Abstract
This study describes a quick (<12 h) assay for detecting temperature decreases in BALB/c and C57BL/6 mice injected intraperitoneally (i.p.) with staphylococcal enterotoxin A (SEA), SEB, or SEC3 or toxic shock syndrome toxin 1 and a potentiating dose of lipopolysaccharide (LPS). Toxin-specific antisera effectively neutralized the temperature fluctuations in this model. Orally administered SEA or SEB (50 μg/animal), with or without LPS, did not have an effect on temperature or lethality. Versus wild-type mice, transgenic knockout mice lacking the p55 receptor for tumor necrosis factor (TNF) or gamma interferon were protected against an i.p. challenge of SEA plus LPS. The p75 receptor for TNF and intercellular adhesion molecule 1 have a negligible role in this toxic shock model.
Staphylococcus aureus causes many diseases in humans (6), and superantigens like the staphylococcal enterotoxins (SEs) plus toxic shock syndrome toxin 1 (TSST-1) are considered important virulence factors that induce immunosuppression in a host, thus providing a distinctly advantageous scenario for a pathogen (11, 25). Current in vivo investigations with the SEs and TSST-1 have vigorously concentrated on murine models (9, 20, 28, 32). Relative to the monkey emetic (36) or rabbit (7) models, mice afford an inexpensive alternative for studying (i) the in vivo effects of the SEs and TSST-1, (ii) neutralizing antibodies and therapeutics used against the SEs and TSST-1, and (iii) recombinantly attenuated SEs and TSST-1 used as vaccine candidates (1, 32, 33, 39, 40).
Various groups have shown that bacterial endotoxin plays a role in augmenting the biological activities of SEs, TSST-1, or streptococcal pyrogenic exotoxins (3, 8, 15, 16, 18, 24, 26, 27, 30, 34, 35), possibly by preventing superantigen-induced death of T cells (38) and thus sustaining a continued, potentially lethal release of proinflammatory cytokines. Previous studies with different SEs and TSST-1 in an LPS-potentiated murine model reveal a strong correlation between toxicity and increased serum levels of proinflammatory cytokines, like interleukins 1 and 6 (IL-1 and IL-6, respectively), tumor necrosis factor (TNF), and gamma interferon (IFN-γ) (32, 33, 39), that play a pivotal role in superantigen-mediated shock (21). Subsequent vaccine efforts with SEA (1), SEB (39, 40), and TSST-1 (33) have also been quite successful in this murine model.
In this report, different SEs and TSST-1 were given orally or injected intraperitoneally (i.p.) into LPS-potentiated mice to determine if body temperature represented a quick and reliable indicator of intoxication. Additional work established the effectiveness of passively administered antiserum in preventing toxin-induced fluctuations of temperature. Finally, experiments in transgenic knockout mice further defined the role of individual cytokines and a lymphocyte adhesion molecule in this model for staphylococcal superantigenic shock.
Purified staphylococcal toxins (Toxin Technology, Sarasota, Fla.) and Escherichia coli LPS (O55:B5) (Difco Laboratories, Detroit, Mich.) were reconstituted in sterile, pyrogen-free phosphate-buffered saline (PBS [pH 7.4]) and stored at −50°C. The endotoxin levels of all toxin preparations were determined by a Limulus amebocyte lysate assay (BioWhittaker, Walkersville, Md.) and contained <1 ng of endotoxin/mg of protein.
Male BALB/c and C57BL/6 mice (18 to 20 g) were housed in a specific-pathogen-free environment. Sterile temperature-identification transponders (IPTT-100) were purchased from Biomedic Data Systems (Maywood, N.J.) and implanted subcutaneously. As previously described (32), mice (n = 6 to 10 per group) were each injected i.p. at zero hour with a SE or TSST-1, followed 4 h later with 80 or 170 μg of LPS for BALB/c or C57BL/6 mice, respectively. Two different strains were used for our studies, because C57BL/6 mice express a different isotype (H-2b) of the class II major histocompatibility complex versus the BALB/c strain (H-2d), and this can have a profound effect upon the in vitro and in vivo properties of these toxins (22, 31, 32, 33, 37). Temperatures were recorded every hour, for a total of 12 h. Tables 1 and 2, respectively, show the temperature results in BALB/c and C57BL/6 mice following an i.p. injection of SEA, SEB, SEC3, or TSST-1. All of these toxins produced significant hypothermic effects within 12 h, relative to uninjected controls or mice given bovine serum albumin (BSA) plus LPS or PBS plus LPS. Although deaths were recorded by 72 h for all toxins tested, there was no lethality within the initial 12-h period of any experiment. The temperature decreases in BALB/c mice were most dramatic with SEB and TSST-1, whereas SEA was more effective in the C57BL/6 strain.
