Abstract
We have examined the role of adenylate cyclase-hemolysin (CyaA) by constructing an in-frame deletion in the Bordetella bronchiseptica cyaA structural gene and comparing wild-type and cyaA deletion strains in natural host infection models. Both the wild-type strain RB50 and its adenylate cyclase toxin deletion (ΔcyaA) derivative efficiently establish persistent infections in rabbits, rats, and mice following low-dose inoculation. In contrast, an inoculation protocol that seeds the lower respiratory tract revealed significant differences in bacterial numbers and in polymorphonuclear neutrophil recruitment in the lungs from days 5 to 12 postinoculation. We next explored the effects of disarming specific aspects of the immune system on the relative phenotypes of wild-type and ΔcyaA bacteria. SCID, SCID-beige, or RAG-1−/− mice succumbed to lethal systemic infection following high- or low-dose intranasal inoculation with the wild-type strain but not the ΔcyaA mutant. Mice rendered neutropenic by treatment with cyclophosphamide or by knockout mutation in the granulocyte colony-stimulating factor locus were highly susceptible to lethal infection by either wild-type or ΔcyaA strains. These results reveal the significant role played by neutrophils early in B. bronchiseptica infection and by acquired immunity at later time points and suggest that phagocytic cells are a primary in vivo target of the Bordetella adenylate cyclase toxin.
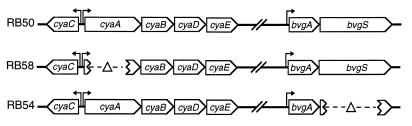
Bordetella bronchiseptica is a broad-host-range, gram-negative bacterium associated with atrophic rhinitis in swine, bronchopneumonia in dogs, and rhinotracheitis in rodents (9). B. bronchiseptica naturally infects laboratory animals, facilitating analysis of the molecular and cellular determinants involved in respiratory tract colonization in the context of naturally occurring bacterium-host interactions. Hallmarks of experimental infection of immunocompetent animals are efficient establishment, long-term persistence, and the absence of acute or chronic disease (5, 37). In B. bronchiseptica and the closely related human pathogens Bordetella pertussis and Bordetella parapertussis, genes encoding virulence and colonization factors are transcriptionally activated by a signal transduction system encoded by the bvgAS operon (Fig. 1) (32, 33). BvgAS-activated gene products on the bacterial cell surface include the putative adhesins pertactin, filamentous hemagglutinin, and fimbriae and the serum resistance protein BrkA (25, 28, 29). BvgAS also induces expression of a type III secretion apparatus (38) and a potent adenylate cyclase toxin which profoundly affects phagocytic cells in vitro (8, 15).
FIG. 1.
Genotypes of B. bronchiseptica strains. RB58 contains an in-frame deletion in the cyaA structural gene. RB54 contains an in-frame deletion in bvgS, resulting in the loss of expression of virulence-associated genes.
The Bordetella adenylate cyclase toxin (CyaA) is a member of the RTX family of bacterial exotoxins (8, 15). Palmitoylation of the 177-kDa CyaA protein by the product of cyaC (Fig. 1) facilitates insertion and transmembrane delivery of the catalytic domain into target cells (14, 17). CyaA-catalyzed production of supraphysiologic amounts of cyclic AMP is stimulated by calmodulin in the eukaryotic cell cytoplasm, an adaptation that is shared with the edema factor component of anthrax toxin (22, 30, 36). The B. bronchiseptica CyaA amino acid sequence is 98% identical to that of B. pertussis (3). Since the initial description of phagocyte impotence resulting from CyaA activity (4), in vitro studies have demonstrated numerous toxic effects on phagocytic cells. These include the inhibition of chemotaxis, phagocytosis, superoxide generation, and bacterial killing by neutrophils and induction of apoptosis in macrophages (4, 7, 15, 21). Determining an in vivo function for CyaA, however, has been more difficult. Compared to wild-type (wt) B. pertussis, a cyaA mutant was recovered in lower numbers from the lungs of mice and induced less macrophage apoptosis and neutrophil infiltration but persisted for at least as long as the wt strain (10, 12, 19, 20, 34, 35). The conclusion that CyaA is a colonization factor underscores the limitations of our understanding of the precise in vivo role(s) of this toxin.
We have examined the interactions between wt and ΔcyaA B. bronchiseptica strains in immunocompetent and immunocompromised mice. We show that mice with severe defects in either lymphocyte or neutrophil function are highly sensitive to B. bronchiseptica infection. A B. bronchiseptica strain with an in-frame deletion in the cyaA structural gene was as virulent as the wt in neutropenic mice but avirulent in B- and T-cell-deficient mice. These data support a model in which CyaA targets one or more aspects of the innate immune response, most likely involving neutrophils.
MATERIALS AND METHODS
Strain construction.
pΔcyaA was constructed by cloning a 5.5-kb BamHI-BsmI fragment encompassing cyaA from B. pertussis into our allelic exchange vector (5), digesting it with ApaLI, and religating it to delete the two consecutive ApaLI fragments which encode the central 1,580 codons of cyaA. The 766-bp BamHI-BsmI fragment remaining in pΔcyaA contains 67 bp of cyaA promoter sequence, the first 61 codons, the last 65 codons, and 206 bp 3′ to the cyaA stop codon. Delivery of this allele to the chromosome of RB50 (wt) by two consecutive homologous recombination events resulted in construction of strain RB58 (ΔcyaA). Southern hybridization analysis confirmed that RB58 was constructed as intended (data not shown). In vitro assays, performed as previously described (16), confirmed that supernatants from RB50, but not RB58, contained adenylate cyclase activity. WD3 (ΔbscN) and 8W1 (ΔbscNΔcyaA) were constructed as in-frame deletions in bscN in RB50 and RB58, respectively, as previously described (38). RB54 was similarly constructed as an in-frame deletion in bvgS as previously described (5).
Animal experiments.
