Abstract
In this study, the expression of the Bordetella pertussis S1 subunit was tested in Streptococcus gordonii, a commensal oral bacterium which has the potential to be a live oral vaccine vehicle. The DNA fragment encoding the N-terminal 179 amino acids of the S1 subunit was ligated into the middle part of spaP, the surface protein antigen P1 gene originating from Streptococcus mutans. The resulting construct, carried on the Escherichia coli-Streptococcus shuttle vector pDL276, was introduced into S. gordonii DL-1 by natural transformation. One of the transformants (RJMIII) produced a 187-kDa protein (the predicted size of the SpaP-S1 fusion protein) which was recognized by both the anti-pertussis toxin (anti-PT) and anti-SpaP antibodies, suggesting that an in-frame fusion had been made. Results from immunogold-electron microscopic studies and cellular fractionation studies showed that the fusion protein was surface localized and was mainly associated with the cell wall of RJMIII, indicating that SpaP was able to direct the fusion protein to the cell surface. A rabbit antiserum raised against heat-killed S. gordonii RJMIII recognized the native S1 subunit of PT in Western blotting and showed a weak neutralization titer to PT by the Chinese hamster ovary cell-clustering assay. BALB/c mice immunized with the heat-killed S. gordonii RJMIII were protected from the toxic effect of PT in the leukocytosis-promoting and histamine sensitization assays. In conclusion, a fragment of the S1 subunit of PT was successfully surface expressed in S. gordonii; the recombinant S1 fragment was found to be immunogenic and could induce protection against the toxic effect of PT in mice.
Pertussis toxin (PT) is a major virulence factor of Bordetella pertussis (25) and is one of the prominent components of acellular pertussis vaccines. PT is an AB toxin, with the A promoter (S1 subunit) being the toxic subunit and the B oligomer being the pentamer that binds to the surface receptors on eucaryotic cells and translocates the toxic subunit across the cell membrane (23). The mature S1 subunit contains 234 amino acids (14) and is immunodominant (5). Antibodies against the S1 subunit have been shown to neutralize the toxin in vitro and protect mice from B. pertussis infection in aerosol and intracerebral challenges (7, 21, 22). The B oligomer is composed of one subunit each of S2, S3, and S5 and two subunits of S4. S2 and S3 mediate adherence of the toxin to host cells. Antibodies to B oligomer or S2 and S3 subunits confer protection against B. pertussis infection in animal models but do so less effectively than antibodies to S1 (7).
The cloning and expression of the S1 subunit in bacteria have been confined mainly to gram-negative bacteria such as Escherichia coli (2, 3, 24) and vaccine strains of Salmonella typhimurium (4, 24). These reports demonstrated that the recombinant S1 is immunogenic, but protective antibodies either were not present in the anti-recombinant S1 antisera or were present at low levels. The expression of S1 in gram-positive bacteria, however, has been limited to Bacillus subtilis (18, 20) and Streptomyces lividans (17). In both of these cases, the S1 subunit was expressed as a soluble extracellular protein. In B. subtilis, the recombinant S1 was found to be immunogenic in animals, but whether the recombinant S1 could induce protective antibodies has not been demonstrated (18). In S. lividans, the recombinant S1 was extensively degraded by proteases.
The oral commensal bacterium Streptococcus gordonii has recently been suggested to be a potential candidate as a live oral vaccine expression vehicle (15, 16). As a first step towards investigating the possibility of generating a live oral vaccine against pertussis, we report in this study the expression of the N-terminal 179-amino-acid fragment of S1 in S. gordonii by using the major surface protein antigen P1 gene (spaP) originating from Streptococcus mutans. The immunogenicity and protective effects of the anti-recombinant S1 antibodies against native PT were investigated.