TABLE 1.
Temperature effects of staphylococcal toxins on BALB/c mice
| Toxin (μg/animal)a | Temp reading (°C) atb:
|
Total no. of dead/alive micec | ||||
|---|---|---|---|---|---|---|
| 0 h | 3 h | 6 h | 9 h | 12 h | ||
| SEA | ||||||
| 10 | 37.6 ± 0.5 | 36.8 ± 0.4 | 35.9 ± 0.5 | 29.4 ± 1.5* | 29.6 ± 1.6* | 8/2 |
| 0.5 | 36.5 ± 1.2 | 35.9 ± 0.8 | 35.5 ± 0.6 | 31.5 ± 1.8* | 31.2 ± 1.9* | 5/5 |
| 10 + PBS | 36.9 ± 0.6 | 36.9 ± 0.5 | 36.9 ± 0.5 | 37.2 ± 0.5 | 37.4 ± 0.7 | 0/10 |
| SEB | ||||||
| 10 | 38.0 ± 1.1 | 37.2 ± 0.3 | 35.6 ± 0.7 | 30.6 ± 0.8* | 29.7 ± 0.7* | 8/0 |
| 0.5 | 37.4 ± 0.8 | 37.0 ± 0.6 | 35.8 ± 0.8 | 29.9 ± 1.8* | 30.5 ± 1.4* | 7/3 |
| 0.1 | 36.2 ± 0.7 | 36.5 ± 0.5 | 36.0 ± 0.4 | 34.9 ± 1.7 | 36.0 ± 1.0* | 0/9 |
| 10 + PBS | 37.6 ± 0.2 | 37.0 ± 0.3 | 36.3 ± 0.4 | 36.1 ± 0.3 | 37.2 ± 0.6 | 0/6 |
| SEC3 | ||||||
| 10 | 36.1 ± 0.6 | 35.6 ± 0.4 | 34.4 ± 0.6* | 30.5 ± 1.5* | 31.1 ± 1.7* | 4/6 |
| 2 | 36.0 ± 1.4 | 36.3 ± 1.5 | 34.9 ± 1.5 | 35.6 ± 0.9 | 36.1 ± 1.0 | 0/10 |
| 10 + PBS | 37.0 ± 0.2 | 36.4 ± 0.5 | 36.0 ± 0.3 | 35.8 ± 0.3 | 37.2 ± 0.3 | 0/10 |
| TSST-1 | ||||||
| 8 | 36.9 ± 0.3 | 36.4 ± 0.5 | 35.5 ± 0.4* | 30.3 ± 2.2* | 28.2 ± 1.2* | 7/0 |
| 0.5 | 37.6 ± 1.1 | 37.0 ± 0.4 | 36.1 ± 0.8 | 32.7 ± 1.8* | 29.7 ± 1.8* | 3/3 |
| 0.1 | 38.2 ± 0.6 | 37.3 ± 0.5 | 36.2 ± 0.5 | 34.6 ± 1.3* | 35.2 ± 1.8* | 0/9 |
| 8 + PBS | 37.0 ± 0.5 | 36.2 ± 0.6 | 36.1 ± 0.5 | 35.9 ± 0.3 | 37.0 ± 0.3 | 0/9 |
| PBS + LPS (80) | 38.7 ± 0.4 | 37.4 ± 0.2 | 36.9 ± 0.5 | 36.5 ± 0.7 | 36.8 ± 1.0 | 0/7 |
| BSA (10) + LPS (80) | 36.6 ± 0.3 | 36.3 ± 0.3 | 36.2 ± 0.5 | 36.0 ± 1.2 | 37.0 ± 0.8 | 0/10 |
Toxin dose per animal, followed 4 h later with an i.p. injection of LPS (80 μg). Toxin controls were given PBS, not LPS. The LPS controls were given PBS plus LPS or BSA plus LPS.
Mean temperature reading ± standard deviation of group designated at time points after the toxin injection (zero hour). *, statistically different (P < 0.05) from the BSA plus LPS controls as determined by a two-tailed t test with SPSS/PC+ (Chicago, Ill.).