Rabbits were obtained from Charles River and were inoculated as previously described (5). BALB/c and C57BL/6 mice and Wistar rats were obtained from B & K Laboratories. SCID, SCID-beige, and nude mice were from University of California at Los Angeles facilities. RAG-1−/−, Beige, and granulocyte colony-stimulating factor (G-CSF)−/− mice were from Jackson Laboratories. Rats and mice lightly sedated with halothane were inoculated with a low dose consisting of 500 to 1,000 bacteria in 5 μl of phosphate-buffered saline (PBS), as previously described (1), except where a high dose is indicated. The high dose consisted of 0.5 × 106 to 1.0 × 106 bacteria in 50 μl of PBS, sufficient to seed the entire respiratory tract with bacteria. For survival curves, after the progression of disease became clear, moribund animals were euthanized to prevent unnecessary suffering. For histological examination, lungs and trachea were excised as a unit. The trachea was cannulated with a blunt-ended 18-gauge needle attached to a syringe. Lungs were carefully filled with 10% formalin and immersed in 10% formalin for 24 h before paraffin embedding, sectioning, and hematoxylin-and-eosin staining. Sections were graded by observers blinded to the treatment of the sample, and the results were confirmed by an independent assessment by a pathologist consultant. For toxicity studies, BALB/c mice were administered RB50 (wt) or RB58 (ΔcyaA) by intraperitoneal injection. BALB/c mice were made neutropenic by intraperitoneal injection of 0.25 g of cyclophosphamide per kg of body weight 4 days prior to inoculation. Blood leukocytes were counted with a hemocytometer, and blood smears were stained with Diff-Quik (Baxter Scientific Products) and observed microscopically to confirm that neutrophils were reduced by more than 90%. Animals were handled in accordance with institutional guidelines. Statistical significance was determined by an unpaired t test.
Cytotoxicity.
J774 cells were cultured in Dulbecco modified Eagle medium with 10% fetal bovine serum. Cells were grown to approximately 80% confluency, and bacteria were added at a multiplicity of infection (MOI) of 10. After a 5-min centrifugation at 500 × g, the mixture was incubated at 37°C for 4 h. Cytotoxicity was determined by using the Cytotox96 (Promega) kit according to the manufacturer’s protocol. Mean values and standard errors were compared by the unpaired t test.
RESULTS
Construction and in vitro analyses of a ΔcyaA mutant of B. bronchiseptica.
We constructed a B. bronchiseptica strain with an in-frame, nonpolar deletion in cyaA (Fig. 1). Deletion of cyaA was accompanied by the loss of hemolytic and adenylate cyclase activities (Materials and Methods). B. pertussis CyaA has previously been reported to be cytotoxic for the macrophage-like cell line J774 (21). To determine if a ΔcyaA B. bronchiseptica strain lacks cytotoxicity for macrophages, we examined the effects of the wt strain RB50, or its ΔcyaA derivative, RB58, on J774 cells in vitro. Both wt and ΔcyaA bacteria efficiently kill J774 cells in vitro within 4 h (Fig. 2). RB54 (Δbvg), which does not express any of the BvgAS-regulated virulence factors, is not cytotoxic for J774 cells. These data indicate that Bvg-regulated factors aside from CyaA are required for macrophage killing by B. bronchiseptica.
FIG. 2.
Cytotoxicity of wt and mutant B. bronchiseptica strains for J774 cells. Bacteria were incubated with J774 cells at an MOI of 10 for 4 h. Cytotoxicity was determined by the release of lactate dehydrogenase as measured with the Cytotox96 kit, and the means and standard errors are presented as percentages of the total lysis by detergent. All strains differ from one another (P < 0.001), except for the wt and ΔcyaA strains and the ΔbscNΔcyaA and Δbvg strains.
We have recently identified a type III secretion system in B. bronchiseptica and constructed an in-frame deletion in bscN (38). BscN is a homolog of YscN which is postulated to provide energy via ATP hydrolysis for the secretion of proteins by the Yersinia type III system (38). A ΔbscN strain is defective in secretion of multiple proteins (38). This mutant is also reduced in its macrophage cytotoxicity in vitro compared to RB50 (P = 0.0002) but maintains significantly higher levels of cytotoxicity than does RB54 (ΔbvgAS) (P < 0.0001), suggesting that there is a type III-independent mechanism of cytotoxicity (38) (Fig. 2). To determine if the remaining cytotoxic activity of the type III secretion mutant (ΔbscN) is due to CyaA, we deleted cyaA from this mutant. The resulting ΔbscNΔcyaA double mutant is significantly reduced in macrophage cytotoxicity compared to the ΔbscN strain (P = 0.0002) (Fig. 2). The RAW264 macrophage-like cell line, the L2 rat lung epithelial cell line, and rat peritoneal macrophages all behaved similarly to J774 cells in this assay. These data indicate that B. bronchiseptica has two independent mechanisms capable of mediating macrophage cytotoxicity. Under the in vitro conditions used here, the type III secretion system mediates more efficient killing than does CyaA.
In vivo comparison of wt and Δcya strains of B. bronchiseptica.
To determine if CyaA plays a role in the initial establishment of infection, rats were inoculated with 10 to 20 CFU of either the wt or ΔcyaA strains delivered in a 5-μl droplet to the external nares. On day 8, B. bronchiseptica was detected in the respiratory tracts of seven of seven animals given wt and six of seven given ΔcyaA bacteria. The 50% infective dose of both strains is therefore less than 20 CFU, suggesting that CyaA is not required for B. bronchiseptica to efficiently establish colonization of the nasal cavity.
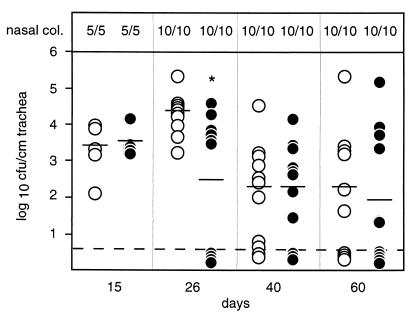
To more closely monitor the kinetics of growth in the nose, spread to the trachea, and persistence in both sites, groups of rats were inoculated with wt or ΔcyaA bacteria (500 CFU in a 5-μl droplet of PBS) and sacrificed on day 14, 26, 40, or 60. All rats were colonized in the nasal cavity at all time points (Fig. 3). On day 15, all rats were colonized in the trachea, indicating that CyaA is not required for colonization of this normally sterile site. A statistically significant difference between the wt and ΔcyaA strains was observed in tracheal colonization levels on day 26 (P < 0.01), but no such difference was observed at any other time point (P ≥ 0.1). Both strains also efficiently infected the nose and spread to the lower respiratory tract of rabbits inoculated by the low-dose regimen (data not shown). These data indicate that CyaA is not required for B. bronchiseptica to efficiently colonize the nasal cavity and spread to the lower respiratory tracts of two of its natural mammalian hosts, rats and rabbits.