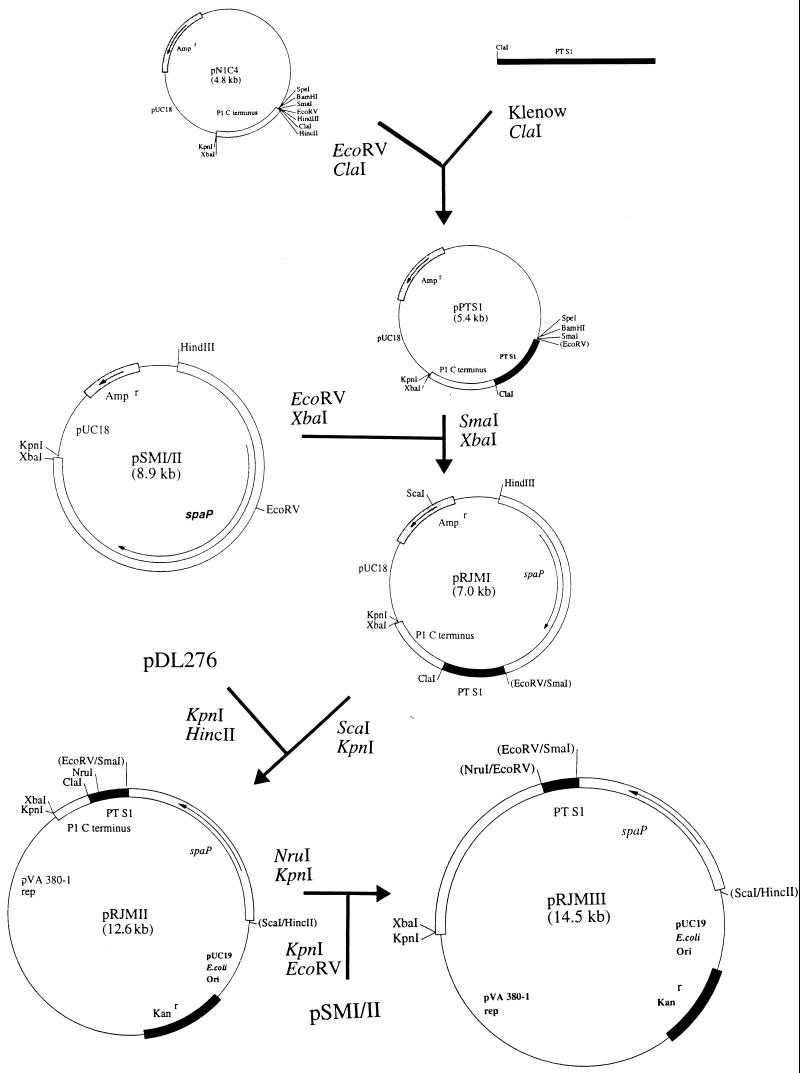
Construction of SpaP-S1 fusion protein.
The strategy used to construct the in-frame fusion between S. mutans SpaP (antigen P1) and the B. pertussis PT S1 subunit is depicted in Fig. 1. The initial gene fusion was constructed on a pUC 18-based plasmid to create pRJMI. To facilitate the expression in streptococci and to avoid the use of the Ampr marker, the fusion gene was cloned into pDL276, an E. coli-streptococcus shuttle vector (6), creating pRJMII. pRJMII was introduced into S. gordonii DL-1 by natural transformation (8). Transformants were selected on Todd-Hewitt agar containing 250 μg of kanamycin/ml. Several transformants were obtained. When these transformants were treated with mutanolysin (8), followed by boiling with the sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) sample buffer of Laemmli (11), all the transformants were found to produce a 98-kDa protein band recognized by the rabbit anti-PT antibodies (see below) in Western immunoblotting. This immunoreactive protein matched the predicted size of SpaP-S1 carried on pRJMII. However, when the transformants were analyzed by whole (intact)-cell enzyme-linked immunosorbent assay (ELISA) (8) and immunoelectron microscopy, none of them showed an appreciable amount of the fusion protein on the cell surface. Since S. gordonii DL-1 produces a number of high-molecular-weight (ca. 190- to 259-kDa) surface proteins (9), the SpaP-S1 fusion protein expressed from pRJMII may be buried among these proteins. Hence, pRJMIII was further constructed by placing the S1 fragment close to the middle part of SpaP. In the construction, we made use of the unique NruI site within the S1 sequence. Hence, the final fusion protein contained only the first 179 amino acids of S1 inserted into the complete SpaP, creating a predicted mature protein of ca. 187 kDa. Initial immunoblotting of lysates of E. coli HB101 carrying pRJMIII indicated the reactivity of a ca. 187-kDa protein band with the anti-PT antibodies, suggesting that correct fusion had been made (data not shown). pRJMIII was transformed into S. gordonii DL-1, and one of the transformants, S. gordonii RJMIII, was chosen for further studies.
