Abstract
Objectives
Mindful Moment is a self-guided, web-based, mindful, and compassionate parenting training for postpartum mothers who experience parenting stress. We aimed to assess Mindful Moment’s feasibility, acceptability, and usability, and to gather preliminary evidence of its effectiveness in reducing parenting stress and outcomes such as mindful parenting, self-compassion, depressive symptoms, anxious symptoms, dispositional mindfulness, mother’s perception of infant temperament, and mother-infant bonding.
Methods
This pilot randomized controlled trial (RCT) was a two-arm trial and followed the CONSORT 2010, CONSORT-EHEALTH, and CONSORT-SPI 2018 extension guidelines. A total of 292 Portuguese mothers were randomly assigned to the intervention group (n = 146) or to the waiting list control group (n = 146) and completed baseline (T1) and postintervention (T2) self-reported assessments.
Results
A total of 31 mothers (21.23%) completed the Mindful Moment intervention. Most mothers evaluated the program as good or excellent (90%), considered that Mindful Moment provided them the kind of help they expected or wanted (61%), were satisfied with the help provided by the program (74.6%), would recommend it to a friend in a similar situation (86.4%), and would use it again if needed (81.4%). Regarding the program’s preliminary effectiveness, mothers in the intervention group presented a greater decrease in parenting stress, a greater increase in dispositional mindfulness, and a greater decrease in their perception of the difficult temperament of their infants from T1 to T2.
Conclusions
This study provides preliminary evidence of the Mindful Moment’s effectiveness and suggests that it is a feasible and acceptable program for postpartum mothers experiencing parenting stress. Further research is needed to confirm these results in a larger RCT.
Trial Registration
ClinicalTrials.gov (NCT04892082).
Keyword: Mindful Moment, Pilot Randomized Controlled Trial, Parenting Stress, Mindful and Compassionate Parenting, Postpartum Period, Web-Based Intervention
The postpartum period is a particularly stressful period in women’s lives and is characterized by numerous challenges and demands (Chivers et al., 2021). This period is marked by numerous reorganizations and changes in mothers’ lives, such as radical changes in familiar routines, greater fatigue and sleep deprivation (e.g., Caçador & Moreira, 2021; Kudo et al., 2014), and great psychological and emotional challenges (Grande et al., 2021). All these challenges may increase parenting stress levels and negatively interfere with parenting.
Parenting stress refers to an aversive psychological and physiological reaction that emerges from attempts to adapt to the demands of parenthood. It arises when parents evaluate their resources as insufficient to respond to parenting demands with success (Deater-Deckard, 2004). During the postpartum period, new tasks and demands may exceed mothers’ perceived resources, leading them to feel difficulties in adapting to the new parenting role. Additionally, it is well established that parenting stress may interfere with sensitive parenting (Booth et al., 2018), increase the likelihood of poorer quality caregiving (Missler et al., 2020), and impair mother-infant bonding (Nordahl et al., 2020). Importantly, it is also associated with poorer indicators of an infant’s development (e.g., Leppert et al., 2018).
Currently, in addition to common postpartum period demands, mothers must deal with the context of the COVID-19 pandemic. Recent studies have already shown that parenting stress levels seem to have been intensified by pandemic-related factors, such as adopted preventive measures (e.g., quarantine, physical distancing, and isolation) that have had a negative impact on parenting practices (e.g., Chung et al., 2020). Specifically, during the postpartum period, several studies have indicated that mothers are experiencing high levels of parenting stress during the current pandemic (e.g., Lin et al., 2022; Omowale et al., 2021). Therefore, it is much needed to promote emotional regulation skills and positive and adaptive parenting skills aimed at helping mothers to better adjust to the postpartum period and to better deal with their parenting stress.
Previous research suggested that mothers’ capacity to regulate their own emotions helps them deal with parenting stress and facilitates more sensitive caregiving (Grande et al., 2021). Also, it may have important implications for both maternal and child emotional health (Morris et al., 2017). Two well-known and highly associated psychological resources that may help mothers regulate their emotions and help them respond more adaptively to parenting stress are mindfulness and self-compassion.
According to Kabat-Zinn (2003), mindfulness is the capacity of being aware, intentionally, of the moment-by-moment experience in a nonjudgmental way. Therefore, mindfulness is intrinsically related to self-compassion, as it pertains to the capacity to observe emotions and mental events without (self-)criticism and with a compassionate attitude. Self-compassion has been described as an attitude of kindness and acceptance toward one’s own suffering and the desire to relieve it, and it involves three interrelated components: self-kindness, common humanity, and mindfulness (Neff, 2003, 2009).
Overall, it has been argued that teaching mindfulness skills to mothers can promote adaptive coping in stressful contexts and in the face of parenting challenges, as well as facilitate sensitive and responsive parenting (Duncan & Bardacke, 2010). In recent years, increasing attention has been given to the application of mindfulness to the parenting context. For instance, a study developed by Parent et al. (2016) with parents of children and adolescents found that higher levels of parents’ dispositional mindfulness were indirectly related to lower levels of negative parenting practices and higher levels of positive parenting practices through higher levels of mindful parenting. Mindful parenting can be described as a more accepting, emotionally attuned, and compassionate way of parenting (Bögels & Restifo, 2014). This mindful approach to parenting includes skills such as the ability to listen to the child with full attention, to adopt a nonjudgmental acceptance of self and child, to be emotionally aware of self and child, to be able to self-regulate in the parenting relationship, and to be compassionate toward the self and the child (Duncan et al., 2009). There is growing evidence that mindful parenting is associated with several positive outcomes in parents and parent–child relationships, such as lower levels of parenting stress (e.g., Moreira & Canavarro, 2018), more positive parenting practices (e.g., Han et al., 2021), and positive parent–child interactions (e.g., Duncan et al., 2015), including in the postpartum period (e.g., Fernandes et al., 2021a).
Similarly, previous studies have consistently found positive associations between self-compassion and positive outcomes in parenting, such as greater parental well-being (Psychogiou et al., 2016), lower parenting stress (Garcia et al., 2021), and more positive parenting practices (Gouveia et al., 2016). In the postpartum period, a recent study showed that mothers’ self-compassion was positively associated with lower levels of parenting stress and higher levels of mindful parenting (Fernandes et al., 2021d).
Additionally, recent systematic reviews suggest that mindful parenting interventions may reduce parenting stress and improve youth psychological functioning (Burgdorf et al., 2019), and parenting interventions that include self-compassion components appear to improve parental self-compassion and mindfulness skills and to reduce depressive and anxious symptoms and parenting stress (Jefferson et al., 2020). Moreover, a recent systematic review that evaluated whether mindfulness- and compassion-based parenting interventions could help parents in the postpartum period develop adaptive parenting skills and provide sensitive and responsive infant care suggested that those interventions seem to be beneficial for promoting positive parenting skills and the quality of parent-infant relationships in the early parenting years, including the postpartum period. However, only seven different face-to-face interventions were identified, showing the scarcity of these types of interventions applied to the postpartum period and the absence of ehealth interventions. Additionally, there is insufficient evidence about the efficacy and effectiveness of those interventions, so future studies with stronger methodologies are needed (Fernandes et al., 2021c).
One of the few mindfulness- and compassion-based interventions developed for postpartum mothers is the Mindful with Your Baby Training (MYBT; Potharst et al., 2017). This intervention is an adaptation of the well-known Mindful Parenting Training (MPT; Bögels & Restifo, 2014) and includes eight weekly group sessions of 2 h in length each, specifically tailored for mothers of babies aged between zero and 18 months, who presented high levels of parenting stress. In a longitudinal study, this training improved mothers’ well-being, self-compassion, mindfulness skills, mindful parenting, parental confidence, and affection and responsivity toward the child. Additionally, this training seemed to reduce mothers’ parenting stress, psychopathology, and hostility expressed during their interactions with their child (Potharst et al., 2017). In a study involving a quasi-experimental nonrandom design, MYBT was shown to decrease parenting stress as well, to improve mothers’ acceptance of the child and to reduce unattuned comments to the child’s mental states in clinically referred mothers of babies and toddlers (Zeegers et al., 2019). Recently, Mindful with Your Baby Training was also studied through a pilot waitlist-controlled trial, in a nonclinical sample of mothers of babies aged between two and 15 months. This study showed that the training improved maternal mindfulness and self-compassion skills, reduced parenting stress, and reduced maternal depressive and anxious symptomatology (Potharst et al., 2022).
The MPT can also be delivered online in a self-guided format. An RCT that included postpartum mothers who were experiencing high levels of parenting stress showed that although only 15.5% of the mothers completed the training, online MPT was effective in improving mothers’ self-compassion and in decreasing symptoms of anxiety and depression and parental overreactivity when compared to a waiting list control (WLC) condition. However, contrary to expectations, the training was not effective in decreasing parenting stress. Only a significant delayed effect (at a 10-week follow-up) was found on a subscale of parenting stress measure (parental role restriction) for the intervention group, with a small effect size (Potharst et al., 2019). Recently, Boekhorst et al. (2021) evaluated online MPT in a nonclinical sample of mothers of toddlers with and without parenting stress. Although only 23.1% of the mothers completed the training, this study highlighted the acceptability of a mindful parenting program for mothers with and without parenting stress. Both studies suggested that the online format increased accessibility and cost-effectiveness as additional advantages to mothers of babies aged between zero and 18 months old.
Online interventions, such as the online MTP, may be particularly suitable for postpartum mothers. Previous studies indicate that traditional face-to-face individual or group interventions are not easily accessible for all mothers during the postpartum period (e.g., Fonseca et al., 2015) and that many mothers identify several barriers (e.g., lack of time to participate in a psychological intervention) for not seeking professional help to cope with emotional difficulties (Fernandes et al., 2021b). In addition, the current pandemic-related restrictions (particularly social distancing) made face-to-face mental health care difficult to access. Therefore, there has been a growing interest and investment in e-mental health as an option to address barriers to seeking help from mental health professionals (Saladino et al., 2020; Wind et al., 2020). For instance, the Portuguese Psychological Association (OPP) recommended implementing psychological interventions for parents and infants using distance communication media during the pandemic context (OPP, 2020).