FIG. 3.
Time course of rat respiratory tract colonization by wt and ΔcyaA B. bronchiseptica. Wistar rats were inoculated intranasally with 50 μl of PBS containing 5 × 105 CFU of either RB50 (wt; open circles) or RB58 (ΔcyaA; solid circles), and the numbers of bacteria present in the trachea were determined at the indicated times postinoculation. Each symbol represents a single animal, bars represent the means, and the dashed line represents the lower level of detection. Nasal colonization (col.) was determined by nasal swab and is presented as the number of B. bronchiseptica-colonized animals over the total number of rats. ∗, P < 0.01.
To monitor bacterial colonization of mice over time, we used two inoculation regimens to examine independent aspects of infection. Low-dose, low-volume inoculation (a range of doses from 10 to 1,000 CFU in a 5-μl droplet of PBS) delivered bacteria to only the nasal cavity and tested the ability of the inoculum to establish infection and spread to the lower respiratory tract. High-dose, high-volume inoculation (0.5 × 106 to 1 × 106 CFU in 50 μl of PBS) of anesthetized mice seeded bacteria throughout the respiratory tract and tested the ability of the bacteria to grow and persist in the normally sterile environment of the lower respiratory tract.
To determine if CyaA is required for efficient colonization of mice by B. bronchiseptica, groups of mice were inoculated with a range of doses of wt or ΔcyaA bacteria. Doses as low as 5 to 10 CFU in a 5-μl droplet were sufficient to colonize the nasal cavity of four of five BALB/c mice inoculated with the wt strain and three of five inoculated with the ΔcyaA strain. Doses of 100 CFU or more established infection in all mice, and infected mice remained colonized with either strain for more than 200 days. wt and ΔcyaA strains infected C57BL/6 mice with similar efficiency. CyaA is therefore not required for efficient establishment or persistence of infection in the mouse nasal cavity, a result consistent with observations with rats.
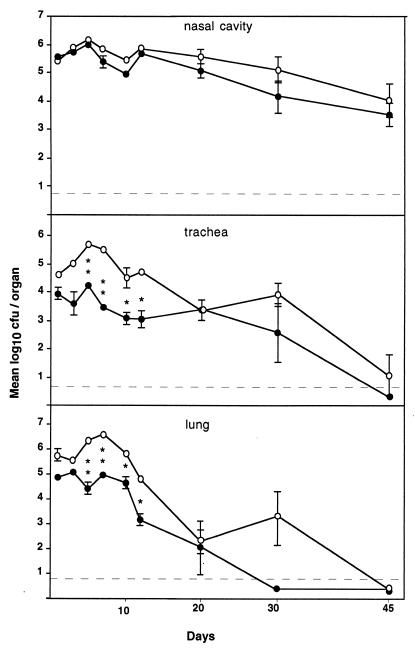
CyaA has been shown elsewhere to be important for the growth of B. pertussis early after inoculation into the lungs of mice (10, 19, 20, 34, 35). To compare the abilities of wt and ΔcyaA B. bronchiseptica strains to grow and persist in the normally sterile environment of the lower respiratory tract, anesthetized mice were inoculated by the high-dose, high-volume regimen and sacrificed at days 1, 3, 5, 7, 10, 12, 20, 30, and 45 postinoculation (Fig. 4). Both wt and ΔcyaA strains grew in the nose to approximately 106 organisms by day 5 and slowly decreased to 104 to 105 by day 45, remaining at these levels for the lives of the animals. Both strains were ultimately cleared from the trachea and lungs of mice by day 45. The two strains differed significantly (P ≤ 0.01) only in the trachea and lungs, sites of immune surveillance, on days 5, 7, 10, and 12. These data indicate that in this high-dose-inoculation mouse model, CyaA is required early after inoculation for maximal growth of B. bronchiseptica in the trachea and lungs.
FIG. 4.
Time course of mouse respiratory tract colonization by wt and ΔcyaA B. bronchiseptica. Groups of three female, 4-week-old, BALB/c mice were inoculated intranasally with 50 μl of PBS containing 5 × 105 CFU of either RB50 (wt; open circles) or RB58 (ΔcyaA; solid circles), and the numbers of CFU present in the nasal cavity, trachea, and lungs were determined at the indicated times postinoculation. ∗, P < 0.01. ∗∗, P < 0.001.
CyaA contributes to neutrophil infiltration and lung pathology.