FIG. 1.
Schematic diagram showing the construction of the spaP-s1 fusion gene. The S1 gene (coding for amino acid residues 2 to 233 of the mature S1) was amplified by PCR from the PT operon carried on pPTX42 (E. coli ATCC 67046 [14]) by standard methods (19) using the primers 5′-GATCCTCCCGCCACCGT-3′ and 5′-GGATCGATAACGAATACGCGATGCT-3′. (The underlined bases are added sequence for a ClaI site.) The amplicon was treated with Klenow fragment, restricted with ClaI, purified from agarose gels with a Gene-Clean kit (Bio 101, La Jolla, Calif.), and ligated into the EcoRV-ClaI sites of pN1C4, a pUC18 derivative carrying the 3′ DNA of spaP from S. mutans, coding for the C-terminal 144 amino acids containing the surface protein anchoring domain of SpaP (8). The ligated DNA was transformed into competent E. coli HB101, and the resulting plasmid was designated pPTS1. To provide the fusion gene with the spaP promoter, the 1.5-kb SmaI-XbaI fragment from pPTS1 was cloned into the EcoRV-XbaI sites of pSMI/II, a pUC18 derivative carrying the complete spaP gene (10). The resulting plasmid isolated from one of the E. coli HB101 transformants was named pRJMI. The 5.6-kb KpnI-ScaI fragment from pRJMI was further cloned into pDL276, creating pRJMII. pRJMIII was further constructed by ligating the 10.0-kb NruI-KpnI fragment from pRJMII to the 4.5-kb EcoRV-KpnI fragment from pSMI/II.
The anti-PT antibodies used were generated by immunizing two New Zealand White rabbits with 0.5 ml of a whole-cell B. pertussis vaccine (Connaught Laboratories Ltd., North York, Ontario, Canada) by subcutaneous injections, followed by booster injections with the same vaccine on days 20, 27, and 48 and a final booster with 110 μg of purified PT in Freund’s incomplete adjuvant (kindly provided by S. Loosmore, Connaught Laboratories Ltd.) on day 65. The titers of the antisera against purified PT (20 ng/well; List Biological Laboratories, Inc., Campbell, Calif.) were determined by an ELISA using methods described previously (13). The titers of anti-PT antibodies were expressed as the reciprocals of the dilutions which produced A405 readings 0.05 higher than the preimmune sera. The titers were 12,800 and 6,400 for the sera from the two rabbits. To eliminate cross-reactivity, pooled sera were adsorbed with S. gordonii DL-1 cells before use. To achieve this, 1 liter of S. gordonii DL-1 grown in TYG (1% tryptone, 0.5% yeast extract, 0.3% K2HPO4, 0.2% glucose [wt/vol]) to the late-exponential phase of growth was centrifuged (at 10,000 × g for 15 min at 4°C). The cells were washed once with phosphate-buffered saline (PBS) and resuspended in 15 ml of PBS. Half of the cell suspension was incubated with 5 ml of the anti-PT rabbit sera at 4°C for 1 h with occasional mixing. The suspension was centrifuged, and the remaining half of the cells was added to the supernatant and incubated for an additional hour. The suspension was again clarified by centrifugation, and the supernatant was used as adsorbed anti-PT antibodies.
Expression and localization of SpaP-S1 fusion protein in S. gordonii.
