Abstract
Background
Endovascular thrombectomy is not available at all hospitals that offer intravenous thrombolysis, prompting debate regarding the preferred transport destination for acute ischemic stroke. This study aimed to quantify real-world travel time and distance of bypass and non-bypass transport models for large-vessel occlusion (LVO) and non-LVO stroke.
Methods
This cross-sectional study included population data of census tracts in the contiguous United States from the 2014-2018 United States Census Bureau’s American Community Survey, stroke (thrombolysis-capable) and thrombectomy-capable centers certified by a state or national body, and road network data from a mapping service. Census tracts were categorized by urbanization level. Data were retrieved March-November 2020. Travel times and distances were calculated for each census tract to each of the following: nearest stroke center (nearest), nearest thrombectomy-capable center (bypass), and nearest stroke center then to the nearest thrombectomy-capable center (transfer). Population-weighted median and interquartile range were calculated nationally and by urbanization.
Results
72,538 census tracts, 2,388 stroke hospitals, and 371 thrombectomy-capable centers were included. Nationally, population-weighted median travel time for nearest and bypass routing was 11.7 min (IQR 7.7, 19.3) and 26.4 min (14.8, 55.1), respectively. For transfer routing, the population-weighted median travel times with 60-min, 90-min, and 120-min door-in-door-out times were 94.1 min (78.5, 127.7), 124.1 min (108.5, 157.7), 154.1 min (138.4, 187.6), respectively.
Conclusions
Bypass routing offers modest travel time benefits for LVO patients and incurs modest penalties for non-LVO patients. Differences are greatest in rural areas. A majority of Americans live in areas for which current guidelines recommend bypass.
INTRODUCTION
In current practice, patients with acute ischemic stroke may warrant treatment with intravenous thrombolysis, endovascular thrombectomy (EVT), or both.1 However, EVT is not available at all hospitals that provide intravenous thrombolysis. Because acute stroke therapies are time-sensitive,2,3 emergency medical services must decide whether to transport patients with suspected acute ischemic stroke to the nearest stroke center, potentially delaying EVT, or bypass the nearest stroke center in favor of the nearest EVT-capable center, potentially delaying intravenous thrombolysis.
Quantifying the real-world travel time and distance associated with bypass and non-bypass models is key to understanding the role of hospital bypass in stroke care. However, relatively little prior work has compared the travel times of various transport strategies at the national level. In this cross-sectional study, we utilize large national datasets, including population data from the United States Census Bureau, stroke hospital data from national and state certifying organizations, and road networks from an online mapping service, to estimate the travel times and distances to appropriate stroke care in bypass and non-bypass models for the population of the United States nationally and by urbanization level.
METHODS
Data Sources
The data that support the findings of this study are available from the corresponding author upon reasonable request. The data sources of this study were public and not individually identifiable, and thus this study was exempt from review by our institutional review board.
Population data were obtained at the census tract level for all census tracts within the contiguous United States from the United States Census Bureau. Total population count of each census tract was obtained from the 2014-2018 American Community Survey 5-Year Estimates.4 The geographic coordinates of the population-weighted centroid for all census tracts were obtained from the United States Census Bureau’s Gazetteer Files.
Census tracts were classified by urbanization level using the 2010 rural-urban commuting area (RUCA) codes.5 The RUCA system integrates measures of population density, urbanization, and daily commuting. Tracts with RUCA code of 1 are defined as metropolitan area core and were classified as urban. Tracts with RUCA codes of 2 or 3, defined as metropolitan areas with high and low commuting respectively, were classified as suburban. Tracts with RUCA codes of 4-10, defined as non-metropolitan, small towns, or rural areas, were classified as rural.
Stroke hospital data were compiled from publicly available national and state level databases of stroke center certification. National-level certification data were obtained from the websites of Joint Commission, Healthcare Facilities Accreditation Program, or Det Norske Veritas Healthcare.6–8 Because many states possess their own list of designated stroke hospitals, state-level certification data were curated from websites of individual state governments, health departments and emergency medical services. Hospital addresses and certification levels as of November 2020 were recorded. Hospitals were classified as stroke centers if they were certified to provide at least intravenous thrombolysis, and as EVT-capable centers if they were certified to provide EVT. The geographic coordinates of all included hospitals were identified using Google Maps (www.google.com/maps).
