Abstract
COPD is predicted to become the third leading cause of morbidity and mortality worldwide by 2030. Cigarette smoking (active or passive) is one of its chief causes, with about 20% of cigarette smokers developing COPD from cigarette smoke (CS)-induced irreversible damage and sustained inflammation of the airway epithelium. Inflammasome activation leads to the cleavage of pro-interleukin (IL)-1β and pro-IL-18, along with the release of pro-inflammatory cytokines via gasdermin D N-terminal fragment membrane pores, which further triggers acute phase pro-inflammatory responses and concurrent pyroptosis. There is currently intense interest in the role of nucleotide-binding oligomerisation domain-like receptor family, pyrin domain containing protein-3 inflammasomes in chronic inflammatory lung diseases such as COPD and their potential for therapeutic targeting. Phytochemicals including polyphenols and flavonoids have phyto-medicinal benefits in CS-COPD. Here, we review published articles from the last decade regarding the known associations between inflammasome-mediated responses and ameliorations in pre-clinical manifestations of CS-COPD via polyphenol and flavonoid treatment, with a focus on the underlying mechanistic insights. This article will potentially assist the development of drugs for the prevention and therapy of COPD, particularly in cigarette smokers.
Short abstract
This review compiles current investigations into the role of polyphenols/flavonoids in the alleviation of cigarette smoke-induced inflammasome; notably it provides a promising hit for rectifying the treatment of COPD. https://bit.ly/36OcUO9
Introduction
COPD has an increasing prevalence and is anticipated to become the third main cause of morbidity and mortality in the global population by 2030 [1]. Vitally, COPD can be caused by prolonged exposure to harmful particles, particulates and gases, infection with acute or chronic inflammatory conditions, or by injuries that include the airways, pulmonary vasculature and lung parenchyma. COPD is categorised by persistent airflow obstruction instigated by exposure to irritants; for instance, cigarette smoke (CS), dust and fumes [2]. Pulmonary injury comprises the phases of initiation (by exposure to CS, pollutants, infectious pathogens and agents), progression and consolidation. The involvement of complex interactions among oxidative stress, inflammation, extracellular matrix proteolysis, autophagic and apoptotic cell death leads to tissue damage [3]. The inflammatory response to progressive inflammation and tissue oxidative stresses leads to airway remodelling, which limits airflow and causes airway obstructions and tissue destruction, resulting in a decrease of forced expiratory volume [4]. In other airway obstructions, a major feature of COPD is pulmonary emphysema, which is described as structural changes and destruction of the alveolar air sacs that lead to decreased gas-exchanging surfaces and impaired gas exchange [5]. From a physio–pathological viewpoint, COPD is concomitant with chronic inflammation influencing the lung parenchyma and peripheral airways that cause irreversible and progressive airflow limitations. This inflammation is indicated by augmented numbers of alveolar macrophages, neutrophils, T-lymphocytes (cytotoxic T-cell type 1, T-helper cell (Th) 1 and Th17 cells) and intrinsic lymphoid cells engaged from the circulation [6]. These cells, as well as structural cells encompassing epithelial and endothelial cells and fibroblasts, secrete a variety of pro-inflammatory mediators, including cytokines, chemokines, growth factors and lipid mediators [7]. Interleukin (IL)-18 is a pro-inflammatory cytokine that was first described as an interferon (IFN)-γ-inducing factor. Similar to IL-1β, IL-18 is synthesised as an inactive precursor that requires processing by caspase-1 into an active-form cytokine [8]. Moreover, several studies used a mouse model to show that IL-18 over-expression results in emphysematous lesions. The data prompts the hypothesis that IL-18 induces an extensive range of COPD-like inflammatory and remodelling responses in the murine lung and induces mixed IL-1, IL-2 and IL-17 responses. IL-18 has been identified as a latent target for future COPD therapeutics to restrain the damaging and remodelling processes arising in COPD lungs [9].
Inflammasome
The functions of innate immune responses act as a first-line defence upon exposure to potentially deleterious stimuli. The innate immune system has evolved various extracellular and intracellular receptors that carry out surveillance for possibly detrimental particulates. Inflammasomes are defined as intracellular innate immune multiplex proteins that are formed and activated upon subsequent interaction with these stimuli [7]. The canonical inflammasomes can be elicited by pathogen-associated molecular patterns (PAMPs) or damage-associated molecular patterns (DAMPs) [10]. Two families of pattern-recognition receptors (PRRs), including the nucleotide-binding domain, leucine-rich repeat containing proteins (NLRs) and absent in melanoma 2 (AIM2)-like receptors, act as sensor components to stimulate the inflammasome [11]. The NLR family consists of several subclasses, including nucleotide-binding oligomerisation domain-like receptor family, pyrin domain containing protein (NLRP) 1, NLRP3, NLRP6, NLRP12 and NLR family CARD domain-containing protein 4 (NLRC4; also known as interleukin converting enzyme protease activating factor (IPAF)). In fact, the NLR family has two common features: the first one is a nucleotide-binding oligomerisation domain, which is bounded by ribonucleotide-phosphates, and the second one is the C-terminal leucine-rich repeat (LRR), which functions as a ligand-recognition domain [12]. In addition, the AIM2-like receptor (ALR) family encompasses two subclasses: AIM2 and interferon gamma inducible protein (IFI) 16. The common feature of the ALR family is PRRs with one or two hematopoietic, IFN-inducible and nuclear (HIN) domains at the C-terminal and a pyrin domain (PYD) at the N-terminal that can bind with cytoplasmic double-strand DNA (dsDNA) to initiate the inflammasome pathway [13].
In mammals, four major types of inflammasome, including NLRP1, NLRP3, NLRC4 and AIM2, have been confirmed by numerous studies of the signalling mechanisms and their functional effects. The activation of different inflammasomes may contribute to important immune response functions or cause cell pyroptosis [14]. The major domains of different inflammasome protein components can be classified as: caspase recruitment domain (CARD), domain with function to find (FIIND), HIN-200/IF120x domain (HIN), LRR, NAIP (neuronal apoptosis inhibitory protein), CIITA (MHC class II transcription activator), HET-E (incompatibility locus protein from Podospora anserina) and TP1 (telomerase-associated protein) (NACHT), and PYD. In general, an unoligomerised inflammasome may consist of two or three protein subunits. The unoligomerised NLRP1 inflammasome is composed of NLRP1 and caspase-1 (CASP1) protein subunits [15]; the unoligomerised NLRP3 inflammasome is composed of NLRP3, ASC (apoptosis-associated speck-like protein containing a caspase recruitment domain) and CASP1 protein subunits [16]; the unoligomerised IPAF (NLRC4) inflammasome is composed of IPAF and CASP1 protein subunits [17]; and the unoligomerised AIM2 inflammasome is composed of AIM2 and CASP1 protein subunits [18]. The NLRP1 protein comprises five domains: PYD, NACHT, LRR, FIIND and CARD; the NLRP3 protein encompasses three domains: PYD, NACHT and LRR; the ASC protein includes two domains: PYD and CARD; the IPAF protein contains three domains: CARD, NACHT and LRR; the CASP1 protein consists of three domains: CARD, p20 and p10. All four major inflammasomes possess one unique CASP1 protein subunit, and the CASP1 can link to the other inflammasome components via CARD–CARD interaction. The activation on PRRs of inflammasome may cause the autocleavage of CASP1 to release the active-form caspase-1 [10]. Inflammasomes are the intracellular multiprotein complexes that can directly or indirectly trigger one or more caspase signalling pathways to process and secrete various pro-inflammatory cytokines, including IL-1α, IL-1β, IL-18 or transforming growth factor-β (TGF-β), and subsequently engage innate immune responses [19, 20].
During bacterial infection, NLRP1 may be responsible for pathogen recognition and resistance. The NLRP1 inflammasome pathway could be activated by various stimuli, i.e. pathogen lethal toxin, muramyl dipeptide or a reduction in intracellular ATP level [15]. Upon cytoplasmic infection by Gram-negative bacteria, NAIPs act as upstream sensors that bind with bacterial ligands and then co-assemble with NLRC4 to constitute NLRC4 inflammasome, which leads to the release of active-form caspase-1 [21, 22]. Of note, AIM2 inflammasome, a cytosolic dsDNA-sensing inflammasome, takes part in host defences and immune responses to DNA virus infections as well as intracellular bacterial infections [23, 24]. During viral infection, mitochondrial misfunction or loss of membranous integrity, dsDNA can appear in the cytoplasm, and that may elicit AIM2 inflammasome pathways [25]. Some investigations have revealed the involvement of AIM2 inflammasome expression in subsequent accelerated COPD development. The redistribution of AIM2 from nucleus to cytoplasm and co-localisation with the cleaved IL-1β indicates that AIM2 inflammasome can be prompted in the airway epithelium and macrophages of COPD patients and CS-exposure mice [26]. An in vitro study showed that the expression of AIM2 in COPD-derived CD14+ peripheral blood mononuclear cells is higher than that in nonsmokers and smokers [26, 27]. The activation of AIM2 inflammasome in a caspase-1- and caspase-4-dependent fashion can cause IL-1α release but not IL-1β, and that can further promote TGF-β release as pro-fibrotic processes [28]. An in vivo study exhibited that the recruited macrophages or dendritic cells in smoking mice increased the AIM2 expression associated with caspase-11 (analogue with human caspase-4) but not caspase-1. CS exposure still caused an induction of alveoli enlargement in caspase-11 dysfunctional (knockout) mice, but the deposition of collagen in the bronchioles was lower than that in CS-exposure normal mice [27]. NLRP3-knockout mice have protective effects on the CS-induced COPD model, whereas IPAF- or AIM2-knockout mice have no protected potential in the same CS-challenge COPD model [29]. According to the limited available evidence, the pathologic mechanisms of AIM2 inflammasome in CS-induced COPD are different from the NLRP3 inflammasome pathway, and it are permeated by caspase-4 and TGF-β release to promote bronchial tissue fibrosis and exacerbated COPD.
In all inflammasomes pathways, the NLRP3 inflammasome could be activated in response to the various types of stimuli by PAMPs and DAMPs, such as toxins, extracellular ATP, cytokines, ion fluxes, endoplasmic reticulum (ER) stress and oxidative stress [30, 31]. The NLRP3 inflammasome entails a cytosolic PRR, an adaptor molecule ASC and the protease precursor procaspase-1. Assembly of the NLRP3 inflammasome complex causes the cleavage and activation of caspase-1 that triggers processing, which releases IL-1β and IL-18 cytokines and causes cell death via pyroptosis [32]. Some inducers, i.e. lipopolysaccharide (LPS), act on the canonical NLRP3 inflammasome pathways to increase cytoplasmic active-form caspase-1, and the synchronous trigger of noncanonical inflammasome pathways to activate caspase-4/11, caspase-5 or caspase-8 as well, and that may modulate cell death by apoptosis or necrosis [33–35].
Macrophages sense danger signals such as bacterial toxins or extracellular ATP derived from tissue damage or infection and initiate the activation of an intracellular molecular complex inflammasome. Pyroptosis is an inflammatory form of programmed cell death (PCD) that is found to be involved in the development of chronic inflammation, i.e. COPD, which is activated by the inflammatory caspase cleavage of gasdermin D (GSDMD) and apoptotic caspase cleavage of gasdermin E [20, 23]. It is critical that the activation of the inflammatory response and inflammasome are tightly regulated [36]. In the immunopathology of COPD, immune and nonimmune inflammatory alterations with oxidative stress imbalances are found, as well as changes in the protease/anti-protease ratio caused by direct and indirect genetic and epigenetic-environmental defects. COPD leads to irreversible tissue damage and chronic inflammation with aberrant tissue repairs, which induces chronic obstruction of the airway, bronchitis and systemic damage [2, 9]. Evidence from a previous review suggested the role of inflammasomes in the pathogenesis of numerous chronic respiratory diseases and acute lung injuries, such as asthma, transfusion-related acute lung injury (ALI), ventilator-induced lung injury, COPD and pulmonary fibrosis [37].
From a physiological viewpoint, the respiratory system provides gas exchange from the external environment for metabolism. The airway and lung are incessantly exposed and challenged to a variety of inhaled pathogen agents, harmful particulates and internal self-derived dangerous signals during their whole lifespan. The innate immune reaction plays a vital role in protecting the pulmonary system from infection and disease, and inflammasome pathways act on the initiation of innate immune responses. Continuously and seriously activated inflammasomes in epithelial cells, macrophages or other immune cells may cause an increasing release of several pro-inflammatory cytokines and the occurrence of cell pyroptosis, which subsequently result in pulmonary tissue remodelling, fibrosis and COPD. Thereby, this article comprehensively reviews and discusses the effects of polyphenols and flavonoids on the inflammasome pathways in CS-induced COPD to provide a deep insight into the benefits of natural medicinal products as pharmaceutics.
Polyphenols and flavonoids
Plants that harbour secondary metabolites such as alkaloids, polyphenols, flavonoids, terpenoids and other specific natural compounds have gained a great deal of attention for the treatment of several clinical complications. Considering the promising results obtained using medicinal plants, with few/no side effects, as well as their easy attainment, comprehensive research on herbal plants to treat disease should be anticipated [38–40]. Polyphenols are natural composites found in many plants. Mostly, the polyphenols are categorised in three major classes: flavonoids, lignans and nonflavonoids (stilbenes and phenolic acids). Flavonoids comprise a large class of food components encompassing the flavone, isoflavanone, flavanone, flavonols catechin and anthocyanin subclasses [41–43]. Remarkably, several biological properties of polyphenols have been scientifically demonstrated, including antiallergic, antiviral, antibacterial, anticarcinogenic, anti-inflammatory, antithrombotic, vasodilatory and hepatoprotective effects [44, 45], as well as benefits in age-associated diseases including cancer, diabetes, Alzheimer's, osteoporosis and Parkinson's [46].
The pathophysiology of CS-COPD
With cigarette smoking (active or passive) being one of the chief causes of its occurrence, about 20% of cigarette smokers develop COPD. Furthermore, estimates suggest that from 25% to 33% of COPD patients are nonsmokers. Notably, CS exposure has been observed to result in irreversible damage and sustained inflammation of the airway epithelium, which might lead to COPD, although the exact pathophysiology remains elusive. CS induces the gathering of inflammatory cells (macrophages, neutrophils and lymphocytes), cytokine production, the triggering of inflammasome components (NLRP3, ASC, caspase-1), depression-related behaviours, and the enhancement of glucocorticoid receptor (GR) signalling. One in vivo study investigated the relationship and underlying molecular mechanism of CS-exposure, COPD and depression, and the evidence indicated that glucocorticoid resistance was manifested during central nervous system inflammation due to CS exposure, and a potential crosstalk-underlined mechanism between the brain and lung was found [47].
