Abstract
Background
Variceal upper gastrointestinal bleeding (VUGIB) occurs in patients with decompensated cirrhosis, but non-VUGIB (NVUGIB) is not uncommon. We compared the outcomes of VUGIB and NVUGIB in cirrhotic patients.
Methods
This retrospective study used Nationwide Inpatient Sample employing International Classification of Diseases codes for adult NVUGIB and VUGIB patients. Mortality, morbidity, and resource utilization were compared. Analyses were performed using STATA; proportions and continuous variables were compared using Fisher’s exact and Student’s t-test, respectively. Confounding variables were adjusted using propensity matching, multivariate logistic and linear regression analyses.
Results
Of 2,166,194 cirrhotics, 92,439 had a diagnosis of NVUGIB and 17,620 VUGIB. VUGIB patients had higher rates of mortality [adjusted odds ratio (aOR) 1.42, 95% confidence interval (CI) 1.19-1.69], hemorrhagic shock (aOR 1.84, 95%CI 1.54-2.17) and intensive care unit admission (aOR 2.47, 95%CI 2.18-2.81), greater hospitalization costs ($16,251 vs. $12,295, P<0.001), more need for packed red blood cell transfusion (aOR 1.12, 95%CI 1.03-1.22) or endoscopic therapy (aOR 2.71, 95%CI 2.47-2.93), and a longer hospital stay compared to NVUGIB. However, NVUGIB had higher aOR of undergoing diagnostic endoscopy and radiography-guided vessel embolization. There were no differences in the rates of acute kidney injury between the 2 groups. Ascites and spontaneous bacterial peritonitis were independently associated with increased VUGIB mortality.
Conclusions
VUGIB in patients with cirrhosis is associated with greater hospital costs, mortality, and morbidity burden than NVUGIB. This study provides updated and current knowledge of patient characteristics and differences in outcomes between VUGIB and NVUGIB, required to successfully address the healthcare delivery gaps.
Keywords: Liver cirrhosis, treatment outcome, gastrointestinal hemorrhage, mortality, morbidity
Introduction
Upper gastrointestinal bleeding (UGIB), broadly classified into variceal UGIB (VUGIB) and non-VUGIB (NVUGIB), results in significant mortality as high as 10-15% [1,2]. VUGIB occurs in patients with decompensated cirrhosis, but NVUGIB is not uncommon, and 30-40% of cirrhotic patients can have NVUGIB [3,4]. Despite advances in the management of UGIB, it remains a strong predictor of overall mortality [5]. UGIB in cirrhotic patients yields higher mortality trends compared to patients who do not have cirrhosis [6,7]. Frailty due to accompanying comorbidities and disturbances in coagulation pathways due to reduced hepatic synthetic function and thrombophilia are mechanisms that lead to greater mortality from UGIB in cirrhotic patients [8-10].
Apart from mortality, UGIB overall is also responsible for greater health resource utilization, including healthcare costs and length of stay (LOS) in patients with cirrhosis [11]. Despite the aforementioned unfavorable outcomes, no study has compared the outcomes of VUGIB and NVUGIB in the cirrhosis population based on a large sample size. Therefore, the present study was undertaken to assess the difference in mortality due to VUGIB and NVUGIB in cirrhotic patients. In addition, we reported the impact of diverse patient characteristics and comorbidities on mortality.
Materials and methods
Study design and database description
This was a retrospective cohort study of adult patients with cirrhosis hospitalized for UGIB across the United States. Data were obtained from the Nationwide Inpatient Sample (NIS) database. The Agency for Healthcare Research and Quality created and maintained this database. It is the largest publicly available all-payer inpatient database and is designed as a stratified probability sample representative of all nonfederal acute care hospitals nationwide. A 20% probability sample of patients from all hospitals is collected. Each discharge is then weighted (weight=total number of discharges from all acute care hospitals in the United States divided by the number of discharges included in the 20% sample), making it nationally representative. Up to 40 discharge diagnoses and up to 25 procedures are recorded. The dataset from 2016-2018 consists of more than 7 million weighted discharges each year, which is a 20% stratified sample from over 4500 nonfederal acute care hospitals in more than 45 states of the United States. This is equivalent to about 35 million yearly discharges nationwide when weighted, and is representative of 95% of hospital discharges nationwide.
Study patients
Patients with a principal International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) diagnosis specific for cirrhosis due to any etiology were included in the study. Patients were excluded if they were younger than 18 years of age. The specific ICD-10-CM codes included are listed in Supplementary Table 1 (207.3KB, pdf) . Using ICD-10-CM codes, patients with VUGIB and NVUGIB were identified among all included cirrhotic patients and their data were extracted for analysis.
The Institutional Review Board of Loyola University Medical Center authorized this study and deemed the research project exempt from approval because it is a retrospective review of already collected de-identified data.
