The number of older adults requiring critical care has increased worldwide as the population ages. People aged 80 years and older represent the fastest growing subgroup in intensive care unit (ICU) admissions. In high-income countries, for example, they already constitute 15% and 20% of all ICU admissions [1–3]. Increasing evidence suggests that outcomes of older patients in ICU are not as poor as one might initially expect. Nonetheless, the appropriateness of admission to ICU remains context-specific. Where there are resource limitations and competing priorities for those beds, it would be better if decision-making incorporated objective parameters to answer core questions, like “Will this older patient benefit from ICU resources?” or “How to best care for this older patient with a critical illness?” Although we do not have the perfect answers to these questions, recent advances regarding older ICU patients are notable [4].
In older people, age-related conditions—frailty, cognitive impairment, functional disability, sensory deficits, comorbidities, polypharmacy—capture an overall baseline vulnerability, pivotal in estimating the patient’s ability to cope with acute insults (e.g., emergency surgery, septic shock) [5–7]. Such conditions share similar pathophysiology mechanisms, including neuromuscular weakness, decreased oxygen utilization, increased inflammation, and immunosenescence, all important in the ICU context. Thus, unlike robust older patients, those with high baseline vulnerability are susceptible to multi-system organ failure and adverse outcomes when facing an acute insult [7–9]. That is why ‘biological age’ differs from ‘chronological age’ and is essential for decision-making in older patients [4–6].
Heterogeneity is a hallmark of the older population, making it challenging to identify early—among older patients of similar age—those more likely to benefit from ICU resources and those in whom escalating acute care would be useless [5–7]. Physiological changes that affect vital signs (e.g., blunted heart rate response to stress) and laboratory findings (e.g., lower serum creatinine) predispose to atypical presentations of acute diseases as people age, particularly in those accumulating frailty and other age-related conditions [10]. Consequently, traditional prognostic tools [the Sequential Organ Failure Assessment (SOFA) score and Simplified Acute Physiology Score (SAPS) II] alone can also misclassify illness severity in older patients [5].
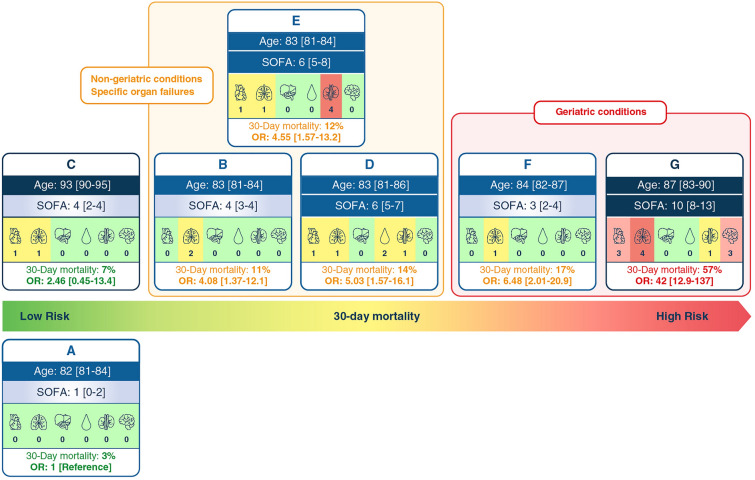
In this issue of Intensive Care Medicine, Mousai and colleagues offer cutting-edge knowledge on this topic [11]. These authors examined the heterogeneity of people aged 80 years and older in critical care by clustering analysis of bedside clinical variables assessed on admission to ICUs in 22 European countries, integrating the VIP2 cohort study [5]. Besides demographic factors, reasons for ICU admission, and SOFA scores, the authors considered information on age-related conditions, which allowed them to identify seven clusters with distinct phenotypes (Fig. 1) [11]. Notably, Mousai and colleagues confirmed the validity of the clusters by providing external validation in another dataset comprising critical care patients affected by coronavirus disease 2019 (COVID-19) (the COVIP study) and by incorporating initially excluded patients with limitations of life-sustaining treatment into sensitivity analyses [7].
Fig. 1.
Distinct clinical and prognostic profiles of older patients from the VIP2 cohort
For many years, ICU admissions in people aged 80 years and older were a synonym for suffering and moral distress in patients and families [4]. However, this view has proven to be superficial, as Mousai and colleagues showed while reporting divergent outcomes across the clusters (Fig. 1) [11]. While 30-day mortality reached 57% in the VIP2 patients with age-related conditions and high SOFA scores, it was only 7% among the oldest old patients presenting very mild age-related impairments and low SOFA scores. Other specific profiles denoting respiratory, cardiac, and renal failure had a 30-days mortality rate of around 10%, with only the phenotype presenting age-related conditions approaching nearly 20% of mortality risk, despite low SOFA scores [11].