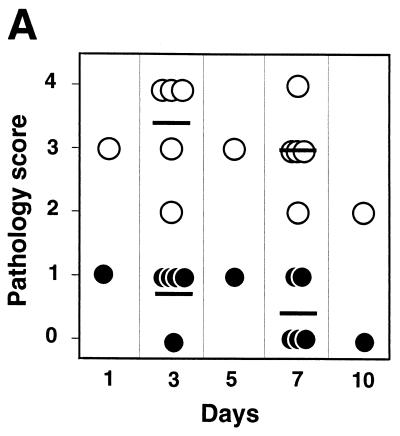
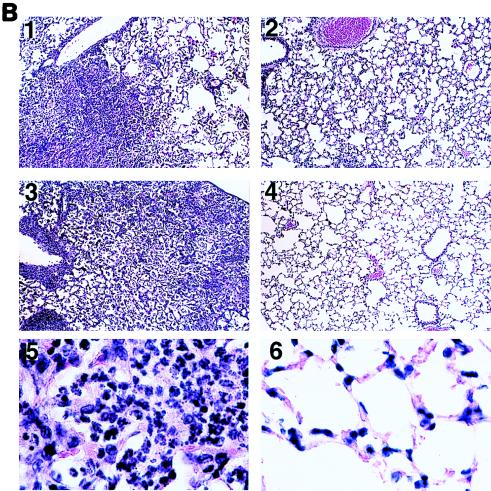
In parallel with the time course of Fig. 4, mice were sacrificed for histological examination of trachea and lungs on days 1, 3, 5, 7, and 10. On day 3, lungs infected with the wt strain showed extensive exudate from blood vessels and accumulation of cells, primarily neutrophils, within alveolar spaces (Fig. 5B, panel 1). Inflammatory cell recruitment continued, filling alveoli in large regions of the lungs by day 7 (Fig. 5B, panel 3). In contrast, lungs infected with the ΔcyaA strain showed only a small amount of infiltration or pathology at days 1 and 3 and very little thereafter (Fig. 5B, panels 2 and 4). On day 3 postinoculation, bronchoalveolar lavage recovered (6.5 ± 1.1) × 106 neutrophils from lungs infected with the wt strain, significantly more than the (3.9 ± 0.8) × 105 neutrophils from lungs infected with the ΔcyaA strain (P = 0.0002). Histological sections were examined in a blinded fashion and graded for pathology. Lungs of mice infected with the wt strain had consistently greater pathology scores, based on the extent of immune cell infiltration, tissue damage, consolidation, and necrosis (Fig. 5A). Lungs infected with the ΔcyaA strain showed only minor diffuse infiltration with little tissue damage and no consolidated or necrotic regions. These data indicate that, following high-dose, high-volume inoculation, the presence of CyaA results in increased pulmonary neutrophil infiltration and damage.
FIG. 5.
Mouse lung pathology induced by wt and ΔcyaA B. bronchiseptica. BALB/c mice were inoculated in parallel with those for Fig. 3. Histological sections of lung tissues were prepared as described in Materials and Methods. (A) Samples were submitted for observation in a blinded fashion. Upon examination, samples were given scores of 0 (no pathology), 1 (mild inflammation in ≤10% of the bronchioles and/or ≤10% of lung tissue), 2 (inflammation in 10 to 30% of bronchioles and/or mild inflammation in 10 to 30% of lung tissue), 3 (inflammation in >30% of bronchioles and mild to moderate inflammation in >30% of lung tissue), and 4 (inflammation in >50% of bronchioles and moderate to severe inflammation in >30% of lung tissue). Bars indicate the averages of five animals. Open circles represent animals infected with RB50 (wt), and solid circles represent animals infected with RB58 (ΔcyaA). (B) Representative sections of lungs infected with wt (panels 1 and 3) or ΔcyaA (panels 2 and 4) bacteria on day 3 (panels 1 and 2) or day 7 (panels 3 and 4). Magnification, ×100 (panels 1 to 4) and ×1,000 (panels 5 and 6).
CyaA is required for virulence in SCID-Beige mice.
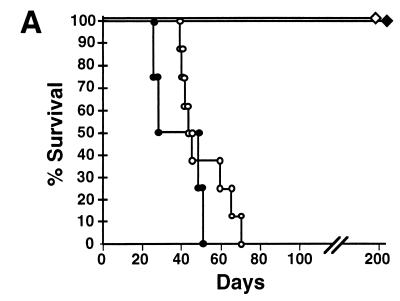
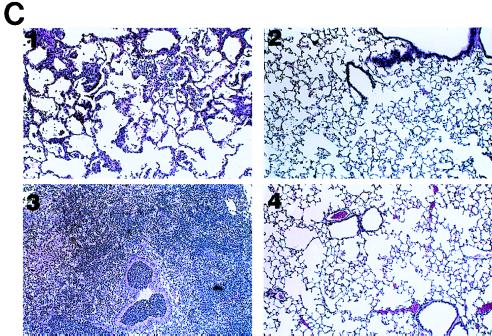
We next explored the effect of disarming one or more aspects of the host immune response on the phenotype of CyaA in vivo. Cytotoxicity assays indicated that CyaA can kill phagocytic cells, and in vivo data identified a role for CyaA early after infection when phagocytes are a prominent aspect of innate immunity. To focus on interactions with the innate immune system, SCID-beige mice (BALB/c genetic background), which are deficient in T and B cells as well as NK cell activities (6, 31), were inoculated intranasally with either wt or ΔcyaA bacteria (Fig. 6A). Both groups of mice were healthy for about 30 days, after which animals infected with wt bacteria began to display signs of illness such as piloerection, weight loss, hunched stature, listlessness, and eventually loss of responsiveness followed by death. In striking contrast to the 100% lethality observed with the wt strain, mice infected with the ΔcyaA strain displayed no symptoms of disease and were healthy for more than 200 days. This dichotomy was observed following low-dose, low-volume or high-dose, high-volume intranasal inoculation. The beige mutation has pleiotropic effects which include defects in macrophage and neutrophil functions (2). However, the wt strain, but not the ΔcyaA strain, also established similarly lethal infections in SCID (both BALB/c and C3H backgrounds) and RAG-1−/− (C57BL/6 background) mice. Addition of the beige mutation to the SCID allele decreased the average time to death, but in animals carrying the beige mutation alone (C57BL/6 background), no lethality was observed (data not shown). Together, these data indicate that T cells and B cells are required to prevent killing by B. bronchiseptica. As expected, RB54 (ΔbvgS) did not kill or colonize SCID-beige mice, indicating that Bvg-activated virulence factors are required for colonization of these animals.
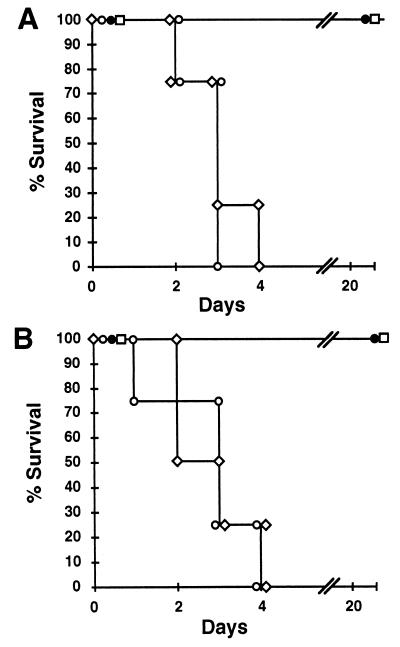
FIG. 6.
