written informed consent to publish the case details and accompanying images. IRB approval is not required due to the retrospective nature of the chart review.
Case Report
A 50-year-old female investment banker sought chiropractic attention for the complaint of intermittent headaches and neck pain. Lightheadedness and palpitation were elicited by moving from seated to standing position, which usually lasted 10 min. She sometimes had difficulty thinking and noticed an association between her lightheadedness and neck pain in the past 3 years. There was no history of trauma or auditory or visual complaints. Her previous neuro-otological and cardiologic examinations excluded otological, neurological, and orthostatic hypotension disorders. She was diagnosed with anxiety and panic attacks due to work stress, and treated with psychiatric medications with no improvement. She also tried acupuncture, physiotherapy exercise, medications like salt tablets, fludrocortisone, pyridostigmine, midodrine, and a beta blocker for control of symptoms, but they were not long lasting. She then sought chiropractic rehabilitation for neck pain and dizziness.
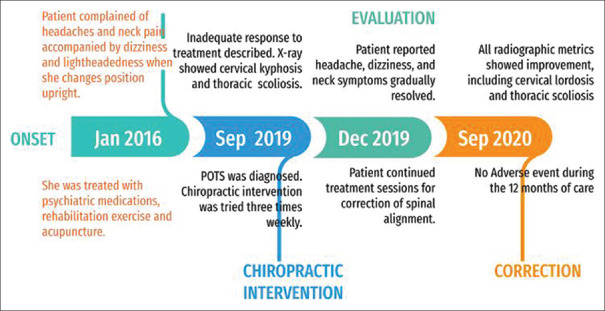
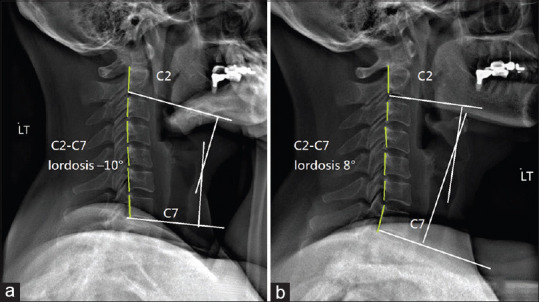
The patient initially presented with a guarded neck. She reported that the intensity of her neck pain and headache was a 5 on a 0–10 numeric pain rating scale. According to the Dizziness Handicap Inventory (DHI) questionnaire, the patient scored 46/100 (mild: <30; moderate: 31–60; and severe: >60). The protective muscle spasm around the neck was observed as a protective mechanism to limit her movement. Muscular hypertonicity was palpated at bilateral upper trapezius, sternocleidomastoid, levator scapula, and rhomboid muscles. Intersegmental joint restriction was identified at C1-2-3, C5-6, C7-T3 segments. Her cervical range of motion was restricted to 30° in passive extension (normal: >60°) and to 70° in bilateral passive rotations (normal: >80°). Her laboratory profiles were normal, but the head-up tilt table test was positive for POTS. Lateral cervical radiograph [Figure 1] revealed a straightened cervical curvature. Global cervical lordosis, defined as Cobb’s angle between C2 and C7 inferior endplates, was –5°. Thoracic image [Figure 2] indicated uneven shoulders level and mild thoracic scoliosis of Cobb’s angle T5-12 12°. After a careful exclusion of other neurological and vestibular diseases, the patient was diagnosed with POTS on the basis of the association between her neck pain, dizziness, mechanical neck dysfunction, and a positive head-up tilt table test.
Figure 1.
Cervical alignment comparison using sagittal radiographs in neutral position. (a) Using Cobb angle (white lines), the C2-C7 spine’s global curvature was initially determined to be –5°, indicating a reversed cervical lordosis. (b) At a 12-month follow-up, the cervical lordosis was corrected by 25° (–5° vs. 20°) using the C2-C7 spine Cobb angle
Figure 2.