Statistical analysis
Analyses were performed using STATA, version MP 14.2 (StataCorp, College Station, Texas, United States). The weighting of patient-level observations was applied to procure estimates for the entire population. We used 2 distinct approaches to adjust for confounders in our analysis: propensity score matching and multivariate regression analysis. Propensity scores were employed to match patients with cirrhosis who had VUGIB to those who suffered from NVUGIB. A non-parsimonious multivariate logistic regression model was developed to estimate the propensity score for developing significant UGIB, using the following variables: age, race, sex, Charlson comorbidity index (CCI) score, income in patient’s zip code, insurance status, hospital size, hospital urban location, hospital teaching status, and hospital region. During model building for propensity scores, the family specified was binomial and link as logit [12]. The double robust method was then used to generate treatment weights, and the inverse probability of treatment weighting was used to match cases with controls using generalized linear models [12]. The match variables were age, sex, race, and relevant comorbidities identified from the literature search (ascites, hepatic encephalopathy, spontaneous bacterial peritonitis, heart failure, hypertension, hyperlipidemia, diabetes, malnutrition, and Clostridioides difficile [C. difficile] infection). In the second analysis, multivariate regression analysis models were used to adjust the results for potential confounders. Multivariate regression models were built by including all confounders significantly associated with the outcome on univariate analysis with a cutoff P-value of 0.2 [13]. Variables deemed clinically important to the outcome based on the literature were included in the model, irrespectively of whether they were significantly associated with the outcome on univariate analysis—international normalized ratio abnormalities, hyponatremia, hypoalbuminemia, presence of ascites, spontaneous bacterial peritonitis, and hepatic encephalopathy. A logistic regression model was used for binary outcomes, and a linear regression model was used for continuous outcomes. The variables adjusted for in the regression models were: sex, age, race, CCI score, insurance status, median household income for patients’ zip codes, hospital location, hospital region, hospital size, hospital teaching status, admission over the weekend, ascites, hepatic encephalopathy, spontaneous bacterial peritonitis, C. difficile infection, coronary artery disease, hypertension, hyperlipidemia, malnutrition, antiplatelet use (8.59% of the cohort), and anticoagulant use (5.60% of the cohort) (heart failure and diabetes are part of the CCI, the analysis for LOS was additionally adjusted for mortality). For the other calculations, proportions were compared using the Fisher exact test, and continuous variables were compared using Student’s t-test. All P-values were 2-sided, with 0.05 as the threshold for statistical significance.
Missing data
Hospital characteristics variables did not have missing data (Supplementary Table 2 (207.3KB, pdf) ). However, 4 variables pertaining to patient characteristics had missing data, most of them a very low percentage (<0.5%), except for race (2.73%) and median income in the patient’s zip code (2.57%). To test whether missing data could introduce bias into the study, we assumed that data were not missing at random and applied a multivariate imputation by chained equations (i.e., MICE) method estimated from sequential multivariate models with fully conditional specifications [14]. Overall, 10 imputed datasets were constructed using information from all covariates used in the regression models and other covariates in the database without missing information. Results with and without imputation were not meaningfully different. Thus, results without imputation are reported.
Results
Patient characteristics
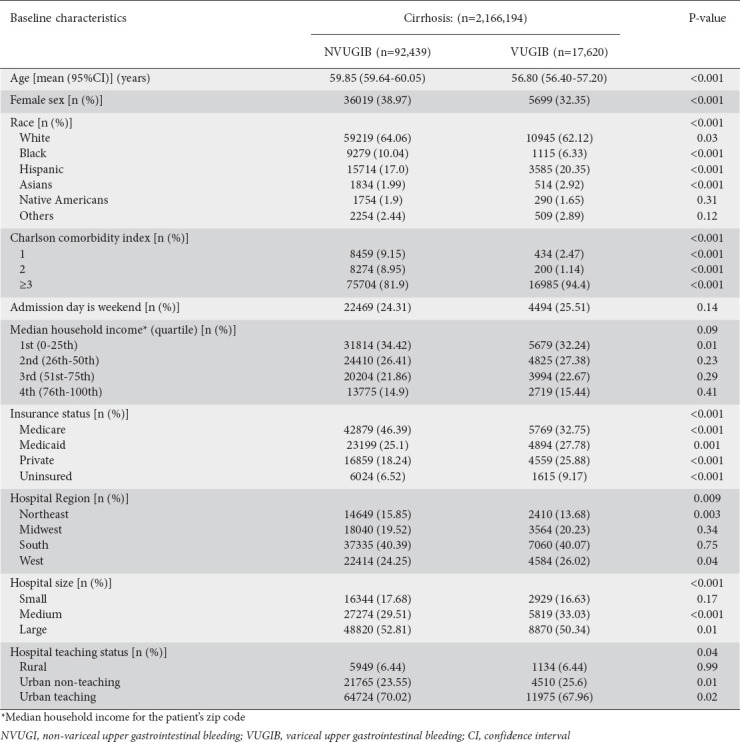
Fig. 1 shows the flow diagram for study inclusion. The total number of patients in the studied NIS cohort was 107,001,355, of whom 2,166,194 (2.02%) had a diagnosis of cirrhosis (Table 1). The causes of cirrhosis included alcohol (42.38%), toxins/poisoning (0.12%), nonalcoholic steatohepatitis (12.35%), passive congestion (0.30%), autoimmune hepatitis (2.14%), biliary cirrhosis (2.93%), chronic viral hepatitis (28.36%), and others (11.42%). Among patients with cirrhosis, 92,439 had NVUGIB, 17,620 were admitted with a primary diagnosis of VUGIB, and 3584 had hepatic encephalopathy. There were no differences between the match variables before and after propensity score matching. Patients with NVUGIB were more likely to be older and female, more likely to be insured by Medicare, less likely to have Medicaid or private insurance, and had no to very little difference in median annual income compared with VUGIB patients. NVUGIB was found more in the White and Black population, while Hispanic and Asian patients with cirrhosis had a higher comparative prevalence of VUGIB. Among VUGIB, 37.21% had diabetes mellitus, and 24.78% had chronic kidney disease. Patients with VUGIB also had higher CCI scores.