Recorded at 72 h.
TABLE 2.
Temperature effects of staphylococcal toxins on C57BL/6 mice
| Toxin (μg/animal)a | Temp reading (°C) atb:
|
Total no. of dead/alive micec | ||||
|---|---|---|---|---|---|---|
| 0 h | 3 h | 6 h | 9 h | 12 h | ||
| SEA | ||||||
| 10 | 36.8 ± 0.7 | 36.5 ± 0.7 | 35.3 ± 0.7* | 30.8 ± 1.5* | 28.9 ± 1.3* | 10/0 |
| 0.5 | 37.8 ± 0.5 | 37.0 ± 0.5 | 35.8 ± 0.8* | 31.1 ± 1.2* | 28.4 ± 1.4* | 9/1 |
| 0.1 | 38.2 ± 0.4 | 36.7 ± 0.6 | 35.9 ± 0.9* | 30.2 ± 1.7* | 28.8 ± 1.4* | 5/4 |
| 10 + PBS | 37.8 ± 0.8 | 36.9 ± 0.5 | 36.0 ± 0.6 | 35.8 ± 0.6 | 36.6 ± 0.6 | 0/10 |
| SEB | ||||||
| 10 | 37.9 ± 0.4 | 36.3 ± 0.4 | 36.1 ± 0.4* | 35.4 ± 1.2 | 34.0 ± 1.6* | 1/8 |
| 2 | 37.3 ± 0.7 | 36.5 ± 0.7 | 36.8 ± 0.5 | 36.6 ± 0.8 | 34.8 ± 1.5 | 0/10 |
| 10 + PBS | 37.8 ± 0.7 | 36.6 ± 0.6 | 35.7 ± 0.8 | 35.6 ± 0.6 | 36.6 ± 0.8 | 0/10 |
| SEC3 | ||||||
| 10 | 36.8 ± 0.9 | 36.9 ± 0.6 | 36.4 ± 0.5* | 34.6 ± 1.9 | 32.6 ± 1.2* | 3/7 |
| 2 | 36.9 ± 0.3 | 36.5 ± 0.8 | 36.1 ± 0.9* | 35.2 ± 1.6 | 33.1 ± 0.9* | 0/10 |
| 10 + PBS | 37.0 ± 0.6 | 36.9 ± 0.6 | 35.9 ± 0.6 | 35.7 ± 0.5 | 37.0 ± 0.4 | 0/10 |
| TSST-1 | ||||||
| 10 | 37.2 ± 0.8 | 37.0 ± 0.6 | 36.5 ± 0.8 | 35.0 ± 1.6* | 32.3 ± 1.5* | 5/5 |
| 2 | 37.6 ± 1.0 | 36.9 ± 0.6 | 36.7 ± 1.0 | 36.0 ± 1.3 | 35.2 ± 0.8 | 3/7 |
| 10 + PBS | 38.1 ± 0.3 | 36.8 ± 0.4 | 36.3 ± 0.4 | 35.9 ± 0.4 | 37.0 ± 0.4 | 0/10 |
| PBS LPS (170) | 38.0 ± 0.8 | 36.9 ± 0.3 | 36.4 ± 0.2 | 36.3 ± 0.4 | 36.1 ± 0.5 | 0/8 |
| BSA (10) + LPS (170) | 37.7 ± 0.5 | 36.7 ± 0.6 | 37.2 ± 0.8 | 36.3 ± 0.9 | 35.4 ± 0.7 | 0/9 |
Toxin dose per animal, followed 4 h later with an i.p. injection of LPS (170 μg). Toxin controls were given PBS, not LPS. The LPS controls were given PBS plus LPS or BSA plus LPS.
Mean temperature reading ± standard deviation of group designated at time points after the toxin injection (zero hour). *, statistically different (P < 0.05) from the BSA plus LPS controls as determined by a two-tailed t test.
Recorded at 72 h.