Travel Time and Distance Estimation
For each census tract, total travel time and road distance was calculated for each of three scenarios: 1) patient transport to the nearest stroke center (nearest) to represent non-bypass transport routing for non-LVO patients; 2) patient transport to the nearest EVT-capable center (bypass) to represent bypass transport routing for all patients; and 3) patient transport to the nearest stroke center followed by inter-hospital transfer to the nearest EVT-capable center (transfer), unless the nearest stroke center was also EVT-capable, to represent non-bypass transport routing for LVO patients. For nearest and bypass routing, the population-weighted centroid of each census tract is taken as the origin and the appropriate hospital is taken as the destination. For transfer routing, the distance of nearest routing is added to the inter-hospital distance between the stroke hospital and its nearest EVT-capable center. Door-in-door-out (DIDO) times of 60, 90, and 120 minutes were added to transfer routing to account for time spent at the stroke hospital prior to transfer, unless the closest stroke hospital was also an EVT-capable center. To calculate the inter-hospital distance for this scenario, stroke hospitals were considered the origins and EVT-capable centers were the destinations.
Travel time and road distance were calculated using ArcGIS Pro software (Version 2.7, ESRI Inc, Redlands, CA) and the StreetMap Premium network dataset (2021 release, ESRI Inc, Redlands, CA). Routing analysis was used to find the closest destination to each origin and calculate the route with shortest travel time based on historical traffic data, speed limits, and other driving road restrictions such as one-way streets. Figure 1 shows a representative map of the different routing strategies for a single census tract.
Figure 1.
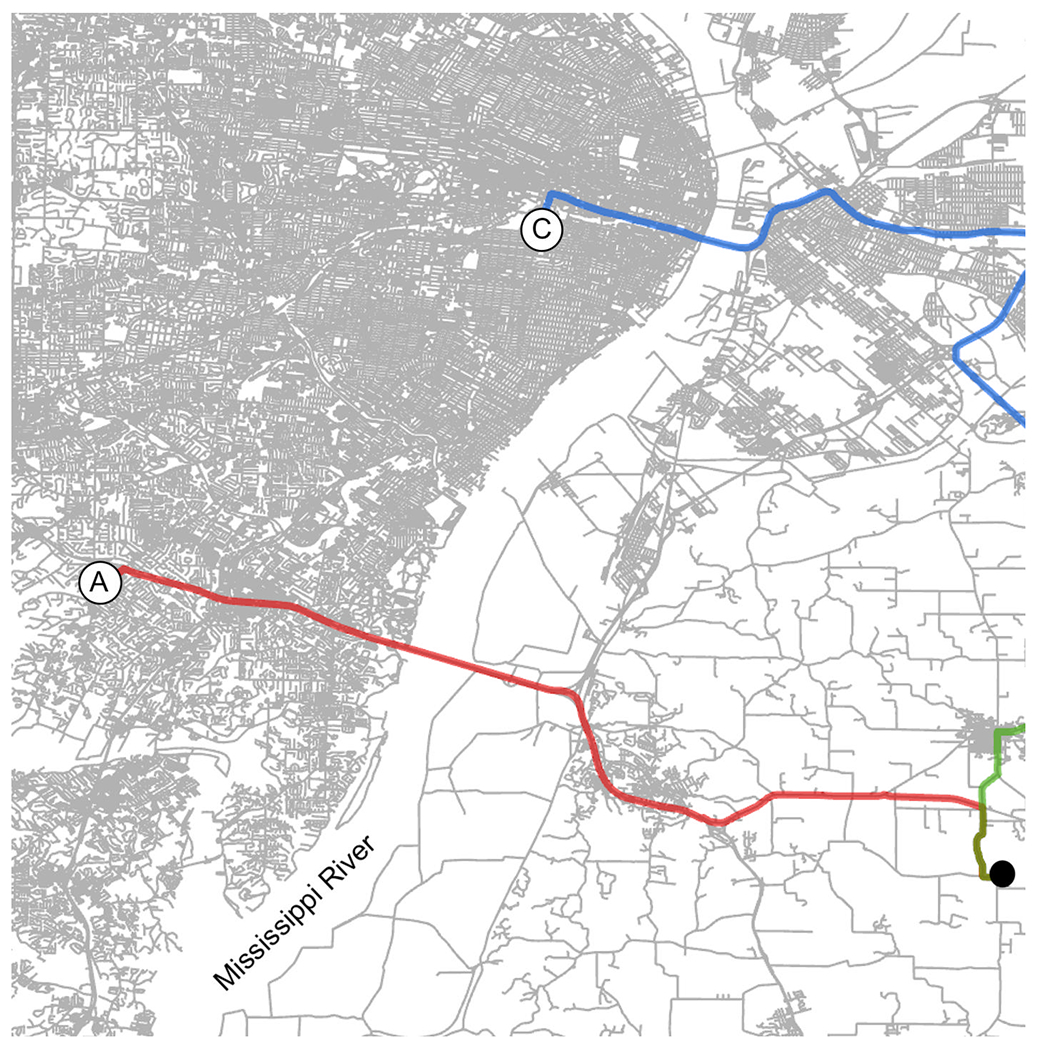
Representative map of transport routes from a census tract (closed black circle) near Saint Louis, Missouri. Bypass routing (red line) transports patients to the nearest EVT-capable center (A). Nearest routing (green line) transports patients to the nearest stroke center (B). Transfer routing comprises nearest routing plus inter-hospital transfer (blue line) to the nearest EVT-capable center (C) from the stroke center.