Recent studies have revealed that mitochondria are engaged in innate immune signalling that shows critical features in CS-induced inflammasome activation, pulmonary inflammation and tissue-remodelling responses. Mitochondrial dysfunction might increase intracellular oxidative stresses, decrease intracellular ATP level and cause mitochondrial DNA leakage into cytoplasm to trigger different inflammasome pathways. It has been revealed that mitochondria play a crucial role on the pathogenesis of CS-induced COPD [48]. While earlier studies have explored the character of membrane-bound Toll-like receptors in CS-induced inflammation, scarce information is available about the role of cytosolic NLRs in modulating CS-mediated inflammatory responses. The key role of the P2X7–NACHT, LRR and PYD domain-containing protein 3–ASC–caspase-1/11–IL-1β/IL-18 axis in CS-induced airway inflammation highlights this pathway as a probable therapeutic target for the treatment of COPD [49]. Triggering receptors expressed on myeloid cells 1 (TREM-1) is a crucial signalling receptor that can amplify pro-inflammatory innate immune responses. The activation of TREM-1 can aggravate the formation of inflammation by activating NLRP3 inflammasome pathways, and blocking TREM-1 may inhibit oxidative stress and decrease pro-inflammatory cytokine expression in order to alleviate ALI [50]. There are two proteins involved in the intercellular communication of epithelial cells: connexins 40 and 43 (Cx40, Cx43). Several studies have indicated that oxidative stress, described as the overproduction of 4-hydroxy-2-nonenal (4-HNE), is a crucial factor in pulmonary fibrosis [51]. CS exposure might induce the activation of nuclear factor-κB (NF-κB) and increase the formation of 4HNE-Cx40 adducts that may cause lung epithelium losses to intercellular junctions and remodelling.
After exposure to CS extract (CSE), 16 human airway epithelial (16HBE) cells increase lactate dehydrogenase release, upregulate the transcription and translation of NLRP3 inflammasome, and augment caspase-1 activity; enhanced IL-1β and IL-18 cytokine release has also been observed. In addition, NLRP3 is required to activate caspase-1. The results suggest that 16HBE cells treated with NLRP3 small interfering RNA or a caspase-1 inhibitor to silence NLRP3 expression can cause a decrease of IL-1β release and cell pyroptosis. CSE-induced inflammation contributed to pyroptosis via the reactive oxygen species (ROS)–NLRP3–caspase-1 pathway in the 16HBE cells. Thereby, NLRP3 inflammasome participated in CSE-induced cell damage and pyroptosis, which affords a new insight into COPD [52].
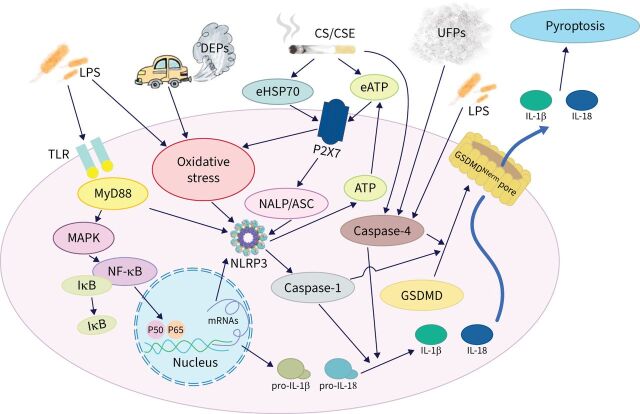
In general, the activation of NLRP3 inflammasome and subsequent cytokine secretion is a life-threatening step for innate immune responses. The activation of NLRP3 inflammasome is triggered by several internal and external factors and consequently results in inflammatory cytokine secretion. Inflammasome formation and activity play risky roles in several pathologies of diseases, such as cardiovascular, digestive, lung, metabolic, renal and central nervous system diseases [53]. CS and CSE exposure may induce inflammation and contribute to epithelial cell pyroptosis through the ROS–NLRP3–caspase-1 pathway in airway and lung tissues [52]. CS exposure leads to acute and chronic injury in lung tissues, as well as acting on the endothelial cells of the cardiovascular system to cause cell pyroptosis and the shrinkage of tunica intima/endocardium and epithelium in the bladder. The activation of NLRP3 inflammasome in endothelial cells by inducible nitric oxide synthase (iNOS) following CS exposure may be mediated by the soluble guanylyl cyclase–cyclic guanosine monophosphate–protein kinase G–tumour necrosis factor-α (TNF-α)-converting enzyme (TACE)–TNF-α pathway [54] as well as CS-induced pyroptosis of bladder tissues by activated the ROS–NLRP3–caspase-1 signalling pathway through the NLRP3 inflammasome activation relative pathways [55]. The nicotine in CS can decrease cell viability and induce ROS generation by triggering the NLRP6 inflammasome and provoke ER stress in human kidney cells to cause chronic kidney disease [56]. GSDMD undergoes proteolytic cleavage with caspase-1 to release its N-terminal fragment, which in turn mediates IL-18 and IL-1β secretions and causes pyroptosis. Pyroptosis is an inflammatory form of PCD, defined as being caspase-GSDMD-dependent. The NLRP3 inflammasome plays an indispensable role in mediating GSDMD activation. Asthma or infections may induce airway inflammation and cell pyroptosis via NLRP3 signalling pathways to cause capase-1 activation. Activated caspase-1 catalyses pro-IL-1β and pro-IL-18 to form IL-1β and IL-18; however, it cleaves GSDMD to form GSDMD N-terminal fragment (GSDMDNterm), which assembles into GSDMDNterm membrane pores and releases pro-inflammatory cytokines, IL-1β and IL-18, and subsequently causes pyroptosis [57, 58]. Current evidence has demonstrated that the NLRP3 inflammasome signalling axis could functionally mediate CS-induced inflammation, cytokine release, mucus production and pyroptosis in airway mucosa, which might be a critical mechanism associated with CS-induced airway remodelling. The involvement of signal pathways or targets in CS-induced lung injury or COPD from current investigations is summarised in table 1. Moreover, the signal pathways or targets of the inflammasomes activated in COPD are illustrated in figure 1.
TABLE 1.
Summary of the involvement of signal pathways or targets in cigarette smoke (CS)-induced lung injury or COPD from current investigations
| Induction model (in vitro) | Induction model (in vivo) | Significant findings | Ref. |
|
CSE treatment: A549 cells
CSE treatment: BEAS-2B cells |
TRP ion channels, TRPA1 and TRPV1, mediate CSE-induced damage of bronchial and alveolar epithelial cells via modulation of oxidative stress, inflammation and mitochondrial damage. | [59] | |
|
CSE/LPS treatment: MDM cells
CSE/LPS treatment: THP-1 cells |
Increased caspase-1 activity via an NLRP3-independent and TLR4–TRIF–caspase-8-dependent pathway. | [60] | |
| CSE treatment: 16HBE cells | CS exposure: male C57BL/6J mice, 30 days, with twice LPS (30 μg per 6 μL) intratracheal instillation | CSE-induced inflammation and contributed to pyroptosis through the ROS–NLRP3–caspase-1 pathway in 16HBE cells. | [52] |
|
CSE treatment: NCI-H292, 16HBE, NHBE cells
CSE treatment: THP-1 cells, MDM cells |
CSE- and eHSP70-induced ATP secretion and differential activation of NLRP3 inflammasome. | [61] | |
| CSE treatment: THP-1 cells, MDM cells | CS exposure: male C57BL/6 mice, 6 months exposure | CSE decreased NLRP3 protein abundance via increased ubiquitin-mediated proteasomal processing. The release of IL-1β and IL-18 was also decreased with CSE. Provides mechanistic insights on immunosuppression in smokers. | [62] |
| CSE treatment: THP-1 cells | CS exposure: C57BL/6 mice, 5 weeks exposure | CS repressed central components of the innate immune response to inhaled asbestos. | [63] |
| CSE treatment: THP-1 cells | MyD88 inhibition markedly attenuated the expression of NLRP3 markers (NLRP3, caspase-1, IL-1β and IL-18), IL-6, SOCS3 and NF-κB. | [64] | |
| CSE/LPS treatment: A549 cells | NLRP3 inflammasome is upregulated in COPD exacerbation and novel biomarkers for COPD exacerbation. | [65] | |
| CS exposure: male C57BL/6 mice (wild type, ASC−/–, NALP3−/–, IPAF−/–, IL-1β−/–, IL-1α−/–, IL-18−/–, IL-18R–/–, caspase-1/11–/– and caspase-11–/–), 3 days LPS (1 mg·mL–1) aerosol for 30 min | A key role for the P2X7–NALP3–ASC–caspase-1/11–IL-1β–IL-18 axis in CS-induced airway inflammation. | [9] | |
| Fresh-frozen lung tissues from COPD patients and healthy CS exposure: NLRX1−/– mutant mice and wild-type mice, exposure 3 months |
CS-dependent NLRX1 inhibition facilitates MAVS/RHL activation and subsequent inflammation, remodelling, protease, cell death, and inflammasome responses. | [66] | |
| CS exposure: female BALB/c mice, exposure 6 weeks plus gestation and lactation periods | Maternal CSE had adverse impacts on the male offspring's lungs, which were partially alleviated by maternal L-carnitine supplementation. Females were less affected by the adverse effects of maternal CSE. | [67] | |
| CSE treatment: RAW264.7 cells | CS exposure: male C57BL/6J mice, exposure 15 weeks | TREM-1 promoted the lung injury and inflammation in COPD mouse through activation of NLRP3 inflammasome-mediated pyroptosis. A novel mechanism of TREM-1 in COPD development. | [68] |
|
CSE treatment: RAW 264.7 cells
LPS treatment: RAW 264.7 cells DEP treatment: RAW 264.7 cells |
PPE (15 μg per 50 μL) intratracheal instillation: C57BL/6 female mice | The NLRP3 inflammasome is activated by DEPs in ex vivo tissue explants from elastase-induced emphysema animal model. NAC inhibits this activation. | [69] |
|
UFP treatment: COPD and non-COPD PBMCs
UFP treatment: smoker and non-smoker PBMCs |
Combustion-generated UFPs induced the release of caspase-4-dependent inflammasome from PBMCs of COPD patients compared with healthy subjects. | [70] | |
| CS exposure: SD rats for 2 months with twice LPS (200 μg per 100 μL) intratracheal instillation | SIRT1 attenuated apoptosis and ER stress in the lung tissues. A positive correlation was identified between SIRT1 and oxygen regulated protein 150. | [71] |
16HBE: human airway epithelial cell; A549: alveolar epithelial cell; ASC: apoptosis-associated speck-like protein containing a caspase recruitment domain; BEAS-2B: human bronchial epithelial cell; CSE: cigarette smoke extract; DEP: diesel exhaust particle; ER: endoplasmic reticulum; eHSP70: extracellular heat shock protein 70kDa; IL: interleukin; IPAF: interleukin converting enzyme protease activating factor; LPS: lipopolysaccharide; MAVS: mitochondrial antiviral signalling protein; MDM: human monocyte-derived macrophage; NAC: N-acetylcysteine (an ROS scavenger); NALP3: NACHT, LRR and PYD domains-containing protein 3; NCI-H292: human lung mucoepidermoid carcinoma cell; NF-κB: nuclear factor-κB; NHBE: normal human bronchial epithelial cell; NLRP3: nucleotide-binding oligomerisation domain-like receptor family, pyrin domain containing protein-3; NLRX1: nucleotide-binding oligomerisation domain, leucine rich repeat containing X1; PBMC: human peripheral blood mononuclear cell; PPE: porcine pancreatic elastase; RAW 264.7: mouse macrophage; RHL: RIG-I-like helicase; ROS: reactive oxygen species; SD: Sprague Dawley; SIRT1: sirtuin 1; SOCS3: suppressor of cytokine signalling 3; THP-1: monocytic leukaemic cell line; TLR: Toll-like receptor; TREM-1: triggering receptor expressed on myeloid cells 1; TRIF: TIR-domain-containing adaptor-inducing interferon-β; TRP: transient receptor potential protein; TRPA1: transient receptor potential cation channel, subfamily A, member 1; TRPV1: transient receptor potential cation channel subfamily V member 1; UFP: ultrafine particulate.
FIGURE 1.
The relationships between current investigations of the signal pathways or targets of inflammasomes involved in COPD. ASC: apoptosis-associated speck-like protein containing a caspase recruitment domain; CS: cigarette smoke; CSE: cigarette smoke extract; DEP: diesel exhaust particle; eATP: extracellular ATP; eHSP70: extracellular heat shock protein 70kDa; GSDMD: gasdermin D; IL: interleukin; LPS: lipopolysaccharide; MAPK: mitogen-activated protein kinase; NALP: NACHT, LRR and PYD domains-containing protein; NF-κB: nuclear factor-κB; NLRP3: nucleotide-binding oligomerisation domain-like receptor family, pyrin domain containing protein-3; TLR: Toll-like receptor; UFP: ultrafine particulate.
Polyphenols treatment via inflammasome in a cigarette smoking model
Currently, there is great interest in the role of inflammasomes in chronic inflammatory lung diseases and their targeting potential for therapy [7]. As alternative therapies, phytocompounds have been broadly used for destruction of inflammatory responses before. Selected phytochemicals have shown inhibitory properties on NLRP3 inflammasome activity in in vitro and in vivo tests [53]. Some flavonoids perform anti-inflammatory effects through the obstruction of NF-κB and NLRP3 inflammasome, suppression of pro-inflammatory cytokine IL-1β, IL-2, IL-6, TNF-α and IL-17A production, down-regulation of chemokines, and decrease of reactive nitrogen species and ROS. The most effective flavonoids for inflammation and modified immune responses are apigenin, quercetin and epigallocatechin-3-gallate (EGCG), although other compounds are still under investigation and cannot be omitted. The promising future of these compounds in different therapies has been discussed [72]. EGCG is the most plentiful catechin in green tea and provides protection against oxidative stress, lipid peroxidation and inflammatory responses caused by CS. Treatment with EGCG can decrease ROS production and suppress the lipid peroxidation induced by CSE and 4-HNE–protein adduct formation in airway epithelial cells. Further, it can inhibit CSE-induced NF-κB activity to decrease pro-inflammatory gene expression (cyclooxygenase-2 (COX-2), IL-6, IL-8, NADPH oxidase 4 (NOX4), iNOS, intercellular adhesion molecule 1, matrix metalloproteinase-9, cyclin-D1) via inhibition of the CSE-induced mitogen-activated protein kinase (MAPK) pathway [73, 74]. EGCG can restore superoxide dismutase (SOD) and catalase activities in the lungs and decrease CS-induced goblet cell hyperplasia and emphysema [75]. CS promotes mucus secretion and has a strongly effects the synthesis and secretion of MUC5AC [76]. Theaflavins are flavonoids extracted from black tea and are major antioxidants with protective effects. These effects are ascribed to the following major polyphenols: theaflavin, theaflavin-3-gallate, theaflavin-3′-gallate and theaflavin-3,3′-digallate [77]. Oral treatments with theaflavins showed the inhibition of epidermal growth factor receptor (EGFR) activation by CS and relieved airway mucous hypersecretion to reduce the levels of mucin MUC5AC [78]. Alternatively, treatment with theaflavin-3,3'-digallate significantly promoted the anti-oxidation capacity of lung tissues and attenuated CSE-induced emphysema and lung injury. Theaflavin-3,3'-digallate can decrease the generation of ROS and the expression levels of TNF-α, IL-1β and IL-6 of BEAS-2B (human bronchial epithelial) cells and inhibits necroptosis via the mediation of p38 MAPK–receptor-interacting serine–threonine-protein kinase 3 (RIPK3)–mixed lineage kinase domain-like pseudokinase (MLKL) signalling pathways. The pro-inflammatory cytokine IL-1 is catalysed by capase-1 from activated NLRP3 inflammasome. The protective effects of theaflavin-3,3'-digallate might inhibit NLRP3 pathways [79].