E-mental health refers to mental health services and information delivered or enhanced through the Internet and related technologies (Christensen et al., 2002). They have the potential for delivering better mental health information and improved and cost-effective mental health services, and they may reduce treatment uptake barriers among at-risk women (Bina, 2020), including postpartum mothers (Lim et al., 2019). Specifically, web-based interventions can be guided by a therapist or fully self-guided. According to Donker et al. (2015), self-guided interventions have particular advantages as they do not require the involvement of a therapist and can therefore be less costly and easily disseminated. Moreover, a self-guided intervention may be done at the participant’s own pace. Recently, a web-based, self-guided preventive intervention was developed to prevent postpartum depression among Portuguese women who presented risk factors for this clinical disorder—the Be a Mom program (Fonseca et al., 2020). However, there is no intervention focused on reducing parenting stress in postpartum mothers through the promotion of a mindful and compassionate approach to parenting.
Hence, the present study describes the results of a pilot randomized controlled trial (RCT) of an online self-guided intervention for mothers in the postpartum period: the Mindful Moment program. Given the pilot nature of this study, we aim to (1) assess the program’s feasibility in terms of adherence, dropout rates, the pattern of program usage (e.g., number of completed modules), the program’s acceptability in terms of the users’ global perceptions of the program and its usability, and (2) gather preliminary evidence of Mindful Moment’s effectiveness in reducing parenting stress (primary outcome) and in changing several secondary outcomes (e.g., self-compassion). The effectiveness of the Mindful Moment program was defined as its ability to significantly reduce parenting stress. It was hypothesized that the Mindful Moment would decrease parenting stress in the intervention group.
Method
The present study consists of an open-label, parallel-group, pilot RCT with two arms designed to test the effectiveness of the Mindful Moment in comparison with a WLC for postpartum mothers presenting moderate or high levels of parenting stress (Parental Stress Scale [PSS] ≥ 41; Mixão, 2007).
Participants
Eligibility criteria to participate in the study were (a) being 18 years of age or more; (b) having a child aged up to 18 months old; (c) presenting moderate or high levels of parenting stress; (d) being female; (e) being Portuguese; (f) being a resident of Portugal; and (g) having Internet access in a desktop, tablet, or telephone. Exclusion criteria were having a current diagnosis of a serious mental health condition (e.g., schizophrenia, substance abuse, bipolar disorder, and personality disorder) (self-reported).
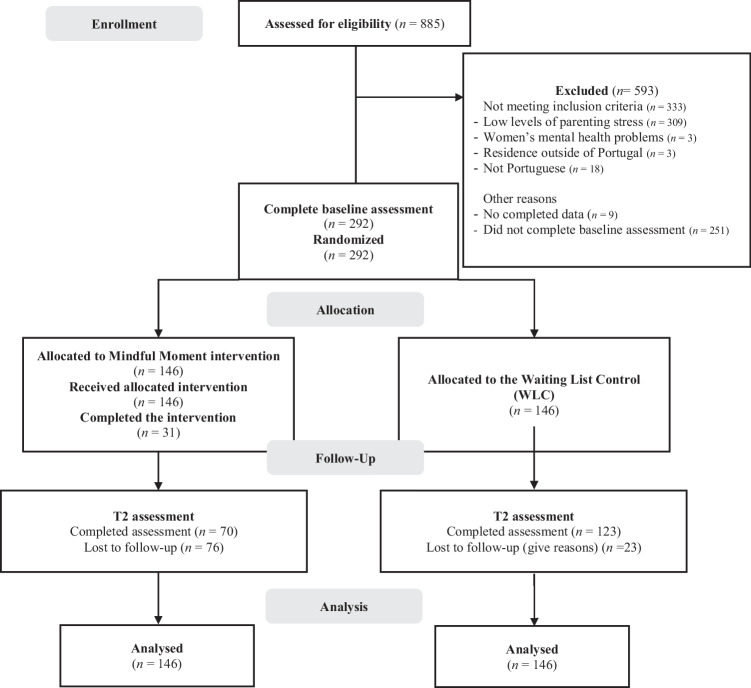
A flow diagram of the participants of the study is presented in Fig. 1. Approximately 885 participants were enrolled in the study. Of the total participants, 593 (67%) were excluded for several reasons (mostly because they did not present moderate/high levels of parenting stress; n = 309, 52.11%). A total of 543 mothers fulfilled the eligibility criteria and received an e-mail invitation to access the Mindful Moment website. Of these, 292 mothers registered on the Mindful Moment website and completed the baseline assessment and were randomized and allocated to the intervention group (n = 146) or to the WLC group (n = 146).
Fig. 1.
Flowchart of the study participants
A sample size of at least 30 participants per condition at postintervention assessment was needed to assess preliminary evidence of effectiveness for the primary outcome (detecting a medium effect size [d = 0.25] with a statistical power of 0.80 in a two-tailed test, p < 0.05). Considering the expected dropout rate for self-guided interventions (> 50%) (e.g., Geraghty et al., 2010), at least 200 participants were needed for randomization. Several online mindfulness interventions evidenced medium effects when compared to inactive control conditions on main outcomes of interest, namely parenting stress (e.g., Spijkerman et al., 2016). The sample size was calculated also considering other self-guided interventions applied to the postpartum period in the Portuguese population (Fonseca et al., 2020; Monteiro et al., 2020), as well as other self-guided interventions (e.g., Beshai et al., 2020).
The final sample was composed of 292 mothers of babies aged between zero and 18 months. The complete baseline sociodemographic, clinical, and COVID-19-related information of mothers and babies of the two groups (intervention group and WLC group) is presented in Table 1.
Table 1.
Sociodemographic, clinical, and COVID-19-related information of the sample
| Experimental group (n = 146) |
Control group (n = 146) |
Comparison analyses | ||
|---|---|---|---|---|
| F/χ2 | p | |||
| Mother’s sociodemographic information | ||||
| Mothers’ age (years) M (SD); range | 34.72 (4.71); 24–46 | 33.34 (5.02); 20–45 | 5.84 | .016* |
| Mothers’ marital status n (%) | 0.46 | .651 | ||
| Living with a partner | 134 (91.8%) | 137 (93.8%) | ||
| Not living with a partner | 12 (8.2%) | 9 (6.2%) | ||
| Mothers’ educational level | ||||
| Basic or secondary education | 8 (7.9%) | 14 (11.6%) | ||
| Higher education | 93 (92.1%) | 107 (88.4%) | ||
| Mothers’ current employment status n (%) | 0.03 | 1 | ||
| Employed | 124 (84.9%) | 123 (84.2%) | ||
| Unemployed, housewives, full-time mothers, students | 22 (15.1%) | 23 (15.8%) | ||
| Maternity leave (yes) | 51 (34.9%) | 54 (37%) | 0.13 | .807 |
| Mothers’ household monthly income n (%) | 0.00 | 1 | ||
| Less than 2000€ | 96 (65.8%) | 96 (65.8%) | ||
| 2000€ or above | 50 (34.2%) | 50 (34.2%) | ||
| Mothers’ area of residence n (%) | 0.02 | 1 | ||
| Urban | 107 (73.3%) | 106 (72.6%) | ||
| Rural | 39 (36.7%) | 40 (27.4%) | ||
| Mothers’ clinical information | ||||
| Number of children n (%) | 0.06 | .904 | ||
| One child | 89 (61%) | 91 (62.3%) | ||
| More than one child | 57 (39%) | 55 (37.7%) | ||
| Previous psychological problems n (%) | 2.32 | .160 | ||
| Yes | 77 (52.7%) | 64 (43.8%) | ||
| No | 69 (47.3%) | 82 (56.2%) | ||
| Current psychological and/or psychiatric problem n (%) | 2.77 | .138 | ||
| Yes | 12 (8.2%) | 21 (14.4%) | ||
| No | 134 (91.8%) | 125 (85.6%) | ||
| Current psychological and/or psychiatric treatment n (%) | 0.87 | .438 | ||
| Yes | 22 (15.1%) | 28 (19.2%) | ||
| No | 124 (84.9%) | 118 (80.8%) | ||
| Obstetric complications n (%) | ||||
| In mothers | 52 (35.6%) | 42 (28.8%) | 1.57 | .260 |
| In babies | 19 (13%) | 10 (6.8%) | 3.10 | .116 |
| Babies’ information | ||||
| Age (months) M (SD); range | 8.21 (5.15); 0–22 | 8.49 (5.55); 0–18 | 0.20 | .658 |
| Sex n (%) | 0.67 | .482 | ||
| Girls | 68 (46.6%) | 75 (51.4%) | ||
| Boys | 78 (53.4%) | 71 (48.6%) | ||
| COVID-19-related information | ||||
| Mother’s COVID-19 diagnosis n (%) | 0.16 | .924 | ||
| Healthy | 130 (89%) | 132 (90.4%) | ||
| Suspected contact with someone infected | 1 (0.7%) | 1 (0.7%) | ||
| Recovered | 15 (10.3%) | 13 (8.9%) | ||
| Baby was infected with COVID-19 n (%) | 0.63 | .597 | ||
| Yes | 6 (4.1%) | 9 (6.2%) | ||
| No | 140 (95.9%) | 137 (93.8%) | ||
| COVID-19 contagion risk group n (%) | 0.04 | 1 | ||
| Yes | 13 (8.9%) | 12 (8.2%) | ||
| No | 133 (91.1%) | 134 (91.8%) | ||
The Portuguese minimum wage in 2020 was 635 €
*p < .05
Procedures
The dissemination of the study was made online through social media websites (Facebook and Instagram). The study was also disseminated in several health care centers through flyers and posters that included information about the study. Recruitment began in April 2021 and lasted until October 2021. We used unpaid cross-postings and paid boosting campaigns (one campaign per week for three days each, targeting women 18–50 years old with interest in maternity and mental health topics) to recruit participants on social media websites. Posts had the following advertisement: “Do you experience stress or difficulties in the mother-infant relationship? Did you have a baby in the last 18 months? Participate in Mindful Moment! We want to know if Mindful Moment is effective in reducing parenting stress. To know if you are eligible to participate in the study, fill out the following form, and the research team will contact you.” Participants who were interested in the study clicked on a link to a survey. The first page of the survey presented the study goals and procedures, as well as the participants’ (e.g., voluntary participation) and researchers’ (e.g., guarantee of confidentiality) roles. Participants were also asked to provide their informed consent to participate in the study. All participants provided their informed consent prior to answering a set of questions to assess eligibility criteria, including the Parental Stress Scale (Mixão et al., 2010), and provided their contact information (e-mail and telephone number). Participants who met the eligibility criteria were contacted through e-mail to make their registration on the Mindful Moment’s website. Participants who did not meet eligibility criteria were sent an e-mail informing them of the reason they could not participate in the study and advising them to seek professional health from the physician or to seek mental health help if needed.