RESULTS
Of the 72,538 census tracts in the contiguous United States, 51,623 (71.2%) tracts were classified as urban, 7,432 (10.2%) as suburban, 13,201 (18.2%) as rural, and 282 (0.4%) did not have corresponding RUCA codes for classification. Hospitals included 2,388 stroke hospitals, of which 371 were EVT-capable centers.
Nationally, the population-weighted median total travel times for nearest and bypass routing were 11.7 min (IQR 7.7, 19.3) and 26.4 min (14.8, 55.1), respectively (Table 1, Figure 2). For transfer routing, the population-weighted median total travel times for 60-min, 90-min, and 120-min DIDO were 94.1 min (78.5, 127.7), 124.1 min (108.5, 157.7), 154.1 min (138.4, 187.6), respectively. Regardless of routing paradigm, travel times were longer in rural areas than in suburban areas, and longer in suburban areas than in urban areas (Figure 3). Nationally, the population-weighted median total distances for nearest, bypass, and transfer routing were 9.3 km (4.9, 20.0), 28.4 km (11.7, 76.1), and 35.3 km (15.3, 90.0), respectively.
Table 1.
Travel time and road distance for nearest, bypass, and transfer routing in patients with LVO and non-LVO stroke. Travel time for transfer routing include door-in-door-out (DIDO) times of 60, 90, and 120-minutes. All data are reported as median (IQR).
| Nearest | Bypass | Transfer | |||
|---|---|---|---|---|---|
|
| |||||
| Time (min) | 60-min DIDO | 90-min DIDO | 120-min DIDO | ||
| National | 11.7 (7.7, 19.3) | 26.4 (14.8, 55.1) | 94.1 (78.5, 127.7) | 124.1 (108.5, 157.7) | 154.1 (138.4, 187.6) |
| Urban | 9.9 (6.9, 13.7) | 19.8 (12.5, 32.9) | 87.5 (73.8, 102.8) | 117.5 (103.7, 132.8) | 147.5 (133.7, 162.8) |
| Suburban | 23.9 (17.8, 31.9) | 46.6 (33.7, 70.1) | 120.5 (100.5, 150.2) | 150.5 (130.5, 180.2) | 180.5 (160.5, 210.2) |
| Rural | 34.2 (18.4, 53.6) | 82.3 (57.8, 118.4) | 163.8 (130.3, 208.4) | 193.7 (160.2, 238.4) | 223.7 (190.1, 268.4) |
|
| |||||
| Distance (km) | |||||
|
| |||||
| National | 9.3 (4.9, 20.0) | 28.4 (11.7, 76.1) | 35.3 (15.3, 90.0) | ||
| Urban | 7.1 (4.1, 11.6) | 18.5 (9.0, 37.4) | 24.5 (11.1, 46.4) | ||
| Suburban | 27.6 (19.3, 39.6) | 60.6 (41.7, 99.1) | 75.2 (49.0, 123.2) | ||
| Rural | 44.0 (20.5, 74.6) | 122.1 (82.0, 182.1) | 148.8 (97.1, 222.4) | ||
Figure 2.