Flavonoids, e.g. (-)-epicatechin, increase tripartite motif-containing protein 25 and nuclear factor erythroid 2-related factor 2 (Nrf2) protein expression to promote ubiquitin-mediated Keap1 degradation and inhibit the activation of NLRP3 inflammasome by CS stimulation [80]. In the CS-induced airway inflammation of rats, baicalin treatment can modulate the histone deacetylase 2 (HDAC2)–NF-κB–plasminogen activator inhibitor type-1 signalling pathway to attenuate inflammation [81]. In the CS-induced COPD model, the TREM-1 level was increased, which activated the NLRP3 inflammasome pathway to aggravate tissue inflammation and lung injury [68]. TREM-1 is a crucial signalling receptor that can amplify pro-inflammatory innate immune responses. The activation of TREM-1 can aggravate the formation of inflammations by activating NLRP3 inflammasome pathways. Blocking TREM-1 may inhibit oxidative stress and decrease pro-inflammatory cytokine expression in response to ALI [50]. TREM-1, as the macrophage's cell surface receptor, is involved in the spread of the inflammatory response to bacterial infections or LPS challenges. Pre-treatment with quercetin, resveratrol and tea polyphenols can inhibit the secretion/shedding of soluble TREM-1 [82–84]. Quercetin is one of polyphenols that functions as an ROS scavenger and adenosine monophosphate-activated protein kinase (AMPK) activator. Peripheral blood mononuclear cells from COPD patients treated with quercetin can activate AMPK and promote the expression of Nrf2, which was found to reverse CSE-induced corticosteroid insensitivity [85]. Quercetin can protect and reduce the oxidative stress of macrophages from CSE exposure via reducing the levels of leukocytes, oxidative stress, histological pattern alterations of pulmonary parenchyma and lung function alterations [86]. In vitro CSE-induced results showed that several fatty acid esters of quercetin-3-O-glucoside had a protective potential against nicotine-induced cell death, membrane lipid peroxidation, and ameliorated the inflammation biomarkers COX-2 and prostaglandin E2 expression [87]. An in vitro study has shown that jaboticabin and 3,3'-dimethyellagic acid-4-O-sulphate are polyphenols originating from jaboticaba and exhibit anti-inflammatory activities induced by CSE [88]. Extracts of Tussilago farfara have a high polyphenol content and excellent antioxidant and good antimicrobic properties [89]. CS-induced lung inflammation can be attenuated by using ethanol extract from T. farfara flower buds through mediating the NLRP3 inflammasome, NF-κB and Nrf2 pathways [90]. N-Acetylcysteine has shown the potential to improve the immune state of COPD patients and a COPD animal model by downregulating pro-inflammatory and inflammatory cytokines, including IL-1β, IFN-γ, TNF-α and IL-18, through modulating and suppressing the NLRP3 inflammasome pathways of macrophages [91]. Magnesium isoglycyrrhizinate (MgIG), glycyrrhizic acid, is an anti-inflammatory agent originally used for treating hepatitis. Animals treated with MgIG experienced reduced inflammatory cell infiltration and accumulation in broncho-alveolar lavage. Decreased IL-6 and TNF-α production was revealed in the serum of CS/LPS-induced COPD rats through the inhibition of NLRP3 pathways [80]. For protection against epithelial injury by CS exposure, corilagin can reduce CS-induced intercellular junction breakdown on epitheliums by inhibiting 4HNE-Cx40 adduct formation and NF-κB activation to diminish CS-induced epithelial changes [92].
Gallic acid (GA) is a natural phenolic composite with high free radical scavenging potential to act as an antioxidant and anti-inflammatory agent [93]. GA treatment can restrain elastase-induced neutrophil infiltration and elevate myeloperoxidase (MPO) activity. In addition, production of the pro-inflammatory cytokines IL-6, TNF-α and IL-1β is suppressed by phosphorylation of p65NF-κB and IκBα with the down-regulation of IL-1β/TNF-α/keratinocyte chemoattractant/macrophage inflammatory protein-2/granulocyte colony stimulating factor gene expression. GA also suppressed the influx of neutrophils and macrophages induced by CS and dampened the expression of TNF-α/MIP-2/KC genes. This could significantly restore the levels of glutathione reductase and catalase, as well as reduce xanthine oxidase activity in lung tissues to attenuate and modulate the tissue oxidative stress and inflammation induced by CS [94, 95]. Exposure to particulate matter (PM) from air pollution decreases Nrf2 expression; GA can restore antioxidant status through activating the Nrf2 pathway to prevent and attenuate lung injury from PM exposure [96]. In CS-induced acute and chronic lung injuries, supplements with pomegranate juice can significantly protect lung tissue from injuries and decrease the expression of inflammatory mediators, apoptosis and oxidative stress [97]. In CSE and porcine pancreatic elastase (PPE)-induced animal models, spray instillations with salvianolic acid B significantly improved the bioavailability about 30∼100 fold over oral administration. The anti-emphysema effects of salvianolic acid B can reduce CSE-induced apoptosis and lipid peroxidation, elevate phosphor-signal transducer and activator of transcription 3 and vascular endothelial growth factor (VEGF) expression, and stimulate lung cell proliferation to enable the reversal of alveolar structural destruction in vivo [98]. CSE may cause inflammation and increase the tissue oxidative stress that leads to decreased elastin formation of fibroblasts by inhibiting the enzyme activity of lysyl oxidase [99]. The bioavailability of isorhapontigenin by oral administration is high and it has good anti-inflammatory effects and pharmacokinetic properties [100]. In vitro cells treated with isorhapontigenin can effectively reduce the levels of ROS and display cytokine-suppressing effects through the inhibited phosphoinositide 3-kinase (PI3K)/protein kinase B (Akt) pathway, which is insensitive to corticosteroids [101]. Silymarin has been reported to attenuate the chronic inflammation and oxidative stress in a CS-induced COPD model and the anti-inflammatory effect of silymarin may thoroughly suppress the activity of the extracellular signal-regulated kinases (ERK)/MAPK pathway [102, 103]. Murine orally received isoflavones led to reduced CS-induced pro-inflammatory cytokine gene expression, decreased inflammatory cells in the bronchoalveolar lavage fluid (BALF) and shrunk pulmonary emphysema [104]. Curcumin is a naturally existing polyphenolic compound present in the rhizome of Curcuma longa belonging to the family Zingiberaceae. The biological activity of curcumin to regulate the function of multiple signal pathways or transductions is linked with the attenuation of acute and chronic diseases. Numerous pre-clinical and clinical studies have demonstrated that curcumin modulated several mediators in cell signal transduction pathways including Akt, AMPK, activator protein 1, β-catenin, enhancer binding protein α, ERK5, p38/MAPK, mammalian target of rapamycin (mTOR), MyD-88, NLRP3 inflammasome, Notch-1, Nrf2, P21 (RAC1) activated kinase 1, PI3K, peroxisome proliferator-activated receptor γ (PPARγ), Rac1, Shh, STAT3, TGF-β, Toll-like receptor (TLR)-4 and Wnt [105–107]. The use of adjuvants such as piperine, curcumin nanoparticles, liposomal curcumin and the curcumin phospholipid complex showed the enhanced bioavailability and therapeutic potential [105]. In vitro, curcumin treatment can activate the PPARγ pathway and inhibit the NF-κB pathway to attenuate CSE-induced cell death and inflammatory cytokine expression. In vivo CS exposure can down-regulate the PPARγ+ cell number in lung tissues; while curcumin treatment can restore it and hinder TNF-α and IL-6 levels of serum to mitigate CS-induced inflammation [106]. Oral curcumin administration can increase the antioxidant gene expression in alveolar macrophage and lung tissue, such as oxygenase-1, glutamate-cysteine ligase and glutathione reductase, increase MPO activity, and decrease the neutrophils and macrophages in BALF to decrease intratracheal PPE- and CS-induced pulmonary inflammation and emphysema in mice [107]. Effective anti-inflammation corticosteroids are widely used in clinical therapies for asthma and COPD treatment. The suppression of pro-inflammatory gene expression by corticosteroids is based on the recruitment of the transcriptional co-repressor HDAC2 into an activated GR complex [108]. Chronic oxidative stress in COPD lungs is impeded HDAC2 activity [109], which blocks steroid efficacy or causes desensitisation [110]. Curcumin can restore and promote HDAC2 expression and activity, which may reverse the steroid insensitivity of asthma or CS-induced COPD [111]. In ALI induced by a serious infection, e.g. sepsis, curcumin treatment can hinder NF-κB, NLRP3 and pyroptosis-related protein expressions and increase sirtuin 1 (SIRT1) expression to demonstrate the protective effects of curcumin on septic ALI through up-regulation of SIRT1 to modulate the NLRP3 inflammasome pathway [112]. The major limiting factor of curcumin medical applications is its low bioavailability. However, there is a new treatment formulation using dry powder inhalation of curcumin for COPD that can provide good solubility and dissolution [113]. There are several classes of polyphenols present in apple juice, including flavanols, dihydrochalcones, flavan-3-ols and phenolic acids. Apple phenolics function as strong anti-inflammatory agents by shielding tissues from inflammatory injury [114]. Animals that received the oral administrate of apple polyphenols had significantly decreased oxidative stress and expression of pro-inflammatory factors in the lungs, reduced CS-induced accumulation of inflammatory cells in airways and lung, which might be partially reduced by inhibiting the P38/MAPK signalling pathway [115]. Increasing studies have illustrated the favourable therapeutic effects of resveratrol against lung diseases by preventing ageing, inflammation, oxidative stress, fibrosis and cancer in vitro and in vivo. Treatment with resveratrol can hinder inflammatory cytokine IL-1β and stimulated anti-inflammatory cytokine IL-8 release from alveolar macrophages in COPD [116]. Additionally, resveratrol treatment attenuates CSE-mediated glutathione (GSH) depletion in alveolar epithelial cells by promoting GSH synthesis and Nrf2 activity [117].
Corticosteroids are inefficient for reducing IL-8 and granulocyte-macrophage colony-stimulating factor (GM-CSF) release from alveolar macrophages, and inflammatory mediators released from the airways smooth the muscle cells of COPD patients. Resveratrol treatment can reduce the release of IL-8 and GM-CSF and restore VEGF release from human airway smooth muscle cells in COPD [118]. The combinative treatment of resveratrol and dexamethasone can significantly reduce all inflammatory parameters [119]. Resveratrol treatment can upregulate SIRT1 and proliferator-activated receptor-γ coactivator-1α (PGC-1α) expression to decrease the level of malondialdehyde and increase activity of SOD [71, 120]. In an in vivo CS-induced or LPS treatment COPD model, oxidative stress and inflammation caused injury to respiratory and cardiovascular systems. Treatment with resveratrol could reduce cardiac oxidative damage, prevent left ventricular remodelling and restore the expression of SIRT1 in the hearts of aged rats with emphysema [121] and may have a protective effect against CSE-induced apoptosis of human bronchial epithelial cells [122]. In an elastase-induced pulmonary emphysema COPD model, the expression of VEGFA, Nrf2, manganese SOD and airspace volume were significantly augmented in the lung tissues of the resveratrol treatment group [123]. In a combined LPS/CE-induced COPD model, resveratrol could significantly decrease the inflammatory cells in BALF and the level of inflammatory-IL-17, IL-6, IL-8, TNF-α and TGF-β cytokines in the lungs [124].
In CS exposure-induced chronic bronchitis, naringin treatment can significantly reduce the concentrations of IL-8, leukotriene B4 and TNF-α in BALF and improve SOD activity in lung tissues [125]. Naringin is a flavanone glycoside found in citrus fruits and grapefruit that is characterised by the following effects: antioxidation, anti-peroxidation and anti-inflammation [126]. Naringin treatment can significantly reduce ovalbumin-induced coughs and airway hyper-responsiveness and inhibit inflammatory cell infiltration and IL-4, IL-5 and IL-13 in BALF [127]. Naringin can restore the IL-10 level, prevent CS-induced neutrophil infiltration and decrease the activation of MPO and MMP-9 with suppressed inflammatory cytokine release, such as TNF-α and IL-8, in a CS-exposed animal model [128]. Liquiritin apioside is a flavonoid from Glycyrrhiza uralensis that can protect lung epithelial cells from CS-induced injury by increasing the levels of anti-oxidative GSH and obstructing the expressions of TGF-β and TNF-α [129].
Additionally, some flavonoids and polyphenols have been found to perform or moderate the AIM2 inflammasome pathway. Quercetin treatment was found to impede NLRP3 inflammasome and the expression of pro-caspase-1 as well as suppressing the expression of AIM2 in a dose-dependent fashion in in vitro and in vivo investigations [130, 131]. Treatment with EGCG failed to decrease AIM2 expression, but it could down-regulate the expression of active caspase-1 and IL-1β in epidermal keratinocytes [132]. Several flavonoids have been demonstrated to have multiple inhibiting effects on different inflammasomes. Glycyrrhizin, one of the triterpenoids, has hindering effects on both NLRP3 and AIM2 inflammasomes to decrease the formation of active-form caspase-1 and IL-1β release [133]. Isorhamnetin can impede AIM2 and NLRP3 inflammasome to decrease several pro-inflammatory cytokine expressions, such as IL-1α, β, IL-18, TGF-β and hyperoside; it suppresses the activation of AIM2 and NLRC4 inflammasome but does not affect cytokine expression [134]. In vitro, THP-1 cells treated with apigenin significantly inhibit NLRP3 and AIM2 inflammation to reduce caspase-1 and IL-1β production [135]. The activation of AIM2 inflammasome expression in A549 and H460 cells could be suppressed by luteolin in a concentration-dependent manner [136]. Some flavonoids can serve as activators of inflammasome, i.e. icariside I and bavachin. Icariside I can promote and regulate bone remodelling and is considered to be a candidate compound for osteoporosis treatment [137]. Bavachin can increase the mRNA levels of oestrogen-responsive genes and serve as the activator of oestrogen receptor [138]. A recent study showed that bavachin and icariside I could selectively exacerbate NLRP3 inflammasome but not NLRC4 or AIM2 to promote the expression and activity of caspase-1, TNF-α and IL-1β and that may cause idiosyncratic hepatocyte toxicity [138, 139].