The temperature effects of orally administered SEA and SEB were also tested in C57BL/6 and BALB/c mice, respectively. Recent work by Blank et al. (5) reveals that mice injected intravenously with SEB (25 μg) plus LPS (50 μg) develop apoptotic epithelial cells lining the colon and jejunum crypts within 16 h. In our model, mice injected i.p. with a sufficient dose of any SE plus LPS develop diarrhea. The oral effects (via gavage) of SEA or SEB at 50 μg/mouse were tested 5 to 10 min after the stomach acidity was neutralized with 0.2 M NaHCO3. The potentiated effects of LPS (80 and 170 μg administered to BALB/c and C57BL/6 mice, respectively) were tested orally and by an i.p. injection at 4 h after the toxin dose. No temperature fluctuations, diarrhea, or death was attributed to orally administered SEA or SEB, with or without LPS.
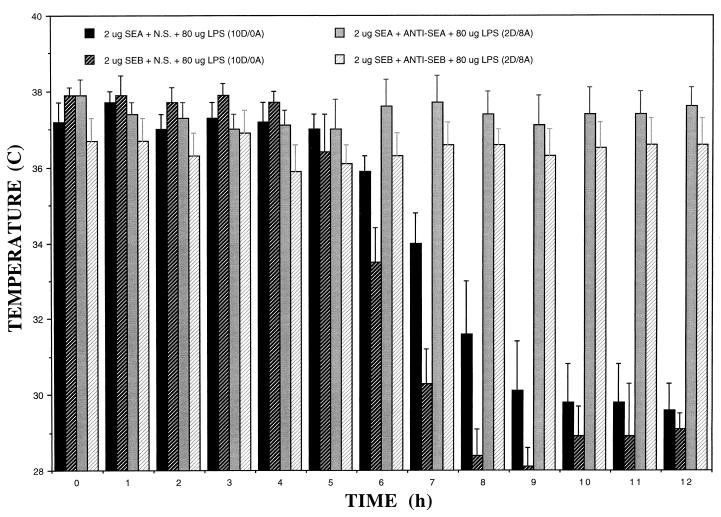
Upon establishing that hypothermia was a reliable parameter of SE or TSST-1 intoxication in mice following an i.p. injection, the next series of experiments determined if this effect was neutralized by toxin-specific antiserum. Goat anti-SEA, anti-SEB, or normal sera (200 μl/mouse) were premixed with SEA or SEB (2 μg/mouse) for 1 h at room temperature before an i.p. injection. Figure 1 shows that the temperature decrease was effectively neutralized in LPS-potentiated mice given hyperimmune serum, relative to that in controls administered toxin plus normal serum. Statistically significant differences in temperature were detected within 6 h and extended to 12 h, thus confirming the utility of temperature as a reliable and quick parameter for antibody neutralization studies.
FIG. 1.
Neutralization of SEA- or SEB-induced temperature decreases among BALB/c mice with anti-SEA or anti-SEB sera. N.S., normal sera. The numbers of dead (D) versus alive (A) mice were recorded at the 72-h time point and appear in parentheses.
Previous experiments with BALB/c or C57BL/6 mice suggest that levels of particular cytokines (IL-1, IL-6, TNF, and IFN-γ) in serum are elevated after an injection of SE or TSST-1 and a potentiating dose of LPS (32, 33, 39). To determine the role of individual cytokines or lymphocyte adhesion molecules like intercellular adhesion molecule 1 (ICAM-1) in temperature-based experiments, transgenic knockout C57BL/6 mice (Jackson Laboratories, Bar Harbor, Maine) were injected with SEA (10 μg) plus 170 μg of LPS (Table 3). Based on temperature and lethality, the molecules that had the most profound effect (i.e., protection) in this model when deleted were p55 TNF receptor > IFN-γ > p75 TNF receptor > ICAM-1 > IL-10. Although there was no difference in lethality or temperature among mice lacking IL-10 versus those of the wild type, all of the IL-10 knockout mice died within 24 h, which was quicker than the time frame of 24 to 58 h for the wild type. The SEA and LPS were necessary for an effect in IL-10 knockout mice, because PBS plus LPS (170 μg/animal) or SEA alone (100 μg/animal) did not elicit a temperature drop or lethality. These results correspond to previous studies suggesting that IL-10 has a protective role in SEB-induced shock, probably via down regulation of IL-1, IL-2, IL-6, TNF-α, and IFN-γ (2, 12, 13, 17).
TABLE 3.