To access the program, participants registered on the Mindful Moment’s website with a protected password. After registration, participants accessed Module 0 (“Introduction to Mindful Moment”), which is a brief informational module, without intervention content, in which the functioning of the program is explained (e.g., its length and structure) and practical suggestions are provided (e.g., using headphones for audio exercises and having a notebook specifically for the Mindful Moment exercises and notes). This module also contained the link for the baseline assessment protocol (Time 1—T1). Participants who completed the baseline assessment were randomized for one of the intervention arms. Those who were allocated to the intervention arm were granted full access to the Mindful Moment program. Participation in the Mindful Moment was free of cost, and no compensation was given to the women for participating in the study.
Participants in the intervention arm received a reminder (by e-mail and telephone) to continue accessing the Mindful Moment once a week for 8 weeks after baseline assessment. Mothers who had a valid telephone number were also contacted by the first author of the present study approximately 3 weeks after baseline to clarify any questions regarding the flow of the program or to help with any difficulties in accessing the website. Participants who completed the program received an e-mail inviting them to complete the postintervention assessment protocol 2–3 days later (Time 2—T2). Participants who did not complete the program were also sent an e-mail with the postintervention assessment 8 weeks after randomization (Time 2—T2). No intervention was offered to participants in the WLC arm, but they were informed that they would receive access to Mindful Moment at the end of the study. Eight weeks after randomization, they were asked to complete the postintervention assessment protocol (Time 2—T2) so that the assessment time was similar to that of the Mindful Moment group. All participants could access usual care from health or mental health services during the study. To reduce dropout rates, e-mail and text message reminders were sent each week to mothers in both groups who failed to complete the T1 and T2 online questionnaires.
Eligible participants who completed the baseline assessment protocol were randomly assigned (parallel assignment; allocation rate 1:1) to the intervention group with access to the Mindful Moment program or to the WLC group. Randomization was performed using a computerized random number generator and was ensured by a second researcher (different from the one responsible for the enrollment and assignment of the participants to the study groups) who had no information about the participants (except the participants’ codes). The randomization sequence was concealed from the researcher responsible for participant enrollment and assignment to groups. After randomization, participants received an e-mail with information about their assigned group.
The intervention arm consisted of the Mindful Moment, which is a self-guided web-based intervention grounded in mindfulness- and compassion-based therapies specifically developed for the postpartum period (Cree, 2010; Potharst et al., 2017, 2019), and on the clinical practice with women in the perinatal period of the researchers who developed the program. Mindful Moment is a completely self-guided program, so no human support is given. However, the first page of the website contains a form so that parents can contact the research team if they need technical support. The Mindful Moment has six sequential modules, with an approximate length of 1 h each. While participants can complete the program at their own pace, it is suggested that they complete one module per week. Each module addresses one or two specific thematic contents. All modules start with a video in which the module’s goals are presented by the main researcher of the present study. Next, the thematic contents and exercises of each module are presented through written materials, visual elements (e.g., images, schemes), and audio tracks. The last section of each module contains recommended homework tasks so that participants can continue the therapeutic practice during the week. For instance, in Module 1, participants are suggested of being aware of their thoughts, body sensations, and response tendencies in parenting stressful situations, with an acceptant, curious, and nonjudgmental posture. Regarding formal practice, participants are suggested of practicing a “3-min breathing space” and a “sitting meditation with attention focused on breathing,” three times a week, each of them. Finally, participants may choose a daily routine activity to practice mindful parenting (e.g., dress or bath the baby).
The Mindful Moment intervention contains psychoeducational materials, formal mediation practices (e.g., breath meditation), self-compassion practices, and mindful parenting exercises. A detailed description of each module is presented in Table 2.
Table 2.
Mindful Moment program
| Module’s title | Content |
|---|---|
| 1. Mindful parenting and parenting stress | Psychoeducation about mindful parenting and parenting stress and exercises to help mothers learn how to respond more adaptively to stressful situations in mother-infant interactions. |
| 2. Beginner’s mind | Psychoeducation about attachment and baby’s signs and exercises to help mothers more easily recognize baby’s signals and respond to them more responsively, without judging or labeling. |
| 3. Self-compassion and self-care | Psychoeducation about compassion and exercises to help mothers develop a more compassionate attitude toward themselves and their parenting role. |
| 4. Reactive vs. responsive parenting | Psychoeducation about the stress response and exercises to help mothers become less reactive in stressful mother-infant situations. |
| 5. Relationship with others [social support and communication] | Psychoeducation and exercises focused on mothers’ relationship with others and on the coparenting relationship. Self-compassion practices. |
| 6. Mindful parenting for life | Reflections on how to promote a mindful parenting approach for the rest of mothers’ lives. |
Measures
Sociodemographic, Clinical, and COVID-19-Related Information
The first part of the assessment protocol was developed by the researchers, and it included standard sociodemographic information (e.g., age), clinical data (e.g., current psychological and/or psychiatric problems), and COVID-19-related information (e.g., mother’s COVID-19 diagnosis).
Mindful Moment’s Feasibility, Acceptability, and Usability
The feasibility of the program was measured by adherence and dropout rates, that is, through the number of completers and users who dropped out from the intervention before completing it. These data were collected through the Mindful Moment website, which allowed reviewing the number of completed modules and the pages accessed in each module.
Also, at the postintervention assessment, participants in the intervention arm completed an additional set of questions about Mindful Moment’s acceptability and usability, developed by the researchers. Specifically, participants were asked about the general quality of the program (“Overall, how do you rate the quality of Mindful Moment?”), answered in a 5-point response scale (0 = very bad; 1 = bad; 2 = reasonable; 3 = good; 4 = excellent); their satisfaction with the support provided by the program (e.g., “Mindful Moment provided me the kind of help I expected or wanted”); their intention to use it again if needed (e.g., “I would use Mindful Moment again, if I needed to”); their intention of recommending it to a friend (e.g., “I would recommend Mindful Moment to a friend in a similar situation”); and the usefulness/relevance of the information learned through the program (e.g., “Mindful Moment helped me to better care for my baby and to better relate with him or her”). These questions were answered on a 2-point response scale (0 = not at all applicable to me/little applicable to me; 1 = very applicable to me/totally applicable to me). Additional questions were presented about the participant’s experience using Mindful Moment, specifically regarding the website and its functioning (e.g., “The graphic design of Mindful Moment (e.g., illustrations, colors used) is attractive”; seven items), each module and exercises (e.g., “The number of modules was adequate”; 16 items), and the mother’s perceived utility of the program (e.g., “To have more positive interactions with the baby”). These questions were answered on a 3-point response scale (0 = disagree; 1 = not agree or disagree; 2 = agree).
Preliminary Effectiveness
Parenting Stress
The Parental Stress Scale (PSS; Berry & Jones, 1995; Mixão et al., 2010) was used to assess parenting stress, both in the eligibility criteria assessment and then as an outcome (postintervention assessment). The questionnaire has 18 items (e.g., “Caring for my child(ren) sometimes takes more time and energy than I have to give”) answered on a 5-point response scale, ranging from 1 (strongly disagree) to 5 (strongly agree). The total score is calculated as the sum of the items, with higher scores indicating greater parenting stress. According to Mixão (2007), a cutoff point might be considered, with scores in PSS < 41 corresponding to low levels of parenting stress and scores ≥ 41 corresponding to moderate or high levels of parenting stress. In the present sample, Cronbach’s alpha coefficient was 0.75 and McDonald’s omega was 0.72, at baseline.
Mindful Parenting
The infant version of the Interpersonal Mindfulness in Parenting Scale (IM-P—infant version; Caiado et al., 2020; Duncan, 2007) was used to assess mindful parenting among parents of infants. This scale contains 28 items (e.g., “It is hard for me to tell what my baby is feeling”), scored on a 5-point response scale, ranging from 1 (never true) to 5 (always true), evaluating mindful parenting skills such as Listening with Full Attention, Emotional Awareness of the Child, Self-Regulation in Parenting, Nonjudgmental Acceptance of Parental Functioning and Compassion for the Child. The total score is the sum of all items, and higher scores indicate higher levels of mindful parenting. At baseline, in the current sample, Cronbach’s alpha coefficient (total score) and McDonald’s omega (total score) were both 0.84.
Self-Compassion
To assess mothers’ self-compassion, the short version of the Self-Compassion Scale (SCS-SF; Castilho et al., 2015; Raes et al., 2011) was used. The SCS-SF comprises 12 items (e.g., “When I’m going through a very hard time, I give myself the caring and tenderness I need”) answered on a 5-point response scale, ranging from 1 (almost never) to 5 (almost always). It is possible to obtain a global measure of self-compassion by estimating the mean of the 12 items, with higher scores indicating higher levels of self-compassion- At baseline, in the present sample, Cronbach’s alpha coefficient was 0.89 and McDonald’s omega was 0.90.
Depressive Symptoms
The Portuguese version of the Edinburgh Postnatal Depression Scale (EPDS; Cox et al., 1987; Figueiredo, 1997) was used to screen for the presence of depressive symptoms in the postpartum period. The EPDS is a widely used 10-item screening scale for antepartum and postpartum depression in which women are asked to rate their emotions (e.g., sadness) over the previous seven days using a 4-point response scale. Higher scores are indicative of greater depressive symptoms. In Portuguese validation studies (Figueiredo, 1997), a score of 10 or higher was found to be indicative of clinically relevant depressive symptoms. In our sample, Cronbach’s alpha coefficient and McDonald’s omega were both 0.85, at baseline.
Anxious Symptoms
The Anxiety Subscale of the Portuguese version of the Hospital Anxiety and Depression Scale (HADS; Pais-Ribeiro et al., 2007; Snaith, 2003) was used to assess levels of anxious symptomatology in the previous week. This subscale contains 7 items (e.g., “I feel tense or wound up”) and uses a 4-point response scale, ranging from 0 (not at all/only occasionally) to 3 (most of the time/a great deal of the time). The total score is the sum of the items, with higher scores indicating higher levels of anxious symptoms. At baseline, in this sample, Cronbach’s alpha coefficient and McDonald’s omega were both 0.81.
Dispositional Mindfulness
Dispositional mindfulness was assessed by the Mindful Attention and Awareness Scale (MAAS; Brown & Ryan, 2003; Gregório & Pinto-Gouveia, 2013). This is a unidimensional self-report measure of trait mindfulness that comprises 15 items (e.g., “I rush through activities without being truly attentive to them”) answered on a 6-point response scale ranging from 1 (almost never) to 6 (almost always). Higher scores reflect higher levels of dispositional mindfulness. At baseline, in this study, Cronbach’s alpha coefficient and McDonald’s omega were both 0.91.