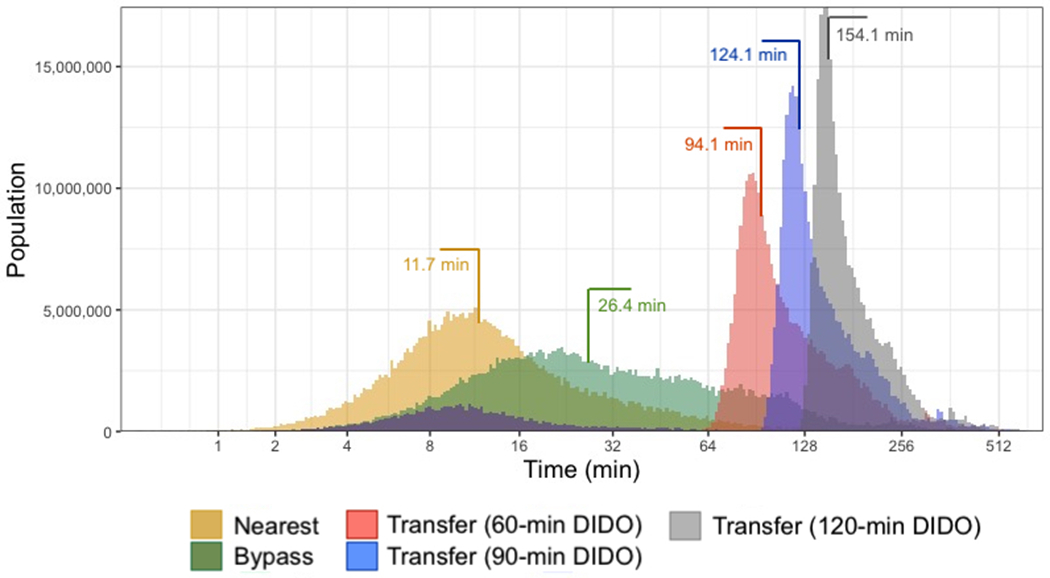
Population-weighted distributions of total travel time for nearest, bypass, and transfer routing at the national level. Travel times for transfer routing include door-in-door-out (DIDO) times of 60, 90, and 120 minutes. Colored lines and numbers indicate population-weighted median total travel time for each distribution.
Figure 3.
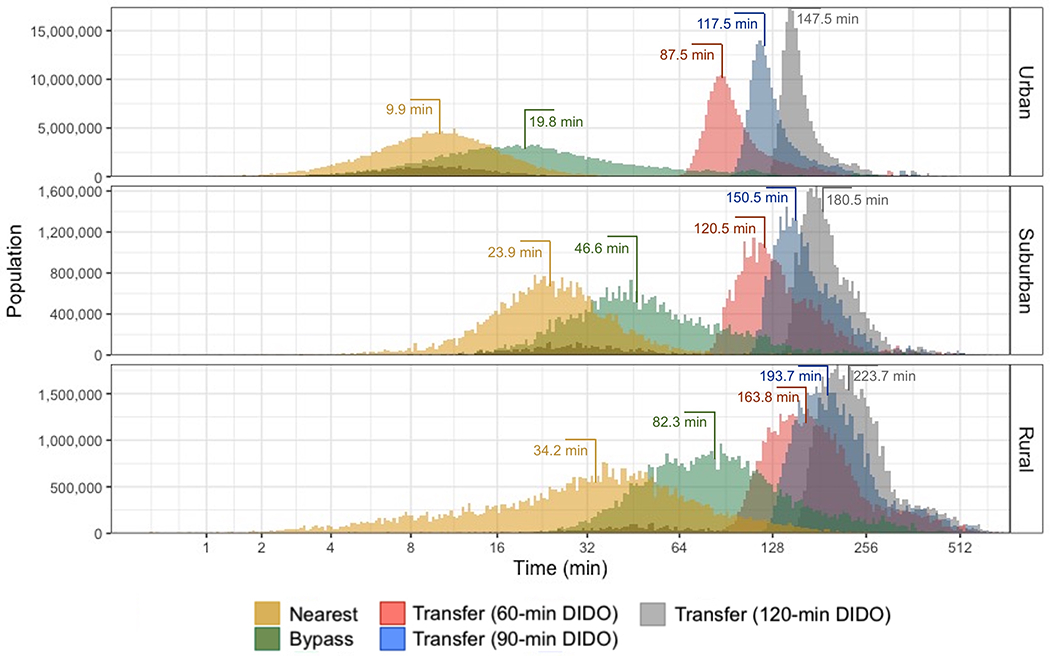
Population-weighted distributions of total travel time for nearest, bypass, and transfer routing separated by urbanization level. Travel times for transfer routing include door-in-door-out (DIDO) times of 60, 90, and 120 minutes. Colored lines and numbers indicate population-weighted median total travel time for each distribution.
With DIDO of 60 minutes, the fraction of patients that can reach an EVT-capable center within 120 minutes was 71.2% nationally, 85.7% in urban areas, 49.5% in suburban areas, and 16.8% in rural areas. With DIDO of 90 minutes, the fraction of patients that can reach an EVT-capable center within 120 minutes was 43.7% nationally, 55.6% in urban areas, 15.4% in suburban areas, and 6.5% in rural areas. With DIDO of 120 minutes, the fraction of patients that can reach an EVT-capable center within 120 minutes was 18.3% nationally, 21.6% in urban areas, 12.3% in suburban areas, and 6.4% in rural areas.
DISCUSSION
In this study, we rigorously quantified the travel time and distance of bypass and non-bypass transport strategies for acute ischemic stroke patients nationally and by urbanization level to determine the value of bypass routing both nationally and regionally. In the bypass routing strategy, stroke patients are transported directly to the nearest EVT-capable center, which may be farther than the nearest stroke center. In the non-bypass routing strategies, stroke patients are transported first to the nearest stroke center, where patients remain if found to have non-LVO stroke or are then transferred to an EVT-capable center if found to have LVO stroke. Nationally, bypass