Infection of SCID-Beige mice with wt and ΔcyaA B. bronchiseptica. (A) Four-week-old SCID-Beige mice were inoculated with B. bronchiseptica, and percent survival over time is shown. Open symbols represent groups of eight animals inoculated with 103 CFU of either RB50 (wt; circles) or RB58 (ΔcyaA; diamonds) delivered in a 5-μl droplet to the external nares. Solid symbols represent groups of four mice inoculated with 5 × 105 CFU of either RB50 (wt; circles) or RB58 (ΔcyaA; diamonds) delivered in a 50-μl volume to the respiratory tract via the nares. (B) Colonization of various tissues by wt and ΔcyaA B. bronchiseptica. Groups of three 4-week-old, female, SCID-Beige mice were inoculated with 1,000 CFU of either RB50 (wt; open bars) or RB58 (ΔcyaA; hatched bars) delivered in a 5-μl droplet to the external nares. Mice were sacrificed at 45 days postinoculation, and colonization levels in the nasal cavity, trachea, lungs, liver, and spleen were determined. Mean log10 CFU per organ or tissue section ± 1 standard error are shown. The dashed line represents the lower limit of detection. ∗, P < 0.01. ∗∗, P < 0.001. (C) Representative sections of SCID-Beige mouse lungs infected with wt (panels 1 and 3) or ΔcyaA (panels 2 and 4) bacteria on day 3 (panels 1 and 2) or day 7 (panels 3 and 4). Magnification, ×100.
SCID-beige mice inoculated with the wt strain by the low-dose, low-volume regimen were moribund at approximately day 45, but those inoculated with the ΔcyaA strain remained healthy. We determined the relative distribution of bacteria at this time point with SCID-beige mice inoculated by the low-dose, low-volume regimen. Colonization levels in various organs were determined 45 days after inoculation. At this time, the wt strain was recovered in high numbers in the nasal cavity, trachea, and lungs as well as other organs including liver and spleen, indicating that the infection had escaped the respiratory tract and had spread systemically (Fig. 6B). The ΔcyaA strain was recovered from the nasal cavity and trachea at 100- to 1,000-fold-lower numbers than was the wt strain and was not detected in the lungs or at systemic sites (P < 0.01 at all sites).
Histological examination of the lungs of SCID-beige mice 3 and 7 days after high-dose, high-volume inoculation revealed that the wt strain produced lung pathology even more severe than that of BALB/c mice at this time point (Fig. 6C, panels 1 and 3). The ΔcyaA strain, however, produced very little lung pathology at day 3, 7, or 45 postinoculation (Fig. 6C, panels 2 and 4, and data not shown). Together, these results show that CyaA is critical to the ability of B. bronchiseptica to cause systemic infections in B- and T-cell-deficient mice, indicating that its target is among the innate immune mechanisms retained by these animals.
Both wt and ΔcyaA strains are highly virulent in neutropenic mice.
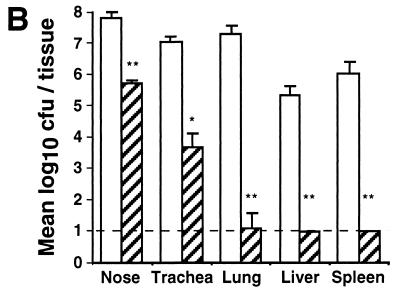
Prominent among the defenses present in lymphocyte-deficient mice are polymorphonuclear neutrophils. If neutrophils are a primary target for CyaA, then mice depleted of neutrophils should be equally susceptible to infection with wt or with ΔcyaA B. bronchiseptica. BALB/c mice were rendered neutropenic by treatment with cyclophosphamide, which reduced their blood neutrophil count by >90%. These mice were rapidly killed by high-dose, high-volume inoculation with the wt strain (Fig. 7A), suggesting that neutrophils play a critical role in the early response to B. bronchiseptica infection. These mice were also rapidly killed by the ΔcyaA strain delivered by the same high-dose, high-volume regimen that caused minimal pathology in normal or SCID-beige mice, indicating that CyaA is not required for B. bronchiseptica killing of neutropenic mice. RB54 (Δbvg) did not kill cyclophosphamide-treated mice, indicating a requirement for Bvg-activated factors other than CyaA. As cyclophosphamide has pleiotropic effects, we used an additional source of neutrophil-deficient animals. G-CSF−/− mice (B6,129 genetic background) lack both genomic copies of the G-CSF gene and have reduced numbers of neutrophils and impaired neutrophil mobilization (23). These animals also quickly succumbed to infection by wt or ΔcyaA, but not RB54 (Δbvg), bacteria (Fig. 7B). Removing neutrophils, therefore, eliminated the in vivo phenotype of CyaA.
FIG. 7.
Comparison of wt and ΔcyaA B. bronchiseptica infections of neutropenic mice. Groups of four BALB/c mice rendered neutropenic by cyclophosphamide treatment (A) or G-CSF−/− mice (B) were inoculated with 5 × 105 CFU of either RB50 (wt; open circles), RB58 (ΔcyaA; open diamonds), RB54 (ΔbvgS; solid circles), or PBS (open squares) delivered in a 50-μl volume. The percentages of animals (n = 4) surviving over time are indicated.
DISCUSSION
Both B. pertussis (20) and B. bronchiseptica (this work) ΔcyaA mutants lack hemolytic and adenylate cyclase activities. The B. pertussis ΔcyaA mutant is also deficient in macrophage cytotoxicity (21); however, the effect of B. bronchiseptica CyaA on macrophages is apparent only when the type III secretion system is disrupted (38) (Fig. 2). The remaining cytotoxicity displayed by the type III mutant (ΔbscN) is attributable to CyaA, as the double mutant (ΔbscNΔcyaA) has no detectable cytotoxicity. The level of cytotoxic activity attributable to B. bronchiseptica CyaA 4 h after infection at an MOI of 10 is in rough agreement with a previous report of B. pertussis CyaA-mediated cytotoxicity, which required 8 h of infection with B. pertussis at an MOI of 100 to achieve 100% death (21). wt B. bronchiseptica, with an intact type III secretion system, kills 100% of macrophages in as little at 2 h at an MOI of 10 (data not shown). The type III secretion system is dramatically more efficient than CyaA in this respect. In vitro experiments, however, do not necessarily indicate in vivo functions.