Figure 1.
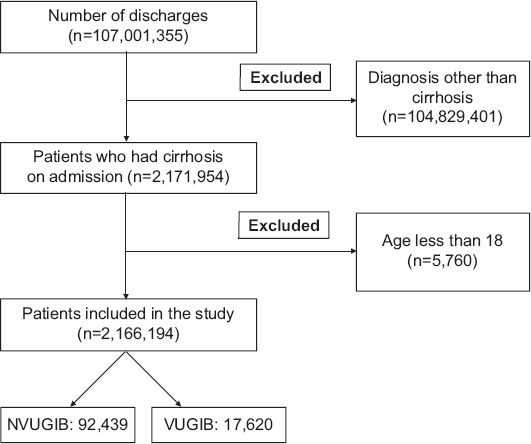
Study selection process
n, number; NVUGIB, non-variceal upper gastrointestinal bleeding; VUGIB, variceal upper gastrointestinal bleeding
Table 1.
Baseline characteristics of patients
Inpatient mortality
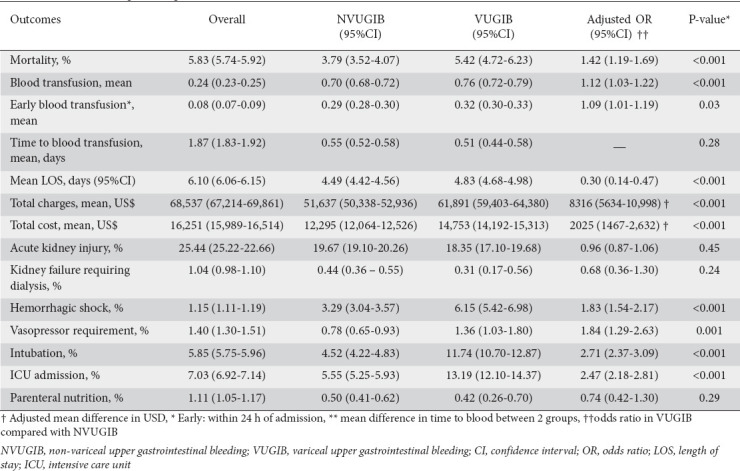
Overall, inpatient mortality due to any cause in cirrhotic patients was 5.83% (Table 2). Mortality was 3.79% for NVUGIB and 5.42% for patients with VUGIB (unadjusted). Even after adjusting for confounders, VUGIB patients had higher odds of inpatient mortality compared to NVUGIB (adjusted odds ratio [aOR] 1.42, 95% confidence interval [CI] 1.19-1.69; P<0.001).
Table 2.
Outcomes in hospitalized patients
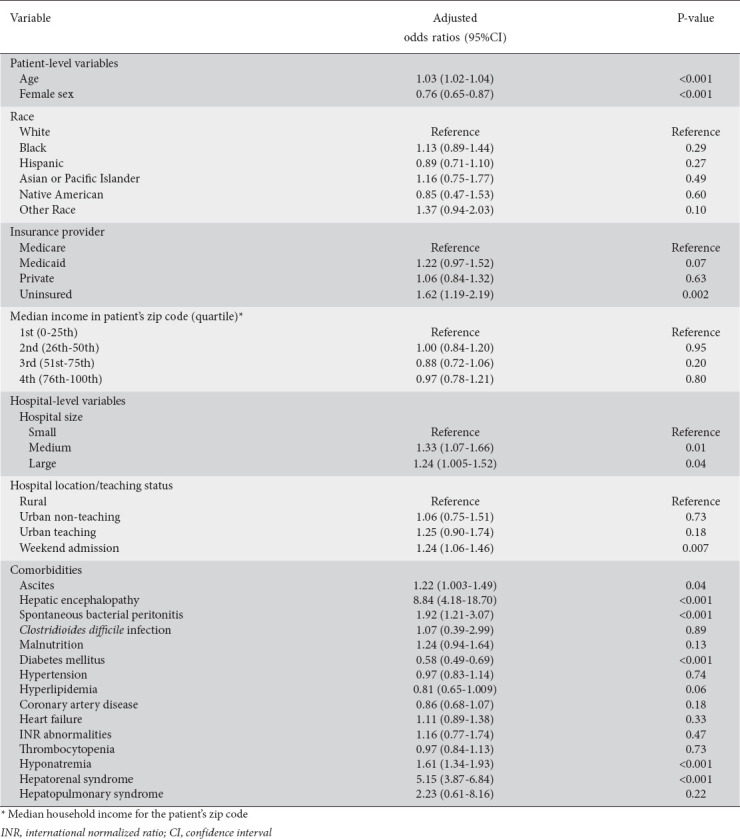
Independent predictors of mortality
Independent predictors of mortality were assessed for VUGIB. The final model (multivariate regression model) is presented in Table 3. The variables that independently increased mortality in VUGIB patients were ascites, hyponatremia, spontaneous bacterial peritonitis, hepatic encephalopathy, hepatorenal syndrome, age, and admission to medium or large-sized hospitals. The variables resulting in lower mortality odds from VUGIB in cirrhosis were diabetes mellitus and female sex.