Mother’s Perception of Infant’s Temperament
The Difficult Infant Temperament Questionnaire (DITQ; Azevedo, 2005; Macedo et al., 2011) was used to assess the mother’s perception of her infant’s temperament. This questionnaire assesses the mother’s perception of her infant’s characteristics and behaviors through eight items (e.g., “Is your baby irritable or fussy?”; “Does your baby cry excessively?”; “Is your baby difficult to comfort or calm down?”), answered on a 6-point response scale, ranging from 1 (never/nearly never) to 6 (always/nearly always). A total score is calculated by summing the eight response scores. Higher scores are suggestive of a mother’s perception of her infant’s temperament as more difficult. At baseline, in the present sample, Cronbach’s alpha coefficient was 0.85 and McDonald’s omega was 0.84.
Mother-Infant Bonding
To assess mother-infant bonding, the Postpartum Bonding Questionnaire (PBQ; Brockington et al., 2006; Nazaré et al., 2012) was used. The PBQ is a self-report questionnaire designed to provide an early indication of mother-infant bonding disorders. It has 12 items (e.g., “I feel distant from my baby”) to be rated on a 5-point response scale, between 0 (never) and 5 (always). The total score is calculated as the sum of the items, with higher scores indicating more impaired mother-infant bonding. In the present sample, at baseline, Cronbach’s alpha coefficient was 0.76 and McDonald’s omega was 0.77.
Data Analyses
Data analyses were conducted using the Statistical Package for the Social Sciences (IBM SPSS, version 25.0). Descriptive statistics were computed for all sociodemographic, clinical, COVID-19-related information, study variables, recruitment, retention data, and Mindful Moment’s acceptability and usability.
Comparison tests (one-way ANOVA or chi-square tests) were used to compare the intervention and control groups in terms of sociodemographic, clinical, and COVID-19-related information. Comparison analyses (one-way ANOVA or chi-square tests) of the baseline information between mothers who completed both assessments and those who dropped out of the study were also conducted. Dropout was defined as not completing the primary outcome (parenting stress) at postintervention assessment regardless of the number of modules completed. Comparison analyses were also conducted between completers and noncompleters. Noncompleters were defined as participants who did not complete at least four modules of the program.
To examine the preliminary evidence of the effectiveness of the program, statistical analyses were performed in accordance with the intention-to-treat (ITT) principle following the CONSORT recommendations, namely the extensions of the CONSORT 2010 checklist for pilot trials (Eldridge et al., 2016), CONSORT-EHEALTH (Eysenbach, 2011) and CONSORT-SPI 2018 Extension (Montgomery et al., 2018).
Therefore, all participants who completed the baseline assessment were included in the analyses even if they did not complete the postintervention assessment. To examine the intervention effects at postintervention for the primary and secondary outcome measures, linear mixed models (LMMs) with an autoregressive covariance structure were conducted. This approach allows us to include all participants of the trial in the analysis regardless of whether they dropped out, obtaining an unbiased estimate of the average causal effect as long as the missing at random assumption holds (Siddiqui et al., 2009), which was the case (Little’s MCAR test χ2 = 338.28, p = 0.880). Time was nested within participants. Participants were included as a random intercept. Time variable was coded as time 1 (baseline) = 1 and time 2 (postintervention) = 2. Group was coded as intervention group = 1 and WLC group = 2. Fixed effects were time, group, time × group interaction, and covariates (variables presenting statistically significant differences between intervention and control groups at baseline and between completers and dropouts at postintervention: age, previous psychological problem). To assess the statistical significance of our results, we adopted the conventional level of significance α = 0.05.
Results
Participants, Recruitment, and Baseline Data
At baseline, no differences were found between mothers from the intervention group and from the control group in sociodemographic, clinical, COVID-related, and study variables, with the exception of mothers’ age, with mothers from the intervention group being significantly older than mothers from the control group (F(1, 291) = 5.84, p = 0.016, η2p = 0.020).
At the postintervention assessment, the overall retention rate was 66.01%, with the intervention arm having significantly higher loss to follow-up than the control arm (intervention group: n = 76, 52.1% vs. control group: n = 23, 15.75%, χ2(1) = 42.93, p < 0.001; Cramer’s V = 0.383).
Potential differences between completers of the study and dropouts (participants who did not complete at least the primary outcome measure at T2, i.e., parenting stress) on baseline sociodemographic, clinical, and COVID-19-related information were explored. Differences in previous psychological problems were found, with participants who dropped out presented a higher proportion of a previous psychological problem than completers (completers: n = 83, 43% vs. dropouts: n = 58, 59%, χ2(1) = 6.36, p = 0.013; Cramer’s V = 0.148).
Mindful Moment’s Feasibility, Acceptability, and Usability
A total of 543 mothers fulfilled the eligibility criteria and received an e-mail invitation to access the Mindful Moment website. Of these, 292 mothers registered on the Mindful Moment website and completed the baseline assessment. After randomization, the intervention group (n = 146) had access to the full intervention. Of these, 31 (21.23%) completed the program (i.e., completed at least four modules), and 13 (8.9%) did not initiate any module.
From 146 participants of the intervention group, about 59 participants answered the questionnaire assessing Mindful Moment’s acceptability and their experience using the program. Of the 59 participants, 17 (28.8%) completed all six modules of the program. Regarding the reasons for not completing Mindful Moment (all 42 participants that reported not completing all modules of the program could choose more than one option), most mothers highlighted lack of time (n = 37; 88.1%), followed by personal issues not related to the program (e.g., disease) (n = 9; 21.4%). Additionally, two mothers answered that Mindful Moment was not useful in their case (4.8%), one mother answered that the internet is not the ideal place to discuss this kind of content (2.4%), two mothers answered that they did not feel comfortable due to the online character of the program (e.g., they missed contact with a psychologist in person; 4.8%), and three mothers answered that they had technical issues (difficulty in access to a computer and to the internet; 7.1%).
Moreover, from 59 mothers, one mother (1.7%) reported that she accessed Mindful Moment with her partner and that this had benefits for her own participation (e.g., higher motivation to participate) and for her partner as well (e.g., acquisition of skills and knowledge). Approximately 43 mothers (72.9%) spoke about their participation in Mindful Moment with someone (participants could choose more than one option), such as their partner (n = 26), a family member (n = 12), or a friend (n = 24).
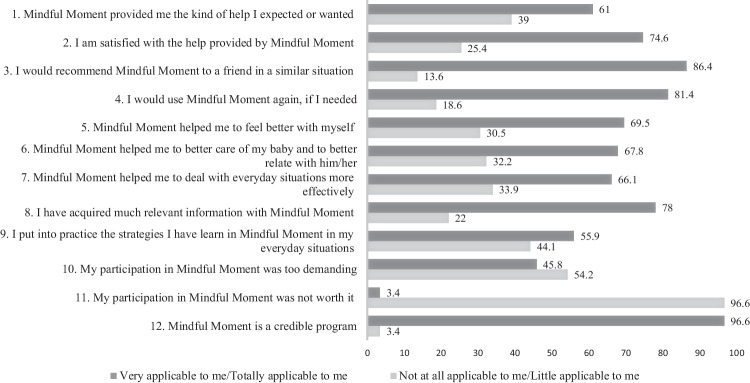
Regarding the perceived quality of Mindful Moment, 90% of mothers evaluated the program as good or excellent. As displayed in Fig. 2, most mothers considered that Mindful Moment provided them the kind of help they expected or wanted, were satisfied with the help provided by Mindful Moment, would recommend it to a friend in a similar situation, and would use it again, if needed. Additionally, mothers have considered that Mindful Moment helped them to feel better about themselves, to better care for their baby and to better relate with them, and to deal with everyday situations more effectively. Most mothers considered that they acquired much relevant information with the program and that they had put into practice the strategies they had learned in Mindful Moment in their everyday situations. However, 27 mothers (45.8%) considered that their participation in Mindful Moment was too demanding, and two mothers considered that their participation was not worth it (3.4%). Overall, 96.6% of mothers considered Mindful Moment to be a credible program. When comparing completers and noncompleters of Mindful Moment, no differences were found in any acceptability question.
Fig. 2.
Participant’s acceptability of Mindful Moment
Regarding the general usability of the program, most mothers agreed that the graphic design of Mindful Moment (e.g., illustrations, colors used) was attractive (n = 46; 78%); that it was easy to navigate through the contents of the program (n = 56; 94.9%); that it was easy to find the content they were looking for (n = 49; 83.1%); that clicking on a button would usually lead them to the place they wanted (n = 49; 83.1%); and that the functioning and organization of Mindful Moment was presented clearly (n = 57; 96.6%). Most mothers disagreed that Mindful Moment’s functioning was very complex (n = 43; 72.9%) or that it was difficult to understand how to use the website (n = 42; 71.2%).
Regarding the general usability of Mindful Moment, compared to completers, a higher proportion of mothers who did not complete the program disagreed with the statements that it was easy to find the content they were looking for in the program (χ2(2) = 6.62, p = 0.037; Cramer’s V = 0.335) and that clicking on a button would usually lead them to the place they wanted (χ2(2) = 6.62, p = 0.037; Cramer’s V = 0.335). Additionally, a higher proportion of noncompleters agreed more that Mindful Moment’s functioning was very complex (χ2(2) = 8.88, p = 0.012; Cramer’s V = 0.388) in comparison with completers.
With regard to the usability of each module, 64.4% (n = 38) of mothers agreed that the number of modules was adequate, 94.9% (n = 56) considered that the language used was clear and easy to understand, and 71.2% (n = 42) considered that the content was presented in an interesting and attractive way. Additionally, most mothers disagreed that Mindful Moment had too much information (n = 35; 59.3%), that the reading of the content became exhausting (n = 32; 54.2%), and that they missed information they were looking for in the program or could not find the information (n = 32; 54.2%). Finally, most mothers agreed that the use of videos at the beginning of each module helped to make the program more real and “human” (n = 48; 81.4%), helped them keep in mind the main message of each module (n = 45; 76.3%), and helped them feel greater proximity to the program (n = 50; 84.7%). When comparing completers and noncompleters, a higher proportion of completers than noncompleters agreed more that the number of modules was adequate (χ2(2) = 8.80, p = 0.012; Cramer’s V = 0.386).