Alternative treatments via inflammasome-mediation for COPD
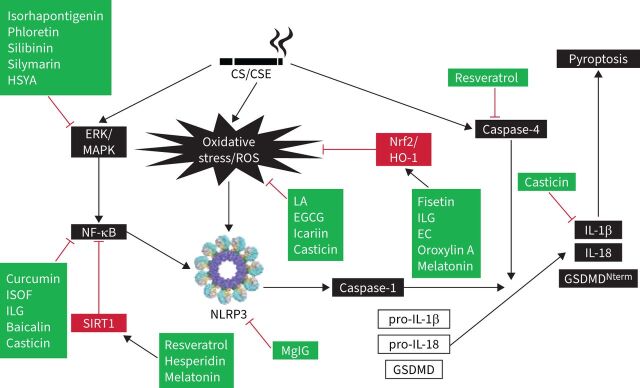
Hydrogen sulphide played a protective role in PM-induced mice emphysema and airway inflammation by hampering the formation of NLRP3 inflammasome and apoptosis via the Nrf2-dependent pathway [140]. Recently, low-molecular-weight anti-inflammatory agents, including antioxidants, inflammasome inhibitors, kinase inhibitors, modulators of inflammatory mediators, phosphodiesterase-4 inhibitors, protease inhibitors, and other agents have shed light on the development of COPD treatment. The molecular docking results of low-molecular-weight agents and targeted proteins provide new insights for targeted COPD treatments, particularly for small-molecule agents [141]. Melatonin showed protection against COPD in vitro and in vivo tests. It activated the intracellular antioxidant thioredoxin-1 (thereby inhibiting the thioredoxin-interacting protein–NLRP3 pathway) and suppressing the impaired mitophagy-mediated inflammasome activation (upregulating PTEN-induced kinase 1, Parkin and LC3B-II expression). Melatonin also enhanced the overall anti-oxidative status of a COPD lung via Nrf2–haem oxygenase-1 axis restoration [142]. Melatonin attenuated airway inflammation via SIRT1-dependent inhibition of NLRP3 inflammasome and IL-1β in rats challenged with CS and LPS [143]. MCC950 is a potent and selective inhibitor of NLRP3 inflammasome and reduced the mRNA expressions of IL-1β, IL-8, TGF-β and MMP-9. At 24 h after LPS instillation, MCC950 could also reduce the protein levels of IL-1β, IL-18 and caspase-1 in mice [144]. Lipoxin receptor agonist (BML-111) may prevent the activation of NLRP3 inflammasome and hinder ROS production via upregulation of Nrf2 in COPD model mice [145]. Forskolin and isoforskolin (ISOF) are polyphenols isolated from Coleus forskohlii and have been reported to have anti-inflammatory and anti-oxidative effects [146]. Forskolin inhibited the activation of NLRP3 inflammasome and decreased the secretions of IL-1β and IL-18 from macrophages [147, 148]. ISOF alleviated the acute exacerbation of COPD by prompting pulmonary function and mitigating inflammation via downregulation of pro-inflammatory cytokines (TNF-α, IL-1β, IL-6), monocyte chemoattractant protein-1, monokine induced by interferon-γ, IP-10, C-reactive protein, Th17/IL-17A and NF-κB/NLRP3 pathways in CS-induced mice [149]. ISOF also tempered IL-1β and IL-18 secretion by NLRP3 inflammasome activation in human macrophages [150]. Treatment with ISOF can downregulate the mTOR level in lung tissues and increase intracellular cyclic adenosine monophosphate levels to relax the histamine-induced contraction of the lungs and trachea smooth muscles. Pre-treatment with ISOF significantly ameliorated the pathological damage to lung tissue and improved pulmonary function in COPD and airway hyper-responsive rats [149, 151]. The differential impact of macrolides-azithromycin on the inflammasome–IL-1β axis may be of consequence in inflammasome-driven diseases, e.g. COPD and asthma [152]. Histidine repressed the activation of NLRP3 inflammasome in both PPE- and LPS-induced COPD mouse models and in vitro mouse alveolar macrophage MH-S cells [153]. Coixol inhibited MAPKs, NF-κB pathways and the activation of NLRP3 inflammasome in LPS-induced RAW 264.7 cells [154]. After long-term PM-exposure-induced lung inflammation and fibrosis, resveratrol intervention improved these adverse effects by preventing autophagy-related NLRP3 inflammasome activation [155]. CS-challenged mice were treated with flavonoids isolated from loquat (Eriobotrya japonica) leaves, the results revealed that flavonoids have a protective effect and putative mechanism of the action of total flavonoids resulted in the inhibition of inflammation and oxidative stress through the regulation of transient receptor potential vanilloid 1 and related signal pathways in lung tissues [156]. Table 2 lists the mediating roles of polyphenols and flavonoids on the amelioration of CS-induced NLRP3 inflammasome in COPD. Additionally, figure 2 illustrates the acting target molecules of the polyphenols and flavonoids on the signal pathways of CS-induced NLRP3 inflammasome. From this diagram, it is obvious that this has been separated into three approaches: the first, CS/CSE, causes the involvement of CS-induced inflammasome signal pathways (shown in black boxes) and the second is the attenuating mediators of regulating signals (shown in red boxes). Thirdly, the acting targets of polyphenols and flavonoids are displayed in green boxes (figure 2). Moreover, quercetogetin suppressed mitophagy-dependent apoptosis by inhibiting the expression of cleaved caspase-3, -8 and -9, and downregulating caspase activity in human lung bronchial epithelial cells (BEAS-2B cells) exposed to CSE [157].
TABLE 2.
The mediating roles of polyphenols and flavonoids on the amelioration of cigarette smoke (CS)-induced inflammasome in COPD
| Active substances | Induction model | Key findings | Ref. |
| Astragalin (kaempferol-3-glucoside), a flavonoid from leaves of persimmon and green tea seeds | CS exposure: BALB/c mice CSE treatment: A549 cells |
Astragalin may interrupt the smoking-induced oxidative stress–MAPK signalling–inflammation axis via disconnection between alveolar PAR activation and pulmonary thromboembolism. | [164] |
| Curcumin | CS exposure: male SD rats CSE treatment: BEAS-2B cells |
Curcumin attenuated CS-induced inflammation in vivoand in vitro, by modulating the PPARγ–NF-κB pathway. | [106] |
| Fisetin, a flavone from apples strawberries and onion | CS exposure: male Wistar rats | Fisetin blunted CS-induced oxidative stress and inflammation in the lungs and prevented tissue damage via the Nrf2-mediated upregulation of antioxidant gene expression. | [165] |
| Hesperidin, a flavanone glycoside | CSE injection: C57BL/6 mice male and female mixed | Hesperidin alleviated inflammation and oxidative stress responses in CSE-induced COPD mice, associated with SIRT1/PGC-1α/NF-κB signalling axis. | [166] |
| Icariin, a flavonoid from Epimedium brevicornum Maxim (Berberidaceae) | CSE treatment: BEAS-2B cells | Decreased CSE-induced inflammation, airway remodelling and ROS production by mitigating GC resistance. Icariin combination with GC can potentially increase therapeutic efficacy and reduce GC resistance in COPD. | [167] |
| ISOF, a flavonoid from Coleus forskohlii | CS exposure: mice and infected with influenza virus A/Puerto Rico/8/34 (H1N1), Th17 cells | The levels of inflammatory mediators (TNF-α, IL-1β, IL-6, IL-17A, MCP-1, MIG, IP-10 and CRP) in the lung homogenate were reduced after ISOF treatment. ISOF alleviated AECOPD by improving pulmonary function and attenuating inflammation via the downregulation of pro-inflammatory cytokines, Th17–IL-17A and NF-κB–NLRP3 pathways. | [149] |
| Isoliquiritigenin, a polyphenol from Glycyrrhizae radix | CS exposure: male C57BL/6N mice | Isoliquiritigenin protected against CS-induced COPD by inhibiting inflammatory and oxidative stress via the regulation of the Nrf2 and NF-κB signalling pathways. | [168] |
| Isorhapontigenin, a polyphenol from Belamcanda chinensis | CS exposure: SD rats CSE treatment: primary HAECs (healthy and COPD), A549 cells |
Isorhapontigenin reduced the activation of NF-κB and AP-1 and notably the PI3 K–Akt–FoxO3A pathway was insensitive to dexamethasone. | [101] |
| Liquiritin apioside, a flavonoid from Glycyrrhiza uralensis | CS exposure: ICR mice CSE treatment: A549 cells |
The protective role of liquiritin apioside on CS-induced the lung epithelial cell injury and are mediated by inhibiting TGF-β and TNF-α expression and increasing anti-oxidative levels of GSH. | [129] |
| MgIG | CS exposure: male Wistar rats with endotracheal-atomized LPS | MgIG might be an alternative for COPD treatment, and the suppression of NLRP3 inflammasome. | [80] |
| Oroxylin A, a flavonoid from Scutellaria baicalensis Georgi | CS exposure: male C57BL/6 mice CSE treatment: BEAS-2B, RAW264.7 cells |
Oroxylin A attenuated oxidative stress and lung inflammation by CS-induced via activating the Nrf2 signalling pathway. | [169] |
| Phloretin, a polyphenol from Prunus mandshurica | CS exposure: male BALB/c mice CSE treatment: NCI-H292 cells |
The protective effect of phloretin on CS-related airway mucus hypersecretion and inflammation, where EGFR, ERK and P38 might be involved. | [170] |
| Sal-B, a polyphenol of danshen | PPE endotracheal treatment: male SD rats CSE intraperitoneal treatment: male SD rats |
Sal-B as one of the first anti-emphysema agents enabling reversal of alveolar structural destruction and loss via local lung treatment by STAT3 activation and VEGF stimulation. | [98] |
| EGCG | CSE treatment: NHBE cells | EGCG sequestered 4-hydroxynonenal and inhibited NF-κB activation, antioxidative and anti-inflammatory effects of EGCG in CSE-treatment AECs. | [73] |
| EC, flavonoid | CS exposure: male Wistar rats CSE treatment: BEAS-2B cells |
The protective effect of EC on experimental COPD rats and elucidated the mechanism of EC promoting Nrf2 activity. | [171] |
| Baicalin, a polyphenol of Scutellaria baicalensis | CS exposure: male SD rats, CSE treatment: HBEpCs | Baicalin ameliorated CS-induced airway inflammation in rats, and these effects were partially attributed to the modulation of HDAC2–NF-κB–PAI-1 signalling. | [81] |
| CS exposure: male BALB/c mice CSE treatment: A549 cells |
Anti-inflammatory effects in CS-induced inflammatory models in mice and A549 cells, achieved by modulating HDAC2. | [172] | |
| Casticin, a flavonoid from Vitex species (Vitex rotundifolia, Vitex agnus-castus) | CS exposure: male Wistar rats | Casticin protected lungs against COPD via improving lung function and inhibition of oxidative stress and inflammation via the reduction of pro-inflammatory cytokines (TNF-α, IL-1β and IL-6). | [173] |
| CS exposure: female C57BL/6 mice | Casticin had significant effects on the lung inflammation induced by CS in a COPD mouse model. | [174] | |
| Naringenin, a flavanone from grapefruit | CS exposure: male BALB/c mice CSE treatment: A549 cells |
Naringenin inhibited the production of pro-inflammatory cytokines such as IL-8, TNF-α, and MMP9 in the BALF and serum of CS-induced animals. | [175] |
| Naringin, a flavonoid glycoside from grapefruit and citrus fruits | CS exposure: male and female guinea pigs | Naringin exhibited antitussive, anti-AHR and anti-inflammation effects on chronic CS exposure-induced chronic bronchitis of guinea pigs. | [125] |
| CS exposure: male and female SD rats | Naringin prevented CS-induced infiltration of neutrophils and activation of MPO and MMP-9, in parallel with suppression of the release of cytokines, TNF-α, IL-8 and IL-10. | [128] | |
| Quercetin, a flavonoid | CSE treatment: J774A.1 cells CSE injection: male C57BL/6 mice | An effective adjuvant effects from quercetin for treating CS exposure. | [176] |
| CSE treatment: U937 cells, COPD patient PBMC | Quercetin restored corticosteroid sensitivity, to be a novel treatment in combination with corticosteroids in COPD. | [85] | |
| Resveratrol | CS exposure: male Wistar rats | Resveratrol inhibited oxidative stress and inflammatory response via the activation and upgrading of the SIRT1/PGC-1α signalling pathways. | [120] |
| CS exposure: male Kunming mice with LPS | Resveratrol has a therapeutic effect on mouse CS-induced COPD and reduced the production of the beclin1 protein. | [124] | |
| CSE treatment: HBEpC | A protective effect against CSE-induced apoptosis, and a molecular pathway involving SIRT1 and ORP150 may be associated with the anti-apoptotic functions, caspase-3 and caspase-4 of resveratrol in HBEpC. | [122] | |
| PPE endotracheal treatment: female C57BL/6JNarl mice CSE treatment: MSC cells |
cis-Resveratrol-regulated VEGFA expression in HSP–VEGFA–MSC significantly improved the therapeutic effects in the treatment of a COPD mouse, avoiding side effects associated with constitutive VEGFA expression. | [123] | |
| CS exposure: male SD rats with LPS | Co-administered with sirtinol, a SIRT1 inhibitor. The combination therapy may serve as a potential approach for treating lung inflammatory conditions like COPD. | [119] | |
| Silibinin, a flavonoid from the milk thistle Silybum marianum | CSE treatment: NCI-H292 cells CS exposure: male C57BL/6 N mice with LPS |
Silibinin effectively suppressed the neutrophilic airway inflammation provoked by treatment with LPS and CS, which was associated with downregulation of ERK phosphorylation. | [177] |
| CS exposure: male C57BL/6N mice with LPS | Silibinin effectively inhibited the fibrotic response induced by CS+LPS exposure, via suppression of TGF-β1/Smad 2/3 signalling, resulting in reduced collagen deposition. | [178] | |
| Silymarin, a flavonoid from the seeds and fruits of milk thistle | CS exposure: male BALB/c mice | Silymarin attenuated inflammation and oxidative stress induced by CS. The anti-inflammatory effect might partly act through the MAPK pathway. | [103] |
| CSE treatment: BEAS-2B cells | Silymarin could attenuate inflammatory responses through intervening in the crosstalk between autophagy and the ERK–MAPK pathway. | [102] | |
| HSYA, a polyphenol from edible plant safflower | CS exposure: male Wistar rats with LPS | HSYA inhibited the phosphorylation of p38 MAPK in the lung tissue of rat. HSYA can attenuate experimentally induced airway remodelling and was attributed to suppression of TGF-β1 expression. | [179] |
| CS exposure: male Wistar rats | HSYA alleviated inflammatory cell infiltration and inhibited inflammatory cytokine expression and increased phosphorylation of p38 MAPK and p65 NF-κB in the lungs of COPD rats. | [180] | |
| Jaboticabin and related polyphenols from jaboticaba (Myrciaria cauliflora) | CSE treatment: SAE cells, Caco-2 cells | The polyphenols, jaboticabin and 3,3'-dimethyellagic acid-4-O-sulphate from jaboticaba both exhibited anti-inflammatory activities. | [88] |
| Apple polyphenol | CS exposure: female ICR mice | Apple polyphenol may be a potential dietary nutrient supplement agent to improve quality of life of COPD patients by inhibiting CS-induced ALI via the p38 MAPK signalling pathway. | [115] |
| DRIAs | CS exposure: male C57BL/6 mice | DRIAs significantly attenuated the pathological changes of COPD via suppression of neutrophilic inflammation. | [104] |
| Anthocyanins delphinidin and cyanidin from the edible fruits of Eugenia brasiliensis | CSE treatment: SAE cells | Delphinidin inhibited IL-8 in the CSE-treated cells in a dose-dependent manner. | [181] |
| Flower buds of Tussilago farfara L. | CS exposure: mice | FTF-EtOH effectively attenuated lung inflammation in vitroand in vivo. The protection of FTF-EtOH against inflammation was produced by activation of Nrf2 and inhibitions of NF-κB and NLRP3 inflammasome. | [90] |
| Glycyrrhiza glabra, Agastache rugosa | Coal fly ash, diesel-exhaust particle exposure: male BALB/c mice | Herbal combinational mixture more effectively inhibited neutrophilic airway inflammation by regulating the expression of inflammatory cytokines and CXCL-2 by blocking the IL-17/STAT3 pathway. | [182] |
| Pomegranate juice | CS exposure: male C57BL/6J mice CSE treatment: A549 cells |
The expression of inflammatory mediators and the emphysematous changes noted with chronic CS exposure were reduced with pomegranate juice supplementation. In vitro, pomegranate juice attenuated the damaging effects of CSE on cultured human alveolar cells. | [97] |
| Total flavonoids from sea buckthorn | CSE/LPS treatment: HBE16 cells CS exposure: male ICR mice with LPS |
Total flavonoids from sea buckthorn including quercetin and isorhamnetin showed potent binding affinities to MAPK1 and PIK3CG, two upstream kinases of ERK and Akt, respectively. Against LPS/CS-induced airway inflammation through inhibition of ERK, PI3 K/Akt and PKCα pathways. | [183] |
| Extracts of Ximenia americana L. | CS exposure: male and female rats | The aqueous extract of X. americana presents itself as a new option for CS-COPD treatment. | [184] |
| Melatonin | CS exposure: male Swiss albino mice CSE treatment: L-132 cells |
Activated the intracellular antioxidant thioredoxin-1 (thereby suppressing the TXNIP–NLRP3 pathway) and inhibited the impaired the mitophagy mediated inflammasome activation (upregulating PINK-1, Parkin, LC3B-II expression). Also improved the overall antioxidant status of the COPD lung via Nrf2–HO-1 axis restoration. | [142] |
| CSE treatment: HAECs | Melatonin effectively protected against smoking-induced vascular injury and atherosclerosis through the Nrf2–ROS–NLRP3 signalling pathway. | [185] | |
| CS exposure: male Wistar rats with LPS | Melatonin attenuated airway inflammation via SIRT1-dependent inhibition of NLRP3 inflammasome and IL-1β in COPD rats. | [143] | |
| TFEB | CSE treatment: RAW 264.7 cells | TFEB acted as autophagy-inducing drugs in restoring of CS-impaired phagocytosis. | [186] |
16HBE: human airway epithelial cells; A549: alveolar epithelial cell; AEC: airway epithelial cell; AECOPD: acute exacerbations of COPD; AHR: airway hyper-responsiveness; ALI: acute lung injury; AP-1: activator protein 1; BALF: bronchoalveolar lavage fluid; BEAS-2B: human bronchial epithelial cell; Caco-2: human intestinal cells; CSE: cigarette smoke extract; CRP: C-reactive protein; CXCL-2: chemokine (C-X-C motif) ligand 2; DRIA: daidzein-rich soy isoflavone aglycone; EC: (-)-epicatechin; EGCG: epigallocatechin gallate; EGFR: epidermal growth factor receptor; ERK: extracellular signal-regulated kinases; FTF-EtOH: ethanol extract of the flower buds of T. farfara L.; GC: glucocorticoid; GSH: glutathione; HAEC: human aortic endothelial cell; HBEpC: human bronchial epithelial cell; HDAC2: histone deacetylase 2; HO-1: haem oxygenase-1; HSP: heat shock protein; HSYA: hydroxysafflor yellow A; IL: interleukin; IP-10: interferon gamma-induced protein 10; ISOF: isoforskolin; J774A.1: mouse macrophage cells; LPS: lipopolysaccharide; MAPK: mitogen-activated protein kinase; MCP-1: monocyte chemoattractant protein-1; MgIG: magnesium isoglycyrrhizinate; MIG: monokine induced by interferon-γ; MMP9: matrix metalloproteinase-9; MPO: myeloperoxidase; MSC: human mesenchymal stem cell; NCI-H292: human lung mucoepidermoid carcinoma cell; NF-κB: nuclear factor-κB; NHBE: normal human bronchial epithelial cell; NLRP3: nucleotide-binding oligomerisation domain-like receptor family, pyrin domain containing protein-3; Nrf2: nuclear factor erythroid 2-related factor 2; ORP150: oxygen-regulated protein 150; PAI1: plasminogen activator inhibitor type-1; PAR: protease-activated receptor; PBMC: human peripheral blood mononuclear cell; PGC-1α: peroxisome proliferator-activated receptor-gamma coactivator-1α; PINK-1: PTEN-induced kinase 1; PKCα: protein kinase C alpha; PPARγ: peroxisome proliferator-activated receptor γ; PPE: porcine pancreatic elastase; RAW 264.7: mouse macrophage; ROS: reactive oxygen species; SAE: human small airway epithelial cell; Sal-B: salvianolic acid B; SD: Sprague Dawley; SIRT1: sirtuin 1; STAT3: signal transducer and activator of transcription 3; TFEB: transcription factor EB; TGF-β: transforming growth factor-β; Th17: T-helper cell 17; TNF-α: tumour necrosis factor-α; TXNIP: thioredoxin interacting protein; U937: human monocyte cells; VEGF: vascular endothelial growth factor; VEGFA: vascular endothelial growth factor A.