Such findings corroborate practical implications. Experienced intensive care clinicians understand that age can attract frailty and other age-related conditions, and those latter factors are responsible for limited reserves to survive critical illness. It would not surprise that a frail patient with a high SOFA score has a very high risk of dying (cluster G). A frail patient in ICU without such a high SOFA score still has a considerable risk of dying (cluster F). On the contrary, an otherwise robust octogenarian (cluster A) or nonagenarian (cluster C), without an illness with high SOFA scores, is highly likely to survive an ICU admission. Mousai and colleagues innovated by presenting this whole picture as distinct phenotypes (Fig. 1), which could aid clinicians in conversations at the bedside on goals of care with patients and families (i.e., advanced care planning or decisions on withdrawing or withholding ICU treatments) [11–13].
Personalized medicine implies considering each patient individually to be able to manage specifically their health care. A midpoint between generalizing all ICU older patients and viewing each patient individually is to identify homogenous sub-groups constituted by patients who share similar clinical characteristics at a time point. In this way, cluster approaches aim to minimize the differences between similar individuals and maximize the differences between individuals with distinct features [14]. However, clustering is not an exact science as results depend on data and methodological approaches. For example, clusters F and G comprised 10% and 30% of patients living in nursing homes, respectively, prior to critical illness, subgroups that would often not be appropriate for ICU admissions. Although observed clusters identified by Mousai and colleagues can be considered solid sub-groups of older patients in the ICU, their findings in Europe lack generalisability to other ICU populations and contexts [11]. Furthermore, their findings were based on ICU and 30-day mortality, arguably very short-term outcomes for this cohort of patients. Future research should focus on patient-centred outcomes, as quality of life and functional measures are the most relevant health aspects for older ICU patients [12].
In conclusion, Mousai and colleagues leveraged routine and vulnerability measures that were obtained at the bedside to describe clusters of older patients sharing similar clinical and prognostic profiles on ICU admission [11]. The next step is looking at which interventions might be appropriate for the different clusters and which interventions might not be. This may involve not admitting older patients with high frailty and SOFA scores to ICU. It may involve providing short-term vasopressor support but not mechanical ventilation or dialysis to other patients. In the meantime, we should acknowledge that age is insufficient reasoning [15]—it is time to integrate geriatrics principles into critical care medicine.
Funding
MJRA is supported by a scholarship from Hospital das Clinicas HCFMUSP, Faculdade de Medicina, Universidade de Sao Paulo (HCFMUSP) with funds donated by Nubank under the #HCCOMVIDA scheme. SB is supported by research grants from the French National Research Agency in the framework of the ‘Investissements d’avenir’ program (ANR-15-IDEX-02) by MIAI @ Grenoble Alpes (ANR-19-P3IA-0003) and the ‘e-health and integrated care’ Chair of Excellence from the Grenoble Alpes University Foundation. The funders had no role in the preparation, review, or approval of the manuscript and decision on its submission.
Author contributions
MJRA, SB, and MA were substantially involved in drafting the manuscript. All authors critically revised the manuscript and approved the final version of the article.