Most mothers (n = 35; 59.3%) agreed that the number of exercises was adequate, assessed the proposed exercises as helpful (n = 48; 81.4%), considered that the tips for performing the exercises were clear and helped them to perform them (n = 44; 74.6%), and assessed the suggested homework activities as interesting and useful (n = 45; 76.3%). However, 13 mothers (22%) found the proposed exercises difficult to accomplish, 38 mothers (64.4%) found the proposed exercises difficult to perform in the presence of the baby, and 41 mothers (69.5%) had difficulty doing the homework exercise during the week. A higher proportion of completers than noncompleters agreed that the number of exercises of Mindful Moment were adequate (χ2(2) = 6.14, p = 0.046; Cramer’s V = 0.323) and that the tips for performing the exercises were clear and helpful (χ2(2) = 10.97, p = 0.004; Cramer’s V = 0.431).
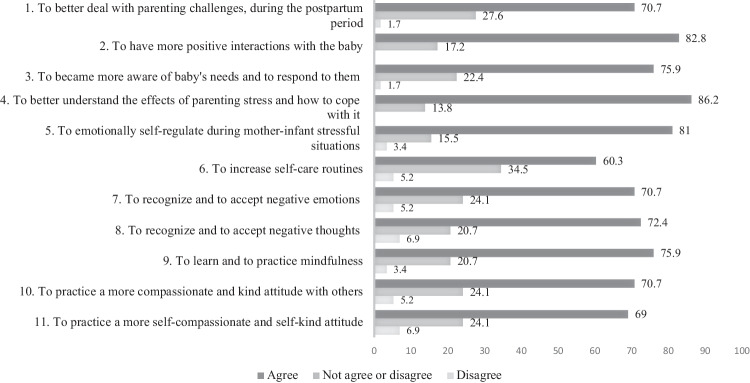
As presented in Fig. 3, overall, mothers had positive perceptions of the Mindful Moment program. For instance, most mothers considered that the program helped them to better understand the effects of parenting stress and how to cope with it (86.2%); to have more positive interactions with the baby (82.8%); and to emotionally self-regulate during mother-infant stressful situations (81%).
Fig. 3.
Participants’ perceived utility of Mindful Moment
Mindful Moment’s Preliminary Effectiveness: Comparison with the Control Group
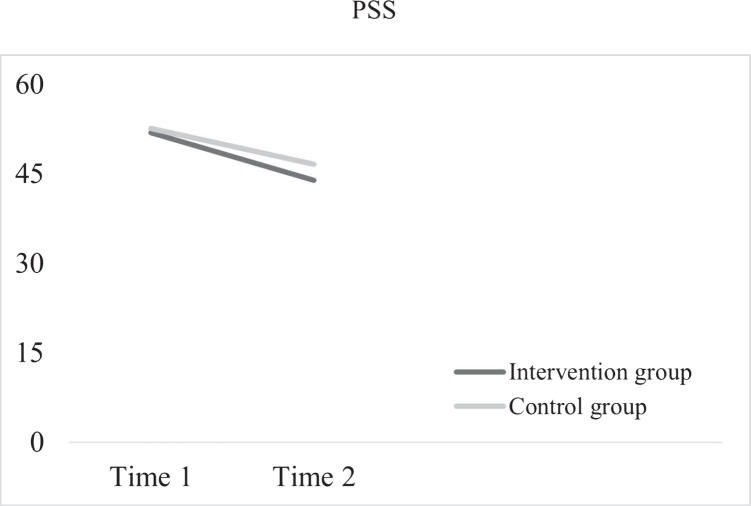
Estimated means and standard deviations, as well as fixed effects for time, group, time × group interaction, and covariates, are presented in Table 3. For the primary outcome measure, the linear mixed model analysis revealed a significant effect of time, a significant effect of group, and a significant time by group interaction. The intervention group had significantly lower PSS scores than the control group from baseline to postintervention. Changes in PSS scores for the intervention and control groups are displayed in Fig. 4.
Table 3.
Estimated marginal means and fixed effects for primary and secondary outcomes
| Group | Time 1 M (SE) |
Time 2 M (SE) |
Effect | B (SE) | 95% CI | p | |
|---|---|---|---|---|---|---|---|
| PSS | Intervention | 51.91 (0.61) | 43.96 (0.80) | Time | 5.97 (0.62) | [4.75, 7.19] | < .001 |
| Control | 52.60 (0.60) | 46.63 (0.64) | Group | − 2.67 (1.03) | [− 4.70, − 0.64] | .010 | |
| Time × group | 1.98 (1.00) | [0.00, 3.95] | .050 | ||||
| Age | 0.00 (0.80) | [− 0.16, 0.16] | .985 | ||||
| Previous psychological problem | 0.66 (0.78) | [− 0.87, 2.20] | .395 | ||||
| IM-P | Intervention | 103.90 (0.92) | 107.73 (1.14) | Time | − 1.59 (0.73) | [− 3.03, − 0.16] | .030 |
| Control | 104.14 (0.91) | 105.73 (0.96) | Group | 2.01 (1.49) | [− 0.93, 4.94] | .180 | |
| Time × group | − 2.24 (1.20) | [− 4.61, 0.12] | .063 | ||||
| Age | 0.16 (0.13) | [− 0.09, 0.41] | .197 | ||||
| Previous psychological Problem | − 3.17 (1.23) | [− 5.59, − 0.75] | .010 | ||||
| SCS-SF | Intervention | 33.23 (0.64) | 35.08 (0.80) | Time | − 1.38 (0.51) | [− 2.39, − 0.37] | .008 |
| Control | 32.30 (0.64) | 33.68 (0.67) | Group | 1.40 (1.05) | [− 0.66, 3.46] | .185 | |
| Time × group | − 0.47 (0.85) | [− 2.14, 1.20] | .579 | ||||
| Age | 0.17 (0.09) | [− 0.00, 0.35] | .051 | ||||
| Previous psychological problem | − 5.02 (0.86) | [− 6.72, − 3.33] | < .001 | ||||
| EPDS | Intervention | 12.41 (0.43) | 10.47 (0.57) | Time | 0.80 (0.40) | [0.02, 1.59] | .045 |
| Control | 12.68 (0.43) | 11.88 (0.46) | Group | − 1.42 (0.73) | [− 2.86, 0.02] | .054 | |
| Time × group | 1.14 (0.66) | [− 1.55, 2.44] | .084 | ||||
| Age | − 0.13 (0.06) | [− 0.24, − 0.02] | .026 | ||||
| Previous psychological problem | 2.58 (0.57) | [1.46, 3.69] | < .001 | ||||
| HADS | Intervention | 10.04 (0.32) | 9.39 (0.42) | Time | 0.03 (0.28) | [− 0.52, 0.58] | .908 |
| Control | 10.07 (0.32) | 10.03 (0.34) | Group | − 0.65 (0.54) | [− 1.71, 0.41] | .232 | |
| Time × group | 0.62 (0.46) | [− 0.29, 1.53] | .178 | ||||
| Age | − 0.12 (0.04) | [− 0.20, − 0.03] | .009 | ||||
| Previous psychological problem | 1.97 (0.43) | [1.13, 2.82] | < .001 | ||||
| MAAS | Intervention | 48.00 (1.15) | 51.58 (1.47) | Time | − 0.33 (0.90) | [− 2.11, 1.44] | .712 |
| Control | 48.29 (1.15) | 48.63 (1.21) | Group | 2.95 (1.91) | [− 0.80, 6.71] | .123 | |
| Time × group | − 3.25 (1.52) | [− 6.25, − 0.25] | .034 | ||||
| Age | 0.09 (0.16) | [− 0.22, 0.41] | .565 | ||||
| Previous psychological problem | − 5.52 (1.56) | [− 8.59, − 2.46] | < .001 | ||||
| DITQ | Intervention | 24.09 (0.65) | 21.79 (0.86) | Time | 0.12 (0.58) | [− 1.03, 1.27] | .837 |
| Control | 23.66 (0.64) | 23.54 (0.69) | Group | − 1.75 (1.11) | [− 3.93, 0.43] | .115 | |
| Time × group | 2.18 (0.97) | [0.26, 4.10] | .026 | ||||
| Age | − 0.10 (0.09) | [− 0.27, 0.08] | .276 | ||||
| Previous psychological probleM | − 0.18 (0.86) | [− 1.87, 0.81] | .834 | ||||
| PBQ | Intervention | 8.31 (0.44) | 6.58 (0.54) | Time | 0.97 (0.34) | [0.29, 1.64] | .005 |
| Control | 9.44 (0.44) | 8.47 (0.46) | Group | − 1.89 (0.71) | [− 3.29, − 0.50] | .008 | |
| Time × group | 0.76 (0.57) | [− 0.36, 1.87] | .182 | ||||
| Age | − 0.03 (0.06) | [− 0.15, 0.09] | .643 | ||||
| Previous psychological problem | 0.19 (0.59) | [− 0.97, 1.35] | .745 |
PSS, Parental Stress Scale; IM-P, Interpersonal Mindfulness in Parenting Scale - Infant version; SCS-SF, Self-Compassion Scale-Short Form; EPDS, Edinburgh Postnatal Depression Scale; HADS, Anxiety Subscale of the Portuguese version of the Hospital Anxiety and Depression Scale; MAAS, Mindful Attention and Awareness Scale; DITQ, Difficult Infant Temperament Questionnaire; PBQ, Postpartum Bonding Questionnaire
Fig. 4.
Intervention and control group trajectories for the PSS (parenting stress) scores from time 1 to time 2 (based on mean estimates from linear mixed models)
For the secondary outcomes, significant effects of time by group interaction were observed for measures of dispositional mindfulness and each mother’s perception of her infant’s temperament. Particularly, participants in the intervention group reported a significantly greater increase in dispositional mindfulness levels from baseline to postintervention than participants in the control group. Participants in the intervention group reported a significantly greater decrease in their perception that their infant had a difficult temperament than participants in the control group from baseline to postintervention. For the remaining secondary outcomes (mindful parenting, self-compassion, depressive symptoms, and mother-infant bonding), a significant effect of time was found, but no interaction effect. In the case of mother-infant bonding, a significant effect of group was also found, with participants in the control group reporting more depressive symptoms and more impaired bonding. No significant effects were found for anxious symptoms.