Table 3.
Independent predictors of mortality
Morbidity
The overall rate of acute kidney injury (AKI) was 19.67% and 18.35% among NVUGIB and VUGIB, respectively, but this difference was not significant after adjusting for confounders (aOR 0.96, 95%CI 0.87-1.06; P=0.45). Similarly, AKI requiring dialysis did not differ between the 2 subgroups (aOR 0.68, 95%CI 0.36-1.30; P=0.24). However, hemorrhagic shock occurred more in VUGIB (6.15% vs. 3.29%), and the variceal group had higher odds even after adjusting for confounders (aOR 1.83, 95%CI 1.54-2.17; P<0.001).
Treatment setting and LOS
The overall mean LOS was 6.10 days for patients hospitalized with cirrhosis, 4.49 days for NVUGIB, and 4.83 days for VUGIB (unadjusted numbers). After adjustment for confounders, patients with VUGIB had a significantly higher mean LOS than NVUGIB (mean adjusted additional LOS: 0.30, 95%CI 0.14-0.44; P<0.001). In addition, 13.19% of VUGIB patients required intensive care unit (ICU) stay compared with 5.55% in NVUGIB (aOR 2.47, 95%CI 2.18-2.81; P<0.001). Similarly, VUGIB patients had higher odds of requiring intubation and vasopressor support (aOR 2.71, 95%CI 2.37-3.09; P<0.001, and aOR 1.84, 95%CI 1.29-2.63; P<0.001, respectively). The indications for intubation included acute respiratory failure (66.08%), hepatic encephalopathy (2.18%), and airway protection (31.74%).
Resource utilization
Total hospitalization charges, total hospitalization costs, and packed red blood cell (PRBC) transfusion were among the markers assessed for resource utilization. The total adjusted hospitalization charges were significantly higher for VUGIB than NVUGIB patients. Similar results were found when examining total hospitalization costs. VUGIB required more transfusion of PBRCs (overall and within the first 24 h) than NVUGIB (aOR 1.12, 95%CI 1.03-1.22; P<0.001 and aOR 1.09, 95%CI 1.01-1.19; P=0.03, respectively). The time to first blood transfusion was similar in both groups (0.55 days vs. 0.51 days, P=0.28).
Treatment modalities
Upper endoscopy
An in-hospital diagnostic endoscopic examination was performed more in NVUGIB than in VUGIB patients (58.54% vs. 26.24% of admissions), while VUGIB required more endoscopic therapy (35.32% vs. 17.20% of admissions). Similar results were reproduced on confounder-adjusted odds analysis (Table 4). In addition, early (within 24 h) upper endoscopy (whether diagnostic or with therapy) was performed more in VUGIB (50.96% vs. 49.04%, P<0.001). The discharge endoscopic diagnoses for NVUGIB were esophagitis (10.8%), esophageal ulcer (3.6%), gastritis (12.8%), gastric ulcer (21.2%), duodenitis (2.5%), duodenal ulcer (14.8%), angiodysplasia (12.7%), Dieulafoy’s lesion (4.2%), and others (17.4%).
Table 4.
In-hospital procedures
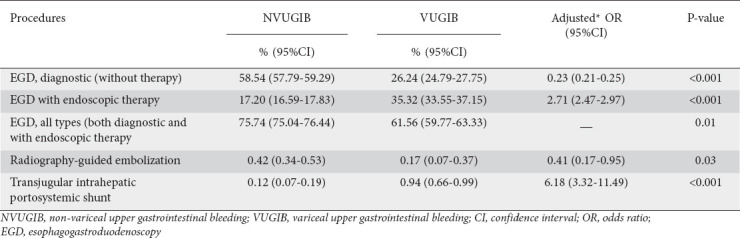
Radiology interventions
Transjugular intrahepatic portosystemic shunt (TIPS) was performed more in VUGIB (aOR 6.18, 95%CI 3.32-11.49; P<0.001). The indication for TIPS was refractory ascites in NVUGIB patients. However, radiography-guided embolization was required more in NVUGIB (0.42% vs. 0.17%). After adjusting for confounders, the NVUGIB group was 59% more likely to have undergone radiologic-guided embolization than the VUGIB group (aOR 0.41, 95%CI 0.17-0.95; P=0.03).
Discussion
We showed that in-hospital mortality in patients with cirrhosis and NVUGIB is 3.79%. This finding is in line with a prior study showing that cirrhotic patients are at higher risk of NVUGIB than the general population [15]. However, it differs from the in-hospital mortality of 2.1% reported by Abougergi et al [16]. A previous study by Tandon et al compared mortality from VUGIB with NVUGIB and yielded results contradictory to ours, as they found no difference in mortality [17]. That study was performed outside of the United States and had a very small sample size. Our study had a large sample size, which reduces the likelihood of beta error in estimates obtained, and the population studied is nationally representative of the inpatient population in the United States. Another plausible explanation is that the mortality trend is specific to the healthcare system in the United States, but studies in different regions across the globe are not available.