FIGURE 2.
The acting target molecules of polyphenols and flavonoids on the signal pathways of cigarette smoke (CS)-induced inflammasome. Black boxes represent effects of CS/cigarette smoke extract (CSE), caused by the involvement of signal pathways. Red boxes contain the attenuating mediators of regulating signals. Green boxes display the acting targets of polyphenols and flavonoids. Black arrows depict stimulation whereas red “T” bars represent suppression. EC: endothelial cell; EGCG: epigallocatechin-3-gallate; ERK: extracellular signal-regulated kinases; GSDMD: gasdermin D; HO-1: haem oxygenase-1; HSYA: hydroxysafflor yellow A; IL: interleukin; ILG: isoliquiritigenin; ISOF: isoforskolin; LA: liquiritin apioside; MAPK: mitogen-activated protein kinase; MgIG: magnesium isoglycyrrhizinate; NF-κB: nuclear factor-κB; NLRP3: nucleotide-binding oligomerisation domain-like receptor family, pyrin domain containing protein-3; Nrf2: nuclear factor erythroid 2-related factor 2; ROS: reactive oxygen species; SIRT1: sirtuin 1.
Future perspectives
Inflammation plays a vital role in the development of COPD. Pyroptosis, an inflammatory form of cell death, may be implicated in the pathogenesis of COPD. The NLRP3 inflammasome enhances inflammatory cell recruitment and mediates immune responses in the lungs. Further, this is involved in numerous diseases characterised by induced lung disease by focusing on pathways causing chronic respiratory epithelial cell injury, cell death, alveolar destruction and tissue remodelling affiliated with the progress of ALI and COPD. The experimental findings may afford mechanistic insights into the immunosuppression in smokers via the CS-activated ROS–NLRP3 axis and induced epithelial cells pyroptosis. According to the abovementioned section, polyphenols and flavonoids may have therapeutic potential in CS-COPD and present exclusive opportunities to develop an approach or strategy to modulate immune functionality via mediating NLRP3 inflammasome. Corticosteroids are the most-used anti-inflammatory agent for asthma and COPD. However, people with severe asthma or COPD show poor response to the anti-inflammatory effects of corticosteroids. The Corticosteroid resistance is a main therapeutic challenge to the management of COPD. Prominently, resveratrol, icariin and quercetin could restore the sensitivity of corticosteroid, and, in combination with corticosteroids, have the potential to form novel treatments for COPD. A panel of clinically effective drugs has displayed potential in restoring steroid- resistance in experimental models. It is highly plausible that some of these phytocompounds or molecules can be efficaciously repositioned for clinical use in the management of COPD. One clinical trial has reported that 21 COPD patients (forced expiratory volume in 1 s (FEV1) 53±15% predicted; age 67±9 years; body mass index 24.5±3.3 kg·m−2) received resveratrol (150 mg·day−1) or placebo for 4 weeks, the results failed to ratify the previously designated positive effects of resveratrol on the mitochondrial function of skeletal muscle in patients with COPD [158]. In mild-to-severe lung disease, COPD patients with FEV1 ranging between >35% and <80% were recruited and supplemented with either quercetin (500∼2000 mg·day−1) or placebo for 1 week. The patients showed no drug-related severe adverse manifestations based on blood tests, which contained complete blood counts and an evaluation of a comprehensive metabolic panel [159].
Questions for future research
Remarkably, underlying mechanisms and some possible causes have led to inconsistent results in observational studies and supplementation trials because investigations in this field are mostly limited to animal models or small clinical trials. More forthcoming cohorts and well-designed clinical trials are needed to support the introduction of individualised phytochemical interventions into health policy.
Points for clinical practice
Recently, NLRP3 inflammasome has been confirmed to play a significant role in the pathogenesis of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and is involved in the cytokine storm formation of ALI associated with coronavirus disease 2019 (COVID-19). Up to date, there are more than 1300 scientific articles that have looked into the link between COPD and COVID-19, and more than 280 reports have explored the inflammasome mechanisms in the pathogenesis of COVID-19. Notably, there is accumulating evidence that the inducers, components, pathways and effectors of inflammasome signal pathways are attributed to the pathogenesis in COPD and SARS-CoV-2 infection [160, 161]. On the other hand, SARS-CoV-2 infection may cause more severity in COPD patients [162]. A clinical report found that curcumin can mediate and down-regulate the NLRP3 inflammasome relative intracellular signal transduction pathways that are involved in inflammation of COVID-19 patients [163]. This is an electrifying outcome for combating COVID-19 and creates a new hope for promoting drug development from the medicinal perspective of curcumin.
Footnotes
Provenance: Submitted article, peer reviewed.
Author contributions: N. Kang, Y. Yu and Y. Mi participated in paper collection and data analysis. Y-S. Fu, J. Guo and J. Wu did manuscript draft preparation. Y-S. Fu and C-F. Weng critically discussed and reviewed the manuscript. All authors have reviewed and approved the final version of manuscript for submission and publication.
Conflict of interest: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest with regard to the content of this report.
Support statement: This work is financially supported by Xiamen Medical College for C-F. Weng (K2019-01).
References
- 1.Wu CT, Li GH, Huang CT, et al. Acute exacerbation of a chronic obstructive pulmonary disease prediction system using wearable device data, machine learning, and deep learning: development and cohort study. JMIR mHealth uHealth 2021; 9: e22591. doi: 10.2196/22591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aghapour M, Ubags ND, Bruder D, et al. Role of air pollutants in airway epithelial barrier dysfunction in asthma and COPD. Eur Respir Rev 2022; 31: 210112. doi: 10.1183/16000617.0112-2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Keir HR, Chalmers JD. Neutrophil extracellular traps in chronic lung disease: implications for pathogenesis and therapy. Eur Respir Rev 2022; 31: 210241. doi: 10.1183/16000617.0241-2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang W, Li F, Li C, et al. Focus on early COPD: definition and early lung development. Int J Chron Obstruct Pulmon Dis 2021; 16: 3217–3228. doi: 10.2147/COPD.S338359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Devasahayam J, LaFreniere K, Naik R. Chronic emphysema. In: StatPearls. Treasure Island, StatPearls Publishing; 2021. Available from: www.ncbi.nlm.nih.gov/books/NBK539910 [PubMed] [Google Scholar]
- 6.Wilkinson TMA. Immune checkpoints in chronic obstructive pulmonary disease. Eur Respir Rev 2017; 26: 170045. doi: 10.1183/16000617.0045-2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pinkerton JW, Kim RY, Robertson A, et al. Inflammasomes in the lung. Mol Immunol 2017; 86: 44–55. doi: 10.1016/j.molimm.2017.01.014 [DOI] [PubMed] [Google Scholar]
- 8.Kaplanski G. Interleukin-18: biological properties and role in disease pathogenesis. Immunol Rev 2018; 281: 138–153. doi: 10.1111/imr.12616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dima E, Koltsida O, Katsaounou P, et al. Implication of interleukin (IL)-18 in the pathogenesis of chronic obstructive pulmonary disease (COPD). Cytokine 2015; 74: 313–317. doi: 10.1016/j.cyto.2015.04.008 [DOI] [PubMed] [Google Scholar]
- 10.Schroder K, Tschopp J. The inflammasomes. Cell 2010; 140: 821–832. doi: 10.1016/j.cell.2010.01.040 [DOI] [PubMed] [Google Scholar]
- 11.Guo H, Callaway JB, Ting JP. Inflammasomes: mechanism of action, role in disease, and therapeutics. Nat Med 2015; 21: 677–687. doi: 10.1038/nm.3893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Martinon F, Gaide O, Pétrilli V, et al. NALP inflammasomes: a central role in innate immunity. Semin Immunopathol 2007; 29: 213–229. doi: 10.1007/s00281-007-0079-y [DOI] [PubMed] [Google Scholar]
- 13.Caneparo V, Landolfo S, Gariglio M, et al. The absent in melanoma 2-like receptor IFN-inducible protein 16 as an inflammasome regulator in systemic Lupus erythematosus: the dark side of sensing microbes. Front Immunol 2018; 9: 1180. doi: 10.3389/fimmu.2018.01180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Zoete MR, Palm NW, Zhu S, et al. Inflammasomes. Cold Spring Harb Perspect Biol 2014; 6: a016287. doi: 10.1101/cshperspect.a016287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chavarría-Smith J, Vance RE. The NLRP1 inflammasomes. Immunol Rev 2015; 265: 22–34. doi: 10.1111/imr.12283 [DOI] [PubMed] [Google Scholar]
- 16.Cassel SL, Joly S, Sutterwala FS. The NLRP3 inflammasome: a sensor of immune danger signals. Semin Immunol 2009; 21: 194–198. doi: 10.1016/j.smim.2009.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schell U, Simon S, Hilbi H. Inflammasome recognition and regulation of the Legionella flagellum. Curr Top Microbiol Immunol 2016; 397: 161–181. [DOI] [PubMed] [Google Scholar]
- 18.Man SM, Karki R, Kanneganti TD. AIM2 inflammasome in infection, cancer, and autoimmunity: role in DNA sensing, inflammation, and innate immunity. Eur J Immunol 2016; 46: 269–280. doi: 10.1002/eji.201545839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lorenz G, Darisipudi MN, Anders HJ. Canonical and non-canonical effects of the NLRP3 inflammasome in kidney inflammation and fibrosis. Nephrol Dial Transplant 2014; 29: 41–48. doi: 10.1093/ndt/gft332 [DOI] [PubMed] [Google Scholar]
- 20.Wright SS, Vasudevan SO, Rathinam VA. Mechanisms and consequences of noncanonical inflammasome-mediated pyroptosis. J Mol Biol 2022; 434: 167245. doi: 10.1016/j.jmb.2021.167245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vance RE. The NAIP/NLRC4 inflammasomes. Curr Opin Immunol 2015; 32: 84–89. doi: 10.1016/j.coi.2015.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sundaram B, Kanneganti TD. Advances in understanding activation and function of the NLRC4 inflammasome. Int J Mol Sci 2021; 22: 1048. doi: 10.3390/ijms22031048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guo Q, Wu Y, Hou Y, et al. Cytokine secretion and pyroptosis of thyroid follicular cells mediated by enhanced NLRP3, NLRP1, NLRC4, and AIM2 inflammasomes are associated with autoimmune thyroiditis. Front Immunol 2018; 9: 1197. doi: 10.3389/fimmu.2018.01197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sharma BR, Karki R, Kanneganti TD. Role of AIM2 inflammasome in inflammatory diseases, cancer and infection. Eur J Immunol 2019; 49: 1998–2011. doi: 10.1002/eji.201848070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang B, Bhattacharya M, Roy S, et al. Immunobiology and structural biology of AIM2 inflammasome. Mol Aspects Med 2020; 76: 100869. doi: 10.1016/j.mam.2020.100869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tran HB, Hamon R, Jersmann H, et al. AIM2 nuclear exit and inflammasome activation in chronic obstructive pulmonary disease and response to cigarette smoke. J Inflamm 2021; 18: 19. doi: 10.1186/s12950-021-00286-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Colarusso C, Terlizzi M, Lamort AS, et al. Caspase-11 and AIM2 inflammasome are involved in smoking-induced COPD and lung adenocarcinoma. Oncotarget 2021; 12: 1057–1071. doi: 10.18632/oncotarget.27964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Colarusso C, Terlizzi M, Molino A, et al. AIM2 inflammasome activation leads to IL-1α and TGF-β release from exacerbated chronic obstructive pulmonary disease-derived peripheral blood mononuclear cells. Front Pharmacol 2019; 10: 257. doi: 10.3389/fphar.2019.00257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eltom S, Belvisi MG, Stevenson CS, et al. Role of the inflammasome-caspase1/11-IL-1/18 axis in cigarette smoke driven airway inflammation: an insight into the pathogenesis of COPD. PLoS One 2014; 9: e112829. doi: 10.1371/journal.pone.0112829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chong WC, Shastri MD, Peterson GM, et al. The complex interplay between endoplasmic reticulum stress and the NLRP3 inflammasome: a potential therapeutic target for inflammatory disorders. Clin Transl Immunology 2021; 10: e1247. doi: 10.1002/cti2.1247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wiegman CH, Li F, Ryffel B, et al. Oxidative stress in ozone-induced chronic lung inflammation and emphysema: a facet of chronic obstructive pulmonary disease. Front Immunol 2020; 11: 1957. doi: 10.3389/fimmu.2020.01957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huang Y, Xu W, Zhou R. NLRP3 inflammasome activation and cell death. Cell Mol Immunol 2021; 18: 2114–2127. doi: 10.1038/s41423-021-00740-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Downs KP, Nguyen H, Dorfleutner A, et al. An overview of the non-canonical inflammasome. Mol Aspects Med 2020; 76: 100924. doi: 10.1016/j.mam.2020.100924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sun X, Kang TB, Lee KH. In vitro and in vivo model for sepsis through non-canonical NLRP3 inflammasome activation. Methods Mol Biol 2022; 2459: 137–147. doi: 10.1007/978-1-0716-2144-8_14 [DOI] [PubMed] [Google Scholar]