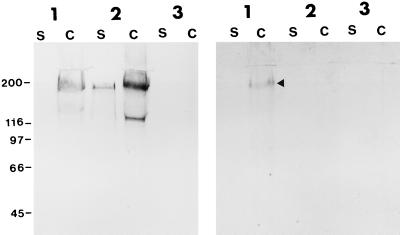
When culture supernatant fluid and cell extracts of S. gordonii RJMIII were analyzed by immunoblotting, a strong, 187-kDa protein band and a weaker, 155-kDa band from the cell extracts were recognized by an anti-SpaP monoclonal antibody (Fig. 2, left panel, lane 1). The same 187-kDa band from the cell extract was also recognized by the adsorbed anti-PT antibodies (Fig. 2, right panel). Samples obtained from S. gordonii DL-1 did not react with either of the antibodies. Samples prepared from S. gordonii DL-1/SMI/II-3 (8), a DL-1 transformant carrying the spaP gene, showed reaction with the anti-SpaP antibody, but not with the anti-PT antibodies. These results strongly indicate that S. gordonii RJMIII is expressing the correct SpaP-S1 fusion protein and that the fusion protein is mainly cell associated.
FIG. 2.
Western blots of S. gordonii expressing the SpaP-S1 fusion protein. (Left) Proteins reacted with the anti-SpaP monoclonal antibody 4-10A (dilution, 1/7000 [1]). (Right) Proteins reacted with the S. gordonii-adsorbed rabbit anti-PT antibodies (dilution, 1/100). Lane 1, recombinant SpaP-S1 S. gordonii RJMIII; lane 2, recombinant S. gordonii DL-1/SMI/II-3 expressing only SpaP; lane 3, parent S. gordonii DL-1. S, proteins from culture supernatant fluids (20 μl); C, proteins extracted from cells by boiling SDS-PAGE sample buffer (20 μl). Arrow indicates the ca. 187-kDa SpaP-S1 fusion protein revealed by the anti-PT antibodies. Numbers on the left are molecular size markers (in kilodaltons).
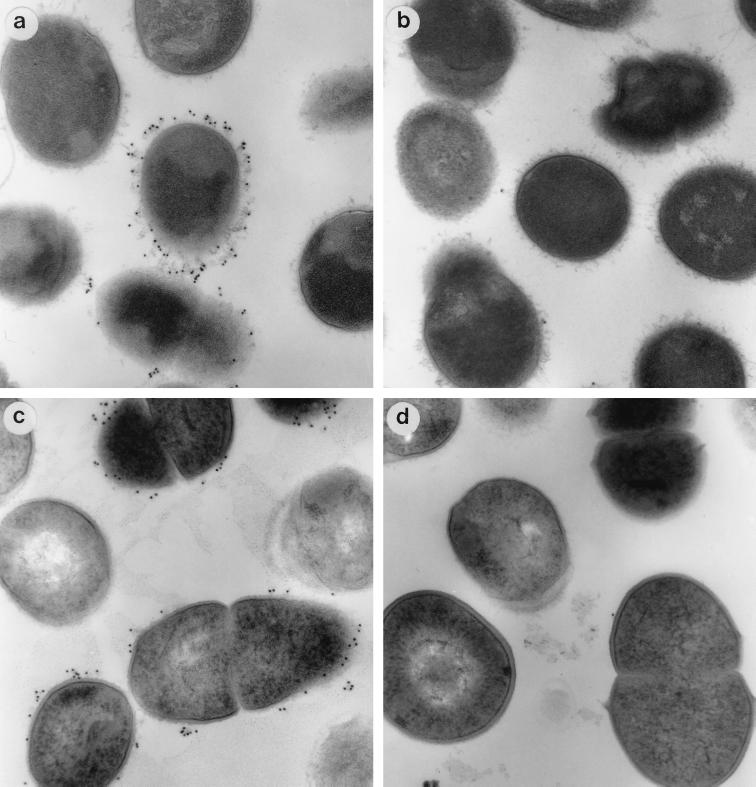
To provide evidence that the fusion protein is surface localized, S. gordonii RJMIII was analyzed by immunoelectron microscopy. Briefly, cells were harvested from 1.5 ml of a late-exponentially grown Todd-Hewitt culture, washed twice in PBS, resuspended, and incubated in 0.5 ml of 1% (wt/vol) gelatin in PBS at room temperature for 10 min. The cells were further treated with 20 mM glycine in PBS for 3 min and 1% (wt/vol) bovine serum albumin (BSA) in PBS for 2 min. After these blocking steps, the cells were resuspended in 100 μl of S. gordonii-adsorbed anti-PT antibodies (dilution, 1/50) or a monoclonal antibody, 4-10A, to SpaP (dilution, 1/100) and were incubated with gentle rocking for 2 h. The cells were washed 4 times with PBS containing 0.1% BSA and were reacted with colloidal gold (diameter, 10 mm)-conjugated goat anti-rabbit immunoglobulin G or goat anti-mouse immunoglobulin G (dilution, 1/20) for 1 h. The cells were then washed 4 times with PBS–0.1% BSA, followed by two washes with PBS, and were finally fixed with 2.5% glutaraldehyde in 0.1 M sodium cacodylate buffer, pH 7.4. Cells were then sectioned and viewed under a Philips 300 electron microscope. As shown in Fig. 3, the fusion protein was clearly found on the cell surface after the cells had been reacted with the anti-SpaP