routing offered modest travel time and distance benefits for patients with LVO stroke and incurs modest penalties for patients with non-LVO stroke. The differences in travel times with bypass and non-bypass routing varied greatly by urbanization level, with less populated regions demonstrating larger differences.
The national median total travel time of 26.4 min for bypass routing suggests that at least 50% of Americans live within a 30-minute drive of an EVT-capable center. These findings generally comport with earlier studies9,10 and support the notion that bypassing the nearest stroke center in favor of an EVT-capable center can improve outcomes.13–15 Though the American Heart Association (AHA) has previously recommended bypass when an EVT-capable center was reachable within 30 minutes,11 recent studies have shown that a uniform application of bypass guidelines nationally is suboptimal.10,12 The AHA has quickly recognized the importance of regionalized transport strategies and in 2021 offered updated bypass guidelines tailored for urban, suburban, and rural environments.16,17 Our work builds on these efforts by quantifying the travel distance of bypass and non-bypass routing models based on urbanization level.
For urban areas, the AHA currently recommends direct transport of patients with suspected LVO to the nearest EVT-capable center if total travel time is less than 30 minutes, ostensibly to avoid the substantial “door in-door out” time penalty incurred in patients needing inter-hospital transfer.17–19 In urban settings, the median time for bypass was 19.8 min, which suggests that most Americans living in urban areas reside where bypass is recommended. Additionally, even for patients without LVO, the median time for bypass adds only a small time penalty compared to the median time for non-bypass of 9.9 minutes. These results together suggest that majority of the urban population of the United States meet the AHA guidelines for bypass without large time delays for non-LVO patients.