In vivo experiments using the low-dose, low-volume inoculation regimen highlight several advantages of the B. bronchiseptica animal model. B. pertussis, which is highly contagious in humans (18), must be delivered in high doses throughout the respiratory tract to establish even a transient infection in mice. It is therefore difficult to extrapolate results obtained with the mouse model to the events that occur during B. pertussis infection of its human host, especially those that occur during initial colonization. The low-dose, low-volume B. bronchiseptica model, on the other hand, rigorously tests the ability of small numbers of bacteria to colonize and grow in the nasal cavity and to spread to the lower respiratory tract. In these assays, CyaA is not required for efficient colonization of the nasal cavity or spread to the trachea, although it may be required for persistence at high levels in the trachea. Although CyaA is not required for colonization, these data suggest that it may be involved in modulating the immune response.
High-dose, high-volume inoculation overcomes the cleansing effect of the mucociliary escalator of the trachea and deposits bacteria deep in the lungs, where debris is less efficiently washed away. Growth within lung alveoli may be less dependent on adhesins involved in attachment to ciliated epithelia and more dependent on toxins and factors that affect the immune response in this normally sterile site. It has previously been shown that in this environment CyaA is critical for the growth of B. pertussis and is involved in neutrophil recruitment and phagocyte apoptosis (10–12, 19, 20, 26, 34, 35). A human B. bronchiseptica isolate with an uncharacterized defect in hemolysin expression was previously compared with a hemolytic human isolate (13). Although a difference in mouse lung colonization was observed, the defect could not be definitively attributed to CyaA.
Determining the role of individual bacterial virulence factors, or specific immune mechanisms, in a complex bacterium-host relationship can be difficult. The classic approach of deleting a single bacterial virulence factor, or a single aspect of host immunity, may reveal the importance of that factor or immune mechanism by throwing the entire interaction out of balance. However, persistent bacterial infections can be carefully balanced, multifactorial, dynamic relationships in which any change on one side may be compensated for by numerous buffering factors on either side. In this context, ablation of a bacterial virulence factor, even a relatively important one, may not result in a perceptible difference in the course of infection. This approach may reveal that a factor is required for infection but seldom provides insight into the mechanisms involved. An alternative tactic is to combine the tools of bacterial and mammalian genetics to alter both sides of the interaction. The advantages of this strategy are twofold. First, disarming the host immune system can destabilize the interaction, allowing differences between wt and mutant bacteria to be more easily identified. Second, by creation of a defect on one side and then identification of a compensatory defect on the other, bacterial virulence factors can be matched to specific immune responses that they affect in vivo. Here we use isogenic wt and ΔcyaA strains in combination with mice with defined immune system defects to identify interactions between CyaA and subsets of the host immune system.
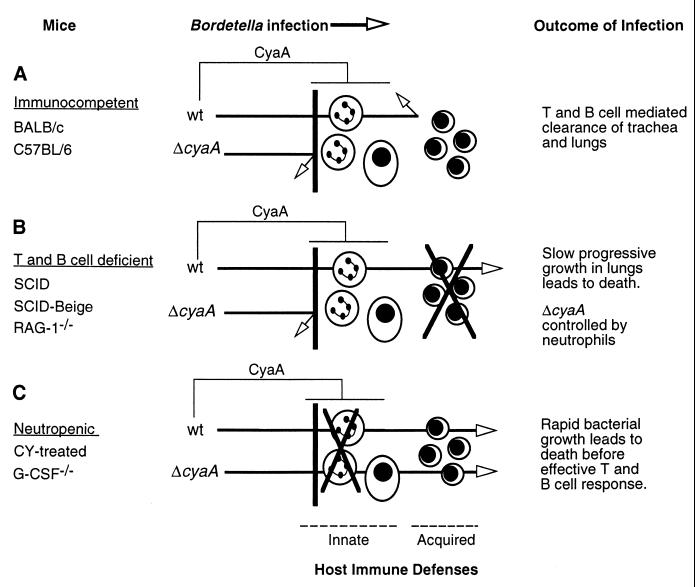
As summarized in Fig. 8, we observed three distinct relationships between the presence or absence of a functional cyaA locus and the outcome of B. bronchiseptica infection. In immunocompetent animals, or animals carrying the beige mutation alone, the summation of host defenses limits infection by wt or ΔcyaA bacteria (Fig. 8A) (24, 27). In contrast, decreased lymphocyte function in RAG-1−/−, SCID, or SCID-beige mice creates a situation where the absence or presence of CyaA determines whether the animal lives or dies (Fig. 8B). Presumably, CyaA is active against immunological defenses that are retained in SCID-beige mice and are able to control infection by the mutant strain, but not by the toxin-expressing wt strain. Neutrophils are prominent immune effector cells that are present and active in these immunocompromised animals. Addition of the beige mutation to the SCID background decreases the time to death, an effect that may result from the lack of NK-mediated activation of phagocytic cells or from inherent phagocyte defects associated with the beige allele (2). If the adenylate cyclase toxin does indeed target phagocytic cells, then eliminating the target should eliminate the phenotype associated with the toxin. Induction of neutropenia with cyclophosphamide, or by knockout mutation in the G-CSF locus, results in identical, lethal infections by wt and by ΔcyaA bacteria (Fig. 8C), indicating that neutrophils are critical to the early defense against B. bronchiseptica infection and that removing neutrophils eliminates the phenotype of CyaA. In normal and SCID-beige mice, the Δcya strain is more efficiently contained with less neutrophil infiltration and pathology than is wt B. bronchiseptica, supporting a model in which CyaA inhibits neutrophil-mediated antibacterial effects. Although this model implicates neutrophils, it does not require that they be the only, or even the primary, target of the toxin. For example, neutrophil activities could be modulated through an intermediary such as macrophages, NK cells, or epithelial cells via immunomodulatory signals. However, it is clear from our results that CyaA targets one or more functions associated with innate immunity and that depletion of neutrophils removes the requirement for CyaA in lethal B. bronchiseptica infection.