Declarations
Conflicts of interest
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Robert R, Skrifvars MB, Ranzani OT. Is this critically ill patient elderly or too old? Intensive Care Med. 2017;43:1884–1886. doi: 10.1007/s00134-017-4965-z. [DOI] [PubMed] [Google Scholar]
- 2.Brummel NE, Ferrante LE. Integrating geriatric principles into critical care medicine: the time is now. Ann Am Thorac Soc. 2018;15:518–522. doi: 10.1513/AnnalsATS.201710-793IP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cobert J, Jeon SY, Boscardin J, Chapman AC, Ferrante LE, Lee S, Smith AK. Trends in geriatric conditions among older adults admitted to US ICUs between 1998 and 2015. Chest. 2022;161:1555–1565. doi: 10.1016/j.chest.2021.12.658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Flaatten H, de Lange DW, Artigas A, Bin D, Moreno R, Christensen S, Joynt GM, Bagshaw SM, Sprung CL, Benoit D, Soares M, Guidet B. The status of intensive care medicine research and a future agenda for very old patients in the ICU. Intensive Care Med. 2017;43:1319–1328. doi: 10.1007/s00134-017-4718-z. [DOI] [PubMed] [Google Scholar]
- 5.Guidet B, de Lange DW, Boumendil A, Leaver S, Watson X, Boulanger C, Szczeklik W, Artigas A, Morandi A, Andersen F, Zafeiridis T, Jung C, Moreno R, Walther S, Oeyen S, Schefold JC, Cecconi M, Marsh B, Joannidis M, Nalapko Y, Elhadi M, Fjølner J, Flaatten H. The contribution of frailty, cognition, activity of daily life and comorbidities on outcome in acutely admitted patients over 80 years in European ICUs: the VIP2 study. Intensive Care Med. 2020;46:57–69. doi: 10.1007/s00134-019-05853-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Montgomery C, Bagshaw SM. Frailty in the age of VIPs (very old intensive care patients) Intensive Care Med. 2017;43:1887–1888. doi: 10.1007/s00134-017-4974-y. [DOI] [PubMed] [Google Scholar]
- 7.Jung C, Flaatten H, Fjølner J, Bruno RR, Wernly B, Artigas A, Bollen Pinto B, Schefold JC, Wolff G, Kelm M, Beil M, Sviri S, van Heerden PV, Szczeklik W, Czuczwar M, Elhadi M, Joannidis M, Oeyen S, Zafeiridis T, Marsh B, Andersen FH, Moreno R, Cecconi M, Leaver S, Boumendil A, De Lange DW, Guidet B. The impact of frailty on survival in elderly intensive care patients with COVID-19: the COVIP study. Crit Care (London, England) 2021;25:149. doi: 10.1186/s13054-021-03551-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Muscedere J, Waters B, Varambally A, Bagshaw SM, Boyd JG, Maslove D, Sibley S, Rockwood K. The impact of frailty on intensive care unit outcomes: a systematic review and meta-analysis. Intensive Care Med. 2017;43:1105–1122. doi: 10.1007/s00134-017-4867-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Subramaniam A, Anstey C, Curtis JR, Ashwin S, Ponnapa Reddy M, Aliberti MJR, Avelino-Silva TJ, Welch C, Koduri G, Prowle JR, Wan YI, Laurent MR, Marengoni A, Lim JP, Pilcher D, Shekar K. Characteristics and outcomes of patients with frailty admitted to ICU with coronavirus disease 2019: an individual patient data meta-analysis. Crit Care Explor. 2022;4:e0616. doi: 10.1097/CCE.0000000000000616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Poco PCE, Aliberti MJR, Dias MB, Takahashi SF, Leonel FC, Altona M, Venys AL, Shin-Ike IA, Garcia BA, Sumita LH, Lima LMO, Garcez FB, Avelino-Silva TJ. Divergent: age, frailty, and atypical presentations of COVID-19 in hospitalized patients. J Gerontol A Biol Sci Med Sci. 2021;76:e46–e51. doi: 10.1093/gerona/glaa280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mousai O, Tafoureau L, Yovell T, Flaatten H, Guidet B, Jung C, de Lange D, Leaver S, Szczeklik W, Fjolner J, van Heerden PV, Joskowicz L, Beil M, Hyams G, Sviri S. Clustering analysis of geriatric and acute characteristics in a cohort of very old patients on admission to ICU. Intensive Care Med. 2022 doi: 10.1007/s00134-022-06868-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Taniguchi LU, Avelino-Silva TJ, Dias MB, Jacob-Filho W, Aliberti MJR. Patient-centered outcomes following COVID-19: frailty and disability transitions in critical care survivors. Crit Care Med. 2022;50:955–963. doi: 10.1097/CCM.0000000000005488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Taniguchi LU, Avelino-Silva TJ, Dias MB, Jacob-Filho W, Aliberti MJR. Association of frailty, organ support, and long-term survival in critically Ill patients with COVID-19. Crit Care Explor. 2022;4:e0712. doi: 10.1097/CCE.0000000000000712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Castela Forte J, Yeshmagambetova G, van der Grinten ML, Hiemstra B, Kaufmann T, Eck RJ, Keus F, Epema AH, Wiering MA, van der Horst ICC. Identifying and characterizing high-risk clusters in a heterogeneous ICU population with deep embedded clustering. Sci Rep. 2021;11:12109. doi: 10.1038/s41598-021-91297-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rivlin MM. Why the fair innings argument is not persuasive. BMC Med Ethics. 2000;1:E1. doi: 10.1186/1472-6939-1-1. [DOI] [PMC free article] [PubMed] [Google Scholar]