Temperature effects of SEA plus LPS on transgenic knockout mice
| Mousea | Temp reading (°C) at b
|
Total no. of dead/alive micec | ||||
|---|---|---|---|---|---|---|
| 0 h | 3 h | 6 h | 9 h | 12 h | ||
| Wild type | 38.0 ± 0.3 | 37.9 ± 0.2* | 34.7 ± 1.3* | 29.7 ± 1.7* | 28.8 ± 1.0* | 10/0 |
| IL-10 knockout | 38.1 ± 0.7 | 37.1 ± 0.5 | 33.8 ± 1.7* | 29.4 ± 0.8* | 28.7 ± 0.8* | 10/0 |
| ICAM-1 knockout | 37.5 ± 0.4 | 37.3 ± 0.9* | 36.1 ± 1.2 | 31.4 ± 2.0* | 30.3 ± 1.6* | 9/1 |
| p75 TNF receptor knockout | 37.3 ± 0.7 | 36.7 ± 1.0 | 34.7 ± 1.9 | 31.3 ± 1.8* | 30.9 ± 1.2* | 7/3 |
| IFN-γ knockout | 36.9 ± 0.8 | 37.2 ± 0.5 | 34.9 ± 2.3 | 31.5 ± 2.2* | 33.2 ± 2.7 | 1/9 |
| p55 TNF receptor knockout | 38.5 ± 0.4* | 36.5 ± 0.5 | 37.3 ± 0.6 | 37.6 ± 0.5* | 36.1 ± 0.8 | 0/9 |
| Wild type (BSA + LPS control) | 37.7 ± 0.5 | 36.7 ± 0.6 | 37.2 ± 0.8 | 36.3 ± 0.9 | 35.4 ± 0.7 | 0/9 |
Mice were each injected i.p. with SEA (10 μg) plus LPS (170 μg). Wild-type controls were injected with BSA (10 μg) plus LPS (170 μg).
Mean temperature reading ± standard deviation of group designated at time points after the toxin injection (zero hour). *, statistically different (P < 0.01) from the wild-type controls given BSA plus LPS as determined by a two-tailed t test.
Recorded at 72 h.
In contrast to IL-10 knockout mice, the p55 TNF receptor and IFN-γ knockout mice were highly protected against the temperature and lethal effects of SEA plus LPS, thus suggesting that these molecules play an important role in toxicity. Previous studies with SEB or TSST-1 (19, 20) show that a neutralizing monoclonal antibody against TNF-α affords protection in a d-galactosamine-potentiated murine model. The p55 receptor for TNF also plays a major role in another LPS-potentiated murine model for SEB (5). Earlier studies report substantially increased amounts of TNF in mouse serum after an injection of SEA, SEB, or TSST-1 plus LPS (32, 33, 40), relative to those in controls given LPS alone, and this elevated level of TNF correlates well with lethality. Additionally, the experiments with IFN-γ knockout mice agree with previous studies showing that neutralizing antibodies against IFN-γ prevent superantigen-induced lethality (5, 12, 17). The role of IFN-γ in the superantigen-LPS synergy may lie in upregulation of the class II major histocompatibility complex and activation of STAT1 molecules that bind to promoter regions of various cytokine genes (5).
The final experiments were done with fas antigen-defective mice that hyperproduce the murine Vβ8.2 T-cell receptor (23). The T lymphocytes from these animals do not undergo superantigen-induced apoptosis and therefore continually produce potentially lethal concentrations of proinflammatory cytokines. It was hypothesized that a temperature deflection would be detected in these mice without a potentiating component like LPS. However, a 100-μg dose of SEB (i.p.) did not have any effect on temperature or lethality in our studies.
Temperature studies seem appropriate for these pyrogenic exotoxins, because they induce fever and in severe cases elicit a subsequent hypothermia, shock, and possibly death (4, 7). Besides abdominal cramps, vomiting, and diarrhea, victims of staphylococcal food poisoning often have a concomitant decrease in temperature (4). A previous report shows that rabbits given TSST-1 plus endotoxin (29), or TSST-1 alone (7), develop hypothermia following a transient fever. A recent study with rabbits injected with SEA alone reveals that the fever response is linked to increased levels of IFN-γ, TNF, IL-1, IL-2, and IL-6 in serum (14). In our murine studies, we did not see a temperature increase with the SEs or TSST-1, with or without LPS. However, proinflammatory cytokines like IFN-γ, TNF, IL-1, and IL-6 are maximally produced in the sera of LPS-potentiated mice within 6 to 8 h after a toxin injection (32, 33, 39, 40).