Historically, predictors independently associated with the mortality from VUGIB described in the literature include age, higher Child-Pugh class and model for end-stage liver disease (MELD) score, low hemoglobin, systolic blood pressure, rebleeding, higher serum bilirubin, impaired renal function, and active bleeding seen on endoscopy [18-21]. Our study found that certain systematic and biologic factors, such as age, self-pay status, admission to larger hospitals, admission over the weekend, ascites, hepatic encephalopathy, spontaneous bacterial peritonitis, hyponatremia and hepatorenal syndrome also predict mortality from VUGIB independently. Age, ascites, hepatic encephalopathy, and hyponatremia represent scoring components for calculating Child-Pugh class and MELD scores [22,23]. Larger hospitals usually act as referral and tertiary care centers for patients with higher comorbidity and higher frailty. Previous studies have resulted in contradictory findings regarding the impact of the day of admission on mortality in VUGIB and NVUGIB. For NVUGIB specifically, most studies found no effect based on the day of admission [24-26]. Ananthakrishnan et al and Abougergi et al reported that weekend admission was not associated with greater odds of mortality for VUGIB. Both studies used a smaller subset of the same dataset that we used and employed the same definition of weekend admission as we did. Ananthakrishnan et al captured 7240 weekend admissions with VUGIB, while there were 3251 patients with VUGIB in the Abougergi et al study. In our study, we were able to use a larger sample size (n=17,620 VUGIB) and demonstrated that weekend admission is independently associated with mortality for VUGIB when compared to NVUGIB. Female sex was associated with lower odds of mortality in VUGIB: a finding in line with prior studies where female sex was associated with better survival outcomes in VUGIB and overall cirrhosis [27,28]. Studies pointing towards more immune suppression following hemorrhage and trauma in males can offer a potential explanation for sex-related differences in mortality trends observed in VUGIB [29].
There was a greater likelihood of hemorrhagic shock, vasopressor requirement, intubation and ICU stay in patients with VUGIB. Hemorrhagic shock is an established phenomenon in patients with VUGIB, usually treated with PBRC transfusion and administration of crystalloids. Prophylactic endotracheal intubation is commonly practiced for airway protection in critically ill patients with UGIB prior to upper endoscopy, despite the limited evidence suggesting a clear outcome benefit [30]. Studies directly comparing endotracheal intubation rates and effects on outcomes are lacking, but we showed that the rate of endotracheal intubation was higher in VUGIB than in NVUGIB (11.74% vs. 4.52%). Hepatic encephalopathy commonly complicates VUGIB and governs the increased rate of endotracheal intubation in the peri-endoscopy period.
We also demonstrated that a greater proportion of patients required endoscopic therapy in the VUGIB group, while endoscopy without therapy (i.e., diagnostic endoscopy) was performed more in NVUGIB patients. Varices are formed because of blockage in the blood flow in the liver with resultant high backpressure, causing the formation of varices with an increased tendency to rupture and bleed [30]. The endoscopic treatment of choice for VUGIB is band ligation. Minor cases of NVUGIB may not need endoscopic therapy and improve with supportive measures. Recurrent bleeding despite endoscopic therapy or failure to achieve hemostasis requires rescue radiologic or surgical intervention to control bleeding. Radiography-guided embolization of the bleeding vessel was performed more in NVUGIB, while TIPS was the most commonly used radiologic procedure in the VUGIB population.
Using a nationally representative sample, we also demonstrated that PRBC transfusion was more common in VUGIB than NVUGIB. There is very limited literature directly comparing blood transfusion requirements between the 2 groups. We also showed that the PRBC transfusion requirement within the first 24 h was also greater in VUGIB. Variceal bleeding correlates with a high hepatic venous pressure gradient (>20 mmHg) [31]; thus, a restricted threshold should be adopted for transfusion while balancing the need to avoid complications from hemorrhagic shock. However, no difference was found in the time from patient presentation to when the first PRBC transfusion was given. This suggests that emergency room providers efficiently prioritize the blood transfusion needs of patients with UGIB, depending on their hemodynamic status, and intervene promptly.
The available literature hints at mixed trends for the difference in LOS between the 2 groups of UGIB. Tandon et al directly compared the LOS between the 2 groups and found no significant difference between them (median LOS, VUGIB: 4.9, NVUGIB: 5.0, P=0.34); however, the results were probably skewed due to the smaller sample size. In our study, the mean LOS for VUGIB ranged from 4.68-4.98, while the NVUGIB range was 4.42-4.56. Prior high-quality evidence suggests that early endoscopy reduces the LOS in UGIB [32]. We found in our dataset that early endoscopy (within 24 h) was performed more in VUGIB (50.96% vs. 49.04, P<0.001), whereas mean LOS was significantly greater by 0.30 days in VUGIB, even though the difference may not be clinically relevant. Total hospital costs and charges were greater in VUGIB as a result of greater resource utilization, be it LOS or requiring comparatively more endoscopic therapy.