- 35.Wu R, Wang N, Comish PB, et al. Inflammasome-dependent coagulation activation in sepsis. Front Immunol 2021; 12: 641750. doi: 10.3389/fimmu.2021.641750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lopez-Castejon G. Control of the inflammasome by the ubiquitin system. FEBS J 2020; 287: 11–26. doi: 10.1111/febs.15118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hosseinian N, Cho Y, Lockey RF, et al. The role of the NLRP3 inflammasome in pulmonary diseases. Ther Adv Respir Dis 2015; 9: 188–197. doi: 10.1177/1753465815586335 [DOI] [PubMed] [Google Scholar]
- 38.Usmani J, Khan T, Ahmad R, et al. Potential role of herbal medicines as a novel approach in sepsis treatment. Biomed Pharmacother 2021; 144: 112337. doi: 10.1016/j.biopha.2021.112337 [DOI] [PubMed] [Google Scholar]
- 39.Li X, Zhao J, Yan T, et al. Cyanidin-3-O-glucoside and cisplatin inhibit proliferation and downregulate the PI3 K/AKT/mTOR pathway in cervical cancer cells. J Food Sci 2021; 86: 2700–2712. doi: 10.1111/1750-3841.15740 [DOI] [PubMed] [Google Scholar]
- 40.Riyaphan J, Pham DC, Leong MK, et al. In silico approaches to identify polyphenol compounds as α-glucosidase and α-amylase inhibitors against type-II diabetes. Biomolecules 2021; 11: 1877. doi: 10.3390/biom11121877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Panche AN, Diwan AD, Chandra SR. Flavonoids: an overview. J Nutr Sci 2016; 5: e47. doi: 10.1017/jns.2016.41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Islam BU, Suhail M, Khan MK, et al. Polyphenols as anticancer agents: toxicological concern to healthy cells. Phytother Res 2021; 35: 6063–6079. doi: 10.1002/ptr.7216 [DOI] [PubMed] [Google Scholar]
- 43.Khan J, Deb PK, Priya S, et al. Dietary flavonoids: cardioprotective potential with antioxidant effects and their pharmacokinetic, toxicological and therapeutic concerns. Molecules 2021; 26: 4021. doi: 10.3390/molecules26134021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Contente ML, Annunziata F, Cannazza P, et al. Biocatalytic approaches for an efficient and sustainable preparation of polyphenols and their derivatives. J Agric Food Chem 2021; 69: 13669–13681. doi: 10.1021/acs.jafc.1c05088 [DOI] [PubMed] [Google Scholar]
- 45.Hendawy OM. Nano-delivery systems for improving therapeutic efficiency of dietary polyphenols. Altern Ther Health Med 2021; 27: 162–177. [PubMed] [Google Scholar]
- 46.Maleki Dana P, Sadoughi F, Mansournia MA, et al. Targeting Wnt signaling pathway by polyphenols: implication for aging and age-related diseases. Biogerontology 2021; 22: 479–494. doi: 10.1007/s10522-021-09934-x [DOI] [PubMed] [Google Scholar]
- 47.Deng X, Fu J, Song Y, et al. Glucocorticoid receptor dysfunction orchestrates inflammasome effects on chronic obstructive pulmonary disease-induced depression: a potential mechanism underlying the cross talk between lung and brain. Brain Behav Immun 2019; 79: 195–206. doi: 10.1016/j.bbi.2019.02.001 [DOI] [PubMed] [Google Scholar]
- 48.Kang MJ, Shadel GS. A mitochondrial perspective of chronic obstructive pulmonary disease pathogenesis. Tuberc Respir Dis 2016; 79: 207–213. doi: 10.4046/trd.2016.79.4.207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mortaz E, Adcock IM, Shafei H, et al. Role of P2X7 receptors in release of IL-1β: a possible mediator of pulmonary inflammation. Tanaffos 2012; 11: 6–11. [PMC free article] [PubMed] [Google Scholar]
- 50.Liu T, Zhou Y, Li P, et al. Blocking triggering receptor expressed on myeloid cells-1 attenuates lipopolysaccharide-induced acute lung injury via inhibiting NLRP3 inflammasome activation. Sci Rep 2016; 6: 39473. doi: 10.1038/srep39473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Reyes-Jiménez E, Ramírez-Hernández AA, Santos-Álvarez JC, et al. Involvement of 4-hydroxy-2-nonenal in the pathogenesis of pulmonary fibrosis. Mol Cell Biochem 2021; 476: 4405–4419. doi: 10.1007/s11010-021-04244-9 [DOI] [PubMed] [Google Scholar]
- 52.Zhang MY, Jiang YX, Yang YC, et al. Cigarette smoke extract induces pyroptosis in human bronchial epithelial cells through the ROS/NLRP3/caspase-1 pathway. Life Sci 2021; 269: 119090. doi: 10.1016/j.lfs.2021.119090 [DOI] [PubMed] [Google Scholar]
- 53.Olcum M, Tastan B, Ercan I, et al. Inhibitory effects of phytochemicals on NLRP3 inflammasome activation: a review. Phytomedicine 2020; 75: 153238. doi: 10.1016/j.phymed.2020.153238 [DOI] [PubMed] [Google Scholar]
- 54.Liao K, Lv DY, Yu HL, et al. iNOS regulates activation of the NLRP3 inflammasome through the sGC/cGMP/PKG/TACE/TNF-α axis in response to cigarette smoke resulting in aortic endothelial pyroptosis and vascular dysfunction. Int Immunopharmacol 2021; 101: 108334. doi: 10.1016/j.intimp.2021.108334 [DOI] [PubMed] [Google Scholar]
- 55.Wu Z, Liu Q, Zhu K, et al. Cigarette smoke induces the pyroptosis of urothelial cells through ROS/NLRP3/caspase-1 signaling pathway. Neurourol Urodyn 2020; 39: 613–624. doi: 10.1002/nau.24271 [DOI] [PubMed] [Google Scholar]
- 56.Zheng CM, Lee YH, Chiu IJ, et al. Nicotine causes nephrotoxicity through the induction of NLRP6 inflammasome and α7 nicotinic acetylcholine receptor. Toxics 2020; 8: 92. doi: 10.3390/toxics8040092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Burdette BE, Esparza AN, Zhu H, et al. Gasdermin D in pyroptosis. Acta Pharm Sin B 2021; 11: 2768–2782. doi: 10.1016/j.apsb.2021.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zhuang J, Cui H, Zhuang L, et al. Bronchial epithelial pyroptosis promotes airway inflammation in a murine model of toluene diisocyanate-induced asthma. Biomed Pharmacother 2020; 125: 109925. doi: 10.1016/j.biopha.2020.109925 [DOI] [PubMed] [Google Scholar]
- 59.Wang M, Zhang Y, Xu M, et al. Roles of TRPA1 and TRPV1 in cigarette smoke -induced airway epithelial cell injury model. Free Radic Biol Med 2019; 134: 229–238. doi: 10.1016/j.freeradbiomed.2019.01.004 [DOI] [PubMed] [Google Scholar]
- 60.Buscetta M, Di Vincenzo S, Miele M, et al. Cigarette smoke inhibits the NLRP3 inflammasome and leads to caspase-1 activation via the TLR4-TRIF-caspase-8 axis in human macrophages. Faseb j 2020; 34: 1819–1832. doi: 10.1096/fj.201901239R [DOI] [PubMed] [Google Scholar]
- 61.Rumora L, Somborac-Bacura A, Hlapcic I, et al. Cigarette smoke and extracellular Hsp70 induce secretion of ATP and differential activation of NLRP3 inflammasome in monocytic and bronchial epithelial cells. Cytokine 2020; 135: 155220. doi: 10.1016/j.cyto.2020.155220 [DOI] [PubMed] [Google Scholar]
- 62.Han S, Jerome JA, Gregory AD, et al. Cigarette smoke destabilizes NLRP3 protein by promoting its ubiquitination. Respir Res 2017; 18: 2. doi: 10.1186/s12931-016-0485-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Morris GF, Danchuk S, Wang Y, et al. Cigarette smoke represses the innate immune response to asbestos. Physiol Rep 2015; 3: e12652. doi: 10.14814/phy2.12652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mehta S, Dhawan V. Molecular insights of cigarette smoke condensate-activated NLRP3 inflammasome in THP-1 cells in a stage-specific atherogenesis. Int Immunopharmacol 2020; 88: 107013. doi: 10.1016/j.intimp.2020.107013 [DOI] [PubMed] [Google Scholar]
- 65.Nachmias N, Langier S, Brzezinski RY, et al. NLRP3 inflammasome activity is upregulated in an in-vitro model of COPD exacerbation. PLoS One 2019; 14: e0214622. doi: 10.1371/journal.pone.0214622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kang MJ, Yoon CM, Kim BH, et al. Suppression of NLRX1 in chronic obstructive pulmonary disease. J Clin Invest 2015; 125: 2458–2462. doi: 10.1172/JCI71747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wang B, Chan YL, Zhou S, et al. Offspring sex affects the susceptibility to maternal smoking-induced lung inflammation and the effect of maternal antioxidant supplementation in mice. J Inflamm 2020; 17: 24. doi: 10.1186/s12950-020-00253-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wang L, Chen Q, Yu Q, et al. TREM-1 aggravates chronic obstructive pulmonary disease development via activation NLRP3 inflammasome-mediated pyroptosis. Inflamm Res 2021; 70: 971–980. doi: 10.1007/s00011-021-01490-x [DOI] [PubMed] [Google Scholar]
- 69.Uh ST, Koo SM, Kim Y, et al. The activation of NLRP3-inflammsome by stimulation of diesel exhaust particles in lung tissues from emphysema model and RAW 264.7 cell line. Korean J Intern Med 2017; 32: 865–874. doi: 10.3904/kjim.2016.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.De Falco G, Colarusso C, Terlizzi M, et al. Chronic obstructive pulmonary disease-derived circulating cells release IL-18 and IL-33 under ultrafine particulate matter exposure in a caspase-1/8-independent manner. Front Immunol 2017; 8: 1415. doi: 10.3389/fimmu.2017.01415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zhang L, Luo B, Ting Y, et al. SIRT1 attenuates endoplasmic reticulum stress and apoptosis in rat models of COPD. Growth Factors 2020; 38: 94–104. doi: 10.1080/08977194.2020.1810029 [DOI] [PubMed] [Google Scholar]
- 72.Martinez G, Mijares MR, De Sanctis JB. Effects of flavonoids and its derivatives on immune cell responses. Recent Pat Inflamm Allergy Drug Discov 2019; 13: 84–104. doi: 10.2174/1872213X13666190426164124 [DOI] [PubMed] [Google Scholar]
- 73.Lakshmi SP, Reddy AT, Kodidhela LD, et al. Epigallocatechin gallate diminishes cigarette smoke-induced oxidative stress, lipid peroxidation, and inflammation in human bronchial epithelial cells. Life Sci 2020; 259: 118260. doi: 10.1016/j.lfs.2020.118260 [DOI] [PubMed] [Google Scholar]
- 74.Syed DN, Afaq F, Kweon MH, et al. Green tea polyphenol EGCG suppresses cigarette smoke condensate-induced NF-κB activation in normal human bronchial epithelial cells. Oncogene 2007; 26: 673–682. doi: 10.1038/sj.onc.1209829 [DOI] [PubMed] [Google Scholar]
- 75.Chan KH, Ho SP, Yeung SC, et al. Chinese green tea ameliorates lung injury in cigarette smoke-exposed rats. Respir Med 2009; 103: 1746–1754. doi: 10.1016/j.rmed.2009.04.027 [DOI] [PubMed] [Google Scholar]
- 76.Haswell LE, Hewitt K, Thorne D, et al. Cigarette smoke total particulate matter increases mucous secreting cell numbers in vitro: a potential model of goblet cell hyperplasia. Toxicol In Vitro 2010; 24: 981–987. doi: 10.1016/j.tiv.2009.12.019 [DOI] [PubMed] [Google Scholar]
- 77.Misra A, Chattopadhyay R, Banerjee S, et al. Black tea prevents cigarette smoke-induced oxidative damage of proteins in guinea pigs. J Nutr 2003; 133: 2622–2628. doi: 10.1093/jn/133.8.2622 [DOI] [PubMed] [Google Scholar]
- 78.Wu H, Li Q, Zhou X, et al. Theaflavins extracted from black tea inhibit airway mucous hypersecretion induced by cigarette smoke in rats. Inflammation 2012; 35: 271–279. doi: 10.1007/s10753-011-9314-8 [DOI] [PubMed] [Google Scholar]
- 79.Luan G, Zhu Z, Wu K, et al. Theaflavin-3,3ʹ-digallate attenuates cigarette smoke extract-induced pulmonary emphysema in mice by suppressing necroptosis. Exp Ther Med 2022; 23: 11. doi: 10.3892/etm.2021.10933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Yang Y, Huang L, Tian C, et al. Magnesium isoglycyrrhizinate inhibits airway inflammation in rats with chronic obstructive pulmonary disease. BMC Pulm Med 2021; 21: 371. doi: 10.1186/s12890-021-01745-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Zhang H, Liu B, Jiang S, et al. Baicalin ameliorates cigarette smoke-induced airway inflammation in rats by modulating HDAC2/NF-κB/PAI-1 signalling. Pulm Pharmacol Ther 2021; 70: 102061. doi: 10.1016/j.pupt.2021.102061 [DOI] [PubMed] [Google Scholar]
- 82.Lagha AB, Grenier D. Tea polyphenols inhibit the activation of NF-κB and the secretion of cytokines and matrix metalloproteinases by macrophages stimulated with Fusobacterium nucleatum. Sci Rep 2016; 6: 34520. doi: 10.1038/srep34520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Fang K, Li HR, Chen XX, et al. Quercetin alleviates LPS-induced depression-like behavior in rats via regulating BDNF-related imbalance of copine 6 and TREM1/2 in the hippocampus and PFC. Front Pharmacol 2020; 10: 1544. doi: 10.3389/fphar.2019.01544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lagha AB, Andrian E, Grenier D. Resveratrol attenuates the pathogenic and inflammatory properties of Porphyromonas gingivalis. Mol Oral Microbiol 2019; 34: 118–130. doi: 10.1111/omi.12260 [DOI] [PubMed] [Google Scholar]
- 85.Mitani A, Azam A, Vuppusetty C, et al. Quercetin restores corticosteroid sensitivity in cells from patients with chronic obstructive pulmonary disease. Exp Lung Res 2017; 43: 417–425. doi: 10.1080/01902148.2017.1393707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Machado-Junior PA, Araujo NPS, Souza ABF, et al. Protective effects of quercetin on livers from mice exposed to long-term cigarette smoke. Biomed Res Int 2020; 2020: 2196207. 10.1155/2020/2196207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Warnakulasuriya SN, Ziaullah Rupasinghe HP. Novel long chain fatty acid derivatives of quercetin-3-O-glucoside reduce cytotoxicity induced by cigarette smoke toxicants in human fetal lung fibroblasts. Eur J Pharmacol 2016; 781: 128–138. doi: 10.1016/j.ejphar.2016.04.011 [DOI] [PubMed] [Google Scholar]