monoclonal antibody (Fig. 3a) or the anti-PT antibodies (Fig. 3b). In contrast, DL-1 cells treated the same way did not exhibit any immunogold particles. To further examine the location of the fusion protein expressed in S. gordonii RJMIII, cellular fractions were prepared from 1 liter of late-exponential culture grown in TYG. Proteins in the supernatant fluids were precipitated with (NH2)SO4 (70% [wt/vol]) and dialyzed against 10 mM Tris buffer, pH 8 (final volume, 15 ml). Cells were washed and broken with a Mickle tissue disintegrator (8). Cell walls were recovered by centrifugation (at 27,000 × g for 30 min at 4°C) and resuspended in 1 ml of 10 mM potassium phosphate buffer, pH 7.5. The cell membrane was separated from the cytoplasm (12 ml) by ultracentrifugation (at 50,000 × g for 1 h at 4°C) and resuspended in 0.25 ml of potassium phosphate buffer. Samples of 15, 1, 12, and 0.25 μl of the extracellular fraction (supernatant), cell wall, cytoplasm, and cell membrane, respectively, were analyzed by Western immunoblotting. These volumes represented proportional amounts of each of the subcellular fractions from the culture. SpaP-S1 was detected by the S. gordonii-adsorbed rabbit anti-PT antibodies (dilution, 1/200). Results showed that the fusion protein was mainly associated with the cell wall, with a small amount found in the extracellular fraction and trace amounts in the cell membrane and cytoplasmic fractions (data not shown). These results strongly indicate that the fusion protein was cell surface localized in S. gordonii RJMIII, and they reconfirm the ability of the C terminus of S. mutans SpaP to anchor to the cell wall in S. gordonii (8).
FIG. 3.
Immunogold electron micrographs of S. gordonii expressing SpaP-S1 fusion protein on the cell surface. After reaction with the monoclonal anti-SpaP antibody (a and b) and the anti-PT antibodies (c and d), the recombinant SpaP-S1 S. gordonii RJMIII cells (a and c) were labeled with gold conjugates, while the parent S. gordonii DL-1 cells (b and d) were not.
Immunogenicity of the recombinant S1.
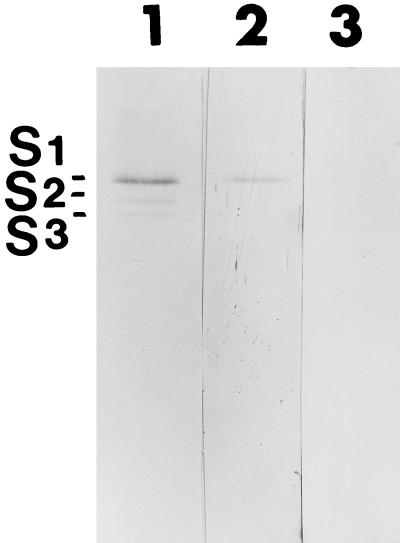
The immunogenicity of the SpaP-S1 fusion protein was investigated by immunizing a New Zealand White rabbit with heat-killed (15 min at 100°C) S. gordonii RJMIII cells (1010 CFU in 1 ml of Freund’s incomplete adjuvant) by using a protocol similar to that described above. The antibody obtained was found to react with the native PT in an ELISA, although the titer of the antiserum was relatively low (1,600). In Western blotting, the anti-SpaP-S1 antiserum clearly recognized the S1 subunit of the native PT, suggesting that the recombinant S1 expressed by S. gordonii is capable of eliciting an immune response (Fig. 4). This finding is consistent with findings by others that recombinant S1 expressed in E. coli, Salmonella, and B. subtilis is immunogenic (2, 3, 18, 24).