This trend is also supported by a prior study comparing the costs between the 2 groups [11]. In the contemporary healthcare delivery system, there is a great deal of focus on cost-effectiveness and viability of systems, as the center of Medicare and Medicaid Services has established a target to cover half of Medicare payments in unconventional and substitute payment models involving value-based purchasing. Prevention of bleeding represents an ideal way of achieving better cost-effectiveness. We showed that VUGIB results in higher resource utilization compared to NVUGIB. Each episode of VUGIB prevented will decrease in-hospital mortality by 42%, LOS by 0.30 days, total hospitalization costs by $1467-2632, and the total hospitalization charges by $5634-10,998 compared to NVUGIB in patients with cirrhosis. These numbers are based on observational findings from a retrospective cohort study, and prospective studies in the future will help directly test and confirm these findings in real-life practice.
There are various limitations to our study. First, the exposure is not completely randomized, given the retrospective nature of our study. We employed propensity matching and multivariate regression models to control for confounders. Even though the results obtained from both methods were similar, which reduces the likelihood of confounding, residual confounding can still exist. Moreover, we controlled for diverse patient and hospital-level characteristics, which further minimizes the risk. Second, an administrative database was used to acquire the data. Claims-based databases such as NIS are inherently vulnerable to missing codes or erroneously entered data [33]. Moreover, UGIB itself is prone to coding inaccuracies, as shown by Joos et al [34]. Nonetheless, the frequency of missing data among the variables we used was less than 2.5%, with a few exceptions, and the multiple imputations method was used to explicate the missing data. Third, the unavailability of laboratory values in the database made it impossible to use UGIB-specific severity scales and MELD score; instead, the CCI, a generalized validated prognostic scale, was used, as in previous studies [26]. Similarly, the overlapping diagnosis of AKI and hepatorenal syndrome in cirrhosis poses challenges in assessment. Even though reflective of clinical practice in the United States, care should be taken during analyzing AKI results in the study, as low baseline creatinine in cirrhotic patients can lead to misdiagnosis of AKI. Finally, we reported the overall inpatient mortality of patients hospitalized with a principal diagnosis of either VUGIB or NVUGIB, as the cause of death could not be determined from the database. We believe further well-designed cohort studies are required to overcome the limitations in this study.
Regardless of these limitations, our study has numerous strengths. To our knowledge, this is the first study that compares the mortality of VUGIB, its predictors and other outcomes, with those of NVUGIB at the national level. Moreover, the NIS database eliminates the commonly encountered limitation of single-center studies by allowing the use of a large sample size, as it is the largest publicly available all-payer database consisting of the inpatient population. Propensity matching is a powerful tool for the analysis of administrative databases and helps control confounding by indication [35]. It relies on a wide range of empirically-derived covariates that serve as surrogates for unmeasured confounding variables while matching cases with controls [36]. Utilizing nationally representative data, our study eliminated biases related to practice patterns in single- or multi-center studies. Similarly, the distinctive variables in the database granted us the opportunity to explore variables such as household income estimates, hospitalization cost and hospital factors, which are not generally possible in single-center studies.
In conclusion, cirrhotic patients with VUGIB have 5 times the inpatient mortality compared with NVUGIB patients. In addition to the already known prognostic indicators, we report that self-pay status, admission to larger hospitals, ascites, spontaneous bacterial peritonitis, and hyponatremia are independent predictors of mortality and should alert treating physicians to a poorer prognosis. VUGIB patients also had a higher likelihood of morbidity measured by hemorrhagic shock, vasopressor requirement, intubation and ICU stay, as well as higher resource utilization as indicated by PRBC transfusion, hospital LOS, adjusted total hospitalization charges and costs, and higher rates of upper endoscopy therapy involving both acuity and complexity of intervention during the procedure. Further research is warranted to test interventions to reduce the morbidity and mortality gap between these 2 subgroups.
Summary Box.
What is already known:
Variceal upper gastrointestinal bleeding (VUGIB) occurs in patients with decompensated cirrhosis, but non-VUGIB (NVUGIB) is not uncommon, and 30-40% of cirrhotic patients can have NVUGIB
Previous studies compared outcomes of VUGIB and NVUGIB in cirrhosis and found similar mortalityrates between the 2 groups using a small sample size
A difference in mortality and other hospitalization outcomes between these 2 groups of upper gastrointestinal bleeding is yet to be determined
What the new findings are:
VUGIB patients with cirrhosis had greater mortality than NVUGIB patients after adjustment for confounders in a large sample
VUGIB also resulted in greater hospital costs and higher rates of hemorrhagic shock, intensive care unit admission, and endoscopic therapy
Ascites and spontaneous bacterial peritonitis were independently associated with increased mortality in VUGIB patients
Acknowledgment
Authors thank Lili Wang (Biostatistician) for helping with statistical analysis.