- 88.Zhao DK, Shi YN, Petrova V, et al. Jaboticabin and related polyphenols from Jaboticaba (Myrciaria cauliflora) with anti-inflammatory activity for chronic obstructive pulmonary disease. J Agric Food Chem 2019; 67: 1513–1520. doi: 10.1021/acs.jafc.8b05814 [DOI] [PubMed] [Google Scholar]
- 89.Sacks D, Baxter B, Campbell BCV, et al. Multisociety consensus quality improvement revised consensus statement for endovascular therapy of acute ischemic stroke. Int J Stroke 2018; 13: 612–632. [DOI] [PubMed] [Google Scholar]
- 90.Xu LT, Wang T, Fang KL, et al. The ethanol extract of flower buds of Tussilago farfara L. attenuates cigarette smoke-induced lung inflammation through regulating NLRP3 inflammasome, Nrf2, and NF-êB. J Ethnopharmacol 2022; 283: 114694. doi: 10.1016/j.jep.2021.114694 [DOI] [PubMed] [Google Scholar]
- 91.Liu X, Lu X, Hu Z. N-Acetylcysteine (NAC) inhibits synthesis of IL-18 in macrophage by suppressing NLRP3 expression to reduce the production of IFN-γ from NK cells. Comput Math Methods Med 2021; 2021: 7596343. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 92.Muresan XM, Cervellati F, Sticozzi C, et al. The loss of cellular junctions in epithelial lung cells induced by cigarette smoke is attenuated by corilagin. Oxid Med Cell Longev 2015; 2015: 631758. doi: 10.1155/2015/631758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Singla E, Puri G, Dharwal V, et al. Gallic acid ameliorates COPD-associated exacerbation in mice. Mol Cell Biochem 2021; 476: 293–302. doi: 10.1007/s11010-020-03905-5 [DOI] [PubMed] [Google Scholar]
- 94.Singla E, Dharwal V, Naura AS. Gallic acid protects against the COPD-linked lung inflammation and emphysema in mice. Inflamm Res 2020; 69: 423–434. doi: 10.1007/s00011-020-01333-1 [DOI] [PubMed] [Google Scholar]
- 95.Qamar W, Sultana S. Polyphenols from Juglans regia L. (walnut) kernel modulate cigarette smoke extract induced acute inflammation, oxidative stress and lung injury in Wistar rats. Hum Exp Toxicol 2011; 30: 499–506. doi: 10.1177/0960327110374204 [DOI] [PubMed] [Google Scholar]
- 96.Radan M, Dianat M, Badavi M, et al. In vivo and in vitro evidence for the involvement of Nrf2-antioxidant response element signaling pathway in the inflammation and oxidative stress induced by particulate matter (PM10): the effective role of gallic acid. Free Radic Res 2019; 53: 210–225. doi: 10.1080/10715762.2018.1563689 [DOI] [PubMed] [Google Scholar]
- 97.Husari A, Hashem Y, Bitar H, et al. Antioxidant activity of pomegranate juice reduces emphysematous changes and injury secondary to cigarette smoke in an animal model and human alveolar cells. Int J Chron Obstruct Pulmon Dis 2016; 11: 227–237. doi: 10.2147/COPD.S97027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Dhapare S, Li H, Sakagami M. Salvianolic acid B as an anti-emphysema agent II: in vivo reversal activities in two rat models of emphysema. Pulm Pharmacol Ther 2018; 53: 52–60. doi: 10.1016/j.pupt.2018.09.002 [DOI] [PubMed] [Google Scholar]
- 99.Polettini J, Silva MG, Kacerovsky M, et al. Screening of lysyl oxidase (LOX) and lysyl oxidase like (LOXL) enzyme expression and activity in preterm prelabor rupture of fetal membranes. J Perinat Med 2016; 44: 99–109. doi: 10.1515/jpm-2014-0337 [DOI] [PubMed] [Google Scholar]
- 100.Dai Y, Yeo SCM, Barnes PJ, et al. Pre-clinical pharmacokinetic and metabolomic analyses of isorhapontigenin, a dietary resveratrol derivative. Front Pharmacol 2018; 9: 753. doi: 10.3389/fphar.2018.00753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Yeo SCM, Fenwick PS, Barnes PJ, et al. Isorhapontigenin, a bioavailable dietary polyphenol, suppresses airway epithelial cell inflammation through a corticosteroid-independent mechanism. Br J Pharmacol 2017; 174: 2043–2059. doi: 10.1111/bph.13803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Li D, Hu J, Wang T, et al. Silymarin attenuates cigarette smoke extract-induced inflammation via simultaneous inhibition of autophagy and ERK/p38 MAPK pathway in human bronchial epithelial cells. Sci Rep 2016; 6: 37751. doi: 10.1038/srep37751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Li D, Xu D, Wang T, et al. Silymarin attenuates airway inflammation induced by cigarette smoke in mice. Inflammation 2015; 38: 871–878. doi: 10.1007/s10753-014-9996-9 [DOI] [PubMed] [Google Scholar]
- 104.Kojima K, Asai K, Kubo H, et al. Isoflavone aglycones attenuate cigarette smoke-induced emphysema via suppression of neutrophilic inflammation in a COPD murine model. Nutrients 2019; 11: 2023. doi: 10.3390/nu11092023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Patel SS, Acharya A, Ray RS, et al. Cellular and molecular mechanisms of curcumin in prevention and treatment of disease. Crit Rev Food Sci Nutr 2020; 60: 887–939. doi: 10.1080/10408398.2018.1552244 [DOI] [PubMed] [Google Scholar]
- 106.Li Q, Sun J, Mohammadtursun N, et al. Curcumin inhibits cigarette smoke-induced inflammation via modulating the PPARγ-NF-κB signaling pathway. Food Funct 2019; 10: 7983–7994. doi: 10.1039/C9FO02159K [DOI] [PubMed] [Google Scholar]
- 107.Suzuki M, Betsuyaku T, Ito Y, et al. Curcumin attenuates elastase- and cigarette smoke-induced pulmonary emphysema in mice. Am J Physiol Lung Cell Mol Physiol 2009; 296: L614–L623. doi: 10.1152/ajplung.90443.2008 [DOI] [PubMed] [Google Scholar]
- 108.Leung DY, Bloom JW. Update on glucocorticoid action and resistance. J Allergy Clin Immunol 2003; 111: 3–22. doi: 10.1067/mai.2003.97 [DOI] [PubMed] [Google Scholar]
- 109.Ito K, Hanazawa T, Tomita K, et al. Oxidative stress reduces histone deacetylase 2 activity and enhances IL-8 gene expression: role of tyrosine nitration. Biochem Biophys Res Commun 2004; 315: 240–245. doi: 10.1016/j.bbrc.2004.01.046 [DOI] [PubMed] [Google Scholar]
- 110.Footitt J, Mallia P, Durham AL, et al. Oxidative and nitrosative stress and histone deacetylase-2 activity in exacerbations of COPD. Chest 2016; 149: 62–73. doi: 10.1378/chest.14-2637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Meja KK, Rajendrasozhan S, Adenuga D, et al. Curcumin restores corticosteroid function in monocytes exposed to oxidants by maintaining HDAC2. Am J Respir Cell Mol Biol 2008; 39: 312–323. doi: 10.1165/rcmb.2008-0012OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Wang Y, Wang Y, Cai N, et al. Anti-inflammatory effects of curcumin in acute lung injury: in vivo and in vitro experimental model studies. Int Immunopharmacol 2021; 96: 107600. doi: 10.1016/j.intimp.2021.107600 [DOI] [PubMed] [Google Scholar]
- 113.Shen Q, Jiang Y, Chen J, et al. A novel curcumin-based drug powder inhalation medicine for chronic obstructive pulmonary disease. Bioinorg Chem Appl 2021; 2021: 8001787. doi: 10.1155/2021/8001787 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 114.Rana S, Bhushan S. Apple phenolics as nutraceuticals: assessment, analysis and application. J Food Sci Technol 2016; 53: 1727–1738. doi: 10.1007/s13197-015-2093-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Bao MJ, Shen J, Jia YL, et al. Apple polyphenol protects against cigarette smoke-induced acute lung injury. Nutrition 2013; 29: 235–243. doi: 10.1016/j.nut.2012.04.008 [DOI] [PubMed] [Google Scholar]
- 116.Culpitt SV, Rogers DF, Fenwick PS, et al. Inhibition by red wine extract, resveratrol, of cytokine release by alveolar macrophages in COPD. Thorax 2003; 58: 942–946. doi: 10.1136/thorax.58.11.942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Kode A, Rajendrasozhan S, Caito S, et al. Resveratrol induces glutathione synthesis by activation of Nrf2 and protects against cigarette smoke-mediated oxidative stress in human lung epithelial cells. Am J Physiol Lung Cell Mol Physiol 2008; 294: L478–L488. doi: 10.1152/ajplung.00361.2007 [DOI] [PubMed] [Google Scholar]
- 118.Knobloch J, Sibbing B, Jungck D, et al. Resveratrol impairs the release of steroid-resistant inflammatory cytokines from human airway smooth muscle cells in chronic obstructive pulmonary disease. J Pharmacol Exp Ther 2010; 335: 788–798. doi: 10.1124/jpet.110.166843 [DOI] [PubMed] [Google Scholar]
- 119.Sadarani BN, Majumdar AS. Resveratrol potentiates the effect of dexamethasone in rat model of acute lung inflammation. Int Immunopharmacol 2015; 28: 773–779. doi: 10.1016/j.intimp.2015.07.038 [DOI] [PubMed] [Google Scholar]
- 120.Wang XL, Li T, Li JH, et al. The effects of resveratrol on inflammation and oxidative stress in a rat model of chronic obstructive pulmonary disease. Molecules 2017; 22: 1529. doi: 10.3390/molecules22091529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Hu YX, Cui H, Fan L, et al. Resveratrol attenuates left ventricular remodeling in old rats with COPD induced by cigarette smoke exposure and LPS instillation. Can J Physiol Pharmacol 2013; 91: 1044–1054. doi: 10.1139/cjpp-2012-0464 [DOI] [PubMed] [Google Scholar]
- 122.Zhang L, Guo X, Xie W, et al. Resveratrol exerts an anti-apoptotic effect on human bronchial epithelial cells undergoing cigarette smoke exposure. Mol Med Rep 2015; 11: 1752–1758. doi: 10.3892/mmr.2014.2925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Chen YB, Lan YW, Chen LG, et al. Mesenchymal stem cell-based HSP70 promoter-driven VEGFA induction by resveratrol alleviates elastase-induced emphysema in a mouse model. Cell Stress Chaperone 2015; 20: 979–989. doi: 10.1007/s12192-015-0627-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Chen J, Yang X, Zhang W, et al. Therapeutic effects of resveratrol in a mouse model of LPS and cigarette smoke-induced COPD. Inflammation 2016; 39: 1949–1959. doi: 10.1007/s10753-016-0430-3 [DOI] [PubMed] [Google Scholar]
- 125.Luo YL, Zhang CC, Li PB, et al. Naringin attenuates enhanced cough, airway hyperresponsiveness and airway inflammation in a guinea pig model of chronic bronchitis induced by cigarette smoke. Int Immunopharmacol 2012; 13: 301–307. doi: 10.1016/j.intimp.2012.04.019 [DOI] [PubMed] [Google Scholar]
- 126.Zeng X, Su W, Liu B, et al. A review on the pharmacokinetic properties of naringin and its therapeutic efficacies in respiratory diseases. Mini Rev Med Chem 2020; 20: 286–293. doi: 10.2174/1389557519666191009162641 [DOI] [PubMed] [Google Scholar]
- 127.Jiao HY, Su WW, Li PB, et al. Therapeutic effects of naringin in a guinea pig model of ovalbumin-induced cough-variant asthma. Pulm Pharmacol Ther 2015; 33: 59–65. doi: 10.1016/j.pupt.2015.07.002 [DOI] [PubMed] [Google Scholar]
- 128.Nie YC, Wu H, Li PB, et al. Anti-inflammatory effects of naringin in chronic pulmonary neutrophilic inflammation in cigarette smoke-exposed rats. J Med Food 2012; 15: 894–900. doi: 10.1089/jmf.2012.2251 [DOI] [PubMed] [Google Scholar]
- 129.Guan Y, Li FF, Hong L, et al. Protective effects of liquiritin apioside on cigarette smoke-induced lung epithelial cell injury. Fundam Clin Pharmacol 2012; 26: 473–483. doi: 10.1111/j.1472-8206.2011.00956.x [DOI] [PubMed] [Google Scholar]
- 130.Lee KM, Kang JH, Yun M, et al. Quercetin inhibits the poly(dA:dT)-induced secretion of IL-18 via down-regulation of the expressions of AIM2 and pro-caspase-1 by inhibiting the JAK2/STAT1 pathway in IFN-γ-primed human keratinocytes. Biochem Biophys Res Commun 2018; 503: 116–122. doi: 10.1016/j.bbrc.2018.05.191 [DOI] [PubMed] [Google Scholar]
- 131.Domiciano TP, Wakita D, Jones HD, et al. Quercetin inhibits inflammasome activation by interfering with ASC oligomerization and prevents interleukin-1 mediated mouse vasculitis. Sci Rep 2017; 7: 41539. doi: 10.1038/srep41539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Yun M, Seo G, Lee JY, et al. Epigallocatechin-3-gallate attenuates the AIM2-induced secretion of IL-1β in human epidermal keratinocytes. Biochem Biophys Res Commun 2015; 467: 723–729. doi: 10.1016/j.bbrc.2015.10.075 [DOI] [PubMed] [Google Scholar]
- 133.Honda H, Nagai Y, Matsunaga T, et al. Isoliquiritigenin is a potent inhibitor of NLRP3 inflammasome activation and diet-induced adipose tissue inflammation. J Leukoc Biol 2014; 96: 1087–1100. doi: 10.1189/jlb.3A0114-005RR [DOI] [PubMed] [Google Scholar]
- 134.Ahn H, Lee GS. Isorhamnetin and hyperoside derived from water dropwort inhibits inflammasome activation. Phytomedicine 2017; 24: 77–86. doi: 10.1016/j.phymed.2016.11.019 [DOI] [PubMed] [Google Scholar]
- 135.Lim H, Min DS, Park H, et al. Flavonoids interfere with NLRP3 inflammasome activation. Toxicol Appl Pharmacol 2018; 355: 93–102. doi: 10.1016/j.taap.2018.06.022 [DOI] [PubMed] [Google Scholar]
- 136.Yu Q, Zhang M, Ying Q, et al. Decrease of AIM2 mediated by luteolin contributes to non-small cell lung cancer treatment. Cell Death Dis 2019; 10: 218. doi: 10.1038/s41419-019-1447-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Liu M, Xu H, Ma Y, et al. Osteoblasts proliferation and differentiation stimulating activities of the main components of Epimedii folium. Pharmacogn Mag 2017; 13: 90–94. doi: 10.4103/0973-1296.197709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Qin N, Xu G, Wang Y, et al. Bavachin enhances NLRP3 inflammasome activation induced by ATP or nigericin and causes idiosyncratic hepatotoxicity. Front Med 2021; 15: 594–607. doi: 10.1007/s11684-020-0809-2 [DOI] [PubMed] [Google Scholar]