The median total travel time for bypass routing for non-LVO patients was higher in suburban and rural settings than in urban settings, reflecting the lower density of resources in these areas. The AHA currently recommends bypass if total travel time is less than 45 minutes in suburban areas and less than 60 minutes in rural areas.17 In suburban areas, the median time for bypass was 46.6 min, suggesting that nearly 50% of individuals in suburban areas meet the AHA thresholds for bypass. Refining pre-hospital triage of suspected LVO stroke may be particularly beneficial in these areas.20,21 In contrast, median travel time for bypass in rural settings was 82.3 min, suggesting that a minority of individuals in rural areas meet AHA thresholds for bypass. We therefore speculate that rural areas may benefit more from alternative approaches such as developing EVT capability, providing air transport, or establishing telehealth infrastructure.17
Shorter DIDO times are associated with better treatment outcomes for patients with LVO due to faster onset to recanalization time18, but real-world DIDO times are often greater than 60 minutes.19 This analysis aimed to quantitatively capture how various DIDO time thresholds impact access to stroke care. We found that with DIDO time of 90 minutes, almost 50% of LVO patients nationally were still within 120 minutes of an EVT-capable center with transfer routing. We also found stark regional variation in the impact of different DIDO thresholds on the ability to satisfy AHA bypass criteria. In urban areas, a DIDO time of 90 minutes allowed more than 50% of LVO patients to reach an EVT-capable center within 120 minutes via transfer routing. In contrast, fewer than 25% of LVO patients in rural areas could reach an EVT-capable center within 120 minutes, even with a shorter DIDO time of 60 minutes. In fact, the relative time delay for thrombolytic administration may be even smaller than the time delay for transport if EVT-capable centers have faster door-to-needle times than other centers.
Our study has several limitations. First, our methodology to identify stroke hospitals may omit hospitals that provide intravenous thrombolysis or EVT without national or state certification. However, using only certified centers ensures reproducibility and focuses on stroke care that meets recognized quality standards. Second, our study assumes patients are transported to the nearest hospital by travel time. Real-world decisions for transporting patients are more complex and patients may not always be taken to the nearest hospital. Finally, our distance and travel time calculations depend on the quality of data from databases of road networks and hospitals, which may contain some inaccuracies.
CONCLUSIONS
Nationally, bypass routing has a modest travel time and distance benefit for patients with LVO stroke and a modest penalty for patients with non-LVO stroke. The impact of bypass on total transport distance is larger in less populated regions. A majority of Americans live in areas for which AHA guidelines recommend bypass of the nearest stroke center for an EVT-capable center.
Sources of funding
This work was supported by the National Center for Advancing Translational Sciences under award number TL1TR002344.
Footnotes
Disclosures
C.Y. Yu, P.D. Panagos, and A.P. Kansagra report no disclosures relevant to the manuscript.
REFERENCES
- 1.Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50(12):E344–E418. doi: 10.1161/STR.0000000000000211 [DOI] [PubMed] [Google Scholar]
- 2.Saver JL, Goyal M, Van Der Lugt A, et al. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: A Meta-analysis. JAMA. 2016;316(12):1279–1289. doi: 10.1001/jama.2016.13647 [DOI] [PubMed] [Google Scholar]
- 3.Saver JL, Fonarow GC, Smith EE, et al. Time to treatment with intravenous tissue plasminogen activator and outcome from acute ischemic stroke. JAMA. 2013;309(23):2480–2488. doi: 10.1001/jama.2013.6959 [DOI] [PubMed] [Google Scholar]
- 4.US Census Bureau. American Community Survey 5-Year Estimate. Accessed May 1, 2020. https://data.census.gov.
- 5.Rural-Urban Commuting Area Codes. USDA Economic Research Service. Accessed April 1, 2021. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/
- 6.Stroke Certification | The Joint Commission. https://www.jointcommission.org/. Accessed May 1, 2020.
- 7.Healthcare Facilities Accreditations Program. Accessed May 1, 2020. https://www.hfap.org/.
- 8.DNV GL Healthcare. Stroke Care Certification Program. Accessed May 1, 2020. https://www.dnvgl.us/assurance/healthcare/stroke-certs.html.