FIG. 8.
Model of the role of CyaA in infection of immunocompetent (A), T- and B-cell-deficient (B), and neutropenic (C) mice. See the text for description.
Mice with specific immune system defects have been used to reveal which aspects of immunity are most important in resisting particular pathogens. Likewise, the use of bacterial mutants with wt animals can sometimes reveal the importance of individual bacterial virulence factors during infection. Although results from these types of analyses may indicate that a specific virulence factor or immune effector function is important, they do not provide information about the mechanisms or specific interactions involved. By combining these two approaches, we have been able to implicate an interaction between a bacterial virulence factor and immune effector cells in vivo.
ACKNOWLEDGMENTS
This work was supported by NIH grant AI38417 (to J.F.M.) and USDA grant 96-35204-3827 (to E.T.H.), and M.H.Y. was supported by a postdoctoral fellowship from the Damon Runyon-Walter Winchell Foundation.
We gratefully acknowledge Nora Rozengurt for consultation on mouse lung pathology.
REFERENCES
- 1.Akerley B J, Cotter P A, Miller J F. Ectopic expression of the flagellar regulon alters development of the Bordetella-host interaction. Cell. 1995;80:611–620. doi: 10.1016/0092-8674(95)90515-4. [DOI] [PubMed] [Google Scholar]
- 2.Appelberg R, Castro A G, Gomes S, Pedrosa J, Silva M T. Susceptibility of beige mice to Mycobacterium avium: role of neutrophils. Infect Immun. 1995;63:3381–3387. doi: 10.1128/iai.63.9.3381-3387.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Betsou F, Sismeiro O, Danchin A, Guiso N. Cloning and sequence of the Bordetella bronchiseptica adenylate cyclase-hemolysin-encoding gene: comparison with the Bordetella pertussis gene. Gene. 1995;162:165–166. doi: 10.1016/0378-1119(95)00339-8. [DOI] [PubMed] [Google Scholar]
- 4.Confer D L, Eaton J W. Phagocyte impotence caused by an invasive bacterial adenylate cyclase. Science. 1982;217:948–950. doi: 10.1126/science.6287574. [DOI] [PubMed] [Google Scholar]
- 5.Cotter P A, Miller J F. BvgAS-mediated signal transduction: analysis of phase-locked regulatory mutants of Bordetella bronchiseptica in a rabbit model. Infect Immun. 1994;62:3381–3390. doi: 10.1128/iai.62.8.3381-3390.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dorshkind K, Keller G M, Phillips R A, Miller R G, Bosma G C, O’Toole M, Bosma M J. Functional status of cells from lymphoid and myeloid tissues in mice with severe combined immunodeficiency disease. J Immunol. 1984;132:1804–1808. [PubMed] [Google Scholar]
- 7.Friedman R L, Fiederlein R L, Glasser L, Galgiani J N. Bordetella pertussis adenylate cyclase: effects of affinity-purified adenylate cyclase on human polymorphonuclear leukocyte functions. Infect Immun. 1987;55:135–140. doi: 10.1128/iai.55.1.135-140.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Glaser P, Ladant D, Sezer O, Pichot F, Ullmann A, Danchin A. The calmodulin-sensitive adenylate cyclase of Bordetella pertussis: cloning and expression in Escherichia coli. Mol Microbiol. 1988;2:19–30. [PubMed] [Google Scholar]
- 9.Goodnow R A. Biology of Bordetella bronchiseptica. Microbiol Rev. 1980;44:722–738. doi: 10.1128/mr.44.4.722-738.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goodwin M S, Weiss A A. Adenylate cyclase toxin is critical for colonization and pertussis toxin is critical for lethal infection by Bordetella pertussis in infant mice. Infect Immun. 1990;58:3445–3447. doi: 10.1128/iai.58.10.3445-3447.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gross M K, Au D C, Smith A L, Storm D R. Targeted mutations that ablate either the adenylate cyclase or hemolysin function of the bifunctional cyaA toxin of Bordetella pertussis abolish virulence. Proc Natl Acad Sci USA. 1992;89:4898–4902. doi: 10.1073/pnas.89.11.4898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gueirard P, Druilhe A, Pretolani M, Guiso N. Role of adenylate cyclase-hemolysin in alveolar macrophage apoptosis during Bordetella pertussis infection in vivo. Infect Immun. 1998;66:1718–1725. doi: 10.1128/iai.66.4.1718-1725.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gueirard P, Minoprio P, Guiso N. Intranasal inoculation of Bordetella bronchiseptica in mice induces long-lasting antibody and T-cell mediated immune responses. Scand J Immunol. 1996;43:181–192. doi: 10.1046/j.1365-3083.1996.d01-30.x. [DOI] [PubMed] [Google Scholar]
- 14.Hackett M, Guo L, Shabanowitz J, Hunt D F, Hewlett E L. Internal lysine palmitoylation in adenylate cyclase toxin from Bordetella pertussis. Science. 1994;266:433–435. doi: 10.1126/science.7939682. [DOI] [PubMed] [Google Scholar]
- 15.Hanski E. Invasive adenylate cyclase toxin of Bordetella pertussis. Trends Biochem Sci. 1989;14:459–463. doi: 10.1016/0968-0004(89)90106-0. [DOI] [PubMed] [Google Scholar]
- 16.Hewlett E, Wolff J. Soluble adenylate cyclase from the culture medium of Bordetella pertussis: purification and characterization. J Bacteriol. 1976;127:890–898. doi: 10.1128/jb.127.2.890-898.1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hewlett E L, Gray M C, Ehrmann I E, Maloney N J, Otero A S, Gray L, Allietta M, Szabo G, Weiss A A, Barry E M. Characterization of adenylate cyclase toxin from a mutant of Bordetella pertussis defective in the activator gene, cyaC. J Biol Chem. 1993;268:7842–7848. [PubMed] [Google Scholar]