Discussion
The aim of the present study was to assess Mindful Moment’s feasibility, acceptability, and usability, and to gather preliminary evidence of Mindful Moment’s effectiveness in reducing parenting stress in a sample of postpartum mothers with moderate or high levels of parenting stress. Overall, the results of our study suggest that Mindful Moment is a feasible, acceptable, and usable program for the target population and that it is superior, over time, to a waiting list control condition in reducing parenting stress, increasing dispositional mindfulness, and decreasing the mothers’ perception of the difficult temperament of their infant.
Feasibility, Acceptability, and Usability
Although only 21.23% of participants completed the Mindful Moment program, this result is congruent with previous research conducted with web-based interventions for the postpartum period (Boekhorst et al., 2021; Potharst et al., 2019) in a self-guided format (Monteiro et al., 2020). Most mothers referred to the lack of time as the main reason for not completing the intervention. The postpartum period is demanding, during which mothers usually spend most of their time taking care of their baby and managing family routines and work, which may leave them with little time for themselves or to participate in a psychological program. In addition, the self-guided character of Mindful Moment may have made it easier for mothers to choose to invest their time in other tasks rather than in the program. It is also important to consider that the recruitment period of the present study started in a period of great COVID-19 pandemic–related restrictions in Portugal (Diário da República Eletrónico [DRE], 2021). Therefore, mothers who were initially recruited were in lockdown and may have been involved in telework or taking care of their baby or other children full-time (schools and kindergartens were closed). This may have made it more difficult for mothers to find the time needed to participate in the program. Thus, we can hypothesize that the adherence rate may have been different if the recruitment of participants had not taken place during the pandemic. Finally, we cannot rule out the hypothesis that the Mindful Moment was simply not attractive enough for most mothers to complete the program.
Overall, the acceptability results are encouraging. Approximately 90% of mothers evaluated the Mindful Moment as good or excellent, and most of them would recommend it to a friend in a similar situation and would use it again if needed. In addition, most mothers considered Mindful Moment to be a credible program. Most mothers considered the program to be usable, reporting positive perceptions regarding website features, modules, and exercises. It is important to highlight that when comparing completers and noncompleters, no differences were found in any acceptability question. It may be hypothesized that all modules (especially the first three modules) were interesting, even for noncompleters. These participants may consider that Mindful Moment have helped them as they expected or wanted, they were satisfied, and they recommend it to a friend and use it again if need it, just like those who participated in four modules at least. Regarding the mother-infant relationship, independently of completing the program, all participants felt that the Mindful Moment have helped them in dealing with mother-infant issues. This pilot study allowed us to understand mothers’ opinions about the Mindful Moment website and program characteristics and to identify the strengths and weaknesses of this intervention. In general, the results indicate that Mindful Moment might be a usable intervention for postpartum mothers experiencing parenting stress.
Preliminary Effectiveness
Mothers who participated in Mindful Moment showed a significant reduction in parenting stress from T1 to T2 compared to the control group, supporting our hypothesis. This result is in accordance with recent studies that suggest that mindfulness- (e.g., Chaplin et al., 2021) and compassion-based interventions (e.g., Jefferson et al., 2020) may contribute to decreased levels of parenting stress, including during the postpartum period (Potharst et al., 2017). However, to our knowledge, the only online mindful- and compassion-based parenting intervention for postpartum mothers has not been shown to be effective in reducing parenting stress (Potharst et al., 2019). The results of our study are promising and suggest that in the Portuguese population, these kinds of interventions might be particularly useful, and that Mindful Moment is effective in reducing parenting stress.
With regard to the secondary outcomes, over time, mothers in the intervention group reported a significantly greater increase in dispositional mindfulness levels and a significantly greater decrease in their perception that their infant had a difficult temperament than mothers in the control group. Although Mindful Moment was designed to address parenting stress, the strategies included in the program also seem to have a relevant clinical effect on these outcomes. These results are consistent with previous studies showing that mindful parenting is positively associated with dispositional mindfulness (Gouveia et al., 2016) and negatively associated with a mother’s perception of her infant having a difficult temperament (Fernandes et al., 2021a).
During the Mindful Moment program, mothers practice mindfulness meditations and other exercises to be more aware and present in mother-infant interactions, to pay attention to the baby’s signals and emotional states, and to pause before automatically reacting in stressful situations. It can be hypothesized that these skills may extend to the individual level, promoting a greater ability to be aware and to sustain attention to general experiences and events occurring in the present moment (Brown et al., 2007) and not only in the parenting context. Likewise, it seems that over time, mothers who participated in the Mindful Moment began to perceive their infants’ temperaments as less difficult, which is in accordance with previous research (Potharst et al., 2017). One of the goals of the Mindful Moment program is to help mothers develop an attitude of curiosity, openness, and acceptance toward their babies and in their interactions with them. In the program, mothers are invited to practice a beginner’s mind in the relationship with their babies; that is, they are invited to see their babies and their behaviors without judging or labeling them. Thus, as mothers become more able to make negative judgments and labels about their baby and to stop focusing on challenging characteristics (e.g., a baby who cries a lot and is difficult to soothe), they may be more able to focus on the positive characteristics and aspects, which may lead them to perceive the infant’s temperament as less difficult. In addition, it is already known that a mother who experiences parenting stress tends to perceive her infant’s temperament as more difficult (Oddi et al., 2013), and this may change as she learns how to better cope with their parenting stress. Future studies should analyze these relationships with long-term assessment time and understand the potential mechanisms of change.
Limitations and Future Research
This study has several limitations that should be acknowledged. First, it is an open-label pilot RCT because researchers and participants could not be blinded to treatment allocation. The knowledge of being in the intervention or control group could have influenced outcomes through an expectancy effect. Nevertheless, to minimize bias, the allocation was concealed and was made by a second investigator. Second, the lack of an active control group does not allow us to exclude the possibility that the effects found were due to social desirability or placebo effects. Third, comparisons between the treatment and control groups on sociodemographic, clinical, and COVID-19 information revealed a significant difference in the mother’s age, with the intervention group including significantly older mothers than the control group, which may suggest that randomization was not completely successful. Therefore, a future RCT should use a stratified randomization method to control and balance the influence of participants’ baseline characteristics.
Fourth, the sample was collected online, which may compromise the representativeness of the sample, since participants who participated in the study were likely to be more interested in mental health and parenting subjects and more motivated to participate in a parenting program than those in the general population. Fifth, this study included only mothers, most of whom were living with their partners and were employed, which limits the generalization of these results to fathers and to mothers with different sociodemographic characteristics. Sixth, the validity of the results may have been affected because only self-reported instruments were used to assess the study variables. Participants may have been influenced by social desirability, and their answers may not reliably reflect their feelings or thoughts. Future studies might include clinical interviews or observational measures to complement data evaluation. Moreover, future studies could gather information on participants’ perspectives, through open-ended questions. Associated with this limitation is the common method bias, since multiple constructs are measured using multiple‐item scales used in our surveys. This potentially leads to spurious correlations among the items measuring these constructs owing to response styles, social desirability, and priming effects which are independent from the true correlations among the constructs being measured (e.g., Podsakoff et al., 2012). Seventh, only two assessment times were included in the present study. A longer-term follow-up is required to ascertain whether differential effects are maintained and to evaluate potential mechanisms that explain mothers’ response to treatment.
Finally, the retention rate was only 66%, and a lower attrition rate was found in the control group (which may be explained by the motivation of mothers to receive the Mindful Moment’s program in the future). Although the low adherence may be explained by lack of time, as mothers reported, it is possible that women who dropped out early from the intervention may have disliked some of the intervention features or contents. In fact, a significant portion of the sample has found the intervention overwhelming (about 41% of mothers agreed that Mindful Moment had too much information and 46% that the reading of the content became exhausting), which may have also contributed to the high dropout rates. Perhaps, the daily homework, which included formal and informal meditation practices and mindful parenting practices, is too demanding for mothers with a young baby who is experiencing moderate or elevated levels of parenting stress, even more during a pandemic or stressful contexts. Possibly, a shorter training (in terms of the number of sessions or the length of each session) would fit better with this online, self-guided program format. Further studies should explore this hypothesis.
Despite these limitations, this study has several strengths. For instance, at a methodological level, this study was developed in accordance with the CONSORT guidelines (Eldridge et al., 2016; Eysenbach, 2011; Montgomery et al., 2018), and the ITT principle was followed, which means that all participants (including the noncompleters from both groups) were included in the analyses. Moreover, the results are promising and support the use of Mindful Moment. This is a low-cost and easily accessible program that may be implemented in primary health care services as an early intervention focused on promoting mindful and compassionate parenting and, consequently, a more positive mother-infant relationship in the postpartum period. Future RCTs with larger samples and long-term follow-up assessments are needed to confirm these findings and to explore potential mechanisms that may explain these results. In addition, it would be important to refine and improve some issues of the Mindful Moment program to improve retention rates. For instance, it would be useful to include more videos or interactive materials with practical examples, since most mothers agreed that the use of videos at the beginning of each module helped to make the program more real and “human” and helped them keep in mind the main message of each module and to feel greater proximity to the program; to simplify the exercises that involve the presence of the baby, since most mothers agreed that the proposed exercises were difficult to perform in the presence of the baby; and to reduce homework assignments, given the lack of time that mothers have reported. Further research is needed to consolidate these findings in a larger RCT that can integrate these modifications.
Author Contribution
DVF: designed and executed the study, conducted the data analyses, and wrote the paper. FM: collaborated with the design and data analyses. MCC collaborated in editing the final manuscript. HM: collaborated with the design and writing of the study, assisted with the data analyses, and collaborated in editing the final manuscript.
Funding
This study was funded by the Portuguese Foundation for Science and Technology (DVF: SFRH/BD/132588/2017; FM: SFRH/BD/115585/2016).
Data Availability
The data that support the findings of this study are available on request from the corresponding author [DVF] on reasonable request. The data are not publicly available due to containing information that could compromise research participant privacy/consent.
Declarations
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The Ethics Committee of the Faculty of Psychology and Educational Sciences of the University of Coimbra approved the study on October 4, 2018. Approval was also obtained from the Center Regional Administration of Health (ARS-Center) to disseminate the study to several health care centers in central Portugal.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Azevedo, M. H. (2005). Saúde após o parto (3 meses). Biblioteca Nacional de Portugal.