Thoracic alignment comparison using anterior–posterior radiographs in neutral position. (a) Tilting of the neck to the left and uneven shoulders (hollow arrows); mild thoracic scoliosis of Cobb’s angle T5-12 12°. (b) At a 12-month follow-up, the thoracic Cobb’s angle was corrected by 5° (12° vs. 7°); and the central sacral vertical line (CSVL) assessment showed significant improvement of spinal scoliosis of coronal balance
Chiropractic rehabilitation included spinal manipulation of the restricted cervical segments and thermal ultrasound therapy to alleviate neck stiffness and restore normal joint mobility, as well as intermittent motorized traction of the cervicothoracic spine to increase intervertebral spaces and decompress neural impingement. Rehabilitation treatments were planned three times a week for 3 months. From the second week on, the patient reported that her pain and dizziness gradually improved and resolved completely within 4 weeks. Near the end of treatment schedules, the majority of neck mobility was regained. The patient’s neck pain decreased from 5/10 to 0/10 on the numeric pain rating scale as a result of treatment. The DHI score decreased from 46 to 0 in this case. For the next 9 months, she continued to receive weekly maintenance treatment aimed at restoring spinal instability. A follow-up radiograph revealed improved cervical and thoracic alignment and curvature. In comparison to the initial image, the cervical lordosis was corrected by 25° (normal is 31°–40°) from -5° to 20° [Figure 1b]; and thoracic scoliosis was corrected by 5° from 12° to 7° [Figure 2b]. The patient was re-evaluated at the 24-month visit and remained symptom-free. The patient reported no adverse events associated with the treatment. For a summary timeline of events, please see Figure 3.
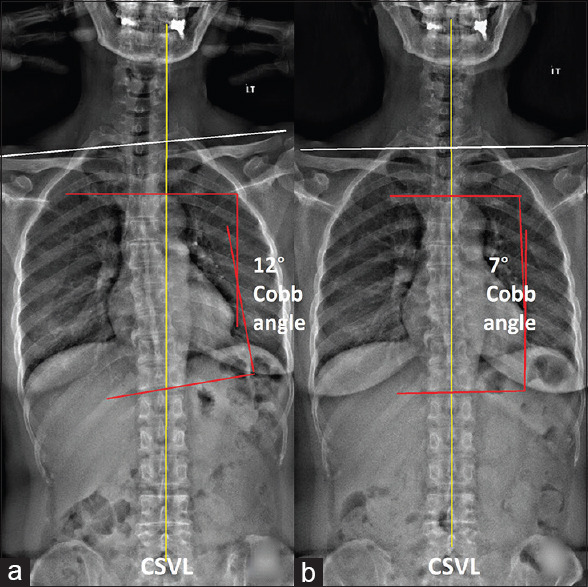
Figure 3.
Clinical timeline of the presenting case
Discussion
As many disease entities can be confused with POTS, it is a syndrome that needs to be characterized over time and with reproducibility.[4] The current evaluation of POTS focuses on confirming the diagnosis, identifying co-morbid illnesses, and ruling out conditions that could cause or mimic the syndrome.[5] However, no single set of criteria is universally accepted by the healthcare community, although many diagnostic criteria have been developed characterizing POTS.[4] In addition, the great majority of clinicians are unfamiliar with or have received little training in assessing and managing the POTS,[2] which often delays the diagnosis and care. Lastly, although numerous medications are frequently used to treat POTS symptoms, no medications are officially approved for POTS by Food and Drug Administration, and the evidence for these medications used to treat POTS is limited.[5]
As POTS is a chronic condition of autonomic nervous system (ANS) disorder,[2] the pathophysiology is completely unknown and heterogeneous.[5] Poor venous return may be a result of impaired vasoconstriction secondary to a number of factors and concurrent clinical syndromes. Clinical management focuses on symptom care. The cervical spine harbors the cervical ganglia, which are the paravertebral ganglia of the sympathetic nervous system. Cervical spine degeneration might cause compression of spinal canal and irritation of the autonomic nervous system.[6] A cohort study (comprised 22,236 subjects with CS vs. 22,236 matched controls) demonstrated that patients with cervical spondylosis (CS) have increased risk of arrhythmia. The overall incidence density rates of arrhythmia were 11.1 and 3.91 per 1,000 person-years in the case and control groups, respectively.[6]
Spinal adjustment has been found to be effective in treating headache associated with autonomic dysfunctions and achieved long-lasting results.[7] The study of Lin et al.[6] supported the use of rehabilitation to protect against future arrhythmias. Manipulative therapeutic impact on parasympathetic nervous system output was found to be specific and sensitive to effector organ and patients who suffer with pain.[8] By using heart rate variability analysis, chiropractic care in a clinical study was found to be effective in regulating both sympathetic and parasympathetic activities.[9] Therefore, it is logical to see the biomechanics and neurological improvement under chiropractic rehabilitation on patients with POTS.