Biography
Loyola Medicine/MacNeal Hospital, Berwyn, IL; University of Missouri, Columbia, MO; University of California San Francisco, CA, USA; Loyola University Medical Center, Maywood, IL
Footnotes
Conflict of Interest: None
References
- 1.Hearnshaw SA, Logan RF, Lowe D, Travis SP, Murphy MF, Palmer KR. Acute upper gastrointestinal bleeding in the UK:patient characteristics, diagnoses and outcomes in the 2007 UK audit. Gut. 2011;60:1327–1335. doi: 10.1136/gut.2010.228437. [DOI] [PubMed] [Google Scholar]
- 2.Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W. Practice Guidelines Committee of the American Association for the Study of Liver Diseases;Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007;46:922–938. doi: 10.1002/hep.21907. [DOI] [PubMed] [Google Scholar]
- 3.Kalafateli M, Triantos CK, Nikolopoulou V, Burroughs A. Non-variceal gastrointestinal bleeding in patients with liver cirrhosis:a review. Dig Dis Sci. 2012;57:2743–2754. doi: 10.1007/s10620-012-2229-x. [DOI] [PubMed] [Google Scholar]
- 4.European Association for the Study of the Liver. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis J Hepatol. 2018;69:406–460. doi: 10.1016/j.jhep.2018.03.024. [DOI] [PubMed] [Google Scholar]
- 5.Vergara M, Clèries M, Vela E, Bustins M, Miquel M, Campo R. Hospital mortality over time in patients with specific complications of cirrhosis. Liver Int. 2013;33:828–833. doi: 10.1111/liv.12137. [DOI] [PubMed] [Google Scholar]
- 6.Lecleire S, Di Fiore F, Merle V, et al. Acute upper gastrointestinal bleeding in patients with liver cirrhosis and in noncirrhotic patients:epidemiology and predictive factors of mortality in a prospective multicenter population-based study. J Clin Gastroenterol. 2005;39:321–327. doi: 10.1097/01.mcg.0000155133.50562.c9. [DOI] [PubMed] [Google Scholar]
- 7.Farooq U, Tarar ZI, Malik A, Amin MK, Sifuentes H. How does cirrhosis impact mortality, morbidity, and resource utilization in non-variceal upper gastrointestinal bleeding?A nationwide analysis. Prz Gastroenterol. 2022 doi: 10.5114/pg.2022.115232. [Online ahead of print] doi:10.5114/pg.2022.115232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Matei D, Groza I, Furnea B, et al. Predictors of variceal or nonvariceal source of upper gastrointestinal bleeding An etiology predictive score established and validated in a tertiary referral center. Gastrointestin Liver Dis. 2013;22:379–384. [PubMed] [Google Scholar]
- 9.Gondal AB, Farooq U, Khanal P, Bakhat K. Su1672 The emerging role of frailty as a prognostic model in end stage liver disease:a systematic review. Gastroenterology. 2020;158(1):S609. [Google Scholar]
- 10.Flores B, Trivedi HD, Robson SC, Bonder A. Hemostasis, bleeding and thrombosis in liver disease. J Transl Sci. 2017;3:10. doi: 10.15761/JTS.1000182. 15761/JTS.1000182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adam V, Barkun AN, Viviane A, Alan BN. Estimates of costs of hospital stay for variceal and nonvariceal upper gastrointestinal bleeding in the United States. Value Health. 2008;11:1–3. doi: 10.1111/j.1524-4733.2007.00208.x. [DOI] [PubMed] [Google Scholar]
- 12.Dugoff EH, Schuler M, Stuart EA. Generalizing observational study results:applying propensity score methods to complex surveys. Health Serv Res. 2014;49:284–303. doi: 10.1111/1475-6773.12090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eric Vittinghoff DVG SCS Charles E McCulloch. Regression Methods in Biostatistics. Boston, MA: Springer; 2012. [Google Scholar]
- 14.White IR, Royston P, Wood AM. Multiple imputation using chained equations:Issues and guidance for practice. Stat Med. 2011;30:377–399. doi: 10.1002/sim.4067. [DOI] [PubMed] [Google Scholar]
- 15.Kruger AJ, Abougergi MS, Jalil S, et al. Outcomes of nonvariceal upper gastrointestinal bleeding in patients with cirrhosis:a national analysis. J Clin Gastroenterol. 2022 Aug 15; doi: 10.1097/MCG.0000000000001746. [Online ahead of print] doi:10.1097/MCG.0000000000001746. [DOI] [PubMed] [Google Scholar]
- 16.Luo JC, Leu HB, Hou MC, et al. Cirrhotic patients at increased risk of peptic ulcer bleeding:a nationwide population-based cohort study. Aliment Pharmacol Ther. 2012;36:542–550. doi: 10.1111/j.1365-2036.2012.05225.x. [DOI] [PubMed] [Google Scholar]
- 17.Tandon P, Bishay K, Fisher S, et al. Comparison of clinical outcomes between variceal and non-variceal gastrointestinal bleeding in patients with cirrhosis. J Gastroenterol Hepatol. 2018;33:1773–1779. doi: 10.1111/jgh.14147. [DOI] [PubMed] [Google Scholar]