The hypothermic effects of endotoxin in rats (10), and probably mice (13), are linked to TNF concentrations which are greatly elevated in the LPS-potentiated mouse model for various staphylococcal superantigens (32, 33, 39). However, our current study clearly revealed that the LPS alone had negligible effects on temperature or lethality. There was an obvious synergistic effect between SEs or TSST-1 with LPS, which was easily detected by decreased temperatures. Additionally, the temperature fluctuations due to SEA or SEB were neutralized with toxin-specific antiserum, thus providing a quick in vivo method for determining antibody efficacy. The utility of a temperature-based murine model for testing vaccines against bacterial superantigens is currently being investigated by this laboratory.
Acknowledgments
The use of computer facilities at Shippensburg University was essential and much appreciated for timely statistical analysis of data. The fas antigen-defective mice were a kind gift of Carl Edwards. Goat anti-SEA and anti-SEB sera were generously provided by Mark Poli.
REFERENCES
- 1.Bavari S, Dyas B, Ulrich R G. Superantigen vaccines: a comparative study of genetically attenuated receptor-binding mutants of staphylococcal enterotoxin A. J Infect Dis. 1996;174:338–345. doi: 10.1093/infdis/174.2.338. [DOI] [PubMed] [Google Scholar]
- 2.Bean A G D, Freiberg R A, Andrade S, Menon S, Zlotnik A. Interleukin 10 protects mice against staphylococcal enterotoxin B-induced lethal shock. Infect Immun. 1993;61:4937–4939. doi: 10.1128/iai.61.11.4937-4939.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beezhold D H, Best G K, Bonventre P F, Thompson M. Synergistic induction of interleukin-1 by endotoxin and toxic shock syndrome toxin-1 using rat macrophages. Infect Immun. 1987;55:2865–2869. doi: 10.1128/iai.55.12.2865-2869.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bergdoll M S. Enterotoxins. In: Easmon C S F, Adlam C, editors. Staphylococci and staphylococcal infections. London, United Kingdom: Academic Press; 1983. pp. 559–598. [Google Scholar]
- 5.Blank C, Luz A, Bendigs S, Erdmann A, Wagner H, Heeg K. Superantigen and endotoxin synergize in the induction of lethal shock. Eur J Immunol. 1997;27:825–833. doi: 10.1002/eji.1830270405. [DOI] [PubMed] [Google Scholar]
- 6.Bohach G A, Fast D J, Nelson R D, Schlievert P M. Staphylococcal and streptococcal pyrogenic toxins involved in toxic shock syndrome and related illnesses. Crit Rev Microbiol. 1990;17:251–272. doi: 10.3109/10408419009105728. [DOI] [PubMed] [Google Scholar]
- 7.Bonventre P F, Thompson M R, Adinolfi L E, Gillis Z A, Parsonnet J. Neutralization of toxic shock syndrome toxin-1 by monoclonal antibodies in vitro and in vivo. Infect Immun. 1988;56:135–141. doi: 10.1128/iai.56.1.135-141.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bulanda M, Zaleska M, Mandel L, Talafantova M, Travnicek J, Kunstmann G, Mauff G, Pulverer G, Heczko P B. Toxicity of staphylococcal toxic shock syndrome toxin 1 for germ-free and conventional piglets. Rev Infect Dis. 1989;11:S248–S253. doi: 10.1093/clinids/11.supplement_1.s248. [DOI] [PubMed] [Google Scholar]
- 9.Chen J Y-J, Qiao Y, Komisar J L, Baze W B, Hsu I-C, Tseng J. Increased susceptibility to staphylococcal enterotoxin B intoxication in mice primed with actinomycin D. Infect Immun. 1994;62:4626–4631. doi: 10.1128/iai.62.10.4626-4631.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Derijk R H, Berkenbosch F. Hypothermia to endotoxin involves the cytokine tumor necrosis factor and the neuropeptide vasopressin in rats. Am J Physiol. 1994;266:R9–R14. doi: 10.1152/ajpregu.1994.266.1.R9. [DOI] [PubMed] [Google Scholar]
- 11.Fleischer B. Superantigens produced by infectious pathogens: molecular mechanism of action and biological significance. Int J Clin Lab Res. 1994;24:193–197. doi: 10.1007/BF02592461. [DOI] [PubMed] [Google Scholar]