In a retrospective chart review of 144 patients with POTS,[10] 70% improved or had resolution of symptoms following appropriate treatment, but in patients who did not respond well, it required multidisciplinary experts with a variety of approaches. Primary care physicians have a key role in providing detailed diagnosis and sourcing better treatment for their patients. The finding of this study might arouse the alertness of physicians that neck pain is likely associated with arrhythmia, especially those who had symptoms of autonomic nervous dysfunction. Patients can suffer from both musculoskeletal pain and autonomic nervous dysfunction, and will have on-going shared management between family physicians and secondary or tertiary care practitioners. Multidisciplinary care allows patients to receive coordinated support and comprehensive care. Non-surgical treatments such as medications, rehabilitation, manipulative therapy, acupuncture, and psychotherapy can be effective in most spine symptoms. This study aims to share understanding of multidisciplinary management on diagnosis and treatments involving medications and rehabilitation for alleviating debilitating symptoms of POTS.
Conclusions
Patients with POTS frequently develop lightheadedness, palpitation, and neck pain. Neck pain and headache management in POTS require a prudent use of therapy that takes patient co-morbidities and co-existing symptoms into account. Multidisciplinary clinical approaches with nonpharmacologic patient-centered modalities such as exercise training, chiropractic rehabilitation, and volume expansion through diet adjustments are recommended.
Key Messages
Postural orthostatic tachycardia syndrome (POTS) refers to dysautonomia characterized by an abnormal heart rate response to a positional change.
Poor venous return may be a result of impaired vasoconstriction secondary to a number of factors and concurrent clinical syndromes.
Patients with POTS will have on-going shared care between family physicians and secondary or tertiary care practitioners.
Multidisciplinary clinical approaches with nonpharmacologic modalities such as physical exercise, chiropractic rehabilitation, and diet recommendations are strongly recommended.
Declaration of patient consent
The author(s) certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his/her consent for his/her clinical information to be reported in the journal. The patient understands that his/her name and initials will not be published and due efforts will be made to conceal their identity.
Ethical statement
This article does not contain studies with human or animal subjects performed by the authors. The authors attest that this case report was determined not to require Institutional Review Board/Ethics Committee review, and the corresponding protocol/approval number is not applicable as this was a retrospective case report.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Chouksey D, Rathi P, Sodani A, Jain R, Ishar HS. Postural orthostatic tachycardia syndrome in patients of orthostatic intolerance symptoms:An ambispective study. AIMS Neurosci. 2021;8:74–85. doi: 10.3934/Neuroscience.2021004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Raj SR, Bourne KM, Stiles LE, Miglis MG, Cortez MM, Miller AJ, et al. Postural orthostatic tachycardia syndrome (POTS):Priorities for POTS care and research from a 2019 National Institutes of Health Expert Consensus Meeting-Part 2. Auton Neurosci. 2021;235:102836. doi: 10.1016/j.autneu.2021.102836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cook GA, Jr, Sandroni P. Management of headache and chronic pain in POTS. Auton Neurosci. 2018;215:37–45. doi: 10.1016/j.autneu.2018.06.004. [DOI] [PubMed] [Google Scholar]
- 4.Olshansky B, Cannom D, Fedorowski A, Stewart J, Gibbons C, Sutton R, et al. Postural orthostatic tachycardia syndrome (POTS):A critical assessment. Prog Cardiovasc Dis. 2020;63:263–70. doi: 10.1016/j.pcad.2020.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vernino S, Bourne KM, Stiles LE, Grubb BP, Fedorowski A, Stewart JM, et al. Postural orthostatic tachycardia syndrome (POTS):State of the science and clinical care from a 2019 national institutes of health expert consensus meeting-Part 1. Auton Neurosci. 2021;235:102828. doi: 10.1016/j.autneu.2021.102828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lin SY, Hsu WH, Lin CC, Lin CL, Tsai CH, Lin CH, et al. Association of arrhythmia in patients with cervical spondylosis:A nationwide population-based cohort study. J Clin Med. 2018;7:236. doi: 10.3390/jcm7090236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chu ECP, Ng M. Long-term relief from tension-type headache and major depression following chiropractic treatment. J Family Med Prim Care. 2018;7:629–31. doi: 10.4103/jfmpc.jfmpc_68_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roy RA, Boucher JP, Comtois AS. Heart rate variability modulation after manipulation in pain-free patients vs patients in pain. J Manipulative Physiol Ther. 2009;32:277–86. doi: 10.1016/j.jmpt.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 9.Zhang J, Dean D, Nosco D, Strathopulos D, Floros M. Effect of chiropractic care on heart rate variability and pain in a multisite clinical study. J Manipulative Physiol Ther. 2006;29:267–74. doi: 10.1016/j.jmpt.2006.03.010. [DOI] [PubMed] [Google Scholar]
- 10.Staples A, Thompson NR, Moodley M. Pediatric-onset postural orthostatic tachycardia syndrome in a single tertiary care center. J Child Neurol. 2020;35:526–35. doi: 10.1177/0883073820916260. [DOI] [PubMed] [Google Scholar]