- 9.Aldstadt J, Waqas M, Yasumiishi M, et al. Mapping access to endovascular stroke care in the USA and implications for transport models. J Neurointerv Surg. Published online 2021. doi: 10.1136/neurintsurg-2020-016942 [DOI] [PubMed] [Google Scholar]
- 10.Sarraj A, Savitz S, Pujara D, et al. Endovascular Thrombectomy for Acute Ischemic Strokes: Current US Access Paradigms and Optimization Methodology. Stroke. 2020;51(4):1207–1217. doi: 10.1161/STROKEAHA.120.028850 [DOI] [PubMed] [Google Scholar]
- 11.Mission: Lifeline Stroke Severity-Based Stroke Triage Algorithm for EMS. American Heart Association. Published 2020. Accessed February 26, 2021. https://www.heart.org/en/professional/quality-improvement/mission-lifeline/mission-lifeline-stroke [Google Scholar]
- 12.Venema E, Burke JF, Roozenbeek B, et al. Prehospital Triage Strategies for the Transportation of Suspected Stroke Patients in the United States. Stroke. 2020;51:3310–3319. doi: 10.1161/STROKEAHA.120.031144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mueller-Kronast N, Froehler MT, Jahan R, Zaidat O, Liebeskind D, Saver JL. Impact of EMS bypass to endovascular capable hospitals: Geospatial modeling analysis of the US STRATIS registry. J Neurointerv Surg. 2020;12(11):1058–1063. doi: 10.1136/neurintsurg-2019-015593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhou MH, Kansagra AP. Effect of routing paradigm on patient centered outcomes in acute ischemic stroke. J Neurointerv Surg. 2019;11(8):762–767. doi: 10.1136/neurintsurg-2018-014537 [DOI] [PubMed] [Google Scholar]
- 15.Holodinsky JK, Williamson TS, Demchuk AM, et al. Modeling Stroke Patient Transport for All Patients with Suspected Large-Vessel Occlusion. JAMA Neurol. 2018;75(12):1477–1486. doi: 10.1001/jamaneurol.2018.2424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Acker JE, Pancioli AM, Crocco TJ, et al. Implementation strategies for emergency medical services within stroke systems of care: A policy statement from the American Heart Association/American Stroke Association expert panel on emergency medical services systems and the stroke council. Stroke. 2007;38(11):3097–3115. doi: 10.1161/STROKEAHA.107.186094 [DOI] [PubMed] [Google Scholar]
- 17.Jauch EC, Schwamm LH, Panagos PD, et al. Recommendations for Regional Stroke Destination Plans in Rural, Suburban, and Urban Communities From the Prehospital Stroke System of Care Consensus Conference. Stroke. 2021;52. doi: 10.1161/STROKEAHA.120.033228 [DOI] [PubMed] [Google Scholar]
- 18.McTaggart RA, Moldovan K, Oliver LA, et al. Door-in-door-out time at primary stroke centers may predict outcome for emergent large vessel occlusion patients. Stroke. 2018;49(12):2969–2974. doi: 10.1161/STROKEAHA.n8.021936 [DOI] [PubMed] [Google Scholar]
- 19.Froehler MT, Saver JL, Zaidat OO, et al. Interhospital Transfer Before Thrombectomy Is Associated With Delayed Treatment and Worse Outcome in the STRATIS Registry (Systematic Evaluation of Patients Treated With Neurothrombectomy Devices for Acute Ischemic Stroke). Circulation. 2017;136(24):2311–2321. doi: 10.1161/CIRCULATIONAHA.n7.028920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jayaraman MV, Hemendinger ML, Baird GL, et al. Field triage for endovascular stroke therapy: A population-based comparison. J Neurointerv Surg. 2020;12(3):233–239. doi: 10.1136/neurintsurg-2019-015033 [DOI] [PubMed] [Google Scholar]
- 21.Zhao H, Coote S, Pesavento L, et al. Large Vessel Occlusion Scales Increase Delivery to Endovascular Centers Without Excessive Harm from Misclassifications. Stroke. 2017;48(3):568–573. doi: 10.1161/STROKEAHA.n6.016056 [DOI] [PubMed] [Google Scholar]