- Beshai, S., Bueno, C., Yu, M., Feeney, J. R., & Pitariu, A. (2020). Examining the effectiveness of an online program to cultivate mindfulness and self-compassion skills (Mind-OP): Randomized controlled trial on Amazon’s Mechanical Turk. Behaviour Research and Therapy, 134. 10.1016/j.brat.2020.103724 [DOI] [PubMed]
- Berry JO, Jones WH. The Parental Stress Scale: Initial psychometric evidence. Journal of Social and Personal Relationships. 1995;12(3):463–472. doi: 10.1177/0265407595123009. [DOI] [Google Scholar]
- Bina R. Predictors of postpartum depression service use: A theory-informed, integrative systematic review. Women and Birth. 2020;33(1):e24–e32. doi: 10.1016/j.wombi.2019.01.006. [DOI] [PubMed] [Google Scholar]
- Boekhorst M, Hulsbosch LP, Nyklíček I, Spek V, Kastelein A, Bögels S, Pop V, Potharst E. An online mindful parenting training for mothers raising toddlers: Assessment of acceptability, effectiveness, and personal goals. Mindfulness. 2021;12(2):519–531. doi: 10.1007/s12671-020-01542-z. [DOI] [Google Scholar]
- Bögels, S., & Restifo, K. (2014). Mindful parenting: A guide for mental health practitioners. Springer Science.
- Booth AT, Macdonald JA, Youssef GJ. Contextual stress and maternal sensitivity: A meta-analytic review of stress associations with the Maternal Behavior Q-Sort in observational studies. Developmental Review. 2018;48:145–177. doi: 10.1016/j.dr.2018.02.002. [DOI] [Google Scholar]
- Brockington IF, Fraser C, Wilson D. The postpartum bonding questionnaire: A validation. Archives of Womens Mental Health. 2006;9(5):233–242. doi: 10.1007/s00737-006-0132-1. [DOI] [PubMed] [Google Scholar]
- Brown KW, Ryan RM. The benefits of being present: Mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology. 2003;84(4):822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- Brown KW, Ryan RM, Creswell JD. Mindfulness: Theoretical foundations and evidence for its salutary effects. Psychological Inquiry. 2007;18(4):211–237. doi: 10.1080/10478400701598298. [DOI] [Google Scholar]
- Burgdorf, V., Szabo, M., & Abbott, M. J. (2019). The effect of mindfulness interventions for parents on parenting stress and youth psychological outcomes: A systematic review and meta-analysis. Frontiers in Psychology, 10. 10.3389/fpsyg.2019.01336 [DOI] [PMC free article] [PubMed]
- Caçador MI, Moreira H. Fatigue and mindful parenting in the postpartum period: The role of difficulties in emotion regulation and anxious and depressive symptomatology. Mindfulness. 2021;12(9):2253–2265. doi: 10.1007/s12671-021-01688-4. [DOI] [Google Scholar]
- Caiado B, Fernandes DV, Moreira H, Canavarro MC. The Interpersonal Mindfulness in Parenting Scale - Infant Version: Psychometric properties and factor structure in a sample of portuguese mothers in the postpartum period. Psychologica. 2020;63(2):139–157. doi: 10.14195/1647-8606_63-2_7. [DOI] [Google Scholar]
- Castilho P, Pinto-Gouveia J, Duarte J. Evaluating the multifactor structure of the long and short versions of the Self-Compassion Scale in a clinical sample. Journal of Clinical Psychology. 2015;71(9):856–870. doi: 10.1002/jclp.22187. [DOI] [PubMed] [Google Scholar]
- Chaplin TM, Turpyn CC, Fischer S, Martelli AM, Ross CE, Leichtweis RN, Miller AB, Sinha R. Parenting-focused mindfulness intervention reduces stress and improves parenting in highly stressed mothers of adolescents. Mindfulness. 2021;12(2):450–462. doi: 10.1007/s12671-018-1026-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chivers BR, Garad RM, Moran LJ, Lim S, Harrison CL. Support seeking in the postpartum period: Content analysis of posts in web-based parenting discussion groups. Journal of Medical Internet Research. 2021;23(7):e26600. doi: 10.2196/26600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen H, Griffiths K, Evans K. E-mental health in Australia: Implications of the internet and related technologies for policy. Commonwealth Department of Health and Ageing; 2002. [Google Scholar]
- Chung, G., Lanier, P., & Wong, P. Y. J. (2020). Mediating effects of parental stress on harsh parenting and parent-child relationship during coronavirus (COVID-19) pandemic in Singapore. Journal of Family Violence 1-12 10.1007/s10896-020-00200-1 [DOI] [PMC free article] [PubMed]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. The British Journal of Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Cree M. Compassion-focused therapy with perinatal and mother-infant distress. International Journal of Cognitive Therapy. 2010;3(2):159–171. doi: 10.1521/ijct.2010.3.2.159. [DOI] [Google Scholar]
- Deater-Deckard K. Parenting stress. Yale University Press; 2004. [Google Scholar]
- Donker T, Blankers M, Hedman E, Ljótsson B, Petrie K, Christensen H. Economic evaluations of internet interventions for mental health: A systematic review. Psychological Medicine. 2015;45(16):3357–3376. doi: 10.1017/s0033291715001427. [DOI] [PubMed] [Google Scholar]
- DRE (2021). Comunicado do Conselho de Ministros de 15 de abril de 2021. Retrieved from https://www.portugal.gov.pt/pt/gc22/governo/comunicado-de-conselho-de-ministros?i=414
- Duncan L. Assessment of mindful parenting among parents of early adolescents: Development and validation of the Interpersonal Mindfulness in Parenting scale [Doctoral Dissertation] The Pennsylvania State University; 2007. [Google Scholar]
- Duncan L, Bardacke N. Mindfulness-based childbirth and parenting education: Promoting family mindfulness during the perinatal period. Journal of Child & Family Studies. 2010;19(2):190–202. doi: 10.1007/s10826-009-9313-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan L, Coatsworth JD, Gayles JG, Geier MH, Greenberg MT. Can mindful parenting be observed? Relations between observational ratings of mother–youth interactions and mothers’ self-report of mindful parenting. Journal of Family Psychology. 2015;29(2):276–282. doi: 10.1037/a0038857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan L, Coatsworth JD, Greenberg MT. A model of mindful parenting: Implications for parent-child relationships and prevention research. Clinical Child and Family Psychology Review. 2009;12(3):255–270. doi: 10.1007/s10567-009-0046-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eldridge, S. M., Chan, C. L., Campbell, M. J., Bond, C. M., Hopewell, S., Thabane, L., & Lancaster, G. A. (2016). CONSORT 2010 statement: Extension to randomised pilot and feasibility trials. Bmj 355. 10.1136/bmj.i5239 [DOI] [PMC free article] [PubMed]
- Eysenbach G. CONSORT-EHEALTH: Improving and standardizing evaluation reports of web-based and mobile health interventions. Journal of Medical Internet Research. 2011;13(4):e126. doi: 10.2196/jmir.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandes DV, Canavarro MC, Moreira H. The mediating role of parenting stress in the relationship between anxious and depressive symptomatology, mothers’ perception of infant temperament, and mindful parenting during the postpartum period. Mindfulness. 2021;12(2):275–290. doi: 10.1007/s12671-020-01327-4. [DOI] [Google Scholar]
- Fernandes DV, Canavarro MC, Moreira H. Mindful parenting interventions for the postpartum period: Acceptance and preferences of mothers with and without depressive symptoms. Mindfulness. 2021;12(2):291–305. doi: 10.1007/s12671-020-01430-6. [DOI] [Google Scholar]
- Fernandes, D. V., Canavarro, M. C., & Moreira, H. (2021c). Mindfulness- and compassion-based parenting interventions applied to the postpartum period: A systematic review. Journal of Child and Family Studies. 10.1007/s10826-021-02175-z
- Fernandes, D. V., Canavarro, M. C., & Moreira, H. (2021d). The role of mothers’ self-compassion on mother–infant bonding during the COVID-19 pandemic: A longitudinal study exploring the mediating role of mindful parenting and parenting stress in the postpartum period. Infant Mental Health Journal 1-15. 10.1002/imhj.21942 [DOI] [PMC free article] [PubMed]
- Figueiredo B. Depressão pós-parto, interação mãe-bebê e desenvolvimento infantil [Dissertação de Doutoramento não publicada] Universidade do Minho; 1997. [Google Scholar]
- Fonseca A, Gorayeb R, Canavarro MC. Women’s help-seeking behaviours for depressive symptoms during the perinatal period: Socio-demographic and clinical correlates and perceived barriers to seeking professional help. Midwifery. 2015;31(12):1177–1185. doi: 10.1016/j.midw.2015.09.002. [DOI] [PubMed] [Google Scholar]
- Fonseca A, Alves S, Monteiro F, Gorayeb R, Canavarro MC. Be a Mom, a web-based intervention to prevent postpartum depression: Results from a pilot randomized controlled trial. Behavior Therapy. 2020;51(4):616–633. doi: 10.1016/j.beth.2019.09.007. [DOI] [PubMed] [Google Scholar]
- Garcia, A. S., Born, S. L., Carotta, C. L., Lavender-Stott, E. S., & Liu, H. L. (2021). Hope and self-compassion to alleviate parenting stress in the context of the COVID-19 pandemic. The Family Journal. 10.1177/10664807211040836 [DOI] [PMC free article] [PubMed]
- Geraghty AW, Wood AM, Hyland ME. Attrition from self-directed interventions: Investigating the relationship between psychological predictors, intervention content and dropout from a body dissatisfaction intervention. Social Science & Medicine. 2010;71(1):30–37. doi: 10.1016/j.socscimed.2010.03.007. [DOI] [PubMed] [Google Scholar]
- Gouveia MJ, Carona C, Canavarro MC, Moreira H. Self-compassion and dispositional mindfulness are associated with parenting styles and parenting stress: The mediating role of mindful parenting. Mindfulness. 2016;7(3):700–712. doi: 10.1007/s12671-016-0507-y. [DOI] [Google Scholar]
- Grande LA, Olsavsky AK, Erhart A, Dufford AJ, Tribble R, Phan KL, Kim P. Postpartum stress and neural regulation of emotion among first-time mothers. Cognitive, Affective, & Behavioral Neuroscience. 2021;21(5):1066–1082. doi: 10.3758/s13415-021-00914-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregório, S., & Pinto-Gouveia, J. (2013). Mindful attention and awareness: Relationships with psychopathology and emotion regulation. The Spanish Journal of Psychology 16. 10.1017/sjp.2013.79 [DOI] [PubMed]
- Han ZR, Ahemaitijiang N, Yan J, Hu X, Parent J, Dale C, DiMarzio K, Singh NN. Parent mindfulness, parenting, and child psychopathology in China. Mindfulness. 2021;12(2):334–343. doi: 10.1007/s12671-019-01111-z. [DOI] [Google Scholar]
- Jefferson FA, Shires A, McAloon J. Parenting self-compassion: A systematic review and meta-analysis. Mindfulness. 2020;11(9):2067–2088. doi: 10.1007/s12671-020-01401-x. [DOI] [Google Scholar]
- Kabat-Zinn J. Mindfulness-based interventions in context: Past, present, and future. Clinical Psychology: Science and Practice. 2003;10(2):144–156. doi: 10.1093/clipsy.bpg016. [DOI] [Google Scholar]
- Kudo N, Shinohara H, Kodama H. Heart rate variability biofeedback intervention for reduction of psychological stress during the early postpartum period. Applied Psychophysiology and Biofeedback. 2014;39(3):203–211. doi: 10.1007/s10484-014-9259-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leppert B, Junge KM, Röder S, Borte M, Stangl GI, Wright RJ, Hilbert A, Lehmann I, Trump S. Early maternal perceived stress and children’s BMI: Longitudinal impact and influencing factors. BMC Public Health. 2018;18(1):1211. doi: 10.1186/s12889-018-6110-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim, S., Tan, A., Madden, S., & Hill, B. (2019). Health professionals’ and postpartum women’s perspectives on digital health interventions for lifestyle management in the postpartum period: A systematic review of qualitative studies. Frontiers in Endocrinology 10. 10.3389/fendo.2019.00767 [DOI] [PMC free article] [PubMed]
- Lin HC, Zehnah PL, Koire A, Mittal L, Erdei C, Liu CH. Maternal self-efficacy buffers the effects of COVID-19–related experiences on postpartum parenting stress. Journal of Obstetric, Gynecologic & Neonatal Nursing. 2022;51(2):177–194. doi: 10.1016/j.jogn.2021.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macedo A, Marques M, Bos S, Maia BR, Pereira T, Soares MJ, Valente J, Gomes AA, Nogueira V, Azevedo MH. Mother’s personality and infant temperament. Infant Behavior and Development. 2011;34(4):552–568. doi: 10.1016/j.infbeh.2011.06.009. [DOI] [PubMed] [Google Scholar]
- Missler M, van Straten A, Denissen J, Donker T, Beijers R. Effectiveness of a psycho-educational intervention for expecting parents to prevent postpartum parenting stress, depression and anxiety: A randomized controlled trial. BMC Pregnancy and Childbirth. 2020;20(1):658. doi: 10.1186/s12884-020-03341-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mixão, M. G. (2007). Comportamentos parentais e recurso às urgências pediátricas: Estudo do stresse parental, percepção de vulnerabilidade infantil e esforço económico familiar. Instituto Superior de Psicologia Aplicada.