- 12.Florquin S, Amraoui Z, Abramowicz D, Goldman M. Systemic release and protective role of IL-10 in staphylococcal enterotoxin B-induced shock in mice. J Immunol. 1994;153:2618–2623. [PubMed] [Google Scholar]
- 13.Gerard C, Bruyns C, Marchant A, Abramowicz D, Vandenabeele P, Delvaux A, Fiers W, Goldman M, Velu T. Interleukin 10 reduces the release of tumor necrosis factor and prevents lethality in experimental endotoxemia. J Exp Med. 1993;177:547–550. doi: 10.1084/jem.177.2.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huang W T, Lin M T, Won S J. Staphylococcal enterotoxin A-induced fever is associated with increased circulating levels of cytokines in rabbits. Infect Immun. 1997;65:2656–2662. doi: 10.1128/iai.65.7.2656-2662.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Keane W F, Gekker G, Schlievert P M, Peterson P K. Enhancement of endotoxin-induced isolated renal tubular cell injury by toxic shock syndrome toxin 1. Am J Pathol. 1986;122:169–176. [PMC free article] [PubMed] [Google Scholar]
- 16.Kim Y B, Watson D W. A purified group A streptococcal pyrogenic exotoxin. Physicochemical and biological properties including the enhancement of susceptibility to endotoxin lethal shock. J Exp Med. 1970;131:611–628. doi: 10.1084/jem.131.3.611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.LeClaire R D, Kell W, Bavari S, Smith T, Hunt R E. Protective effects of niacinamide in staphylococcal enterotoxin B induced toxicity. Toxicology. 1996;107:69–81. doi: 10.1016/0300-483x(95)03202-q. [DOI] [PubMed] [Google Scholar]
- 18.Luhm J, Kirchner H, Rink L. One-way synergistic effect of low superantigen concentrations on lipopolysaccharide-induced cytokine production. J Int Cytol Res. 1997;17:229–238. doi: 10.1089/jir.1997.17.229. [DOI] [PubMed] [Google Scholar]
- 19.Miethke T, Duschek K, Wahl C, Heeg K, Wagner H. Pathogenesis of the toxic shock syndrome: T cell mediated lethal shock caused by the superantigen TSST-1. Eur J Immunol. 1993;23:1494–1500. doi: 10.1002/eji.1830230715. [DOI] [PubMed] [Google Scholar]
- 20.Miethke T, Wahl C, Heeg K, Echtenacher B, Krammer P H, Wagner H. T cell mediated lethal shock triggered in mice by the superantigen staphylococcal enterotoxin B: critical role of tumor necrosis factor. J Exp Med. 1992;175:91–98. doi: 10.1084/jem.175.1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miethke T, Wahl C, Regele D, Gaus H, Heeg K, Wagner H. Superantigen mediated shock: a cytokine release syndrome. Immunobiology. 1993;189:270–284. doi: 10.1016/S0171-2985(11)80362-1. [DOI] [PubMed] [Google Scholar]
- 22.Mollick J A, Chintagumpala M, Cook R G, Rich R R. Staphylococcal exotoxin activation of T cells: role of exotoxin-MHC class II binding affinity and class II isotype. J Immunol. 1991;146:463–468. [PubMed] [Google Scholar]
- 23.Mountz J D, Baker T J, Borcherding D R, Bluethmann H, Zhou T, Edwards C K. Increased susceptibility of fas mutant MRL-lpr/lpr mice to staphylococcal enterotoxin B-induced septic shock. J Immunol. 1995;155:4829–4837. [PubMed] [Google Scholar]
- 24.Murai T, Nakagawa Y, Ogawa Y. Potentiation of lethal endotoxin shock by streptococcal pyrogenic exotoxin in rabbits: possible relevance of hyperreactivity of macrophages to endotoxin. FEMS Immunol Med Microbiol. 1996;13:269–272. doi: 10.1111/j.1574-695X.1996.tb00250.x. [DOI] [PubMed] [Google Scholar]
- 25.Muraille E, De Smedt T, Andris F, Pajak B, Armant M, Urbain J, Moser M, Leo O. Staphylococcal enterotoxin B induces an early and transient state of immunosuppression characterized by Vβ-unrestricted T cell unresponsiveness and defective antigen-presenting cell functions. J Immunol. 1997;158:2638–2647. [PubMed] [Google Scholar]