- 139.Gao Y, Xu G, Ma L, et al. Icariside I specifically facilitates ATP or nigericin-induced NLRP3 inflammasome activation and causes idiosyncratic hepatotoxicity. Cell Commun Signal 2021; 19: 13. doi: 10.1186/s12964-020-00647-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Jia G, Yu S, Sun W, et al. Hydrogen sulfide attenuates particulate matter-induced emphysema and airway inflammation through Nrf2-dependent manner. Front Pharmacol 2020; 11: 29. doi: 10.3389/fphar.2020.00029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Ti H, Zhou Y, Liang X, et al. Targeted treatments for chronic obstructive pulmonary disease (COPD) using low-molecular-weight drugs (LMWDs). J Med Chem 2019; 62: 5944–5978. doi: 10.1021/acs.jmedchem.8b01520 [DOI] [PubMed] [Google Scholar]
- 142.Mahalanobish S, Dutta S, Saha S, et al. Melatonin induced suppression of ER stress and mitochondrial dysfunction inhibited NLRP3 inflammasome activation in COPD mice. Food Chem Toxicol 2020; 144: 111588. doi: 10.1016/j.fct.2020.111588 [DOI] [PubMed] [Google Scholar]
- 143.Peng Z, Zhang W, Qiao J, et al. Melatonin attenuates airway inflammation via SIRT1 dependent inhibition of NLRP3 inflammasome and IL-1β in rats with COPD. Int Immunopharmacol 2018; 62: 23–28. doi: 10.1016/j.intimp.2018.06.033 [DOI] [PubMed] [Google Scholar]
- 144.Wang L, Lei W, Zhang S, et al. MCC950, a NLRP3 inhibitor, ameliorates lipopolysaccharide-induced lung inflammation in mice. Bioorg Med Chem 2021; 30: 115954. doi: 10.1016/j.bmc.2020.115954 [DOI] [PubMed] [Google Scholar]
- 145.Cao Y, Zhou X, Yin Z, et al. The anti-inflammatory effect of BML-111 on COPD may be mediated by regulating NLRP3 inflammasome activation and ROS production. Prostaglandins Other Lipid Mediat 2018; 138: 23–30. doi: 10.1016/j.prostaglandins.2018.08.001 [DOI] [PubMed] [Google Scholar]
- 146.Du X, Shi R, Wang Y, et al. Isoforskolin and forskolin attenuate lipopolysaccharide-induced inflammation through TLR4/MyD88/NF-κB cascades in human mononuclear leukocytes. Phytother Res 2019; 33: 602–609. doi: 10.1002/ptr.6248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Chen Y, Wen JG, Feng JJ, et al. Forskolin attenuates the NLRP3 inflammasome activation and IL-1β secretion in human macrophages. Pediatr Res 2019; 86: 692–698. doi: 10.1038/s41390-019-0418-4 [DOI] [PubMed] [Google Scholar]
- 148.Renema P, Hardy KS, Housley N, et al. cAMP signaling primes lung endothelial cells to activate caspase-1 during Pseudomonas aeruginosa infection. Am J Physiol Lung Cell Mol Physiol 2020; 318: L1074–L1083. doi: 10.1152/ajplung.00185.2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Xiao C, Cheng S, Li R, et al. Isoforskolin alleviates AECOPD by improving pulmonary function and attenuating inflammation which involves downregulation of Th17/IL-17A and NF-κB/NLRP3. Front Pharmacol 2021; 12: 721273. doi: 10.3389/fphar.2021.721273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Xiao C, Cheng S, Lin H, et al. Isoforskolin, an adenylyl cyclase activator, attenuates cigarette smoke-induced COPD in rats. Phytomedicine 2021; 91: 153701. doi: 10.1016/j.phymed.2021.153701 [DOI] [PubMed] [Google Scholar]
- 151.Liang X, Wang J, Chen W, et al. Inhibition of airway remodeling and inflammation by isoforskolin in PDGF-induced rat ASMCs and OVA-induced rat asthma model. Biomed Pharmacother 2017; 95: 275–286. doi: 10.1016/j.biopha.2017.08.063 [DOI] [PubMed] [Google Scholar]
- 152.Gualdoni GA, Lingscheid T, Schmetterer KG, et al. Azithromycin inhibits IL-1 secretion and non-canonical inflammasome activation. Sci Rep 2015; 5: 12016. doi: 10.1038/srep12016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Tian Q, Xu M, He B. Histidine ameliorates elastase- and lipopolysaccharide-induced lung inflammation by inhibiting the activation of the NLRP3 inflammasome. Acta Biochim Biophys Sin 2021; 53: 1055–1064. doi: 10.1093/abbs/gmab072 [DOI] [PubMed] [Google Scholar]
- 154.Hu Y, Zhou Q, Liu T, et al. Coixol Suppresses NF-κB, MAPK pathways and NLRP3 inflammasome activation in lipopolysaccharide-induced RAW 264.7 cells. Molecules 2020; 25: 894. doi: 10.3390/molecules25040894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Ding S, Wang H, Wang M, et al. Resveratrol alleviates chronic ‘real-world’ ambient particulate matter-induced lung inflammation and fibrosis by inhibiting NLRP3 inflammasome activation in mice. Ecotoxicol Environ Saf 2019; 182: 109425. doi: 10.1016/j.ecoenv.2019.109425 [DOI] [PubMed] [Google Scholar]
- 156.Jian T, Chen J, Ding X, et al. Flavonoids isolated from loquat (Eriobotrya japonica) leaves inhibit oxidative stress and inflammation induced by cigarette smoke in COPD mice: the role of TRPV1 signaling pathways. Food Funct 2020; 11: 3516–3526. doi: 10.1039/C9FO02921D [DOI] [PubMed] [Google Scholar]
- 157.Son ES, Kim SH, Ryter SW, et al. Quercetogetin protects against cigarette smoke extract-induced apoptosis in epithelial cells by inhibiting mitophagy. Toxicol In Vitro 2018; 48: 170–178. doi: 10.1016/j.tiv.2018.01.011 [DOI] [PubMed] [Google Scholar]
- 158.Beijers RJ, Gosker HR, Sanders KJ, et al. Resveratrol and metabolic health in COPD: A proof-of-concept randomized controlled trial. Clin Nutr 2020; 39: 2989–2997. doi: 10.1016/j.clnu.2020.01.002 [DOI] [PubMed] [Google Scholar]
- 159.Han MK, Barreto TA, Martinez FJ, et al. Randomised clinical trial to determine the safety of quercetin supplementation in patients with chronic obstructive pulmonary disease. BMJ Open Respir Res 2020; 7: e000392. doi: 10.1136/bmjresp-2018-000392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Singh D, Mathioudakis AG, Higham A. Chronic obstructive pulmonary disease and COVID-19: interrelationships. Curr Opin Pulm Med 2022; 28: 76–83. doi: 10.1097/MCP.0000000000000834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Wieczfinska J, Kleniewska P, Pawliczak R. Oxidative stress-related mechanisms in SARS-CoV-2 infections. Oxid Med Cell Longev 2022; 2022: 5589089. doi: 10.1155/2022/5589089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Ahmad Malik J, Ahmed S, Shinde M, et al. The impact of COVID-19 on comorbidities: a review of recent updates for combating It. Saudi J Biol Sci 2022; 29: 3586–3599. doi: 10.1016/j.sjbs.2022.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Saeedi-Boroujeni A, Mahmoudian-Sani MR, Bahadoram M, et al. COVID-19: A case for inhibiting NLRP3 inflammasome, suppression of inflammation with curcumin? Basic Clin Pharmacol Toxicol 2021; 128: 37–45. doi: 10.1111/bcpt.13503 [DOI] [PubMed] [Google Scholar]
- 164.Kim YH, Kang MK, Lee EJ, et al. Astragalin inhibits cigarette smoke-induced pulmonary thrombosis and alveolar inflammation and disrupts par activation and oxidative stress-responsive MAPK-signaling. Int J Mol Sci 2021; 22: 3692. doi: 10.3390/ijms22073692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Hussain T, Al-Attas OS, Alamery S, et al. The plant flavonoid, fisetin alleviates cigarette smoke-induced oxidative stress, and inflammation in Wistar rat lungs. J Food Biochem 2019; 43: e12962. 10.1111/jfbc.12962 [DOI] [PubMed] [Google Scholar]
- 166.Wang S, He N, Xing H, et al. Function of hesperidin alleviating inflammation and oxidative stress responses in COPD mice might be related to SIRT1/PGC-1α/NF-κB signaling axis. J Recept Signal Transduct Res 2020; 40: 388–394. doi: 10.1080/10799893.2020.1738483 [DOI] [PubMed] [Google Scholar]
- 167.Hu L, Liu F, Li L, et al. Effects of icariin on cell injury and glucocorticoid resistance in BEAS-2B cells exposed to cigarette smoke extract. Exp Ther Med 2020; 20: 283–292. doi: 10.3892/etm.2020.8702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Yu D, Liu X, Zhang G, et al. Isoliquiritigenin inhibits cigarette smoke-induced COPD by attenuating inflammation and oxidative stress via the regulation of the Nrf2 and NF-κB signaling pathways. Front Pharmacol 2018; 9: 1001. doi: 10.3389/fphar.2018.01001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Li J, Tong D, Liu J, et al. Oroxylin A attenuates cigarette smoke-induced lung inflammation by activating Nrf2. Int Immunopharmacol 2016; 40: 524–529. doi: 10.1016/j.intimp.2016.10.011 [DOI] [PubMed] [Google Scholar]
- 170.Wang H, Yang T, Wang T, et al. Phloretin attenuates mucus hypersecretion and airway inflammation induced by cigarette smoke. Int Immunopharmacol 2018; 55: 112–119. doi: 10.1016/j.intimp.2017.12.009 [DOI] [PubMed] [Google Scholar]
- 171.Tian X, Xue Y, Xie G, et al. (-)-Epicatechin ameliorates cigarette smoke-induced lung inflammation via inhibiting ROS/NLRP3 inflammasome pathway in rats with COPD. Toxicol Appl Pharmacol 2021; 429: 115674. doi: 10.1016/j.taap.2021.115674 [DOI] [PubMed] [Google Scholar]
- 172.Li L, Bao H, Wu J, et al. Baicalin is anti-inflammatory in cigarette smoke-induced inflammatory models in vivo and in vitro: a possible role for HDAC2 activity. Int Immunopharmacol 2012; 13: 15–22. doi: 10.1016/j.intimp.2012.03.001 [DOI] [PubMed] [Google Scholar]
- 173.Li J, Qiu C, Xu P, et al. Casticin improves respiratory dysfunction and attenuates oxidative stress and inflammation via inhibition of NF-κB in a chronic obstructive pulmonary disease model of chronic cigarette smoke-exposed rats. Drug Des Devel Ther 2020; 14: 5019–5027. doi: 10.2147/DDDT.S277126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Lee H, Jung KH, Lee H, et al. Casticin, an active compound isolated from Vitex Fructus, ameliorates the cigarette smoke-induced acute lung inflammatory response in a murine model. Int Immunopharmacol 2015; 28: 1097–1101. doi: 10.1016/j.intimp.2015.07.041 [DOI] [PubMed] [Google Scholar]
- 175.Liu J, Yao J, Zhang J. Naringenin attenuates inflammation in chronic obstructive pulmonary disease in cigarette smoke induced mouse model and involves suppression of NF-κB. J Microbiol Biotechnol 2018; in press [ 10.4014/jmb.1810.10061]. [DOI] [PubMed] [Google Scholar]
- 176.Da Silva Araújo NP, De Matos NA, Leticia Antunes Mota S, et al. quercetin attenuates acute lung injury caused by cigarette smoke both in vitro and in vivo. COPD 2020; 17: 205–214. doi: 10.1080/15412555.2020.1749253 [DOI] [PubMed] [Google Scholar]
- 177.Park JW, Shin NR, Shin IS, et al. Silibinin inhibits neutrophilic inflammation and mucus secretion induced by cigarette smoke via suppression of ERK-SP1 pathway. Phytother Res 2016; 30: 1926–1936. doi: 10.1002/ptr.5686 [DOI] [PubMed] [Google Scholar]
- 178.Ko JW, Shin NR, Park SH, et al. Silibinin inhibits the fibrotic responses induced by cigarette smoke via suppression of TGF-β1/Smad 2/3 signaling. Food Chem Toxicol 2017; 106: 424–429. doi: 10.1016/j.fct.2017.06.016 [DOI] [PubMed] [Google Scholar]
- 179.Wang Y, Xue C, Dong F, et al. Hydroxysafflor yellow a attenuates small airway remodeling in a rat model of chronic obstructive pulmonary disease. Biol Pharm Bull 2014; 37: 1591–1598. doi: 10.1248/bpb.b14-00198 [DOI] [PubMed] [Google Scholar]
- 180.Jin M, Xue CJ, Wang Y, et al. Protective effect of hydroxysafflor yellow A on inflammatory injury in chronic obstructive pulmonary disease rats. Chin J Integr Med 2019; 25: 750–756. doi: 10.1007/s11655-018-2577-2 [DOI] [PubMed] [Google Scholar]
- 181.Flores G, Dastmalchi K, Paulino S, et al. Anthocyanins from Eugenia brasiliensis edible fruits as potential therapeutics for COPD treatment. Food Chem 2012; 134: 1256–1262. doi: 10.1016/j.foodchem.2012.01.086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Kim SH, Hong JH, Yang WK, et al. Herbal combinational medication of Glycyrrhiza glabra, Agastache rugosa containing glycyrrhizic acid, tilianin inhibits neutrophilic lung inflammation by affecting CXCL2, interleukin-17/STAT3 signal pathways in a murine model of COPD. Nutrients 2020; 12: 926. doi: 10.3390/nu12040926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Ren QC, Li XH, Li QY, et al. Total flavonoids from sea buckthorn ameliorates lipopolysaccharide/cigarette smoke-induced airway inflammation. Phytother Res 2019; 33: 2102–2117. doi: 10.1002/ptr.6404 [DOI] [PubMed] [Google Scholar]
- 184.Sousa Carvalho GF, Marques LK, Sousa HG, et al. Phytochemical study, molecular docking, genotoxicity and therapeutic efficacy of the aqueous extract of the stem bark of Ximenia americana L. in the treatment of experimental COPD in rats. J Ethnopharmacol 2020; 247: 112259. doi: 10.1016/j.jep.2019.112259 [DOI] [PubMed] [Google Scholar]
- 185.Zhao Z, Wang X, Zhang R, et al. Melatonin attenuates smoking-induced atherosclerosis by activating the Nrf2 pathway via NLRP3 inflammasomes in endothelial cells. Aging 2021; 13: 11363–11380. 10.18632/aging.202829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Pehote G, Bodas M, Brucia K, et al. Cigarette smoke exposure inhibits bacterial killing via TFEB-mediated autophagy impairment and resulting phagocytosis defect. Mediators Inflamm 2017; 2017: 3028082. doi: 10.1155/2017/3028082 [DOI] [PMC free article] [PubMed] [Google Scholar]