- 18.Kumar AS, Sibia RS. Predictors of in-hospital mortality among patients presenting with variceal gastrointestinal bleeding. Saudi J Gastroenterol. 2015;21:43–46. doi: 10.4103/1319-3767.151226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Teng W, Chen WT, Ho YP, et al. Predictors of mortality within 6 weeks after treatment of gastric variceal bleeding in cirrhotic patients. Medicine (Baltimore) 2014;93:e321. doi: 10.1097/MD.0000000000000321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ahmed G, Basel E, Aida A, Anthony A. Predictors of mortality in patients with acute upper gastrointestinal hemorrhage who underwent endoscopy and confirmed to have variceal hemorrhage. Alexandria Journal of Medicine. 2015;51:295–304. [Google Scholar]
- 21.Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J. Portal hypertensive bleeding in cirrhosis:Risk stratification, diagnosis, and management:2016 practice guidance by the American Association for the study of liver diseases. Hepatology. 2017;65:310–335. doi: 10.1002/hep.28906. [DOI] [PubMed] [Google Scholar]
- 22.Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60:646–649. doi: 10.1002/bjs.1800600817. [DOI] [PubMed] [Google Scholar]
- 23.Wiesner R, Edwards E, Freeman R, et al. United Network for Organ Sharing Liver Disease Severity Score Committee. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology. 2003;124:91–96. doi: 10.1053/gast.2003.50016. [DOI] [PubMed] [Google Scholar]
- 24.Nahon S, Pariente A, Latrive JP. Group of Investigators of the Association Nationale des Gastroentérologues des Hôpitaux Généraux (ANGH). Weekend admission does not influence the mortality of upper gastrointestinal bleeding caused by peptic ulcers:results of a French prospective study of the association nationale des gastroentérologues des hôpitaux généraux group. Clin Gastroenterol Hepatol. 2009;7:911. doi: 10.1016/j.cgh.2009.03.018. author reply 912. [DOI] [PubMed] [Google Scholar]
- 25.Tsoi KK, Chiu PW, Chan FK, Ching JY, Lau JY, Sung JJ. The risk of peptic ulcer bleeding mortality in relation to hospital admission on holidays:a cohort study on 8,222 cases of peptic ulcer bleeding. Am J Gastroenterol. 2012;107:405–410. doi: 10.1038/ajg.2011.409. [DOI] [PubMed] [Google Scholar]
- 26.Abougergi MS, Travis AC, Saltzman JR. Impact of day of admission on mortality and other outcomes in upper GI hemorrhage:a nationwide analysis. Gastrointest Endosc. 2014;80:228–235. doi: 10.1016/j.gie.2014.01.043. [DOI] [PubMed] [Google Scholar]
- 27.Haukeland JW, Småstuen MC, Pålsdatter PP, et al. Effect of gender on mortality and causes of death in cirrhotic patients with gastroesophageal varices A retrospective study in Norway. PLoS One. 2020;15:e0230263. doi: 10.1371/journal.pone.0230263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nilsson E, Anderson H, Sargenti K, Lindgren S, Prytz H. Incidence, clinical presentation and mortality of liver cirrhosis in Southern Sweden:a 10-year population-based study. Aliment Pharmacol Ther. 2016;43:1330–1339. doi: 10.1111/apt.13635. [DOI] [PubMed] [Google Scholar]
- 29.Angele MK, Schwacha MG, Ayala A, Chaudry IH. Effect of gender and sex hormones on immune responses following shock. Shock. 2000;14:81–90. doi: 10.1097/00024382-200014020-00001. [DOI] [PubMed] [Google Scholar]
- 30.Ben-Menachem T, Decker GA, Early DS, et al. ASGE Standards of Practice Committee. Adverse events of upper GI endoscopy. Gastrointest Endosc. 2012;76:707–718. doi: 10.1016/j.gie.2012.03.252. [DOI] [PubMed] [Google Scholar]
- 31.de Franchis R, Bosch J, Garcia-Tsao G, Reiberger T, Ripoll C. Baveno VII Faculty. Baveno VII - Renewing consensus in portal hypertension. J Hepatol. 2022;76:959–974. doi: 10.1016/j.jhep.2021.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Singh A, Siddiqui MT, Al-Yaman W, et al. Utility of endoscopy in hospitalized patients with gastrointestinal hemorrhage and pulmonary hypertension. Dig Dis Sci. 2021;66:4159–4168. doi: 10.1007/s10620-020-06803-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Klabunde CN, Warren JL, Legler JM. Assessing comorbidity using claims data:an overview. Med Care. 2002;40(IV):26–35. doi: 10.1097/00005650-200208001-00004. [DOI] [PubMed] [Google Scholar]
- 34.Joos C, Lawrence K, Jones AE, Johnson SA, Witt DM. Accuracy of ICD-10 codes for identifying hospitalizations for acute anticoagulation therapy-related bleeding events. Thromb Res. 2019;181:71–76. doi: 10.1016/j.thromres.2019.07.021. [DOI] [PubMed] [Google Scholar]
- 35.Seeger JD, Williams PL, Walker AM. An application of propensity score matching using claims data. Pharmacoepidemiol Drug Saf. 2005;14:465–476. doi: 10.1002/pds.1062. [DOI] [PubMed] [Google Scholar]
- 36.Austin PC, Wu CF, Lee DS, Tu JV. Comparing the high-dimensional propensity score for use with administrative data with propensity scores derived from high-quality clinical data. Stat Methods Med Res. 2020;29:568–588. doi: 10.1177/0962280219842362. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