- 26.Parsonnet J, Gillis Z A. Production of tumor necrosis factor by human monocytes in response to toxic shock syndrome toxin-1. J Infect Dis. 1988;158:1026–1033. doi: 10.1093/infdis/158.5.1026. [DOI] [PubMed] [Google Scholar]
- 27.Priest B P, Schlievert P M, Dunn D L. Treatment of toxic shock syndrome with endotoxin-neutralizing antibody. J Surg Res. 1989;46:527–531. doi: 10.1016/0022-4804(89)90014-0. [DOI] [PubMed] [Google Scholar]
- 28.Sarawar S R, Blackman M A, Doherty P C. Superantigen shock in mice with an inapparent viral infection. J Infect Dis. 1994;170:1189–1194. doi: 10.1093/infdis/170.5.1189. [DOI] [PubMed] [Google Scholar]
- 29.Schlievert P M. Enhancement of host susceptibility to lethal endotoxin shock by staphylococcal pyrogenic exotoxin type C. Infect Immun. 1982;36:123–128. doi: 10.1128/iai.36.1.123-128.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schlievert P M, Watson D W. Group A streptococcal pyrogenic exotoxin: pyrogenicity, alteration of blood-brain barrier, and separation of sites for pyrogenicity and enhancement of lethal endotoxin shock. Infect Immun. 1978;21:753–763. doi: 10.1128/iai.21.3.753-763.1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Scholl P R, Diez A, Karr R, Sekaly R P, Trowsdale J, Geha R S. Effect of isotypes and allelic polymorphism on the binding of staphylococcal exotoxins to MHC class II molecules. J Immunol. 1990;144:226–230. [PubMed] [Google Scholar]
- 32.Stiles B G, Bavari S, Krakauer T, Ulrich R G. Toxicity of staphylococcal enterotoxins potentiated by lipopolysaccharide: major histocompatibility complex class II molecule dependency and cytokine release. Infect Immun. 1993;61:5333–5338. doi: 10.1128/iai.61.12.5333-5338.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stiles B G, Krakauer T, Bonventre P F. Biological activity of toxic shock syndrome toxin 1 and a site-directed mutant, H135A, in a lipopolysaccharide-potentiated mouse lethality model. Infect Immun. 1995;63:1229–1234. doi: 10.1128/iai.63.4.1229-1234.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stone R L, Schlievert P M. Evidence for the involvement of endotoxin in toxic shock syndrome. J Infect Dis. 1987;155:682–689. doi: 10.1093/infdis/155.4.682. [DOI] [PubMed] [Google Scholar]
- 35.Sugiyama H, McKissic E M, Bergdoll M S, Heller B. Enhancement of bacterial endotoxin lethality by staphylococcal enterotoxin. J Infect Dis. 1964;114:111–118. doi: 10.1093/infdis/114.2.111. [DOI] [PubMed] [Google Scholar]
- 36.Surgalla M J, Bergdoll M S, Dack G M. Some observations of the assay of staphylococcal enterotoxin by the monkey-feeding test. J Lab Clin Med. 1953;41:782–788. [PubMed] [Google Scholar]
- 37.Uchiyama T, Saito S, Inoko H, Yan X-J, Imanishi K, Araake M, Igarashi H. Relative activities of distinct isotypes of murine and human major histocompatibility complex class II molecules in binding toxic shock syndrome toxin 1 and determination of CD antigens expressed on T cells generated upon stimulation by the toxin. Infect Immun. 1990;58:3877–3882. doi: 10.1128/iai.58.12.3877-3882.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vella A T, McCormack J E, Linsley P S, Kappler J W, Marrack P. Lipopolysaccharide interferes with the induction of peripheral T cell death. Immunity. 1995;2:261–270. doi: 10.1016/1074-7613(95)90050-0. [DOI] [PubMed] [Google Scholar]
- 39.Woody M A, Krakauer T, Stiles B G. Staphylococcal enterotoxin B mutants (N23K and F44S): biological effects and vaccine potential in a mouse model. Vaccine. 1997;15:133–139. doi: 10.1016/s0264-410x(96)00166-1. [DOI] [PubMed] [Google Scholar]
- 40.Woody M A, Krakauer T, Ulrich R G, Stiles B G. Differential immune responses to staphylococcal enterotoxin B mutations in a hydrophobic loop dominating the interface with major histocompatibility complex class II receptors. J Infect Dis. 1998;177:1013–1022. doi: 10.1086/515250. [DOI] [PubMed] [Google Scholar]