- Mixão, M. L., Leal, I., & Maroco, J. (2010). Escala de Stress Parental. In I. Leal & J. Maroco (Eds.), Avaliaçãoem sexualidade eparentalidade. LivPsic.
- Monteiro F, Fonseca A, Pereira M, Alves S, Canavarro MC. What protects at-risk postpartum women from developing depressive and anxiety symptoms? The role of acceptance-focused processes and self-compassion. Journal of Affective Disorders. 2019;246:522–529. doi: 10.1016/j.jad.2018.12.124. [DOI] [PubMed] [Google Scholar]
- Monteiro F, Pereira M, Canavarro MC, Fonseca A. Be a Mom's efficacy in enhancing positive mental health among postpartum women presenting low risk for postpartum depression: Results from a pilot randomized trial. International Journal of Environmental Research and Public Health. 2020;17(13):4679. doi: 10.3390/ijerph17134679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montgomery P, Grant S, Mayo-Wilson E, Macdonald G, Michie S, Hopewell S, Moher D. Reporting randomised trials of social and psychological interventions: The CONSORT-SPI 2018 Extension. Trials. 2018;19(1):407. doi: 10.1186/s13063-018-2733-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreira H, Canavarro M. The association between self-critical rumination and parenting stress: The mediating role of mindful parenting. Journal of Child and Family Studies. 2018;27(2):2265–2275. doi: 10.1007/s10826-018-1072-x. [DOI] [Google Scholar]
- Morris AS, Criss MM, Silk JS, Houltberg BJ. The impact of parenting on emotion regulation during childhood and adolescence. Child Development Perspectives. 2017;11(4):233–238. doi: 10.1111/cdep.12238. [DOI] [Google Scholar]
- Nazaré, B., Fonseca, A., & Canavarro, M. C. (2012). Postpartum Bonding Questionnaire: Estudo da versão portuguesa numa amostra comunitária. VIII Congresso Iberoamericano de Avaliação Psicológica/XV Conferência Internacional de Avaliação Psicológica: Formas e Contextos.
- Neff KD. Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self and Identity. 2003;2(2):85–101. doi: 10.1080/15298860309032. [DOI] [Google Scholar]
- Neff KD. Self-compassion. In: Leary MR, Hoyle RH, editors. Handbook of individual differences in social behavior. The Guilford Press; 2009. pp. 561–573. [Google Scholar]
- Nordahl D, Rognmo K, Bohne A, Landsem IP, Moe V, Wang CEA, Høifødt RS. Adult attachment style and maternal-infant bonding: The indirect path of parenting stress. BMC Psychology. 2020;8(1):58. doi: 10.1186/s40359-020-00424-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oddi KB, Murdock KW, Vadnais S, Bridgett DJ, Gartstein MA. Maternal and infant temperament characteristics as contributors to parenting stress in the first year postpartum. Infant and Child Development. 2013;22(6):553–579. doi: 10.1002/icd.1813. [DOI] [Google Scholar]
- Omowale SS, Casas A, Lai YH, Sanders SA, Hill AV, Wallace ML, Rathbun SL, Gary-Webb TL, Burke LE, Davis EM, Mendez DD. Trends in stress throughout pregnancy and postpartum period during the COVID-19 pandemic: Longitudinal study using ecological momentary assessment and data from the postpartum mothers mobile study. JMIR Mental Health. 2021;8(9):e30422. doi: 10.2196/30422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Portuguese Psychological Association (2020). Recomendações para a intervenção psicológica durante a gravidez e puerpério. https://www.ordemdospsicologos.pt/ficheiros/documentos/intervencaopsicologica_gravidez_puerperio.pdf
- Pais-Ribeiro J, Silva I, Ferreira T, Martins A, Meneses R, Baltar M. Validation study of a Portuguese version of the Hospital Anxiety and Depression Scale. Psychology, Health & Medicine. 2007;12(2):225. doi: 10.1080/13548500500524088. [DOI] [PubMed] [Google Scholar]
- Parent J, McKee LG, J, N. R., & Forehand, R. The association of parent mindfulness with parenting and youth psychopathology across three developmental stages. Journal of Abnormal Child Psychology. 2016;44(1):191–202. doi: 10.1007/s10802-015-9978-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Podsakoff PM, MacKenzie SB, Podsakoff NP. Sources of method bias in social science research and recommendations on how to control it. Annual Review of Psychology. 2012;63:539–569. doi: 10.1146/annurev-psych-120710-100452. [DOI] [PubMed] [Google Scholar]
- Potharst E, Aktar E, Rexwinkel M, Rigterink M, Bögels S. Mindful With Your Baby: Feasibility, acceptability, and effects of a mindful parenting group training for mothers and their babies in a mental health context. Mindfulness. 2017;8(5):1236–1250. doi: 10.1007/s12671-017-0699-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potharst, E., Boekhorst, M., Cuijlits, I., van Broekhoven, K., Jacobs, A., Spek, V., Nyklicek, I., Bögels, S., & Pop, V. (2019). A randomized control trial evaluating an online mindful parenting training for mothers with elevated parental stress. Frontiers in Psychology 10. 10.3389/fpsyg.2019.01550 [DOI] [PMC free article] [PubMed]
- Potharst ES, Veringa-Skiba I, van Broekhuizen E, Bögels SM. Mindful with your baby for mothers of infants with (parental) stress in a non-clinical setting: A wait-list controlled pilot trial. BMC Pregnancy and Childbirth. 2022;22(1):1–11. doi: 10.1186/s12884-022-04640-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Psychogiou L, Legge K, Parry E, Mann J, Nath S, Ford T, Kuyken W. Self-compassion and parenting in mothers and fathers with depression. Mindfulness. 2016;7(4):896–908. doi: 10.1007/s12671-016-0528-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raes F, Pommier E, Neff KD, Van Gucht D. Construction and factorial validation of a short form of the Self-Compassion Scale. Clinical Psychology & Psychotherapy. 2011;18(3):250–255. doi: 10.1002/cpp.702. [DOI] [PubMed] [Google Scholar]
- Saladino, V., Algeri, D., & Auriemma, V. (2020). The psychological and social impact of COVID-19: New perspectives of well-being. Frontiers in Psychology 11. 10.3389/fpsyg.2020.577684 [DOI] [PMC free article] [PubMed]
- Siddiqui O, Hung HM, O'Neill R. MMRM vs. LOCF: A comprehensive comparison based on simulation study and 25 NDA datasets. Journal of Biopharmaceutical Statistics. 2009;19(2):227–246. doi: 10.1080/10543400802609797. [DOI] [PubMed] [Google Scholar]
- Snaith R. The hospital anxiety and depression scale. Health and Quality of Life Outcomes. 2003;1:29–29. doi: 10.1186/1477-7525-1-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spijkerman MP, Pots WT, Bohlmeijer ET. Effectiveness of online mindfulness-based interventions in improving mental health: A review and meta-analysis of randomised controlled trials. Clinical Psyhcology Review. 2016;45:102–114. doi: 10.1016/j.cpr.2016.03.009. [DOI] [PubMed] [Google Scholar]
- Wind, T. R., Rijkeboer, M., Andersson, G., & Riper, H. (2020). The COVID-19 pandemic: The ‘black swan’ for mental health care and a turning point for e-health. Internet interventions 20. 10.1016/j.invent.2020.100317 [DOI] [PMC free article] [PubMed]
- Zeegers, M. A. J., Potharst, E., Veringa-Skiba, I. K., Aktar, E., Goris, M., Bögels, S. M., & Colonnesi, C. (2019). Evaluating Mindful With Your Baby/Toddler: Observational changes in maternal sensitivity, acceptance, mind-mindedness, and dyadic synchrony. Frontiers in Psychology 10. 10.3389/fpsyg.2019.00753 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author [DVF] on reasonable request. The data are not publicly available due to containing information that could compromise research participant privacy/consent.