FIG. 4.
Western blots showing the specific reactivity of the rabbit anti-SpaP-S1 serum with the S1 subunit of PT. The rabbit anti-PT antiserum (dilution, 1/200) (lane 1) reacted with the S1, S2, and S3 of PT (1 μg; List Biological Laboratories, Inc.). The rabbit anti-SpaP-S1 antiserum (dilution, 1/100) (lane 2) reacted with the S1 subunit of PT only. Preimmune serum (dilution, 1/100) (lane 3) obtained from the same rabbit used to raise the anti-SpaP-S1 serum did not react with PT.
Protective effects of recombinant S1.
The ability of the rabbit anti-SpaP-S1 antiserum to neutralize the cytotoxic effect of PT was assessed by the Chinese hamster ovary (CHO) cell-clustering assay using the method described previously (7). In the assay, 4 times the minimum clustering dose of native PT (Massachusetts Biologics Laboratories, Jamaica Plain, Mass.) was used to allow for a twofold variation. Neutralization titers of antibodies were expressed as the reciprocals of the dilutions which showed the complete neutralization of the cell-clustering effect of PT. The immune serum showed a weak neutralization titer of 4, while the preimmune serum did not show any activity (neutralization titer, 0). The anti-SpaP-S1 antibody was subsequently concentrated sevenfold by (NH)2SO4 precipitation (12) and demonstrated a neutralization titer of 32. A rabbit anti-SpaP antibody prepared previously (12) was similarly concentrated sevenfold and showed a neutralization titer of 2. These results suggest that the anti-SpaP-S1 antibody had a weak ability to neutralize the cytotoxic effect of PT on the CHO cells. Previous studies by Barbieri et al. (2) and Boucher et al. (3) also found that the anti-recombinant S1 antibodies showed weak neutralizing abilities in the CHO cell-clustering assay.
The in vivo protective effect of the recombinant S1 was assessed by the leukocytosis-promoting and histamine-sensitizing assays (7). A cohort of BALB/c female mice (3 weeks old; n = 5) were immunized intraperitoneally (i.p.) with heat-killed (10 min at 100°C) S. gordonii RJMIII cells (109 CFU in 0.2 ml of Freund’s complete adjuvant). The animals were boosted with freshly prepared heat-killed cells in Freund’s incomplete adjuvant via the same route 2 and 3 weeks later. A cohort of nonimmunized mice (n = 6) was used as a control. At 7 days after the last booster, sera were obtained from the animals; the immunized mice had a titer of 12,800 against the native PT by ELISA. Each animal from the immunized and control groups was then injected i.p. with 0.5 μg of native PT (Massachusetts Biologics Laboratories) in 0.2 ml of PBS. The total leukocyte (WBC) count was determined with a hemacytometer on 1 μl of blood taken from the tail vein before and after PT injection. Before PT challenge, the control and immunized mice had average WBC counts of 9.14 × 109/liter (range, 4.5 × 109 to 12.2 × 109) and 8.28 × 109/liter (range, 5.5 × 109 to 10.0 × 109), respectively. Three days after PT injection, the control mice had an average WBC count of 29.8 × 109/liter (range, 26.5 × 109 to 35.0 × 109), 3.3 times higher than that before PT challenge. The average WBC count of the immunized mice was 11.5 × 109/liter (range, 8.75 × 109 to 15.75 × 109) after PT injection, 1.4 times higher than that before the challenge. Each animal was further given 2 mg of histamine diphosphate (Sigma Chemical Co., St. Louis, Mo.) i.p. 4 days after PT challenge, and deaths within 24 h of histamine administration were recorded. All five of the immunized mice survived the treatment, while only one of the six control mice survived. These results strongly suggest that the recombinant S1 fragment expressed by S. gordonii can induce protective antibodies in vivo.