- 18.Kendrick P L. Secondary familial attack rates from pertussis in vaccinated and unvaccinated children. Am J Hyg. 1940;32:89–91. [Google Scholar]
- 19.Khelef N, Bachelet C M, Vargaftig B B, Guiso N. Characterization of murine lung inflammation after infection with parental Bordetella pertussis and mutants deficient in adhesins or toxins. Infect Immun. 1994;62:2893–2900. doi: 10.1128/iai.62.7.2893-2900.1994. . (Erratum, 62:5707.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Khelef N, Sakamoto H, Guiso N. Both adenylate cyclase and hemolytic activities are required by Bordetella pertussis to initiate infection. Microb Pathog. 1992;12:227–235. doi: 10.1016/0882-4010(92)90057-u. [DOI] [PubMed] [Google Scholar]
- 21.Khelef N, Zychlinsky A, Guiso N. Bordetella pertussis induces apoptosis in macrophages: role of adenylate cyclase-hemolysin. Infect Immun. 1993;61:4064–4071. doi: 10.1128/iai.61.10.4064-4071.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leppla S H. Anthrax toxin edema factor: a bacterial adenylate cyclase that increases cyclic AMP concentrations of eukaryotic cells. Proc Natl Acad Sci USA. 1982;79:3162–3166. doi: 10.1073/pnas.79.10.3162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lieschke G J, Grail D, Hodgson G, Metcalf D, Stanley E, Cheers C, Fowler K J, Basu S, Zhan Y F, Dunn A R. Mice lacking granulocyte colony-stimulating factor have chronic neutropenia, granulocyte and macrophage progenitor cell deficiency, and impaired neutrophil mobilization. Blood. 1994;84:1737–1746. [PubMed] [Google Scholar]
- 24.Mills K H, Barnard A, Watkins J, Redhead K. Cell-mediated immunity to Bordetella pertussis: role of Th1 cells in bacterial clearance in a murine respiratory infection model. Infect Immun. 1993;61:399–410. doi: 10.1128/iai.61.2.399-410.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mooi F R, Jansen W H, Brunings H, Gielen H, van der Heide H G J, Walvoort H C, Guinee P A M. Construction and analysis of Bordetella pertussis mutants defective in the production of fimbriae. Microb Pathog. 1992;12:127–135. doi: 10.1016/0882-4010(92)90115-5. [DOI] [PubMed] [Google Scholar]
- 26.Oldenburg D J, Gross M K, Smith A L, Storm D R. Virulence of a Bordetella pertussis strain expressing a mutant adenylyl cyclase with decreased calmodulin affinity. Microb Pathog. 1993;14:489–493. doi: 10.1006/mpat.1993.1048. [DOI] [PubMed] [Google Scholar]
- 27.Redhead K, Watkins J, Barnard A, Mills K H. Effective immunization against Bordetella pertussis respiratory infection in mice is dependent on induction of cell-mediated immunity. Infect Immun. 1993;61:3190–3198. doi: 10.1128/iai.61.8.3190-3198.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Relman D A, Domenighini M, Tuomanen E I, Rappuoli R, Falkow S. Filamentous hemagglutinin of Bordetella pertussis: nucleotide sequence and crucial role in adherence. Proc Natl Acad Sci USA. 1989;86:2634–2641. doi: 10.1073/pnas.86.8.2637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Roberts M, Cropley I, Chatfield S, Dougan G. Protection of mice against respiratory Bordetella pertussis infection by intranasal immunization with P.69 and FHA. Vaccine. 1993;11:866–872. doi: 10.1016/0264-410x(93)90363-3. [DOI] [PubMed] [Google Scholar]
- 30.Robertson D L, Tippetts M T, Leppla S H. Nucleotide sequence of the Bacillus anthracis edema factor gene (cya): a calmodulin-dependent adenylate cyclase. Gene. 1988;73:363–371. doi: 10.1016/0378-1119(88)90501-x. [DOI] [PubMed] [Google Scholar]
- 31.Roder J, Duwe A. The beige mutation in the mouse selectively impairs natural killer cell function. Nature. 1979;278:451–453. doi: 10.1038/278451a0. [DOI] [PubMed] [Google Scholar]
- 32.Uhl M A, Miller J F. Central role of the BvgS receiver as a phosphorylated intermediate in a complex two-component phosphorelay. J Biol Chem. 1996;271:33176–33180. doi: 10.1074/jbc.271.52.33176. [DOI] [PubMed] [Google Scholar]
- 33.Uhl M A, Miller J F. Integration of multiple domains in a two-component sensor protein: the Bordetella pertussis BvgAS phosphorelay. EMBO J. 1996;15:1028–1036. [PMC free article] [PubMed] [Google Scholar]
- 34.Weiss A A, Goodwin M S. Lethal infection by Bordetella pertussis mutants in the infant mouse model. Infect Immun. 1989;57:3757–3764. doi: 10.1128/iai.57.12.3757-3764.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Weiss A A, Hewlett E L, Myers G A, Falkow S. Pertussis toxin and extracytoplasmic adenylate cyclase as virulence factors of Bordetella pertussis. J Infect Dis. 1984;150:219–222. doi: 10.1093/infdis/150.2.219. [DOI] [PubMed] [Google Scholar]
- 36.Wolff J, Cook G H, Goldhammer A R, Berkowitz S A. Calmodulin activates prokaryotic adenylate cyclase. Proc Natl Acad Sci USA. 1980;77:3841–3844. doi: 10.1073/pnas.77.7.3841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yoda H, Nakayama K, Nakagawa M. Experimental infection of Bordetella bronchiseptica to rabbits. Exp Anim. 1982;31:113–118. [PubMed] [Google Scholar]
- 38.Yuk M H, Harvill E T, Miller J F. The bvgAS virulence control system regulates type III secretion in Bordetella bronchiseptica. Mol Microbiol. 1998;28:945–959. doi: 10.1046/j.1365-2958.1998.00850.x. [DOI] [PubMed] [Google Scholar]