In conclusion, we have successfully surface-expressed in S. gordonii the N-terminal 179-amino-acid S1 fragment as a fusion protein to the S. mutans SpaP antigen. The recombinant S1 is immunogenic and can protect mice from the toxic effect of PT. Construction of this recombinant S. gordonii will allow us to pursue an animal infection model in the future.
Acknowledgments
We thank Annette Morris for assistance in the CHO cell-clustering assay.
This study is supported by an intramural grant from the Faculties of Dentistry and Medicine and in part by the Medical Research Council of Canada.
REFERENCES
- 1.Ayakawa G Y, Boushell L W, Crowley P J, Erdos G W, McArthur W P, Bleiweis A S. Isolation and characterization of monoclonal antibodies specific for antigen P1, a major surface protein of mutans streptococci. Infect Immun. 1987;55:2759–2767. doi: 10.1128/iai.55.11.2759-2767.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barbieri J T, Armellini D, Molkentin J, Rappuoli R. Construction of a diphtheria toxin A fragment-C180 peptide fusion protein which elicits a neutralizing antibody response against diphtheria toxin and pertussis toxin. Infect Immun. 1992;60:5071–5077. doi: 10.1128/iai.60.12.5071-5077.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boucher P, Sato H, Sato Y, Locht C. Neutralizing antibodies and immunoprotection against pertussis and tetanus obtained by use of a recombinant pertussis toxin-tetanus toxin fusion protein. Infect Immun. 1994;62:449–456. doi: 10.1128/iai.62.2.449-456.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dalla-Pozza T, Yan H, Meek D, Guzman C A, Walker M J. Construction and characterization of Salmonella typhimurium aroA simultaneously expressing the five pertussis toxin subunits. Vaccine. 1998;16:522–529. doi: 10.1016/s0264-410x(97)80006-0. [DOI] [PubMed] [Google Scholar]
- 5.De Magistris M T, Romano M, Bartoloni A, Rappuoli R, Tagliabue A. Human T cell clones define S1 subunit as the most immunogenic moiety of pertussis toxin and determine its epitope map. J Exp Med. 1989;169:1519–1532. doi: 10.1084/jem.169.5.1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dunny G M, Lee L N, LeBlanc D J. Improved electroporation and cloning vector system for gram-positive bacteria. Appl Environ Microbiol. 1991;57:1194–1201. doi: 10.1128/aem.57.4.1194-1201.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Halperin S A, Issekutz T B, Kasina A. Modulation of Bordetella pertussis infection with monoclonal antibodies to pertussis toxin. J Infect Dis. 1991;163:355–361. doi: 10.1093/infdis/163.2.355. [DOI] [PubMed] [Google Scholar]
- 8.Homonylo-McGavin M K, Lee S F. Role of the C terminus in antigen P1 surface localization in Streptococcus mutans and two related cocci. J Bacteriol. 1996;178:801–807. doi: 10.1128/jb.178.3.801-807.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jenkinson H F, Lamont R J. Streptococcal adhesion and colonization. Crit Rev Oral Biol Med. 1997;8:175–200. doi: 10.1177/10454411970080020601. [DOI] [PubMed] [Google Scholar]
- 10.Kelly C, Evans P, Bergmeier L A, Lee S F, Progulske-Fox A, Bleiweis A S, Lehner T. Sequence analysis of the cloned streptococcal cell surface antigen I/II (P1) FEBS Lett. 1989;258:127–132. doi: 10.1016/0014-5793(89)81632-1. [DOI] [PubMed] [Google Scholar]
- 11.Laemmli U K. Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature. 1970;227:680–685. doi: 10.1038/227680a0. [DOI] [PubMed] [Google Scholar]
- 12.Lee S F. Identification and characterization of a surface protein-releasing enzymatic activity in Streptococcus mutans and other pathogenic streptococci. Infect Immun. 1992;60:4032–4039. doi: 10.1128/iai.60.10.4032-4039.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee S F. Active release of bound antibody by Streptococcus mutans. Infect Immun. 1995;63:1940–1946. doi: 10.1128/iai.63.5.1940-1946.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Locht C, Keith J M. Pertussis toxin gene: nucleotide sequence and genetic organization. Science. 1986;232:1258–1264. doi: 10.1126/science.3704651. [DOI] [PubMed] [Google Scholar]
- 15.Medaglini D, Pozzi G, King T P, Fischetti V. Mucosal and systemic immune responses to a recombinant protein expressed on the surface of the oral commensal bacterium Streptococcus gordonii after oral colonization. Proc Natl Acad Sci USA. 1995;92:6868–6872. doi: 10.1073/pnas.92.15.6868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Medaglini D, Rush C M, Sestini P, Pozzi G. Commensal bacteria as vectors for mucosal vaccines against sexually transmitted diseases: vaginal colonization with recombinant streptococci induces local and systemic antibodies in mice. Vaccine. 1997;15:1330–1337. doi: 10.1016/s0264-410x(97)00026-1. [DOI] [PubMed] [Google Scholar]
- 17.Paradis F W, Shareck F, Dupont C, Kluepfel D, Morosoli R. Expression and secretion of beta-glucuronidase and pertussis toxin S1 by Streptomyces lividans. Appl Microbiol Biotechnol. 1996;45:646–651. doi: 10.1007/s002530050742. [DOI] [PubMed] [Google Scholar]
- 18.Runeberg-Nyman K, Engstrom O, Lofdahl S, Ylostalo S, Sarvas M. Expression and secretion of pertussis toxin S1 in Bacillus subtilis. Microb Pathog. 1987;3:461–468. doi: 10.1016/0882-4010(87)90016-7. [DOI] [PubMed] [Google Scholar]
- 19.Sambrook J, Fritsch E F, Maniatis T. Molecular cloning: a laboratory manual. 2nd ed. Cold Spring Harbor, N.Y: Cold Spring Harbor Laboratory; 1989. [Google Scholar]
- 20.Saris P, Taira S, Airaksinen U, Palva A, Sarvas M, Palva I, Runeberg-Nyman K. Production and secretion of pertussis toxin subunits in Bacillus subtilis. FEMS Microbiol Lett. 1990;56:143–148. doi: 10.1111/j.1574-6968.1990.tb04138.x. [DOI] [PubMed] [Google Scholar]
- 21.Sato H, Ito A, Chiba J, Sato Y. Monoclonal antibody against pertussis toxin: effect on toxin activity and pertussis infections. Infect Immun. 1984;46:422–428. doi: 10.1128/iai.46.2.422-428.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sato H, Sato Y, Ohishi I. Comparison of pertussis toxin (PT)-neutralizing activities and mouse-protective activities of anti-PT mouse monoclonal antibodies. Infect Immun. 1991;59:3832–3835. doi: 10.1128/iai.59.10.3832-3835.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tamura M, Nogimori K, Murai S, Yajima M, Ito K, Katada T, Ui M, Ishii S. Subunit structure of islet-activating protein, pertussis toxin, in conformity with the A-B model. Biochemistry. 1982;21:5516–5522. doi: 10.1021/bi00265a021. [DOI] [PubMed] [Google Scholar]
- 24.Walker M J, Rohde M, Timmis K N, Guzman C A. Specific lung mucosal and systemic immune responses after oral immunization of mice with Salmonella typhimurium aroA, Salmonella typhi Ty21a, and invasive Escherichia coli expressing recombinant pertussis toxin S1 subunit. Infect Immun. 1992;60:4260–4268. doi: 10.1128/iai.60.10.4260-4268.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weiss A A, Hewlett E L. Virulence factors of Bordetella pertussis. Annu Rev Microbiol. 1986;40:661–686. doi: 10.1146/annurev.mi.40.100186.003305. [DOI] [PubMed] [Google Scholar]